Chapter 10 Toddler and Preschooler Nutrition Through the




- Slides: 59
Chapter 10 Toddler and Preschooler Nutrition Through the Life Cycle Judith E. Brown
Definitions of the Life Cycle Stage • Toddlers— 1 -3 years – Characterized by rapid increase in gross & fine motor skills • Preschool-age children— 3 -5 years – Characterized by increasing autonomy, broader social circumstances, increasing language skills, & expanding self-control
Importance of Nutrition Status • During toddler and preschool years, adequate nutrition is required to achieve full growth & development • Undernutrition impairs cognition & ability to explore environment
Tracking Toddler and Preschooler Health • Economic & nutrition status of U. S. children – 18% live in poverty (2006) – 14% have no health insurance – 33% lived in single-parent families (make them more likely to live in poverty)
Healthy People 2010 • Healthy People 2010 – objectives for the nation for improvements in health status by the year 2010 • Healthy People 2020 is under development (www. hhs. gov) • Table 10. 1 lists the objectives for toddlers and preschoolers with results to date
Normal Growth and Development • From birth to 1 year, average infant triples his birthweight • Toddlers gain 8 oz and grow 0. 4 in per month • Preschoolers gain 4. 4 lb and grow 2. 75 in per year
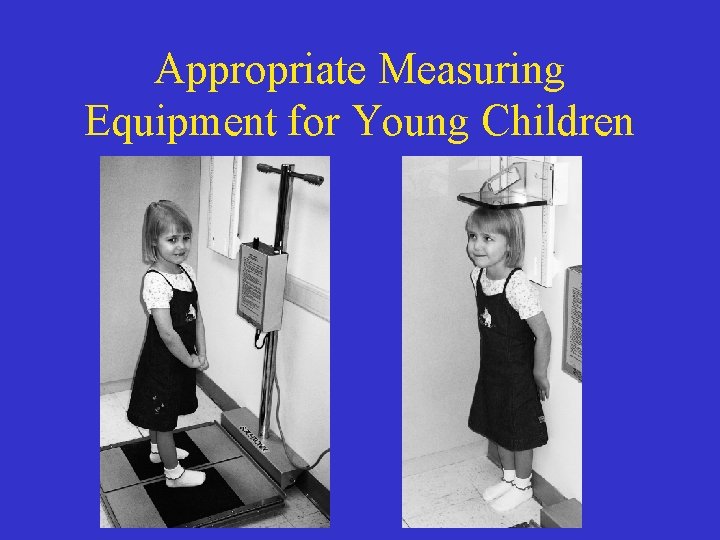
Monitoring Children’s Growth • Use calibrated scales & height board • Toddlers under age 2 years – Weighed without clothes or diaper – Determine recumbent length • Children over age 2 years – Weighed with light clothing – Measure stature with no shoes
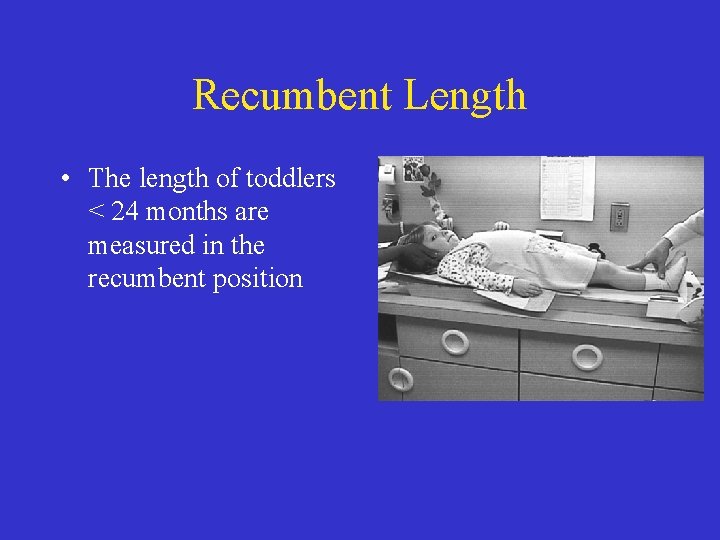
Recumbent Length • The length of toddlers < 24 months are measured in the recumbent position
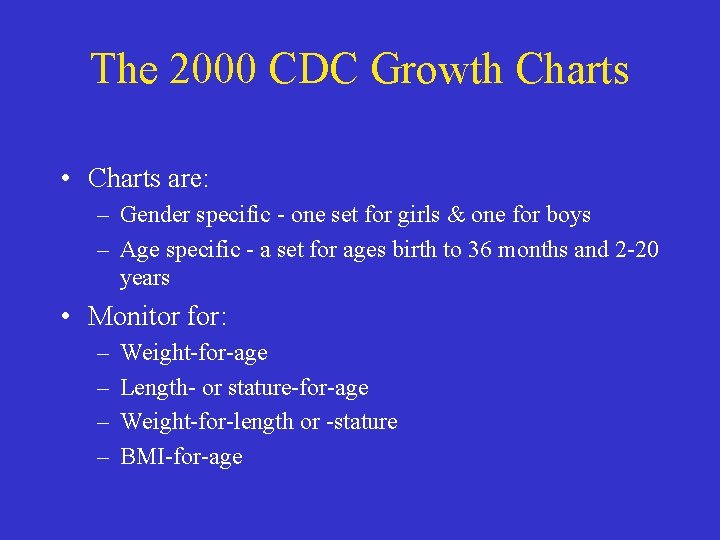
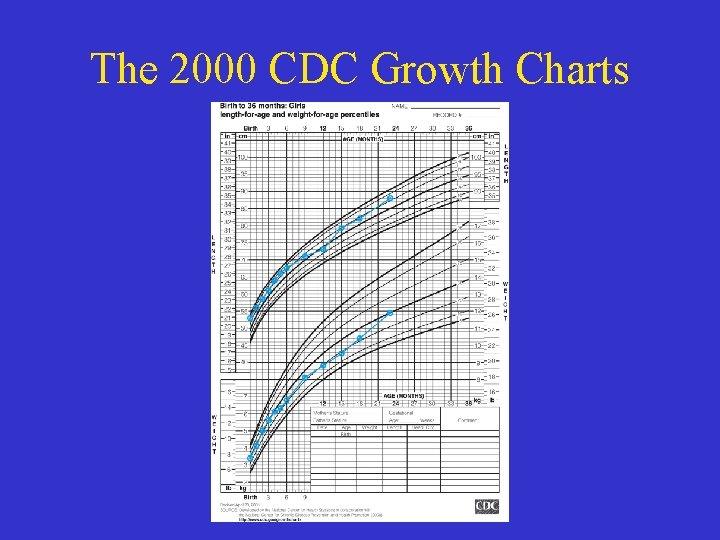
The 2000 CDC Growth Charts • Charts are: – Gender specific - one set for girls & one for boys – Age specific - a set for ages birth to 36 months and 2 -20 years • Monitor for: – – Weight-for-age Length- or stature-for-age Weight-for-length or -stature BMI-for-age
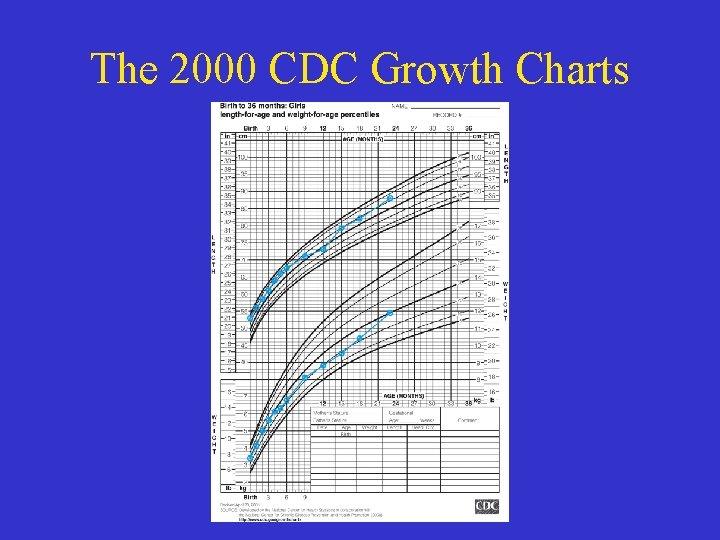
The 2000 CDC Growth Charts
WHO Growth Standards • WHO (World Health Organization) published growth standards for children from birth to 5 years. • International growth standards regardless of ethnicity or socioeconomic status. • See the “Resources” section at the end of the chapter or www. who. int/childgrowth
Common Problems with Measuring & Plotting Growth Data • Error in measuring may result in errors in health status assessment • Use of calibrated equipment and plotting accuracy are vital
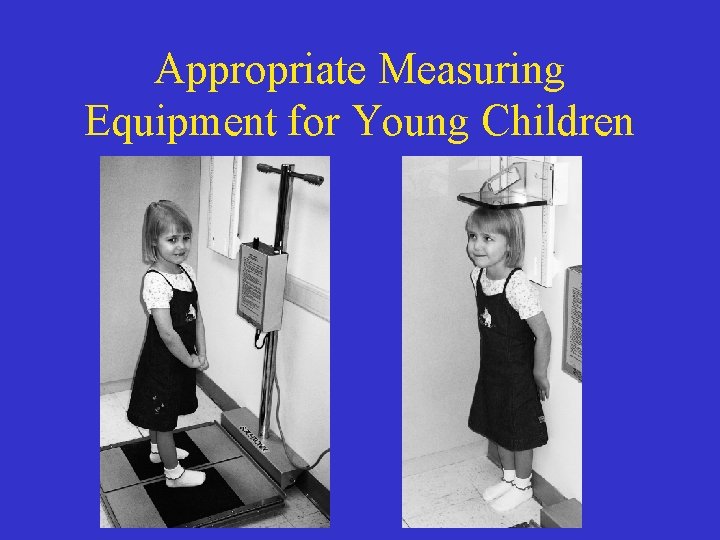
Appropriate Measuring Equipment for Young Children
Physiological and Cognitive Development: Toddlers • A time of expanding physical and developmental skills • Walking begins as a “toddle, ” improving in balance & agility • Progress by month – – – 15—crawl upstairs 18—run stiffly 24—walk up stairs one foot at a time 30—alternate feet going up stairs 36—ride a a tricycle
Cognitive Development of Toddlers • Toddlers “orbit” around parents • Transitions from self-centered to more interactive • Vocabulary expands: – 10 -15 words at 18 months – 100 at 2 years – 3 -word sentences by 3 years • Temper tantrums common (the terrible two’s)
Development of Feeding Skills of Toddlers • • • Gross & fine motor development improved 9 -10 months—weaning bottle begins 12 to 14 months—completely weaned 12 months—refined pincer 18 -24 months—able to use tongue to clean lips & has developed rotary chewing • Adult supervision vital to prevent choking

Feeding Behaviors of Toddlers • • Rituals in feeding are common May have strong preferences & dislikes Food jags common Serve new foods with familiar foods & when child is hungry • Toddlers imitate parents & older siblings
Appetite and Food Intake of Toddlers • Slowing growth results in decreased appetite • Toddler-sized portions average 1 tablespoon per year of age • Nutrient-dense snacks needed but avoid grazing on sugary foods that limit appetite for basic foods at meals

Cognitive Development of Preschool-Age Children • Egocentric—cannot accept another’s point of view • Learning to set limits for himself • Cooperative & organized group play • Vocabulary expands to >2000 words • Begins using complete sentences
Development of Feeding Skills of Preschool-Age Children • • Can use a fork, spoon, & cup Spills occur less frequently Foods should be cut into bite-size pieces Adult supervision still required
Feeding Behaviors of Preschool. Age Children • Appetite related to growth • Appetite increases prior to the “spurts” of growth • Include child in meal selection & preparation
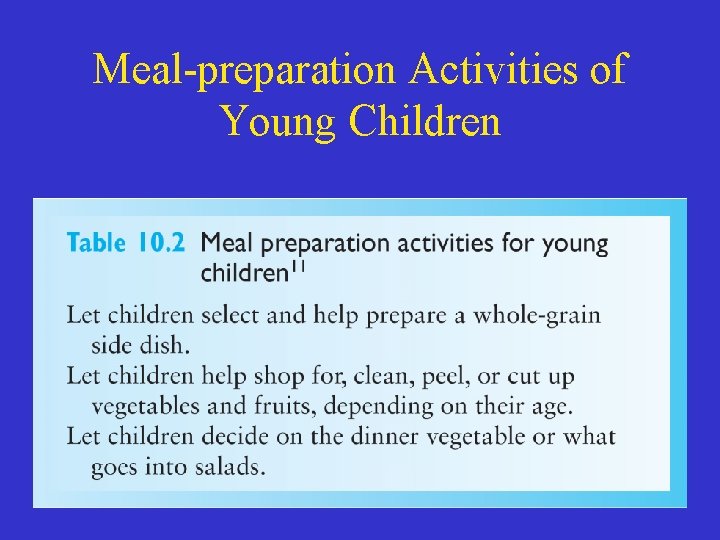
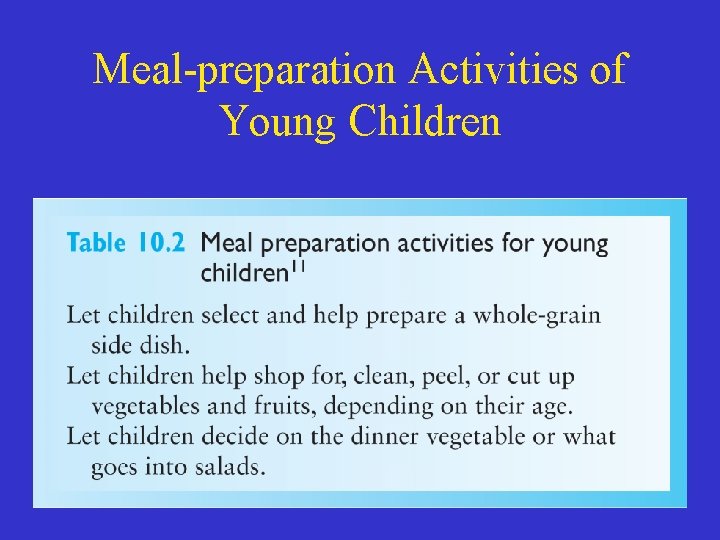
Meal-preparation Activities of Young Children
Innate Ability to Control Energy Intake & Preschool-Age Children • Children adjust caloric intake to meet caloric needs • Avoid encouraging child to “clean your plate” • Healthful eating habits must be learned
Appetite and Food Intake of Preschool-Age Children • • May prefer familiar foods Serve child-sized portions Make foods attractive Strong-flavored or spicy foods may not be accepted • Control amount eaten between meals to ensure appetite for basic foods
Temperament differences • Temperament—the behavioral style of the children. Three main temperaments: – 40% “easy” temperaments – 10% “difficult” temperaments – 15% “slow-to-warm-up” – Remaining styles are “intermediate low” to “intermediate high”
Temperament differences • “Easy”—adapts to regular schedules & accepts new foods • “Difficult”—slow to adapt and may be negative to new foods • “Slow-to-warm-up”—slow adaptability, negative to new foods but can learn to accept new foods • “Intermediate low” to “intermediate high” – a mixture of behaviors

Food Preference Development, Appetite, and Satiety • Prefer sweet & slightly salty, reject sour & bitter foods • Eat familiar foods • May need 8– 10 exposures to new foods before acceptance • Food intake related to parent’s preferences
Appetite and Satiety • Consumption of foods high in sugar and/or fat before meals decreases intake of basic foods • Offering large portions increases food intake and may promote obesity • Restriction of palatable foods increases preference for the foods
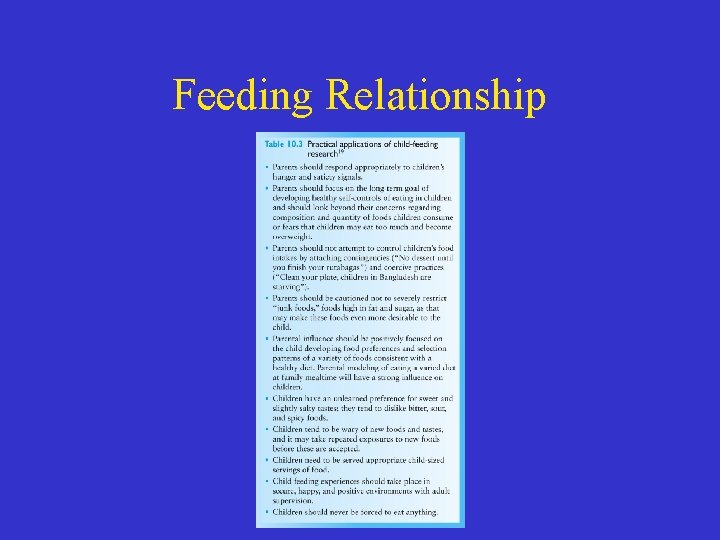
Feeding Relationship • Parent or caretaker responsibilities: – “What” children are offered to eat – The environment in which food is served including “when” & “where” foods are offered • Child’s responsibilities: – “How much” they eat – “Whether” they eat a particular meal or snack
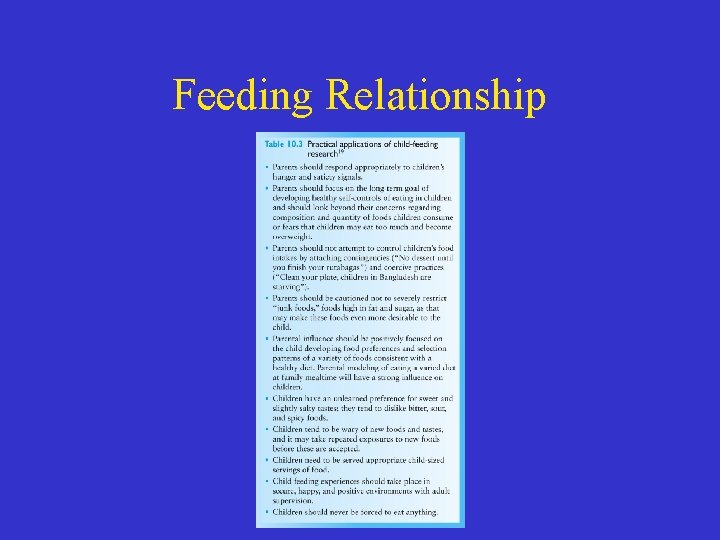
Feeding Relationship
Energy Needs • Dietary Reference Intakes (DRIs) have been developed • The reports present a comprehensive set of reference values for nutrient intakes of healthy individuals • Table 10. 4 gives the Estimated Energy Requirements for reference boys and girls
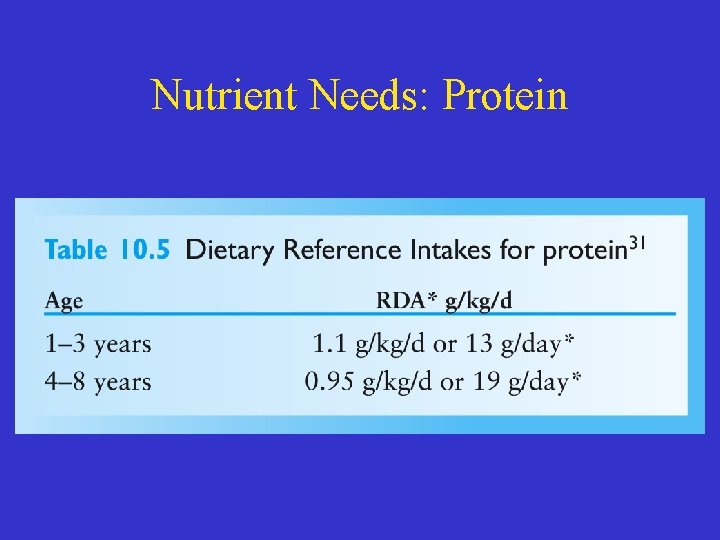
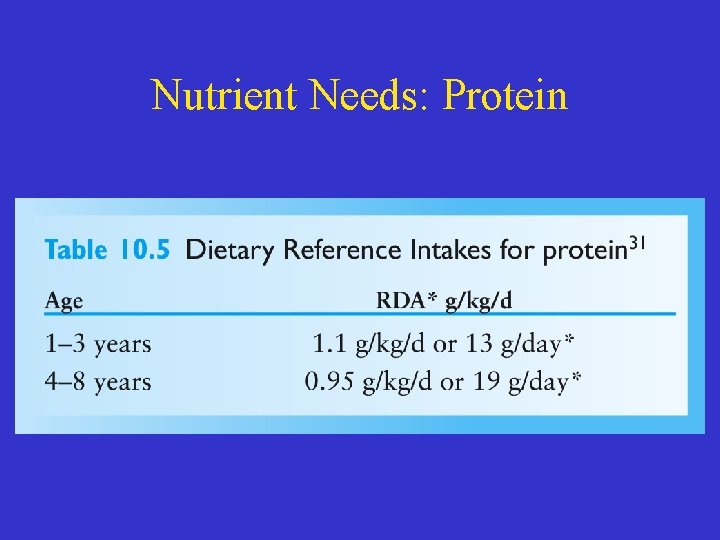
Nutrient Needs: Protein
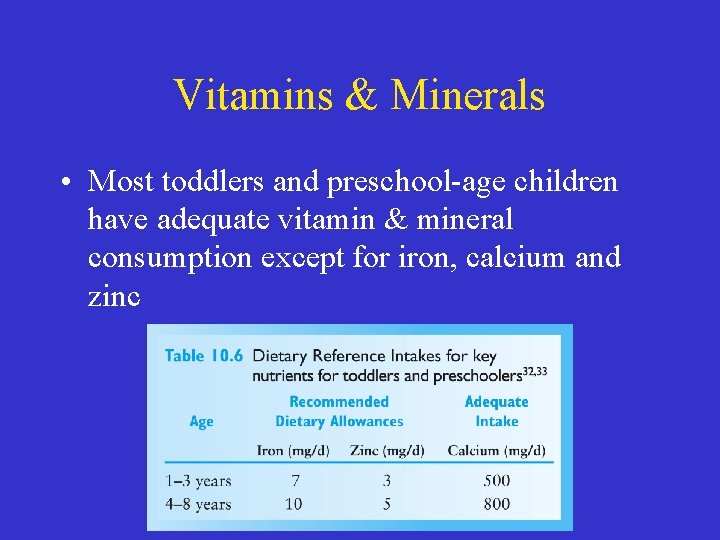
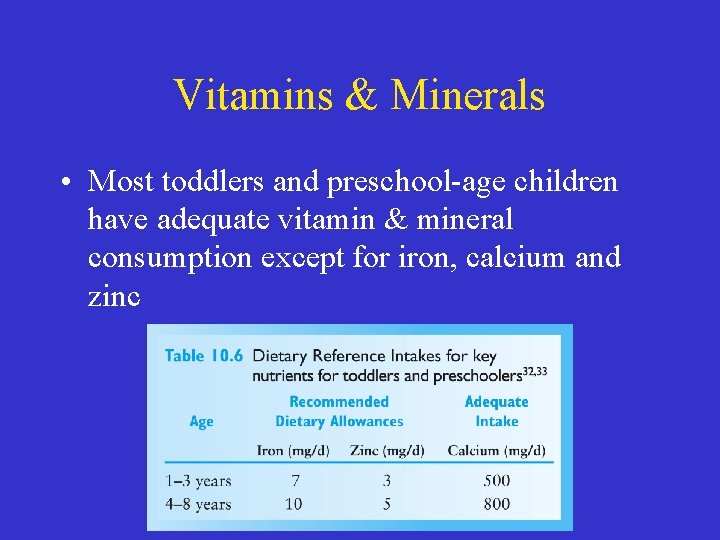
Vitamins & Minerals • Most toddlers and preschool-age children have adequate vitamin & mineral consumption except for iron, calcium and zinc
Common Nutrition Problems • • • Iron-deficiency anemia Dental caries Constipation Lead poisoning Food security Food safety
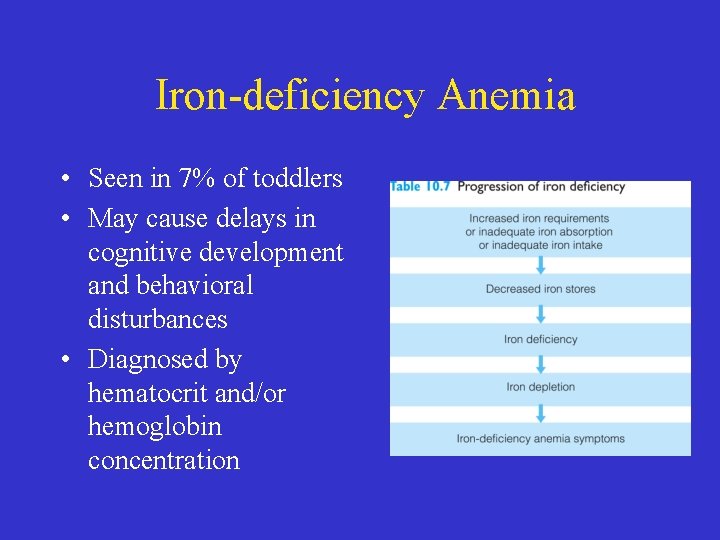
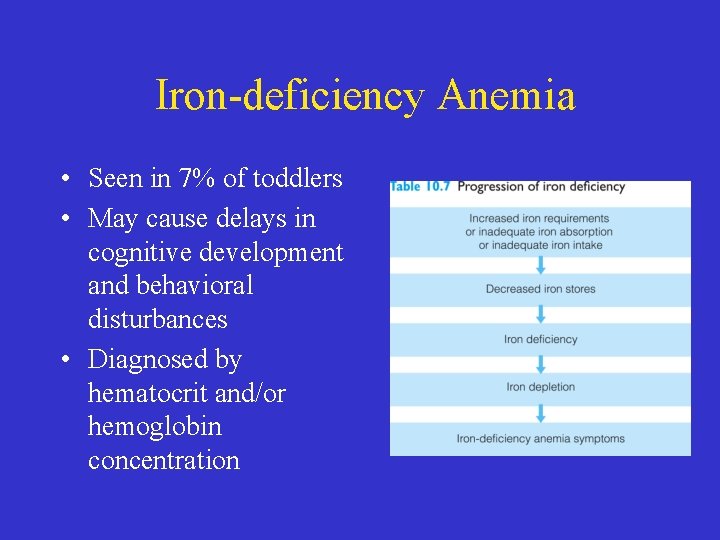
Iron-deficiency Anemia • Seen in 7% of toddlers • May cause delays in cognitive development and behavioral disturbances • Diagnosed by hematocrit and/or hemoglobin concentration
Iron-deficiency Anemia • Preventing Iron Deficiency: – Nutrition-Limit milk consumption to 24 oz/d since milk is a poor source of iron – Infants at risk should be tested at 9 to 12 months, 6 months later, and annually from ages 2 to 5 • Intervention for Iron Deficiency – Iron supplements – Counseling with parents – Repeat screening
Dental Caries • Prevalence: – 1 in 5 children ages 2 to 4 • Causes: – Bedtime bottle with juice or milk – Streptococcus mutans – Sticky carbohydrate foods • Prevention: – Fluoride—supplemental amounts vary by age & fluoride content of water supply
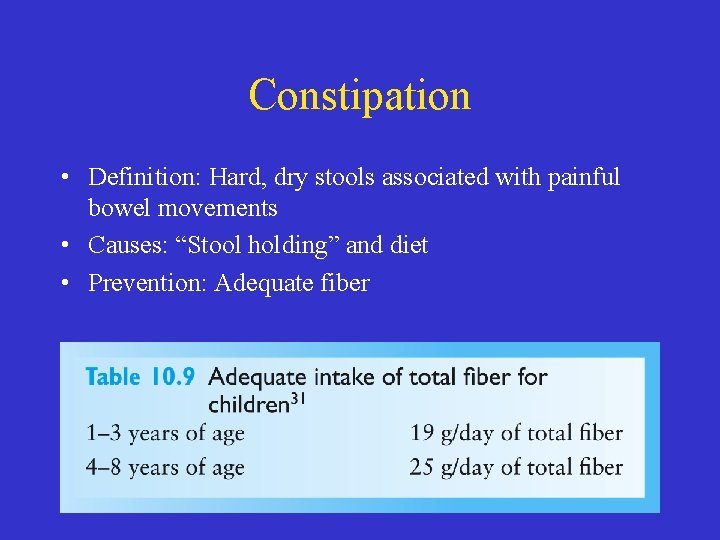
Constipation • Definition: Hard, dry stools associated with painful bowel movements • Causes: “Stool holding” and diet • Prevention: Adequate fiber
Lead Poisoning • Seen in ~2. 2% of children ages 1 -5 • Low levels of lead exposure linked to lower IQ & behavioral problems • High blood lead levels may decrease growth • Reduce lead poisoning by eliminating sources of lead
Food Security • Defined as access at all times to sufficient supply of safe, nutritious foods • Insecurity more common in minority populations • A concern for growing children since food insecurity may hinder growth & development
Food Safety • Young children vulnerable to food poisoning • Food safety practices by Fight. BAC: – Clean: wash hands & surfaces often – Separate: don’t cross-contaminate – Cook: cook to proper temperature – Chill: refrigerate promptly
Prevention of Nutrition-Related Disorders • Overweight and obesity • Prevention and treatment of overweight and obesity • Nutrition and prevention of cardiovascular disease • Vitamin and mineral supplements • Herbal supplements
Overweight and Obesity • Of children ages 2 -5: – 10. 4% are overweight (BMI/age ≥ 95%) – 20. 6% are at risk for becoming overweight (BMI/age ≥ 85%-95%) • BMI is lowest from ages 4 -6 years • Adiposity rebound—normal increase in BMI that occurs after BMI declines • Best treatment is allowing child to “grow into his or height”

Prevention of Overweight & Obesity • Limit sugar-sweet beverages • Encourage fruits & vegetables • Limit TV • Daily breakfast • Limit fast foods • Limit portions • Calcium rich diets • Diets high in fiber • Follow the DRI for carbs, pro & fat • Promote physical activity • Limit energy-dense foods
Nutrition and Prevention of Cardiovascular Disease • Limit dietary saturated fats, trans fat & cholesterol • Acceptable total fat intake ranges: – 2 to 3 years— 30 to 35% of calories – 4 to 18 years— 25 to 35% of calories • For children at high risk of CVD limit saturated fat to < 7% of calories & cholesterol to < 200 mg
Vitamin and Mineral Supplements • A varied diet provides all vitamins & minerals needed • AAP recommends supplements for certain groups of children: – From deprived families – With anorexia, poor appetites or poor diets, or a dietary program for wt mgmt – Who consume only a few types of foods – Vegetarians without dairy products
Herbal Supplements • Parents who take herbs are likely to give them to their children • Advise parents of potential risks of herbal therapies & the need to closely monitor the child if given supplements
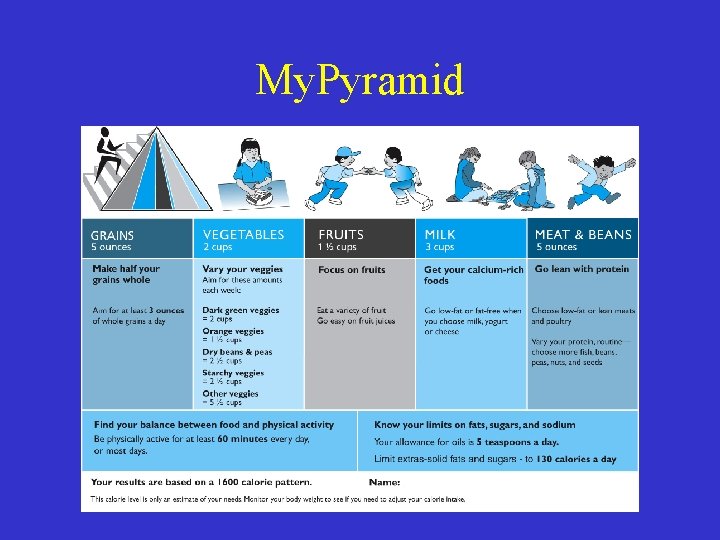
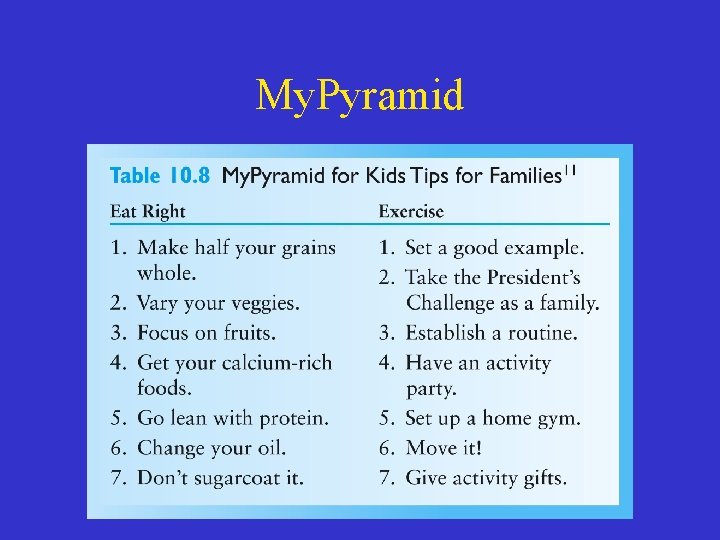
Dietary and Physical Activity Recommendations • Dietary guidelines – Offer a variety of foods, limiting foods high in fat & sugar – 60 minutes of vigorous physical activity each day • My. Pyramid developed by the USDA for young children
My. Pyramid
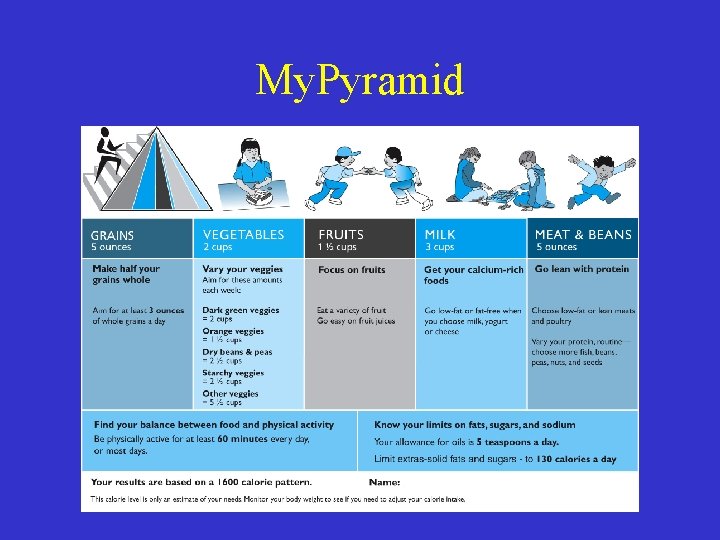
My. Pyramid
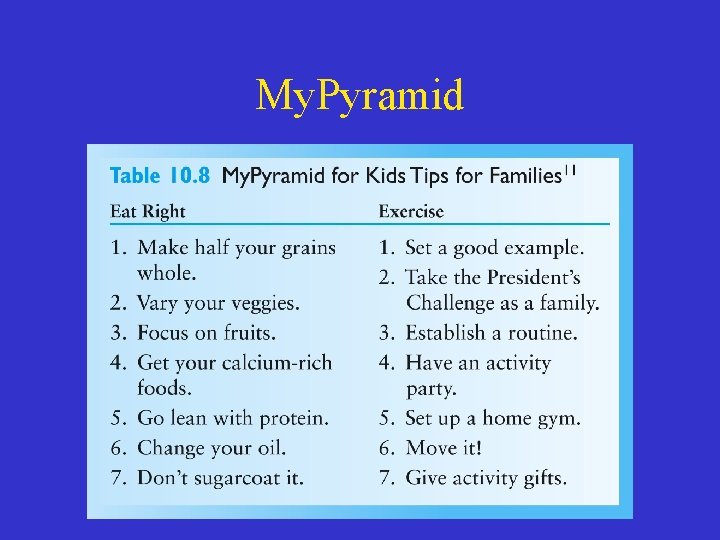
My. Pyramid
Recommendations for Intake • Iron- meats, fortified cereal, dried beans and peas • Fiber- fruits, vegetables, whole grains • Fat- follow food guide pyramid • Calcium- dairy, canned fish with soft bones, green leafy vegetables, calcium-fortified beverages • Fluids- beverages, foods and sips of water
Recommended vs. Actual Food Intake • Dietary intake of children ages 2 -5 – Energy exceeded by 31% – Consistently low “mean” intakes of zinc, folic acid, Vit D and Vit E – Total fat is 31% of calories – Sodium intake is 2150 -2400 mg (rec 2300 mg) – Table 10. 10 shows the mean % of calories
Other Concerns • Cross-cultural considerations – Build on cultural practices • Reinforce positive practices • Attempt change for more benefit • Vegetarian diets – Vegan and macrobiotic diet children tend to have lower growth rates but remain within normal ranges
Other Concerns • Vegetarian diet guidelines – Several meals / day (3 meals, 2 -3 snacks) – Avoid excessive bulky foods (i. e. bran) – Include energy dense foods (cheese / avocado) – Fat-30% with omega-3 fatty acids – Sources of Vitamin B 12, Vitamin D and Calcium should be included or supplemented
Other Concerns • Child-care nutrition standards – Nearly half of preschool-age children attend a child care program – Standards for child care vary by state – Offer food at intervals not less than 2 hours & no more 3 hours
Other Concerns • Physical activity recommendations – Children need at least 60 minutes of play activity each day – Suggested activities • • Taking a nature walk Riding a tricycle or bicycle Walking, skipping, running Most important—have fun while being active!
Nutrition Intervention for Risk Reduction • Model program – Bright Futures in Practice: Nutrition • Public food and nutrition programs – WIC’s Farmers’ Market Nutrition Program – Head Start and Early Head Start – Supplemental Nutrition Assistance Program (formerly Food Stamps)
 Brigance screens
Brigance screens Banajee list of toddler vocabulary
Banajee list of toddler vocabulary Antibiotics for uti in toddler
Antibiotics for uti in toddler Drdp modified essential view
Drdp modified essential view Toddler dönemi nedir
Toddler dönemi nedir Site:slidetodoc.com
Site:slidetodoc.com Infant/toddler sensory profile score sheet
Infant/toddler sensory profile score sheet Fever in toddler
Fever in toddler Malaguzzi quotes
Malaguzzi quotes Tangental sawing
Tangental sawing The embryo gets nutrition from mother through
The embryo gets nutrition from mother through Nutrition through life cycle
Nutrition through life cycle Through one man sin entered
Through one man sin entered Tarnow fletcher furcation classification
Tarnow fletcher furcation classification Night of the scorpion story
Night of the scorpion story Kelsey carbonetta
Kelsey carbonetta Fitness chapter 7
Fitness chapter 7 A saturated fatty acid holds all the hydrogen atoms it can.
A saturated fatty acid holds all the hydrogen atoms it can. Chapter 4 nutrition and your personal fitness
Chapter 4 nutrition and your personal fitness Chapter 11 nutrition and diets
Chapter 11 nutrition and diets Chapter 11 nutrition and diets
Chapter 11 nutrition and diets Chapter 10 lesson 4 nutrition labels and food safety
Chapter 10 lesson 4 nutrition labels and food safety Chapter 10 lesson 4 nutrition labels and food safety
Chapter 10 lesson 4 nutrition labels and food safety Nutrition and hydration chapter 15
Nutrition and hydration chapter 15 Chapter 6 microbial nutrition and growth
Chapter 6 microbial nutrition and growth Skin structure growth and nutrition
Skin structure growth and nutrition Chapter 6 microbial nutrition and growth
Chapter 6 microbial nutrition and growth Chapter 11 nutrition and diet
Chapter 11 nutrition and diet Seven fitness nutrition
Seven fitness nutrition Streak plate method
Streak plate method Chapter 55 nutrition and health
Chapter 55 nutrition and health Chapter 15 maternal and fetal nutrition
Chapter 15 maternal and fetal nutrition Chapter 8 nutrition and hydration
Chapter 8 nutrition and hydration Chapter 8 food and nutrition
Chapter 8 food and nutrition Optimal nutritional status definition
Optimal nutritional status definition Soap nutrition
Soap nutrition Chapter 15 digestion and nutrition
Chapter 15 digestion and nutrition Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Ng-html
Ng-html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Tư thế worms-breton
Tư thế worms-breton Chúa yêu trần thế alleluia
Chúa yêu trần thế alleluia Môn thể thao bắt đầu bằng từ chạy
Môn thể thao bắt đầu bằng từ chạy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Cong thức tính động năng
Cong thức tính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Phép trừ bù
Phép trừ bù Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng xinh xinh thế chỉ nói điều hay thôi
Cái miệng xinh xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ