Chapter 15 Sexually Transmitted Infections STIs Infections that

- Slides: 59
Chapter 15 Sexually Transmitted Infections
STI’s • Infections that can be transmitted through sexual activity • May be caused by a bacteria, virus, fungus, or other organism • Some are curable, some are not • Left untreated, STIs can cause pain, sickness, infertility, birth defects, and sometimes, death • STIs are very common (see next slide) • You can have more than one STI at a time, and you can get the same STI more than once.
Incidence of STIs • Startling statistics – ~1/2 of the STIs diagnosed annually in the US occur among people under 25 – ~19, 000 new cases each year in US – Approximately 3 million teenagers are infected w/STIs each year – 25% of U. S. population > 1 STI by age 35 – Largest proportion of AIDS cases infected in teens or 20 s
Factors contributing to high rates of STIs in the US • Main reason: multiple sexual partners and unprotected sex--especially prevalent behavior in adolescence and early adulthood • Use of oral contraceptive • Limited access to health care • Practitioners do not ask questions about patients’ sexual behaviors • Some diseases have no obvious symptoms • Difficulty talking to partner
Info in this chapter • You will learn about the most common STIs – Prevalence – How to recognize them – What should be done to treat them – How to avoid contracting or transmitting them • Information may be graphic at times • Purpose is not to scare you or discourage you from exploring joys of sexuality – Rather, information here is intended to help you make better decisions and be healthy
For each STI: • Know what causes it (bacteria, virus, other organism, etc. ) • Know how it can be transmitted, and how to avoid transmission • Know what the symptoms are • Know how it is treated, if treatment is available
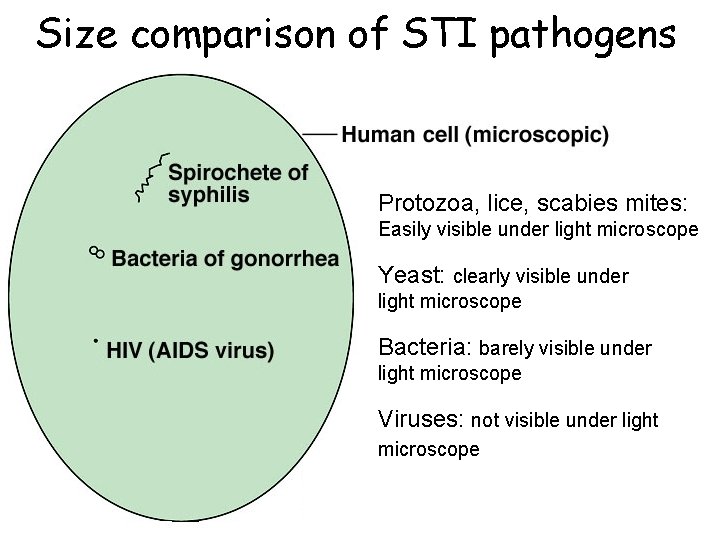
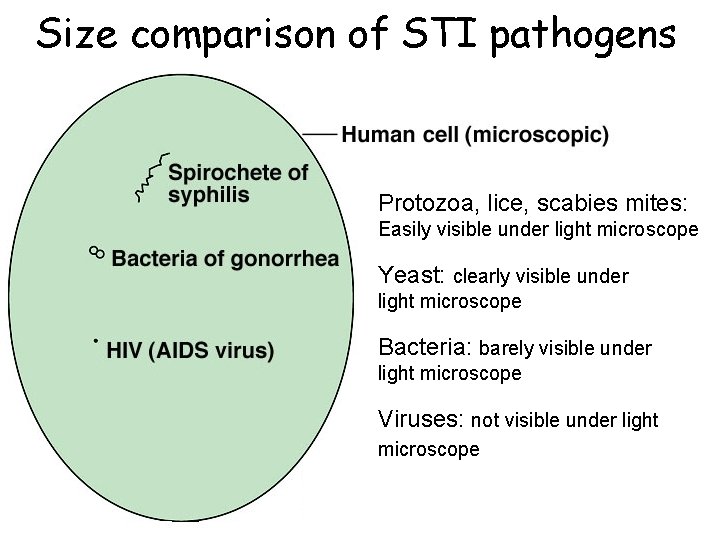
Size comparison of STI pathogens Protozoa, lice, scabies mites: Easily visible under light microscope Yeast: clearly visible under light microscope Bacteria: barely visible under light microscope Viruses: not visible under light microscope
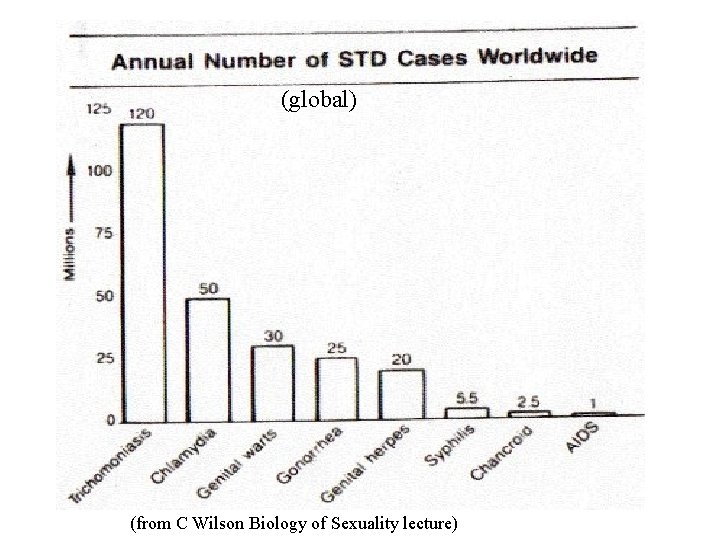
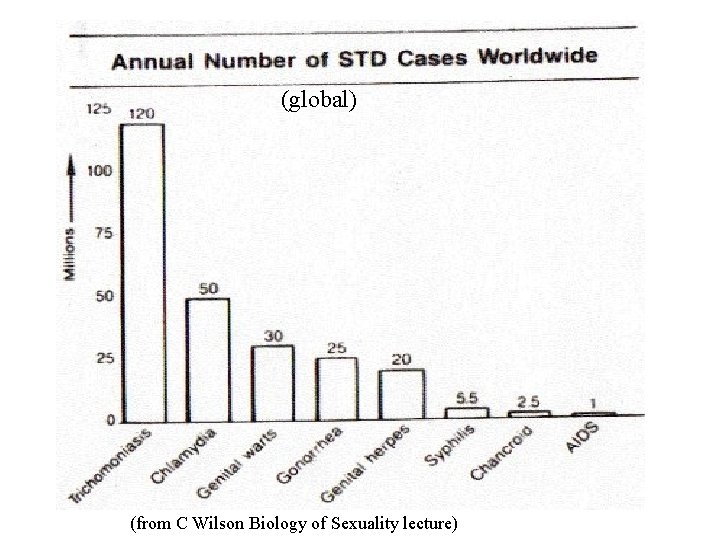
(global) (from C Wilson Biology of Sexuality lecture)
Bacterial infections • • • Chlamydia Gonorrhea Nongonococcal urethritis (NGU) Syphilis Bacterial vaginosis
Chlamydia • Caused by: bacterium Chlamydia trachomatis that infects the urogenital system • Prevalence: The most common bacterial STI in the US (3 -4 million new cases a yr. in US) • Transmission: primarily penile-vaginal, oral-genital, oral-anal, or genital-anal contact; can also be spread by fingers from one body site to another. • Symptoms: – In majority of cases, none! – if present: • Women: mild irritation or itching, burning urination, slight vaginal discharge • Men: urethral discharge, burning urination
Chlamydia (cont. ) • Consequences if left untreated: • Women: pelvic inflammatory disease (PID) – Bacterial infection spreads from cervix up into uterine lining, fallopian tubes, and possibly ovaries. – Symptoms of PID include disrupted menstruation, chronic pelvic pain, lower back pain, fever, nausea, vomiting, and headache. – Even after treatment, scar tissue from PID can block fallopian tubes and cause infertility or ectopic pregnancy (very dangerous) • Men: epididymitis (infection of the epididymis) or urethritis (infection of the urethral tube) – Symptoms of epididymitis: heaviness in testis; small, hard, painful swelling in testis; inflamed scrotum – Symptoms of urethritis: penile discharge, burning urination
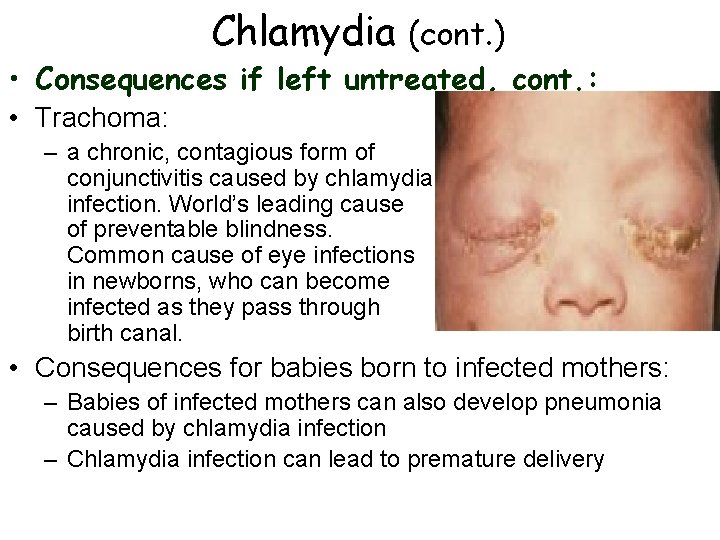
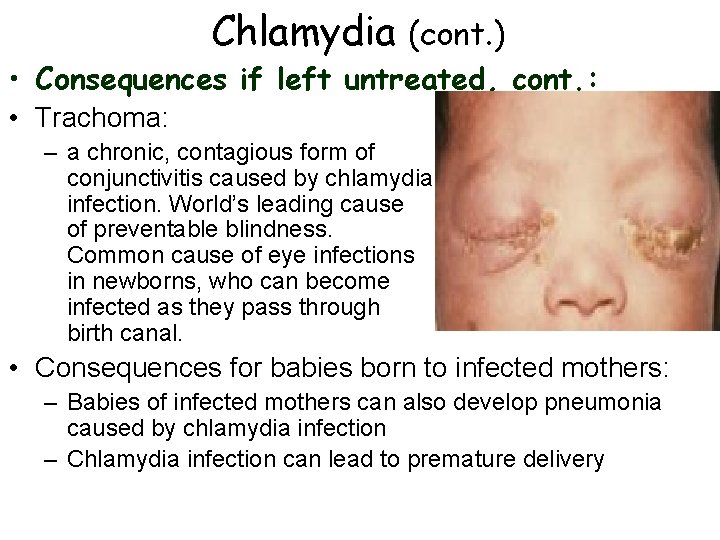
Chlamydia (cont. ) • Consequences if left untreated, cont. : • Trachoma: – a chronic, contagious form of conjunctivitis caused by chlamydia infection. World’s leading cause of preventable blindness. Common cause of eye infections in newborns, who can become infected as they pass through birth canal. • Consequences for babies born to infected mothers: – Babies of infected mothers can also develop pneumonia caused by chlamydia infection – Chlamydia infection can lead to premature delivery

Chlamydia (cont. ) • Treatment: • 7 -day treatment of doxycycline, or one dose of azithromycin • All exposed sexual partners should be treated
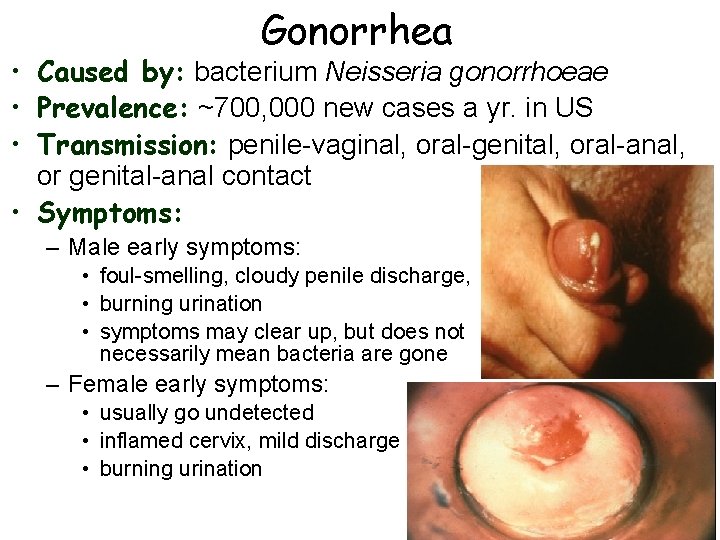
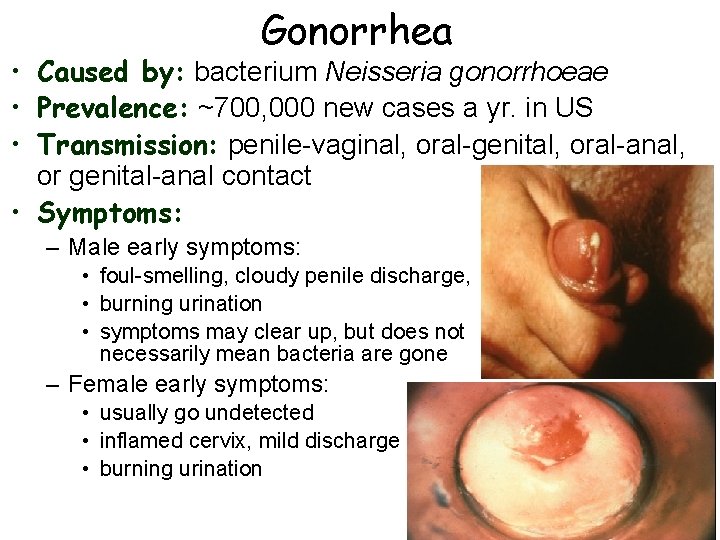
Gonorrhea • Caused by: bacterium Neisseria gonorrhoeae • Prevalence: ~700, 000 new cases a yr. in US • Transmission: penile-vaginal, oral-genital, oral-anal, or genital-anal contact • Symptoms: – Male early symptoms: • foul-smelling, cloudy penile discharge, • burning urination • symptoms may clear up, but does not necessarily mean bacteria are gone – Female early symptoms: • usually go undetected • inflamed cervix, mild discharge • burning urination
Gonorrhea (cont. ) • Consequences if left untreated: • Men: prostate abcesses, painful BMs, difficult urination, possible sterility due to scar tissue in epididymis after epididymitis • Women: PID (often more severe than w/chlamydia infection), ectopic pregnancy, severe pelvic pain due to scar-tissue adhesions across pelvis • Both sexes: can enter bloodstream and spread throughout body in ~2% of cases, causing fever, loss of appetite, arthritic pain, can invade heart, liver, CNS – Can cause blindness in infants (due to conjunctivitis)
Gonorrhea (cont. ) • Treatment: • Dual therapy of two antibiotic regimens • Often, chlamydia infections accompany gonorrhea infection--dual therapy will treat both infections • Resistant bacteria require special treatment • All exposed sexual partners should be treated
Nongonococcal Urethritis • Any urethral inflammation not caused by gonorrhea – Main infecting organisms: Chlamydia trachomatis and Mycoplasma genitalium – Can also result from other infectious agents, allergic reactions to vaginal secretions, or irritation from soaps, contraceptives, or deodorant sprays • Prevalence: quite common in men; symptoms in women are usually undetected • Transmission: mainly through penile-vaginal coitus • Symptoms: – Men: penile discharge, burning urination – Women: frequently, no symptoms; may have mild itching, burning urination, vaginal discharge of pus
Nongonococcal Urethritis (cont. ) • Consequences if left untreated: • Men: can spread to prostate, epididymis, or both • Women: cervial inflammation, PID • Treatment: • 7 -day treatment of doxycycline, or one dose of azithromycin • All exposed sexual partners should be treated
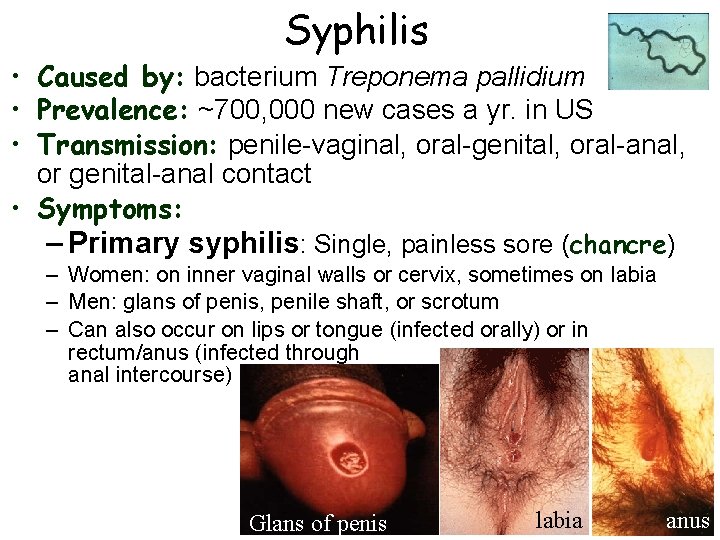
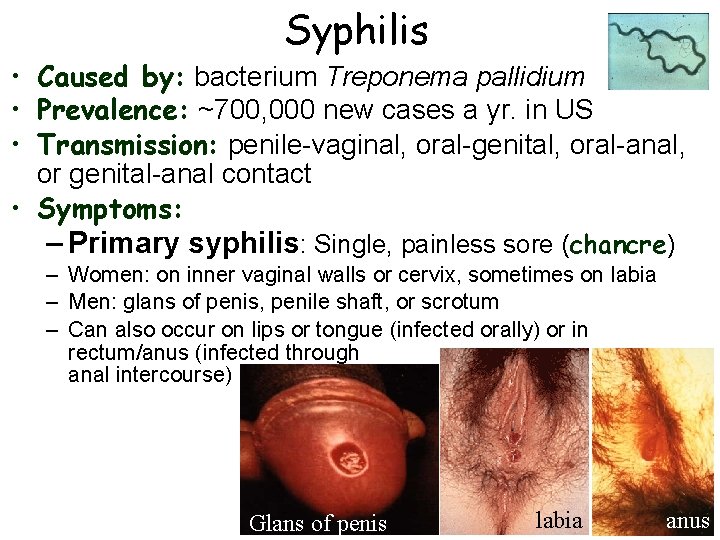
Syphilis • Caused by: bacterium Treponema pallidium • Prevalence: ~700, 000 new cases a yr. in US • Transmission: penile-vaginal, oral-genital, oral-anal, or genital-anal contact • Symptoms: – Primary syphilis: Single, painless sore (chancre) – Women: on inner vaginal walls or cervix, sometimes on labia – Men: glans of penis, penile shaft, or scrotum – Can also occur on lips or tongue (infected orally) or in rectum/anus (infected through anal intercourse) Glans of penis labia anus
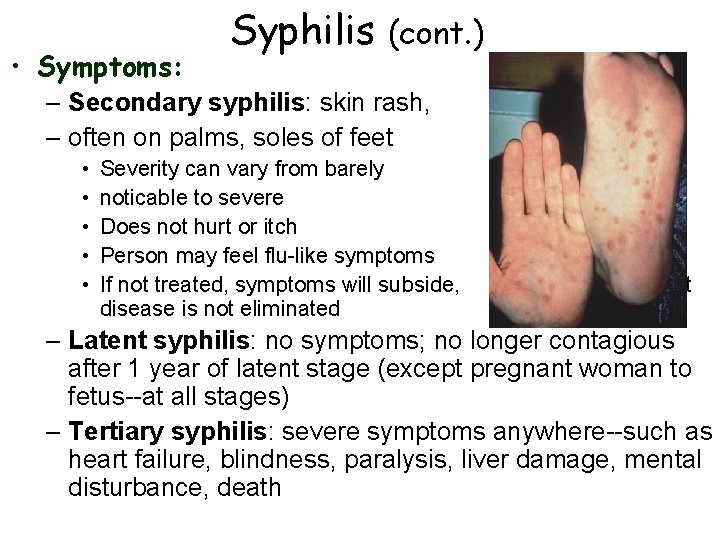
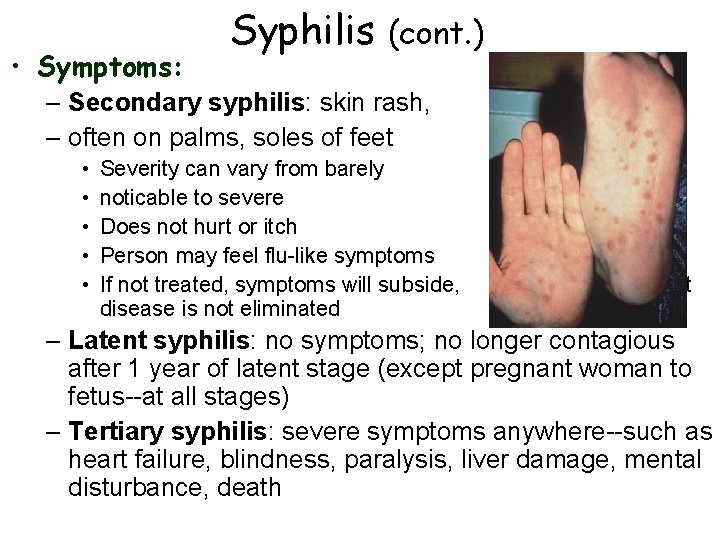
• Symptoms: Syphilis (cont. ) – Secondary syphilis: skin rash, – often on palms, soles of feet • • • Severity can vary from barely noticable to severe Does not hurt or itch Person may feel flu-like symptoms If not treated, symptoms will subside, disease is not eliminated but – Latent syphilis: no symptoms; no longer contagious after 1 year of latent stage (except pregnant woman to fetus--at all stages) – Tertiary syphilis: severe symptoms anywhere--such as heart failure, blindness, paralysis, liver damage, mental disturbance, death
Syphilis (cont. ) • Treatment: • Primary, secondary, or latent syphilis (< 1 yr) early cases treated with benzathine penicillin G or other antibiotic • All exposed sexual partners should be treated • Treated patients need blood tests at 3 -month intervals to make sure they are free of bacterium • To prevent birth defects, death to fetus, it is recommended that all pregnant women are tested for syphilis at first prenatal visit
Viral infections • Herpes Simplex Virus (HSV) • Human papillomavirus (HPV) – a. k. a. genital warts • Hepatitis – 3 types (HAV, HBV, HCV) • Human immunodeficiency virus (HIV)
Herpes • Caused by: Herpes simplex virus (HSV) – Two sexually transmitted types: HSV-1 and HSV-2 – HSV-1 is usually oral herpes (cold sores), but can infect genitals; HSV-2 usually causes genital lesions, but can also infect the mouth • Prevalence: >100 million Americans have oral herpes; >45 million Americans (20 -25%) have genital herpes • Transmission: – Genital herpes: penile-vaginal, oral-genital, oral-anal, or genital-anal contact – Oral herpes: through kissing, or oral-genital contact – Herpes sores are highly contagious--need to avoid contact between lesions and someone else’s body – Can still transmit herpes even if no lesions are present
Herpes (cont. ) • How to reduce risk of transmission: – Herpes virus cannot pass through latex condoms – During an outbreak (for most people, ~3 times/yr), best to avoid sexual contact with the lesion area--condoms should not be relied on when lesions are present – Between outbreaks--safest strategy is to use condoms, oral dams, etc. since there can sometimes be asymptomatic viral shedding • Condoms aren’t 100% effective at preventing transmission, since they don’t cover entire genital area, but they reduce risk significantly – Medications are available that reduce the amount of asymptomatic viral shedding that occurs between outbreaks--can significantly reduce risk of transmission
• Recurrence: Herpes (cont. ) – After lesions heal, virus retreats up nerve fibers and stays dormant in nerve cells in the spinal column – Flare-ups occur when virus moves back down along fibers to genitals or lips – Triggered by wide variety of factors, such as: stress, anxiety, depression, acidic food, UV light, fever, poor nutrition, fatigue – Symptoms during recurrent attacks tend to be milder than primary episode, heal more quickly – Prodromal symptoms: symptoms that warn of an impending herpes outbreak • Burning, throbbing, or tingling at sites of infection • Sometimes includes pain in legs, thighs, groin, or buttocks • Viral shedding is more common during prodromal symptoms than beforehand--best to avoid contact w/infected area from first sign of prodromal symptoms until sores have healed
Herpes (cont. ) • Other complications: • Women: – Increased incidence of cervical cancer--women with herpes should get Pap smears every 6 -12 months – Newborn baby can be infected by passage through birth canal--can cause severe damage or death • C-section recommended for women w/active symptomatic disease • Both sexes: – Ocular herpes infection can occur if virus is transferred from a sore to the eye • Must be treated quickly to avoid eye damage
• Treatment: Herpes (cont. ) • Reduce frequency of outbreaks • Treat symptoms of outbreaks and speed healing • Two types of therapies – Suppressive therapy: medication taken daily to prevent recurrent outbreaks; also reduces asymptomatic viral shedding between outbreaks – Episodic treatment: medication taken to treat outbreaks when they occur • Antiviral drugs-- reduce viral shedding and the duration and severity of outbreaks – Acyclovir (trade name Zovirax) – Valacyclovir (trade name Valtrex) – Famiclovir (trade name Famvir)
Genital warts • Caused by: Human papilloma virus (HPV) – There are over 100 strains, ~1/2 cause genital infections • Prevalence: >15% of Americans; >6 million new cases in US each year • Transmission: – Penile-vaginal, oral-genital, oral-anal, or genital-anal contact – Condoms do provide some protection, but don’t prevent transmission of viral infections on vulva, base of penis, scrotus, and other genital areas not covered by condoms – HPV is most commonly transmitted by people who are asymptomatic
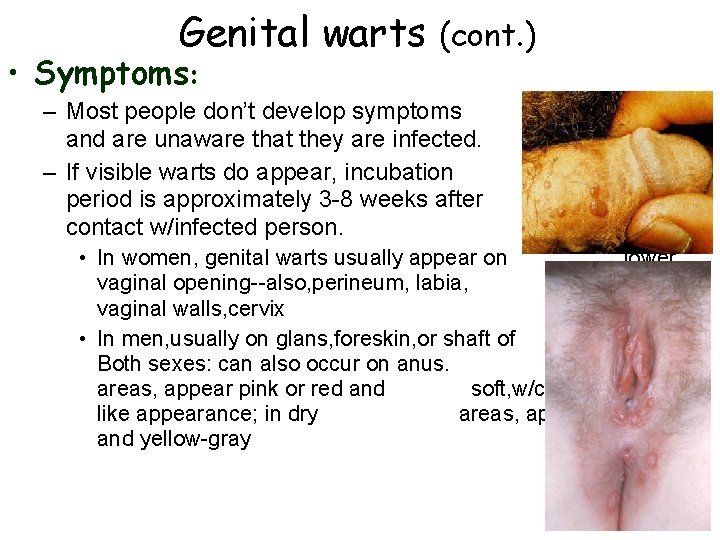
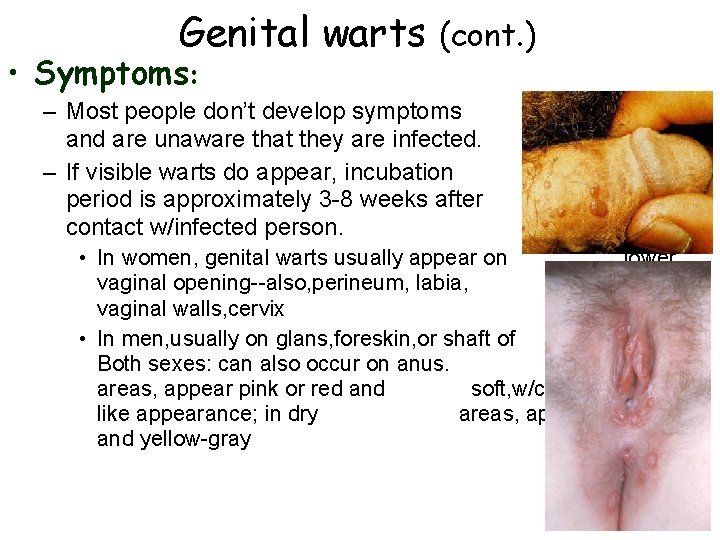
Genital warts • Symptoms: (cont. ) – Most people don’t develop symptoms and are unaware that they are infected. – If visible warts do appear, incubation period is approximately 3 -8 weeks after contact w/infected person. • In women, genital warts usually appear on lower vaginal opening--also, perineum, labia, inner vaginal walls, cervix • In men, usually on glans, foreskin, or shaft of penis. Both sexes: can also occur on anus. In moist areas, appear pink or red and soft, w/cauliflowerlike appearance; in dry areas, appear hard and yellow-gray
Genital warts (cont. ) • Consequences: • Certain strains of HPV are associated with cancers of the cervix, vagina, vulva, urethra, penis, & anus • HPV infections account for 85 -90% of risk for development of cervical cancer – Risk of HPV-induced cervical cancer is minimal if regular Pap testing and treatment of precancerous lesions is done • Pregnant women that are + for HPV can transmit the virus to their babies during birth – Can cause respiratory papillomatosis in infants--HPV infection of upper respiratory tract
Genital warts (cont. ) • Treatment: • Visible genital warts are removed by either cryotherapy (freezing) or chemical treatment; larger warts may require minor surgery to remove – Removal doesn’t necessarily prevent recurrence – Warts may disappear on their own • New: prevention via vaccine • Gardisil: vaccine against 4 strains of HPV that together cause 70% of cervical cancers and 90% of genital warts • US Dept. of Health and Human Services committee voted unanimously that females age 11 -26 should be vaccinated – Most health officials believe vaccination before puberty is best, before teens become sexually active
Hepatitis • Caused by: Hepatitis virus--attacks the liver – There are three types, each caused by a different hepatitis virus, hepatitis A (most common), hepatitis B, and hepatitis C • Prevalence: worldwide, >170 million people (5 million in US) have Hep. C infection (the most health-threatening of the 3 types) • Transmission: – All 3 types of hepatitis can be transmitted through sexual contact, but Hep. B (and somewhat, Hep. A)are transmitted more often through sex – Needle-sharing is also a common mode of transmission (most common mode of transmission for Hep. C) – Hep. A spread primarily through fecal-oral route • Oral-anal sexual contact • Infected food handlers not washing hands after using bathroom – From infected mother to fetus or infant
Hepatitis (cont. ) • Symptoms: – Symptoms vary considerably: • • May have no symptoms May have mild flu-like symptoms May have high fever, vomiting, severe abdominal pain Jaundice can occur--yellowing of whites of the eyes or the skin due to increased breakdown of RBC. • Consequences: • Chronic infection w/Hep. B or Hep. C is a major risk factor for liver cancer • ~20 -25% of Hep. C+ people manifest progressive disease resulting in severe liver complications--liver cancer, cirrhosis, liver failure
• Treatment: Hepatitis (cont. ) • Hep. A: bed rest, fluid intake--usually runs its course in a few weeks to a few months • Hep. B: same as Hep. A, except that some Hep. B infections can become chronic and persist for >6 months – Chronic Hep. B infections are treated w/several antiviral drugs • Hep. C: more serious for the 20 -25% of Hep. C+ people with progressive chronic Hep. C infection--antiviral drugs can help somewhat for some strains of Hep. C (especially AIDS patients) • Vaccines • Available for Hep. A and Hep. B – High risk people (health care workers, injection drug users, sexually active people w/multiple sex partners, etc. ) should be immunized – CDC recommends that children be immunized for Hep. B
Common Vaginal Infections • Vaginitis: general term applied to variety of vaginal infections – May be caused by organisms that are already present in vagina • Sexual activity may introduce organism, or may throw off balance of ‘good’ microbes in the vagina – Bacterial vaginosis: caused by anaerobic bacteria, Mycoplasma bacteria, or Gardnerella vaginalis – Candidiasis: caused by yeast infection w/Candida albicans – Trichomoniasis: caused by one-celled protozoan Trichomonas vaginalis
Bacterial vaginosis (BV) • Very common vaginal infection • Occurs more frequently among sexually active women, though can occur in women who have not experience sexual intercourse • Symptoms (in women): foul-smelling pasty discharge, usually gray, can be white, yellow, or green – Most men are asymptomatic--some develop urethritis or bladder infection • If untreated, can increase risk of PID • If untreated in pregnant woman, associated w/ premature rupture of amniotic sac, preterm labor • Treatment w/oral or topical Flagyl (metronidazole) or clindamycin cream
Candidiasis • Also very common vaginal infection--3/4 of women will have at least one genital yeast infection in their lifetime • Candida albicans yeast are normally present in the vagina of many women--also present in mouth and intestines of many people – Only causes infection/disease when yeast becomes overgrown – Can occur during pregnancy, from antibiotics, spermicidal creams, oral contraceptives, high-sugar diet, diabetes • Symptoms (in women): – white, clumpy, cottage-cheese discharge – Intense itching and soreness of vaginal and vulval tissues • Treatment: topical intravaginal creams, available over the counter--wise to be diagnosed by a doctor first; – many women self diagnose incorrectly
Trichomoniasis • • Common in women and men 7 -8 new cases each year in US Primarily spread through sexual contact Symptoms (women): Trichomonas vaginalis – White or yellow-green discharge, frothy, w/unpleasant odor – Irritated vaginal and vulval tissues -- can increase a woman’s susceptibility to HIV infection – If untreated, can damage cervical cells, may lead to cervical cancer; in pregnant women, can lead to premature rupture of amniotic sac and preterm delivery • Symptoms (men): usually none, may have frequent or painful urination or slight urethral discharge • Treatment: metronidazole (Flagyl) – All sexual partners should be treated
Ectoparasitic infections • Ectoparasites: parasitic organisms that live on the outer skin surfaces • 2 common STIs caused by ectoparasites: 1) pubic lice 2) scabies
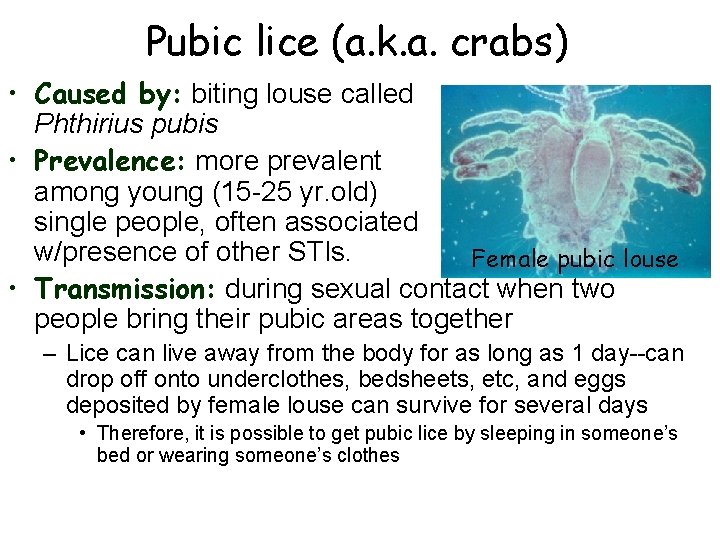
Pubic lice (a. k. a. crabs) • Caused by: biting louse called Phthirius pubis • Prevalence: more prevalent among young (15 -25 yr. old) single people, often associated w/presence of other STIs. Female pubic louse • Transmission: during sexual contact when two people bring their pubic areas together – Lice can live away from the body for as long as 1 day--can drop off onto underclothes, bedsheets, etc, and eggs deposited by female louse can survive for several days • Therefore, it is possible to get pubic lice by sleeping in someone’s bed or wearing someone’s clothes
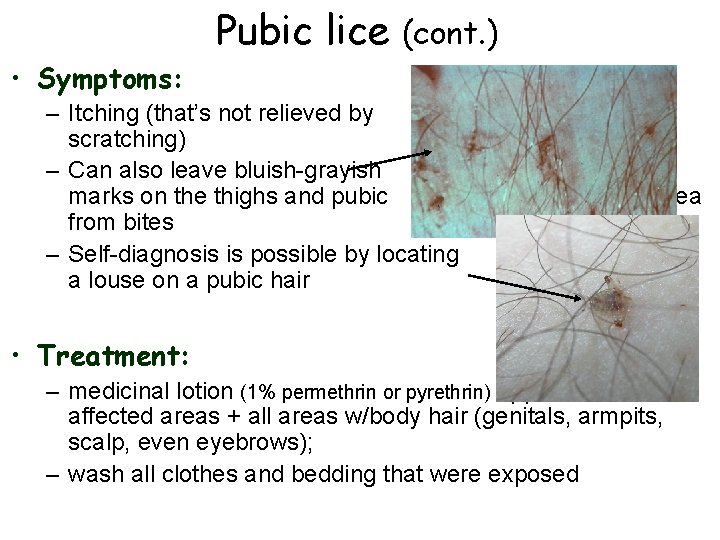
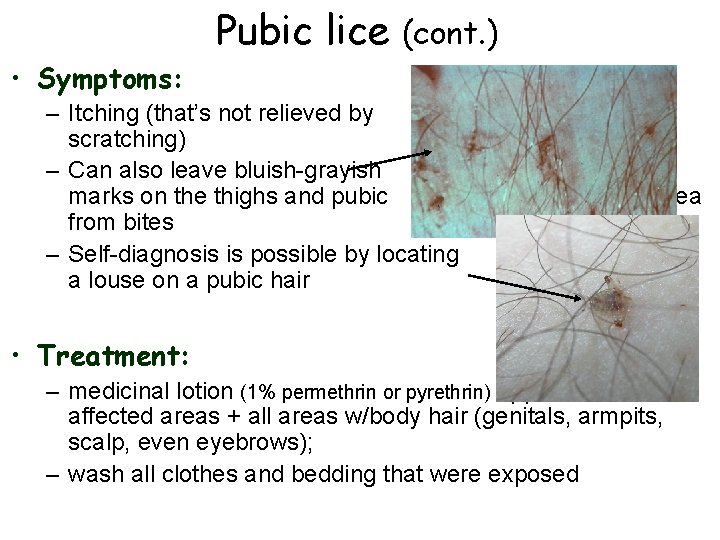
Pubic lice (cont. ) • Symptoms: – Itching (that’s not relieved by scratching) – Can also leave bluish-grayish marks on the thighs and pubic from bites – Self-diagnosis is possible by locating a louse on a pubic hair area • Treatment: – medicinal lotion (1% permethrin or pyrethrin) applied to all affected areas + all areas w/body hair (genitals, armpits, scalp, even eyebrows); – wash all clothes and bedding that were exposed
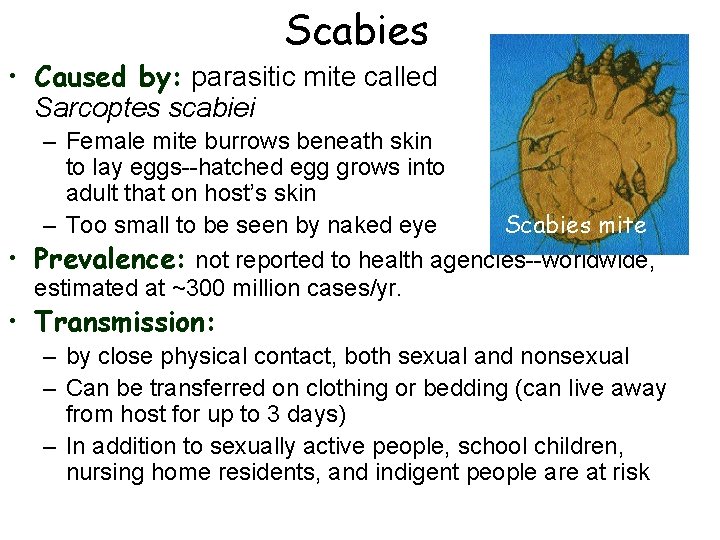
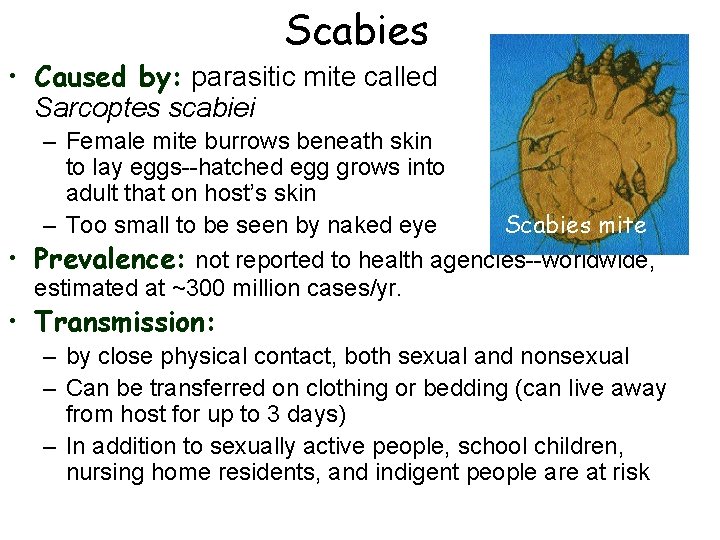
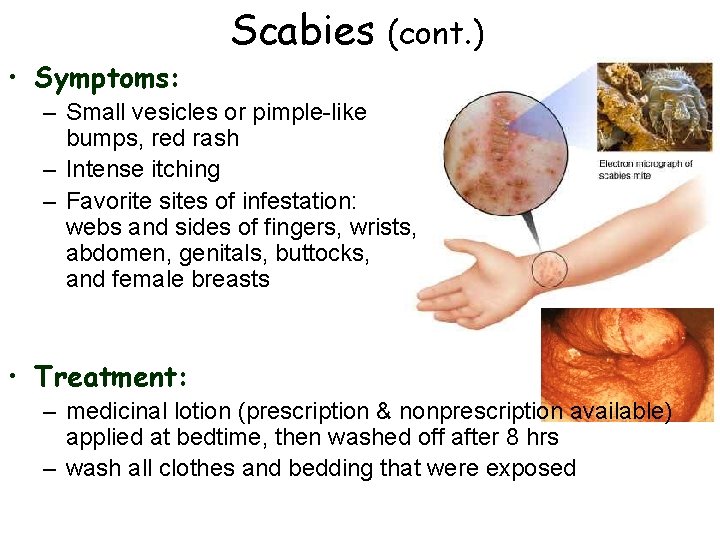
Scabies • Caused by: parasitic mite called Sarcoptes scabiei – Female mite burrows beneath skin to lay eggs--hatched egg grows into adult that on host’s skin – Too small to be seen by naked eye Scabies mite • Prevalence: not reported to health agencies--worldwide, estimated at ~300 million cases/yr. • Transmission: – by close physical contact, both sexual and nonsexual – Can be transferred on clothing or bedding (can live away from host for up to 3 days) – In addition to sexually active people, school children, nursing home residents, and indigent people are at risk
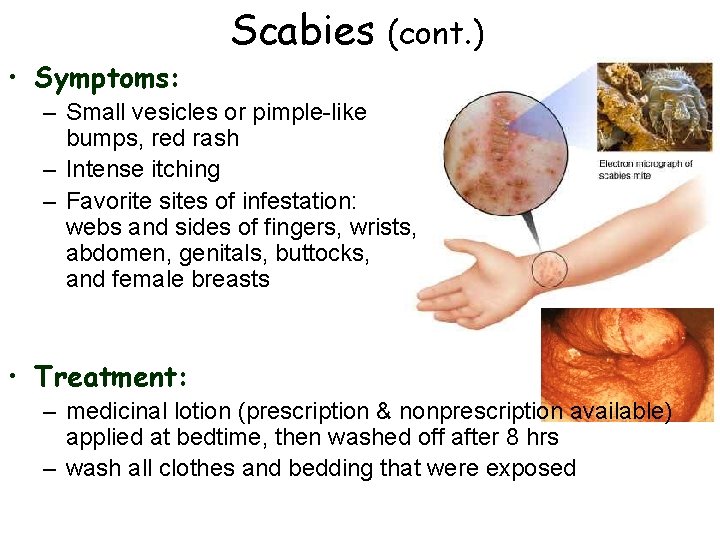
• Symptoms: Scabies (cont. ) – Small vesicles or pimple-like bumps, red rash – Intense itching – Favorite sites of infestation: webs and sides of fingers, wrists, abdomen, genitals, buttocks, and female breasts • Treatment: – medicinal lotion (prescription & nonprescription available) applied at bedtime, then washed off after 8 hrs – wash all clothes and bedding that were exposed
Aqcuired immunodeficiency sydrome (AIDS) • Caused by: • Infection w/the human immunodeficiency virus (HIV) • 2 strains, HIV-1, and HIV-2: HIV-1 is more virulent and causes most cases in US; HIV-2 exists along w/HIV-1 in some African countries • History • Research indicates that HIV originated from a subspecies of chimpanzees that reside in central/SW Africa – Chimps harbor a simian immunodeficiency virus (SIV) that genetically converted to HIV • HIV evolved from SIV sometime around 1931, but likely remained confined to a small isolated population – Eventually, migration into large cities and global travel spread the virus worldwide
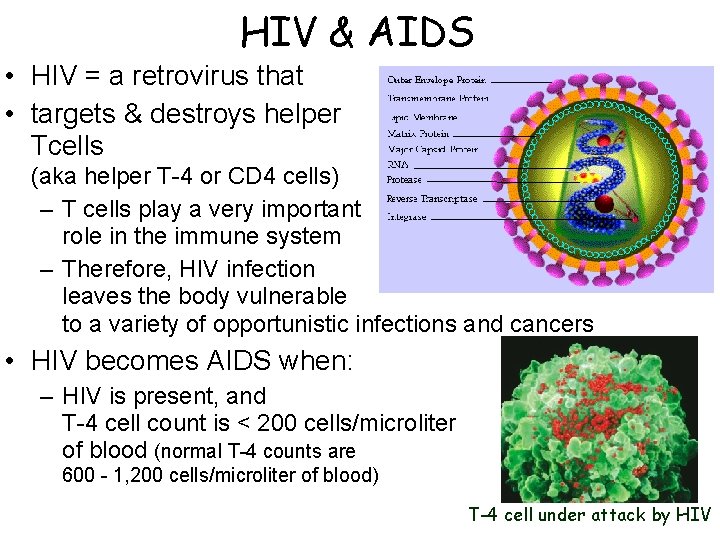
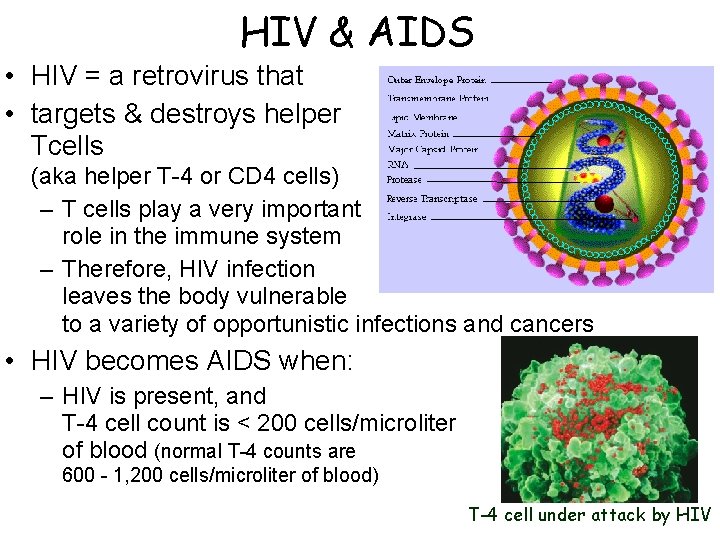
HIV & AIDS • HIV = a retrovirus that • targets & destroys helper Tcells (aka helper T-4 or CD 4 cells) – T cells play a very important role in the immune system – Therefore, HIV infection leaves the body vulnerable to a variety of opportunistic infections and cancers • HIV becomes AIDS when: – HIV is present, and T-4 cell count is < 200 cells/microliter of blood (normal T-4 counts are 600 - 1, 200 cells/microliter of blood) T-4 cell under attack by HIV
HIV/AIDS: prevalence in U. S. • >1 million cases reported as of Jan 2006 • > 525, 000 people died of AIDS since first diagnosis • Estimated ~1. 2 million people currently HIV+, and ~25 50% of these people are unaware of their HIV status • Overall rate of new HIV infections in US has slowed, but number of new infections among teenagers, women, and racial and ethnic minorities continues to rise – Teenagers: multiple sexual partners, less likely to have access to or to use condoms; substance abuse, feel invulnerable – Ethnic and racial minorities: reduced access to health care, cultural or language barriers to information about STI prevention, differences in high-risk behaviors – Women: fastest-growing HIV-infected population in US. --HIV more easily transmitted from men-to-women than vice versa
Women and HIV/AIDS • Number of women infected w/HIV is steadily increasing • Women are more easily infected from heterosexual intercourse w/and HIV+ partner than men are – Semen contains higher concentration of HIV than vaginal fluids – Female mucosal surface is exposed to HIV in ejaculate longer than a man’s penis is exposed to HIV in vaginal secretions – Larger area of mucosal surface is exposed in vagina/on vulva than on the penis – Female mucosal surface is exposed to greater potential trauma than the penis--can cause small tears that allow virus to enter – Some women have unprotected receptive anal intercourse--the single-most risky behavior in terms of HIV infection for both men and women – Adolescent women are more vulnerable to HIV infection b/c their reproductive tracts are immature--more susceptible to infection
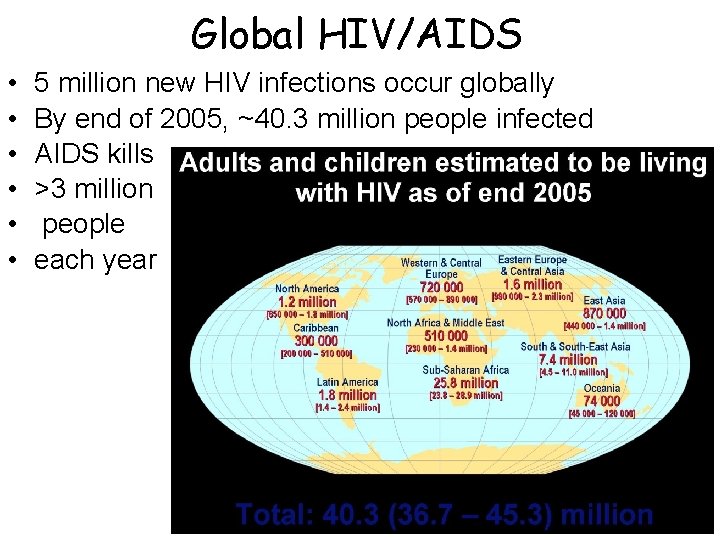
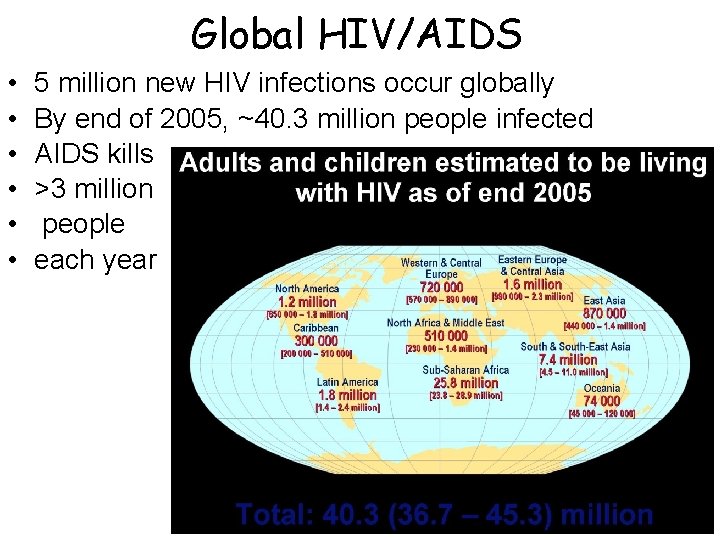
Global HIV/AIDS • • • 5 million new HIV infections occur globally By end of 2005, ~40. 3 million people infected AIDS kills >3 million people each year
AIDS in Africa • AIDS has reached epidemic proportions in sub. Saharan Africa; >15% of all adults are HIV+ – 2/3 (25. 8 million) of all people living w/AIDS live in sub. Saharan Africa – over 80% of AIDS deaths have occurred in Africa, primarily sub-Saharan Africa – 75% of HIV infections in African youth are of females – over 10. 5 million AIDS orphans in sub-Saharan Africa • Factors contributing: – Widespread poverty, lack of medical care, widespread ignorance about HIV prevention – Cultural factors, gender roles – General feeling of hopelessness
AIDS: Transmission • HIV in bodily fluids: – blood, semen, vaginal secretions, breast milk – NOTE: saliva, urine, tears--concentration of virus (if any) way too low to transmit infection. • Can be transmitted: – Through vaginal or anal intercourse or oral-genital contact – Through contaminated blood (needles, blood transfusion) – From mother to fetus before birth, infant during birth or after through breastfeeding • Likelihood of transmission during sexual contact: – Depends on infected person’s viral load (#virus particles per ml of blood) – Is greater when HIV is transmitted directly into blood, (through small tears in rectal tissues or vaginal walls)
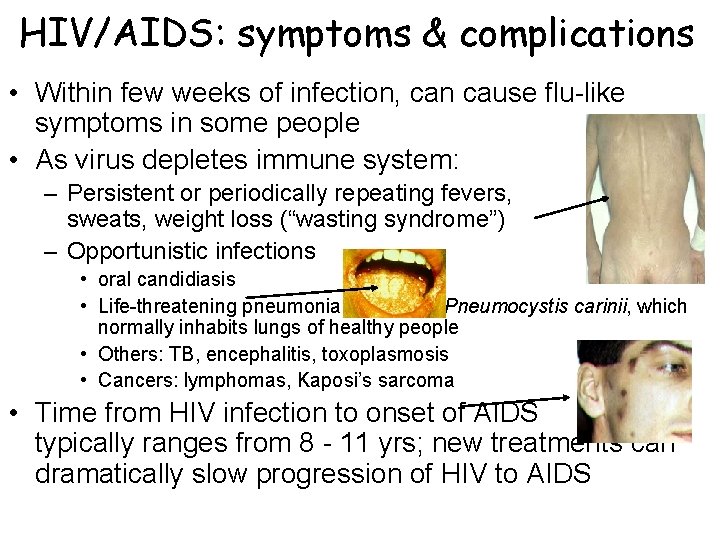
HIV/AIDS: symptoms & complications • Within few weeks of infection, can cause flu-like symptoms in some people • As virus depletes immune system: – Persistent or periodically repeating fevers, sweats, weight loss (“wasting syndrome”) – Opportunistic infections night • oral candidiasis • Life-threatening pneumonia caused by Pneumocystis carinii, which normally inhabits lungs of healthy people • Others: TB, encephalitis, toxoplasmosis • Cancers: lymphomas, Kaposi’s sarcoma • Time from HIV infection to onset of AIDS typically ranges from 8 - 11 yrs; new treatments can dramatically slow progression of HIV to AIDS
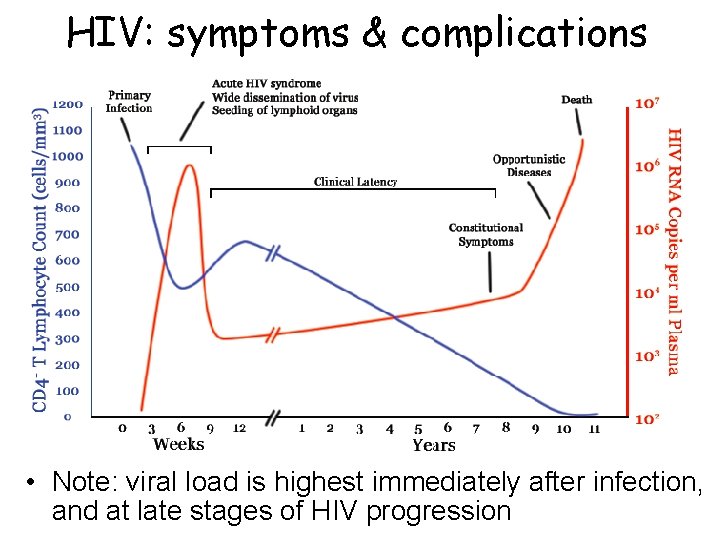
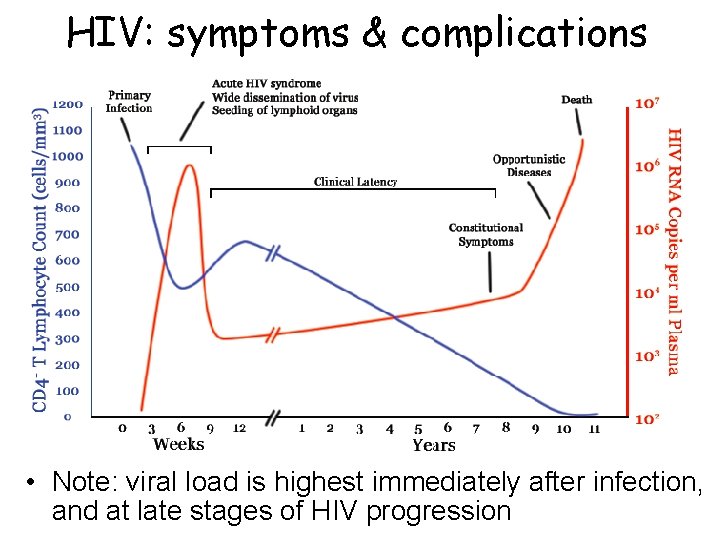
HIV: symptoms & complications • Note: viral load is highest immediately after infection, and at late stages of HIV progression
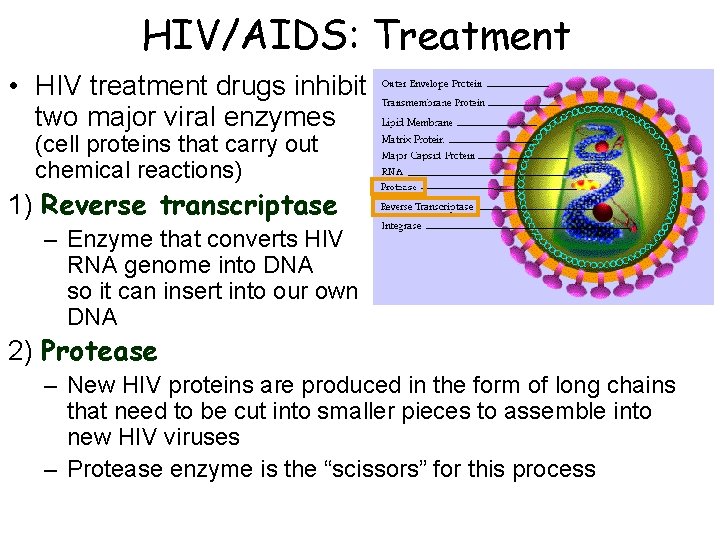
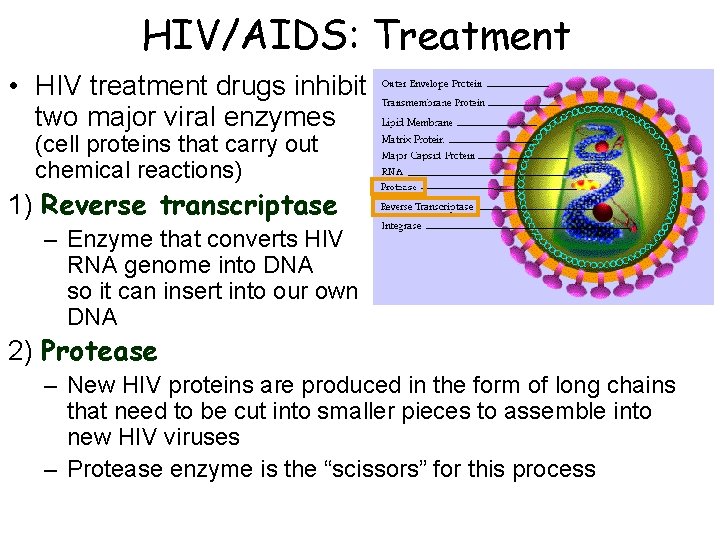
HIV/AIDS: Treatment • HIV treatment drugs inhibit two major viral enzymes (cell proteins that carry out chemical reactions) 1) Reverse transcriptase – Enzyme that converts HIV RNA genome into DNA so it can insert into our own DNA 2) Protease – New HIV proteins are produced in the form of long chains that need to be cut into smaller pieces to assemble into new HIV viruses – Protease enzyme is the “scissors” for this process
Drug therapy to prevent mother-tochild transmission (MTCT) of HIV • Zidovudine (an RT inhibitor) can reduce MTCT by 2/3 if given to both HIV-infected mothers & their newborns – Drug is given orally to pregnant women during gestation, by IV during labor, and orally to newborn for first 6 weeks of life – # of infants infected through MTCT in U. S. has declined dramatically due to widespread use of this treatment – Treatment regimen is very costly, and involves multiple treatments, making it hard to administer in many poorer countries – Recent studies in S. Africa & Uganda: infants given either a single dose or a short-course regimen of nevirapine (RT inhibitor) experienced excellent protection from HIV infection – Infected mother must still refrain from breastfeeding to avoid infecting newborn
The search for a vaccine • Vaccine: a harmless variant or protein/DNA fragment from a pathogen (e. g. the HIV virus) that prevents infection by the pathogen by stimulating the immune system to develop long-lasting defenses. • Several attempts have been made to develop a vaccine against HIV--so far, w/disappointing results • Many more vaccine candidates (over 30 as of 2005) are currently being tested • Many challenges confront vaccine researchers: – Absence of ideal animal model for research – HIV is a very complicated virus w/multiple strains – HIV can change rapidly through genetic mutation
Preventing STIs • Only sure-fire way is abstinence, or monogamous relationship btwn 2 uninfected people • Get tested for STIs, insist that your partner do too – May want to wait for results before engaging in sexual activity that can put you at risk • Communicate w/partners about safe sex – Get to know potential sexual partners well enough to develop trust and communication – Inform a partner if you have an STI • Avoid sex w/multiple partners or w/individuals at high risk for STIs • Use condoms or oral dams • If you use injected drugs, do not share needles
Condoms • Latex condoms are highly effective in preventing transmission of HIV, chlamydia, gonorrhea, NGU, bacterial vaginosis, and trichomoniasis – Condoms are less effective in preventing infections transmitted by skin-to-skin contact, such as syphilis, herpes, HPV, and are ineffective in preventing pubic lice and scabies – Condoms from sheep’s membrane contain small pores that may permit passage of viruses (HIV, HSV, hepatitis) – Studies on couples where one partner is infected show that with consistent condom use, HIV infection rates for the uninfected partner are below 1% per year. • CDC recommends against using condoms containing nonoxynol-9 (N-9), which can cause genital lesions that create an entry point for HIV and other STI pathogens
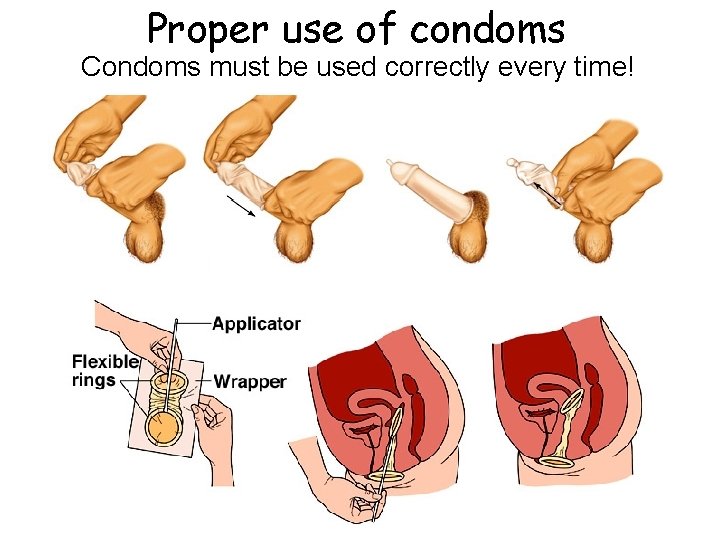
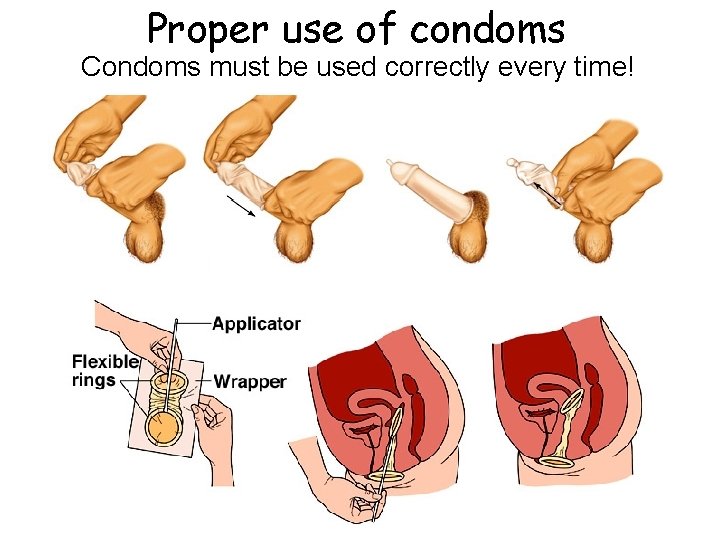
Proper use of condoms Condoms must be used correctly every time!
Proper use of condoms • Store condoms in a cool, dry place away from direct sunlight • Throw away condoms past expiration date or condoms in damaged packages • Put on a condom before any genital contact occurs • Be sure that the condom is adequately lubricated--if you add lube, use only water-based lube (oil-based lubes deteriorate latex) • Unroll condom directly onto erect penis; if penis is uncircumcised, pull back foreskin before putting on condom • After ejaculation, hold base of condom before withdrawal so condom does not slip off • Note: rates of condom slippage and breakage are higher during anal intercourse than vaginal intercourse, so be extra careful during anal penetration
 Chapter 25 sexually transmitted infections and hiv/aids
Chapter 25 sexually transmitted infections and hiv/aids Chapter 24 lesson 1 sexually transmitted diseases
Chapter 24 lesson 1 sexually transmitted diseases Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Sti std
Sti std Nursing management of reproductive tract infection
Nursing management of reproductive tract infection Sexually transmitted disease
Sexually transmitted disease Ngoại tâm thu thất chùm đôi
Ngoại tâm thu thất chùm đôi Premature atrial contraction
Premature atrial contraction Thể thơ truyền thống
Thể thơ truyền thống Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Walmart thất bại ở nhật
Walmart thất bại ở nhật Tìm vết của đường thẳng
Tìm vết của đường thẳng Con hãy đưa tay khi thấy người vấp ngã
Con hãy đưa tay khi thấy người vấp ngã Tôn thất thuyết là ai
Tôn thất thuyết là ai Gây tê cơ vuông thắt lưng
Gây tê cơ vuông thắt lưng Sau thất bại ở hồ điển triệt
Sau thất bại ở hồ điển triệt How do whales reproduce sexually
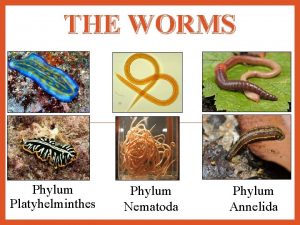
How do whales reproduce sexually Asexual reproduction in flatworms
Asexual reproduction in flatworms Parasitism phylum
Parasitism phylum What is sexually dimorphic mean
What is sexually dimorphic mean Rules of consent
Rules of consent Reproduction of protist
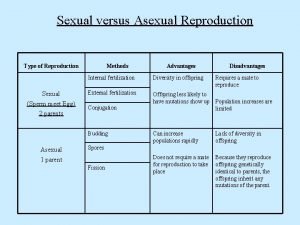
Reproduction of protist Sexual abuse quiz
Sexual abuse quiz Starfish aboral view
Starfish aboral view Chrysophta
Chrysophta Vasocongestion definition
Vasocongestion definition Annelids
Annelids Sexual harassment quiz
Sexual harassment quiz Sexual propagation
Sexual propagation Cnidaria class
Cnidaria class Radial symmetry
Radial symmetry Sexually frustrated meaning
Sexually frustrated meaning Body structure of porifera
Body structure of porifera How do birds mate
How do birds mate Sexual dimorphism
Sexual dimorphism Sexually dangerous persons act illinois
Sexually dangerous persons act illinois Opportunistic infections
Opportunistic infections Can methotrexate cause yeast infections
Can methotrexate cause yeast infections Opportunistic infections
Opportunistic infections Transmitted light examination in questioned document
Transmitted light examination in questioned document A song transmitted orally which tells a story
A song transmitted orally which tells a story Johnson and johnson botnet infections
Johnson and johnson botnet infections Storch infections
Storch infections Storch infections
Storch infections Bone and joint infections
Bone and joint infections In case of pivot bearing the rate of wear is
In case of pivot bearing the rate of wear is Neurosiphyllis
Neurosiphyllis Electronically transmitted postal ballot system
Electronically transmitted postal ballot system Bacterial vaginosis
Bacterial vaginosis Postpartum infections
Postpartum infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Genital infections
Genital infections Amber blumling
Amber blumling The totality of learned socially transmitted behavior
The totality of learned socially transmitted behavior Salmonella life cycle
Salmonella life cycle Classification of acute gingival infections
Classification of acute gingival infections Red tent summary
Red tent summary Sparknotes great gatsby chapter 8
Sparknotes great gatsby chapter 8 Chapter 10 chemical reactions
Chapter 10 chemical reactions Chapter 11 stoichiometry test
Chapter 11 stoichiometry test