ARC DefiniteConfirmed Acute coronary syndrome AND Angiographic confirmation





- Slides: 41

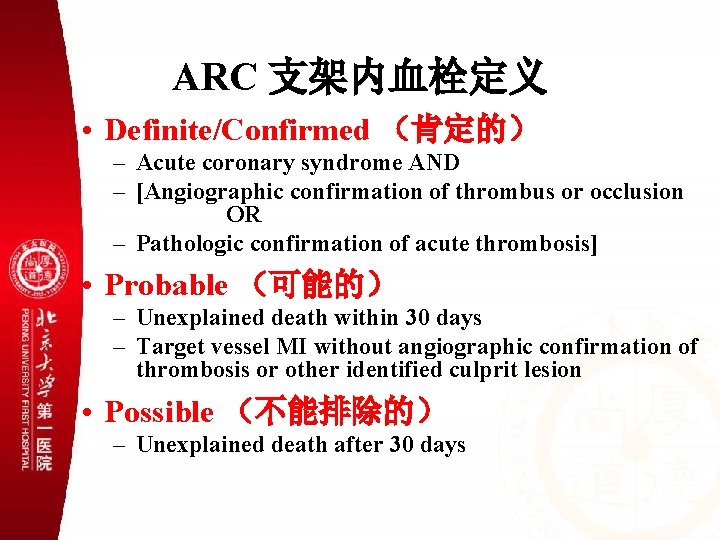
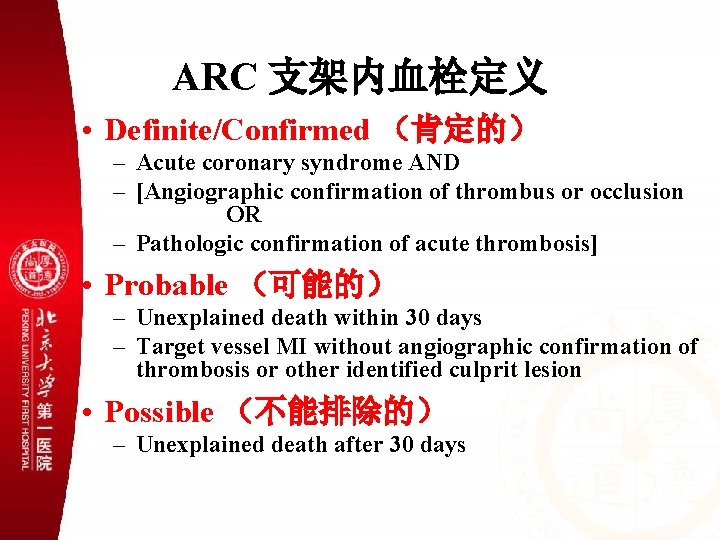
ARC 支架内血栓定义 • Definite/Confirmed (肯定的) – Acute coronary syndrome AND – [Angiographic confirmation of thrombus or occlusion OR – Pathologic confirmation of acute thrombosis] • Probable (可能的) – Unexplained death within 30 days – Target vessel MI without angiographic confirmation of thrombosis or other identified culprit lesion • Possible (不能排除的) – Unexplained death after 30 days
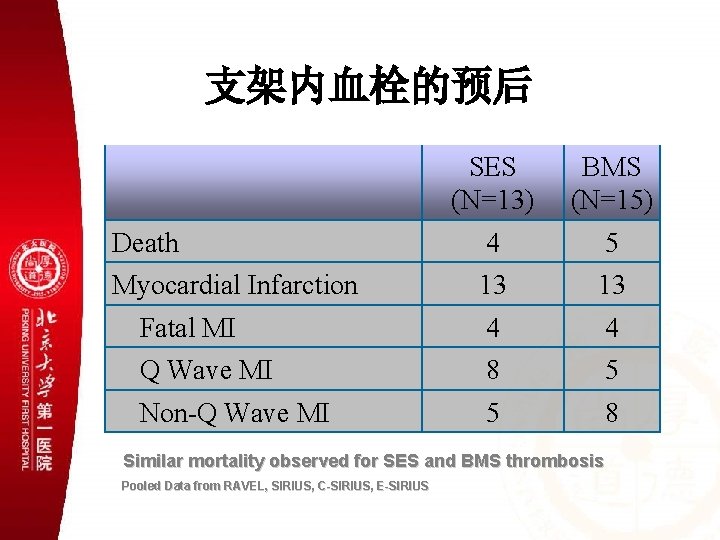
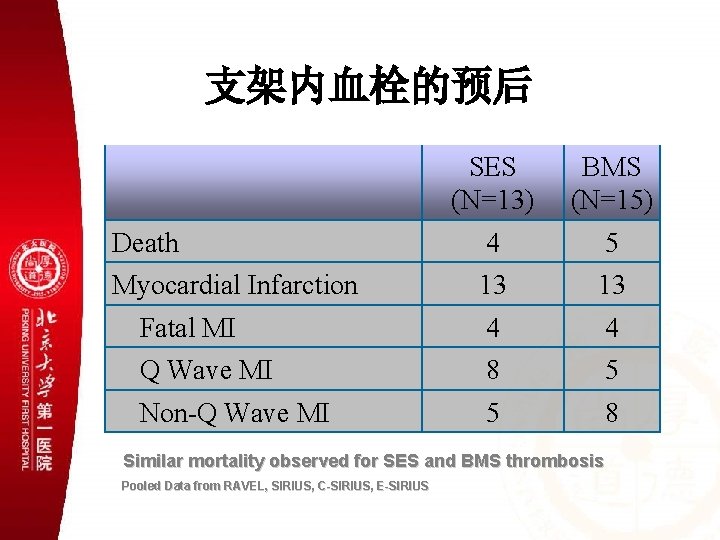
支架内血栓的预后 SES (N=13) BMS (N=15) Death 4 5 Myocardial Infarction 13 13 Fatal MI 4 4 Q Wave MI 8 5 Non-Q Wave MI 5 8 Similar mortality observed for SES and BMS thrombosis Pooled Data from RAVEL, SIRIUS, C-SIRIUS, E-SIRIUS
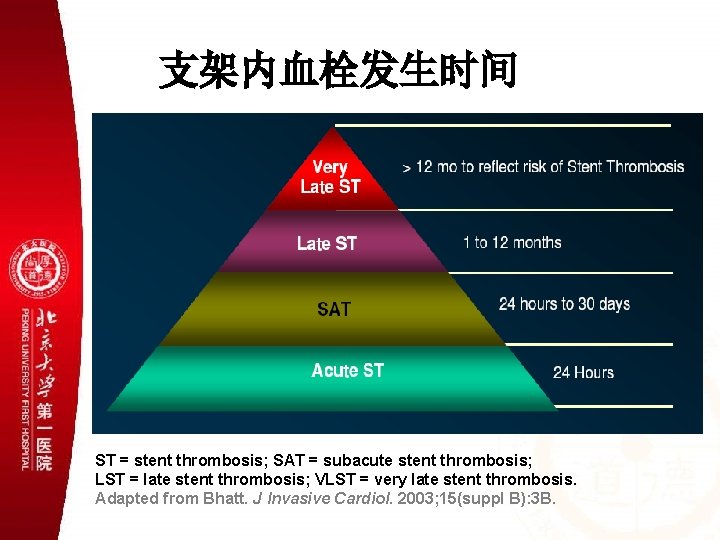
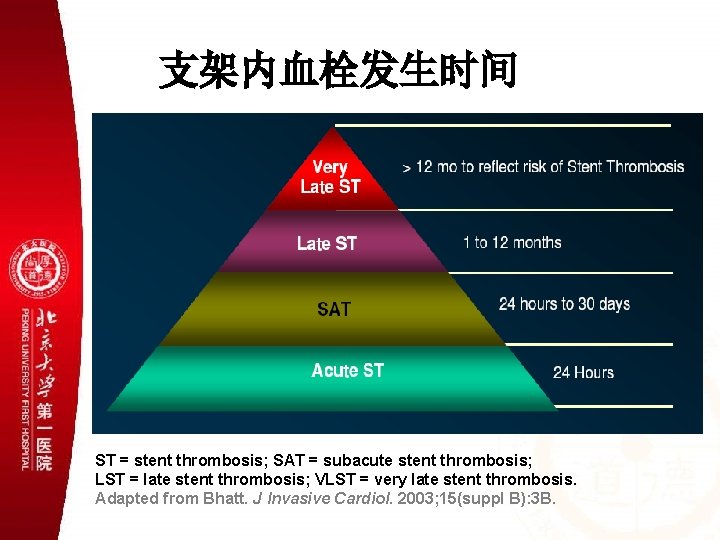
支架内血栓发生时间 ST = stent thrombosis; SAT = subacute stent thrombosis; LST = late stent thrombosis; VLST = very late stent thrombosis. Adapted from Bhatt. J Invasive Cardiol. 2003; 15(suppl B): 3 B.
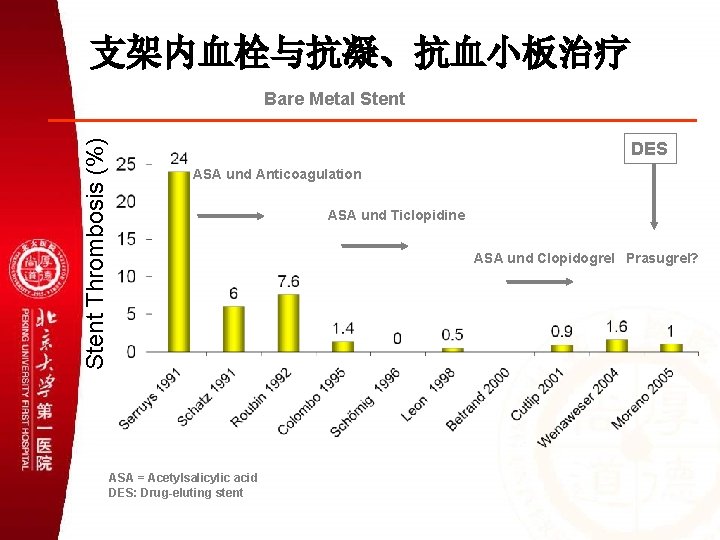
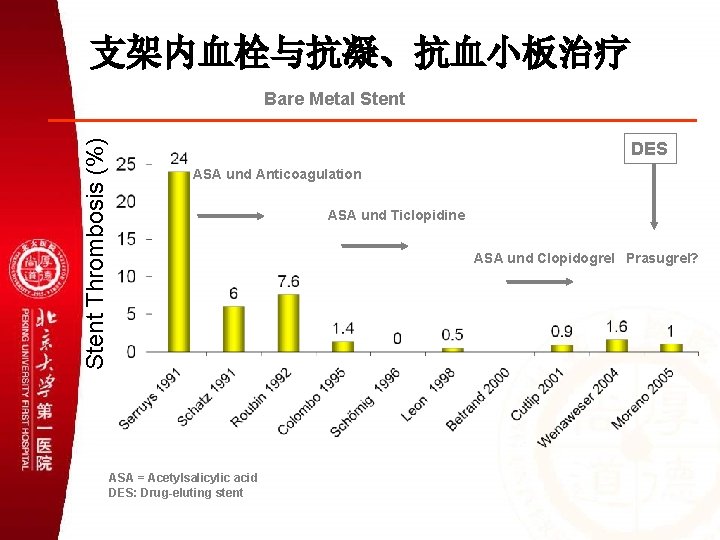
支架内血栓与抗凝、抗血小板治疗 Stent Thrombosis (%) Bare Metal Stent DES ASA und Anticoagulation ASA und Ticlopidine ASA und Clopidogrel Prasugrel? ASA = Acetylsalicylic acid DES: Drug-eluting stent
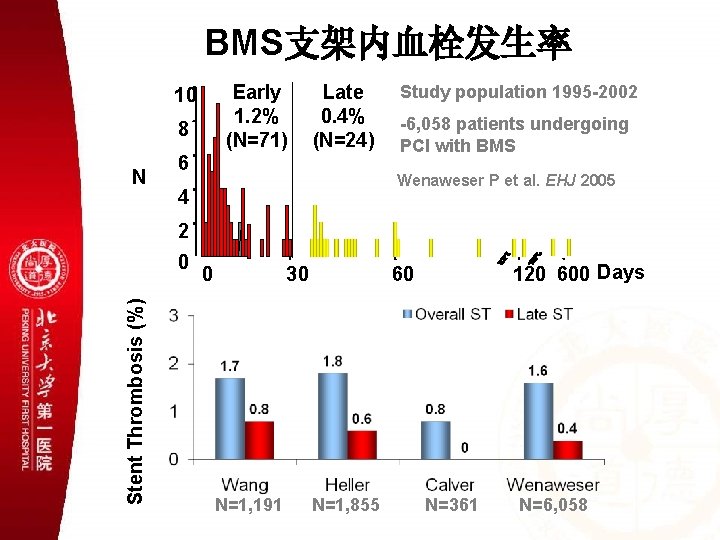
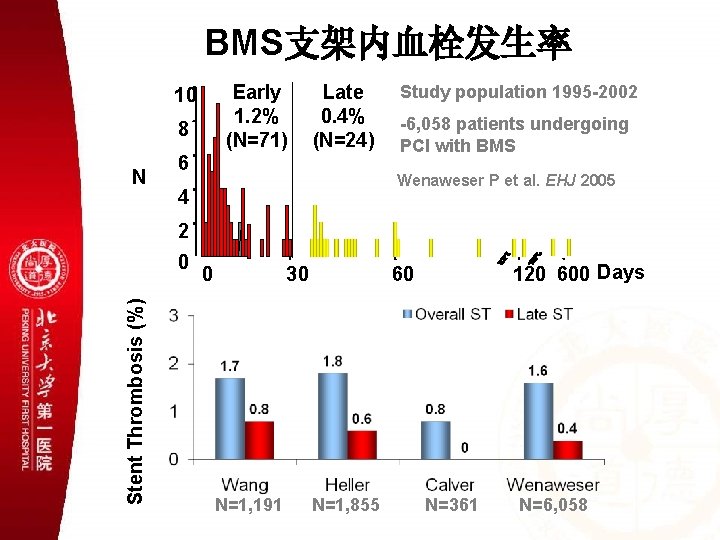
BMS支架内血栓发生率 Early 1. 2% (N=71) 10 8 N Late 0. 4% (N=24) 6 Study population 1995 -2002 -6, 058 patients undergoing PCI with BMS Wenaweser P et al. EHJ 2005 4 2 Stent Thrombosis (%) 0 0 30 N=1, 191 120 600 Days 60 N=1, 855 N=361 N=6, 058
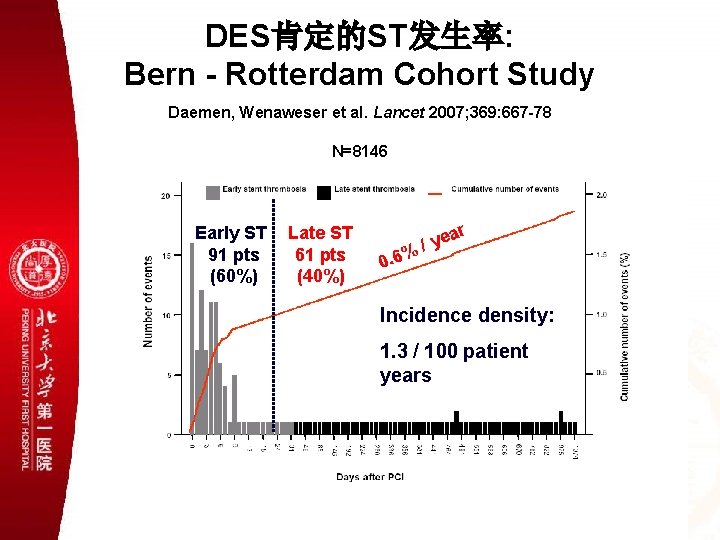
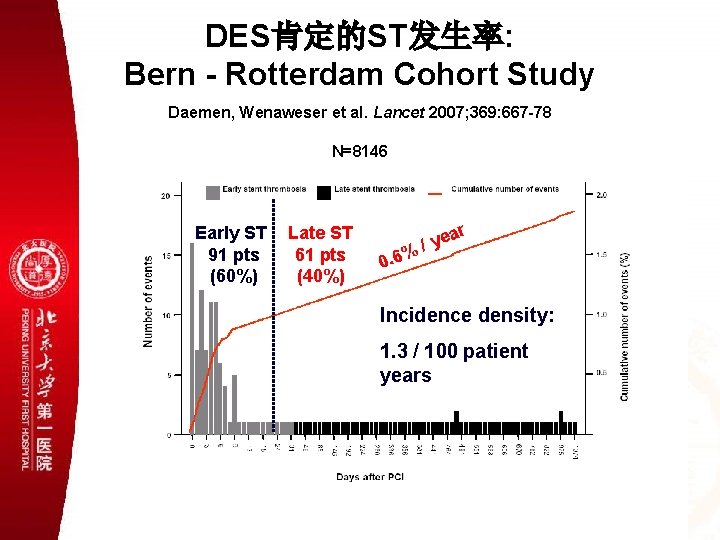
DES肯定的ST发生率: Bern - Rotterdam Cohort Study Daemen, Wenaweser et al. Lancet 2007; 369: 667 -78 N=8146 Early ST 91 pts (60%) Late ST 61 pts (40%) ar ye %/ 0. 6 Incidence density: 1. 3 / 100 patient years
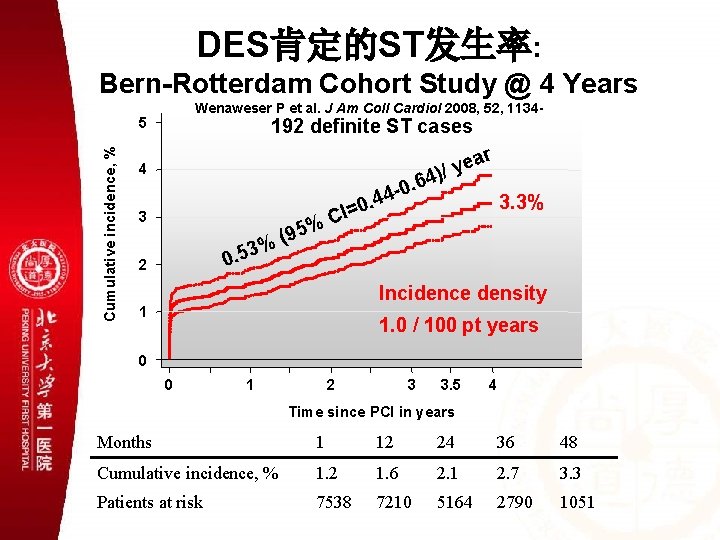
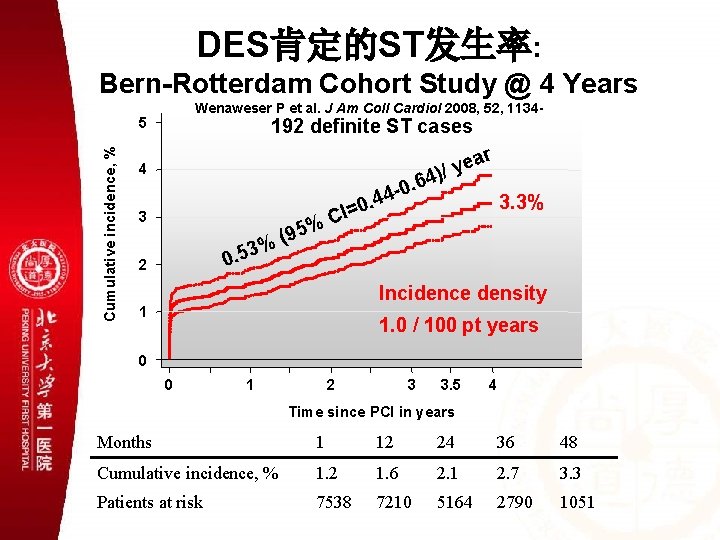
DES肯定的ST发生率: Bern-Rotterdam Cohort Study @ 4 Years Wenaweser P et al. J Am Coll Cardiol 2008, 52, 1134 - Cumulative incidence, % 5 192 definite ST cases 4 0. 6 4 4 ea y / ) r 4 . 3 95 ( % % 0 CI= 3. 3% 3 0. 5 2 Incidence density 1 1. 0 / 100 pt years 0 0 1 2 3 3. 5 4 Time since PCI in years Months 1 12 24 36 48 Cumulative incidence, % 1. 2 1. 6 2. 1 2. 7 3. 3 Patients at risk 7538 7210 5164 2790 1051
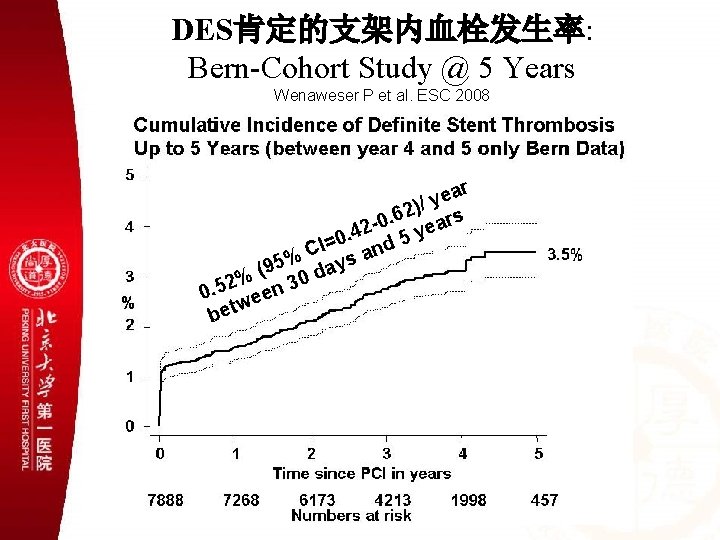
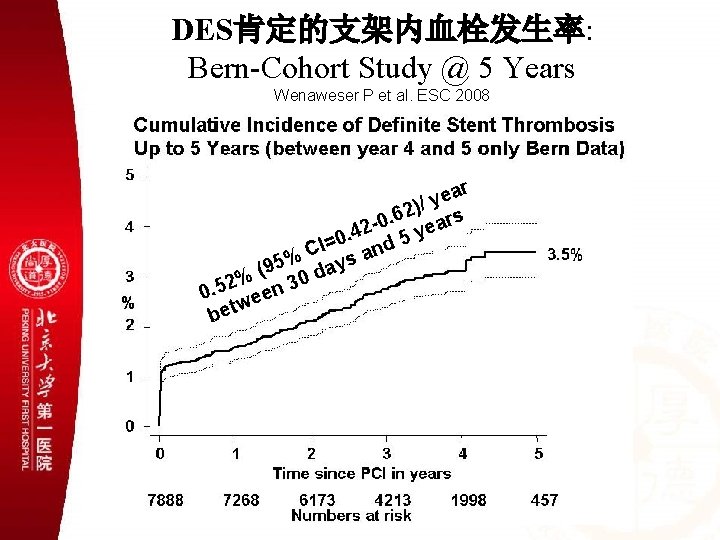
DES肯定的支架内血栓发生率: Bern-Cohort Study @ 5 Years Wenaweser P et al. ESC 2008 ar e y )/ 2 6 rs 0. a 2 e y. 4 0 5 = CI s and % 95 day ( 2% n 30 5. 0 ee w t be
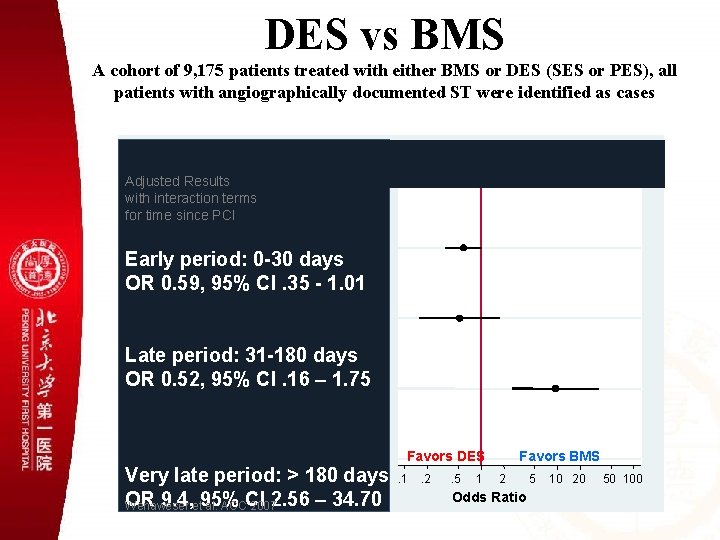
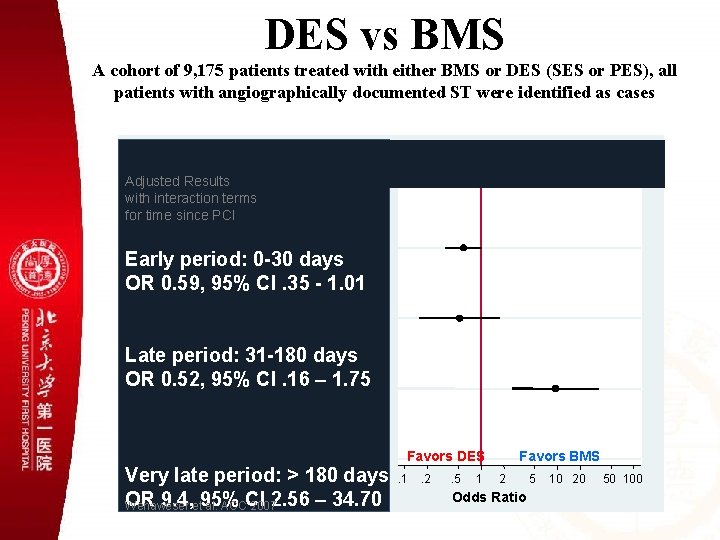
DES vs BMS A cohort of 9, 175 patients treated with either BMS or DES (SES or PES), all patients with angiographically documented ST were identified as cases Time after PCI >180 days 31 -180 days 0 -30 days Adjusted Results with interaction terms for time since PCI Early period: 0 -30 days OR 0. 59, 95% CI. 35 - 1. 01 Late period: 31 -180 days OR 0. 52, 95% CI. 16 – 1. 75 Favours DES Favours BMS Very. 1 late days. 2. 5 period: 1 2 5 >10180 20 50 100 Odds Ratio OR 9. 4, et 95% Wenaweser al. ACCCI 20072. 56 – 34. 70 Favors DES. 1 . 2 . 5 1 Favors BMS 2 Odds Ratio 5 10 20 50 100
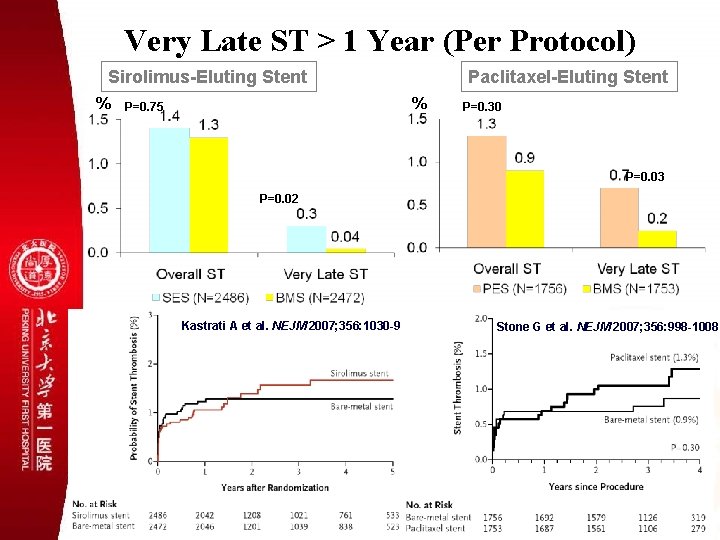
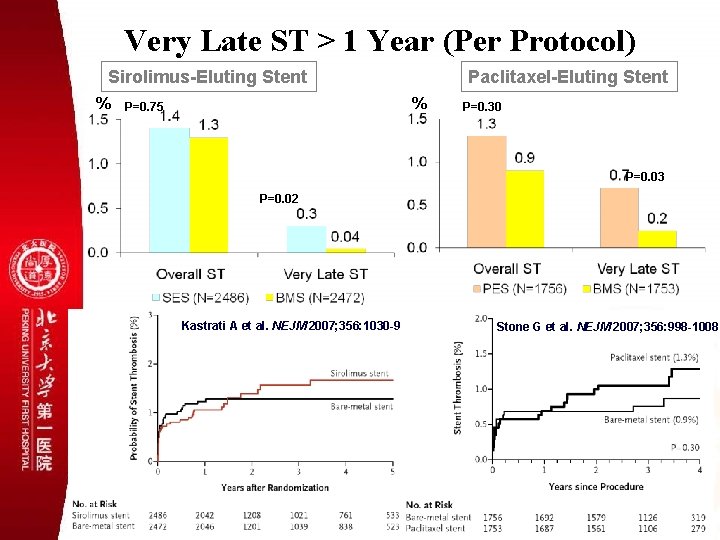
Very Late ST > 1 Year (Per Protocol) Sirolimus-Eluting Stent % Paclitaxel-Eluting Stent % P=0. 75 P=0. 30 P=0. 03 P=0. 02 Kastrati A et al. NEJM 2007; 356: 1030 -9 Stone G et al. NEJM 2007; 356: 998 -1008
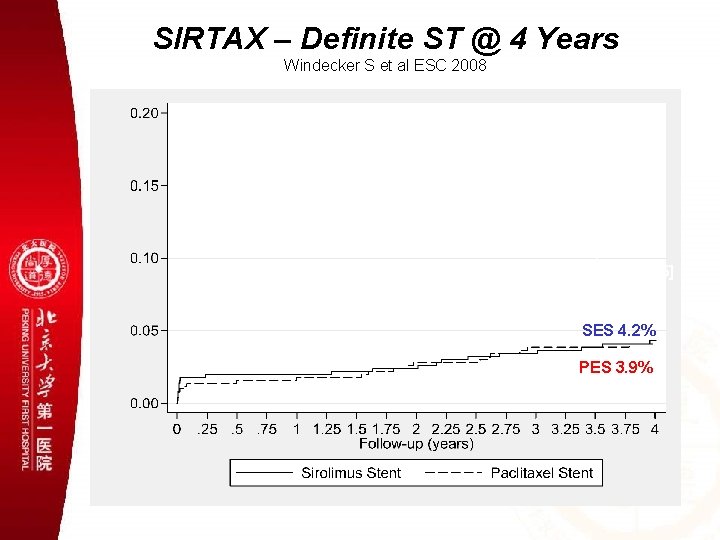
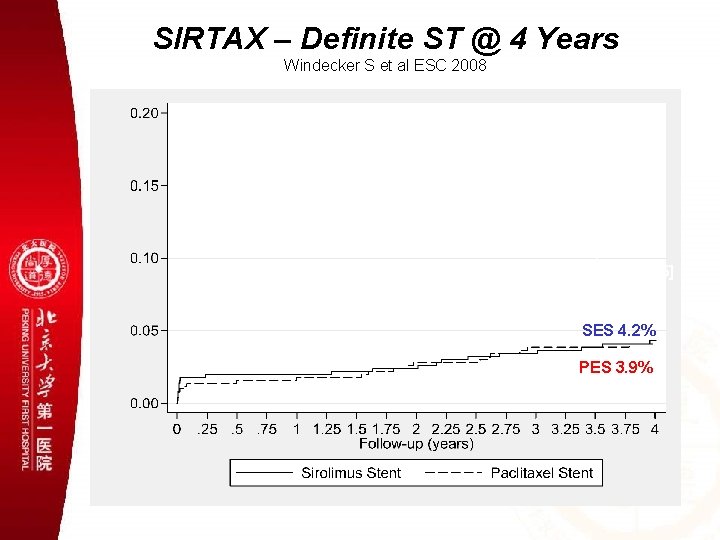
SIRTAX – Definite ST @ 4 Years Windecker S et al ESC 2008 4 -year HR 3 -year HR 1. 06 [0. 57, 1. 95] 2 -year HR 0. 90 [0. 47, 1. 73] P = 0. 86 1 -year HR 0. 86 [0. 40, 1. 87] P = 0. 75 1. 12 [0. 46, 2. 76] P = 0. 71 SES 4. 2% P = 0. 01 3. 7% 2. 8% PES 3. 9% 2. 0% 3. 4% 2. 4% 1. 8%
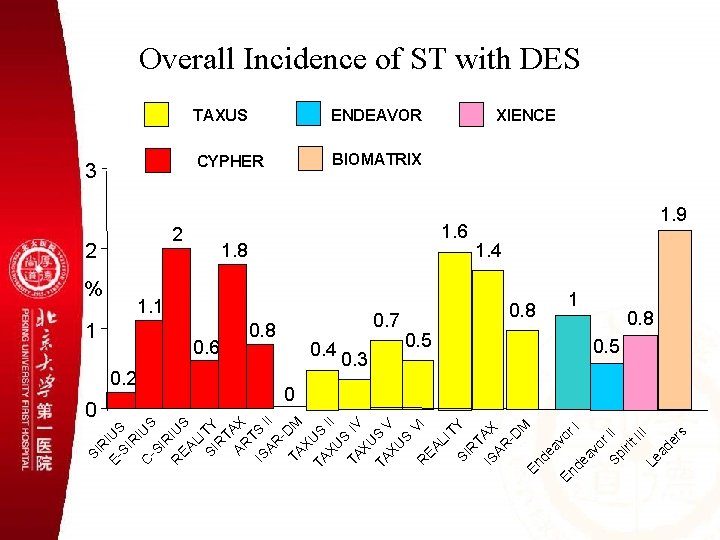
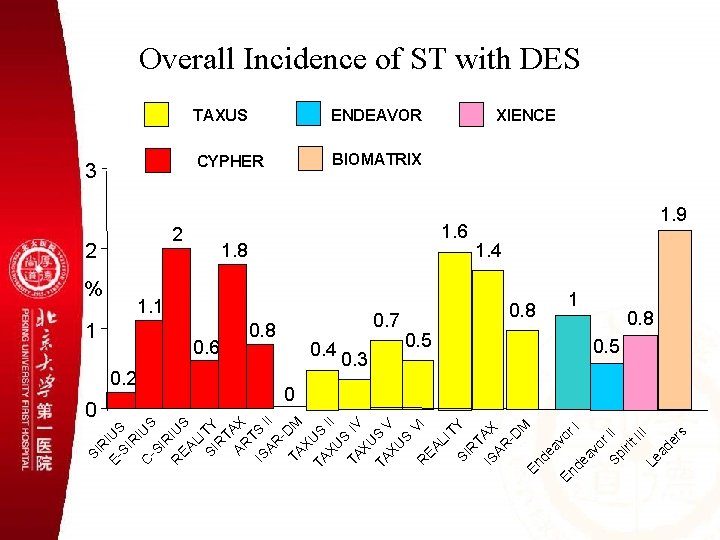
SI R E- IUS SI R C IUS -S IR R IUS EA LI SI TY R T AR AX T IS S AR II TA DM X TA US XU II S TA IV XU TA S XU V S V R EA I LI TY SI R T IS AX AR -D M En de av or En I de av or Sp II iri t. I II Le ad er s Overall Incidence of ST with DES 3 2 % 1 0. 2 0 TAXUS ENDEAVOR CYPHER BIOMATRIX 2 1. 8 1. 1 0. 6 0. 8 0. 7 0. 4 0. 3 0. 5 XIENCE 1. 6 1. 9 1. 4 0. 8 1 0. 8 0. 5 0
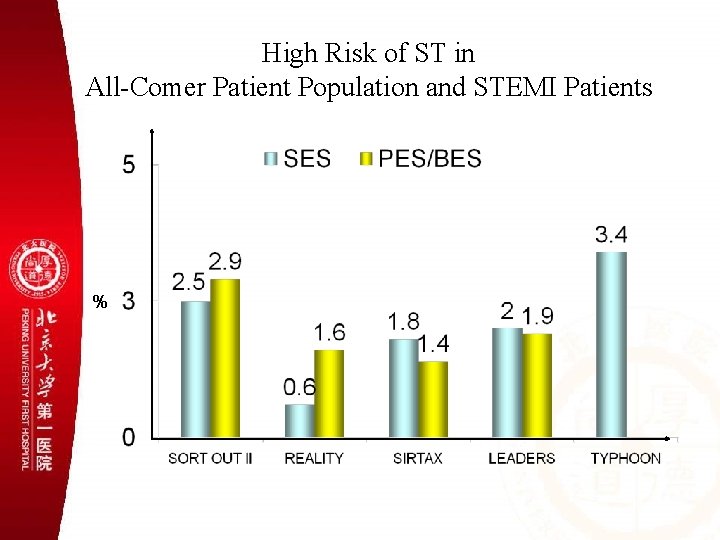
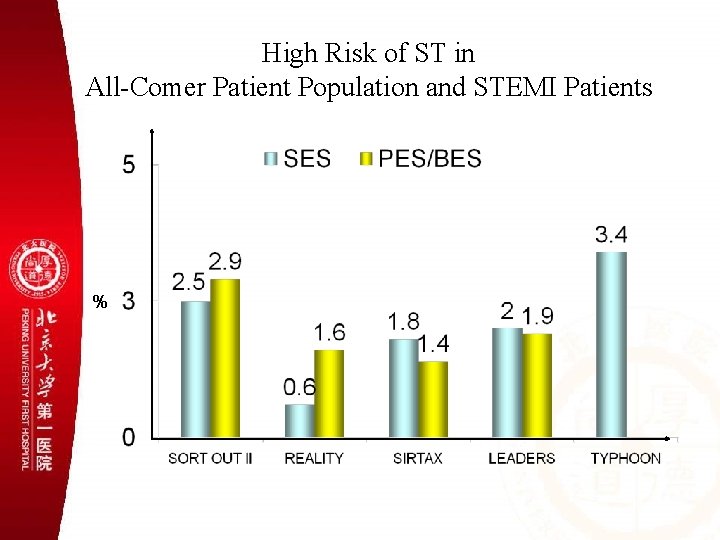
High Risk of ST in All-Comer Patient Population and STEMI Patients %
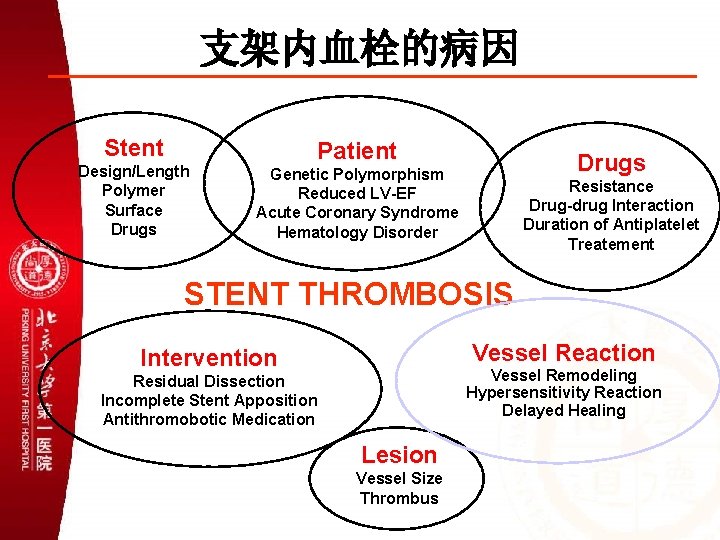
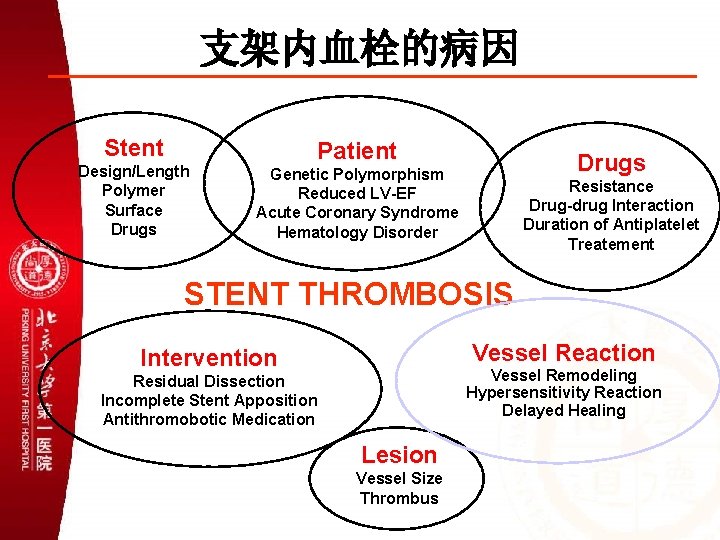
支架内血栓的病因 Stent Design/Length Polymer Surface Drugs Patient Drugs Genetic Polymorphism Reduced LV-EF Acute Coronary Syndrome Hematology Disorder Resistance Drug-drug Interaction Duration of Antiplatelet Treatement STENT THROMBOSIS Vessel Reaction Intervention Vessel Remodeling Hypersensitivity Reaction Delayed Healing Residual Dissection Incomplete Stent Apposition Antithromobotic Medication Lesion Vessel Size Thrombus

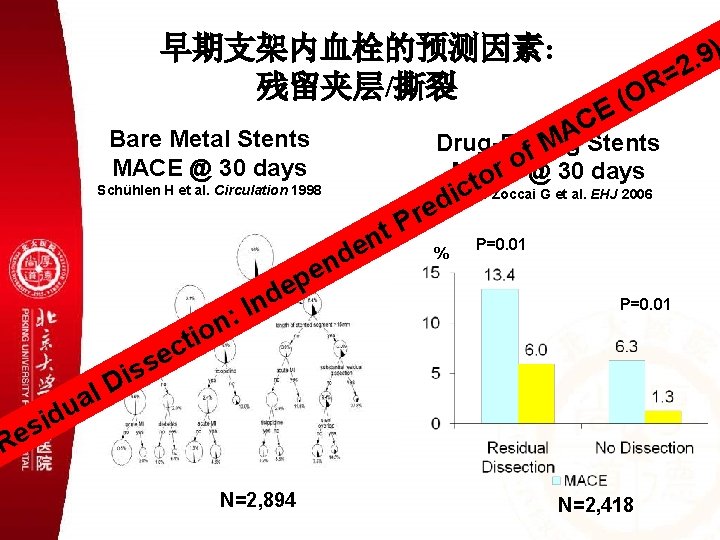
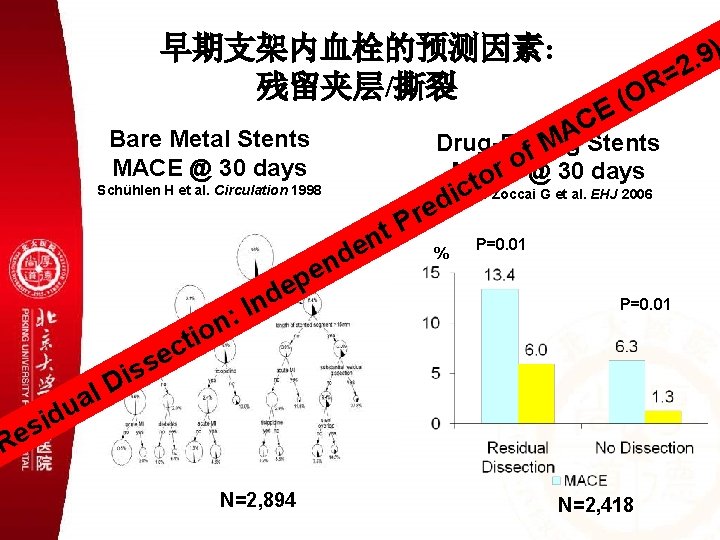
早期支架内血栓的预测因素: 残留夹层/撕裂 t c i red Schühlen H et al. Circulation 1998 Biondi-Zoccai G et al. EHJ 2006 P t n e d n e ep l a u s s i D ( E C A Stents Drug-Eluting M f o MACE or @ 30 days Bare Metal Stents MACE @ 30 days d n I : n io ) 9. 2 = OR % P=0. 01 t c e id s e R N=2, 894 N=2, 418
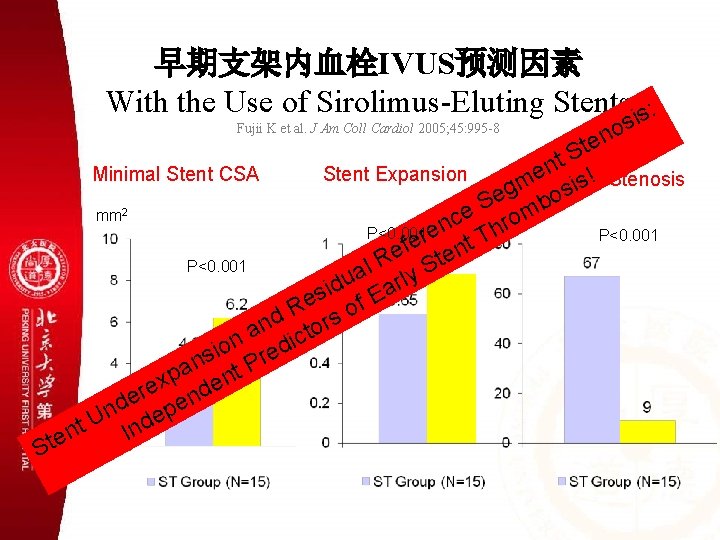
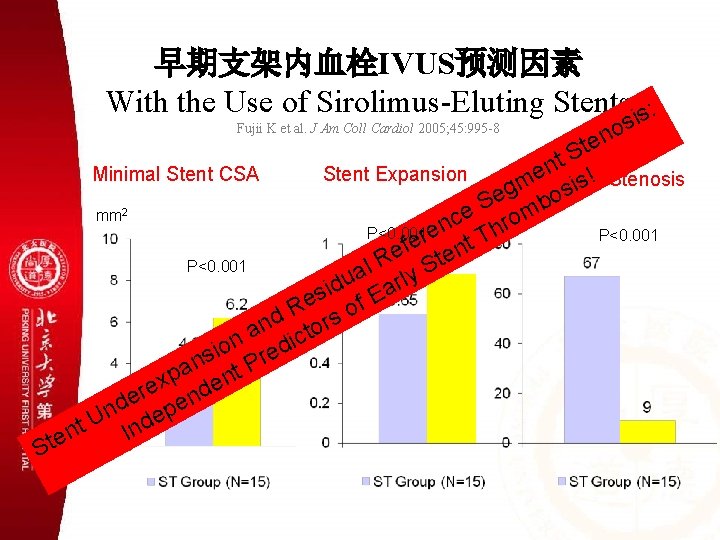
早期支架内血栓IVUS预测因素 With the Use of Sirolimus-Eluting Stents is: Fujii K et al. J Am Coll Cardiol 2005; 45: 995 -8 s o n te S t n Minimal Stent CSA Stent Expansion e ! Stenosis Residual s m i eg bos S mm 2 e % rom c n h P<0. 001 re P<0. 001 T e t f e ten R P<0. 001 al rly S u id Ea s e of R nd tors a ic n d o i s Pre n pa ent x re nd epe U d t n n I Ste
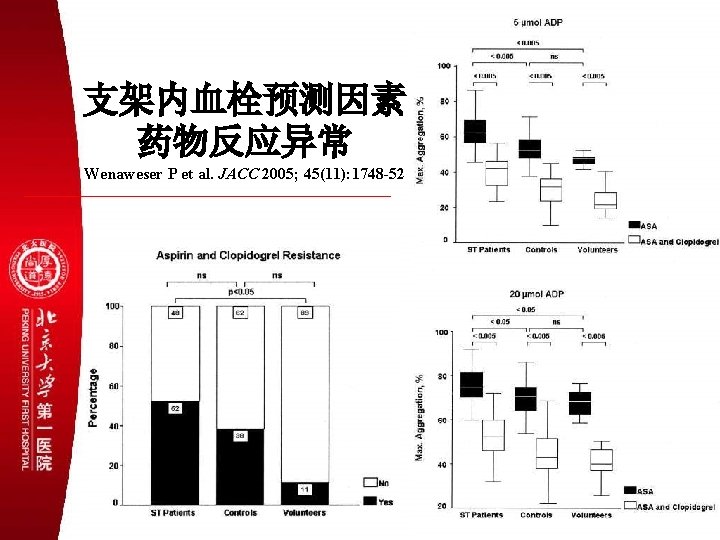
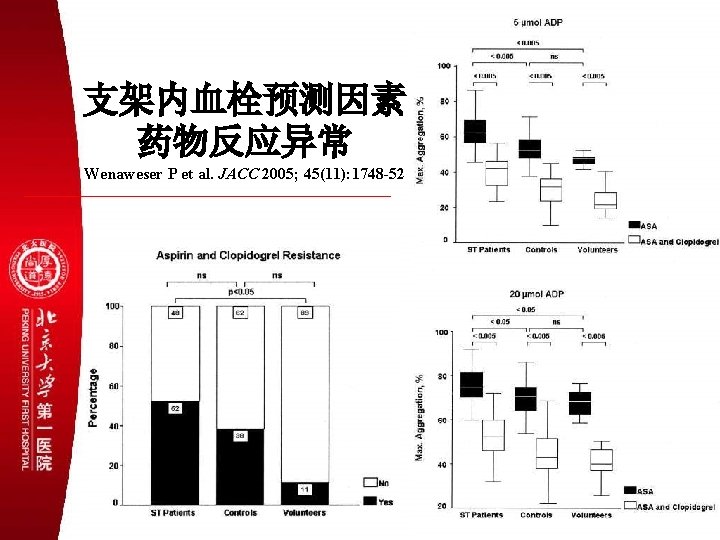
支架内血栓预测因素 药物反应异常 Wenaweser P et al. JACC 2005; 45(11): 1748 -52
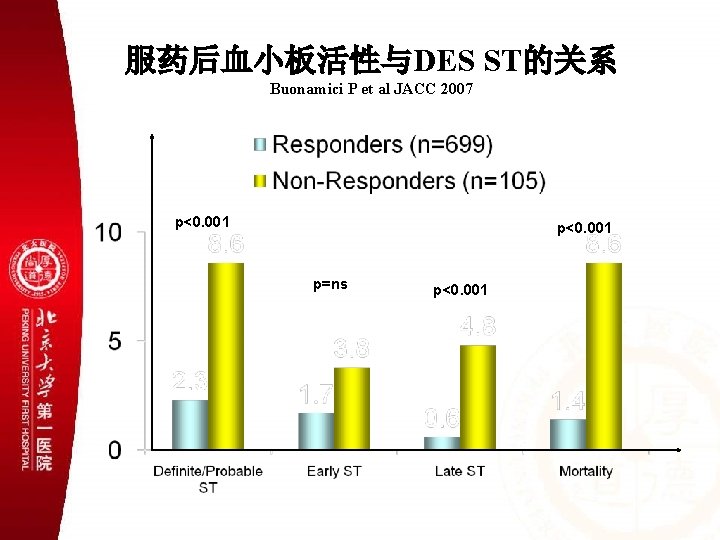
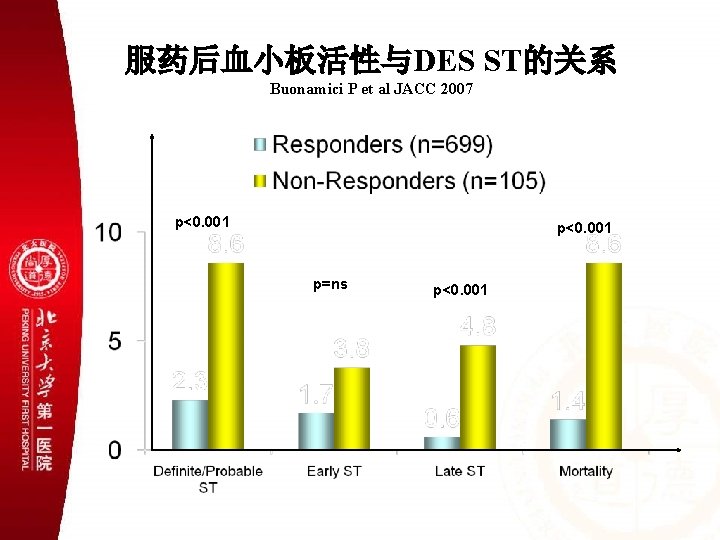
服药后血小板活性与DES ST的关系 Buonamici P et al JACC 2007 p<0. 001 p=ns p<0. 001
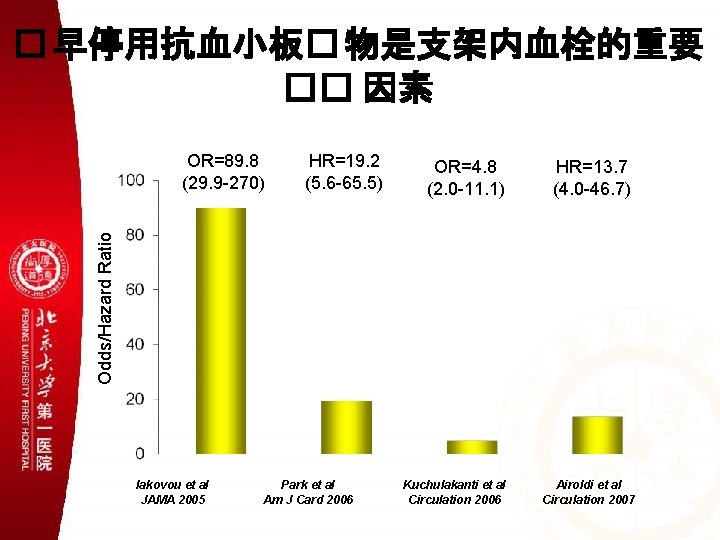
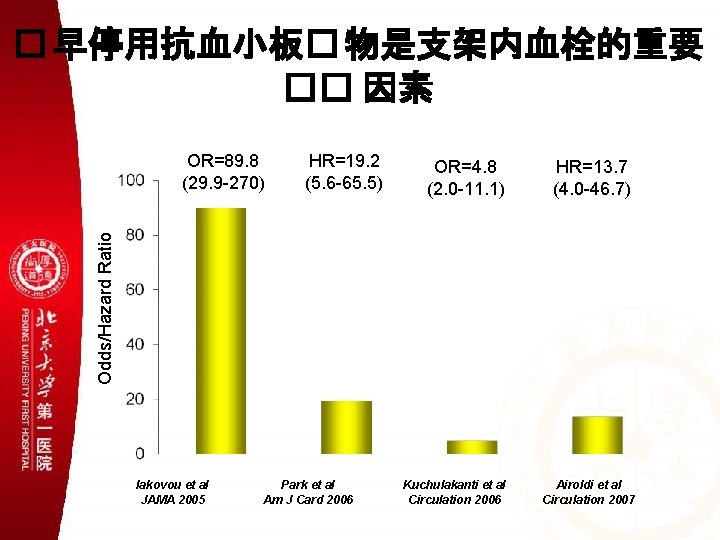
� 早停用抗血小板� 物是支架内血栓的重要 �� 因素 HR=19. 2 (5. 6 -65. 5) OR=4. 8 (2. 0 -11. 1) HR=13. 7 (4. 0 -46. 7) Odds/Hazard Ratio OR=89. 8 (29. 9 -270) Iakovou et al JAMA 2005 Park et al Am J Card 2006 Kuchulakanti et al Circulation 2006 Airoldi et al Circulation 2007
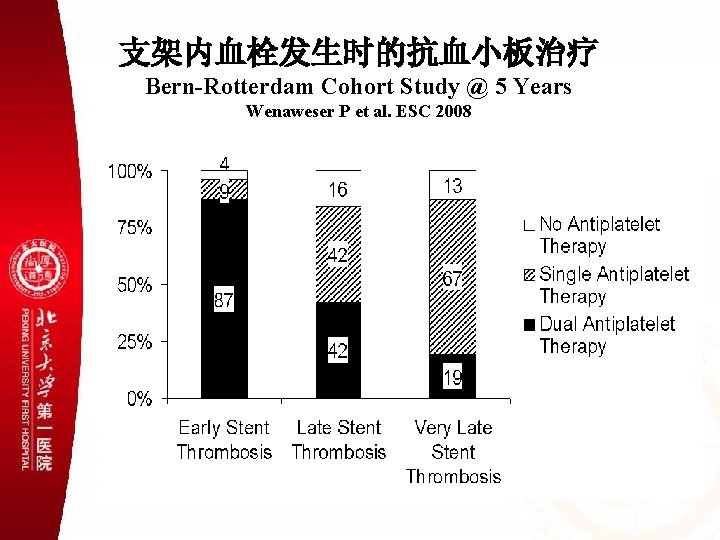
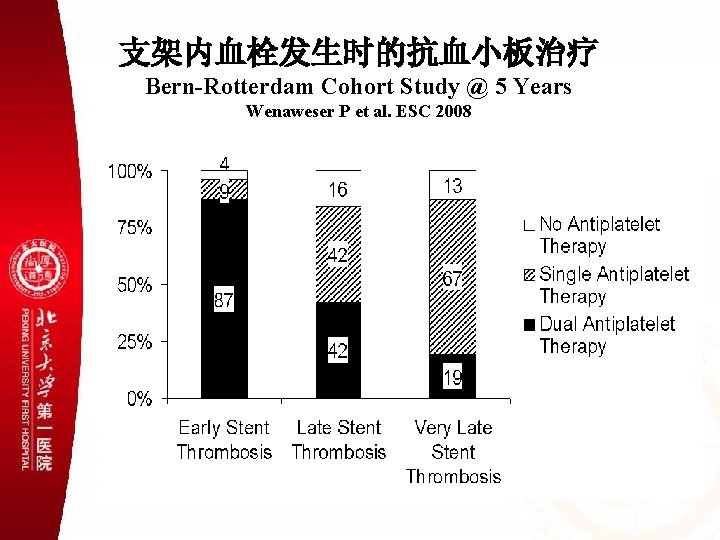
支架内血栓发生时的抗血小板治疗 Bern-Rotterdam Cohort Study @ 5 Years Wenaweser P et al. ESC 2008
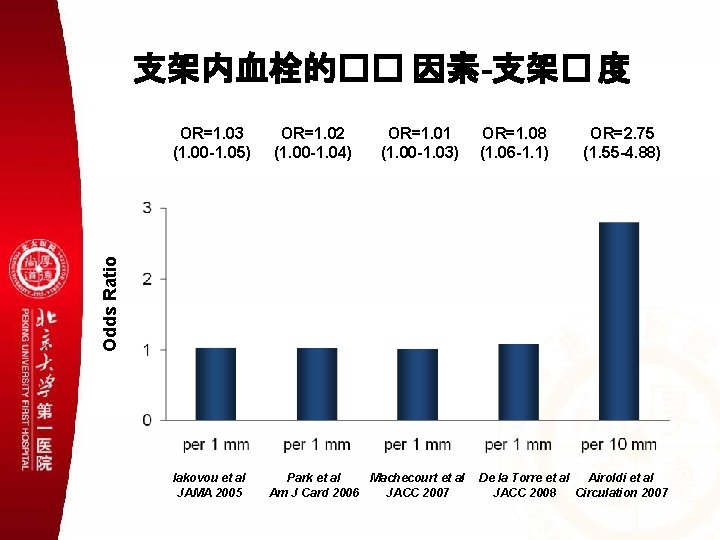
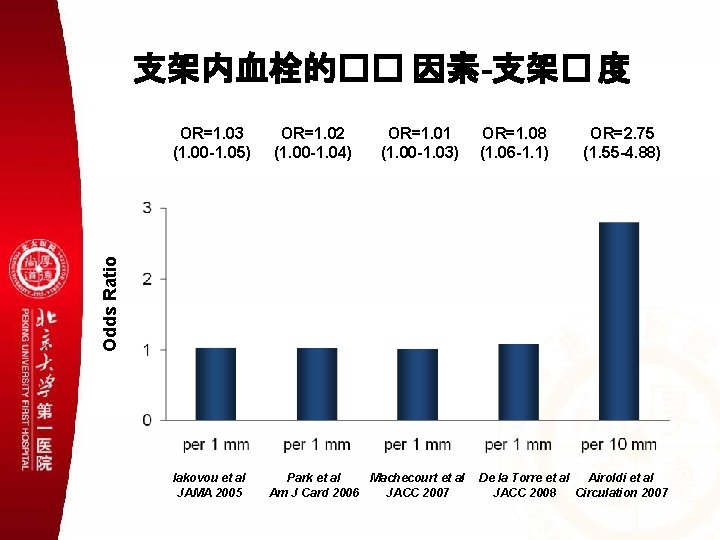
支架内血栓的�� 因素-支架� 度 OR=1. 02 (1. 00 -1. 04) OR=1. 01 (1. 00 -1. 03) OR=1. 08 (1. 06 -1. 1) OR=2. 75 (1. 55 -4. 88) Odds Ratio OR=1. 03 (1. 00 -1. 05) Iakovou et al JAMA 2005 Park et al Machecourt et al Am J Card 2006 JACC 2007 De la Torre et al Airoldi et al JACC 2008 Circulation 2007
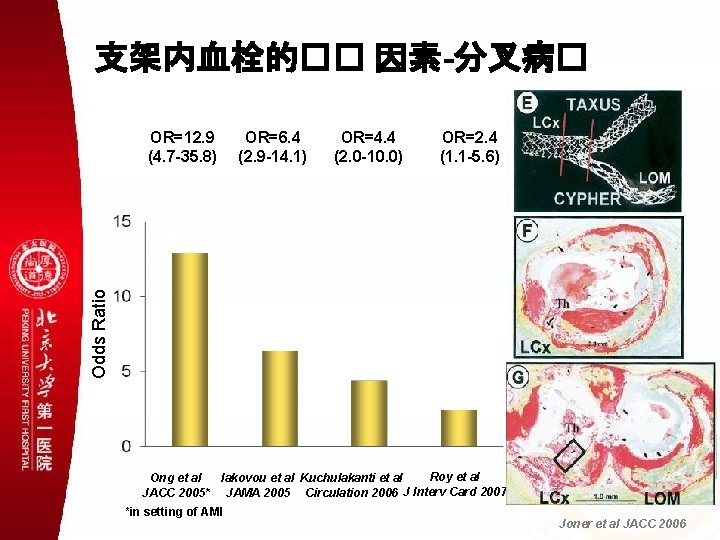
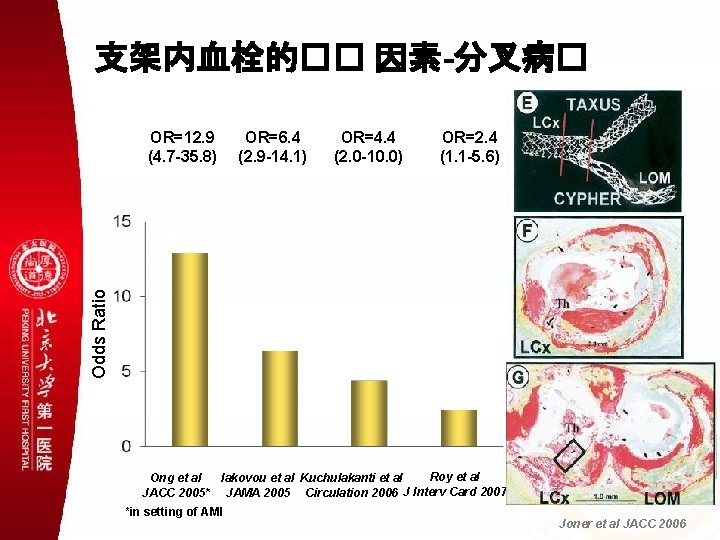
支架内血栓的�� 因素-分叉病� OR=6. 4 (2. 9 -14. 1) OR=4. 4 (2. 0 -10. 0) OR=2. 4 (1. 1 -5. 6) Odds Ratio OR=12. 9 (4. 7 -35. 8) Roy et al Ong et al Iakovou et al Kuchulakanti et al J Interv Card 2007 JACC 2005* JAMA 2005 Circulation 2006 *in setting of AMI Joner et al JACC 2006
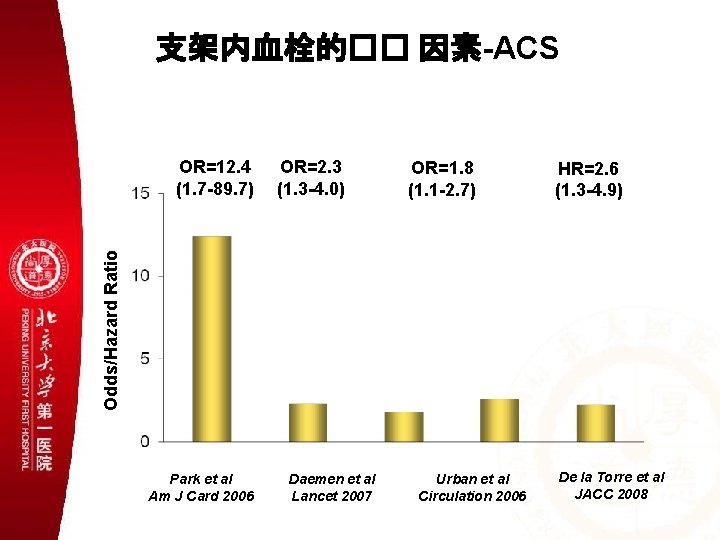
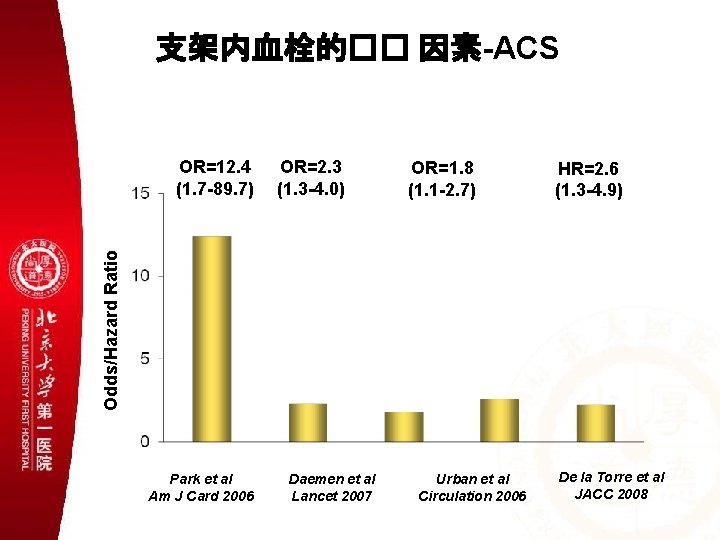
支架内血栓的�� 因素-ACS OR=2. 3 (1. 3 -4. 0) OR=1. 8 (1. 1 -2. 7) HR=2. 6 (1. 3 -4. 9) Odds/Hazard Ratio OR=12. 4 (1. 7 -89. 7) Park et al Am J Card 2006 Daemen et al Lancet 2007 Urban et al Circulation 2006 De la Torre et al JACC 2008
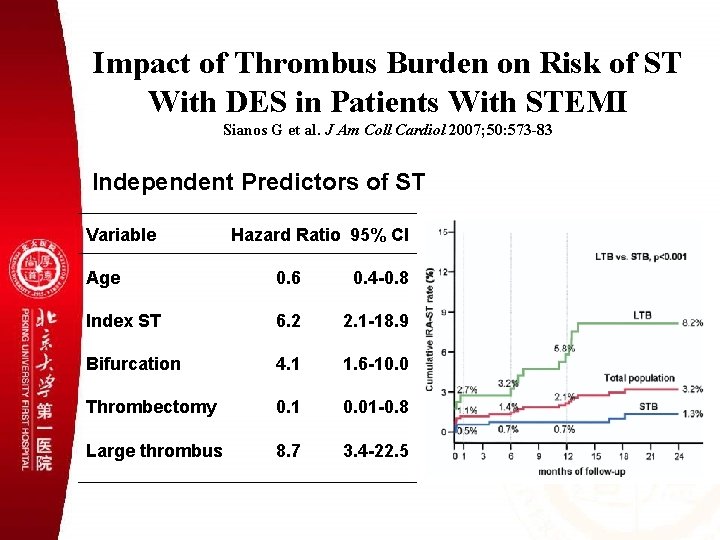
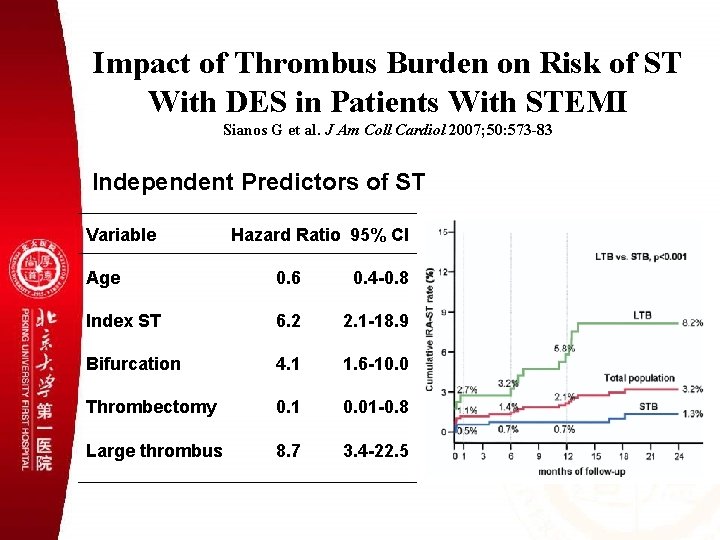
Impact of Thrombus Burden on Risk of ST With DES in Patients With STEMI Sianos G et al. J Am Coll Cardiol 2007; 50: 573 -83 Independent Predictors of ST Variable Hazard Ratio 95% CI Age 0. 6 0. 4 -0. 8 Index ST 6. 2 2. 1 -18. 9 Bifurcation 4. 1 1. 6 -10. 0 Thrombectomy 0. 1 0. 01 -0. 8 Large thrombus 8. 7 3. 4 -22. 5
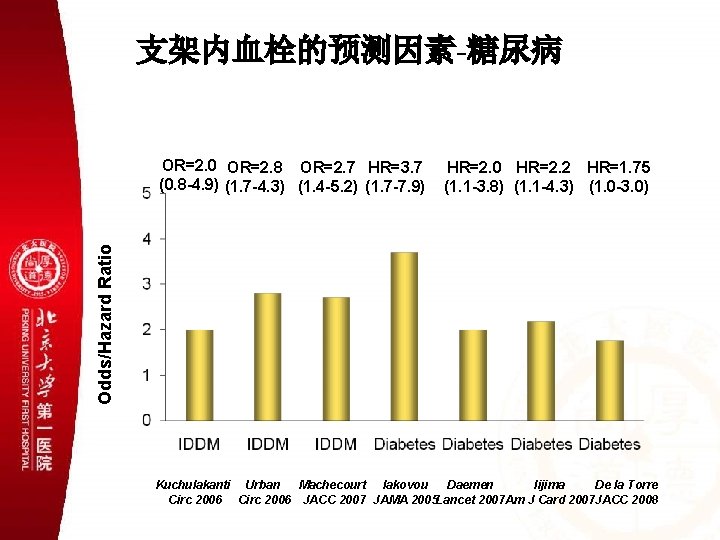
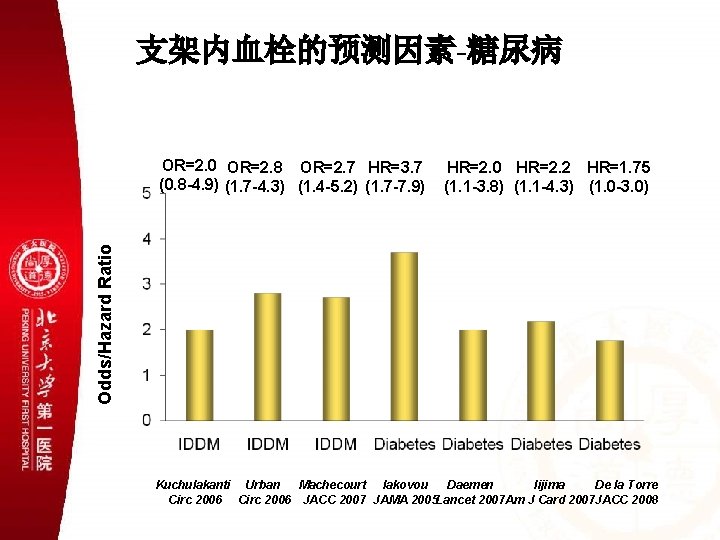
支架内血栓的预测因素-糖尿病 HR=2. 0 HR=2. 2 HR=1. 75 (1. 1 -3. 8) (1. 1 -4. 3) (1. 0 -3. 0) Odds/Hazard Ratio OR=2. 0 OR=2. 8 OR=2. 7 HR=3. 7 (0. 8 -4. 9) (1. 7 -4. 3) (1. 4 -5. 2) (1. 7 -7. 9) Kuchulakanti Urban Machecourt Iakovou Daemen Iijima De la Torre Circ 2006 JACC 2007 JAMA 2005 Lancet 2007 Am J Card 2007 JACC 2008
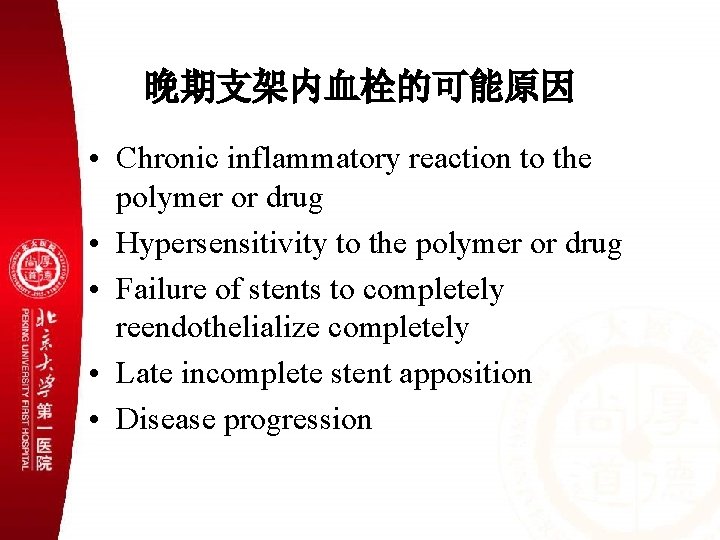
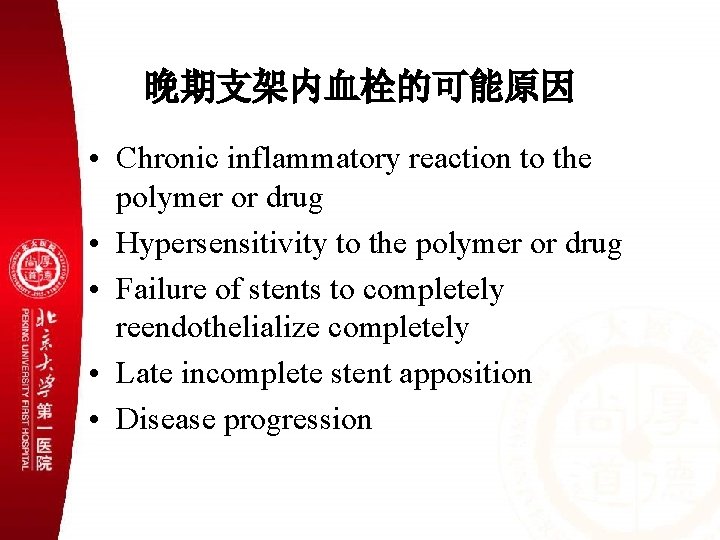
晚期支架内血栓的可能原因 • Chronic inflammatory reaction to the polymer or drug • Hypersensitivity to the polymer or drug • Failure of stents to completely reendothelialize completely • Late incomplete stent apposition • Disease progression
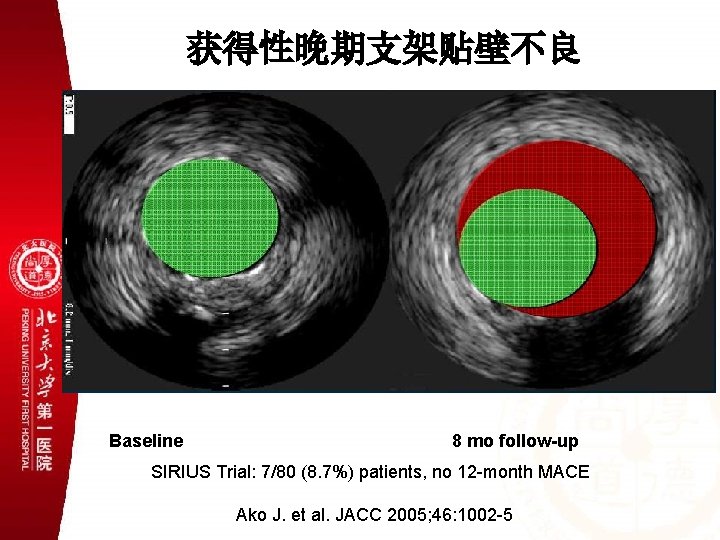
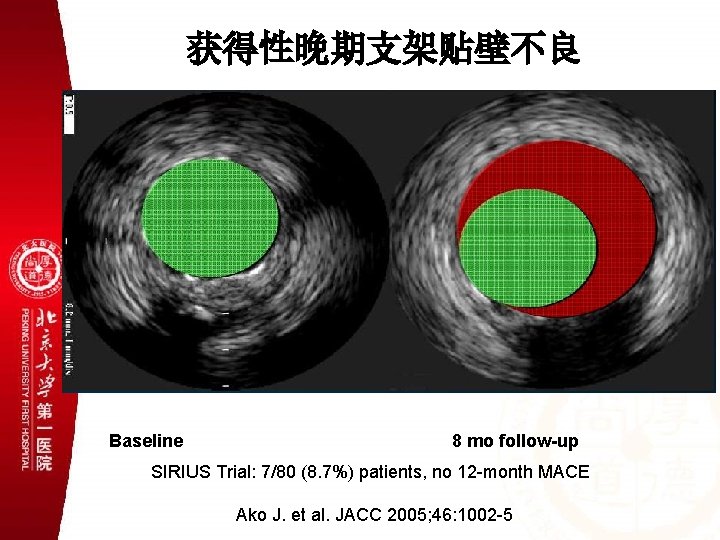
获得性晚期支架贴壁不良 Baseline 8 mo follow-up SIRIUS Trial: 7/80 (8. 7%) patients, no 12 -month MACE Ako J. et al. JACC 2005; 46: 1002 -5
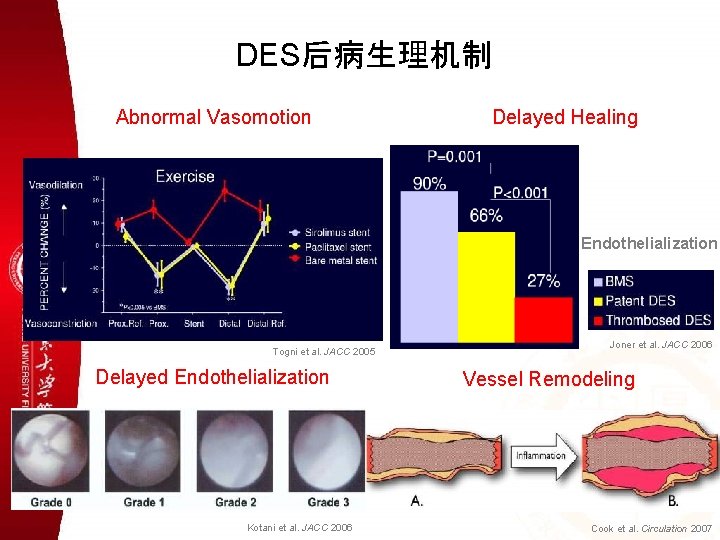
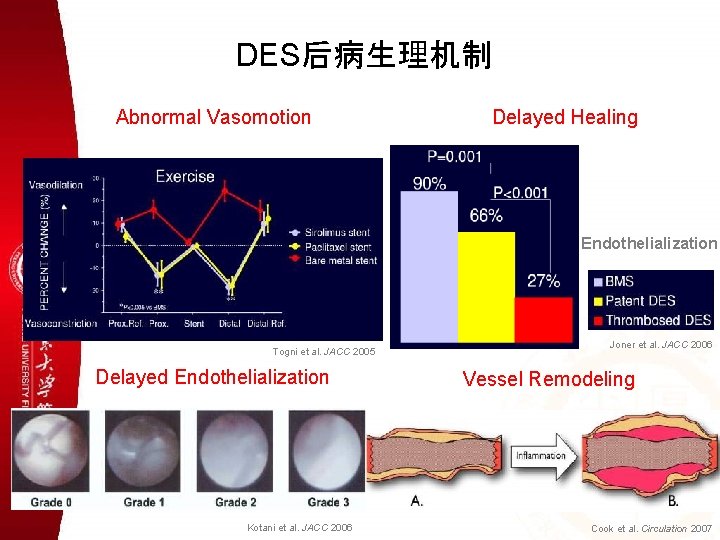
DES后病生理机制 Abnormal Vasomotion Delayed Healing Endothelialization Togni et al. JACC 2005 Delayed Endothelialization Kotani et al. JACC 2006 Joner et al. JACC 2006 Vessel Remodeling Cook et al. Circulation 2007

FDA DES Panel Meeting 专家共识 ØThere is an increase in “very late” (>1 yr) stent thrombosis associated with current DES • ~2 -4 per 1000 pts per year (? continous hazard, ? patient and lesion predictors) • Data from multiple sources indicate that DES are associated with delayed healing responses and increased inflammation • The causes of late DES thrombosis are multifactorial; device, procedural, and patient factors (often multiple = perfect storm)
FDA DES Panel Meeting 专家共识 • There may be a link between post-DES reduced neo-intimal hyperplasia (late loss) and delayed late healing responses which contributes to late stent thrombosis • DES stent thrombosis is highly definition dependent; need for revised standardized definitions and adjudication methods (ARC) to facilitate inter-study comparisons
专家共识 Ø“Off-label DES use – increased incidence of late DES thrombosis and death/MI cw “on-label”, but inadequate controls; results inconsistent! • Few RCTs (underpowered); FDA sanctioned registries = insufficient sample size and FU, represents major data gap and source of concern • Large population studies (SCAAR) fraught with methodologic flaws (e. g. risk adjustment issues)

专家共识 ØDuration of dual anti-platelet therapy should extend beyond the present product labels • One year is reasonable compromise (esp. for “off-label” DES use) • Must balance against the increased risk of bleeding with dual anti-platelet therapy • Additional studies immediately required to better clarify optimal anti-platelet therapy
专家共识 ØAssess patient and lesion characteristics to establish restenosis risk profile • Determine relative value of DES vs. BMS in every patient (no more “unrestricted” use) • Consider both on-label and off-label situations (ironically, off-label use scenarios may be more compelling) • Increased restenosis risk = favor DES • Increased safety concerns = favor No DES
专家共识 ØAssess patient factors which may preclude long term (at least one year) dual AP therapy • • • Planned or possible intercurrent surgery Bleeding Hx or tendencies Other concomitant medications (e. g. coumadin) • Socio-economic factors which may affect Plavix compliance
专家共识 ØConsider alternatives to DES, if risk-benefit assessments prove unfavorable • CABG – unprotected LM disease, complex MVD (esp. diabetics), recurrent ISR (esp. VBT) • BMS – Plavix dependence concerns, large (>4 mm diameter) vessels, ? AMI pts, ? low restenosis risk lesions • Balloon PCI – sidebranch in bifurcations (provisional stent only), small vessels in distal locations
专家共识 ØOptimize DES implantation techniques • Adequate lesion preparation (pre-dilatation) • High pressure implantation methodologies (like previous BMS strategies) • Avoid undersizing and inflow/outflow obstruction (mod stenoses or dissections) • Implant stent edges into normal references segments • Consider IVUS guidance (esp. LAD)
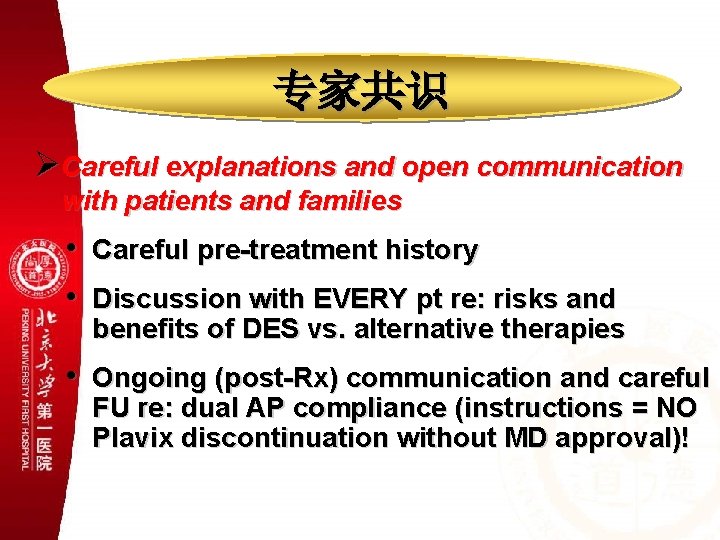
专家共识 ØCareful explanations and open communication with patients and families • • Careful pre-treatment history Discussion with EVERY pt re: risks and benefits of DES vs. alternative therapies • Ongoing (post-Rx) communication and careful FU re: dual AP compliance (instructions = NO Plavix discontinuation without MD approval)!

 Acute coronary syndrome
Acute coronary syndrome Global registry of acute coronary events
Global registry of acute coronary events Coronary steal
Coronary steal Classification of antianginal drugs
Classification of antianginal drugs Angiographic equipment
Angiographic equipment Angiography equipment list
Angiography equipment list Mentoring circle
Mentoring circle Minar arc
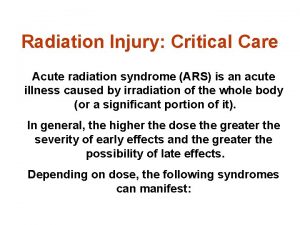
Minar arc Acute radiation syndrome
Acute radiation syndrome Firas mussa md
Firas mussa md Arc promoteur vs arc investigateur
Arc promoteur vs arc investigateur Arc emu88 com arc info 09 100009 html
Arc emu88 com arc info 09 100009 html Subacromial bursitis
Subacromial bursitis Subacromial space
Subacromial space Holy orders matter
Holy orders matter In the poem watch me grow to what is reading compared
In the poem watch me grow to what is reading compared Fossa ovalis
Fossa ovalis Heart sounds location
Heart sounds location Coronary personality
Coronary personality Sinus of venae cavae
Sinus of venae cavae Ali sepahdari
Ali sepahdari Cardiac plexus
Cardiac plexus Coronary artery disease
Coronary artery disease Cpr routine
Cpr routine Anterior aortic sinus
Anterior aortic sinus Good morning blood
Good morning blood Annulus of vieussens
Annulus of vieussens Pk papyrus covered coronary stent system
Pk papyrus covered coronary stent system Flow of coronary circulation
Flow of coronary circulation Unlocking of knee joint
Unlocking of knee joint Coronary blood flow
Coronary blood flow Anemia or hypoproteinemia will ______ blood viscosity.
Anemia or hypoproteinemia will ______ blood viscosity. Coronary artery disease pathophysiology
Coronary artery disease pathophysiology Mesa coronary calcium score
Mesa coronary calcium score Ischemic heart disease
Ischemic heart disease Circulatory system crash course
Circulatory system crash course Cardiac output animation
Cardiac output animation Coronary circulation of heart
Coronary circulation of heart Where is the pulmonary semilunar valve located
Where is the pulmonary semilunar valve located Mesa coronary calcium score
Mesa coronary calcium score Coronary heart disease
Coronary heart disease Cag spider view
Cag spider view