Case scenario3 Palmoplantar psoriasis with nail involvement History










- Slides: 44
Case scenario-3 Palmoplantar psoriasis with nail involvement
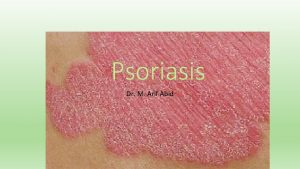
History of presenting illness § 35 year old male § Clerk by profession § Scaly lesions on palms and soles – 5 years § Exacerbation of lesions with fissuring and pain – Difficulty in walking and working in office – 15 days
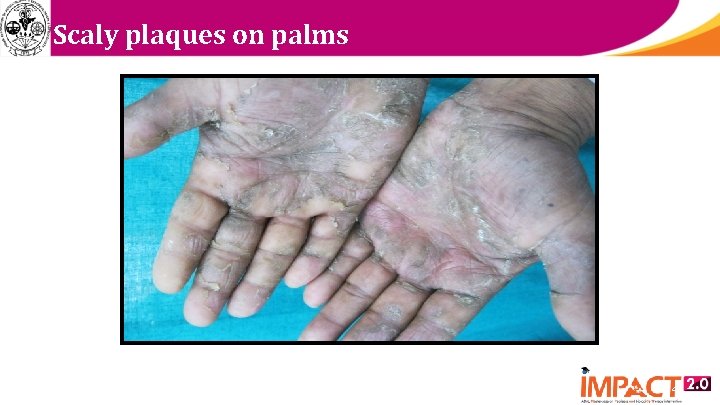
Examination § Well defined scaly plaques – Both palms and soles § Nails – Pitting of all nails – Oil spot 3
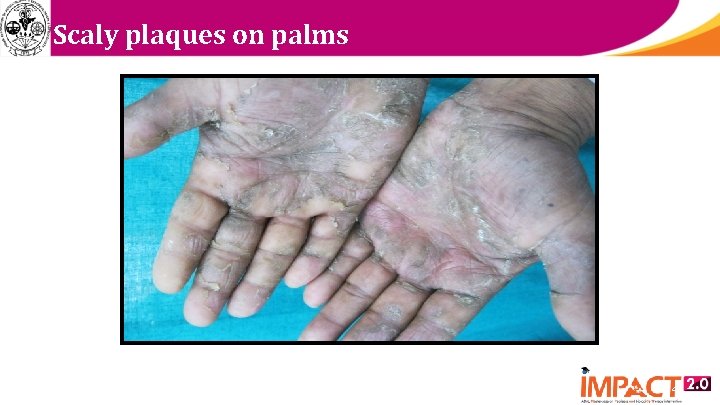
Scaly plaques on palms 4

Scaly plaques on soles 5

Nail changes 6
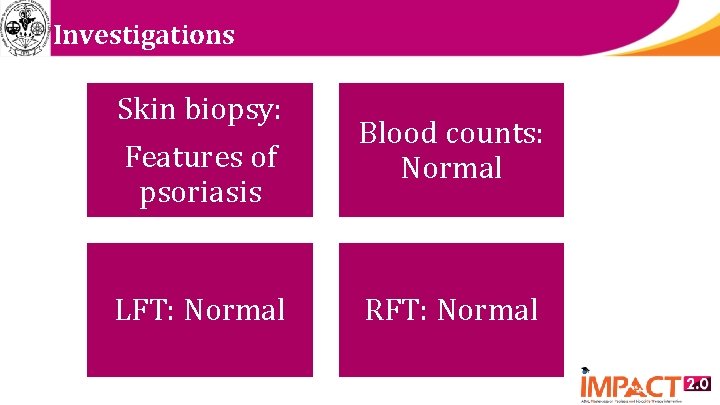
Investigations Skin biopsy: Features of psoriasis LFT: Normal Blood counts: Normal 7 RFT: Normal
How different is palmoplantar psoriasis as a variant of psoriasis? § Affects approx 5% of all psoriasis patients § Second most common form of psoriasis § Disabling and difficult-to-treat variant § Epidemiology is poorly defined § Age of onset is later § More common in: – manual laborers, drivers, farmers, housewives
What is its effect on Quality of life? § Even with less BSA involvement – more likely to suffer from significant impact on Qo. L – significantly more likely to report problems • with mobility, self-care, and usual daily activities – level of functional impairment more § So considered independent criterion of severity – discordance b/w BSA involvement & QOL impact – even justifying the use of biologic therapies
What are the common manifestations? § With or without psoriasis elsewhere on body § Clinical forms: – well-demarcated, erythematous, scaly plaques – thick, scaly, hyperkeratotic plaques – painful fissures – pustules – nail involvement

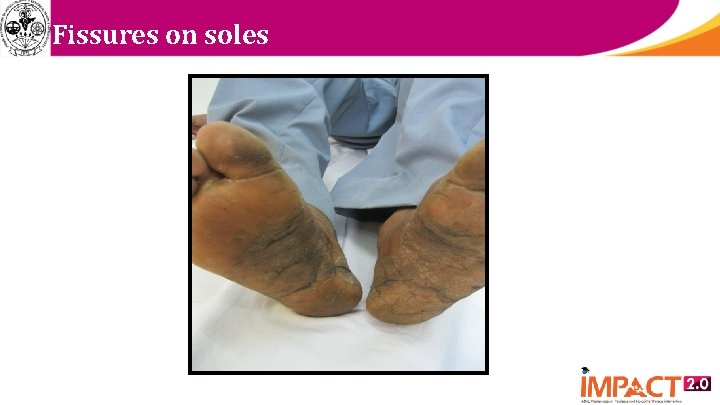
Extensive fissuring
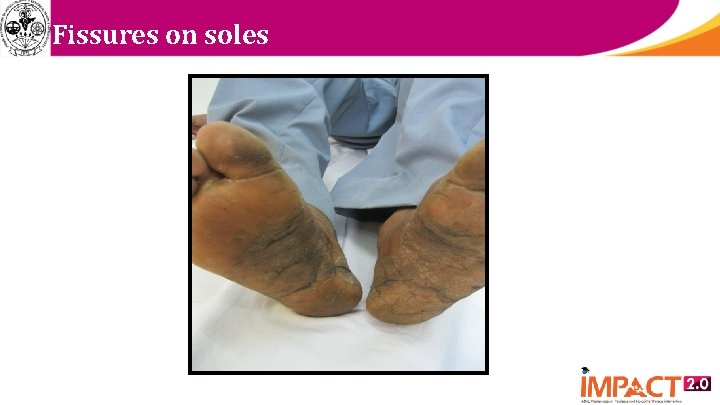
Fissures on soles

Nails

Pustular lesions
What are the triggers? § Trauma § Smoking § Irritants § Genetics: same as psoriasis vulgaris Smoking Genetics: same as psoriasis vulgaris Irritants
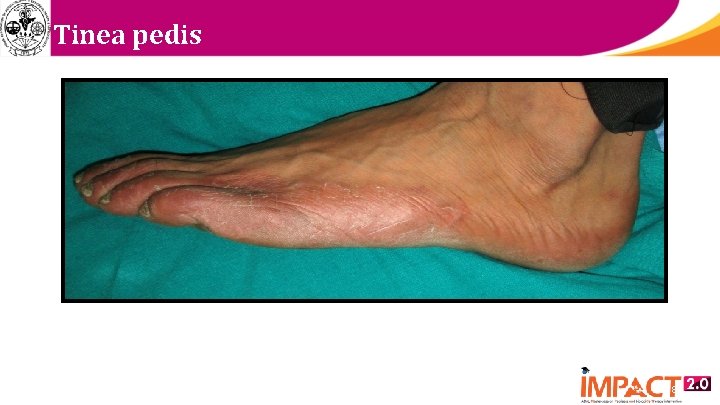
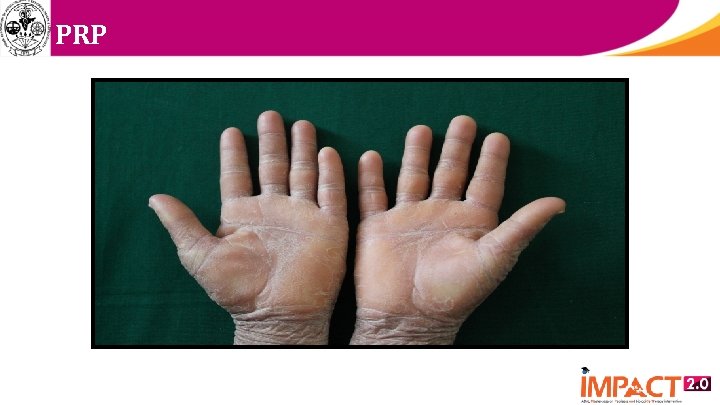
Differential diagnosis § Chronic eczema § Tinea manum/pedis § Pityriasis rubra pilaris § Cutaneous T cell lymphoma § Acquired keratoderma – Greater risk of misdiagnosis when nails affected

Hand eczema 17
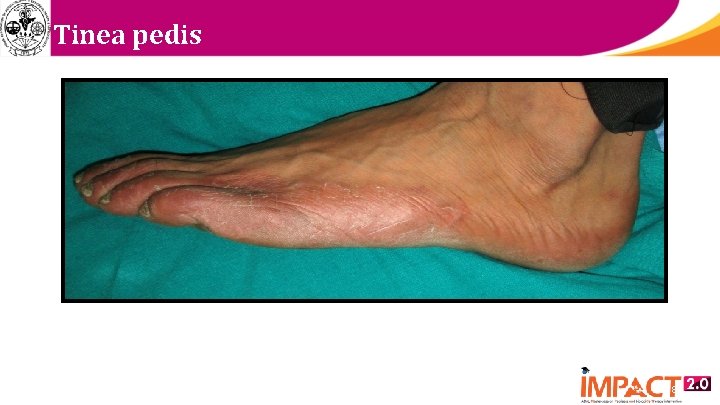
Tinea pedis 18
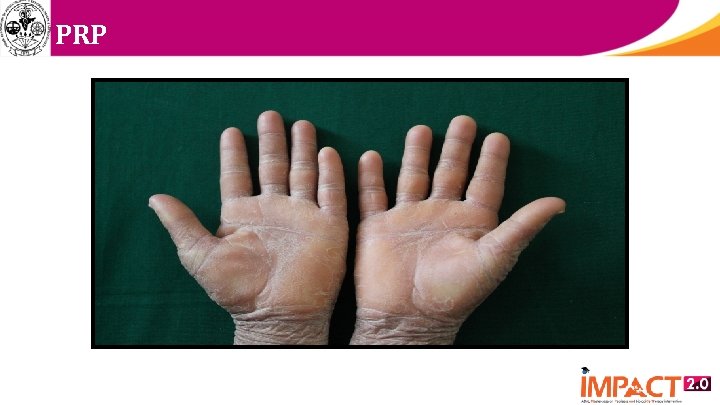
PRP
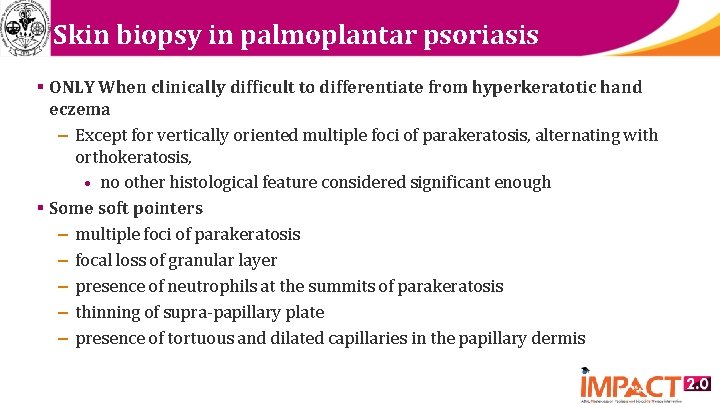
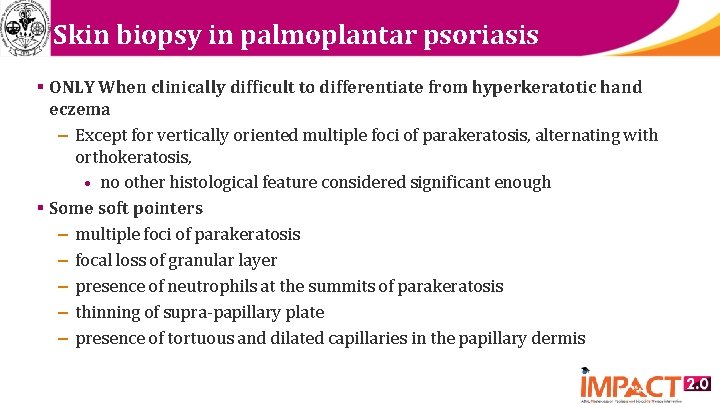
Skin biopsy in palmoplantar psoriasis § ONLY When clinically difficult to differentiate from hyperkeratotic hand eczema – Except for vertically oriented multiple foci of parakeratosis, alternating with orthokeratosis, • no other histological feature considered significant enough § Some soft pointers – multiple foci of parakeratosis – focal loss of granular layer – presence of neutrophils at the summits of parakeratosis – thinning of supra-papillary plate – presence of tortuous and dilated capillaries in the papillary dermis
What are the treatment options? § First line: Topicals § Severe functional impairment, failure of topicals: – Phototherapy – Systemic therapy – Biologics
How to decide on which therapy? § Physical and emotional effects § Benefits and side effects of each therapy § Disease type § Topical treatment: results often disappointing – poor penetration through thick stratum corneum
What are the topical therapies available? § Topical corticosteroids – potent to super-potent, for up to 6 -8 weeks § Keratolytics: Salicylic acid, Urea § Calcipotriol § Tazarotene § Coal tar § Anthralin § Emollients
Factors which increase efficacy of topicals? § Occlusion § Combination of topical corticosteroids with: – Salicylic acid – Calcipotriol – Tazarotene – Phototherapy, Systemics and Biologics § Salicylic acid should not be combined with – Calcipotriene or UVB
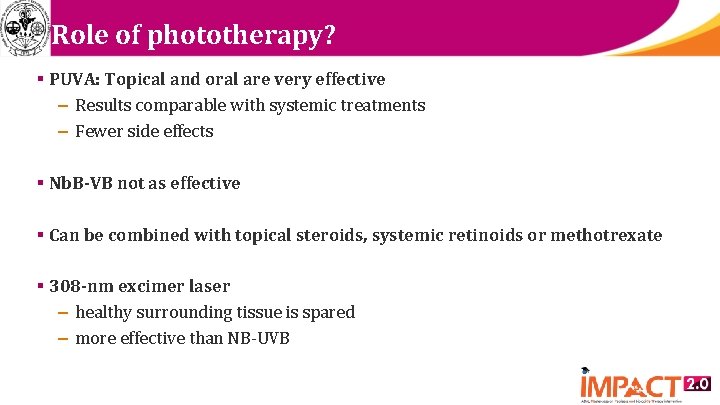
Role of phototherapy? § PUVA: Topical and oral are very effective – Results comparable with systemic treatments – Fewer side effects § Nb. B-VB not as effective § Can be combined with topical steroids, systemic retinoids or methotrexate § 308 -nm excimer laser – healthy surrounding tissue is spared – more effective than NB-UVB
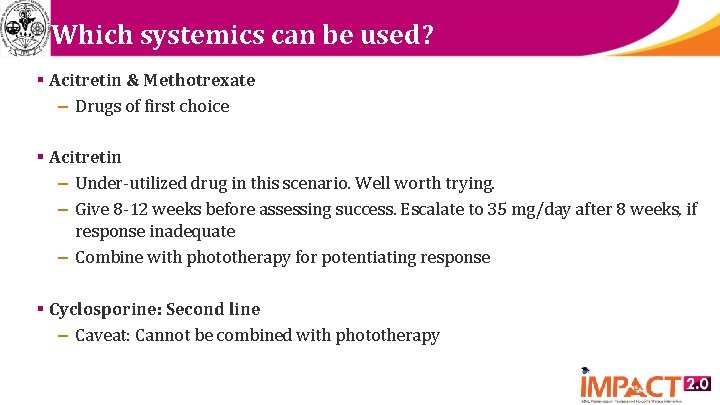
Which systemics can be used? § Acitretin & Methotrexate – Drugs of first choice § Acitretin – Under-utilized drug in this scenario. Well worth trying. – Give 8 -12 weeks before assessing success. Escalate to 35 mg/day after 8 weeks, if response inadequate – Combine with phototherapy for potentiating response § Cyclosporine: Second line – Caveat: Cannot be combined with phototherapy
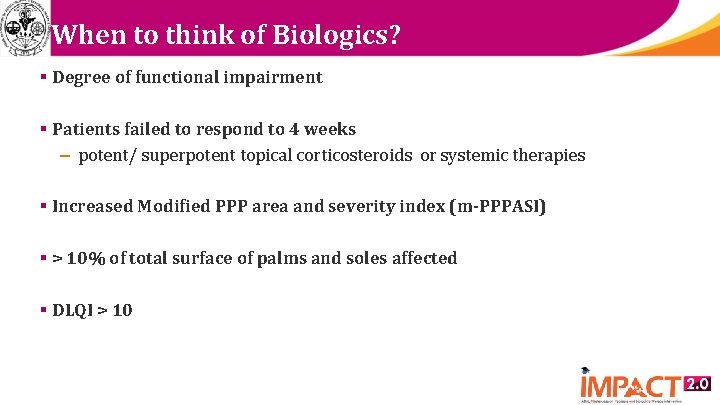
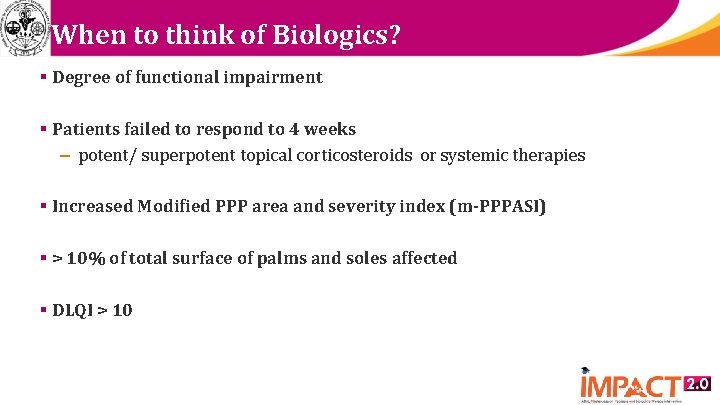
When to think of Biologics? § Degree of functional impairment § Patients failed to respond to 4 weeks – potent/ superpotent topical corticosteroids or systemic therapies § Increased Modified PPP area and severity index (m-PPPASI) § > 10% of total surface of palms and soles affected § DLQI > 10
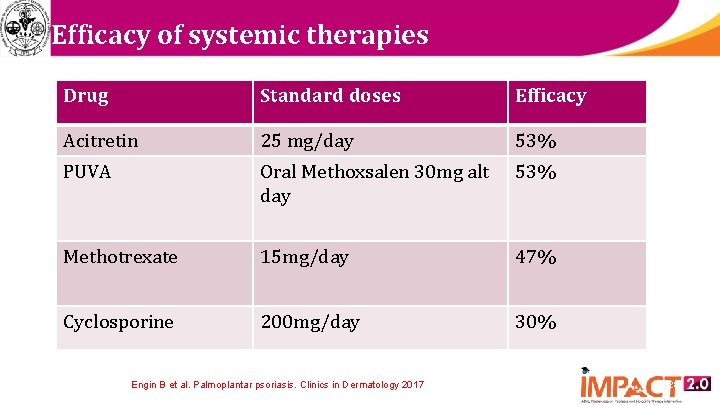
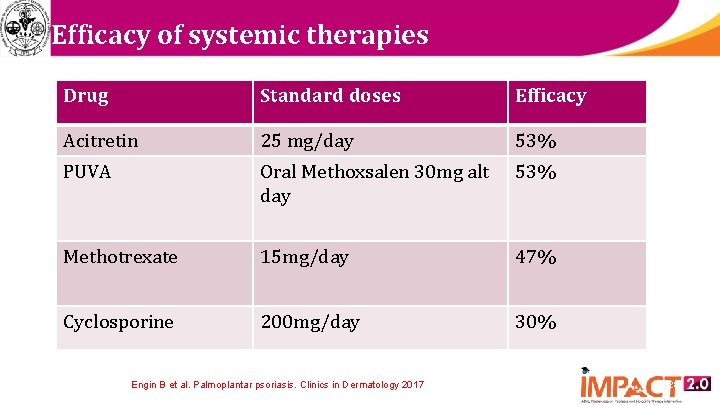
Efficacy of systemic therapies Drug Standard doses Efficacy Acitretin 25 mg/day 53% PUVA Oral Methoxsalen 30 mg alt day 53% Methotrexate 15 mg/day 47% Cyclosporine 200 mg/day 30% Engin B et al. Palmoplantar psoriasis. Clinics in Dermatology 2017; 35: 19 -21 28
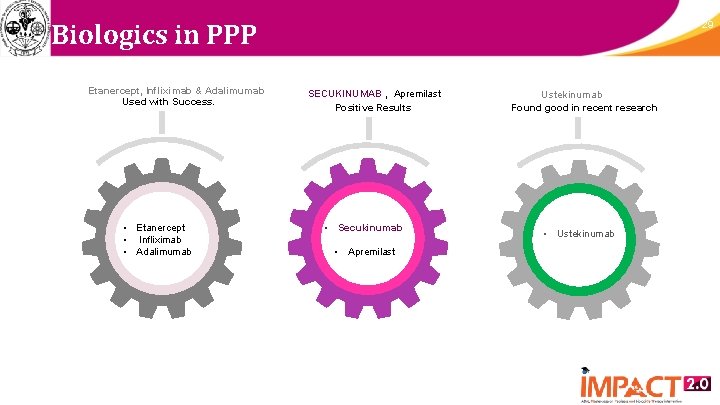
Biologics in PPP Etanercept, Infliximab & Adalimumab Used with Success. • Etanercept • Infliximab • Adalimumab 29 SECUKINUMAB , Apremilast Positive Results • Secukinumab • Apremilast Ustekinumab Found good in recent research • Ustekinumab
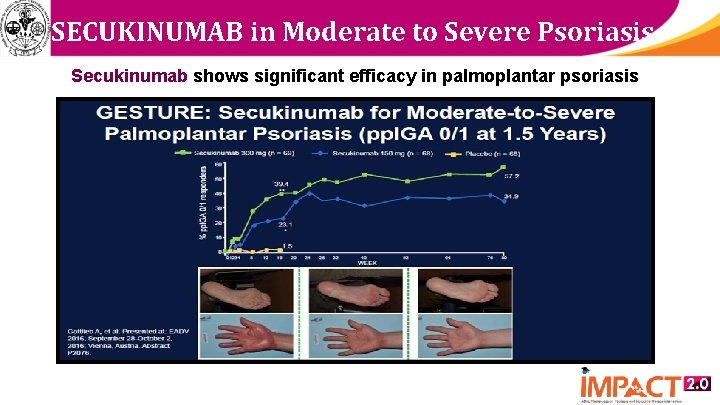
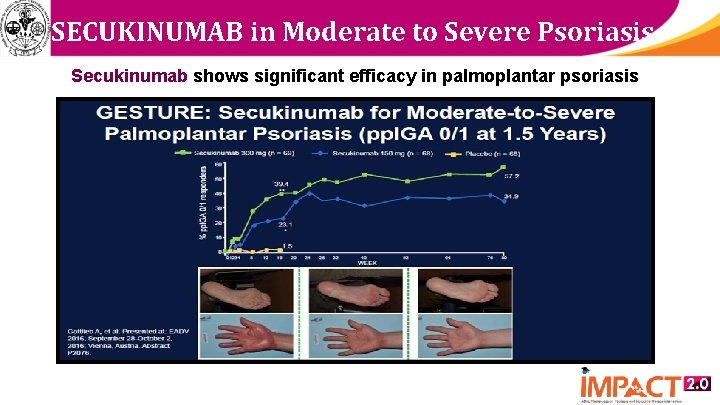
SECUKINUMAB in Moderate to Severe Psoriasis Secukinumab shows significant efficacy in palmoplantar psoriasis
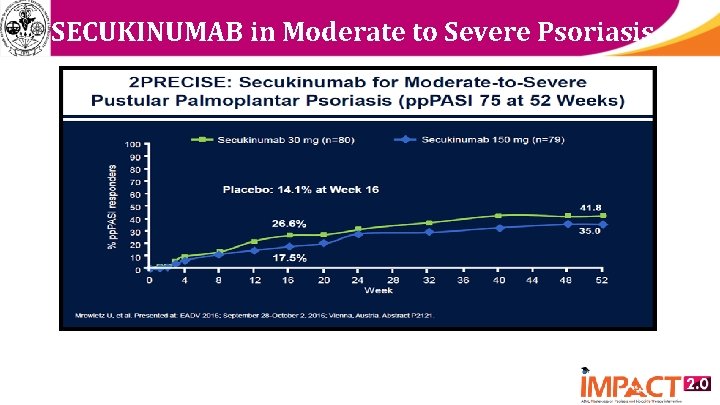
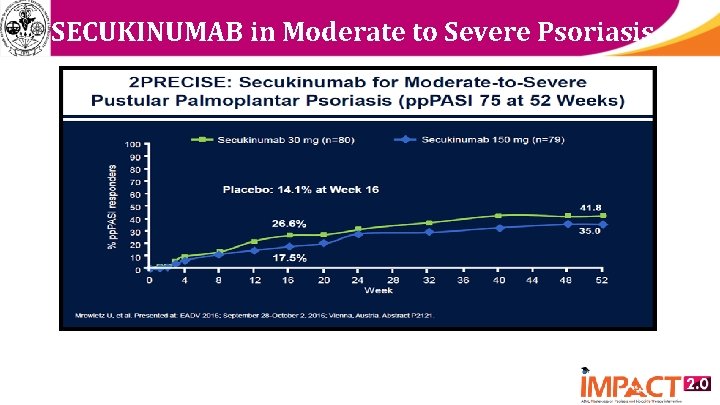
SECUKINUMAB in Moderate to Severe Psoriasis
Treatment of patient in question § Tab Methotrexate 15 mg/week § Tab Folic acid 1 mg X 5/7 days § Topical Calcipotriol with Betamethasone cream in the morning § Topical Urea ointment at night § Good response after 8 weeks
Nail psoriasis § 10 -78%: concurrent nail psoriasis in palmoplantar psoriatics* § Isolated nail involvement: 5 -10% § 10% more common in males § More frequently associated with: – Scalp psoriasis – Genital psoriasis – Psoriatic arthritis. (70 -80% of psoriatic arthritis patients have nail psoriasis) § Significant physical and psychological handicap § Indicator of severe disease (joints) *Dogra A, Arora AK. Nail psoriasis: The journey so far. Indian J Dermatol 2014; 59: 319 -33

DIP jt involvement: Nail association
Common manifestations of nail psoriasis Common manifestations § Pitting: commonest of nail psoriasis – length of pit • suggestive of duration – deeper pit • suggestive of involvement of intermediate and ventral matrix – may be arranged in transverse or longitudinal rows or disorganized

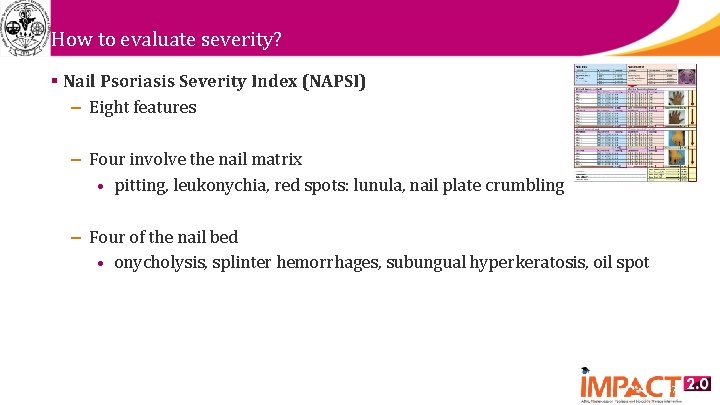
How to evaluate severity? § Nail Psoriasis Severity Index (NAPSI) – Eight features – Four involve the nail matrix • pitting, leukonychia, red spots: lunula, nail plate crumbling – Four of the nail bed • onycholysis, splinter hemorrhages, subungual hyperkeratosis, oil spot 37

Treatment- General measures § Nails should be kept short – avoids exacerbating onycholysis – avoids accumulation of exogenous material under nail § Avoid trauma to nails – prevents onycholysis and entry of pathogens § Protection against irritants § Avoid aggressive manicure of the cuticle – may provoke paronychia § Cosmetic camouflage not advisable 39
Treatment options available Topical therapy § Nail matrix involvement – Intralesional steroids – Tazarotene – Topical potent steroids § Nail bed involvement – Calcipotriol and topical steroids – Tazarotene – Cyclosporine 40
Other options § Clobetasol lacquer § Iontophoresis – Dexamethasone § Intralesional – Methotrexate – Cyclosporine § Laser: PDL*, Fractional CO 2 followed by tazarotene/potent steroids *- Limited nail involvement
Many nails involved § PUVA § Acitretin – Low doses § Methotrexate § Cyclosporine § Biologics – Infliximab – Etanercept – Secukinumab
What is the role of biologics? § Conventional treatment for nail psoriasis – unsatisfactory, tedious and inconvenient § Most of the treatment options – achieve only a moderate efficacy – complete clearance is infrequent § Efficacy of conventional therapy – decreases with time § Role of biologics – efficacy in both the skin and nail components

Thank you 44
 Physiopathologie psoriasis
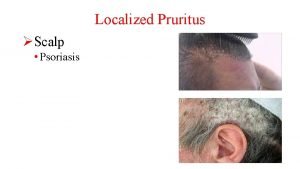
Physiopathologie psoriasis Seborrheic dermatitis red spots on scalp
Seborrheic dermatitis red spots on scalp Psoriasis
Psoriasis Pityriasis rosea differential
Pityriasis rosea differential Psoriasis ungual
Psoriasis ungual Anatomy and physiology of psoriasis
Anatomy and physiology of psoriasis Grattage test in psoriasis
Grattage test in psoriasis Psoriasis arthritis nhs
Psoriasis arthritis nhs Rehaklinik psoriasis arthritis
Rehaklinik psoriasis arthritis Cancerous mole signs
Cancerous mole signs Psoriasis annularis
Psoriasis annularis Best worst and average case
Best worst and average case Nails canterbury
Nails canterbury What's history
What's history History of nail
History of nail History of nail
History of nail Involvement decision making
Involvement decision making Total member involvement pdf
Total member involvement pdf Panther involvement network
Panther involvement network 7 principles of social work felix biestek
7 principles of social work felix biestek Panther involvement network
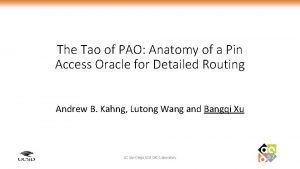
Panther involvement network Pin.gsu.edu
Pin.gsu.edu How can employee involvement measures motivate employees
How can employee involvement measures motivate employees Gaisce record sheet
Gaisce record sheet Furcationplasty
Furcationplasty Brazil ww2 involvement
Brazil ww2 involvement Active community participation definition
Active community participation definition What drove european involvement in asian commerce
What drove european involvement in asian commerce Father involvement activities
Father involvement activities Contoh social judgment theory
Contoh social judgment theory Epstein's model
Epstein's model Through and through furcation
Through and through furcation 4 levels of parenting
4 levels of parenting Pacing continuum
Pacing continuum Panther involvement network
Panther involvement network Panther involvement network
Panther involvement network Panther involvement network
Panther involvement network Muscular involvement continuum
Muscular involvement continuum Allies ww1
Allies ww1 Tarnside curve of involvement
Tarnside curve of involvement Panther involvement network
Panther involvement network Tarnside curve of involvement
Tarnside curve of involvement Class 2 furcation
Class 2 furcation A national policy of avoiding involvement in world affairs
A national policy of avoiding involvement in world affairs Factors affecting performance in netball
Factors affecting performance in netball