Anesthesia and Moderate Sedation Logman mohammed alshaikh Overview

- Slides: 50
Anesthesia and Moderate Sedation Logman mohammed alshaikh
Overview • Anesthesia is a state of depressed CNS activity, marked by depression of consciousness, loss of responsiveness to stimulation, and/or muscle relaxation.
Overview Anesthesia is classified as general or local. General anesthesia causes loss of sensation, consciousness, and reflexes. It is the method used when a client is undergoing major surgery, or one that will require complete muscle relaxation. Local anesthesia causes loss of sensation without loss of consciousness. Local anesthetics block transmission along nerves. In turn, this provides for loss of autonomic function and muscle paralysis in a specific area of the body.
General Anesthesia The phases of general anesthesia are Induction – IV lines initiated, preoperative medications given, airway secured Maintenance – surgery performed, airway maintenance Emergence – surgery completed, removal of assistive airway devices
cont • Anesthetics used during general anesthesia are classified as either injectable or inhaled. Inhaled anesthetics are volatile gases or liquids that are dissolved in oxygen. Injectable anesthetics are given intravenously (IV).
cont - Examples of inhalation anesthetic agents include halothane (Fluothane), isoflurane (Forane), and nitrous oxide in combination with oxygen. Examples of IV anesthetic agents include benzodiazepines, etomidate (Amidate), propofol (Diprivan), ketamine (Ketalar), and short-acting barbiturates such as methohexital (Brevital) and thiopental (pentothal).
cont ■ Propofol is the most commonly used anesthetic agent. ■ Propofol can be used while clients are on mechanical ventilation, during radiation therapy, and having a diagnostic procedure. ■ Do not administer propofol if client has an allergy to eggs or soybean oil.
cont Inhalation anesthetics are eliminated predominantly through exhalation. The rate of elimination depends upon pulmonary ventilation and blood flow to the lungs. Postoperative administration of oxygen and encouraging the client to take deep breaths are important interventions.
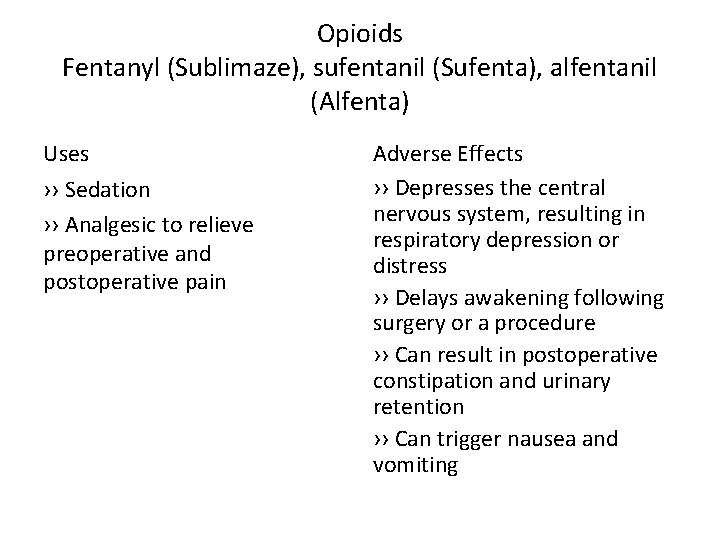
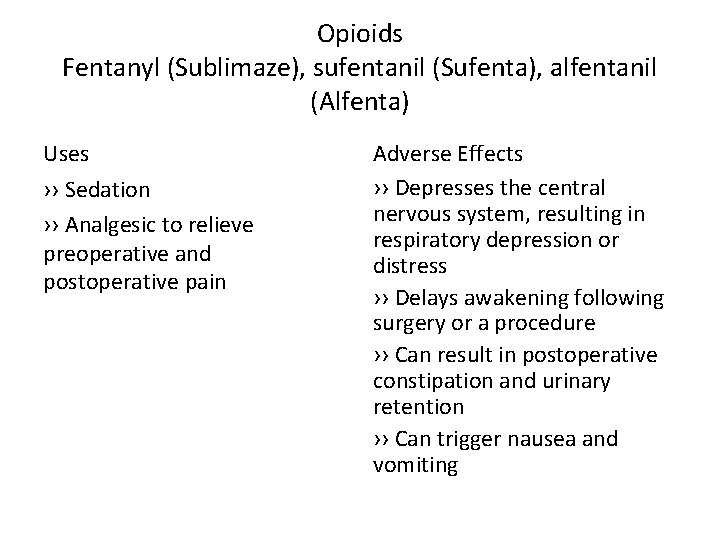
Opioids Fentanyl (Sublimaze), sufentanil (Sufenta), alfentanil (Alfenta) Uses ›› Sedation ›› Analgesic to relieve preoperative and postoperative pain Adverse Effects ›› Depresses the central nervous system, resulting in respiratory depression or distress ›› Delays awakening following surgery or a procedure ›› Can result in postoperative constipation and urinary retention ›› Can trigger nausea and vomiting
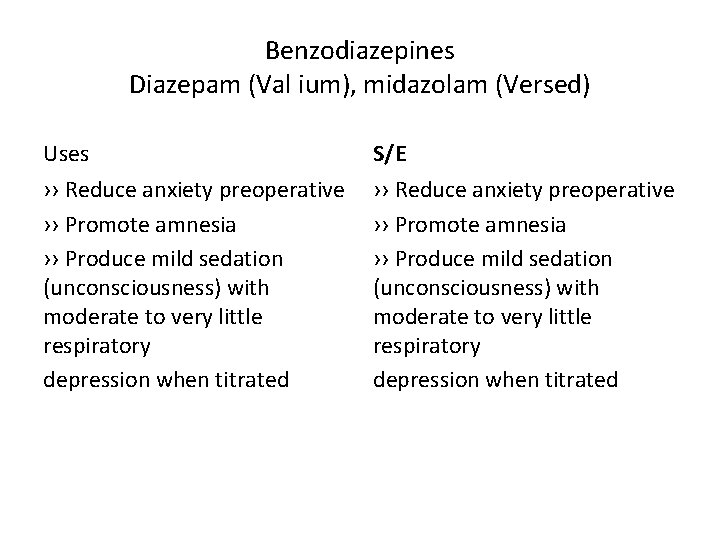
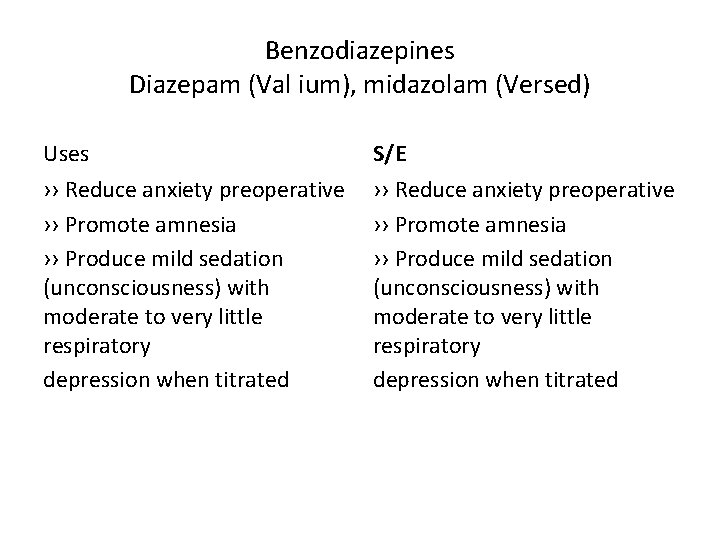
Benzodiazepines Diazepam (Val ium), midazolam (Versed) Uses S/E ›› Reduce anxiety preoperative ›› Promote amnesia ›› Produce mild sedation (unconsciousness) with moderate to very little respiratory depression when titrated
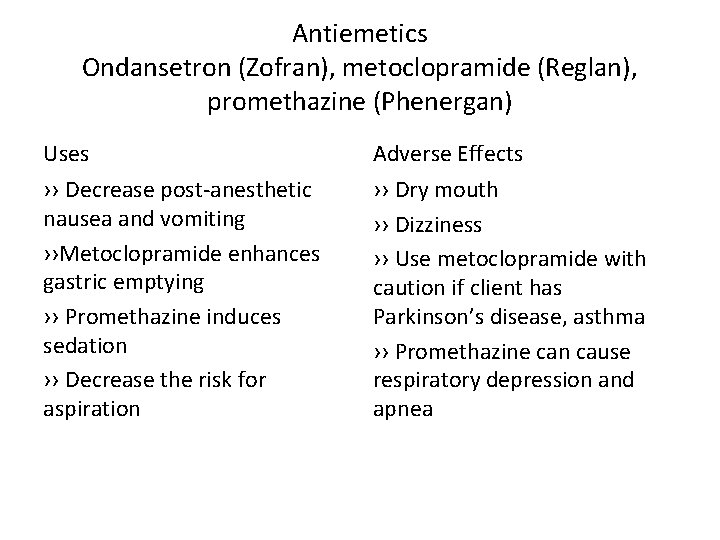
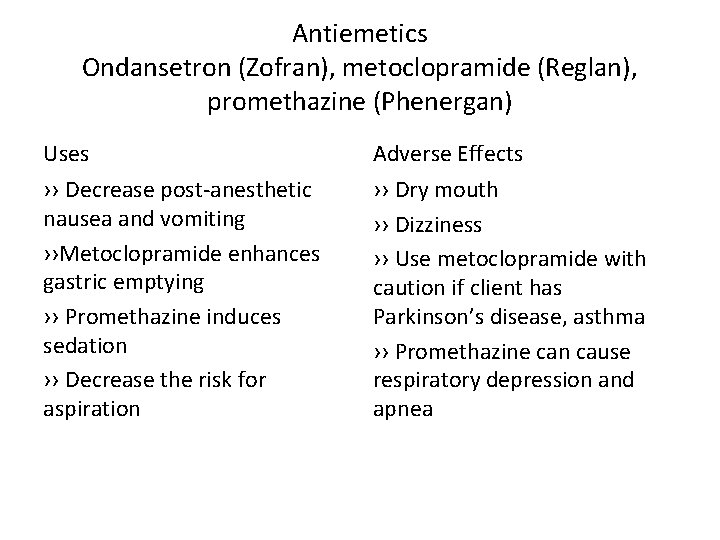
Antiemetics Ondansetron (Zofran), metoclopramide (Reglan), promethazine (Phenergan) Uses Adverse Effects ›› Decrease post-anesthetic nausea and vomiting ››Metoclopramide enhances gastric emptying ›› Promethazine induces sedation ›› Decrease the risk for aspiration ›› Dry mouth ›› Dizziness ›› Use metoclopramide with caution if client has Parkinson’s disease, asthma ›› Promethazine can cause respiratory depression and apnea
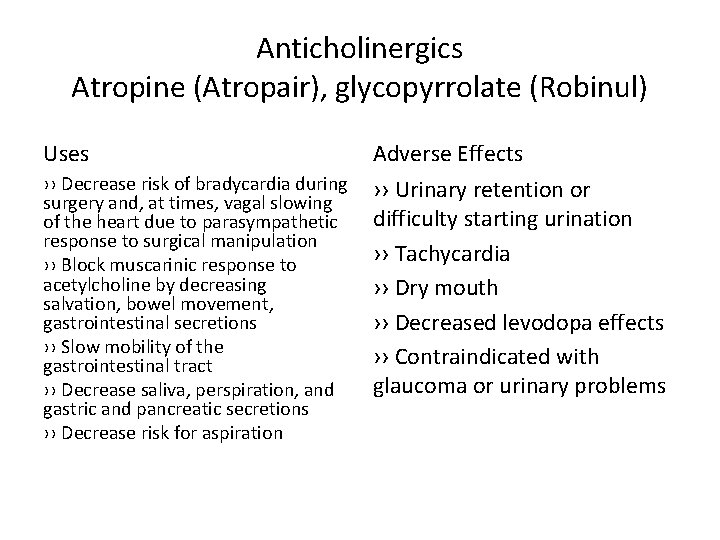
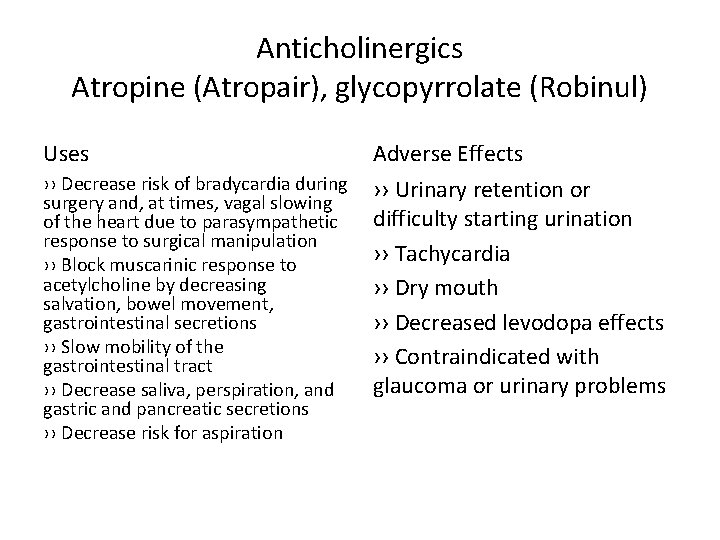
Anticholinergics Atropine (Atropair), glycopyrrolate (Robinul) Uses Adverse Effects ›› Decrease risk of bradycardia during surgery and, at times, vagal slowing of the heart due to parasympathetic response to surgical manipulation ›› Block muscarinic response to acetylcholine by decreasing salvation, bowel movement, gastrointestinal secretions ›› Slow mobility of the gastrointestinal tract ›› Decrease saliva, perspiration, and gastric and pancreatic secretions ›› Decrease risk for aspiration ›› Urinary retention or difficulty starting urination ›› Tachycardia ›› Dry mouth ›› Decreased levodopa effects ›› Contraindicated with glaucoma or urinary problems
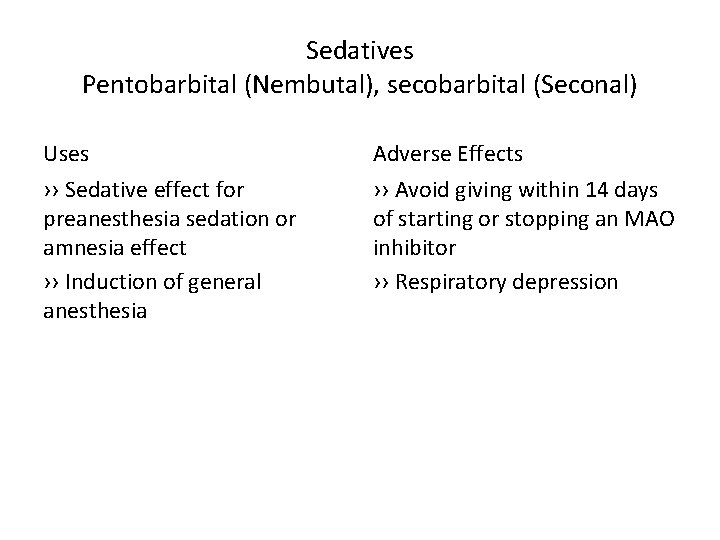
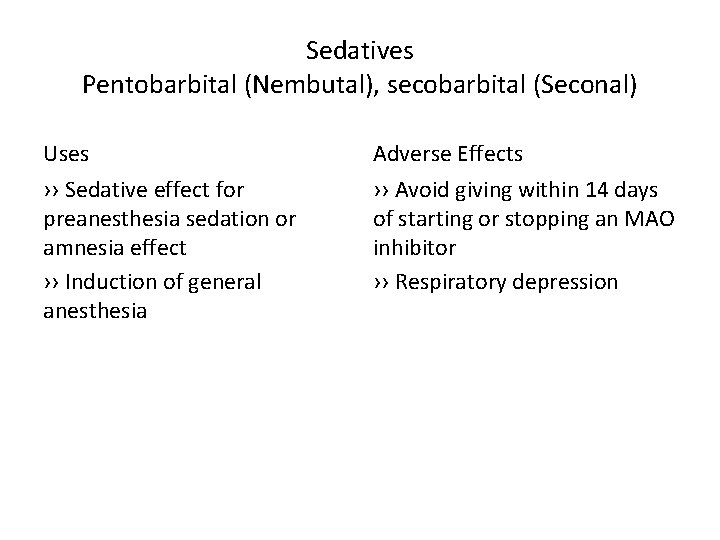
Sedatives Pentobarbital (Nembutal), secobarbital (Seconal) Uses Adverse Effects ›› Sedative effect for preanesthesia sedation or amnesia effect ›› Induction of general anesthesia ›› Avoid giving within 14 days of starting or stopping an MAO inhibitor ›› Respiratory depression
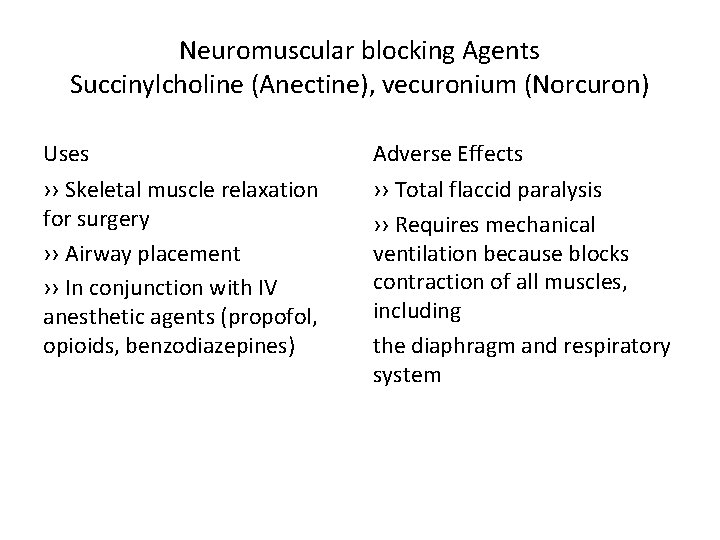
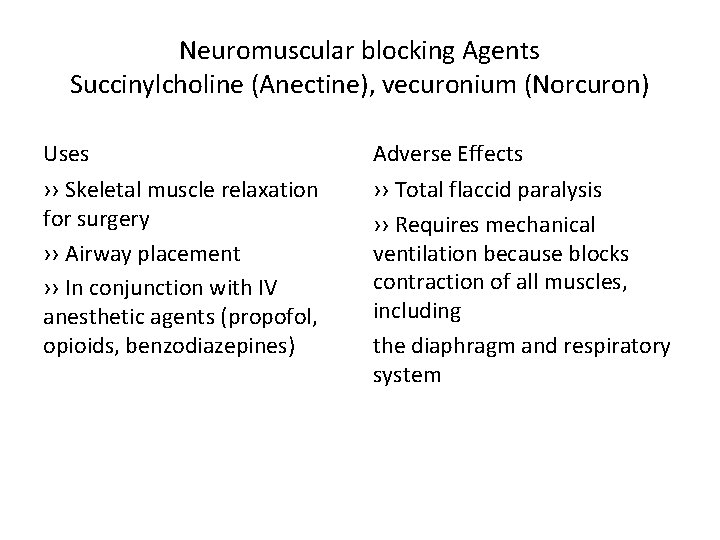
Neuromuscular blocking Agents Succinylcholine (Anectine), vecuronium (Norcuron) Uses Adverse Effects ›› Skeletal muscle relaxation for surgery ›› Airway placement ›› In conjunction with IV anesthetic agents (propofol, opioids, benzodiazepines) ›› Total flaccid paralysis ›› Requires mechanical ventilation because blocks contraction of all muscles, including the diaphragm and respiratory system
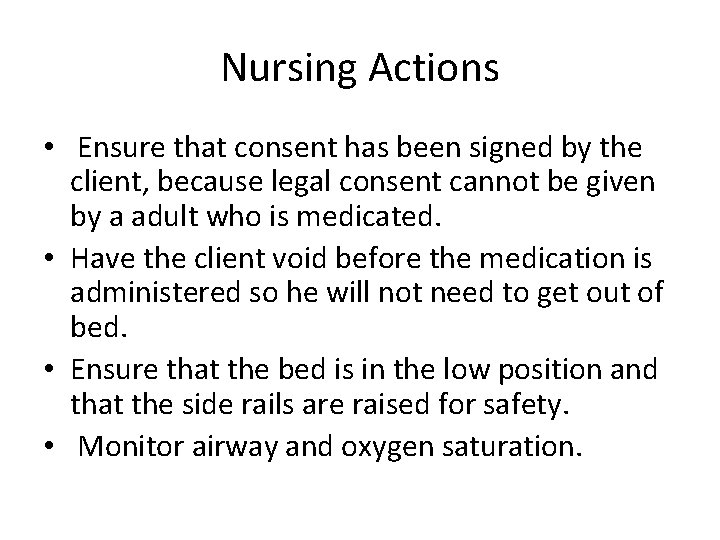
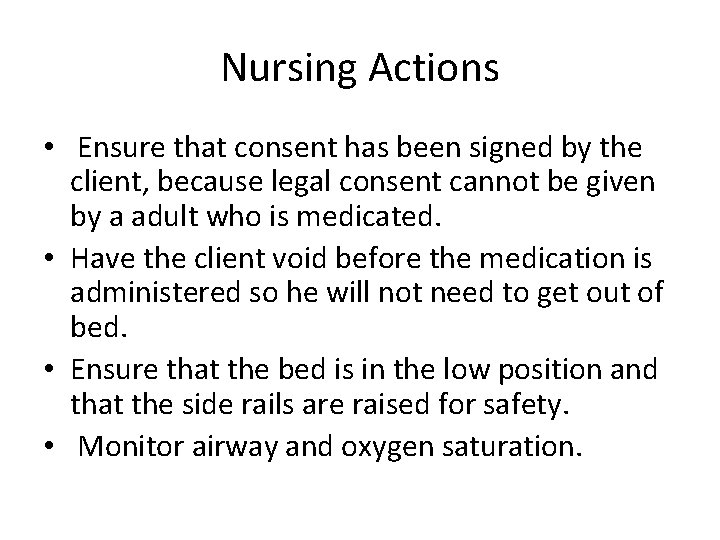
Nursing Actions • Ensure that consent has been signed by the client, because legal consent cannot be given by a adult who is medicated. • Have the client void before the medication is administered so he will not need to get out of bed. • Ensure that the bed is in the low position and that the side rails are raised for safety. • Monitor airway and oxygen saturation.
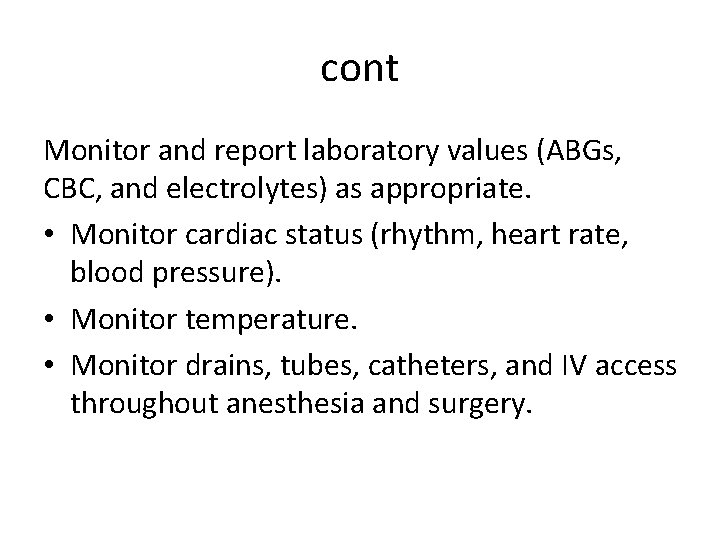
cont Monitor and report laboratory values (ABGs, CBC, and electrolytes) as appropriate. • Monitor cardiac status (rhythm, heart rate, blood pressure). • Monitor temperature. • Monitor drains, tubes, catheters, and IV access throughout anesthesia and surgery.
cont • Assess level of sedation and anesthesia (level of consciousness, vital signs). • If hypotension occurs as an adverse effect of medication or dehydration, lower the head of bed, administer a prescribed IV fluid bolus, and monitor. • Notify the surgeon and anesthesiologist if abnormalities are noted.
Complications of General Anesthesia Malignant hyperthermia (MH) C/F ›› Acute life-threatening medical emergency. ›› Inherited muscle disorder, chemically induced by anesthetic agents. ›› Triggering agents include inhalation anesthetic agents, and the muscle relaxant succinylcholine
CONT ›› Hyper metabolic condition causing an alteration in calcium activity in muscle cells (muscle rigidity, hyperthermia, and damage to the central nervous system). ›› Tachycardia is a first manifestation, dysrhythmias, muscle rigidity, hypotension, tachypnea, cyanosis and protein in urine (myoglobinuria). ›› Elevated temperature is a late manifestation – rising 1° to 2° C (2° to 4° F) every 5 min.
cont Treatment ›› Terminate surgery ›› Dantrolene (Dantrium) is a muscle relaxant to treat the condition ›› 100% oxygen, arterial blood gases ›› Infuse iced IV 0. 9% sodium chloride ›› Apply a cooling blanket, ice to axillae, groin, neck and head, iced lavage
2. Overdose of anesthetic C/F ›› Anesthetic and prescribed medication may cause complication related to the metabolize and interaction of the medication with the anesthetic. ››May occur in an older client who has preexisting conditions ››Occur in a client who has poor liver or kidney function
cont Treatment ›› The nurse should complete pre-operative screening, documentation, and inform the provider or surgeon of pre-existing medical conditions and prescribed medications and allergies.
Unrecognized hypoventilation c/f ›› Cardiac arrest, hypoxia and damage to the brain, and death may occur because of failure to adequately provide oxygen and exchange gases to the client during the surgery.
cont Treatment ››Monitor the end-tidal carbon dioxide levels of the client’s expirations. ›› Check for malfunction of equipment and manually ventilate the client.
Intubation Problems c/f ›› Injury to teeth, lips, and vocal cord during intubation may occur because the client’s mouth is too small, inability to open the client’s mouth wide, and mouth tumors. ›› Neck injury from improper neck extension during intubation may occur. ›› Sore throat
cont Treatment ›› Nurse assist anesthesiologist with the intubation ›› Have available tracheostomy set-up.
Local Anesthesia • There are three main methods of administration of local anesthesia • Topical – Applied directly to the skin or mucous membranes • Local infiltration – Injected directly into tissues through which a surgical incision is to be made. • Regional nerve block – Injected into or around specific nerves:
• four types of regional nerve blocks: • Spinal – Anesthetic is injected into the cerebral spinal fluid (CSF) in the subarachnoid space to provide autonomic, sensory, and motor blockade to the body below the level of innervation. • Epidural – Anesthetic is injected into the epidural space in the thoracic or lumbar areas of the spine, where sensory pathways are blocked, but motor function remains.
cont • Nerve block – Injection of anesthetic around or into an area of nerves to block sensation. Often used for surgery to an extremity or for chronic pain. • Field block – Injection of anesthetic around the operative field commonly used for procedures of the chest, plastic surgery, dental, and hernia repairs. • Peripheral – injection of anesthetic into a specific nerve for analgesic and anesthetic use.
cont • Examples of local anesthetic agents include procaine (Novocain) and lidocaine (Xylocaine). • Concurrent administration of a vasoconstrictor, usually epinephrine, is often used with local anesthetic administration to prolong the effects and to decrease the risk of systemic toxicity. This practice is avoided for distal injuries (finger) due to decreased circulation. Prolonged vasoconstriction could lead to tissue necrosis.
Complications and Nursing Actions • Observe the client for systemic toxic reaction due to central nervous system (CNS) stimulation(headache, blurred vision. . etc). If untreated leads to unconsciousness, low blood pressure, apnea, cardiac arrest, and death.
cont ■Establish the client’s airway, apply oxygen, and monitor oxygen saturation. Then notify the anesthesiologist and inform the surgeon. ■ Prepare to monitor client following anesthesiologist administering a fast-acting barbiturate such as thiopental (Pentothal) or methohexital (Brevital). ■ Monitor and report laboratory values (ABGs, CBC, and electrolytes) as appropriate.
cont - Monitor cardiac status (rhythm, heart rate, blood pressure). - Monitor drains, tubes, catheters, and IV access throughout anesthesia and surgery -Assess motor function to ensure paralysis does not ensue (movement returns first, then sense of touch, pain, warmth, and sensation of cold).
con • Monitor for autonomic nervous system blockade (epidural and spinal) to include hypotension, bradycardia, nausea, and vomiting. ■ Lower head of bed, increase IV fluid if no restrictions, and frequently monitor vital signs. • CSF leakage (spinal and epidural) manifests with a severe headache when head of bed is elevated. ■ Keep head of bed flat to promote the dura tear to heal. ■ Provide a quiet environment. ■ Keep the client well hydrated to help replace CSF loss.
Moderate Sedation • Moderate sedation is the administration of sedatives and/or hypnotics to the point where the client is relaxed enough that minor procedures can be performed without discomfort, yet the client can respond to verbal stimuli, retains protective reflexes (gag reflex), is easily arousable, and, most importantly, independently maintains a patent airway.
cont • Only a qualified provider can administer moderate sedation. These include anesthesiologists, certified registered nurse anesthetists (CRNAs), RNs who are certified in advanced cardiac life support (ACLS) and are under the supervision of one of the previously mentioned providers.
cont • Continuously monitor a client who is undergoing moderate sedation. During the procedure, an RN must be present to monitor the client, with no other responsibilities at that time. This nurse is to remain with the client at all times before, during, and immediately after the procedure.
Procedures that may require moderate sedation include: • Minor surgical procedures (dental, podiatric, plastic, and ophthalmic procedures). • Diagnostic procedures (various types of endoscopy, bone marrow aspiration, lumbar puncture). • Wound care (suturing, dressing changes, incision and drainage of abscesses, burn debridement). • Reduction and immobilization of fractures. • Placement and removal of implanted devices, catheters, and tubes.
Medications • Medications used during moderate sedation • Opioids – morphine, fentanyl (Sublimaze), alfentanil (Alfenta) • Anesthetics – propofol (Diprivan) • Benzodiazepines – midazolam (Versed), diazepam (Valium), lorazepam (Ativan)
cont • Dosages required for “light sedation” are highly individualized and require careful titration. • When a client receives moderate sedation, naloxone hydrochloride (Narcan) is used, if needed, to reverse the adverse effects of the opioid. If needed, flumazenil (Romazicon) is administered to reverse the adverse effects of the benzodiazepines.
Nursing Actions Preprocedure ◯ Obtain a full history from the client, including allergies, medication usage, and pre-existing medical conditions (pulmonary disease). Any previous experiences with sedation or anesthesia should to be reported, especially any adverse reactions. Note the last dose of each of the client’s prescribed medications, especially if it could alter the client’s response (diuretic, antihypertensive, narcotic). ◯ Provide education about the procedure and the medications to be used. ◯ Perform a full assessment on the client, including baseline vital signs, cardiac rhythm, and level of consciousness.
cont ◯ Determine the last time the client ate or drank (generally NPO for 6 hr or more before the procedure). ■ The client may have clear liquids up to 2 hr before the surgery or procedure. ■ Instruct the client to adhere to the instructions to remain NPO, or the surgery or procedure may be cancelled.
◯ Establish IV access and administer fluids as prescribed. ◯ Verify that the client signed the informed consent. ◯ Attach monitoring equipment to the client. ◯ Remove dentures (in case intubation would become necessary).
cont • Intraprocedure ◯ Remain with the client at all times. Allow other staff to assist the provider with the procedure, if indicated. ◯ Continually assess and monitor level of consciousness (Glasgow coma scale score), cardiac rhythm, respiratory status, and vital signs. ◯ Maintain a safe environment for the older adult client due to sensory limitations.
cont ◯ Pay careful attention to cardiac and respiratory status for older adult clients, as problems can arise more quickly. ◯ During the procedure, the following equipment must be present within immediate reach for routine monitoring and in case deep sedation with respiratory depression occurs. ■ Fully equipped emergency cart that includes emergency medications, airway and ventilatory equipment, defibrillator, and IV supplies ■ A 100% oxygen source and administration supplies, airways, manual resuscitation bag, and suction equipment ■ ECG monitor/display, noninvasive blood pressure monitor, pulse oximeter, thermometer, and stethoscope
cont • Postprocedure ◯ The nurse who is monitoring should continue to record vital signs and level of consciousness until the client is fully awake and all assessment criteria return to presedation levels. Only then can the nurse remove the monitor and all emergency equipment from the bedside.
cont Typical discharge criteria ■ Level of consciousness as on admission ■ Vital signs stable for 30 to 90 min ■ Ability to cough and deep breathe ■ Ability to tolerate oral fluids ■ Ability to void ■ Absence of nausea, vomiting, shortness of breath, or dizziness
Complications and Nursing Actions • Before, during, and after the procedure, emergency equipment is to remain at the client’s bedside. Some complications that can arise from moderate sedation include: ◯ Airway obstruction, respiratory depression, cardiac arrhythmias, hypotension, and anaphylaxis ■ Insert airway and suction.
◯ Respiratory depression ■ Administer oxygen and reversal agents, such as naloxone (Narcan) and flumazenil (Romazicon). ◯ Cardiac arrhythmias ■ Set up a 12 -lead ECG and provide antidysrhythmics and fluids.

thanks