Psoriasis Definition Psoriasis is a common chronic disfiguring















- Slides: 56
Psoriasis
Definition Psoriasis is a common, chronic, disfiguring, inflammatory and proliferative condition of the skin; in which both genetic and environmental influences play a critical role characterised by red, scaly, sharply demarcated indurated plaques of various sizes, particularly over extensor surfaces and scalp.

Aetiopathogenesis Genetic predisposition: HLA-B 13, B 17, and Cw 6 Epidermal Antigen hyperproliferation driven activation of autoreactive T-cells Angiogenesis Multifactorial inheritance Overexpression of Th 1 cytokines such as IL 2, IL 6, IL 8, IL 12, INF - γ, TNF α
Trigger factors Trauma (Koebner phenomenon): Mechanical, chemical, radiation trauma. Infections: Streptococcus, HIV Stress Alcohol and smoking Metabolic Sunlight: factors: pregnancy, hypocalcemia usually beneficial but in some may cause exacerbation
Trigger factors Drugs: Beta-blockers NSAIDS ACE inhibitors Lithium Antimalarials Terbinafine Calcium channel blockers Captopril Withdrawal of corticosteroids
Patient Profile Sex: Adults (M=F) but in adolescents (F>M) Age: 2 peak age ranges 1 st peak : 16 -22 years 2 nd peak: 57 -60 years Earlier age of onset: Female sex Positive family history 3 -fold higher risk in siblings of patients with onset before 15 years of age
History Patients give H/O Prominent itchy, red areas with increased skin scaling and peeling. New lesions appearing at sites of injury/trauma to the skin (Koebner phenomenon) Actual clearance of lesions following trauma to the skin (Reverse Koebner phenomenon) Exacerbation Significant 20% in winter, improvement in summer joint pain, stiffness, deformity in 10 -
Morphology Classical Lesion: Erythematous, round to oval well defined scaly plaques with sharply demarcated borders Scales: Psoriatic plaques typically have a dry, thin, silvery-white or micaceous scale. Sites: Elbows, knees, extensors of extremities, scalp & sacral region in a symmetric pattern. Palms/ soles involved commonly
Morphology Auspitz sign: Removing the scale reveals a smooth, red, glossy membrane with tiny punctate bleeding points Grattage test: On grattage, characteristic coherence of scales seen as if one scratches a wax candle(‘signe de la tache de bougie)
Morphology Koebner’s phenomenon Linear distribution of the plaques seen along scratch marks or at sites of trauma Woronoff‘s ring Psoriatic plaques occasionally appear to be immediately encircled by a paler peripheral zone.
Morphological Types Chronic plaque psoriasis: plaques with less scaling Follicular Linear psoriasis: follicular papules. psoriasis: linear arrangement of plaques Annular/ figurate psoriasis: ring shaped or other patterns. Rupoid, elephantine and ostraceous psoriasis
Morphological Types Guttate psoriasis: Common in children , good prognosis Pustular psoriasis: Crops of pustules based on erythema ◦ Localised / generalised ◦ Impetigo herpetiformis Erythrodermic psoriasis: 16 -24% of all cases of exfoliative dermatitis











Distributional Variation Scalp psoriasis Palmoplantar psoriasis Nail psoriasis: pitting, onycholysis, subungual hyperkeratosis, or the oil-drop sign. (25 -50%) Mucosal Inverse psoriasis: ◦ spares the typical extensor surfaces ◦ affects intertriginous (i. e, axillae, inguinal folds, inframammary creases) areas with minimal scaling.
Psoriasis in children and in HIV Psoriasis in children: Plaques Diaper Face not as thick as in adults, less scaly area in infants, flexural areas in children involvement more common than in adults Psoriasis in HIV: Acute onset Severe Poor flares prognosis
Psoriatic arthritis Seen in 5 -10% of psoriatic patients Types: 1. Classic (16%)-DIP joint involvement 2. Oligoarticular (70%) 3. Rheumatoid type(15%) 4. Psoriatic spondylitis (5%) 5. Arthtritis mutilans (5%) Contd…
Psoriatic arthritis Associations: Tenosynovitis Enthesitis Osteolysis New bone formation Joint fibrosis & ankylosis
Complicated psoriasis Erythrodermic Generalised Psoriatic psoriasis pustular psoriasis arthritis



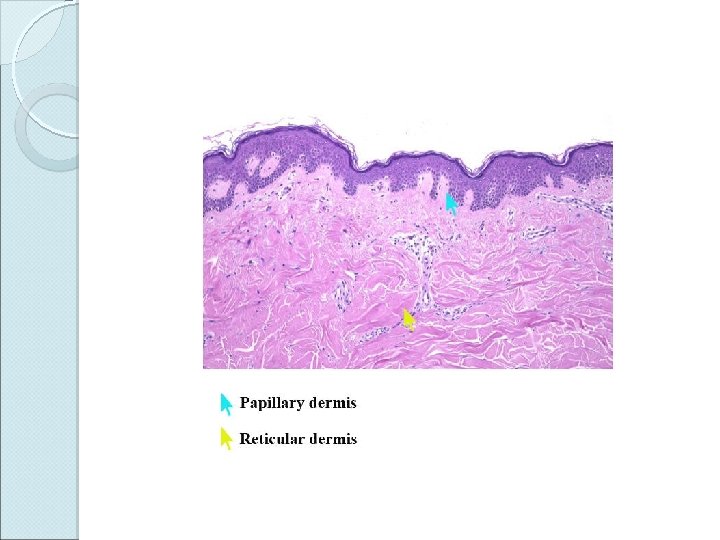
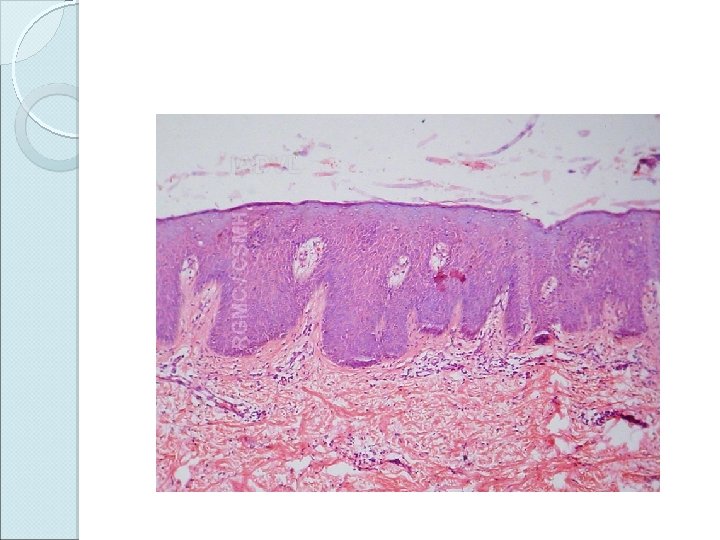
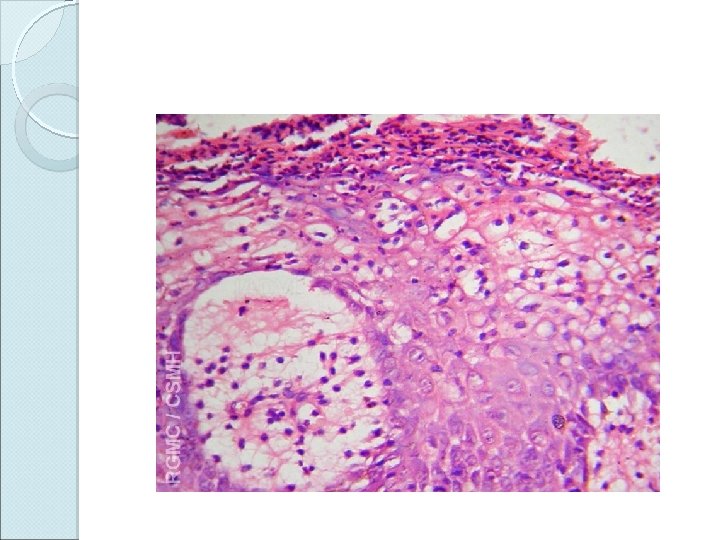
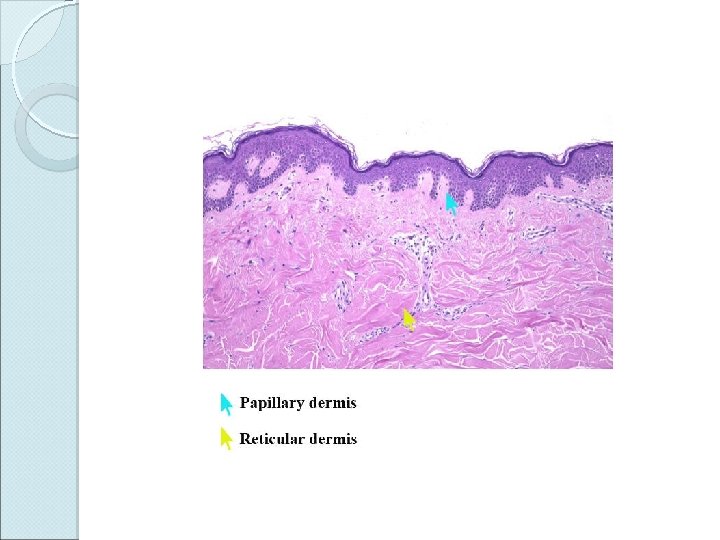
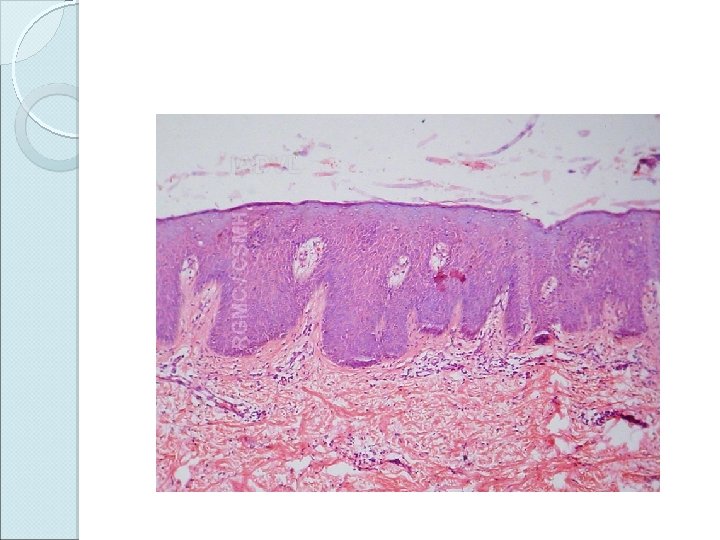
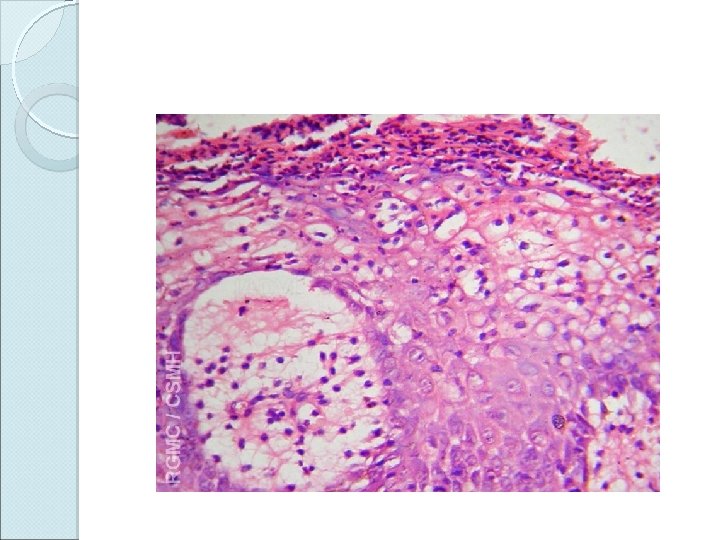
Histopathology Skin biopsy findings: Parakeratosis Microabscesses of Munro in the horny layer Absence of granular layer Regular elongation of rete ridges (camel-foot shaped) Suprapapillary thinning of st. malpighii Spongiform pustules of Kogoj Dilated and tortuous capillaries in dermal papillae Superficial perivascular inflammatory infiltrate
Differential diagnosis Nummular Tinea corporis Lichen planus Secondary Pityriasis Drug eczema syphilis rosea eruption Candidiasis Tinea unguium Seborrheic dermatitis
Treatment General measures: Counselling regarding the natural course of the disease Weigh reduction in obese patients. Avoidance of trauma or irritating agents. Reduce intake of alcoholic beverages. Reduce emotional stress Sunlight and sea bathing improve psoriasis except in photosensitive
Topical therapy Emollients: white soft paraffin & liquid paraffin Corticosteroids: Potent steroids like fluocinolone acetonide, betamethasone dipropionate or clobetasol propionate 5 -10% Coal tar: for stable but resistant plaques 0. 1 -1% dithranol: for few stable, thick, resistant plaques Contd…
Topical therapy Keratolytics & humectants: as adjuvants eg. Salicylic acid 3 -10%, urea 10 -20% Calcipotriene Tazarotene Macrolactams (calcineurin inhibitors): Tacrolimus & Pimecrolimus.
Response to topical therapy Effects of topical therapy evident in 2 -3 weeks Clearing of scale is usually observed first, followed by flattening of the treated plaques Resolution of erythema may take 6 -8 weeks
Phototherapy 1. Extensive and widespread disease 2. Resistance to topical therapy
PUVA photochemotherapy (PUVA) Combined use of a photosensitizing drug methoxsalen (8 -methoxypsoralens) with UVA irradiation (320 -400 nm) Mechanism of action: 1. Interferes with DNA synthesis → decrease cellular proliferation 2. Induces apoptosis of cutaneous lymphocytes (localized immunosuppression).
Method of administering PUVA 0. 6 mg/kg of 8 -MOP(methoxypsoralen) given 2 hrs before irradiation Initial dose of UVA is 2 -5 J/cm 2 with exposure time of 5 mins PUVA administered 2 -3 times per week in an outpatient setting. Every week UVA dose increased by 20% and exposure time by 5 mins Maintenance treatments every 2 -4 weeks until remission Relief with 20 -30 treatments
Side Effects Nausea, pruritus, burning sensation. Long-term complications ◦ photo damage to the skin ◦ skin cancer
UVB phototherapy Irradiation Effective with light of wavelength 290 -320 nm for moderate to severe psoriasis Usually combined with one or more topical treatments like tar or anthralin Narrow-band UVB phototherapy Use of a fluorescent bulb with a narrow emission spectrum that peaks at 311 nm (UVB spectrum, 290 -320 nm). More effective than broadband UVB for the treatment of plaque-type psoriasis
Systemic Agents Indications: Resistant to both topical treatment and phototherapy Active psoriatic arthritis. Physically, psychologically, socially or economically disabling disease Steroids: only used in life threatening situations like erythrodermic & pustular psoriasis. Cyclosporin: Immune modulator ◦ Used in erythrodermic & resistant psoriasis ◦ Limitations: expensive & nephrotoxic and hypertensive
Systemic Agents Methotrexate: ◦ Three doses of 2. 5 -5 mg orally 12 hrly or 7. 5 -15 mg single dose; administered every week. ◦ Contraindicated in hepatic & renal diseases. Close monitoring of blood counts & hepatic function essential. Acitretin: ◦ For widespread psoriasis; combination with PUVA reduces total cumulative dose of UV irradiation ◦ Contraindicated in pregnancy & women of child bearing age
Biological therapies Selective, immunologically directed intervention at key steps in the pathogenesis of the disease. Mechanism of action: Inhibits the initial cytokine release and Langerhans cell migration Targets activated T cells, prevents further T-cell activation, and eliminates pathologic T cells; Inhibits proinflammatory cytokines, such as TNF
Biological therapies Indications: Severe, recalcitrant cases Psoriatic arthritis Mode of administration: Intravenous, Subcutaneous Biological agents: Efalizumab (Raptiva) Etanercept (Enbrel ) Infliximab (Remicade)
Prognosis Course of plaque psoriasis is unpredictable. Characterised by remissions and relapses Often intractable to treatment Relapses in most patients Improves in warm weather Poor Prognostic factors: Early onset, Family history, Stress, HIV infection
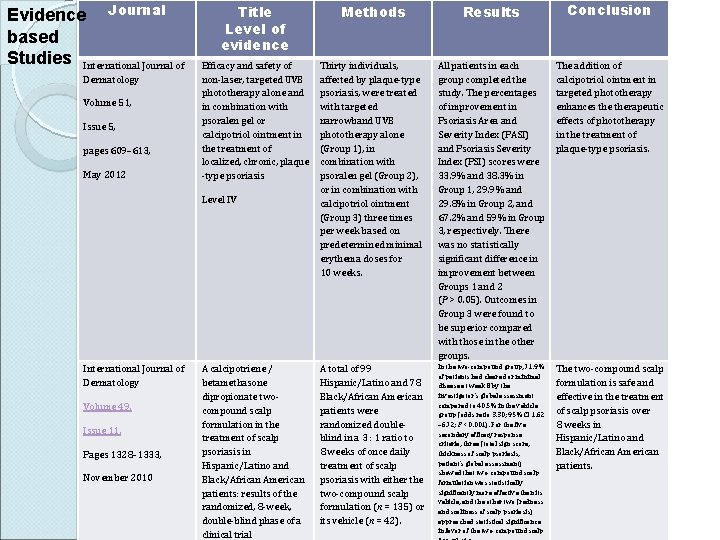
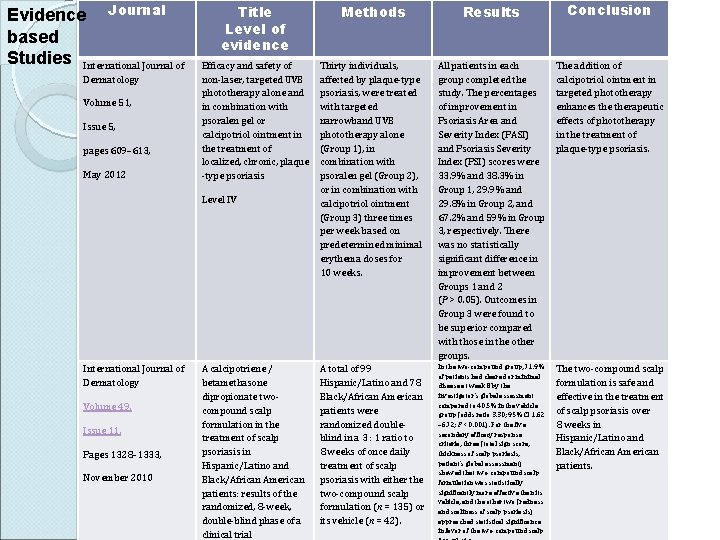
Evidence Journal based Studies International Journal of Dermatology Volume 51, Issue 5, pages 609– 613, May 2012 Title Level of evidence Methods Results Conclusion Efficacy and safety of non-laser, targeted UVB phototherapy alone and in combination with psoralen gel or calcipotriol ointment in the treatment of localized, chronic, plaque -type psoriasis Thirty individuals, affected by plaque-type psoriasis, were treated with targeted narrowband UVB phototherapy alone (Group 1), in combination with psoralen gel (Group 2), or in combination with calcipotriol ointment (Group 3) three times per week based on predetermined minimal erythema doses for 10 weeks. All patients in each group completed the study. The percentages of improvement in Psoriasis Area and Severity Index (PASI) and Psoriasis Severity Index (PSI) scores were 33. 9% and 38. 3% in Group 1, 29. 9% and 29. 8% in Group 2, and 67. 2% and 59% in Group 3, respectively. There was no statistically significant difference in improvement between Groups 1 and 2 (P > 0. 05). Outcomes in Group 3 were found to be superior compared with those in the other groups. The addition of calcipotriol ointment in targeted phototherapy enhances therapeutic effects of phototherapy in the treatment of plaque-type psoriasis. A total of 99 Hispanic/Latino and 78 Black/African American patients were randomized doubleblind in a 3 : 1 ratio to 8 weeks of once daily treatment of scalp psoriasis with either the two-compound scalp formulation (n = 135) or its vehicle (n = 42). In the two-compound group, 71. 9% of patients had cleared or minimal disease at week 8 by the investigator’s global assessment compared to 40. 5% in the vehicle group (odds ratio 3. 30; 95% CI 1. 62 – 6. 72; P < 0. 001). For the five secondary efficacy response criteria, three (total sign score, thickness of scalp psoriasis, patient’s global assessment) showed that two-compound scalp formulation was statistically significantly more effective than its vehicle, and the other two (redness and scaliness of scalp psoriasis) approached statistical significance in favor of the two-compound scalp The two-compound scalp formulation is safe and effective in the treatment of scalp psoriasis over 8 weeks in Hispanic/Latino and Black/African American patients. Level IV International Journal of Dermatology Volume 49, Issue 11, Pages 1328– 1333, November 2010 A calcipotriene / betamethasone dipropionate twocompound scalp formulation in the treatment of scalp psoriasis in Hispanic/Latino and Black/African American patients: results of the randomized, 8 -week, double-blind phase of a clinical trial
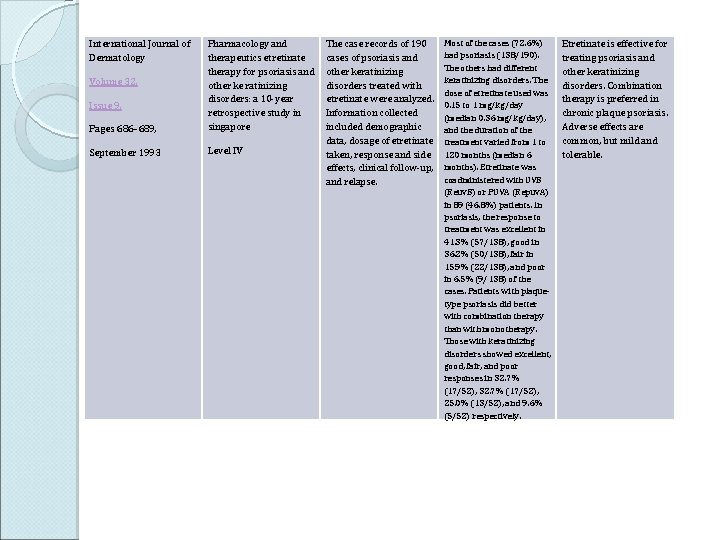
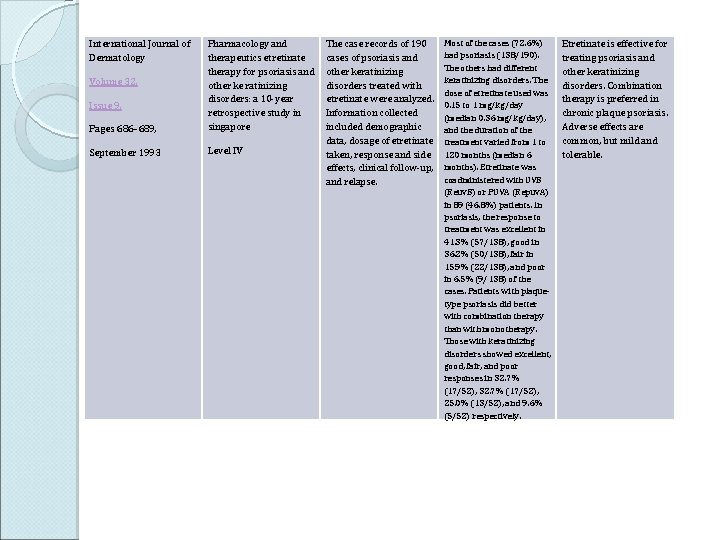
International Journal of Dermatology Pages 686– 689, Pharmacology and therapeutics etretinate therapy for psoriasis and other ke ratinizing disorders: a 10 -year retrospective study in singapore September 1993 Level IV Volume 32, Issue 9, The case records of 190 cases of psoriasis and other keratinizing disorders treated with etretinate were analyzed. Information collected included demographic data, dosage of etretinate taken, response and side effects, clinical follow-up, and relapse. Most of the cases (72. 6%) had psoriasis (138/190). The others had different keratinizing disorders. The dose of etretinate used was 0. 15 to 1 mg/kg/day (median 0. 36 mg/kg/day), and the duration of the treatment varied from 1 to 120 months (median 6 months). Etretinate was coadministered with UVB (Reuv. B) or PUVA (Repuv. A) in 89 (46. 8%) patients. In psoriasis, the response to treatment was excellent in 41. 3% (57/138), good in 36. 2% (50/138), fair in 15. 9% (22/138), and poor in 6. 5% (9/138) of the cases. Patients with plaquetype psoriasis did better with combination therapy than with monotherapy. Those with keratinizing disorders showed excellent, good, fair, and poor responses in 32. 7% (17/52), 25. 0% (13/52), and 9. 6% (5/52) respectively. Etretinate is effective for treating psoriasis and other keratinizing disorders. Combination therapy is preferred in chronic plaque psoriasis. Adverse effects are common, but mild and tolerable.
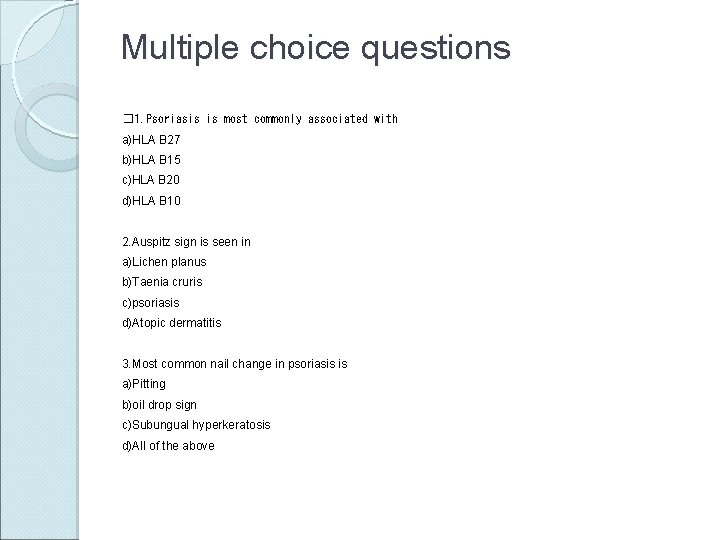
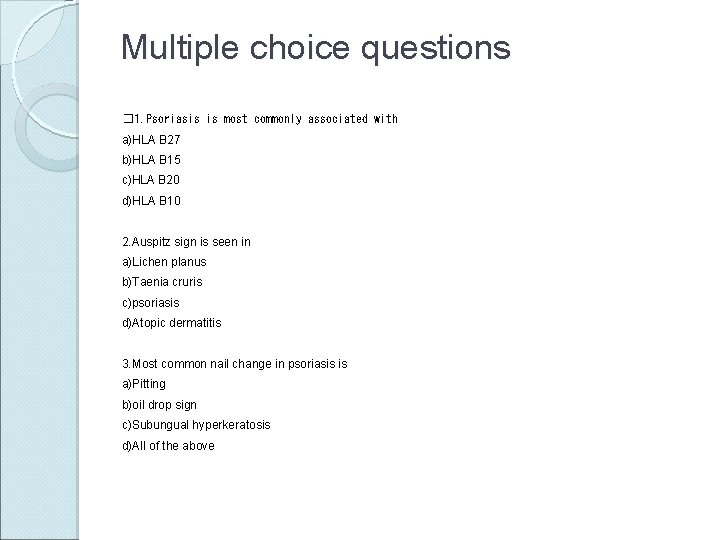
Multiple choice questions � 1. Psoriasis is most commonly associated with a)HLA B 27 b)HLA B 15 c)HLA B 20 d)HLA B 10 2. Auspitz sign is seen in a)Lichen planus b)Taenia cruris c)psoriasis d)Atopic dermatitis 3. Most common nail change in psoriasis is a)Pitting b)oil drop sign c)Subungual hyperkeratosis d)All of the above
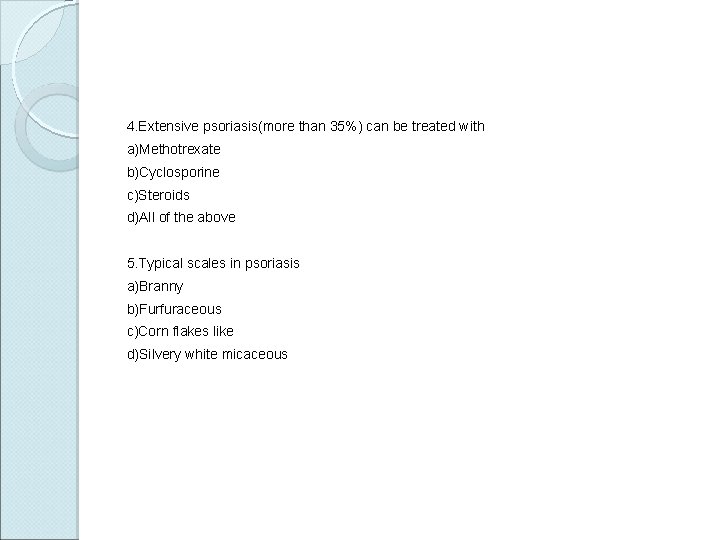
4. Extensive psoriasis(more than 35%) can be treated with a)Methotrexate b)Cyclosporine c)Steroids d)All of the above 5. Typical scales in psoriasis a)Branny b)Furfuraceous c)Corn flakes like d)Silvery white micaceous
Thank you