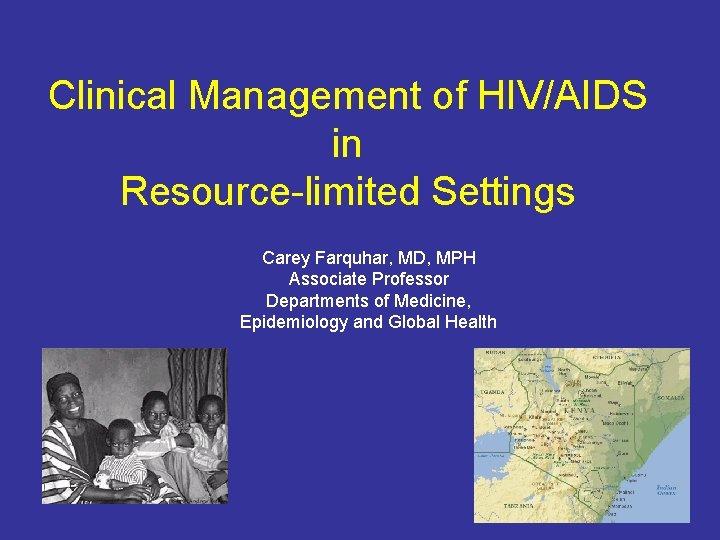
Clinical Management of HIVAIDS in Resourcelimited Settings Carey





- Slides: 51
Clinical Management of HIV/AIDS in Resource-limited Settings Carey Farquhar, MD, MPH Associate Professor Departments of Medicine, Epidemiology and Global Health
Outline • Special considerations • Natural history • Opportunistic infections • Antiretroviral therapy • Prevention of HIV transmission – Heterosexual – Mother-to-child
Kenya
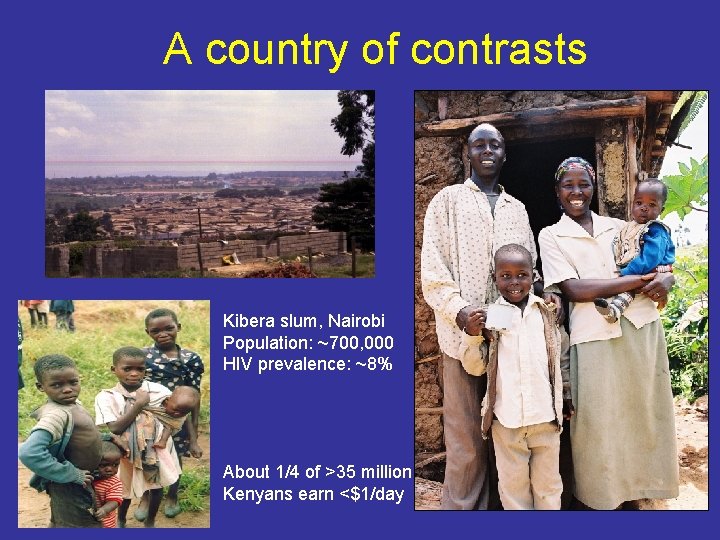
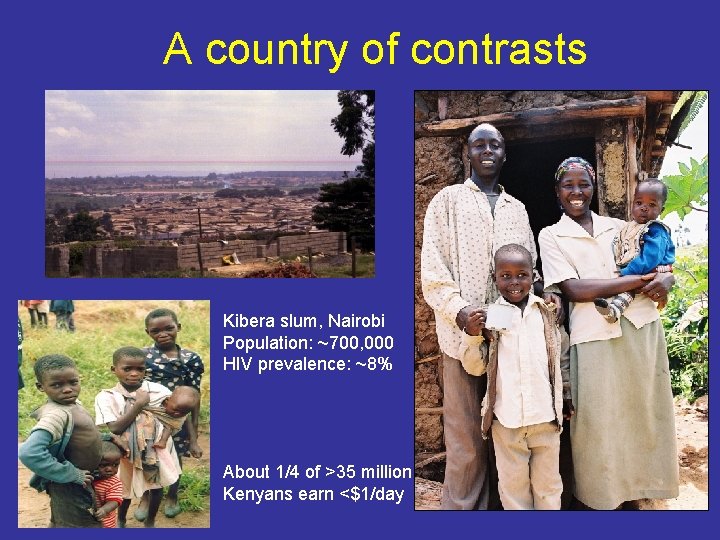
A country of contrasts Kibera slum, Nairobi Population: ~700, 000 HIV prevalence: ~8% About 1/4 of >35 million Kenyans earn <$1/day

Unique issues in developing countries Women and children Orphans Lack of resources Stigma
Stigma HIV infected persons suffer from discrimination, abuse, rejection, and abandonment. People often refuse HIV testing, do not disclose HIV status, or seek care.
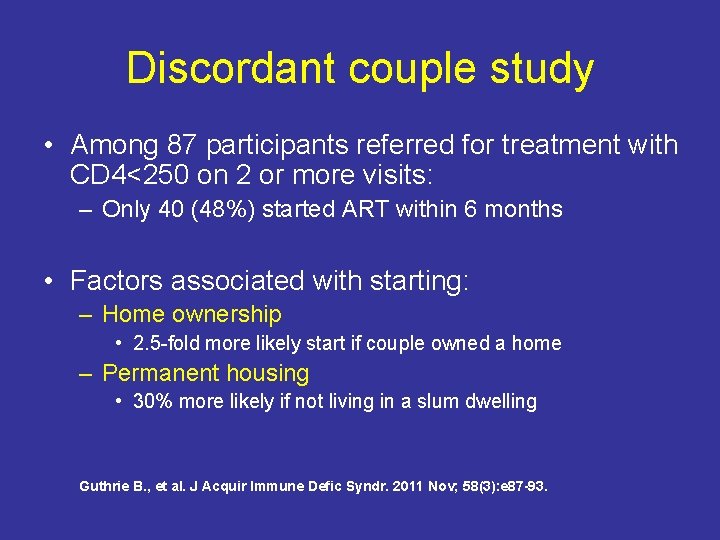
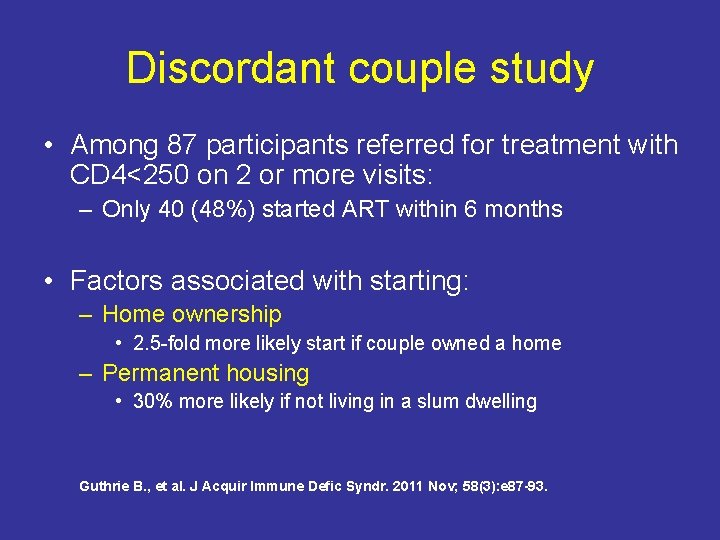
Discordant couple study • Among 87 participants referred for treatment with CD 4<250 on 2 or more visits: – Only 40 (48%) started ART within 6 months • Factors associated with starting: – Home ownership • 2. 5 -fold more likely start if couple owned a home – Permanent housing • 30% more likely if not living in a slum dwelling Guthrie B. , et al. J Acquir Immune Defic Syndr. 2011 Nov; 58(3): e 87 -93.
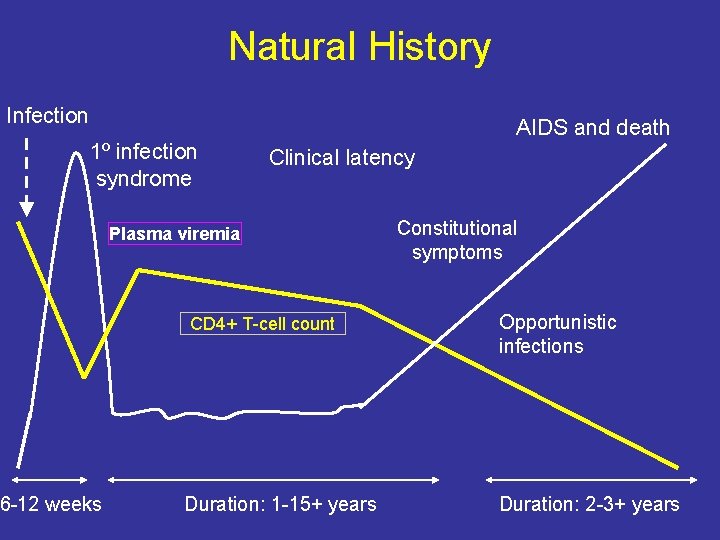
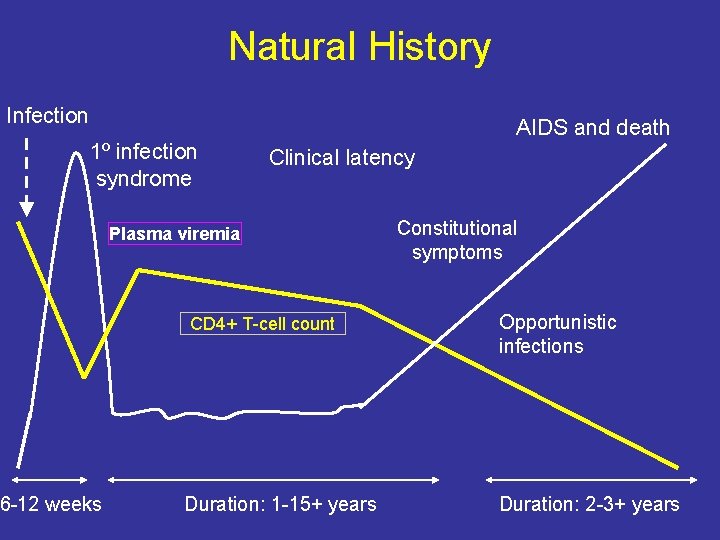
Natural History Infection 1º infection syndrome 6 -12 weeks AIDS and death Clinical latency Plasma viremia CD 4+ T-cell count Duration: 1 -15+ years Constitutional symptoms Opportunistic infections Duration: 2 -3+ years
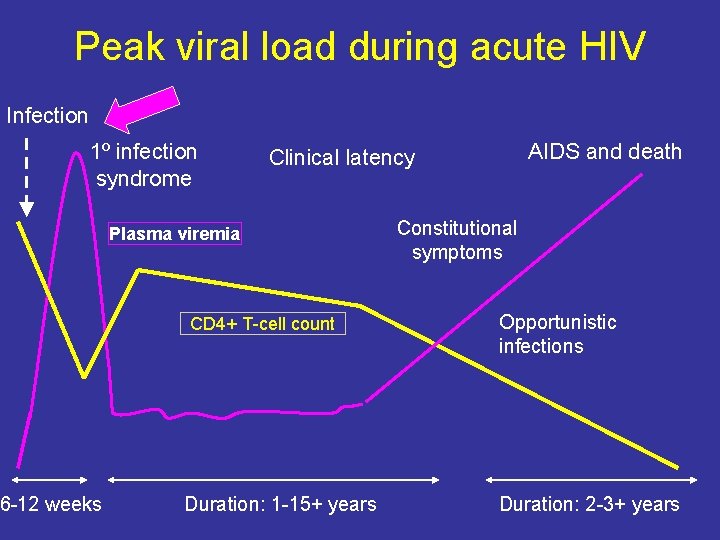
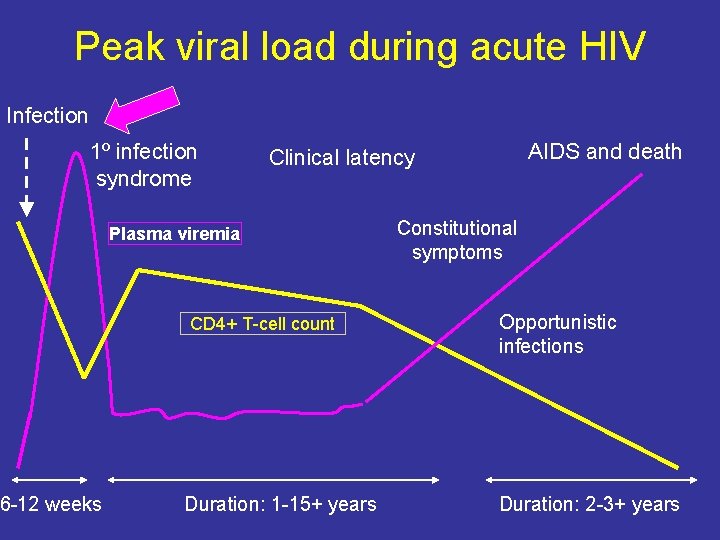
Peak viral load during acute HIV Infection 1º infection syndrome 6 -12 weeks AIDS and death Clinical latency Plasma viremia CD 4+ T-cell count Duration: 1 -15+ years Constitutional symptoms Opportunistic infections Duration: 2 -3+ years
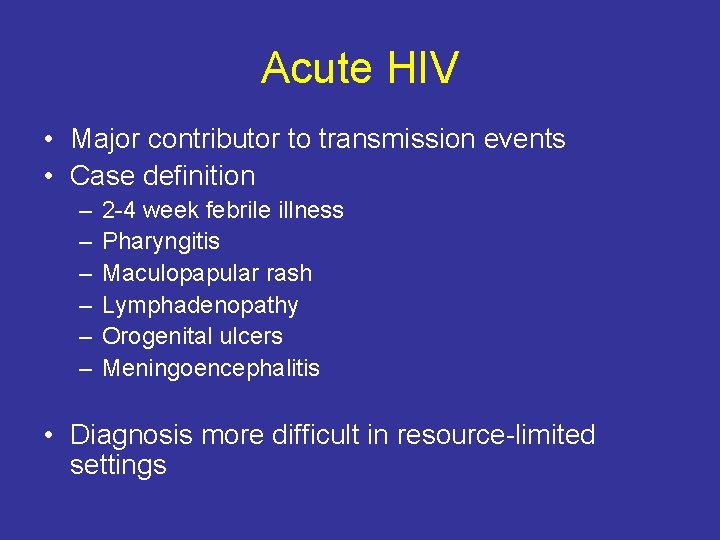
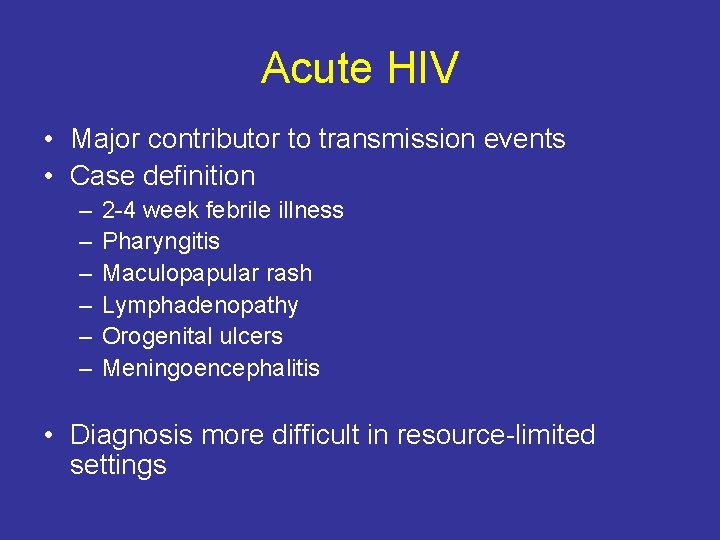
Acute HIV • Major contributor to transmission events • Case definition – – – 2 -4 week febrile illness Pharyngitis Maculopapular rash Lymphadenopathy Orogenital ulcers Meningoencephalitis • Diagnosis more difficult in resource-limited settings
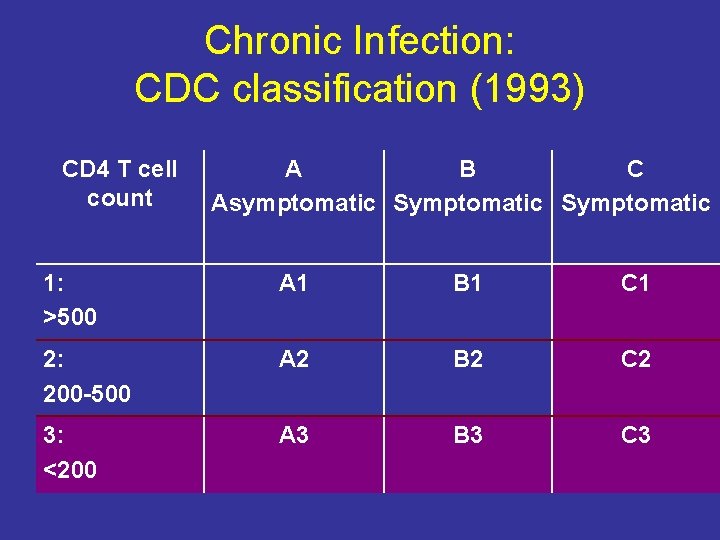
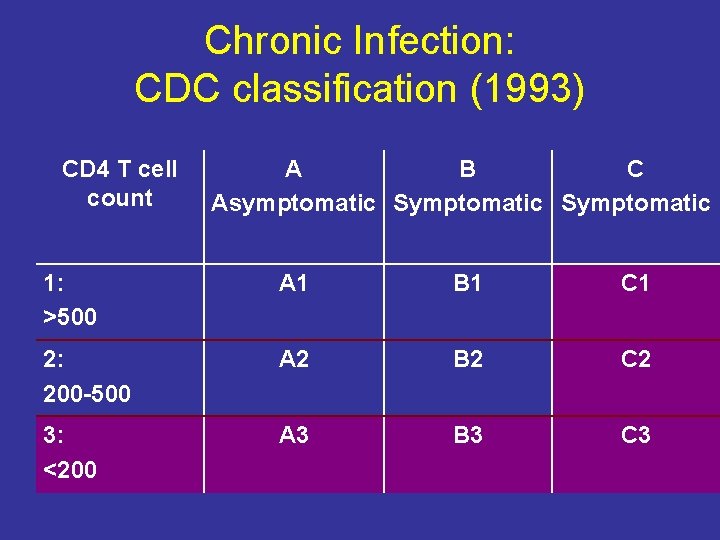
Chronic Infection: CDC classification (1993) CD 4 T cell count A B C Asymptomatic Symptomatic 1: >500 A 1 B 1 C 1 2: 200 -500 A 2 B 2 C 2 3: <200 A 3 B 3 C 3
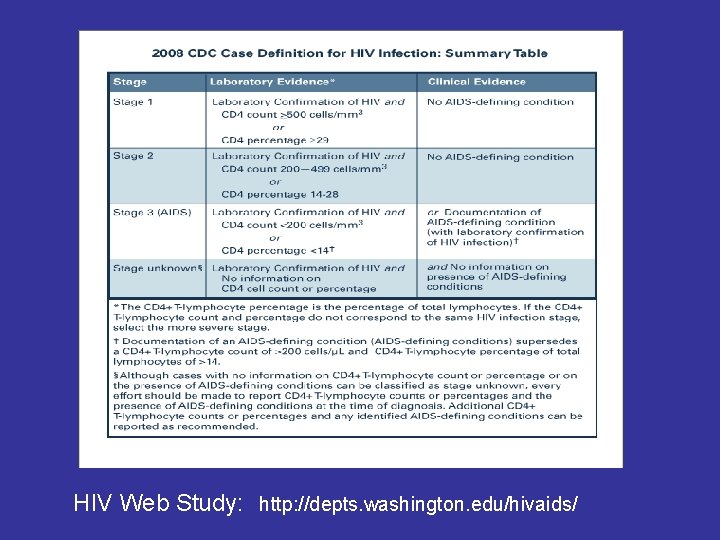
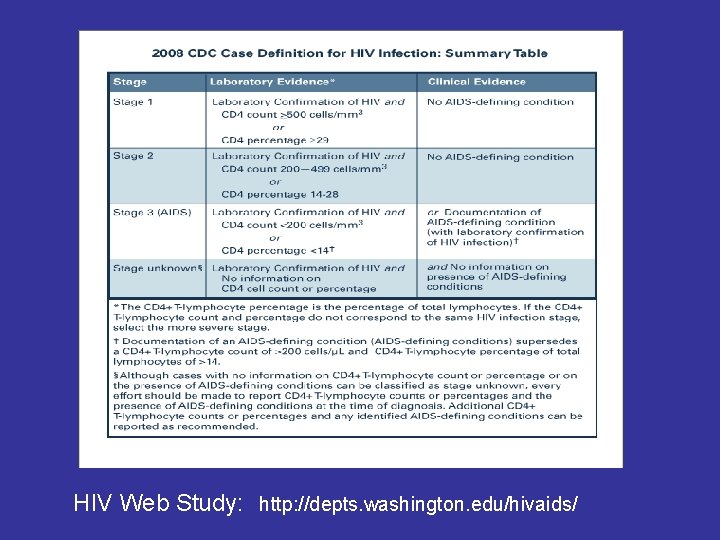
HIV Web Study: http: //depts. washington. edu/hivaids/
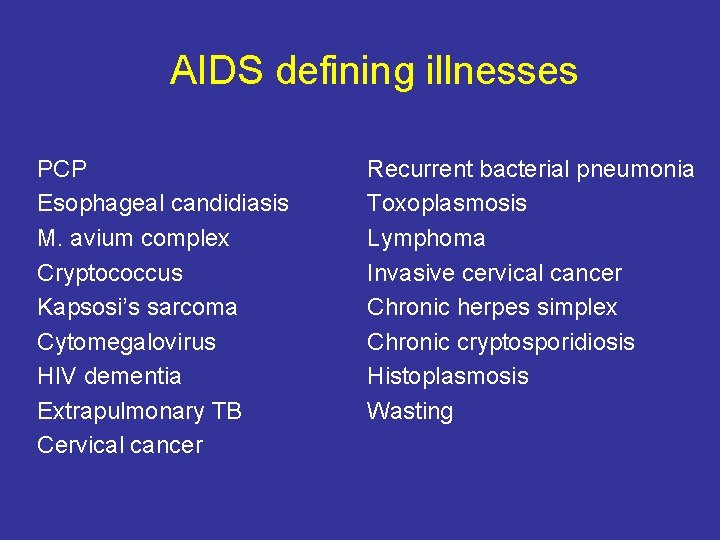
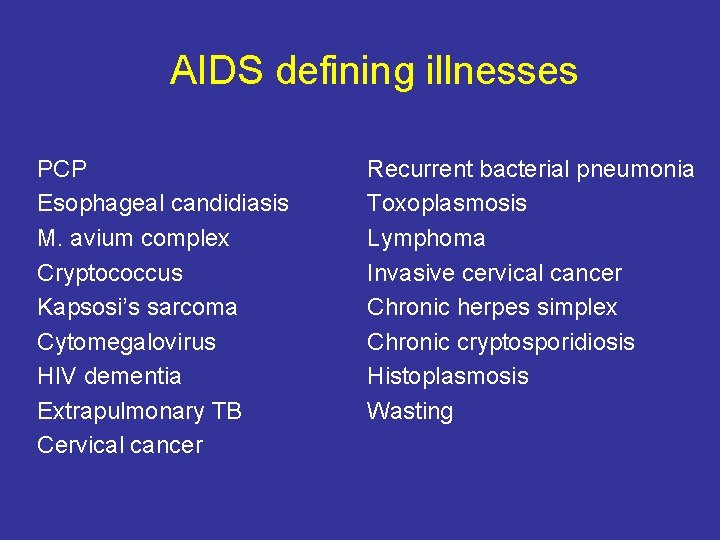
AIDS defining illnesses PCP Esophageal candidiasis M. avium complex Cryptococcus Kapsosi’s sarcoma Cytomegalovirus HIV dementia Extrapulmonary TB Cervical cancer Recurrent bacterial pneumonia Toxoplasmosis Lymphoma Invasive cervical cancer Chronic herpes simplex Chronic cryptosporidiosis Histoplasmosis Wasting
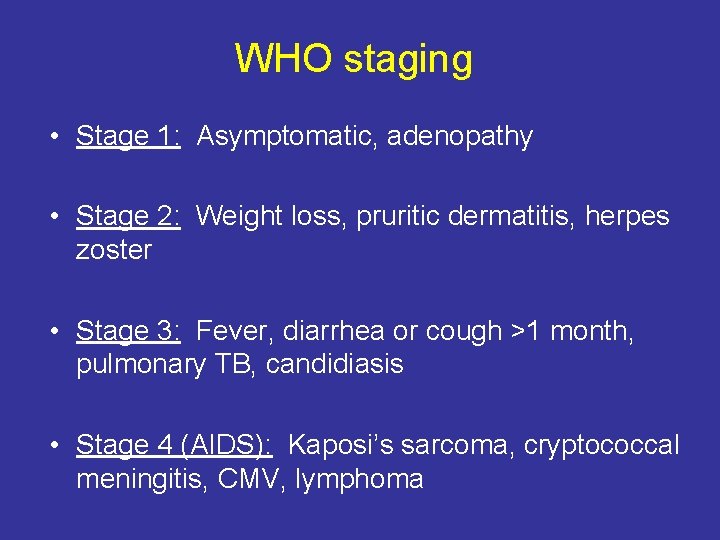
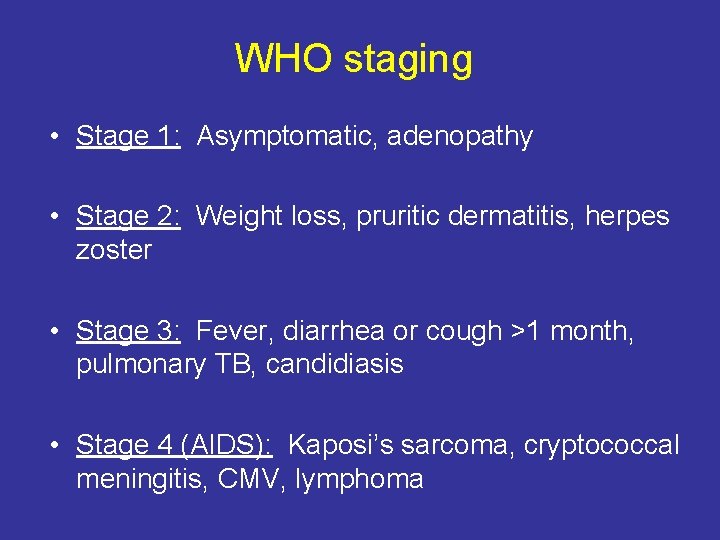
WHO staging • Stage 1: Asymptomatic, adenopathy • Stage 2: Weight loss, pruritic dermatitis, herpes zoster • Stage 3: Fever, diarrhea or cough >1 month, pulmonary TB, candidiasis • Stage 4 (AIDS): Kaposi’s sarcoma, cryptococcal meningitis, CMV, lymphoma
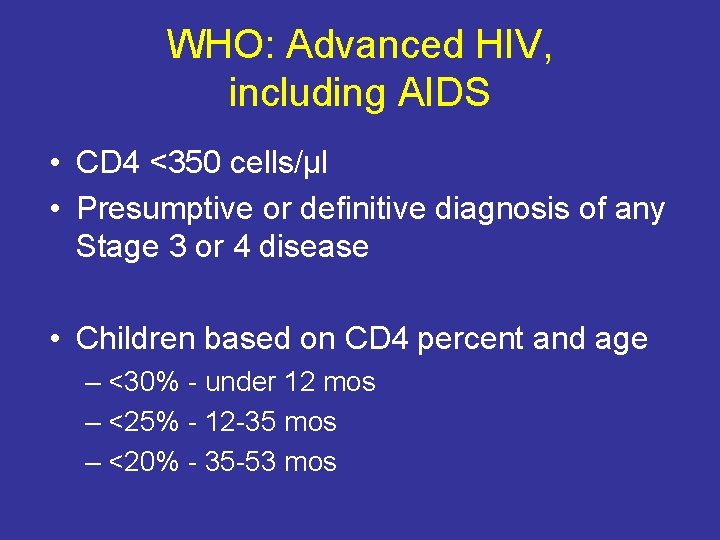
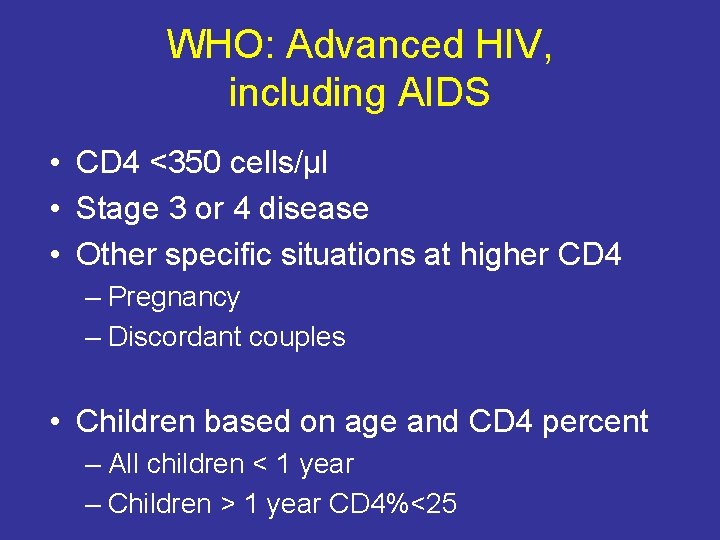
WHO: Advanced HIV, including AIDS • CD 4 <350 cells/μl • Presumptive or definitive diagnosis of any Stage 3 or 4 disease • Children based on CD 4 percent and age – <30% - under 12 mos – <25% - 12 -35 mos – <20% - 35 -53 mos
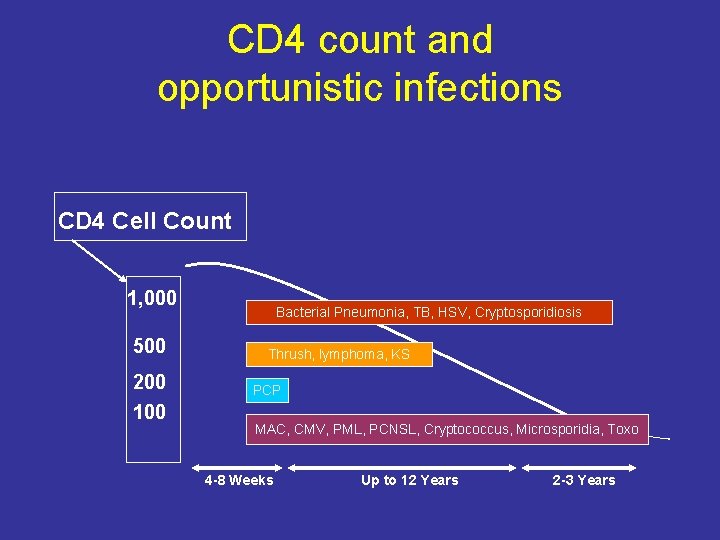
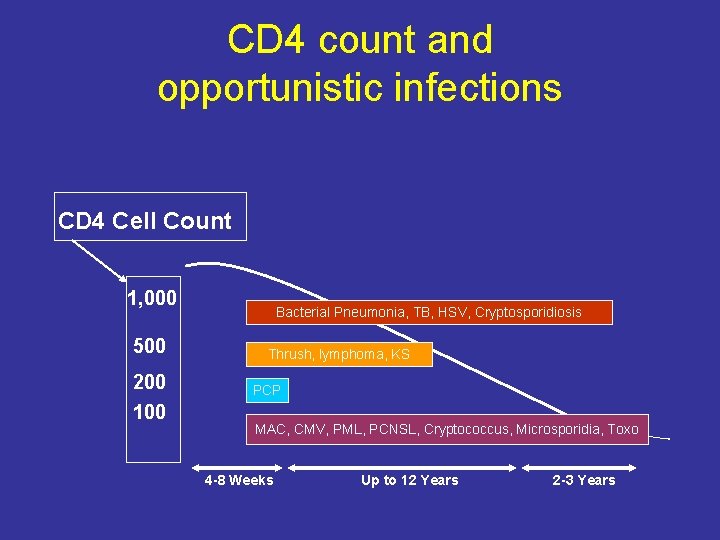
CD 4 count and opportunistic infections CD 4 Cell Count 1, 000 500 200 100 Bacterial Pneumonia, TB, HSV, Cryptosporidiosis Thrush, lymphoma, KS PCP MAC, CMV, PML, PCNSL, Cryptococcus, Microsporidia, Toxo 4 -8 Weeks Up to 12 Years 2 -3 Years
Common AIDS-related conditions in Africa • • Candidiasis Tuberculosis Malaria Cryptococcal meningitis Kaposi’s sarcoma HSV/VZV Pneumococcal pneumonia Skin problems – Atopic dermatitis • Salmonellosis
Salmonella enteritis • In Cote d’Ivoire, bacterial enteritis accounted for 7% of admissions to ID hospital – Salmonella typhi most common among hospitalized patients with enteritis • Non-typhoidal salmonella species: – 18 -20% of blood stream infections in Tanzania, Uganda, and Malawi – 7 -12% in Kenya and Cote d’Ivoire
Less common • Mycobacterium avium complex (MAC) • Pneumocystis jiroveci pneumonia (PCP) • Cytomegalovirus retinitis (CMV) Why is this?
Case #1 You are working in the Hope Clinic in Nairobi. An HIV-1 infected women complains of not being able to eat for 3 days. She has had severe pain with swallowing. Her last CD 4 count was 250 (1 year ago) What is your diagnosis and what are your recommendations?


Case #2 You are spending a month at a rural hospital in South Africa and have admitted a women with headache, confusion, and fever. She also has a rash. She is HIV-infected but does not know her CD 4 count and is not taking any medications. She has been healthy up until this point. What is your differential diagnosis?

Mandell, Atlas of Infectious Diseases
Management of cryptococcal meningitis • Challenging to treat – Amphotericin B plus flucytosine best regimen • Toxic, expensive, intravenous – Consolidation and maintenance costly • Threshold to stop fluconazole is CD 4>100 – Early initiation of ART associated with high mortality • 3 -fold higher among those starting ART w/in 72 hrs – WHY?
Case #3 A man with unknown HIV status presents to the clinic where you are working in Western Kenya. He has skin breakdown on his penis and groin with ulceration and purulence. What is on your differential and what should you offer him?

Pediatric HIV infection
The HIV epidemic in children • 90% infected through maternal transmission – In utero, during delivery, via breastfeeding • Annual incidence of ~500, 000 cases • 3 million children living with HIV/AIDS in Africa
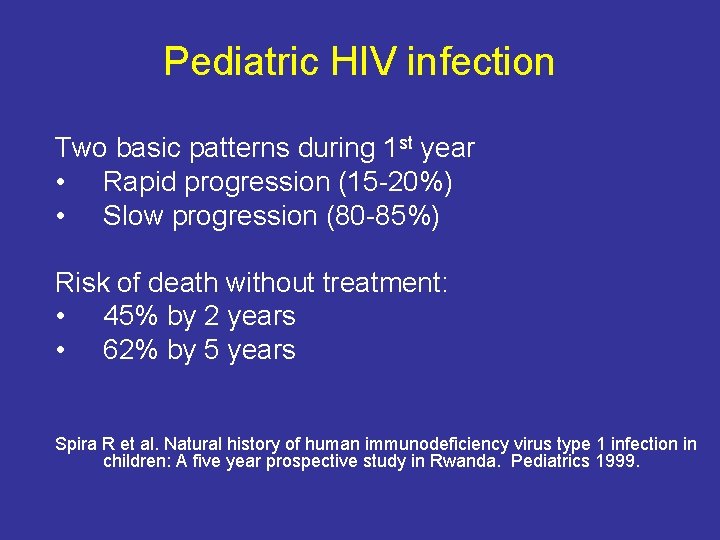
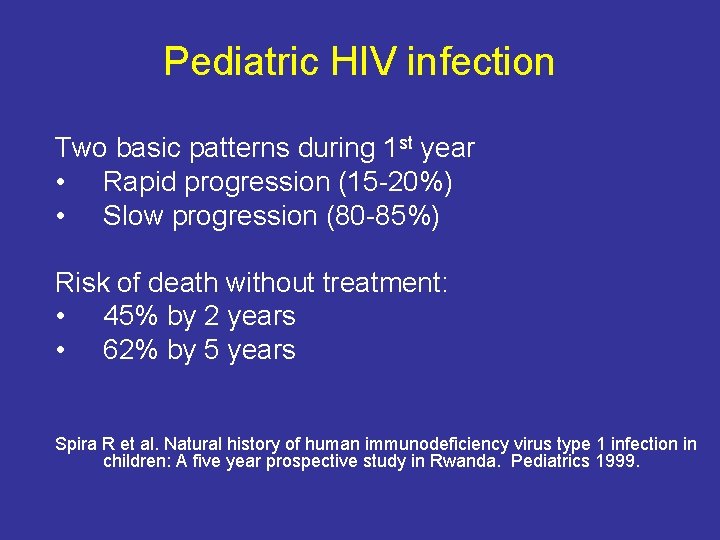
Pediatric HIV infection Two basic patterns during 1 st year • Rapid progression (15 -20%) • Slow progression (80 -85%) Risk of death without treatment: • 45% by 2 years • 62% by 5 years Spira R et al. Natural history of human immunodeficiency virus type 1 infection in children: A five year prospective study in Rwanda. Pediatrics 1999.
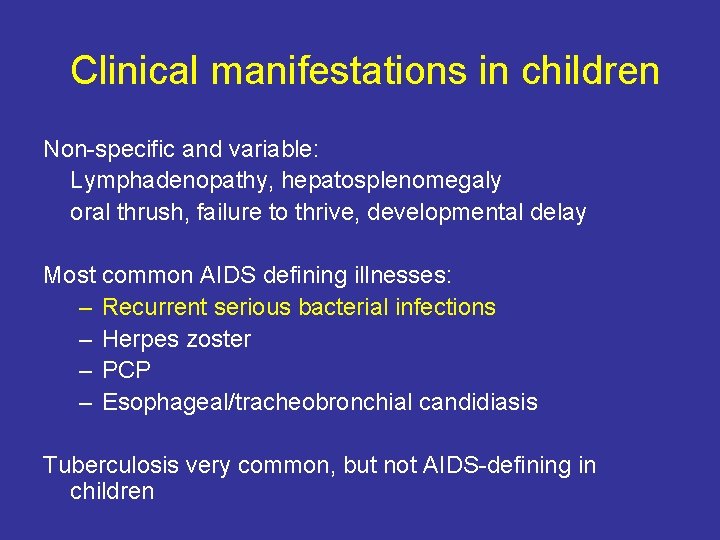
Clinical manifestations in children Non-specific and variable: Lymphadenopathy, hepatosplenomegaly oral thrush, failure to thrive, developmental delay Most common AIDS defining illnesses: – Recurrent serious bacterial infections – Herpes zoster – PCP – Esophageal/tracheobronchial candidiasis Tuberculosis very common, but not AIDS-defining in children
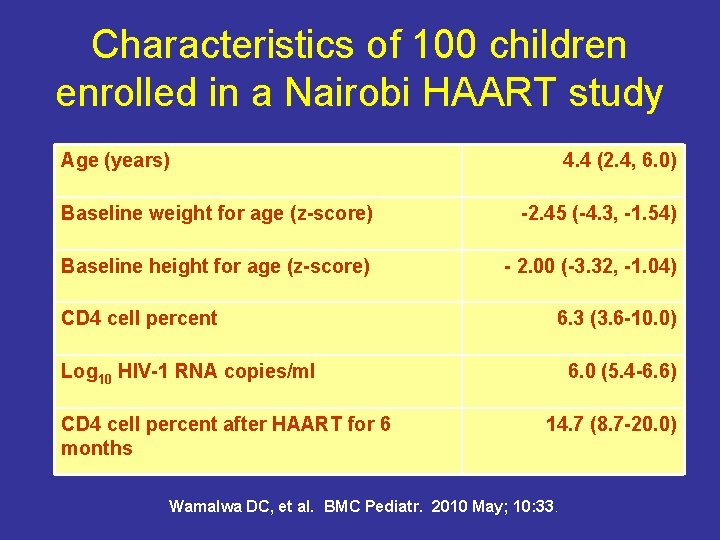
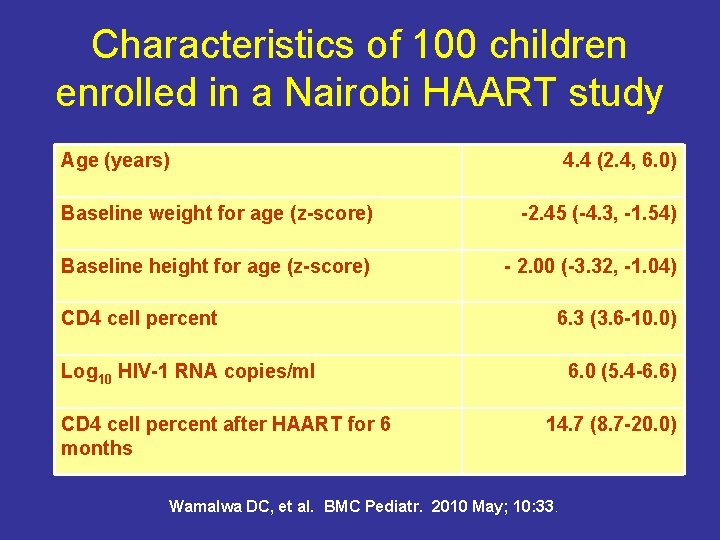
Characteristics of 100 children enrolled in a Nairobi HAART study Age (years) 4. 4 (2. 4, 6. 0) Baseline weight for age (z-score) -2. 45 (-4. 3, -1. 54) Baseline height for age (z-score) - 2. 00 (-3. 32, -1. 04) CD 4 cell percent 6. 3 (3. 6 -10. 0) Log 10 HIV-1 RNA copies/ml CD 4 cell percent after HAART for 6 months 6. 0 (5. 4 -6. 6) 14. 7 (8. 7 -20. 0) Wamalwa DC, et al. BMC Pediatr. 2010 May; 10: 33.
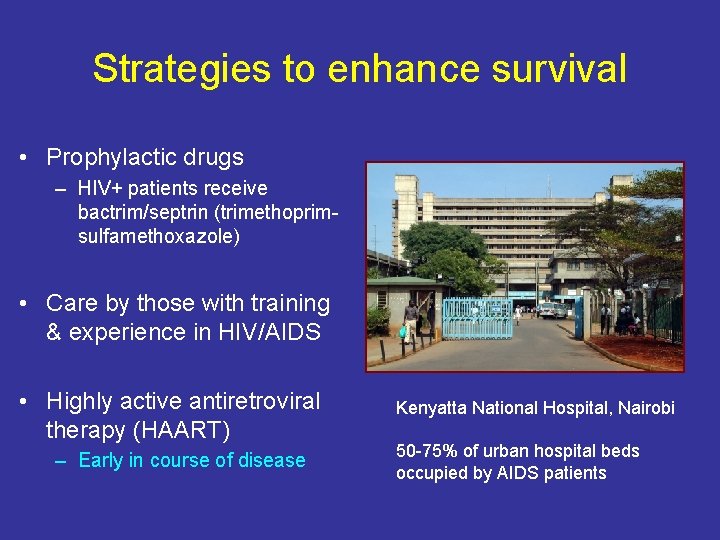
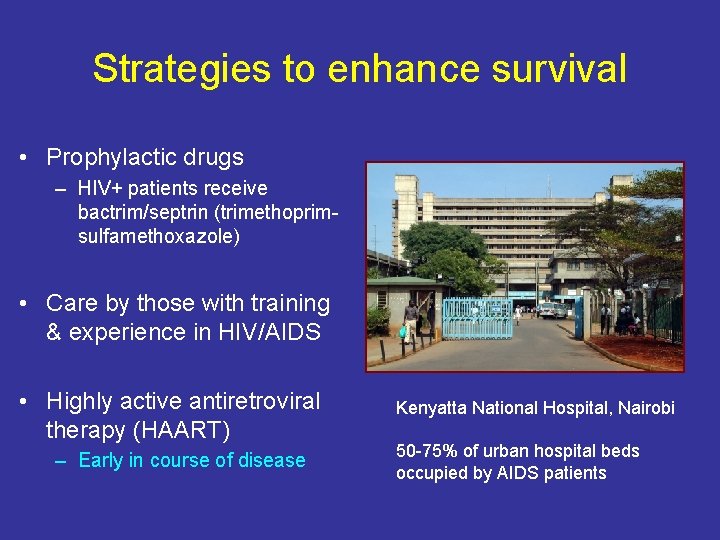
Strategies to enhance survival • Prophylactic drugs – HIV+ patients receive bactrim/septrin (trimethoprimsulfamethoxazole) • Care by those with training & experience in HIV/AIDS • Highly active antiretroviral therapy (HAART) – Early in course of disease Kenyatta National Hospital, Nairobi 50 -75% of urban hospital beds occupied by AIDS patients
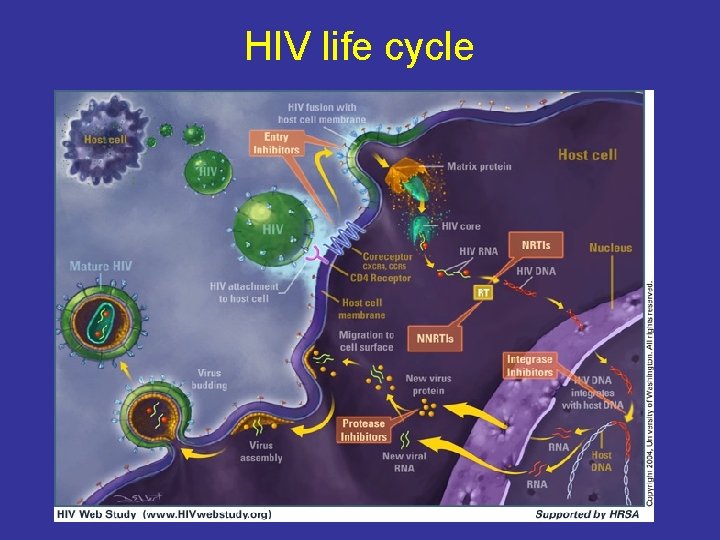
What is HAART? Combination therapy to avoid resistance – – – Nucleoside/nucleotide reverse transcriptase inhibiters (NRTI) Non-nucleoside reverse transcriptase inhibitors (NNRTI) Protease inhibitors (PI) Entry inhibitors Integrase inhibitors Three drugs from at least 2 different classes Keys to success are compliance and monitoring
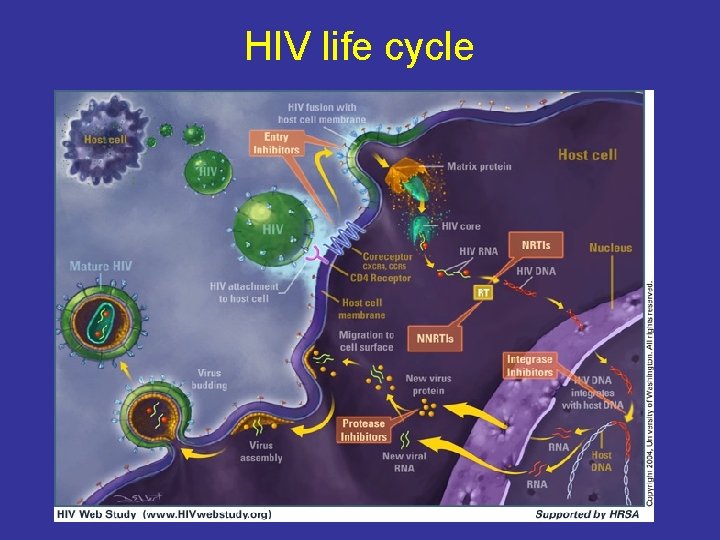
HIV life cycle
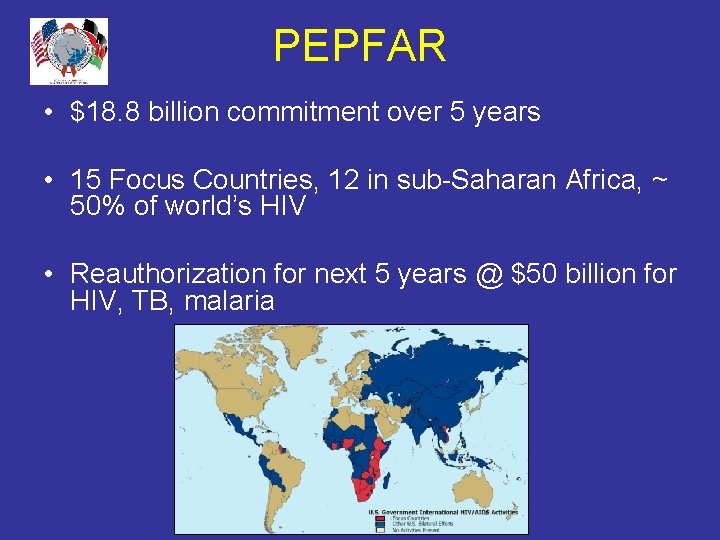
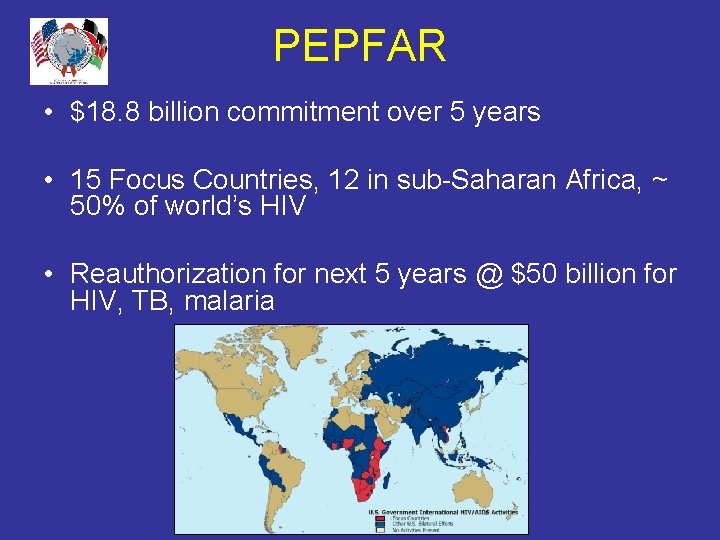
PEPFAR • $18. 8 billion commitment over 5 years • 15 Focus Countries, 12 in sub-Saharan Africa, ~ 50% of world’s HIV • Reauthorization for next 5 years @ $50 billion for HIV, TB, malaria
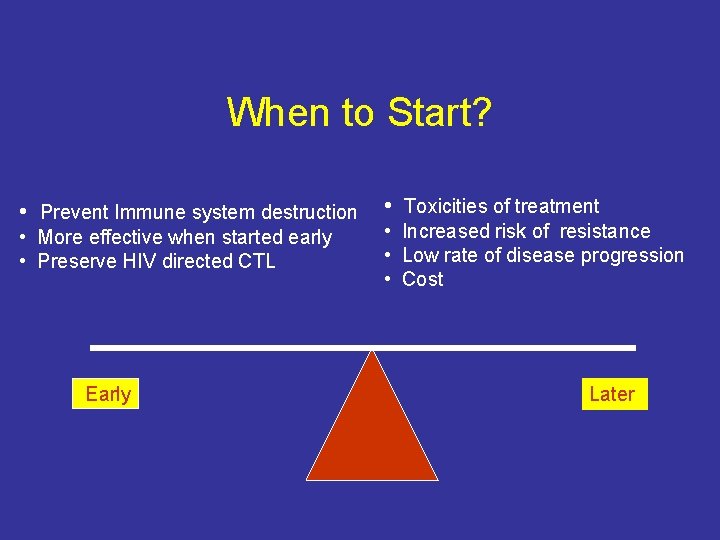
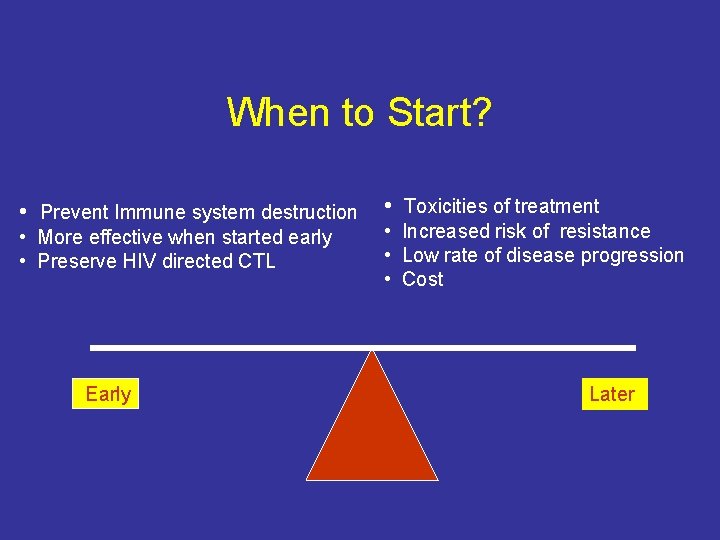
When to Start? • Prevent Immune system destruction • More effective when started early • Preserve HIV directed CTL Early • Toxicities of treatment • Increased risk of resistance • Low rate of disease progression • Cost Later
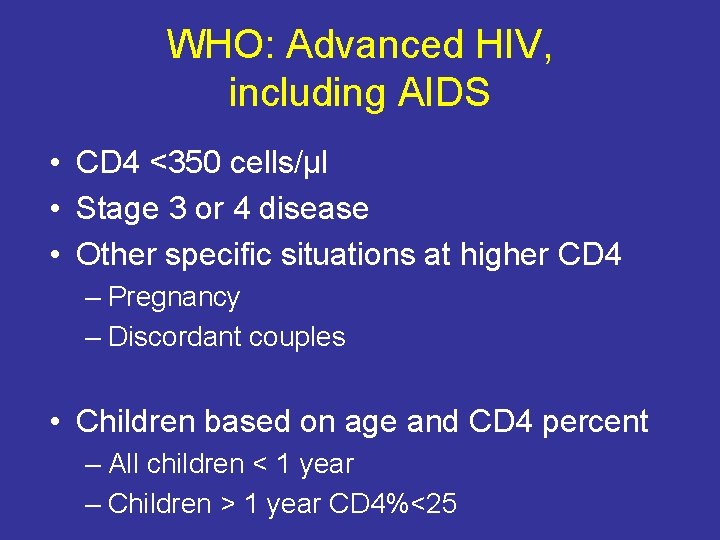
WHO: Advanced HIV, including AIDS • CD 4 <350 cells/μl • Stage 3 or 4 disease • Other specific situations at higher CD 4 – Pregnancy – Discordant couples • Children based on age and CD 4 percent – All children < 1 year – Children > 1 year CD 4%<25
Case #4 A 27 year women with a CD 4 count of 72 begins nevirapine, lamivudine and zidovudine. At the time she has no complaints except fatigue. She presents 4 weeks later with chest pain, dry cough and fevers. What is on your differential?
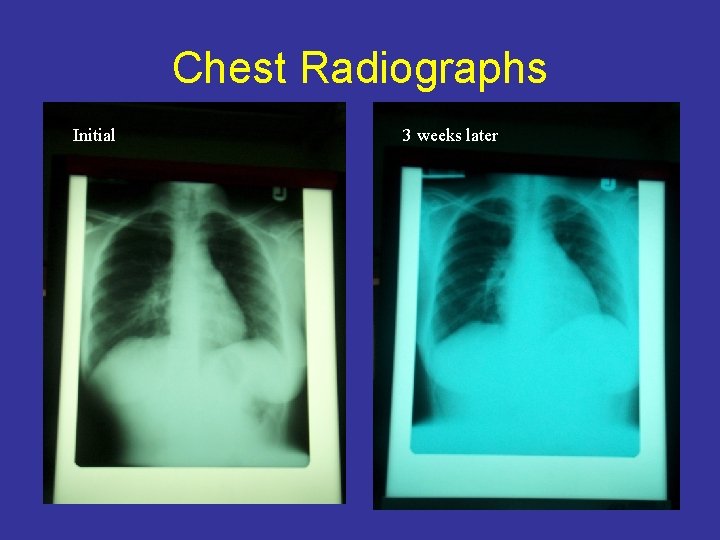
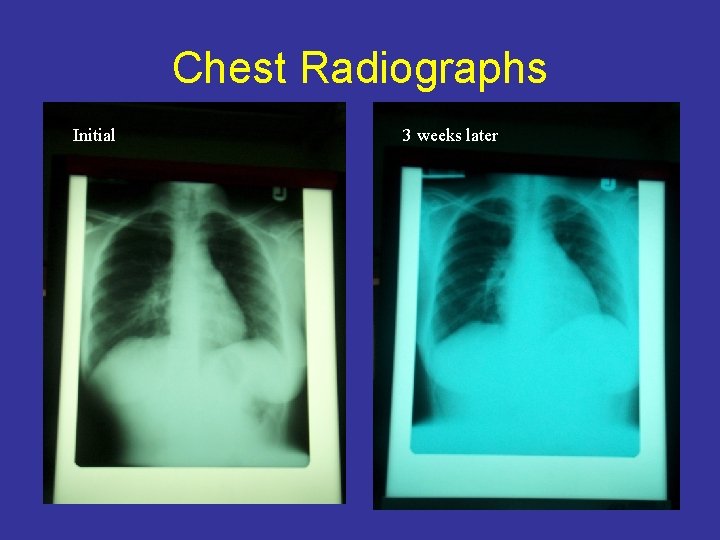
Chest Radiographs Initial 3 weeks later
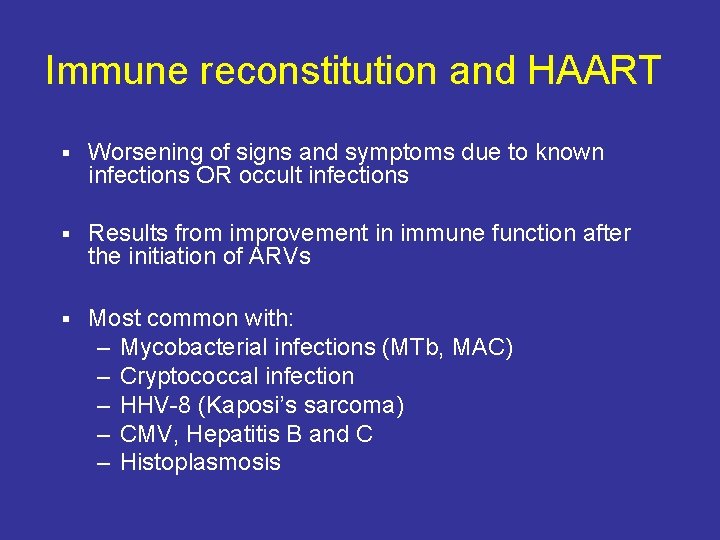
Immune reconstitution and HAART § Worsening of signs and symptoms due to known infections OR occult infections § Results from improvement in immune function after the initiation of ARVs § Most common with: – Mycobacterial infections (MTb, MAC) – Cryptococcal infection – HHV-8 (Kaposi’s sarcoma) – CMV, Hepatitis B and C – Histoplasmosis
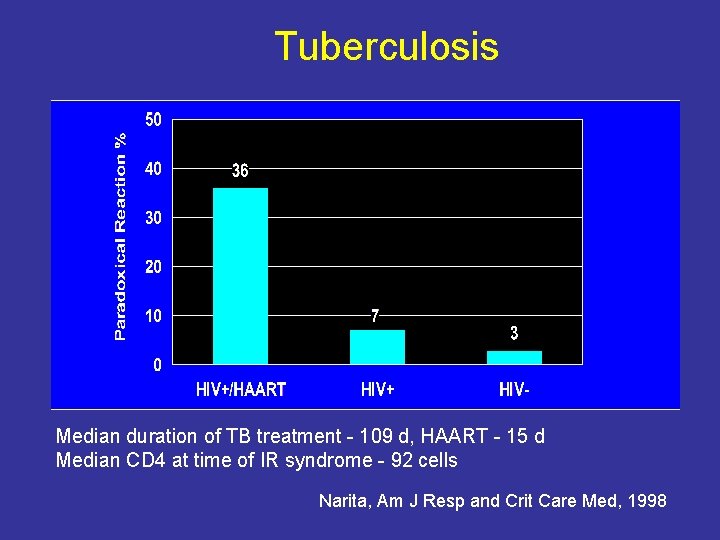
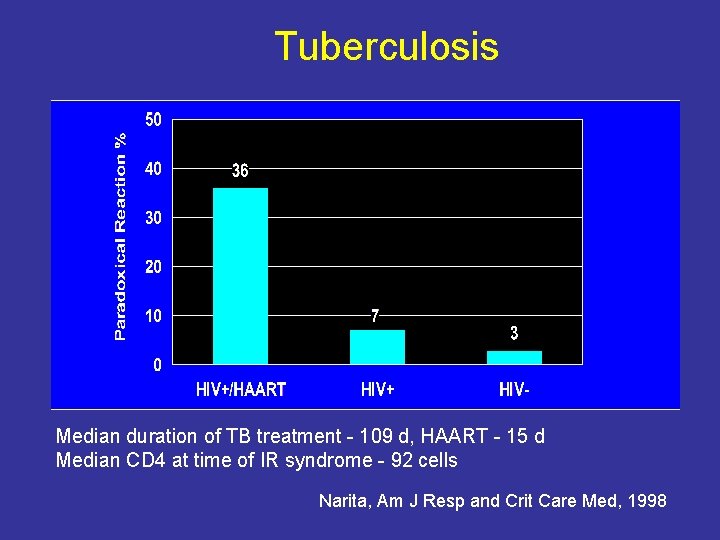
Tuberculosis graph Median duration of TB treatment - 109 d, HAART - 15 d Median CD 4 at time of IR syndrome - 92 cells Narita, Am J Resp and Crit Care Med, 1998
ARVs with Pulmonary TB WHO recommendations: November 2009 – Start TB treatment first – Use Efavirenz as preferred NNRTI – Treat with ART immediately if CD 4<50 – Treat within 2 -4 weeks if CD 4>50 – Start ART within 8 weeks
Prevention Couple treatment with strong message about preventing transmission – – – Condoms & “safe” sex Treatment of STDs Circumcision Future vaccines & microbicides Interventions to prevent mother-to-child HIV-1 transmission – Treatment as prevention – Pre-exposure prophylaxis (Pr. EP
Case #5 A 23 year old Kenyan woman presents with her first pregnancy for antenatal care at 24 weeks gestation and is found to be positive for HIV by rapid ELISA testing. She is counseled regarding interventions to prevent HIV transmission. Is a CD 4 count and HIV viral load indicated? If so, how will this change management?
Case #5 Her CD 4 count is 360 cells/ul and no HIV viral load is performed. She is asymptomatic with respect to her HIV infection. What regimen will she be prescribed to prevent MTCT? Is there an alternative regimen?
Case #5 She tells you her sister also has HIV and her baby died. She wants to do everything she can to prevent her baby from becoming infected and is interested in formula feeding. One problem she sees with formula feeding is that she is reluctant to tell her husband that she has HIV.
Case #5 She delivers a healthy infant and decides to breastfeed because she still hasn’t told her partner. She wants to know if the baby is infected and plans to stop breastfeeding early. What additional counseling will she need regarding infant feeding?
Case #5 She successfully weans at 6 months, returns at 15 months for an HIV ELISA, and is told that her baby is not infected. How should you advise her now regarding follow-up care?
Resources • CDC guidelines and educational materials (domestic) – http: //aidsinfo. nih. gov/guidelines – http: //aidsinfo. nih. gov/contentfiles/lvguidelines/adultandadolescentgl. pdf • UNAIDS/WHO recommendations and updates (international) – http: //www. who. int/hiv/pub/en/ • Country-specific guidelines for everything, including: – ARV therapy – adults, children – HIV testing (couple counseling and testing; homebased testing) – Prevention of mother-to-child transmission
Asante sana
 Guilherme carey ou william carey
Guilherme carey ou william carey Addie and assure model
Addie and assure model Lonnie david franklin jr childhood
Lonnie david franklin jr childhood Reverend william carey
Reverend william carey Ms carey ap psych
Ms carey ap psych Bigemine nabız
Bigemine nabız Dick and carrey
Dick and carrey Addie carey
Addie carey Siobhan carey
Siobhan carey Colleen carey
Colleen carey Lou carey biografia
Lou carey biografia Gdc data center
Gdc data center Carey business school career development office
Carey business school career development office Sheppard vs maxwell summary
Sheppard vs maxwell summary Carey brothers logistics
Carey brothers logistics Murmurs made easy
Murmurs made easy Engblom vs carey
Engblom vs carey Deep learning dummies
Deep learning dummies Naomi campbell face shape
Naomi campbell face shape Design model
Design model Allan carey
Allan carey Carey schwartz
Carey schwartz Carey nachenberg slides
Carey nachenberg slides Linda carey
Linda carey Carey y cia
Carey y cia Carey coombs üfürümü
Carey coombs üfürümü Clinical risk management in dentistry
Clinical risk management in dentistry Clinical metadata management tool
Clinical metadata management tool Society of clinical data management
Society of clinical data management Integrated clinical services management
Integrated clinical services management Clinical trial financial management
Clinical trial financial management Sae reconciliation in clinical data management
Sae reconciliation in clinical data management Oxytoxics
Oxytoxics Vray animation settings
Vray animation settings Vray frame buffer
Vray frame buffer Custom display in ecdis
Custom display in ecdis What is the rising action in the three little pigs
What is the rising action in the three little pigs Where is the necklace setting
Where is the necklace setting Hunger games setting description
Hunger games setting description Setting the boy in the striped pajamas
Setting the boy in the striped pajamas The alchemist conflict and resolution
The alchemist conflict and resolution Pacemaker settings
Pacemaker settings Teams voicemail greeting
Teams voicemail greeting Copyright
Copyright Exposition elements
Exposition elements The setting of dr jekyll and mr hyde
The setting of dr jekyll and mr hyde Function of community health nurse
Function of community health nurse Basic cpap settings
Basic cpap settings Power bi report server scale out
Power bi report server scale out Niv modes and settings
Niv modes and settings Multiple baseline vs multiple probe design
Multiple baseline vs multiple probe design Msi acpi settings
Msi acpi settings