Childhood Hip Deformity Judson W Karlen MD Phoenix














- Slides: 76
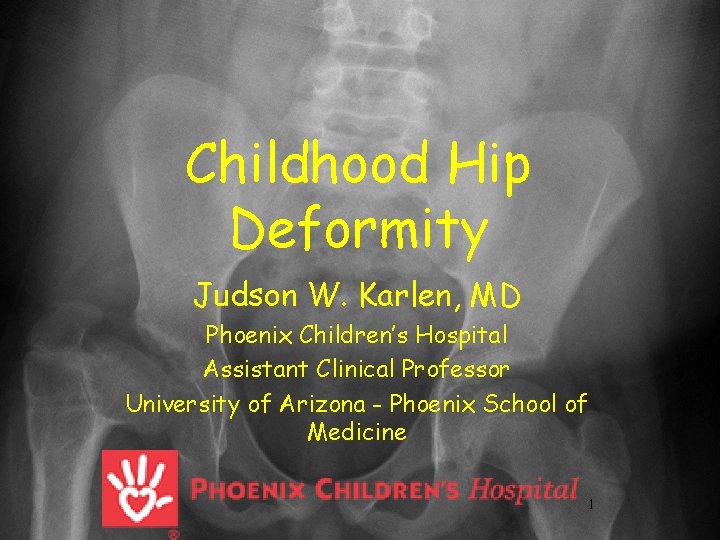
Childhood Hip Deformity Judson W. Karlen, MD Phoenix Children’s Hospital Assistant Clinical Professor University of Arizona - Phoenix School of Medicine 1
Objectives • Review etiology of childhood hip deformity • “Common” Disorders – Slipped Capital Femoral Epiphysis – Legg-Calve-Perthes – Hip Dysplasia
Objectives • Review etiology of childhood hip deformity • Common Disorders – Slipped Capital Femoral Epiphysis – Legg-Calve-Perthes – Hip Dysplasia
Slipped Capital Femoral Epiphysis • • 13 yo M 3 month history of left knee pain Limp at the end of the day Plays sports, has not missed practices. No history of injury. No night pain, fevers. Exam – limp, able to run, jump, no tenderness about the knee


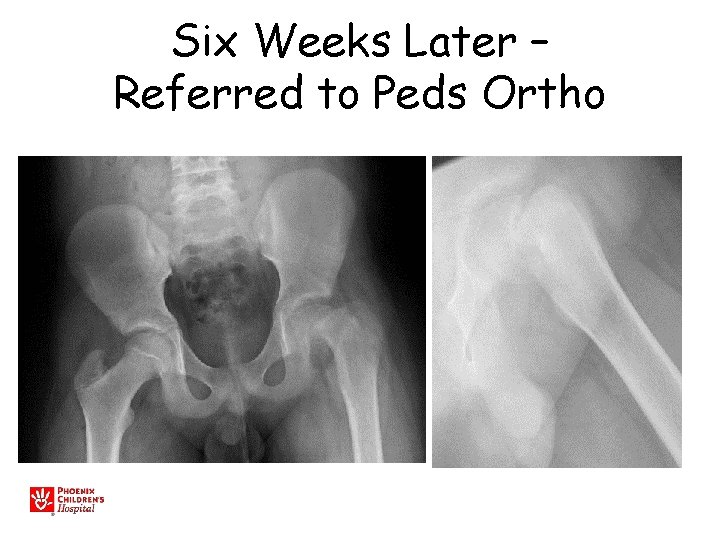
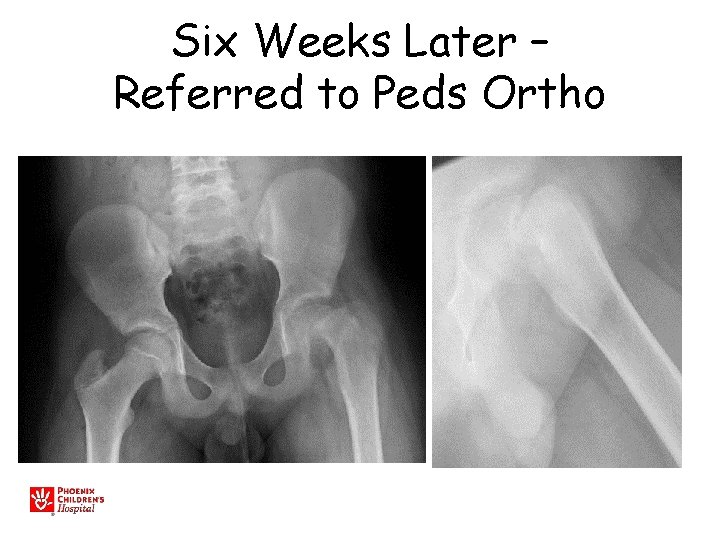
Six Weeks Later – Referred to Peds Ortho
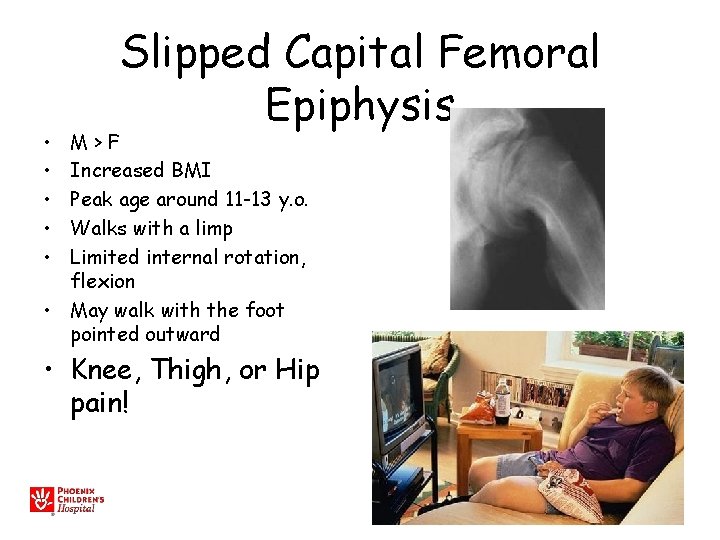
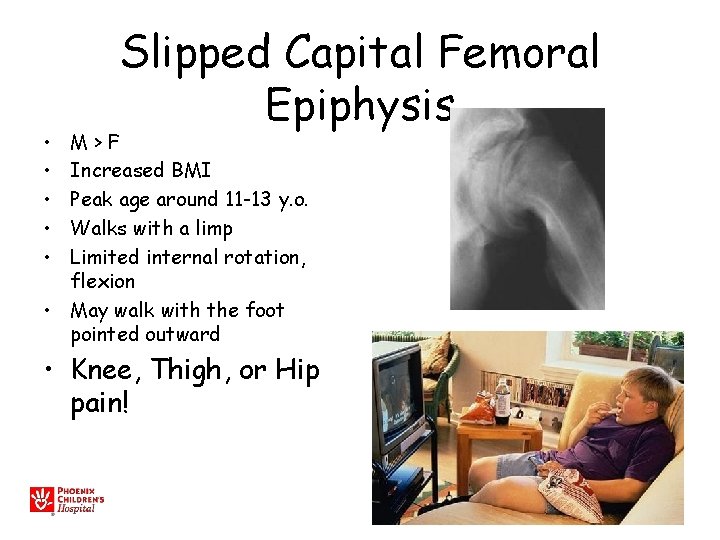
• • • Slipped Capital Femoral Epiphysis M>F Increased BMI Peak age around 11 -13 y. o. Walks with a limp Limited internal rotation, flexion • May walk with the foot pointed outward • Knee, Thigh, or Hip pain!
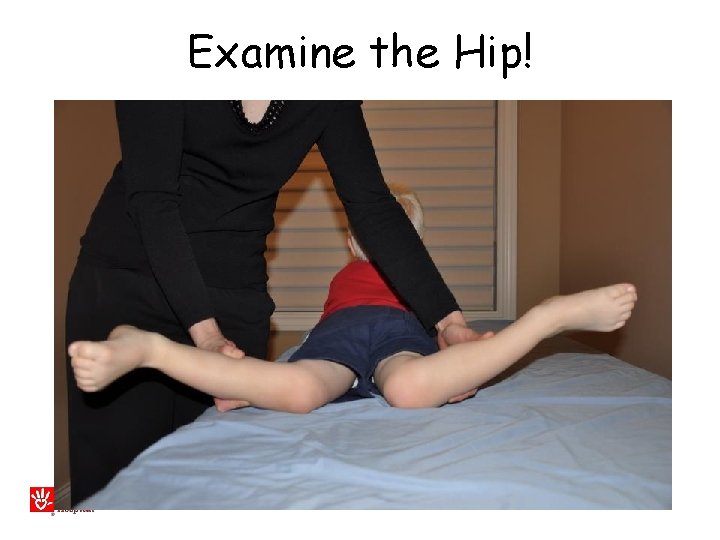
Examine the Hip!
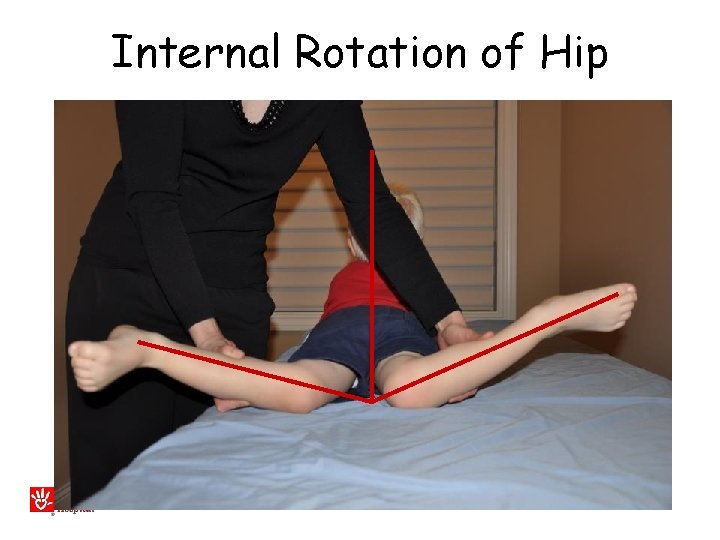
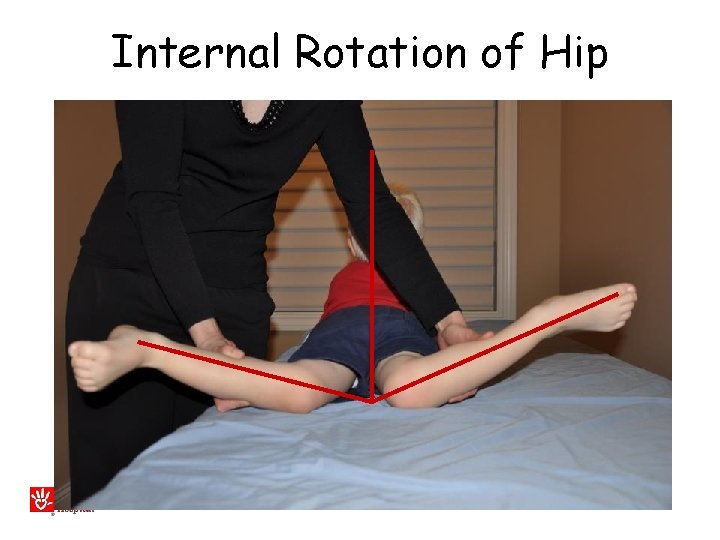
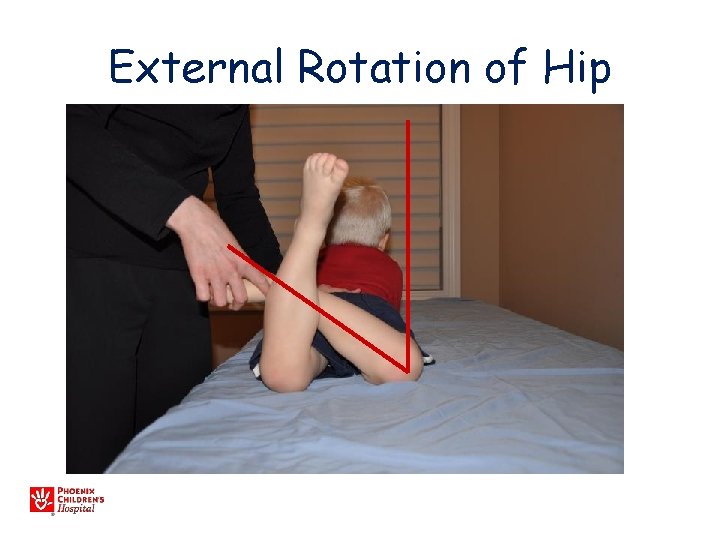
Internal Rotation of Hip
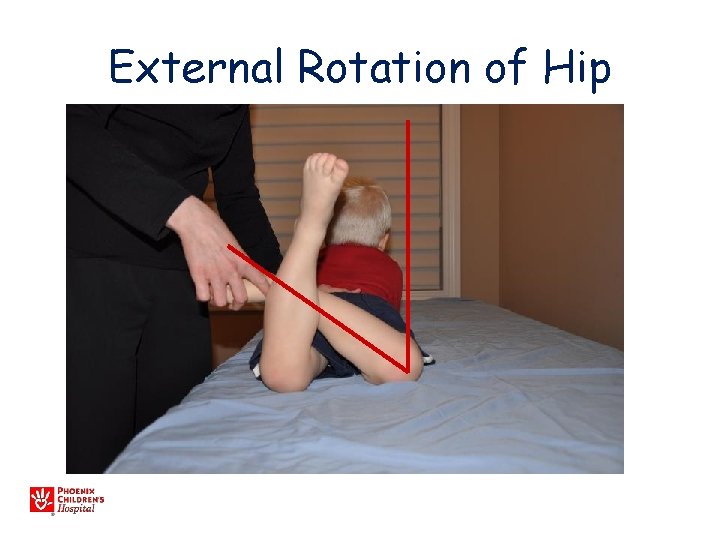
External Rotation of Hip

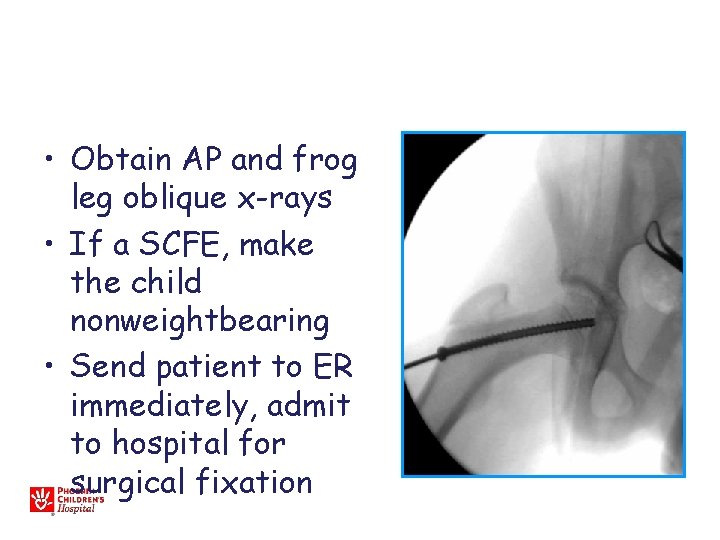
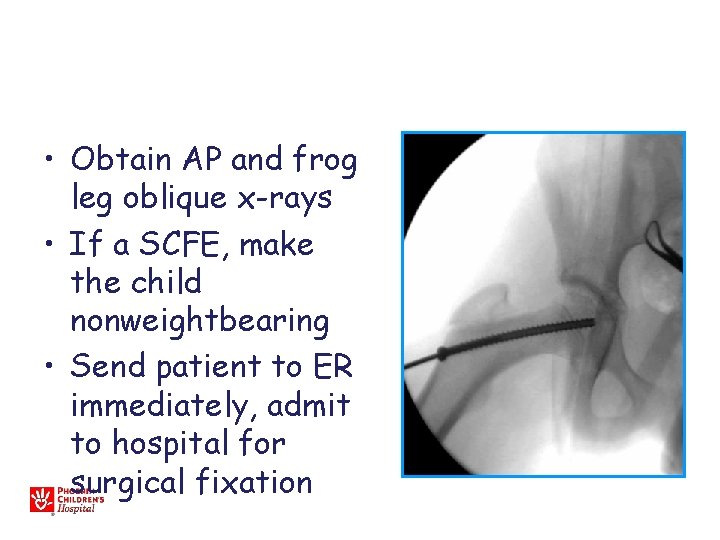
• Obtain AP and frog leg oblique x-rays • If a SCFE, make the child nonweightbearing • Send patient to ER immediately, admit to hospital for surgical fixation
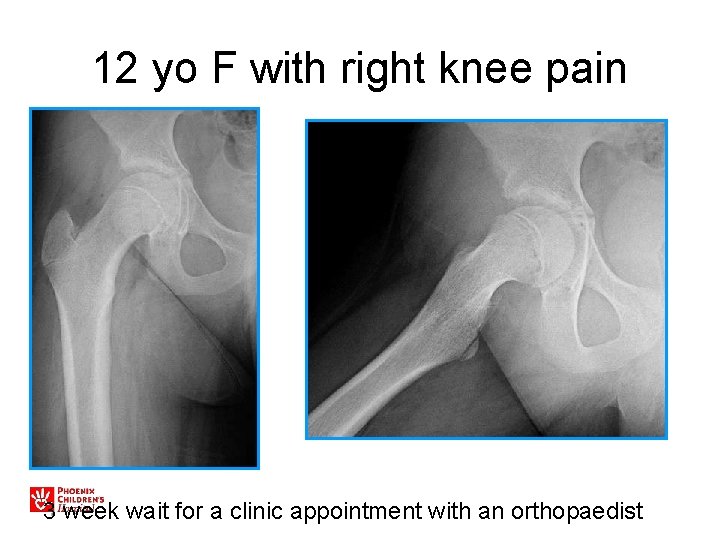
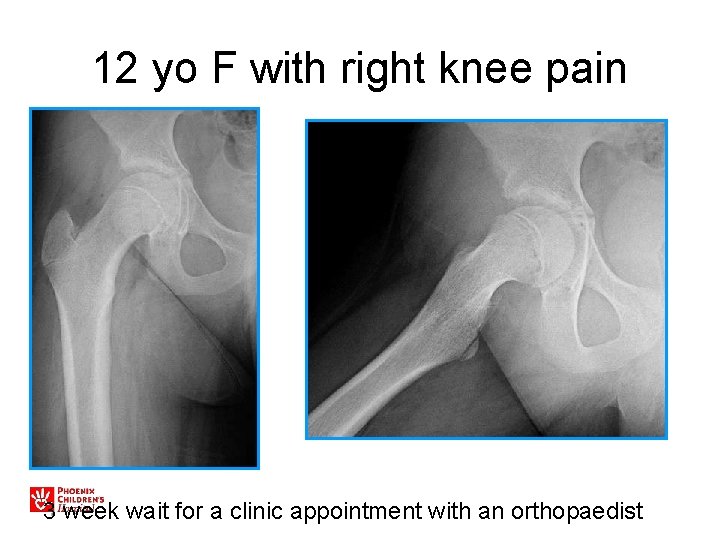
12 yo F with right knee pain 3 week wait for a clinic appointment with an orthopaedist
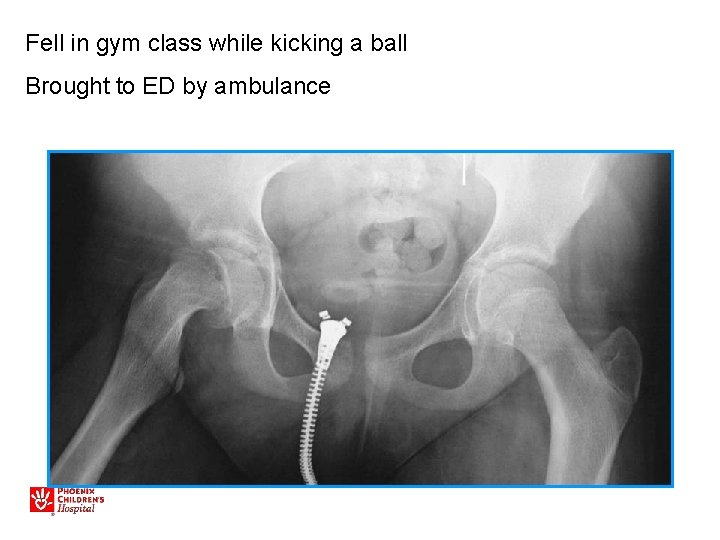
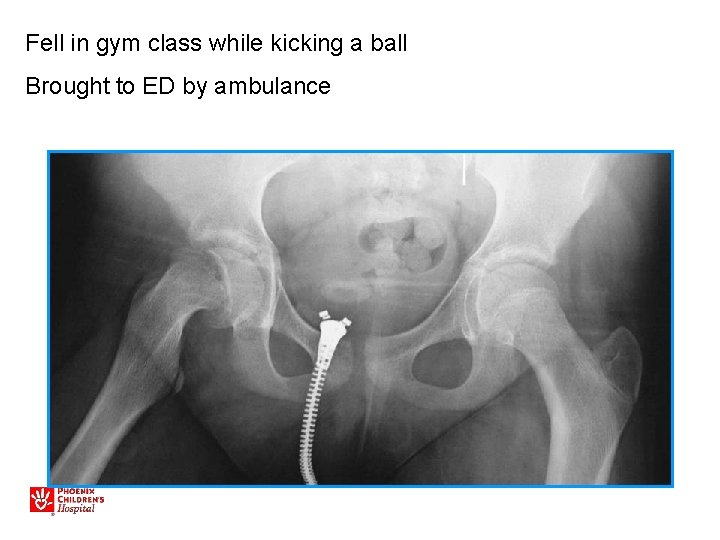
Fell in gym class while kicking a ball Brought to ED by ambulance
Unstable SCFE • • • (5% of slips) Unable to bear weight or mobilize “Hip fracture” May have antecedent pain Minimal trauma High rate of osteonecrosis (20 -50%)
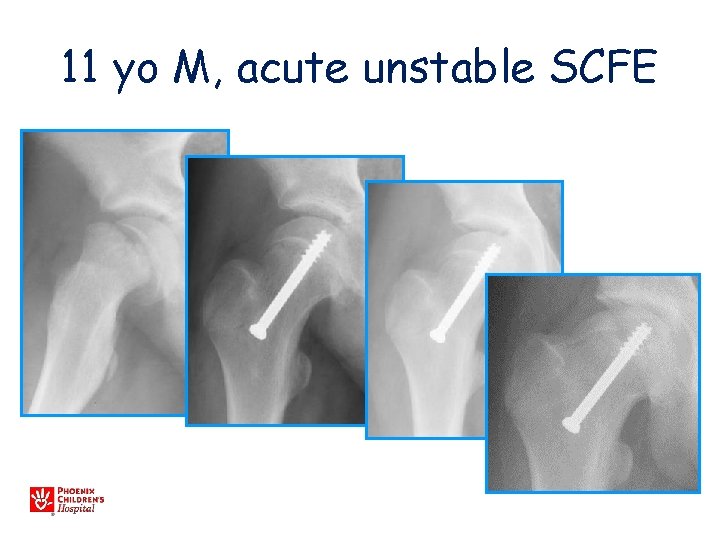
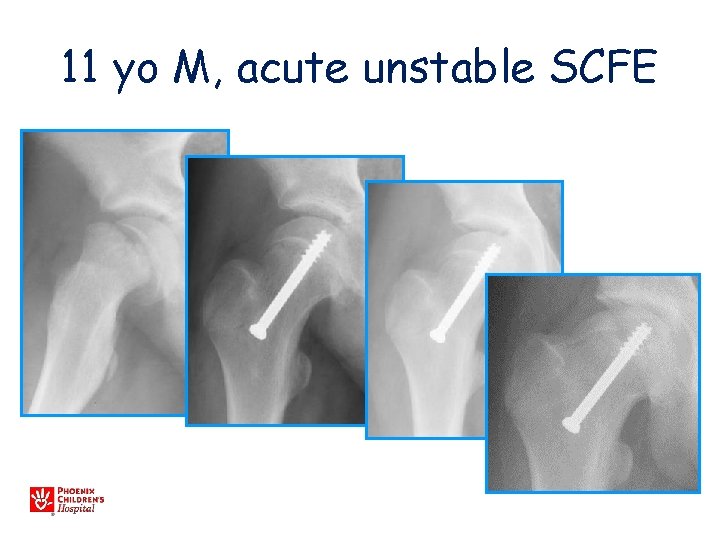
11 yo M, acute unstable SCFE
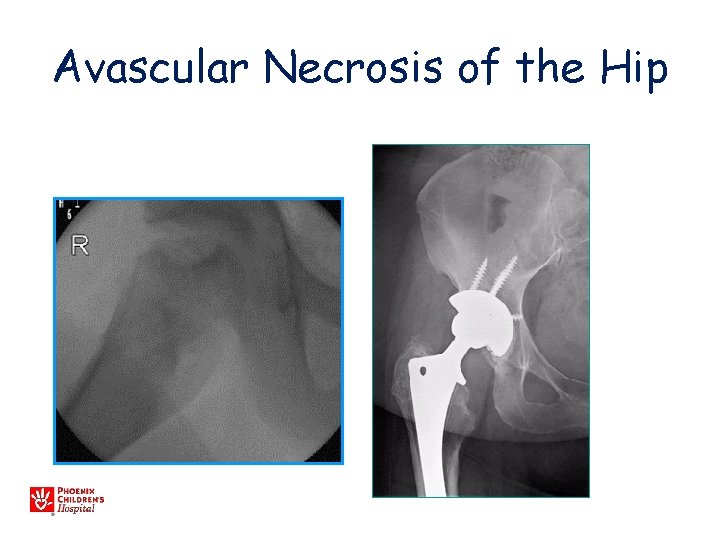
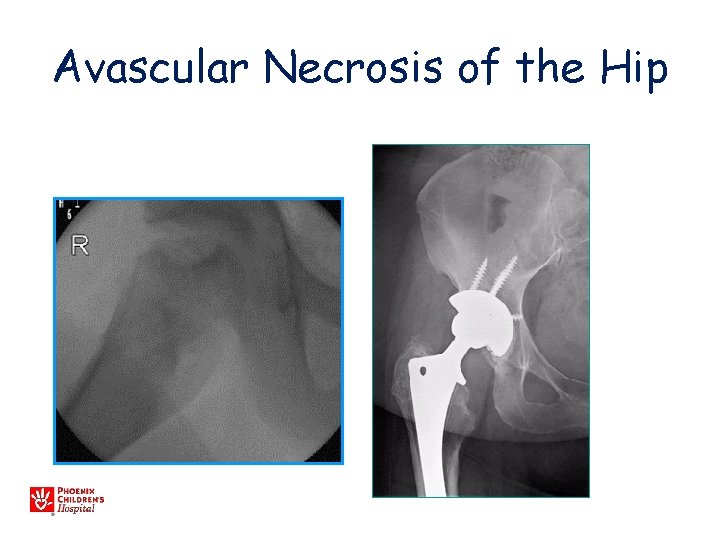
Avascular Necrosis of the Hip
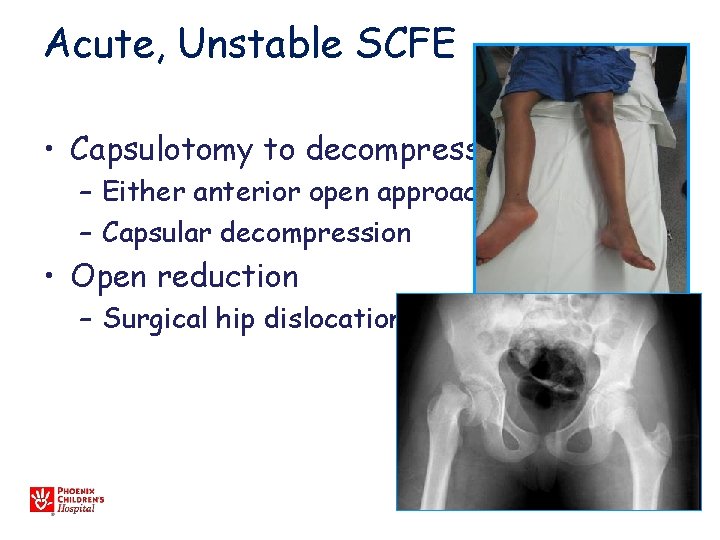
Acute, Unstable SCFE • Capsulotomy to decompress – Either anterior open approach – Capsular decompression • Open reduction – Surgical hip dislocation
SCFE: Key Points Any child with knee pain • Examine hip range of motion – Prone and supine • Check AP and frog lateral hip films, particularly if limited hip motion • Any SCFE is an urgent referral – go to ER, see orthopaedist, admit to hospital for bedrest, surgical condition
Objectives • Review etiology of childhood hip deformity • Common Disorders – Slipped Capital Femoral Epiphysis – Legg-Calve-Perthes – Hip Dysplasia
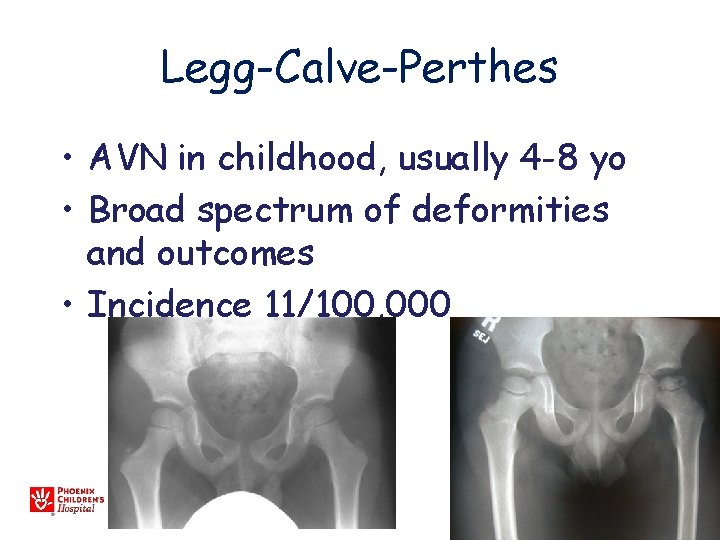
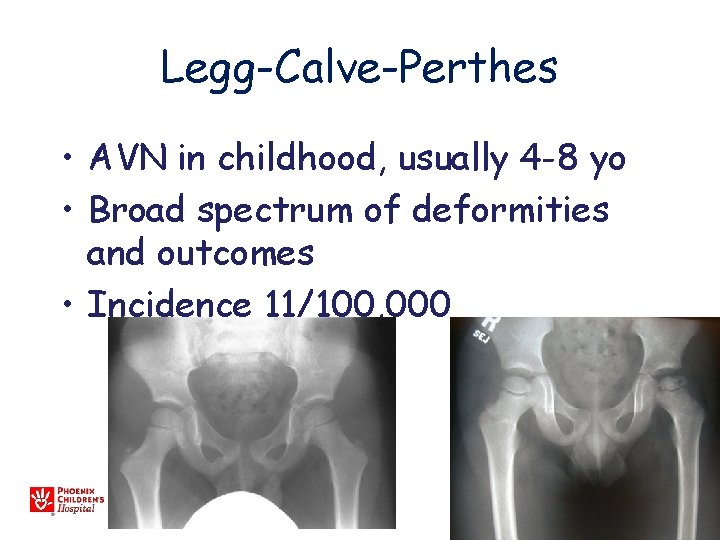
Legg-Calve-Perthes • AVN in childhood, usually 4 -8 yo • Broad spectrum of deformities and outcomes • Incidence 11/100, 000
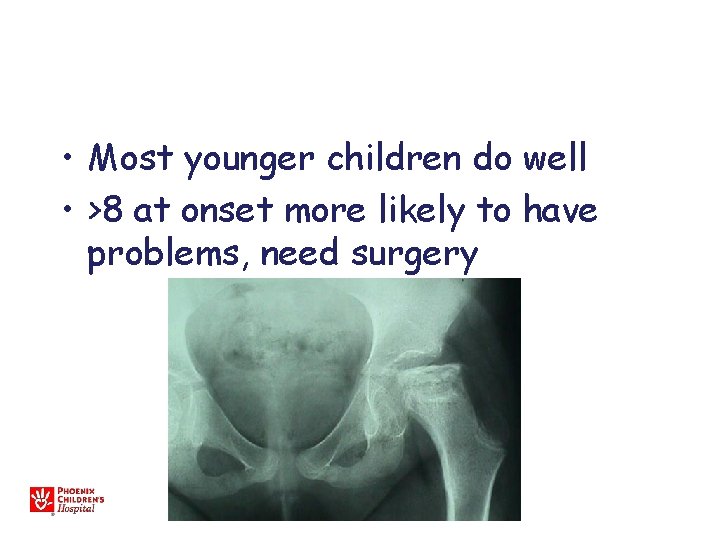
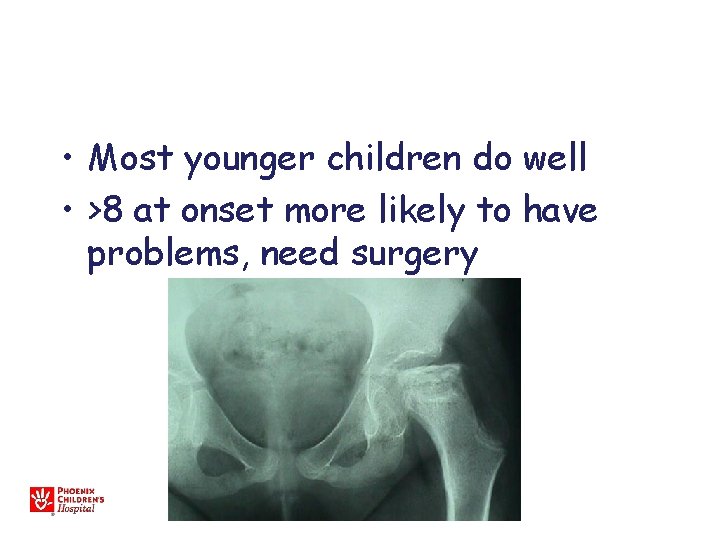
• Most younger children do well • >8 at onset more likely to have problems, need surgery
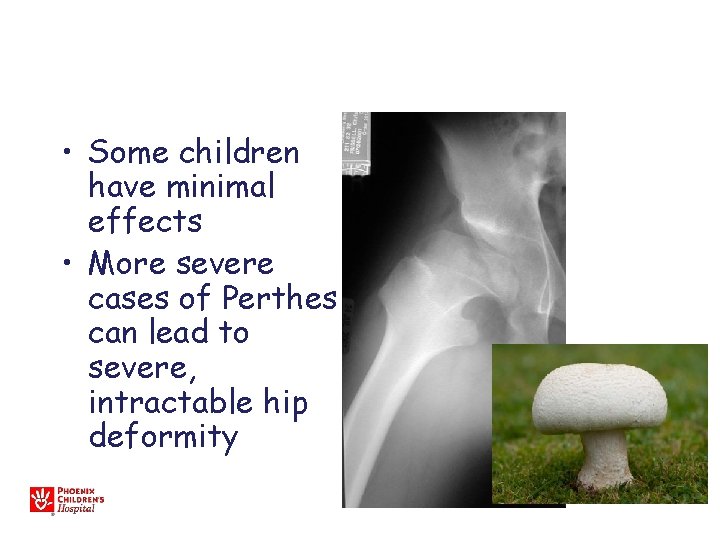
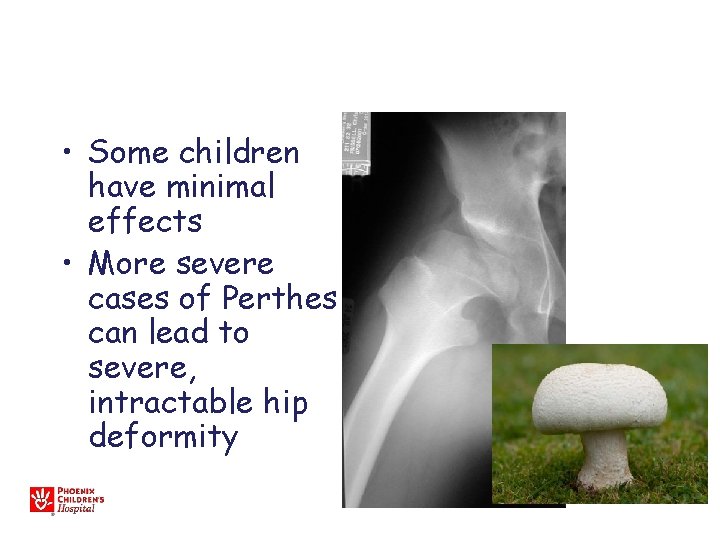
• Some children have minimal effects • More severe cases of Perthes can lead to severe, intractable hip deformity



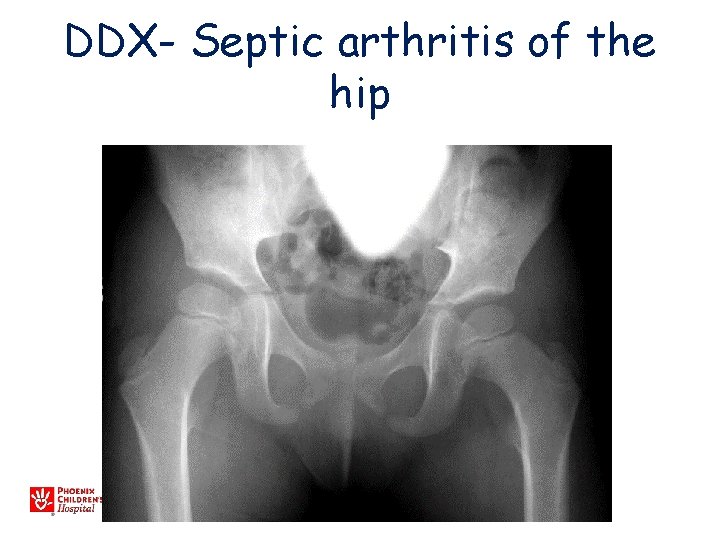
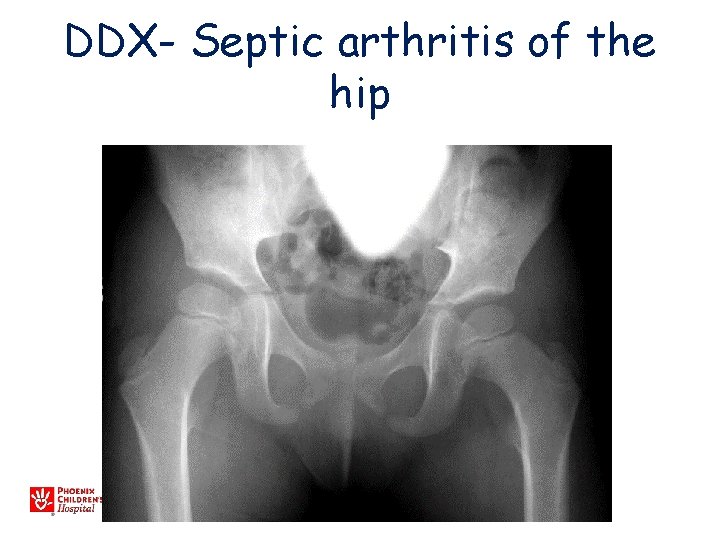
DDX- Septic arthritis of the hip
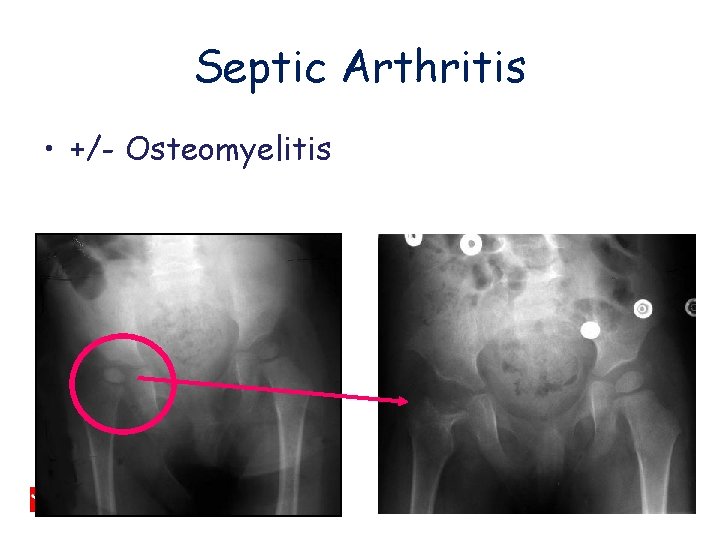
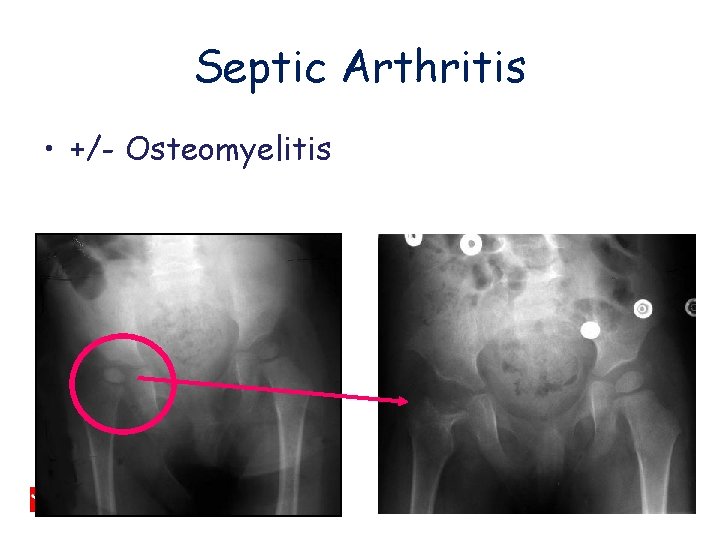
Septic Arthritis • +/- Osteomyelitis
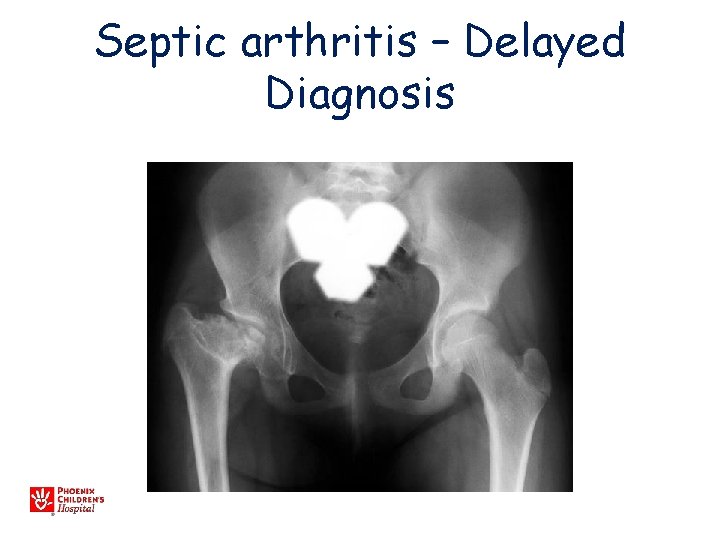
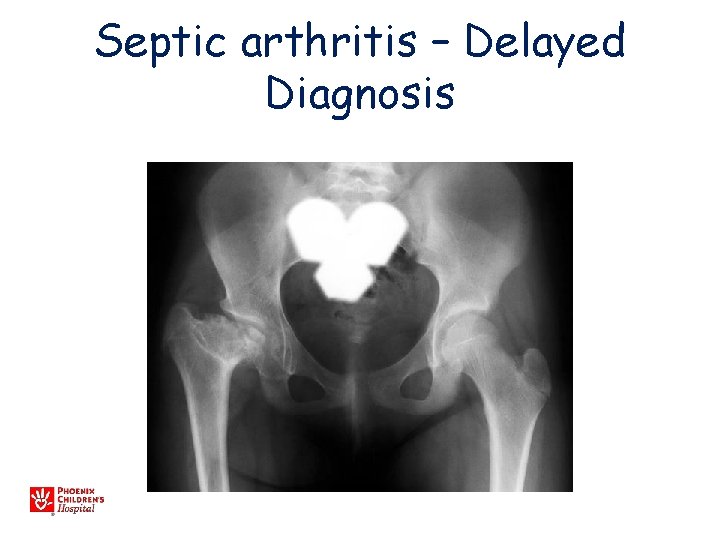
Septic arthritis – Delayed Diagnosis
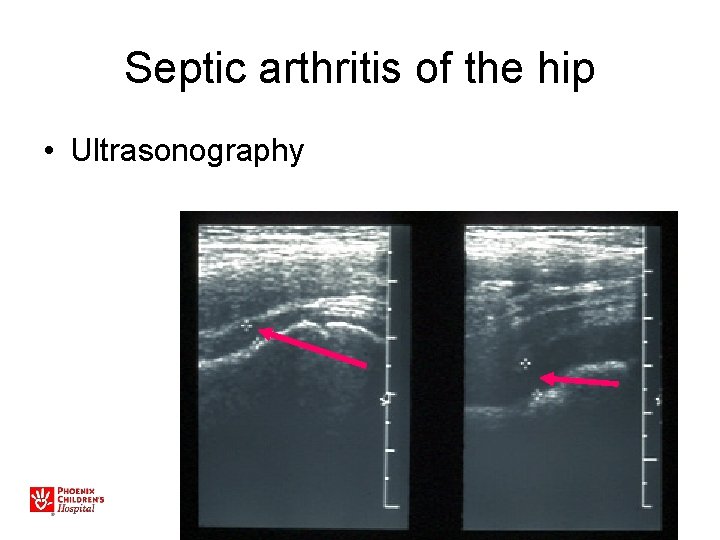
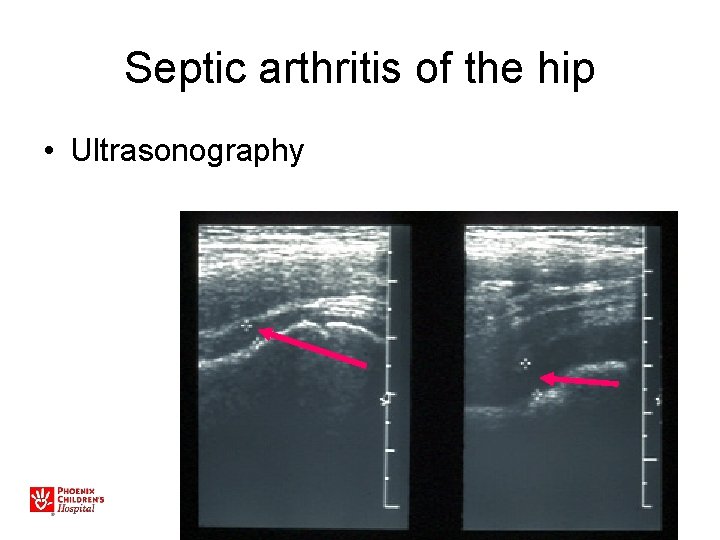
Septic arthritis of the hip • Ultrasonography
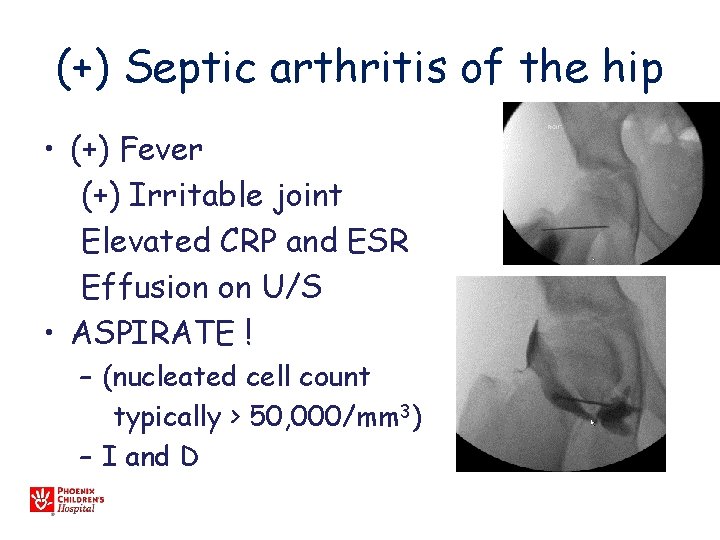
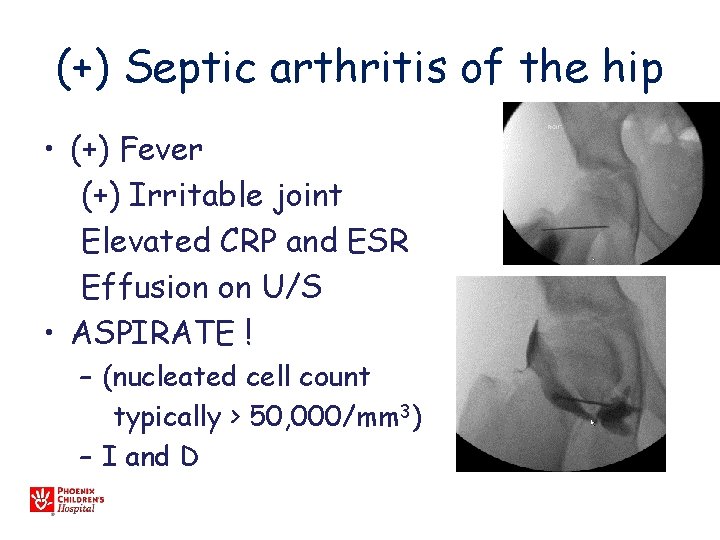
(+) Septic arthritis of the hip • (+) Fever (+) Irritable joint Elevated CRP and ESR Effusion on U/S • ASPIRATE ! – (nucleated cell count typically > 50, 000/mm 3) – I and D
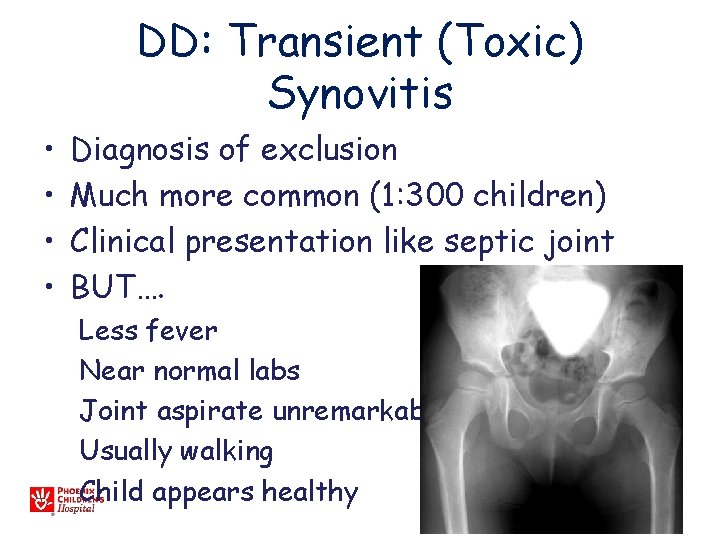
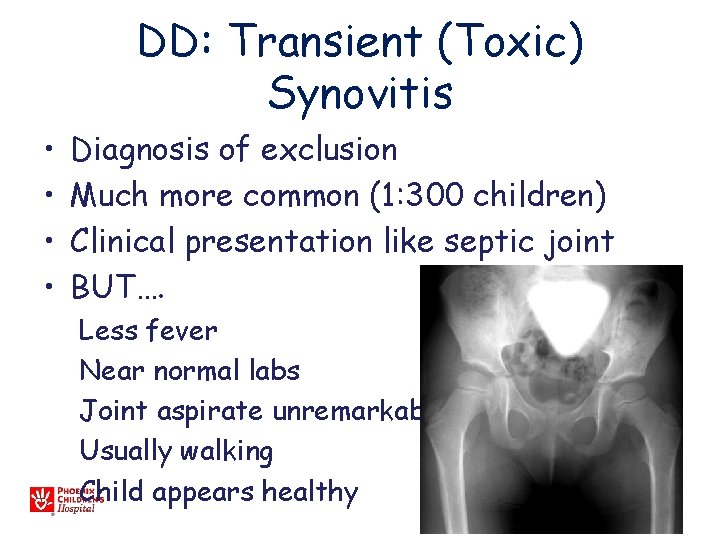
DD: Transient (Toxic) Synovitis • • Diagnosis of exclusion Much more common (1: 300 children) Clinical presentation like septic joint BUT…. Less fever Near normal labs Joint aspirate unremarkable Usually walking Child appears healthy
Transient (Toxic) Synovitis • Treatment Anti-inflammatories Activity restriction Typically resolves over 7 -10 days If doesn’t resolve in 2 - 3 weeks, consider more imaging/work-up
Objectives • Review etiology of childhood hip deformity • Common Disorders – Slipped Capital Femoral Epiphysis – Legg-Calve-Perthes – Hip Dysplasia
Developmental Dysplasia of the Hip (DDH) • Old term: CDH (congenital) • Spectrum of abnormalities from shallow hip to dislocation • Poor formation of hip joint • May lead to clinical or subclinical instability

Risk Factors • 10/1000 live births – 1/1000 dislocated at birth • Female (7: 1) • Breech position – Female, breech, firstborn – Nearly 10% risk! • Ethnic (Native American) • Family history • Oligohydramnios – Torticollis, metatarsus adductus
Effects • Hip with DDH may become normal, have residual instability, subluxate, or dislocate • Instability/subluxation leads to abnormal wear • Untreated, will lead to adult hip DJD in 25 -50%, accounts for about 20% of hip replacements
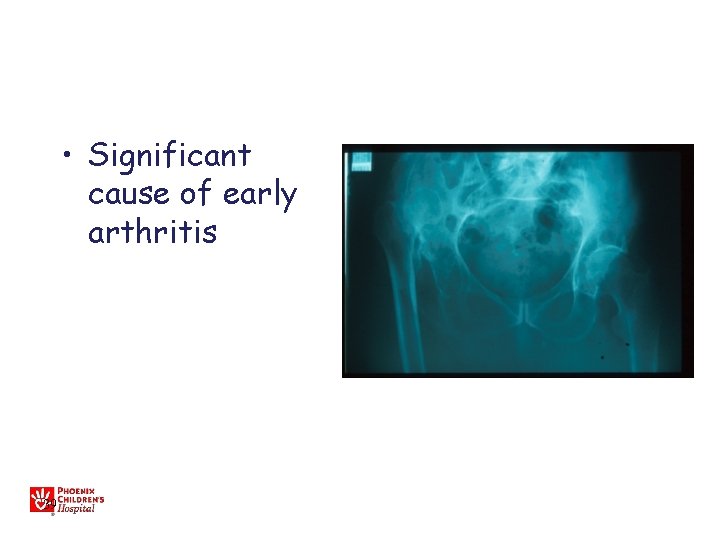
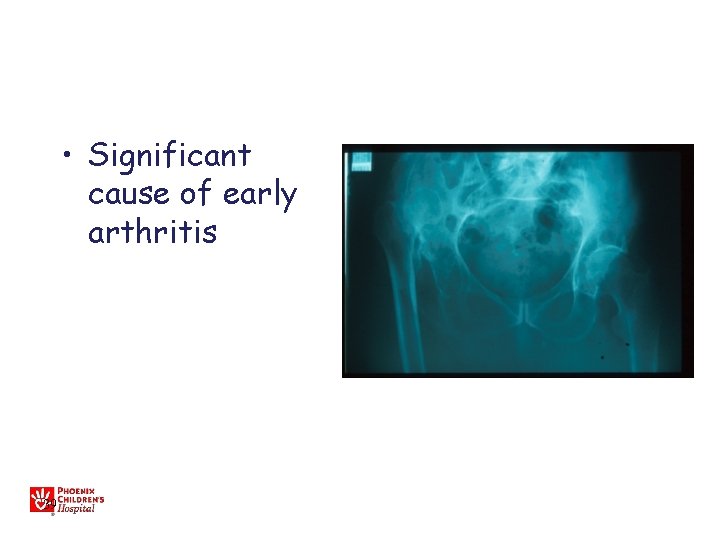
• Significant cause of early arthritis 39
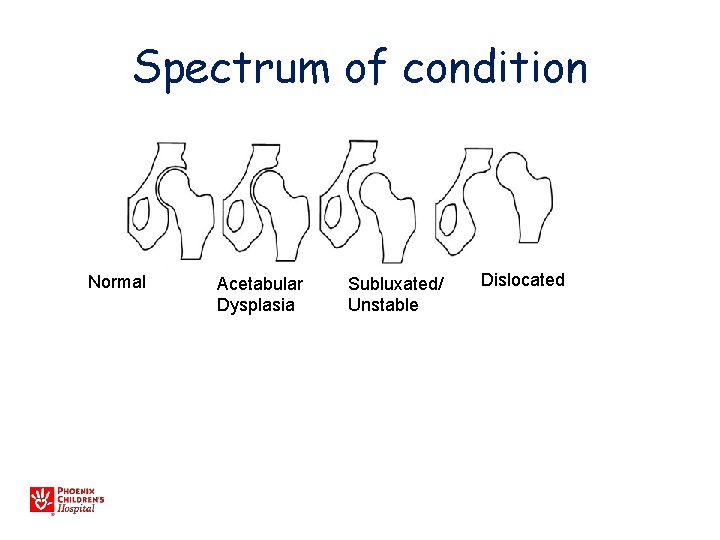
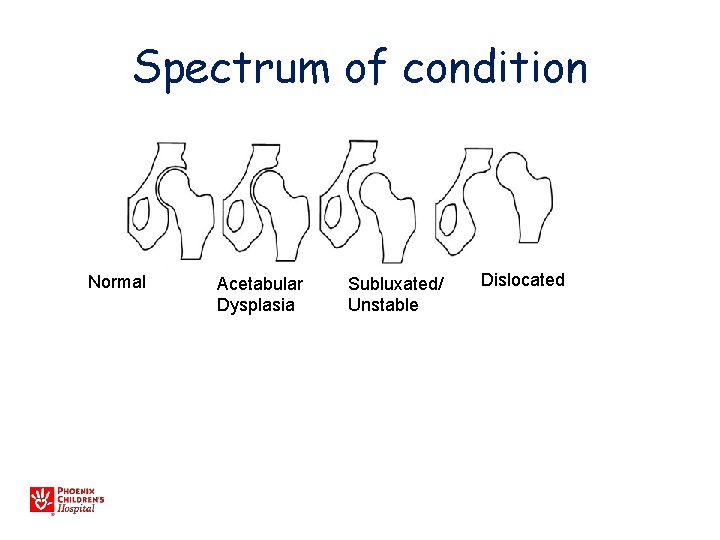
Spectrum of condition Normal Acetabular Dysplasia Subluxated/ Unstable Dislocated
Diagnosis • Primarily physical exam • Ultrasound • X-ray – After 4 months • MRI/CT (usually only pre or post op)
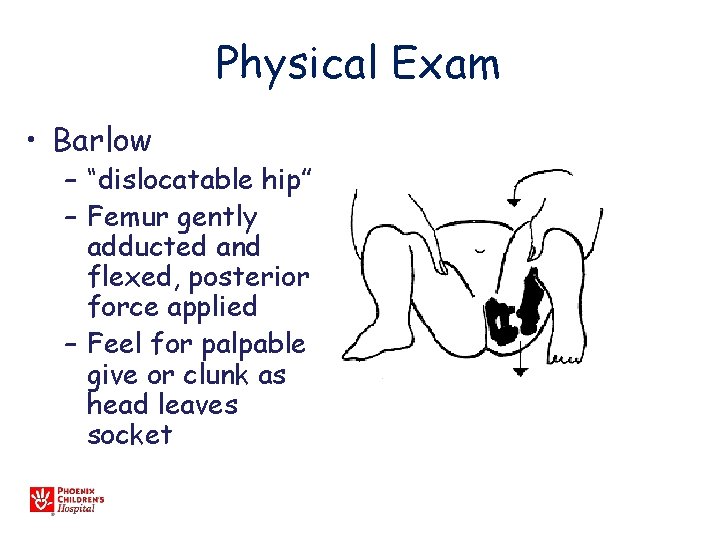
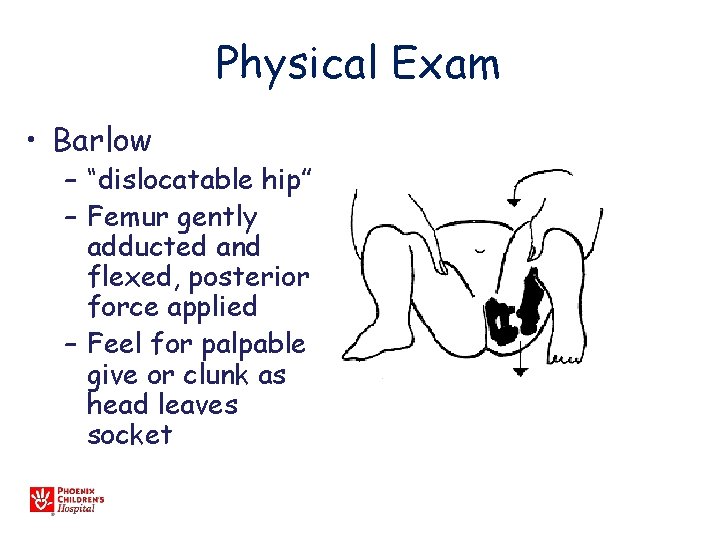
Physical Exam • Barlow – “dislocatable hip” – Femur gently adducted and flexed, posterior force applied – Feel for palpable give or clunk as head leaves socket
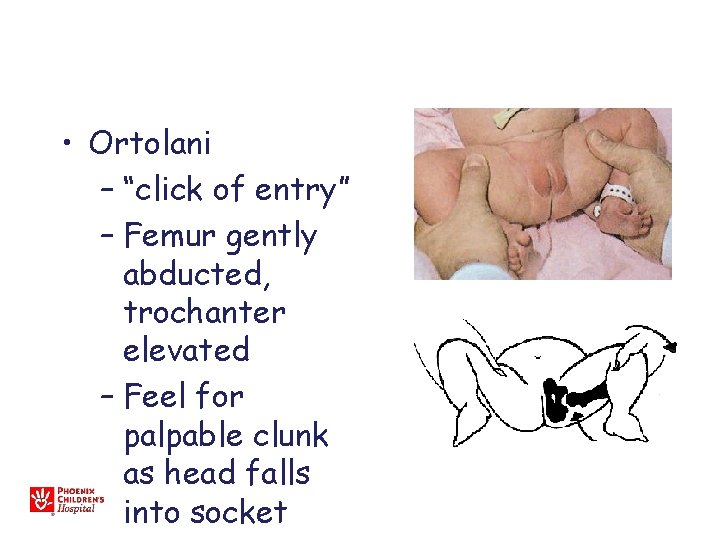
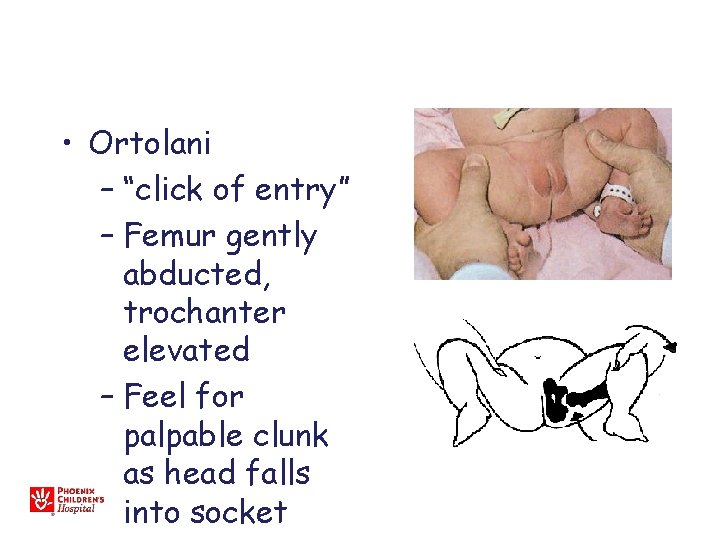
• Ortolani – “click of entry” – Femur gently abducted, trochanter elevated – Feel for palpable clunk as head falls into socket
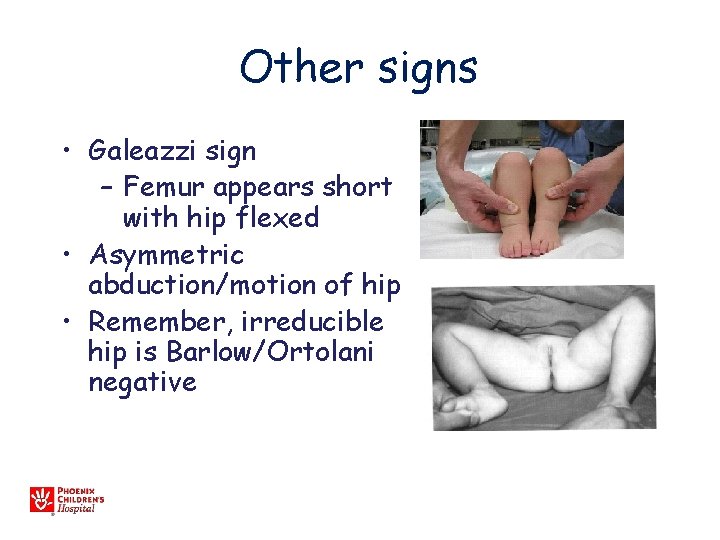
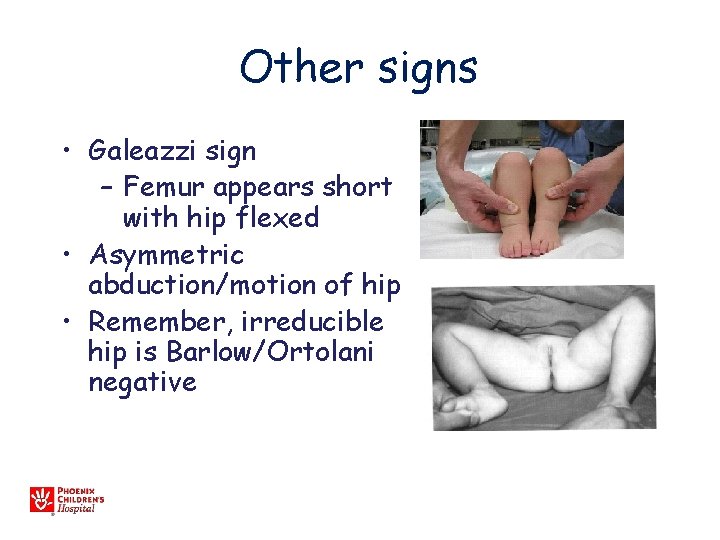
Other signs • Galeazzi sign – Femur appears short with hip flexed • Asymmetric abduction/motion of hip • Remember, irreducible hip is Barlow/Ortolani negative
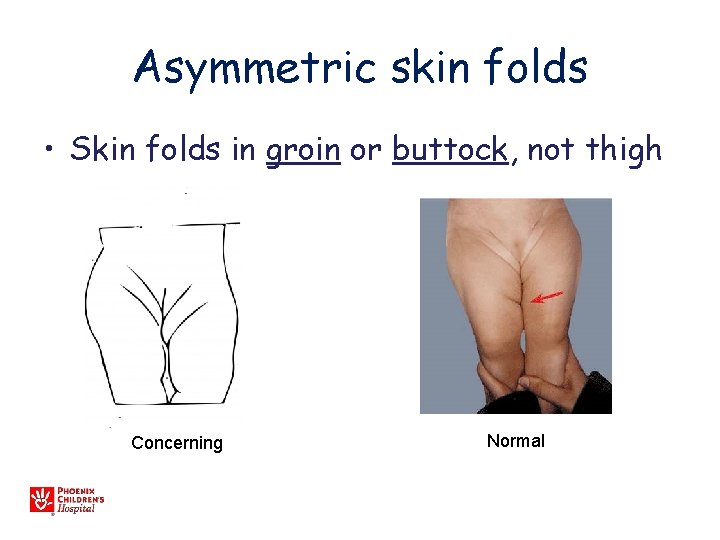
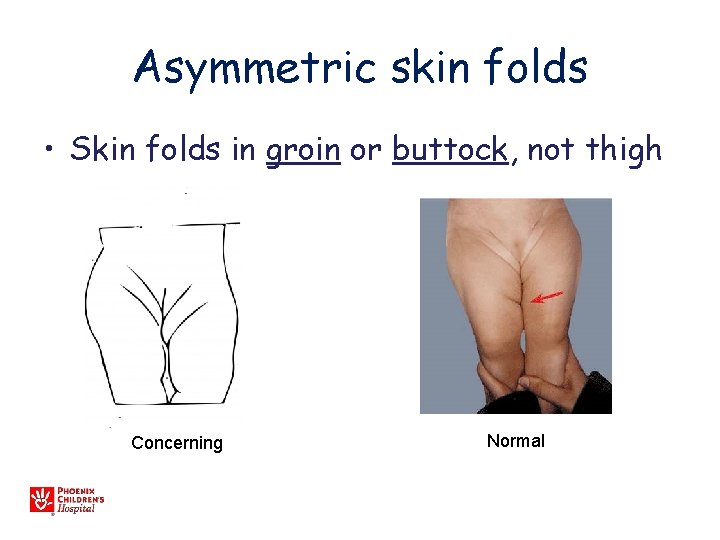
Asymmetric skin folds • Skin folds in groin or buttock, not thigh Concerning Normal
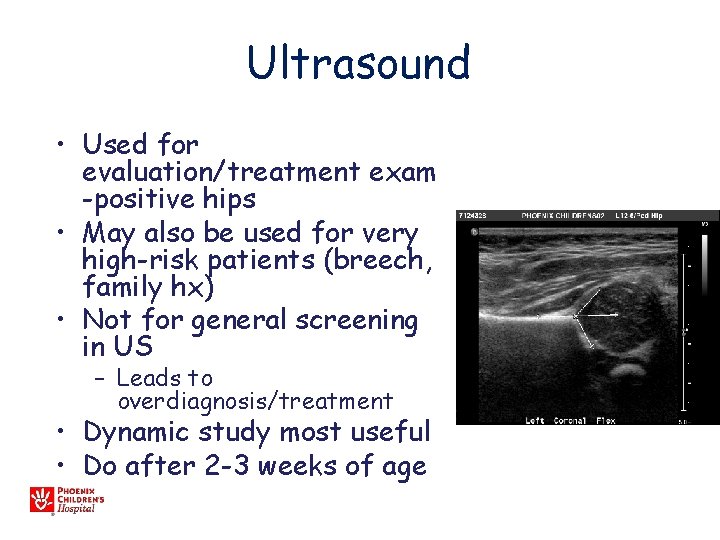
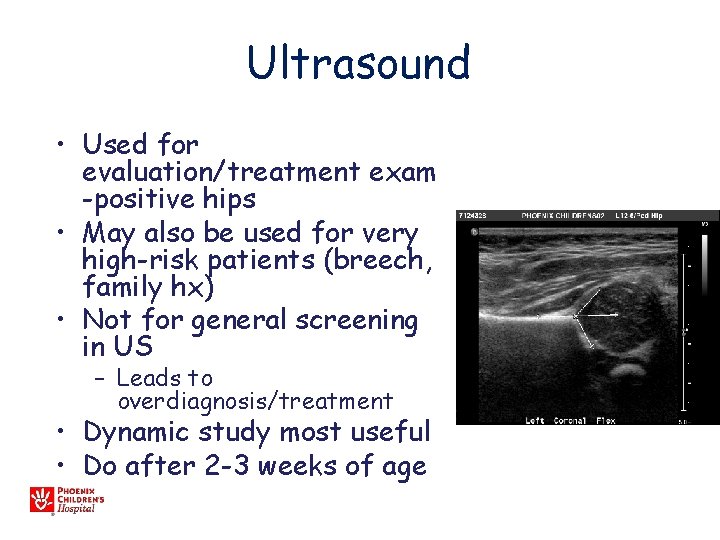
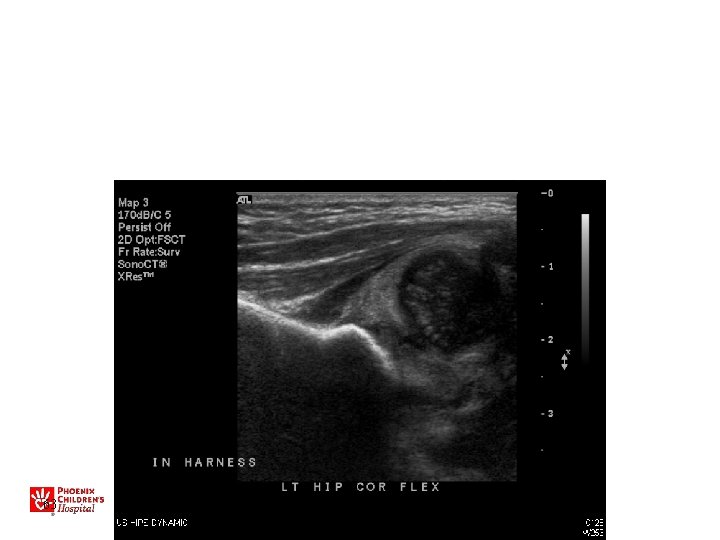
Ultrasound • Used for evaluation/treatment exam -positive hips • May also be used for very high-risk patients (breech, family hx) • Not for general screening in US – Leads to overdiagnosis/treatment • Dynamic study most useful • Do after 2 -3 weeks of age
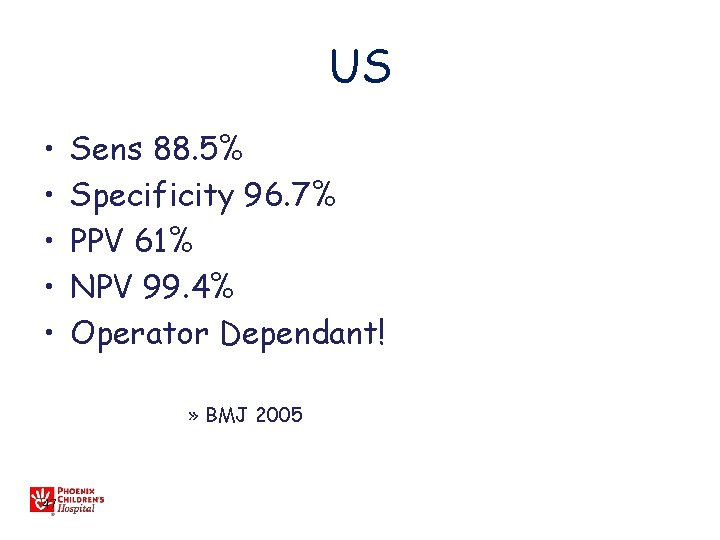
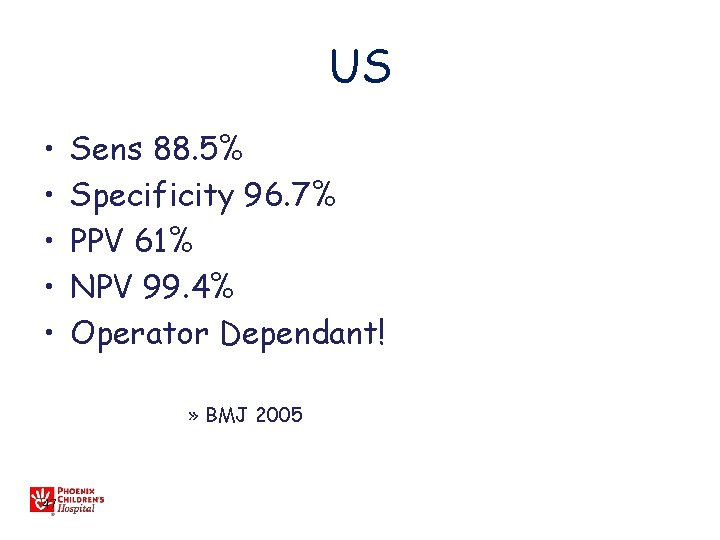
US • • • Sens 88. 5% Specificity 96. 7% PPV 61% NPV 99. 4% Operator Dependant! » BMJ 2005 47
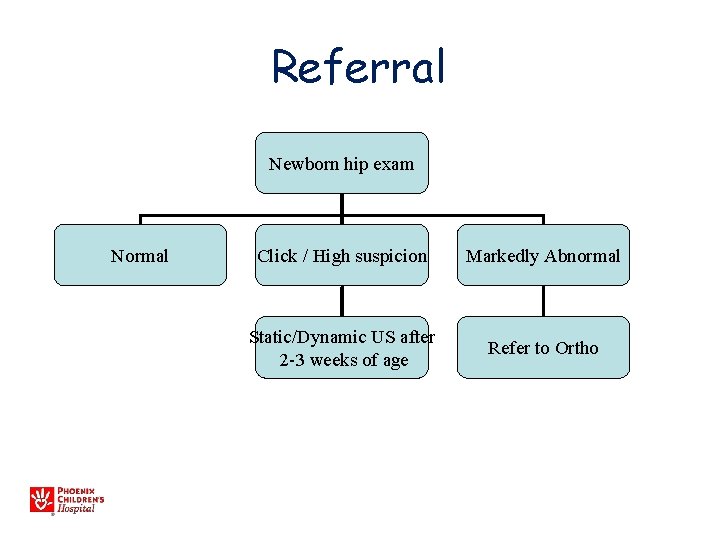
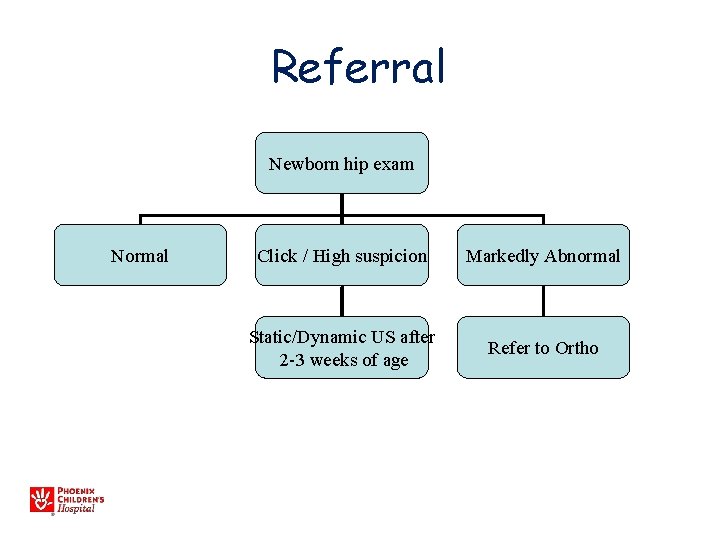
Referral Newborn hip exam Normal Click / High suspicion Markedly Abnormal Static/Dynamic US after 2 -3 weeks of age Refer to Ortho
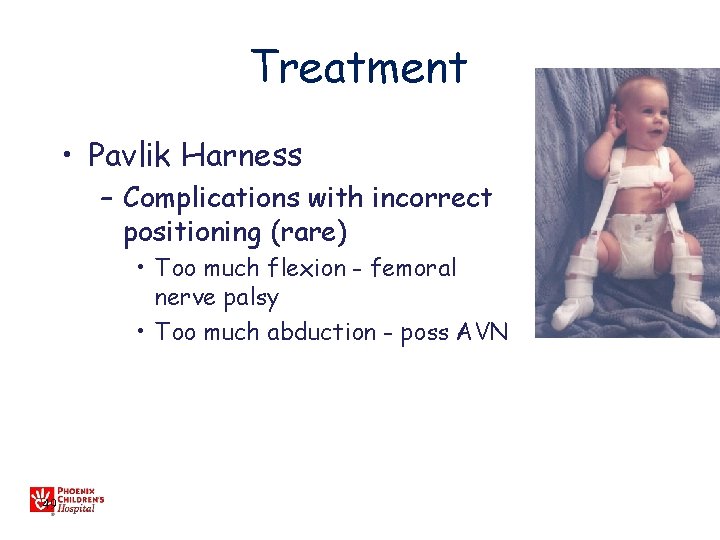
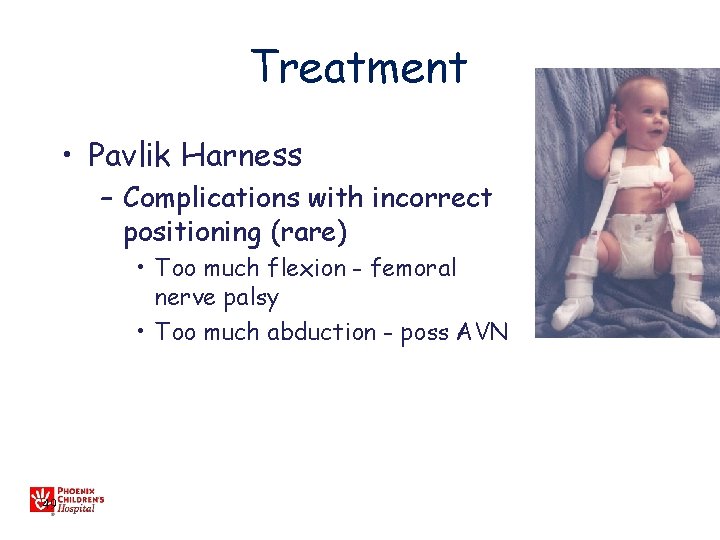
Treatment • Pavlik Harness – Complications with incorrect positioning (rare) • Too much flexion - femoral nerve palsy • Too much abduction - poss AVN 49
Treatment • Pediatrics 12/09 – Some cases of mild dysplasia resolve – May be no detriment in observing for 6 wks – Does NOT apply to unstable hips 50 50
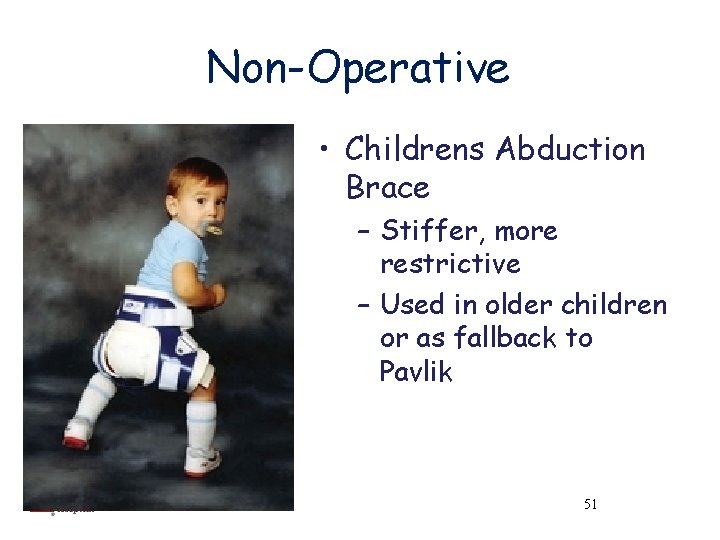
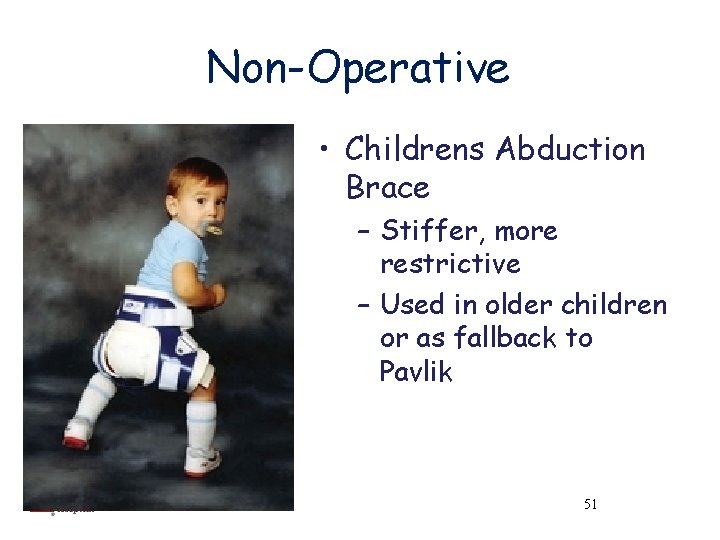
Non-Operative • Childrens Abduction Brace – Stiffer, more restrictive – Used in older children or as fallback to Pavlik 51 51
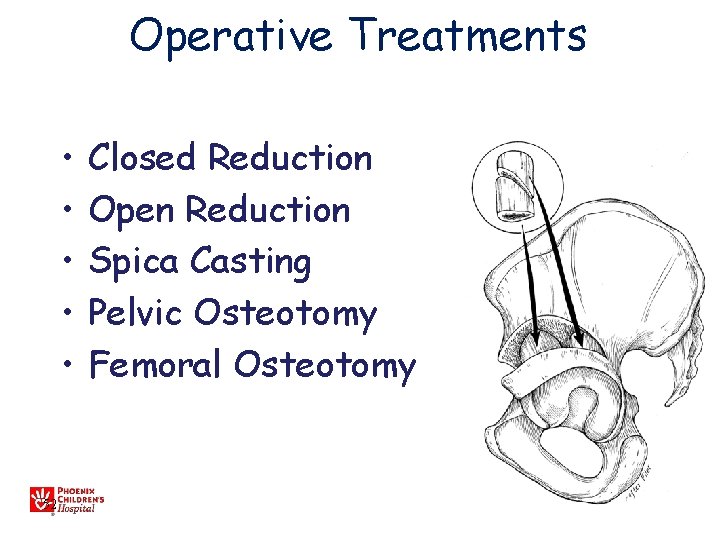
Operative Treatments • • • 52 Closed Reduction Open Reduction Spica Casting Pelvic Osteotomy Femoral Osteotomy
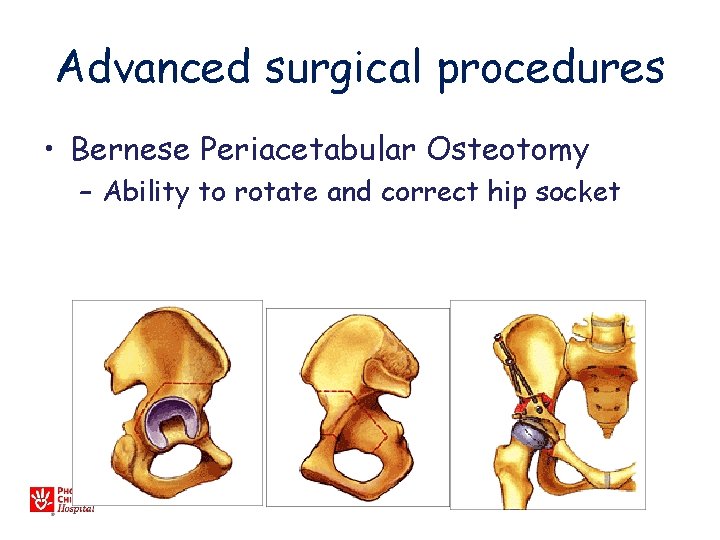
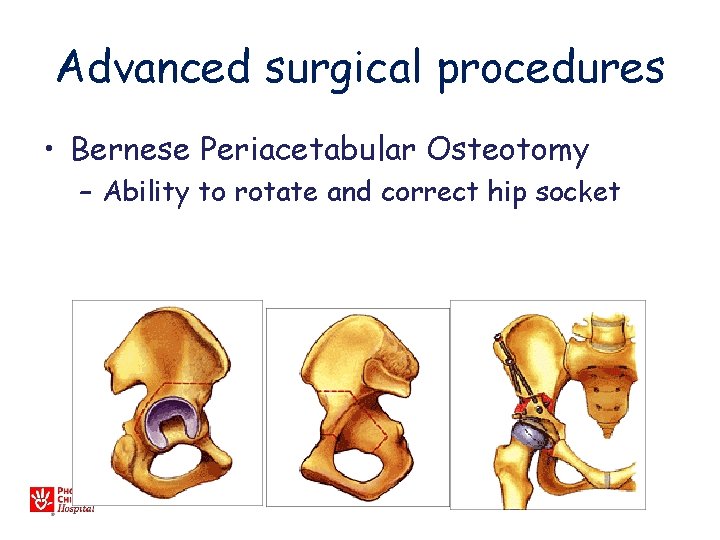
Advanced surgical procedures • Bernese Periacetabular Osteotomy – Ability to rotate and correct hip socket
• Early diagnosis and appropriate treatment can minimize operative treatments 54 54
DDH CASES 55
8 day old female infant • • 56 Mother’s first child Breech, C-section Otherwise healthy R hip dislocated, can be reduced with Ortolani

57
• Pavlik Harness treatment for 8 weeks 58
59
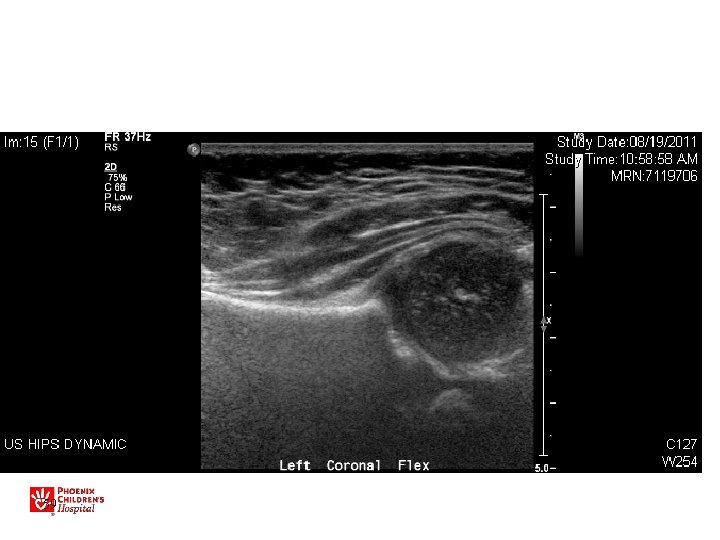
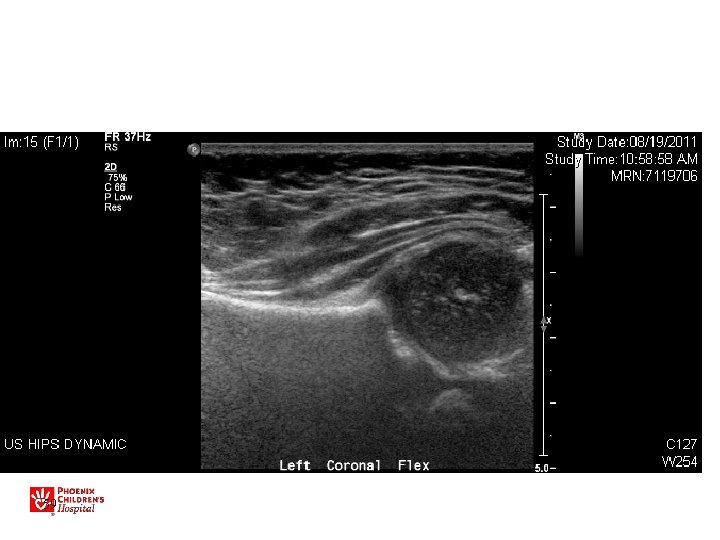
9 day old female infant • Mother’s first child • Breech • R hip dislocated, can be reduced with Ortolani • Decreased abduction, positive Galeazzi 60

61
• Pavlik Harness 62
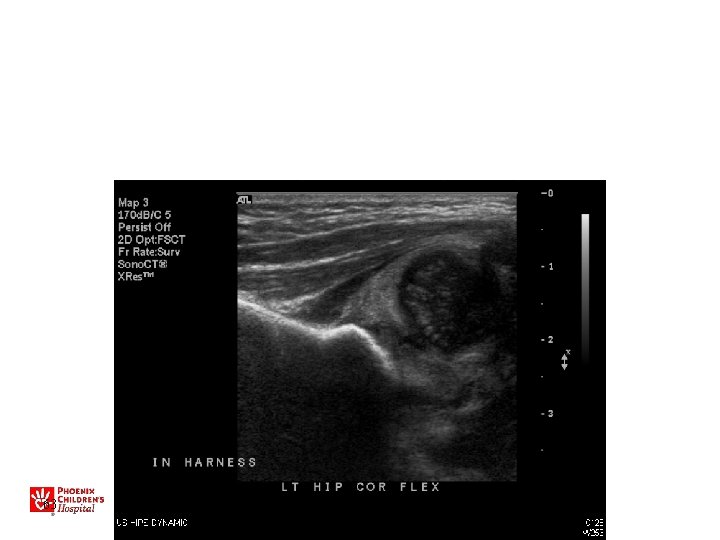
63
• Abduction brace 64

65

66
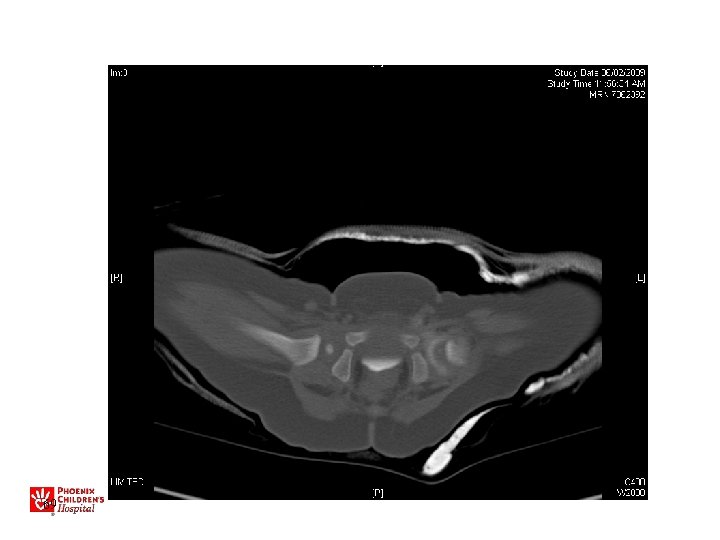
• Arthrogram • Closed reduction • Cast 67

68
69
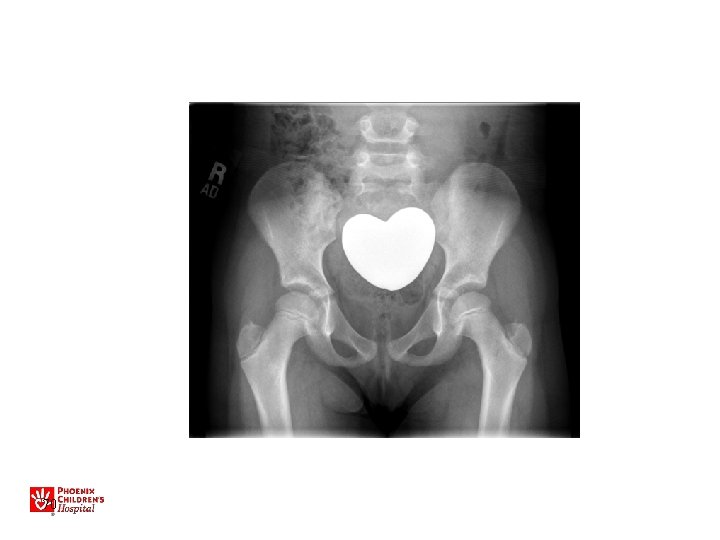
70
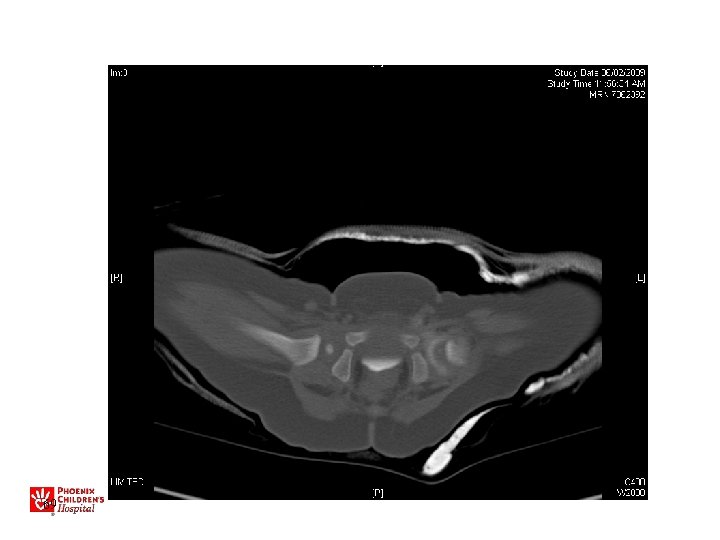
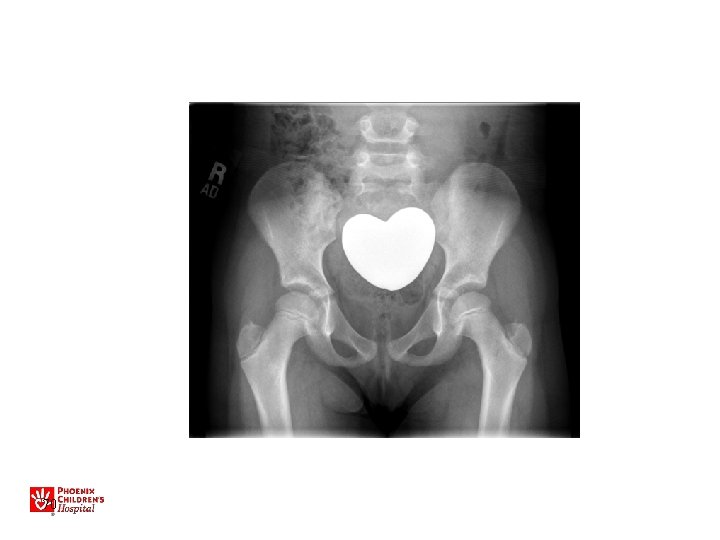
13 yo with hip pain, limp • Family has noted increased pain with activity, not able to walk long distances • No infantile treatment or history • Patient has features of Charcot-Marie. Tooth (associated with hip dysplasia)

• Bilateral periacetabular osteotomies • Bilateral femoral osteotomies

Recommended Reading • Guille JT, Pizzutillo PD, Mac. Ewen GD. Development dysplasia of the hip from birth to six months. J Am Acad Orthop Surg. 2000 Jul-Aug; 8(4): 232 -42. – Comprehensive orthopaedic review • Shipman S, Helfand M, Nygren P, Bougatsos Screening for Developmental Dysplasia of the Hip US Prev Services Task Force 2006 – Reviews available literature, but conclusions are “incomplete” • Mahan S, Katz J, Kim Y. To screen or not to screen? A decision analysis of the utility of screening for DDH. JBJS 2009 91: 1705 -19 75
Thank you!
 Judson karlen
Judson karlen Dean karlen
Dean karlen Barbro karlen debunked
Barbro karlen debunked Nancy judson
Nancy judson Judson odell
Judson odell Hip hop hip to the hippity
Hip hop hip to the hippity Hip to the hippity hop
Hip to the hippity hop Early middle childhood
Early middle childhood Ulcer niche and ulcer notch
Ulcer niche and ulcer notch Boutonniere and swan neck deformity
Boutonniere and swan neck deformity Structural deformity
Structural deformity Swan neck deformity
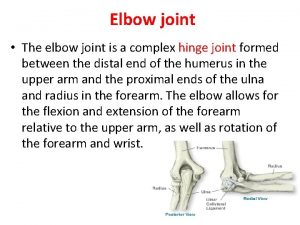
Swan neck deformity Humeroulnar joint
Humeroulnar joint Swan neck deformity
Swan neck deformity Triple alliance
Triple alliance Clare fy
Clare fy Klisic sign
Klisic sign Venous ulcer grading
Venous ulcer grading Gunstock deformity adalah
Gunstock deformity adalah Swan neck deformity
Swan neck deformity Vulpius procedure
Vulpius procedure Froment's sign
Froment's sign Caplan syndrome
Caplan syndrome Ape hand
Ape hand Dinner fork vs garden spade deformity
Dinner fork vs garden spade deformity Boutonniere and swan neck deformity
Boutonniere and swan neck deformity Aterior
Aterior Policeman tip palsy
Policeman tip palsy Anatomy standard
Anatomy standard Gunstock deformity
Gunstock deformity Bell clapper deformity pictures
Bell clapper deformity pictures Is it good to drink water
Is it good to drink water Dorsiflexion of wrist
Dorsiflexion of wrist Leukocyte esterase
Leukocyte esterase Erb's palsy
Erb's palsy Policeman tip hand
Policeman tip hand Gun stock deformity
Gun stock deformity Objective examination of patient
Objective examination of patient Boutonniere and swan neck deformity
Boutonniere and swan neck deformity Thoracodorsal nerve supplies
Thoracodorsal nerve supplies Perinatal period
Perinatal period Spencel
Spencel Osteite condensante
Osteite condensante Froment's sign
Froment's sign Intrinsic plus position
Intrinsic plus position Chapter 24 the forearm wrist hand and fingers
Chapter 24 the forearm wrist hand and fingers Eular criteria for rheumatoid arthritis
Eular criteria for rheumatoid arthritis Part of the elbow joint
Part of the elbow joint Genua recurvata
Genua recurvata Kaiser wilhelm deformity
Kaiser wilhelm deformity Stork leg deformity
Stork leg deformity Extra articular manifestations of rheumatoid arthritis
Extra articular manifestations of rheumatoid arthritis Bird beak deformity volvulus
Bird beak deformity volvulus Phoenix media planning
Phoenix media planning Classification of periradicular lesions
Classification of periradicular lesions Phoenix infant academy
Phoenix infant academy Aetna better health wv
Aetna better health wv Studentvue pxu
Studentvue pxu Lcps phoenix
Lcps phoenix City of phoenix sbe
City of phoenix sbe Champion phoenix trial
Champion phoenix trial University of phoenix
University of phoenix Phoenix echris
Phoenix echris Lisc phoenix
Lisc phoenix Phoenix controls corporation
Phoenix controls corporation Microsoft dynamics ax user group
Microsoft dynamics ax user group Uscis po box 20700 phoenix
Uscis po box 20700 phoenix Phoenix union high school district 210
Phoenix union high school district 210 Phoenix compiler
Phoenix compiler Phoenix embosser
Phoenix embosser Cientista phoenix arizona sangue
Cientista phoenix arizona sangue Computer science university of phoenix
Computer science university of phoenix Phoenix life cycle
Phoenix life cycle Emotional or subjective acting
Emotional or subjective acting Barriers to critical thinking university of phoenix
Barriers to critical thinking university of phoenix Bungee jumping phoenix
Bungee jumping phoenix Phoenix controls honeywell
Phoenix controls honeywell