Illness Nutrition Care Chapter 14 Nutrition Diet Therapy






- Slides: 29
Illness & Nutrition Care Chapter 14 Nutrition & Diet Therapy (7 th Edition)
Nutrition in Health Care Nutrition & Diet Therapy (7 th Edition)
Effects of Illness on Nutrition Status • Relationship between nutrition & illness is complex – Medical problems can alter nutrient needs & result in malnutrition • • Reduction in food intake Interference with digestion & absorption Alteration of nutrient metabolism & excretion Increase metabolic stress & energy needs – Poor nutrition can affect course of disease & body’s response to treatment • Dietary changes required for acute illness usually temporary; chronic illnesses may require longterm dietary modification Nutrition & Diet Therapy (7 th Edition)
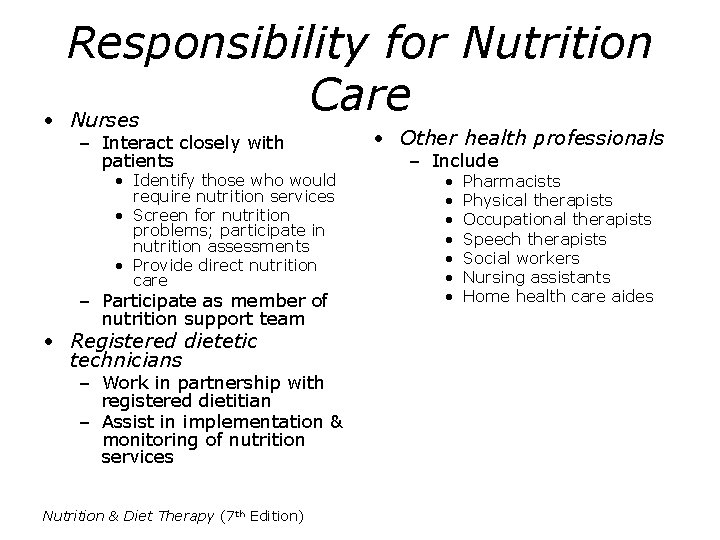
Responsibility for Nutrition Care • Physician—prescribes diet orders & other aspects of nutrition care – Critical pathways outline • Nurses, registered coordinated, dieticians, other health comprehensive plan for professionals identify specific diagnoses, treatments, procedures problems, suggest strategies, provide – Implementation requires all members of nutritional services • Cooperative effort of multidisciplinary health care team – Roles of team members often overlap Nutrition & Diet Therapy (7 th Edition)
Responsibility for Nutrition Care • Registered dietitian (RD) – Food & nutrition expert – Role includes • Conduct nutrition assessment • Diagnose nutritional problems • Develop, implement & evaluate nutrition care plans • Plan & approve menus • Provide nutrition education • May manage food services in health care institution Nutrition & Diet Therapy (7 th Edition) • Registered dietitian has academic & professional requirements to qualify for RD credential conferred by American Dietetic Association • Qualifications include – Bachelor’s degree in nutrition or dietetics – Supervised internship – Successful completion of national examination
Responsibility for Nutrition Care • Nurses – Interact closely with patients • Identify those who would require nutrition services • Screen for nutrition problems; participate in nutrition assessments • Provide direct nutrition care – Participate as member of nutrition support team • Registered dietetic technicians – Work in partnership with registered dietitian – Assist in implementation & monitoring of nutrition services Nutrition & Diet Therapy (7 th Edition) • Other health professionals – Include • • Pharmacists Physical therapists Occupational therapists Speech therapists Social workers Nursing assistants Home health care aides
Nutrition Screening • Assessment tool that helps to identify malnourished patients, or those at risk • Information includes – Admitting diagnosis – Information on medical record – Physical measurements & lab test results – Responses of patient or caregiver during initial interview or assessment Nutrition & Diet Therapy (7 th Edition)
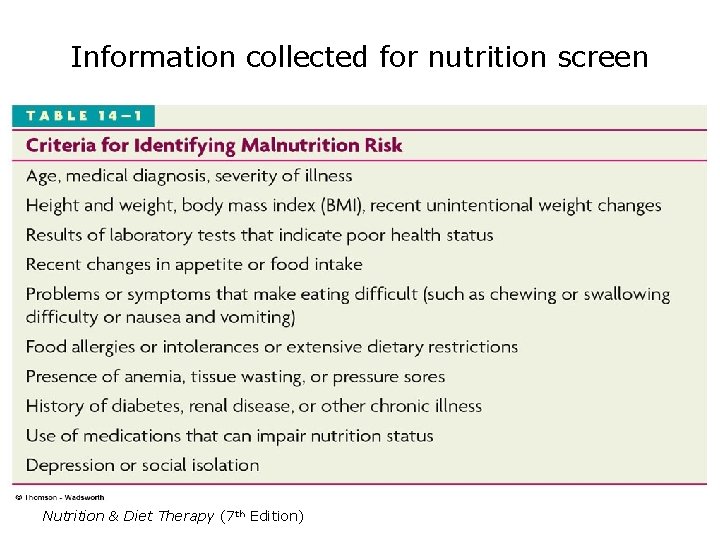
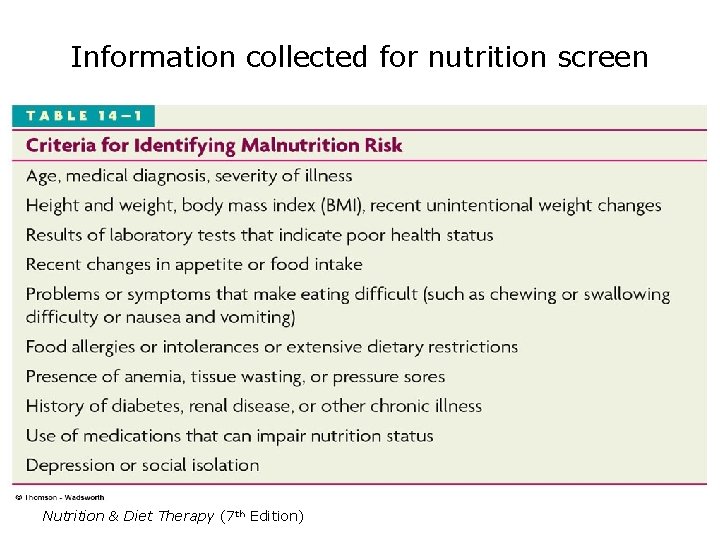
Information collected for nutrition screen Nutrition & Diet Therapy (7 th Edition)
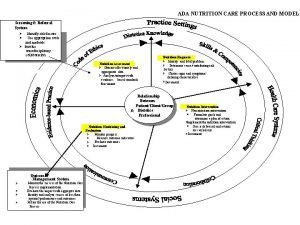
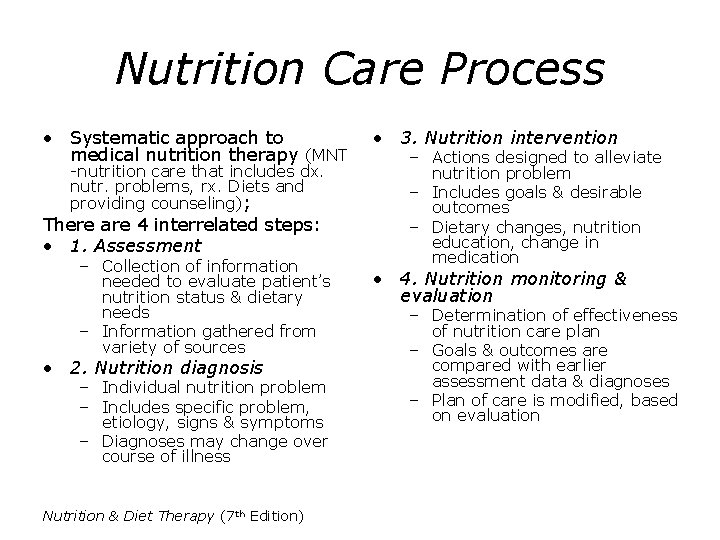
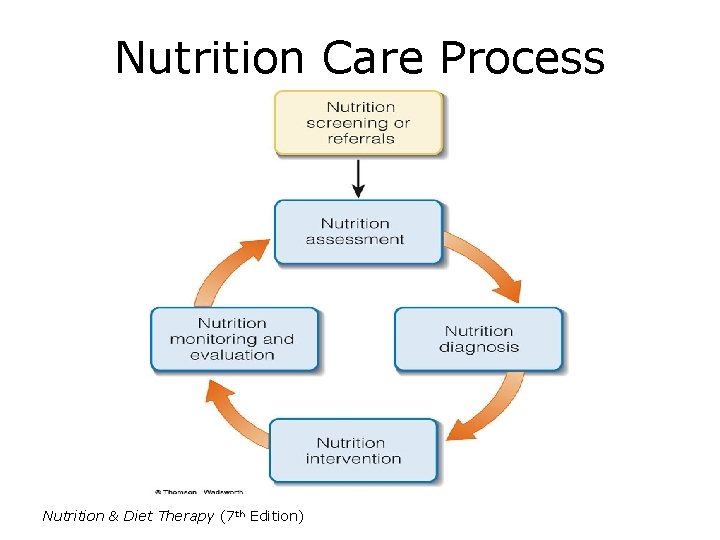
Nutrition Care Process • Systematic approach to medical nutrition therapy (MNT -nutrition care that includes dx. nutr. problems, rx. Diets and providing counseling); There are 4 interrelated steps: • 1. Assessment – Collection of information needed to evaluate patient’s nutrition status & dietary needs – Information gathered from variety of sources • 2. Nutrition diagnosis – Individual nutrition problem – Includes specific problem, etiology, signs & symptoms – Diagnoses may change over course of illness Nutrition & Diet Therapy (7 th Edition) • 3. Nutrition intervention – Actions designed to alleviate nutrition problem – Includes goals & desirable outcomes – Dietary changes, nutrition education, change in medication • 4. Nutrition monitoring & evaluation – Determination of effectiveness of nutrition care plan – Goals & outcomes are compared with earlier assessment data & diagnoses – Plan of care is modified, based on evaluation
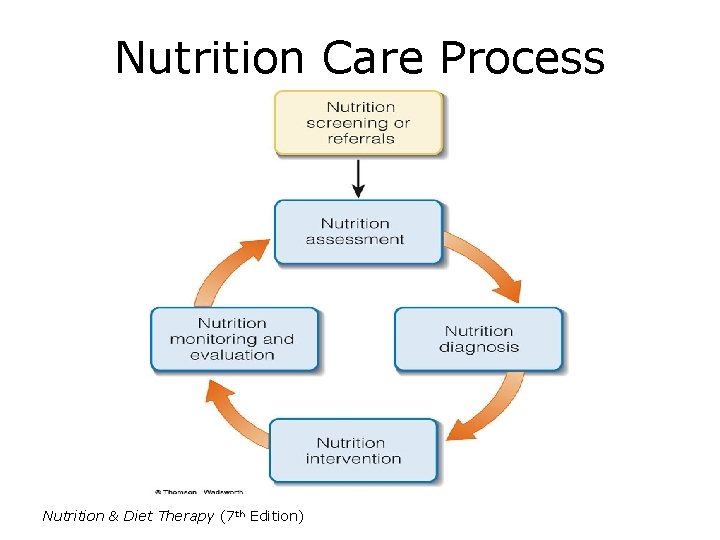
Nutrition Care Process Nutrition & Diet Therapy (7 th Edition)

Nutrition Assessment Nutrition & Diet Therapy (7 th Edition)

Historical Information • Information about patient’s nutrition status & nutrient needs • Identifies personal preferences that need to be considered in nutrition care plan • Information gathered from patient or caregiver, or from medical record • Includes – Medical history – Social history – Diet history Nutrition & Diet Therapy (7 th Edition)

Nutrition & Diet Therapy (7 th Edition)
Food Intake Data • Use of combination of methods to obtain information regarding food intake – 24 -hour recall: detailed description of foods & beverages consumed in a 24 -hour period are outlined; may reflect typical day – Food frequency questionnaire: written survey of food consumption during specific period of time, including those relevant to patient’s medical condition – Food record: written account of food consumed during specified period; usually over several consecutive days – Direct observation: observation of meal trays or shelf inventories; used to conduct kcalorie counts Nutrition & Diet Therapy (7 th Edition)

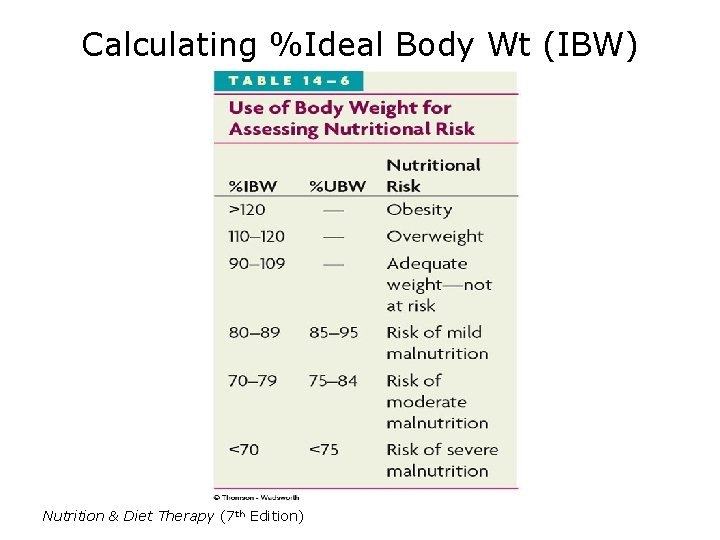
Anthropometric Data • Measures of body size that can reveal problems related to overnutrition & protein-energy malnutrition – Height (or length) & weight; BMI – Percentage of body fat – Circumferences of head (in children), waist & limbs • Anthropometric assessment in infants & children – Used to evaluate growth patterns – Usually plotted on growth charts – Growth patterns below 5 th percentile may be cause for concern Nutrition & Diet Therapy (7 th Edition) • Anthropometric assessment in adults – Routinely measured during illness – Changes must be evaluated carefully • Unintentional weight loss may indicate malnutrition • Weight gain may result from fluid retention • In assessing significance of change, must consider rate as well as amount – Including skin fold measurements & limb circumference can help identify changes in body composition that need to be addressed in treatment plan
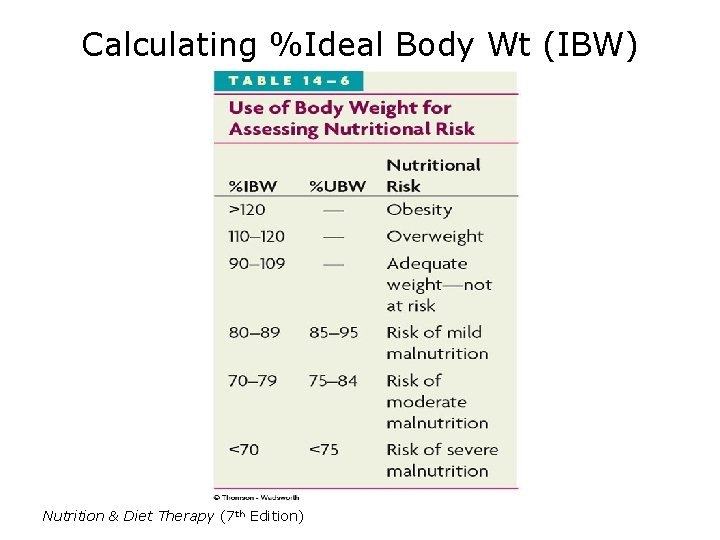
Calculating %Ideal Body Wt (IBW) Nutrition & Diet Therapy (7 th Edition)
Biochemical Analyses (Labs) • Provide information about PEM, vitamin & mineral status, fluid & electrolyte balance, organ function • Include analysis of blood & urine samples • Different factors can influence test results, making interpretation difficult • Variety of tests usually required to diagnose nutrition problems Nutrition & Diet Therapy (7 th Edition)

Biochemical Analyses • Plasma proteins – Help in assessment of protein status – May fluctuate for other reasons – Values must be considered with other data – Tests include • • Total protein Albumin Transferrin Prealbumin & retinolbinding protein Nutrition & Diet Therapy (7 th Edition) • Other routine tests with nutritional implications – Hematology (RBC, Hb, Hct) – Chemistry (Alb) – Serum enzymes (Ck, AST, ALT) – Serum electrolytes (Na, K) – Glucose (glu, Hb. A 1 C) – Blood urea nitrogen (BUN) and Creatinine (Cr)
Physical Examination • Most physical signs of malnutrition are nonspecific—can reflect many causes – Nutrient deficiencies – Fluid imbalances – Functional impairments related to nutritional problems • Clinical signs of deficiencies may be reflected in – Skin, hair & nails – Eyes – Lips, mouth & gums Nutrition & Diet Therapy (7 th Edition) • Physical signs of malnutrition are often evident in parts of the body where cells are replaced at a rapid rate
Implementing Nutrition Care Nutrition & Diet Therapy (7 th Edition)
Dietary Modifications • Energy & nutrient needs are met by standard (regular)diet; modified diet is prescribed when different texture is needed or when certain foods need to be eliminated because of a condition. • Diets altered by – 1. Changing consistency & texture of foods: used for patients with chewing or swallowing impairments • Mechanically altered • Blenderized liquid • Clear liquid – 2. Altering nutrient content: may relieve symptoms of disease, preventing or reversing malnutrition • Fat-restricted • Fiber-restricted • High-kcalorie, high-protein • Need to be adjusted to satisfy individual preferences & tolerances Nutrition & Diet Therapy (7 th Edition)
Dietary Modifications • Diet manuals – Include detail of specific foods to include or exclude in modified diet – May be compiled from resources from American Dietetic Association • Alternative feeding routes – Used in situations where nutrient needs are high, patient appetite is poor, or patient is unable to meet nutrient needs orally • Tube feedings: delivery of nutritionally-complete formulas through tube placed into stomach or intestine or nasogastric (temp) • Intravenous feedings: delivery of nutrients via the vascular system; may be used when patient’s condition prohibits use of GI tract to deliver nutrients (PPN, TPN) Nutrition & Diet Therapy (7 th Edition) • Diet order – Physician has primary responsibility for prescribing appropriate diet – Orders must be precise to avoid confusion (2 g. Na instead of “low sodium”) – Often done in consultation with dietitian or nurse • Nothing by mouth (NPO) – Restriction of any food, beverages, medications by mouth – Commonly used during acute illness or diagnostic tests involving GI tract
Determining Energy Requirements • Energy needs affected by patient's – – – Health problem Treatments Current nutrition status Activity level Gender, height, weight, and age – – Fever Mechanical ventilation Restlessness (psychiatric) Presence of open wounds • Several methods can be used to calculate energy requirements • Calculation based on medical problem, activity level & stress level • In critical patients, needs increased further due to • Energy needs for critical care patients usually range 25 -30 kcalories per kg body weight daily—often exceeding 2000 kcalories Nutrition & Diet Therapy (7 th Edition)

Approaches to Nutrition Care • Nutrition care plan often involves dietary modifications & nutrition education • Plan should be compatible with desires & abilities of the patient • Long-term dietary intervention—must take into account current food habits, lifestyle & degree of motivation – Determine individual’s readiness to change – Emphasize what to eat, rather than what not to eat – Suggest only one or two changes at a time Nutrition & Diet Therapy (7 th Edition) • Dietary counseling requires sensitivity to cultural orientation, educational background, & motivation for change
Approaches to Nutrition Care • Nutrition education – Allows patients to learn about dietary factors that affect their medical condition – Should be tailored to patient’s age, level of literacy, cultural background – Learning style should be considered • • Discussion, supplemented with written materials Visual examples One-on-one or group sessions Follow-up sessions to assess learning – Other tools • Sample menus • Diet analysis software • Informational packages Nutrition & Diet Therapy (7 th Edition)
Documenting Nutrition Care • All nutrition care is described in medical record • SOAP note – Subjective information obtained in interview with patient or family; includes main symptoms & complaints – Objective information available from nutrition screening or assessment data; includes biochemical analyses, anthropometric tests, physical exams – Assessment includes brief evaluation of subjective & objective data; includes diagnosis of nutrition problem – Plan describes recommendations, dietary prescriptions, special equipment, nutrition education, referrals Nutrition & Diet Therapy (7 th Edition)
Improving Food Intake • Loss of appetite common among patients in hospitals or other medical care facilities – Result of medical condition, treatment, emotional distress – Can be affected by medications & other treatments that alter taste perceptions • Nurses & dietetic technicians have central role in helping patients to eat Nutrition & Diet Therapy (7 th Edition) • • • Helping patients to eat Empathize with patient Motivate patient Help patient select foods he likes & mark menus appropriately Suggest foods that require little effort to eat Help patient prepare for meal Check patient’s tray to confirm correct diet & food selections Help with eating (open milk container, etc) Try to solve eating problems Take a positive attitude toward hospital foods
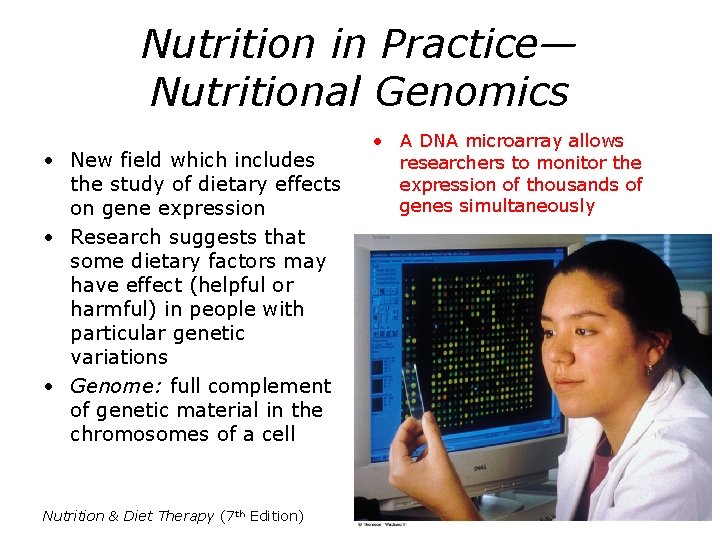
Nutrition in Practice— Nutritional Genomics • New field which includes the study of dietary effects on gene expression • Research suggests that some dietary factors may have effect (helpful or harmful) in people with particular genetic variations • Genome: full complement of genetic material in the chromosomes of a cell Nutrition & Diet Therapy (7 th Edition) • A DNA microarray allows researchers to monitor the expression of thousands of genes simultaneously
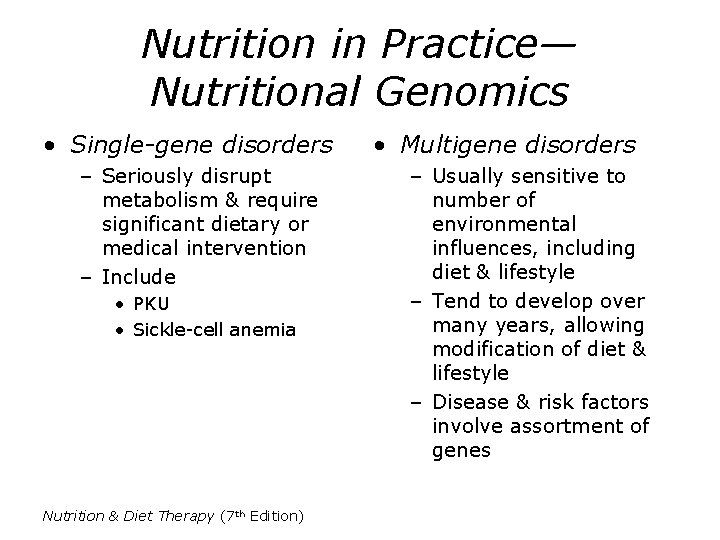
Nutrition in Practice— Nutritional Genomics • Single-gene disorders – Seriously disrupt metabolism & require significant dietary or medical intervention – Include • PKU • Sickle-cell anemia Nutrition & Diet Therapy (7 th Edition) • Multigene disorders – Usually sensitive to number of environmental influences, including diet & lifestyle – Tend to develop over many years, allowing modification of diet & lifestyle – Disease & risk factors involve assortment of genes
 Nutrition and diet therapy nursing
Nutrition and diet therapy nursing Chapter 11 nutrition and diet
Chapter 11 nutrition and diet Chapter 11 nutrition and diet
Chapter 11 nutrition and diet Dash diet vs mediterranean diet
Dash diet vs mediterranean diet Improving chronic illness care model
Improving chronic illness care model Levels of care primary secondary tertiary quaternary
Levels of care primary secondary tertiary quaternary Both psychoanalysis and humanistic therapy stress
Both psychoanalysis and humanistic therapy stress Bioness bits cost
Bioness bits cost Humanistic therapies aim to boost
Humanistic therapies aim to boost Soap nutrition
Soap nutrition Medical nutrition therapy for stroke
Medical nutrition therapy for stroke Medical nutrition therapy for hypertension
Medical nutrition therapy for hypertension Related image
Related image Chapter 20 mental health and mental illness
Chapter 20 mental health and mental illness Chapter 17 1 providing first aid
Chapter 17 1 providing first aid Unit 15:11 providing first aid for sudden illness
Unit 15:11 providing first aid for sudden illness Nutrition care process
Nutrition care process Nutrition care process terminology
Nutrition care process terminology Pes statement for diabetes
Pes statement for diabetes Ada 411
Ada 411 Nutrition care process
Nutrition care process Meal percentage intake chart
Meal percentage intake chart Nutrition in primary health care
Nutrition in primary health care Chapter 2 planning a healthy diet
Chapter 2 planning a healthy diet Illness and wellness continuum
Illness and wellness continuum Glenn krauss
Glenn krauss Historical views of mental illness psychology ocr
Historical views of mental illness psychology ocr Food borne illness poster
Food borne illness poster In times of illness na pamphlet
In times of illness na pamphlet Foodborne illness vocabulary
Foodborne illness vocabulary