Chronic Myeloid Leukemia Leukemia n ALL AML CLL







- Slides: 15

Chronic Myeloid Leukemia
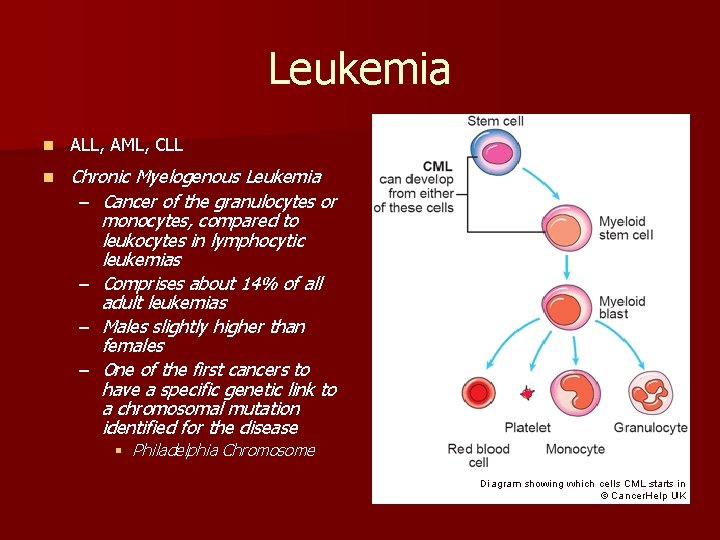
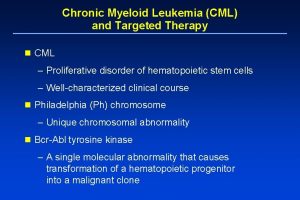
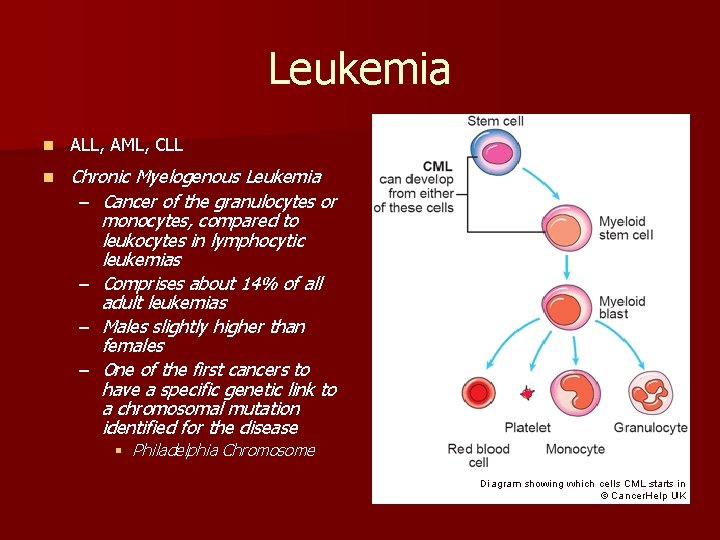
Leukemia n ALL, AML, CLL n Chronic Myelogenous Leukemia – Cancer of the granulocytes or monocytes, compared to leukocytes in lymphocytic leukemias – Comprises about 14% of all adult leukemias – Males slightly higher than females – One of the first cancers to have a specific genetic link to a chromosomal mutation identified for the disease § Philadelphia Chromosome

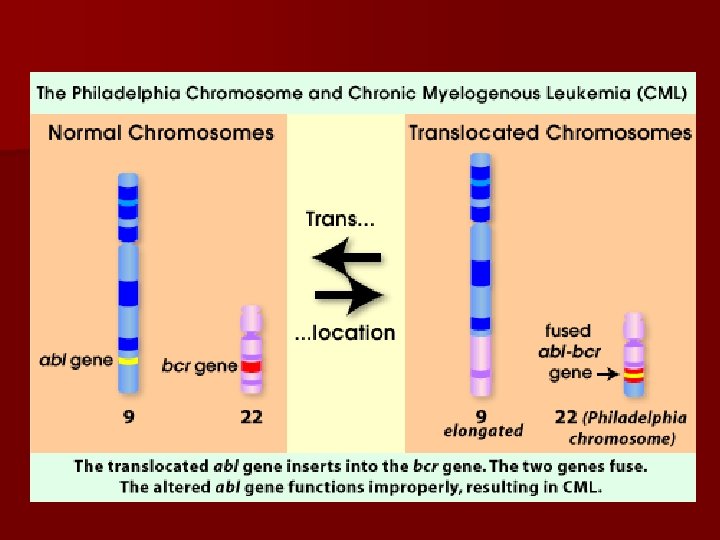
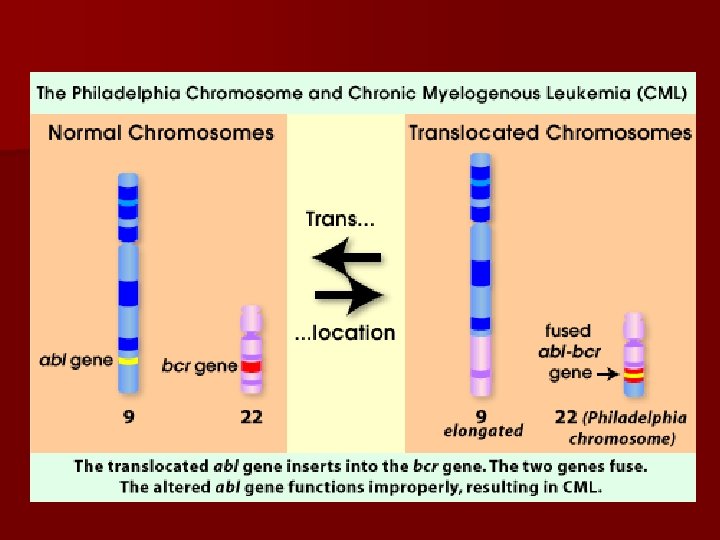
Pathophysiology Disorder of the stem cells in bone marrow n General infection fighting cells are the most harmed > granulocytes and monocytes (aka, neutrophils) n These immature cells take over the body’s mature neutrophils and hinder the body’s ability to fight infection properly n CML is caused by a genetic mutation with chromosomes 9 and 22 in the body n Abl on chromosome 9 is translocated to chromosome 22 and fuses with Bcr n This ABL-BCR protein is an unregulated tyrosine kinase and thus, is the source of the reproduction of immature granulocytes n Other functions include: upstream changes of DNA repair mechanisms, suppression of the body’s programmed cell death proteins, and changes in cytoskeletal structures n


How you are diagnosed n Usually by accident! Routine WBC test shows elevated leukocytes n Confirmed with bone marrow biopsy and FISH and/or PCR that shows presence of Philadelphia Chromosome n Presence of myeloid cells in peripheral blood determines staging of disease n n S/SX: lethargy, pallor, night sweats, weight loss, anorexia, fever, lymphadenopathy, splenomegaly
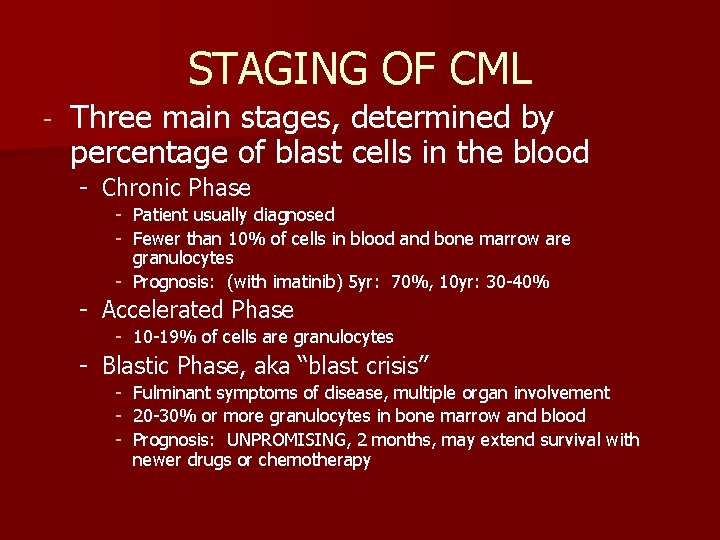
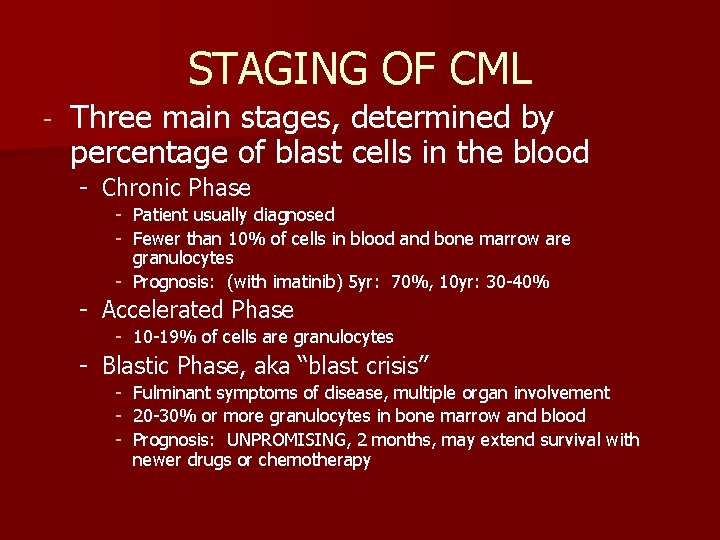
STAGING OF CML - Three main stages, determined by percentage of blast cells in the blood - Chronic Phase - Patient usually diagnosed - Fewer than 10% of cells in blood and bone marrow are granulocytes - Prognosis: (with imatinib) 5 yr: 70%, 10 yr: 30 -40% - Accelerated Phase - 10 -19% of cells are granulocytes - Blastic Phase, aka “blast crisis” - Fulminant symptoms of disease, multiple organ involvement - 20 -30% or more granulocytes in bone marrow and blood - Prognosis: UNPROMISING, 2 months, may extend survival with newer drugs or chemotherapy

Treatment Options: n Pharmacotherapy – Newer drugs are prolonging chronic phase and increasing the number of patients who enter into remission – They are easier on the body versus SCT – Old Standard: hydroxyurea (no possible cytogenic response) or interferon alpha + cytarabine – New Standard: tyrosine kinase inhibitors § Imatinib, dasatanib, nilotonib n Stem Cell Transplant – Using bone marrow from a donor to “resupply” the patient – Can be the only “curative” measure, although many drawbacks § Must be good candidates for surgery § Must have a relatively short time from diagnosis to transplant § Matching donor § Possible relapse of CML § Rejection (GVHD)

How to measure treatment n Hematologic response – The response that reflects a decrease in white blood cell count and platelets – A hematological response in CML would be shown when a patient went from about a 10% granulocyte count to a 4% granulocyte count – Good prognostic sign n Cytogenic response – Reduction or elimination of Ph+ cells in bone marrow – Can be Complete, Major or Minor § 0%, 1 -34%, 35 -90% respectively in bone marrow cells – Done by FISH and/or PCR – Chronic phase patients who have cytogenic responses have a significant increase in survival and a deterrence to progression to accelerated or blast phases – Better prognostic sign
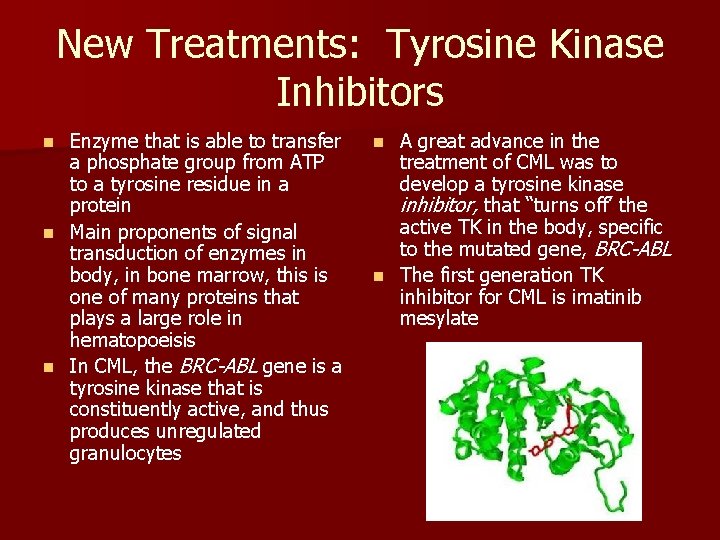
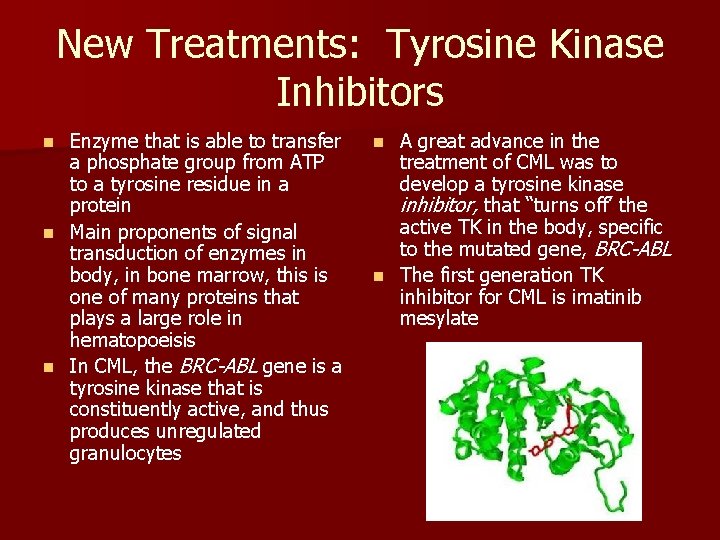
New Treatments: Tyrosine Kinase Inhibitors Enzyme that is able to transfer a phosphate group from ATP to a tyrosine residue in a protein n Main proponents of signal transduction of enzymes in body, in bone marrow, this is one of many proteins that plays a large role in hematopoeisis n In CML, the BRC-ABL gene is a tyrosine kinase that is constituently active, and thus produces unregulated granulocytes n A great advance in the treatment of CML was to develop a tyrosine kinase inhibitor, that “turns off’ the active TK in the body, specific to the mutated gene, BRC-ABL n The first generation TK inhibitor for CML is imatinib mesylate n

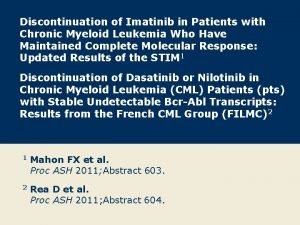
Imatinib mesylate n n n First generation TK inhibitor n Side Effects: Fluid retention (76%), diarrhea (30 -60%), Dosed in 400 mg and 800 mg nausea (43 -73%), fatigue, tablets muscle cramps, bone pain, Binds the closed form of the rash, neutropenia, ATP binding site in BRC-ABL thrombocytopenia (although IRIS study: 97% pts in might be signs of hematological remission and effectiveness) major cytogenic remission was – Most can be alleviated with 87% compared to interferon common medications and are alpha + cytarabine after 19 not a cause of discontinuation months n Resistance occurs IRIS Follow-up five year study: if patient shows a 3 -log molecular response to imatanib, then probability of progression-free survival at 4 years is 98% (Frame 2006)
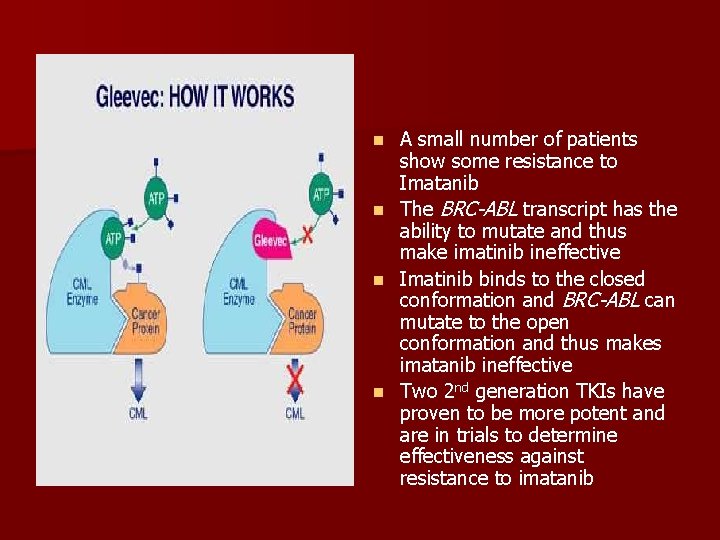
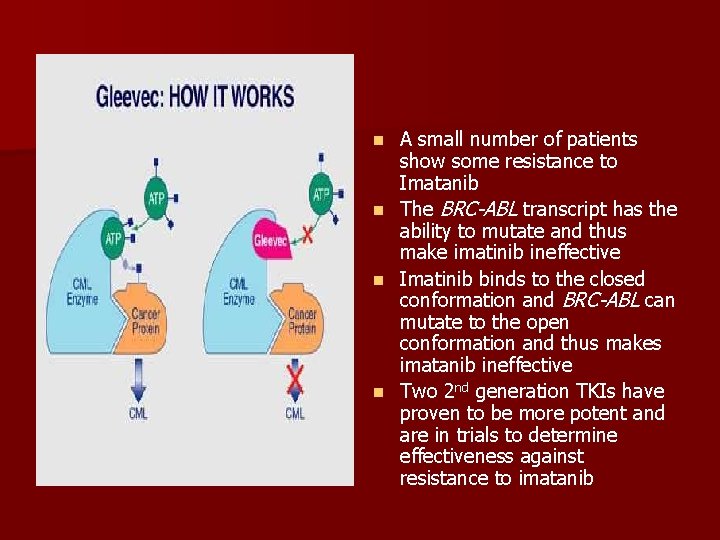
n n A small number of patients show some resistance to Imatanib The BRC-ABL transcript has the ability to mutate and thus make imatinib ineffective Imatinib binds to the closed conformation and BRC-ABL can mutate to the open conformation and thus makes imatanib ineffective Two 2 nd generation TKIs have proven to be more potent and are in trials to determine effectiveness against resistance to imatanib
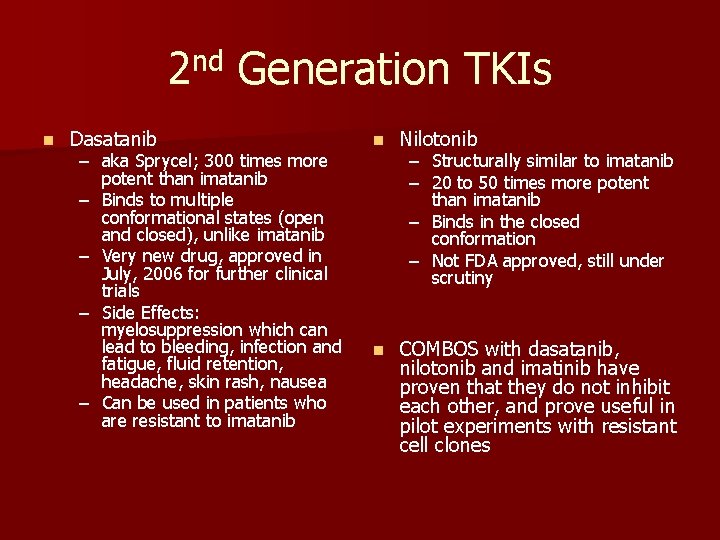
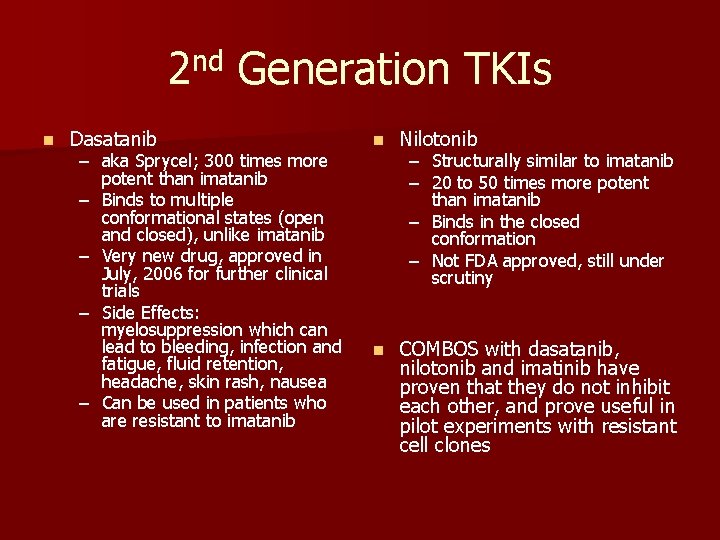
2 nd Generation TKIs n Dasatanib – aka Sprycel; 300 times more potent than imatanib – Binds to multiple conformational states (open and closed), unlike imatanib – Very new drug, approved in July, 2006 for further clinical trials – Side Effects: myelosuppression which can lead to bleeding, infection and fatigue, fluid retention, headache, skin rash, nausea – Can be used in patients who are resistant to imatanib n Nilotonib n COMBOS with dasatanib, nilotonib and imatinib have proven that they do not inhibit each other, and prove useful in pilot experiments with resistant cell clones – Structurally similar to imatanib – 20 to 50 times more potent than imatanib – Binds in the closed conformation – Not FDA approved, still under scrutiny
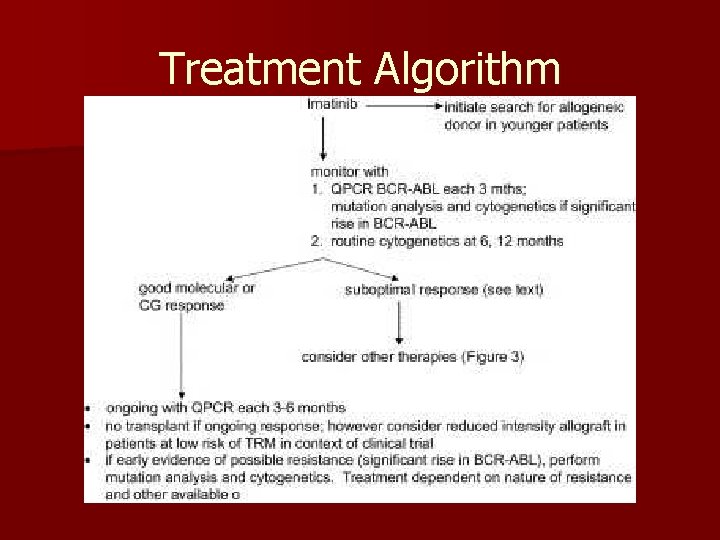
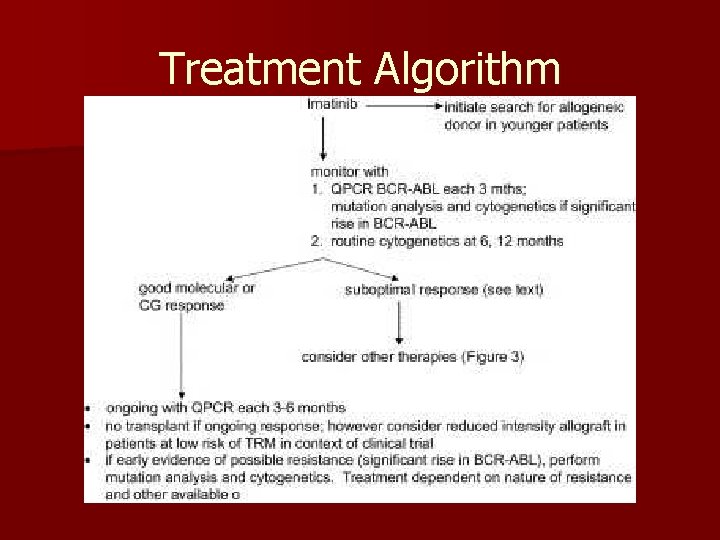
Treatment Algorithm
References n n n n Faderl S, Kantarjian HM. Chronic Myelogenous Leukemia and Other Myeloproliferative Disorders. [ BOOK, check citing!]. ACP Medicine. 2006. vol 2(2570 -79) Fausel C. Novel treatment strategies for chronic myeloid leukemia. Am J Health-Syst Pharm. 2006 Dec 1; 63(Suppl 8): S 15 -S 20. Grigg A, Hughes T. Role of Allogenic Stem Cell Transplantation for Chronic Myeloid Leukemia in the Imatinib Era. Biol Blood Marrow Transplant. 2006 Mar 29; 12: 795 -807. http: //www. gleevec. com/info/page/safety_info http: //www. cmlmedicalmonitor. com/medicalmonitor/education/ayd_response. asp? trial=show http: //www. pharmcast. com/Patents/Yr 2002/Mar 2002/032602/6362162_CM L 032602. htm http: //images. google. com/images? q=PHILADELPHIA+CHROMOSOME+imag e&hl=en&sa=X&oi=images&ct=title http: //commons. wikimedia. org/wiki/Image: Bcr-abl_fusion_gene. jpg