Acute leukemia in Pediatrics Young shil Park Division














- Slides: 52
Acute leukemia in Pediatrics Young shil, Park Division of Hematology-Oncology Department of Pediatrics Kyung Hee University Hospital at Gangdong
Introduction most common malignant neoplasms in childhood about 41% of all malignancies that occur in children younger than 15 yr of age an annual incidence of 4. 1 new cases per 100, 000 children younger than 15 yr of age

Acute Lymphoblastic Leukemia
the first disseminated cancer shown to be curable model malignancy for the principles of cancer diagnosis, prognosis, and treatment heterogeneous group of malignancies
ALL Epidemiology striking peak incidence between 2– 6 yr of age more common in children with certain chromosomal abnormalities such as Down syndrome Bloom syndrome ataxia-telangiectasia Fanconi syndrome
Etiology unknown B-cell ALL and Epstein-Barr viral infections in certain developing countries
Pathogenesis Classification • Morphology • Phenotypic characteristics ( cell membrane markers ) • Cytogenetic and molecular genetic features
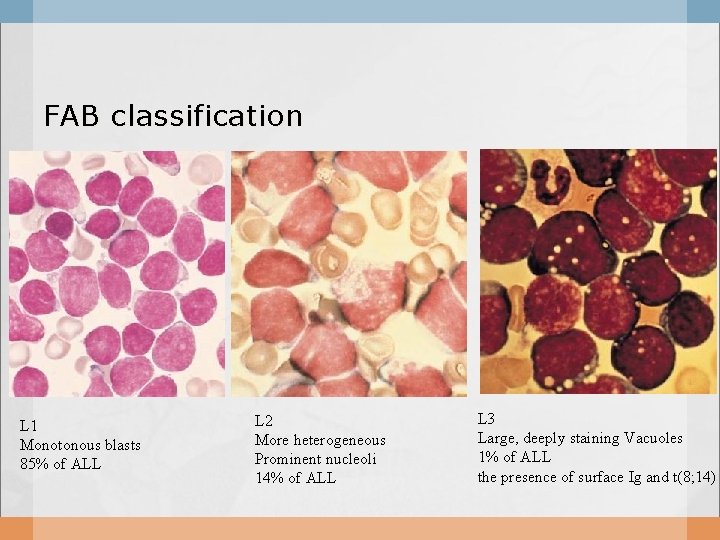
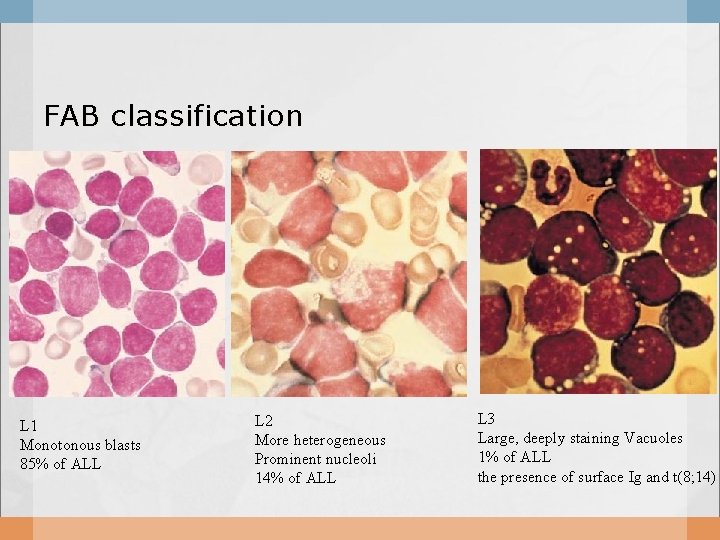
FAB classification L 1 Monotonous blasts 85% of ALL L 2 More heterogeneous Prominent nucleoli 14% of ALL L 3 Large, deeply staining Vacuoles 1% of ALL the presence of surface Ig and t(8; 14)
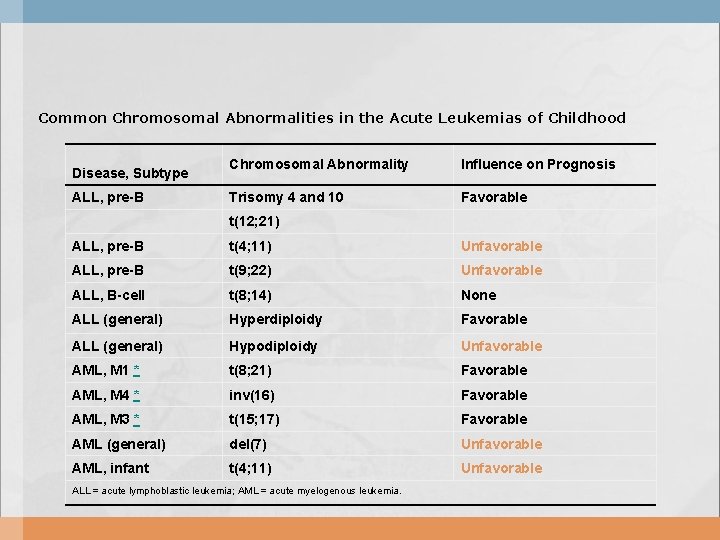
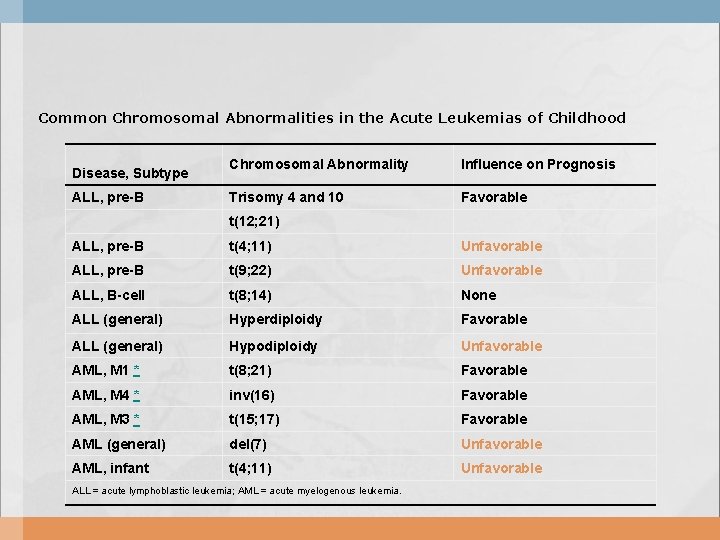
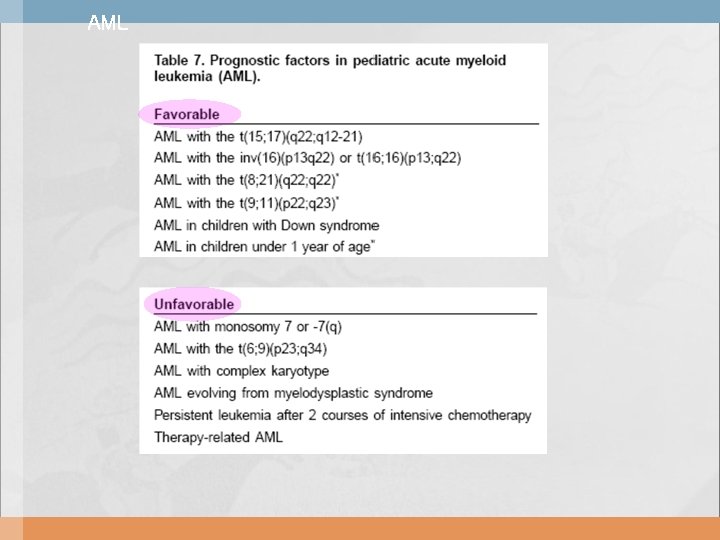
Common Chromosomal Abnormalities in the Acute Leukemias of Childhood Chromosomal Abnormality Influence on Prognosis ALL, pre-B Trisomy 4 and 10 Favorable t(12; 21) ALL, pre-B t(4; 11) Unfavorable ALL, pre-B t(9; 22) Unfavorable ALL, B-cell t(8; 14) None ALL (general) Hyperdiploidy Favorable ALL (general) Hypodiploidy Unfavorable AML, M 1 * t(8; 21) Favorable AML, M 4 * inv(16) Favorable AML, M 3 * t(15; 17) Favorable AML (general) del(7) Unfavorable AML, infant t(4; 11) Unfavorable Disease, Subtype ALL = acute lymphoblastic leukemia; AML = acute myelogenous leukemia.
Estimated Frequency of Specific Genotypes of ALL in Children NEJM 2004; 350: 1535 -48
Estimated Frequency of Specific Genotypes of Pediatric ALL in single center in Korea, 2006, 소아과 추계

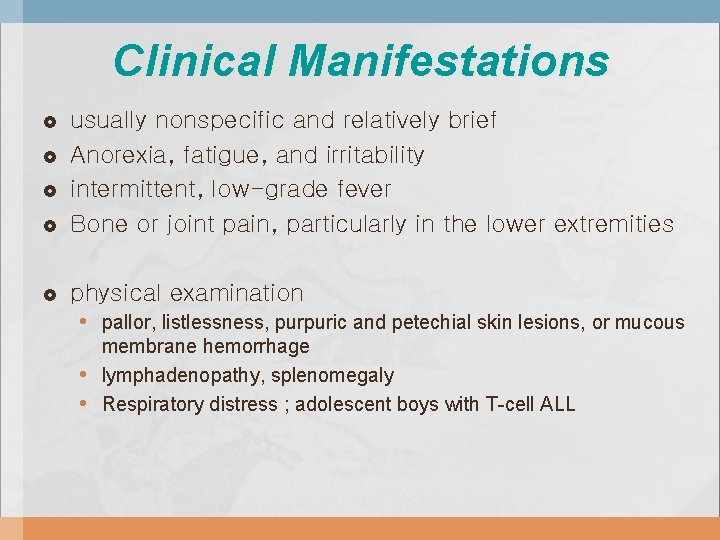
Clinical Manifestations usually nonspecific and relatively brief Anorexia, fatigue, and irritability intermittent, low-grade fever Bone or joint pain, particularly in the lower extremities physical examination • pallor, listlessness, purpuric and petechial skin lesions, or mucous • • membrane hemorrhage lymphadenopathy, splenomegaly Respiratory distress ; adolescent boys with T-cell ALL

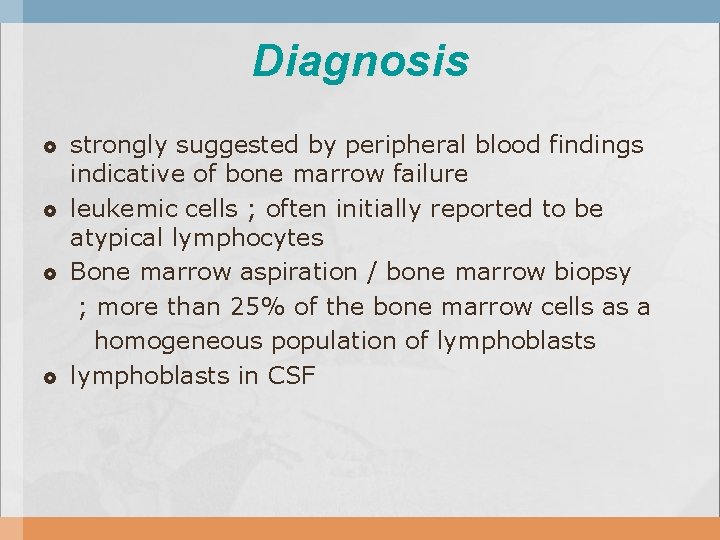
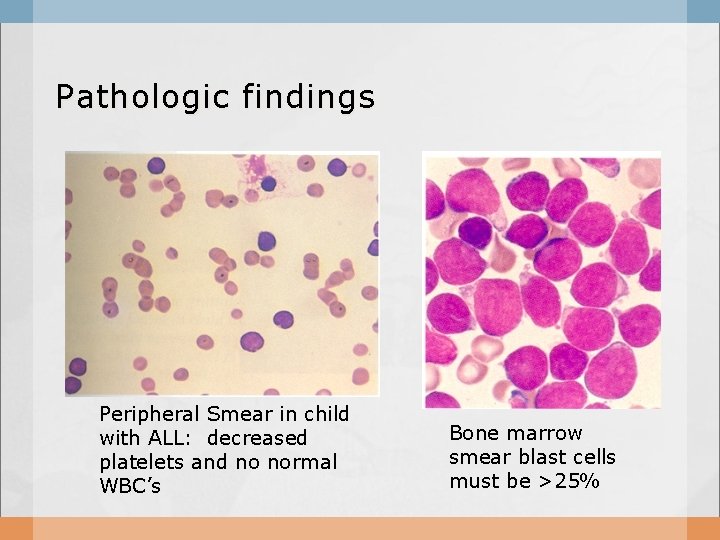
Diagnosis strongly suggested by peripheral blood findings indicative of bone marrow failure leukemic cells ; often initially reported to be atypical lymphocytes Bone marrow aspiration / bone marrow biopsy ; more than 25% of the bone marrow cells as a homogeneous population of lymphoblasts in CSF
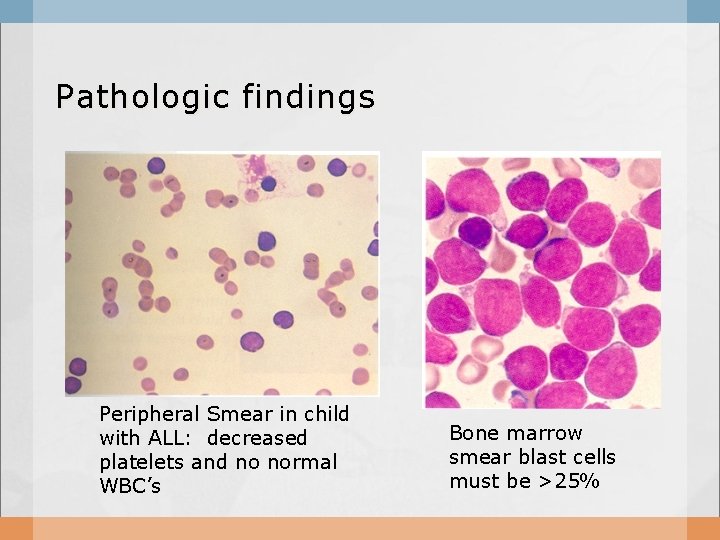
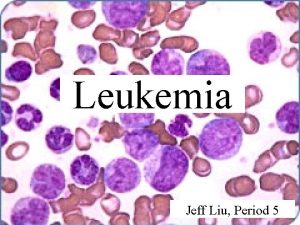
Pathologic findings Peripheral Smear in child with ALL: decreased platelets and no normal WBC’s Bone marrow smear blast cells must be >25%
DIFFERENTIAL DIAGNOSIS acute myelogenous leukemia (AML) neuroblastoma, Ewing's sarcoma aplastic anemia infectious mononucleosis in patients with acute onset of fever and lymphadenopathy
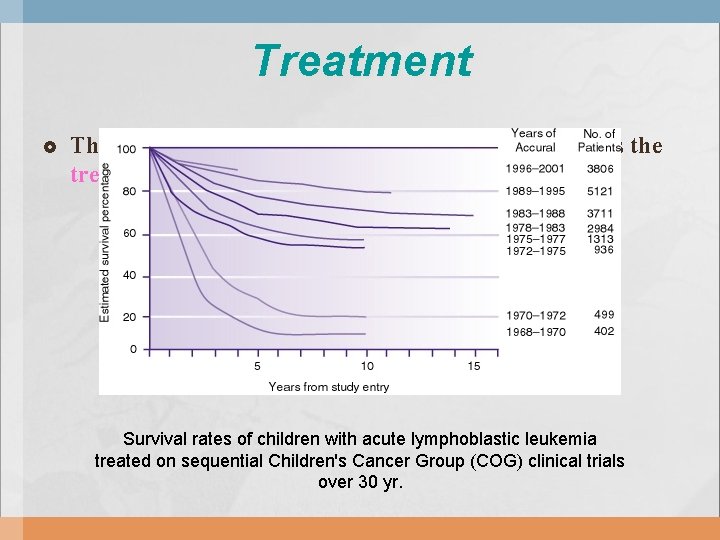
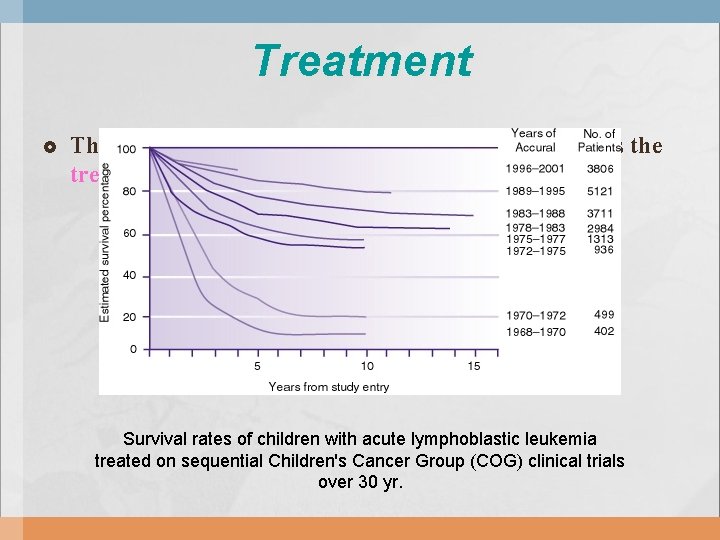
Treatment The single most important prognostic factor in ALL is the treatment. Survival rates of children with acute lymphoblastic leukemia treated on sequential Children's Cancer Group (COG) clinical trials over 30 yr.
the estimated clinical risk of relapse in the patient Ø the age of the patient at the time of diagnosis Ø the initial leukocyte count Ø the speed of response to treatment
ALL-Treatment older than 10 yr of age initial leukocyte count of more than 50, 000/μL specific chromosomal abnormalities such as t(9; 22) or t(4; 11)
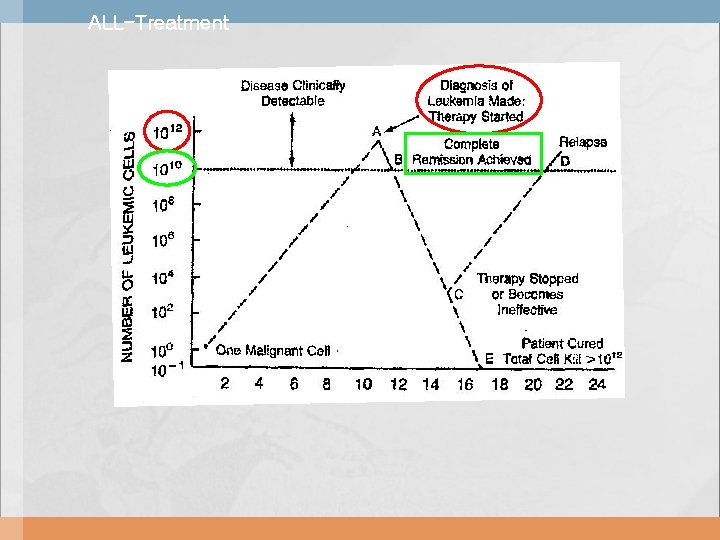
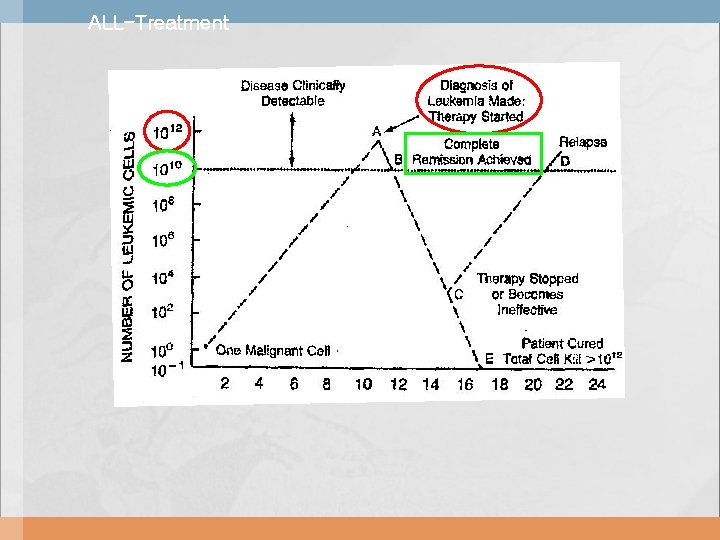
ALL-Treatment
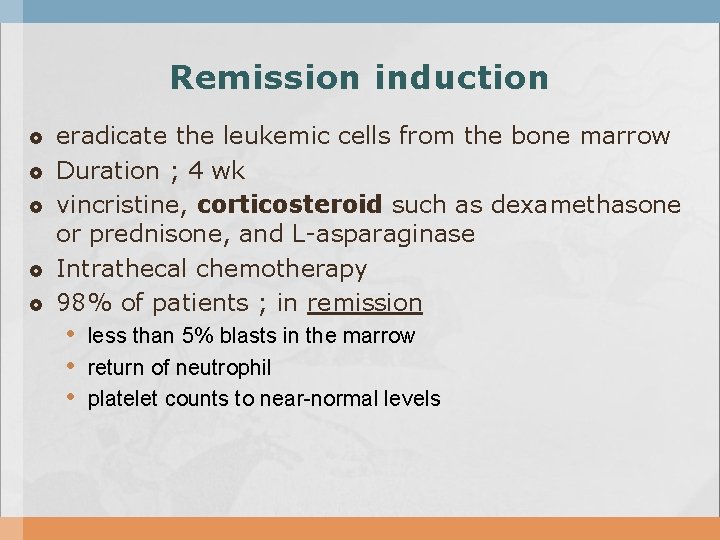
Remission induction eradicate the leukemic cells from the bone marrow Duration ; 4 wk vincristine, corticosteroid such as dexamethasone or prednisone, and L-asparaginase Intrathecal chemotherapy 98% of patients ; in remission • less than 5% blasts in the marrow • return of neutrophil • platelet counts to near-normal levels
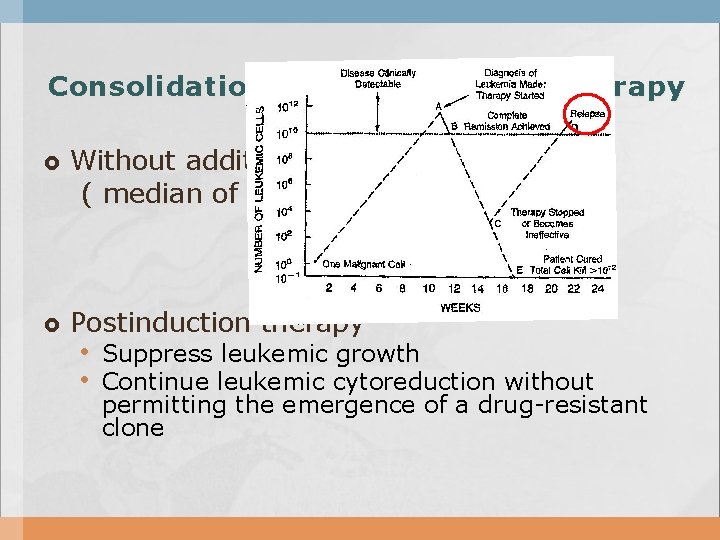
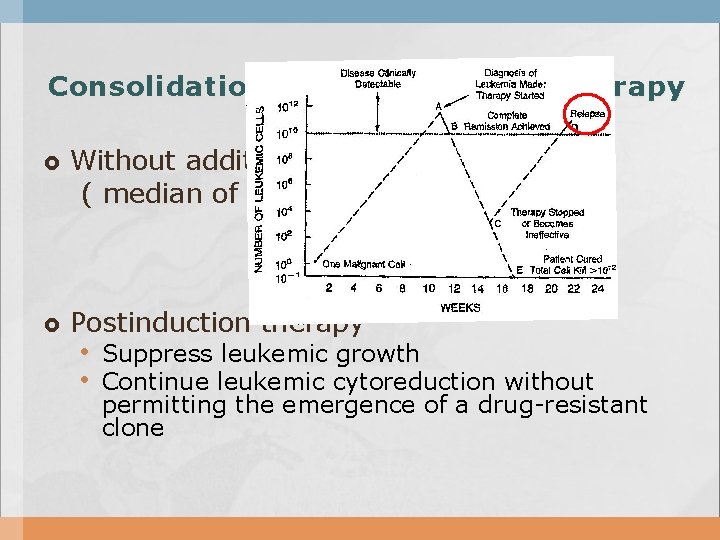
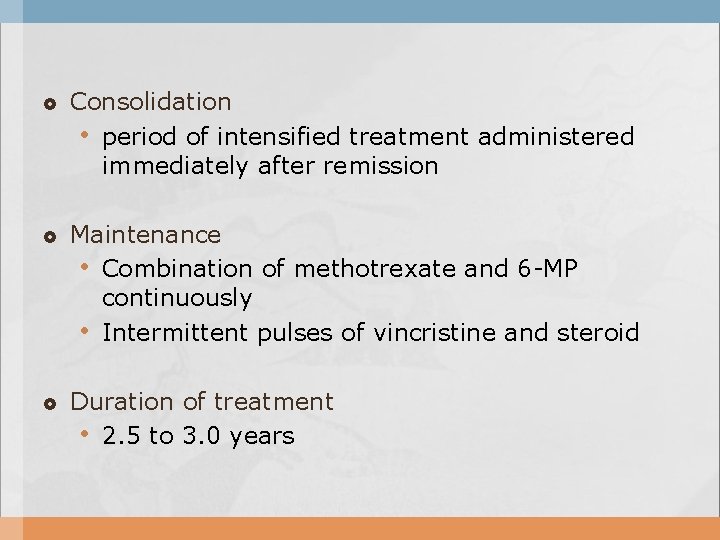
Consolidation and Maintenance therapy Without additional therapy, relapse ( median of 1 to 2 months ) Postinduction therapy • Suppress leukemic growth • Continue leukemic cytoreduction without permitting the emergence of a drug-resistant clone
Consolidation • period of intensified treatment administered immediately after remission Maintenance • Combination of methotrexate and 6 -MP continuously • Intermittent pulses of vincristine and steroid Duration of treatment • 2. 5 to 3. 0 years
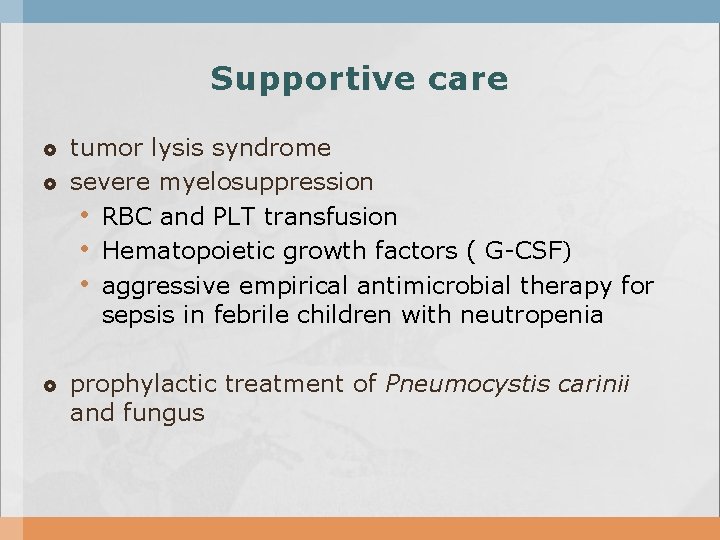
Supportive care tumor lysis syndrome severe myelosuppression • RBC and PLT transfusion • Hematopoietic growth factors ( G-CSF) • aggressive empirical antimicrobial therapy for sepsis in febrile children with neutropenia prophylactic treatment of Pneumocystis carinii and fungus
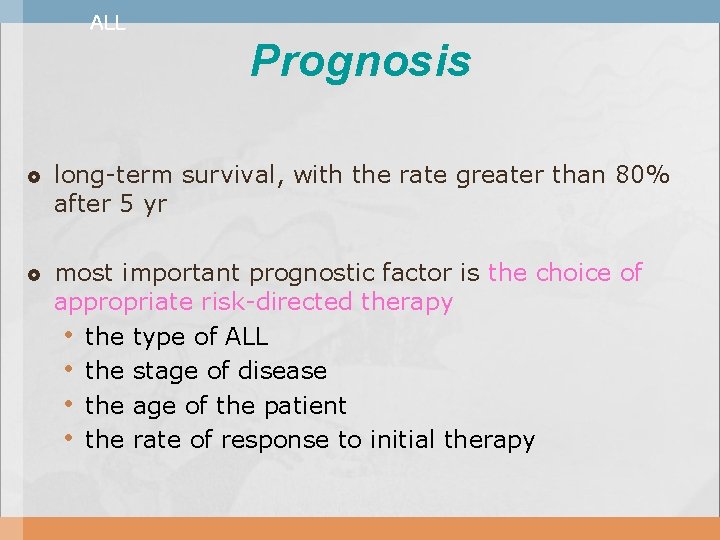
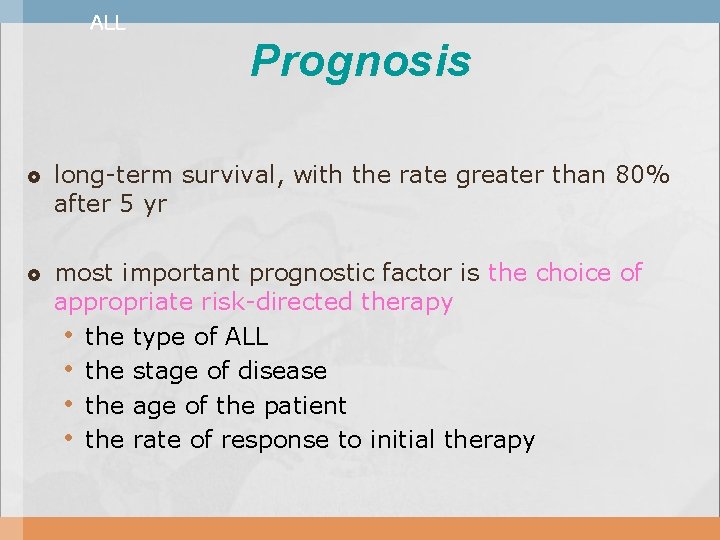
ALL Prognosis long-term survival, with the rate greater than 80% after 5 yr most important prognostic factor is the choice of appropriate risk-directed therapy • the type of ALL • the stage of disease • the age of the patient • the rate of response to initial therapy


Relapse Bone marrow, CNS, and testis Relapse in the bone marrow ; 15– 20% of patients Testicular relapse in 1– 2% of boys with ALL • usually after completion of therapy • painless swelling of one or both testes
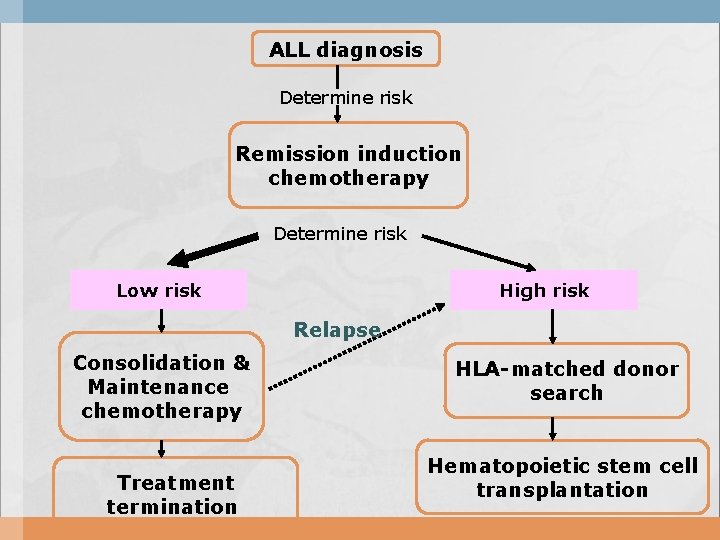
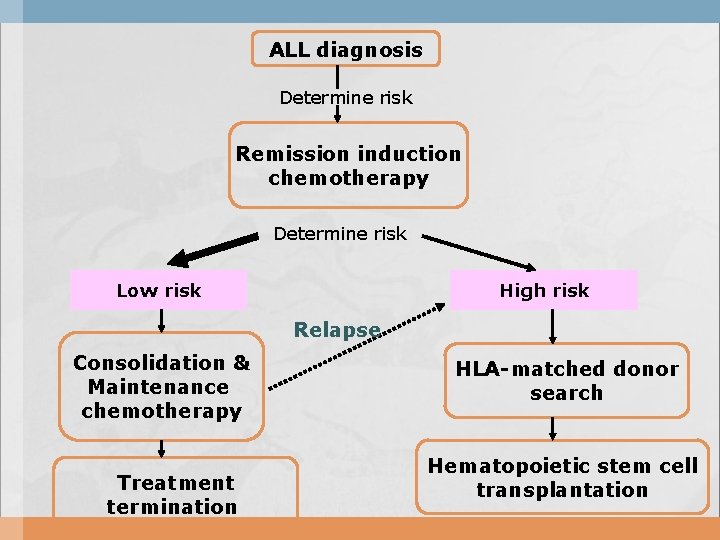
ALL diagnosis Determine risk Remission induction chemotherapy Determine risk Low risk High risk Relapse Consolidation & Maintenance chemotherapy Treatment termination HLA-matched donor search Hematopoietic stem cell transplantation
Acute Myelogenous Leukemia
AML Epidemiology 11% of the cases of leukemia in childhood In Korea ; 일년에 100명 정도의 신환
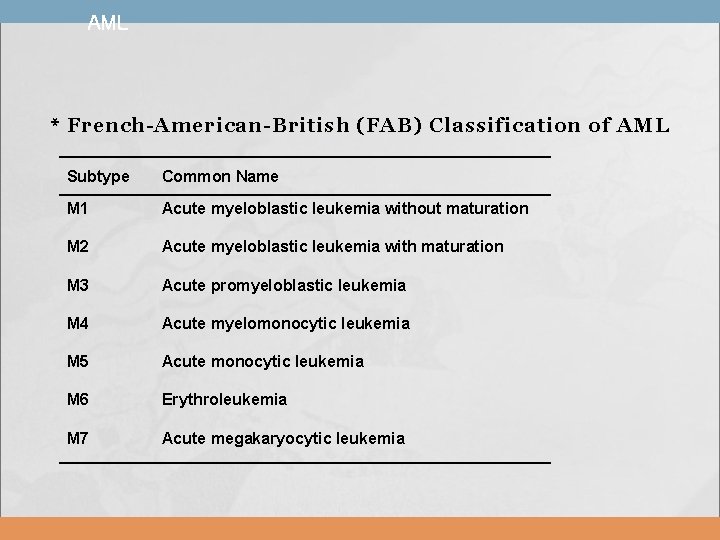
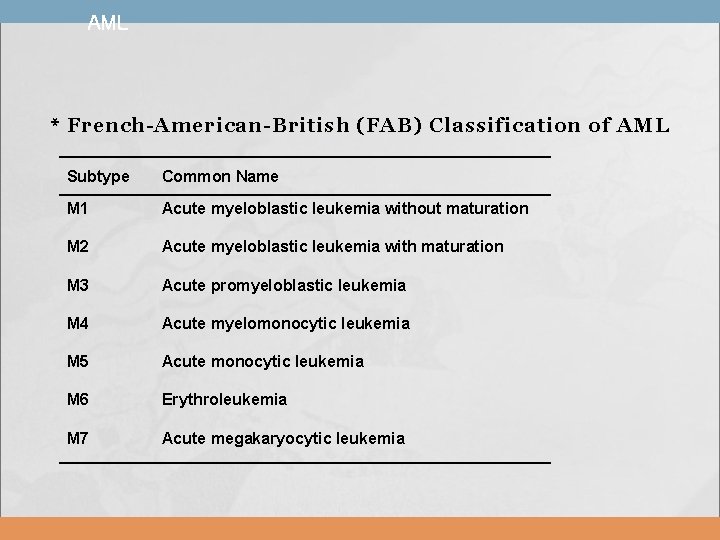
AML * French-American-British (FAB) Classification of AML Subtype Common Name M 1 Acute myeloblastic leukemia without maturation M 2 Acute myeloblastic leukemia with maturation M 3 Acute promyeloblastic leukemia M 4 Acute myelomonocytic leukemia M 5 Acute monocytic leukemia M 6 Erythroleukemia M 7 Acute megakaryocytic leukemia
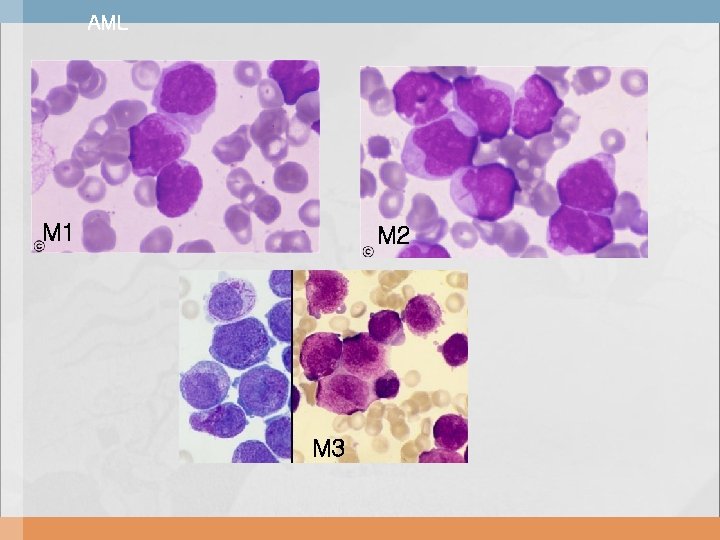
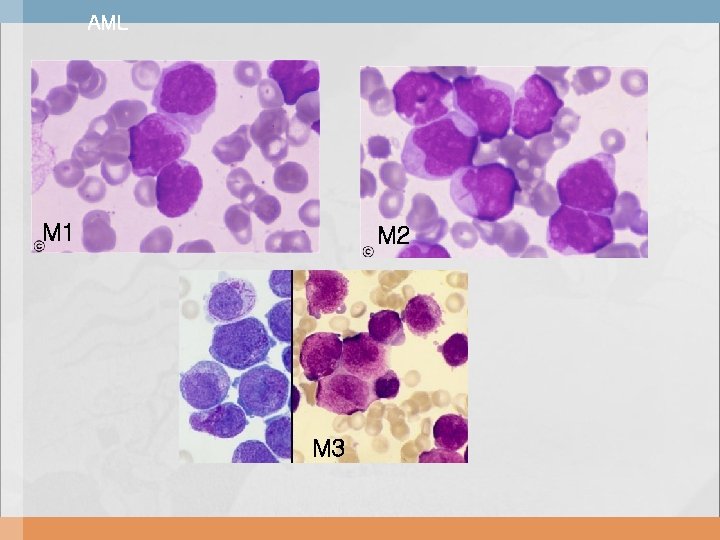
AML M 1 M 2 M 3
AML combination of morphologic, immunophenotypic, and cytogenetic studies


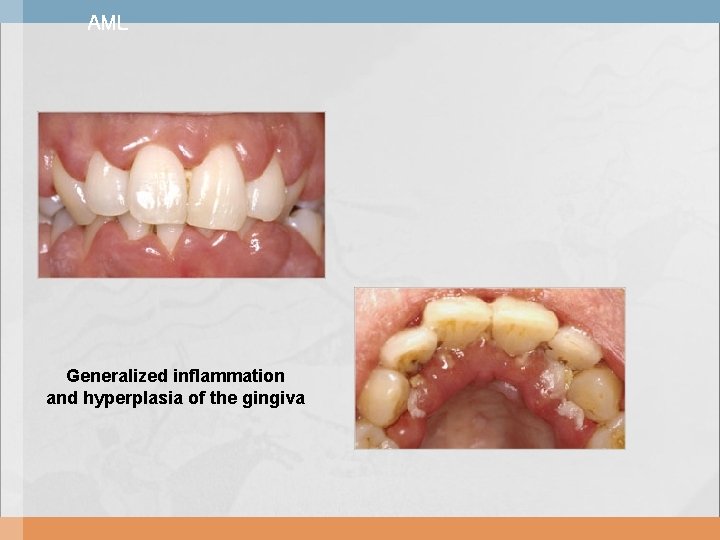
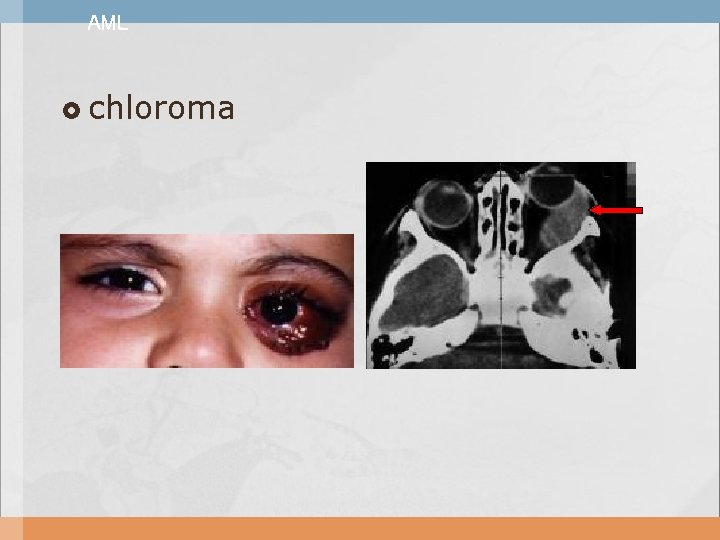
AML Clinical manifestations Due to replacement of bone marrow by malignant cells Due to secondary bone marrow failure Infiltration of the gingiva Discrete masses ( chloroma or granulocytic sarcoma )
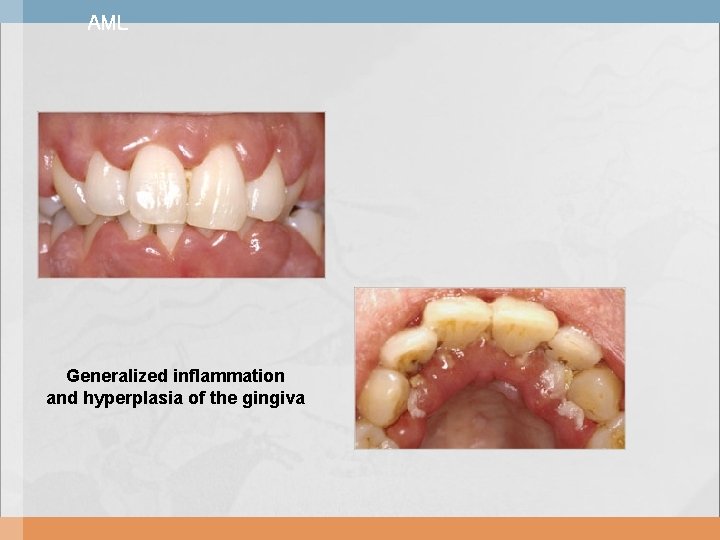
AML Generalized inflammation and hyperplasia of the gingiva
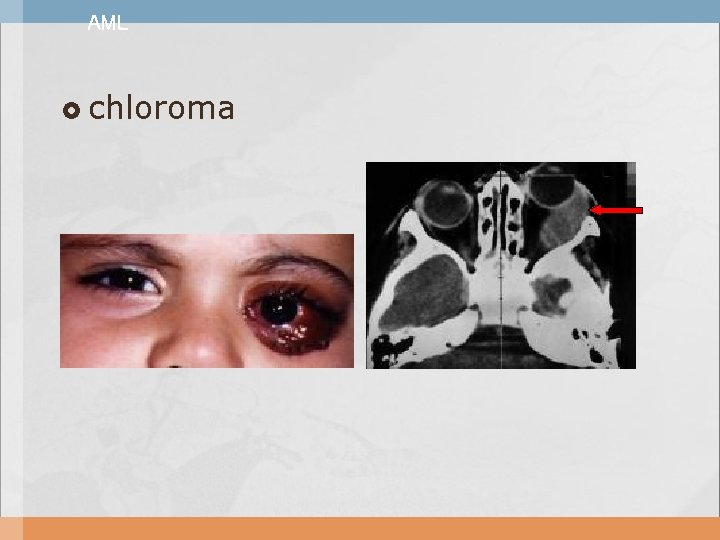
AML chloroma






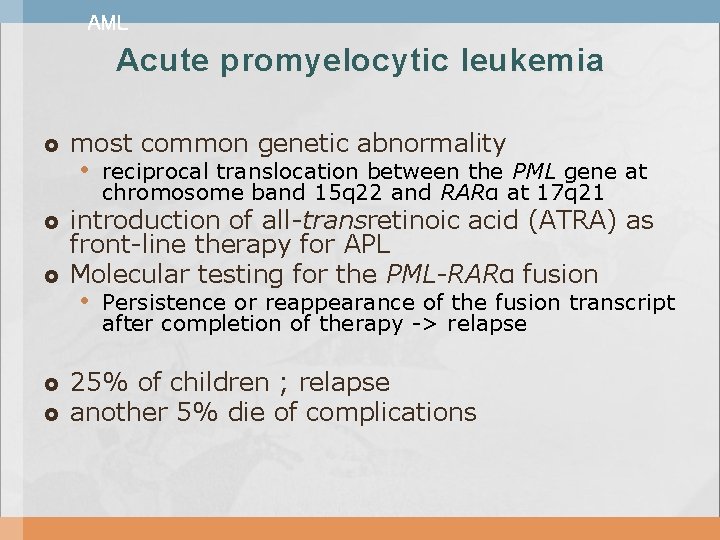
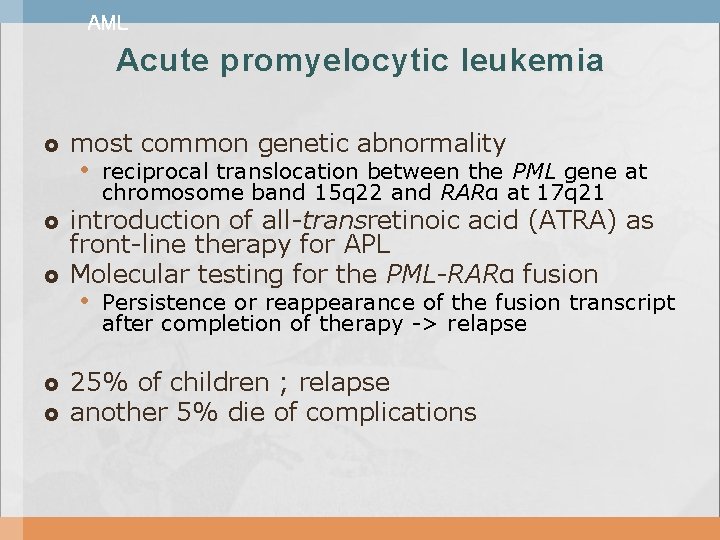
AML Acute promyelocytic leukemia most common genetic abnormality • reciprocal translocation between the PML gene at chromosome band 15 q 22 and RARα at 17 q 21 introduction of all-transretinoic acid (ATRA) as front-line therapy for APL Molecular testing for the PML-RARα fusion • Persistence or reappearance of the fusion transcript after completion of therapy -> relapse 25% of children ; relapse another 5% die of complications
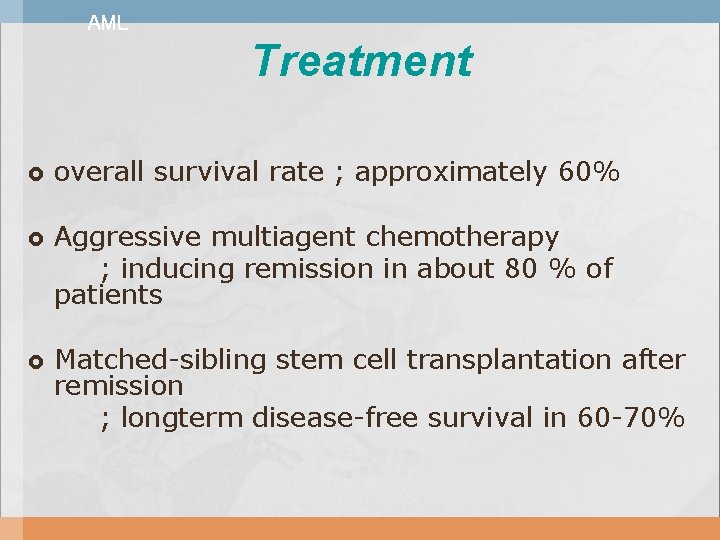
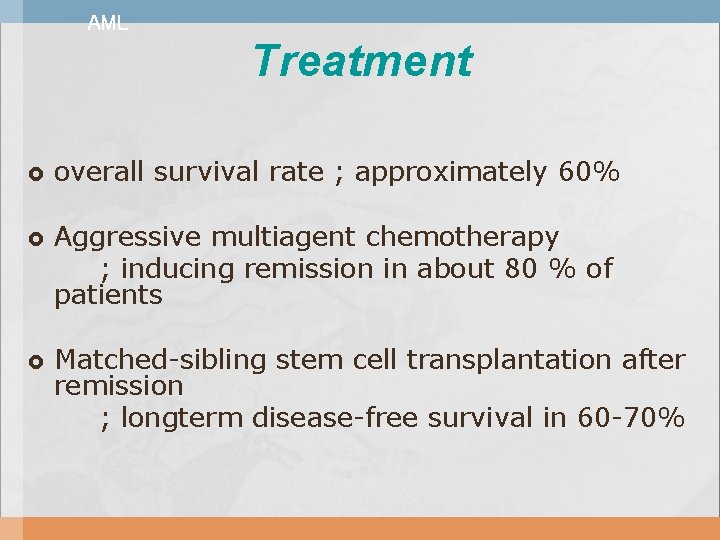
AML Treatment overall survival rate ; approximately 60% Aggressive multiagent chemotherapy ; inducing remission in about 80 % of patients Matched-sibling stem cell transplantation after remission ; longterm disease-free survival in 60 -70%
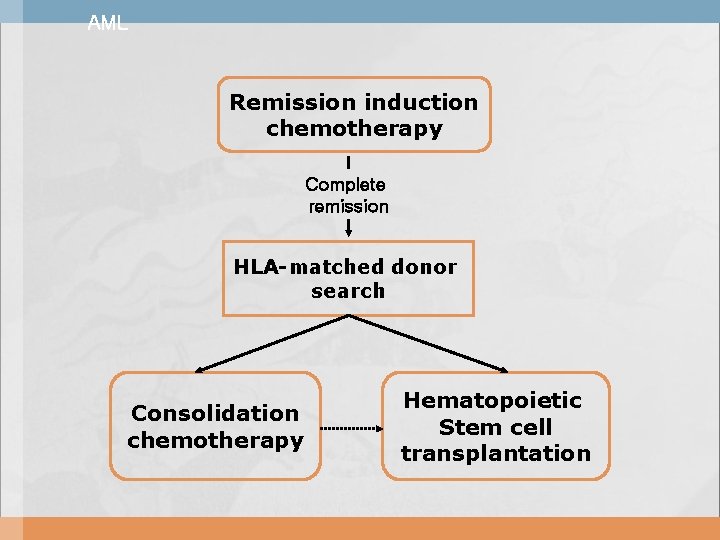
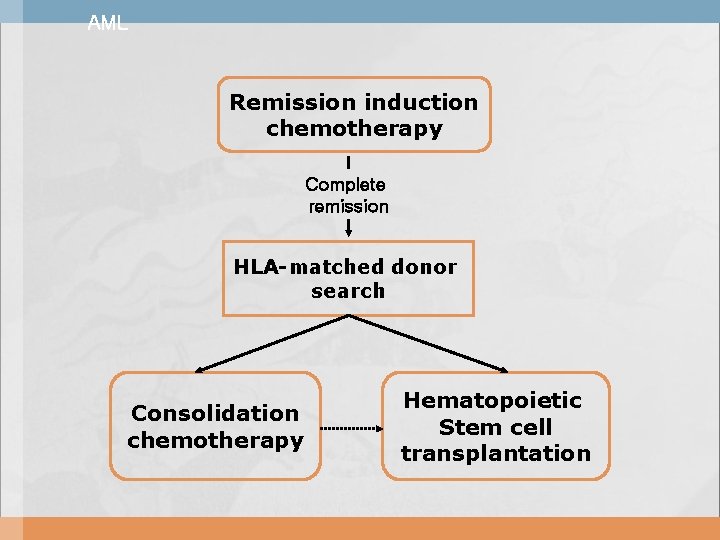
AML Remission induction chemotherapy Complete remission HLA-matched donor search Consolidation chemotherapy Hematopoietic Stem cell transplantation
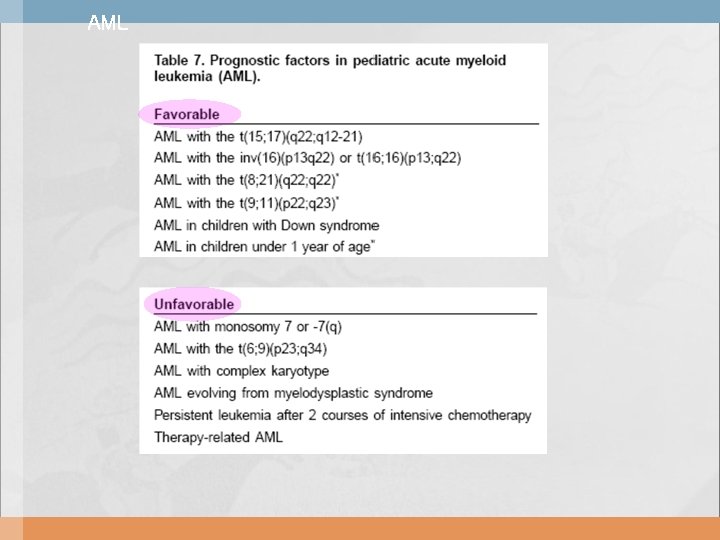
AML

Thank you for your attention~!
 Shil park
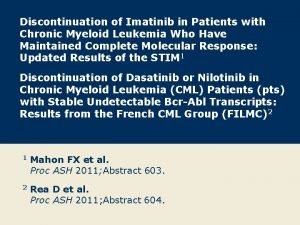
Shil park Clinicaloptions
Clinicaloptions Platelet clumper
Platelet clumper Acute mylogenous leukemia
Acute mylogenous leukemia Linelidomide
Linelidomide Krvná plazma funkcia
Krvná plazma funkcia Leukemia
Leukemia Nk leukemia
Nk leukemia Zhang wang leukemia
Zhang wang leukemia Asparagine
Asparagine Leukemia vs lymphoma
Leukemia vs lymphoma Hairy cell leukemia
Hairy cell leukemia Leukemia statics
Leukemia statics Ostomy medical term suffix
Ostomy medical term suffix Leukemoid reaction
Leukemoid reaction Pas stain procedure slideshare
Pas stain procedure slideshare Mark juckett md
Mark juckett md Lll leukemia
Lll leukemia Lymphoproliferative disease
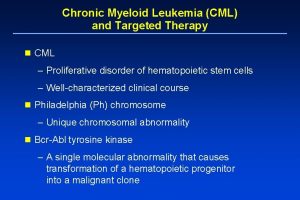
Lymphoproliferative disease Chronic myeloid leukemia
Chronic myeloid leukemia Limfoblast
Limfoblast Cml stages
Cml stages Myelobast
Myelobast Clast medical terminology
Clast medical terminology Chronic myeloid leukemia
Chronic myeloid leukemia Orchard park community center
Orchard park community center Duke pediatrics durham nc
Duke pediatrics durham nc Mummy restraint in pediatrics
Mummy restraint in pediatrics Modern concept of pediatric nursing ppt
Modern concept of pediatric nursing ppt Introduction of pediatrics
Introduction of pediatrics River valley pediatrics
River valley pediatrics Pulse grading 2+
Pulse grading 2+ Vancouver clinic pediatrics
Vancouver clinic pediatrics Im injection sites and volumes pediatrics
Im injection sites and volumes pediatrics Nelson pediatrics
Nelson pediatrics Assessment of pain
Assessment of pain Nelson pediatrics
Nelson pediatrics 11yo
11yo Carrie tingley pediatrics
Carrie tingley pediatrics Psychiatry shelf percentiles
Psychiatry shelf percentiles Normal vital signs for adults
Normal vital signs for adults What is a buretrol
What is a buretrol Prof sn singh
Prof sn singh Equipment used in pediatrics
Equipment used in pediatrics Trends of pediatric nursing
Trends of pediatric nursing Jaundice physical exam
Jaundice physical exam Albugenol solucion para nebulizar
Albugenol solucion para nebulizar Tlc pediatrics flint
Tlc pediatrics flint Practical approach pediatrics
Practical approach pediatrics Chest pain in pediatrics
Chest pain in pediatrics Type of jaundice
Type of jaundice Chest pain in pediatrics
Chest pain in pediatrics Xxx
Xxx