1 Pulmonary Vascular Disease 2 Pleural Disease Prof




- Slides: 54
1. Pulmonary Vascular Disease 2. Pleural Disease Prof. Frank Carey
Pulmonary Circulatuion r Dual l l supply Pulmonary arteries Bronchial arteries r Low pressure system r Pulmonary artery receives entire cardiac output (a filter)
Low pressure system…. r Thin walled vessels r Low incidence of atherosclerosis At normal pressures
Pulmonary Oedema r Accumulation l l of fluid in the lung Interstitium Alveolar spaces r Causes a restrictive pattern of disease
Pulmonary Oedema (causes) Haemodynamic ( hydrostatic pressure) Due to cellular injury 1. 2. Alveolar lining cells ii. Alveolar endothelium Localised – pneumonia Generalised – adult respiratory distress syndrome (ARDS) i.
ARDS r Diffuse alveolar damage syndrome (DADS) r Shock lung l Causes include sepsis, diffuse infection (virus, mycoplasma), severe trauma, oxygen
Pathogenesis of ARDS Injury (eg bacterial endotoxin) r Infiltration of inflammatory cells r Cytokines r Oxygen free radicals r Injury to cell membranes
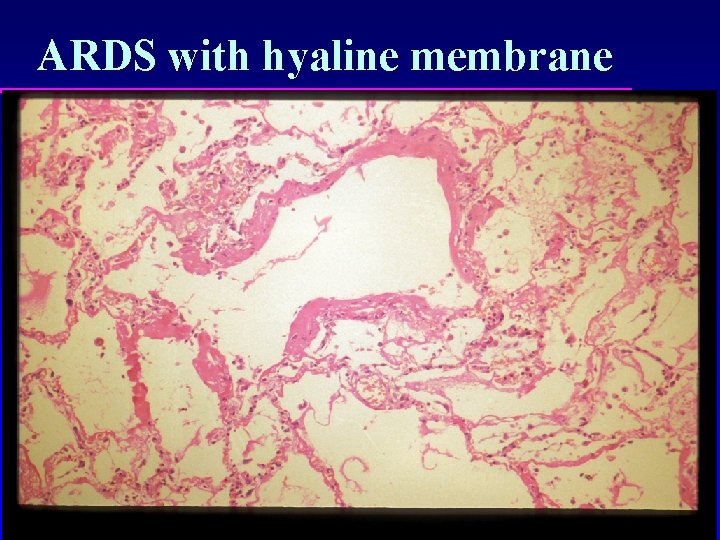
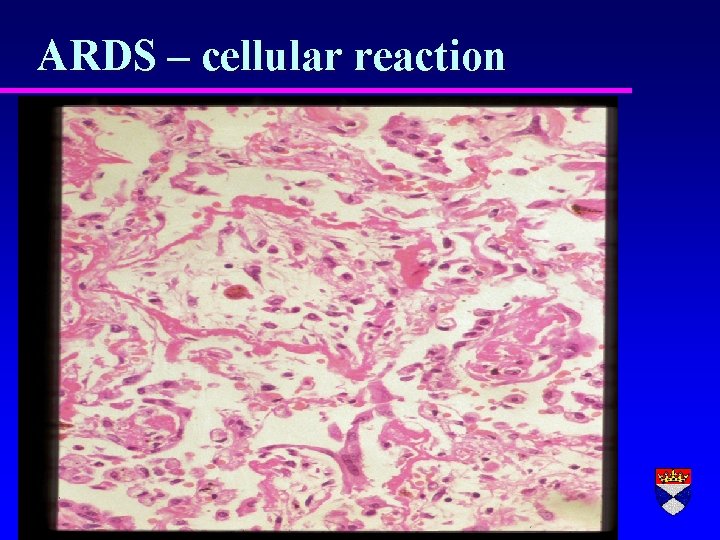
Pathology of ARDS r Fibrinous exudate lining alveolar walls (hyaline membranes) r Cellular regeneration r Inflammation
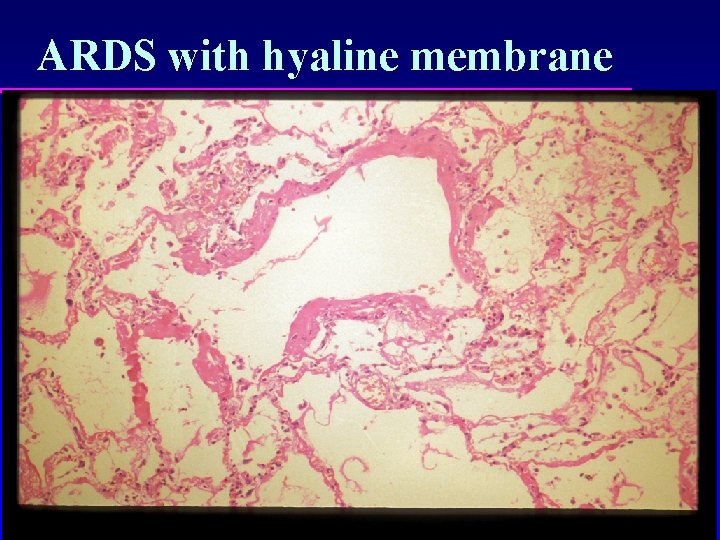
ARDS with hyaline membrane
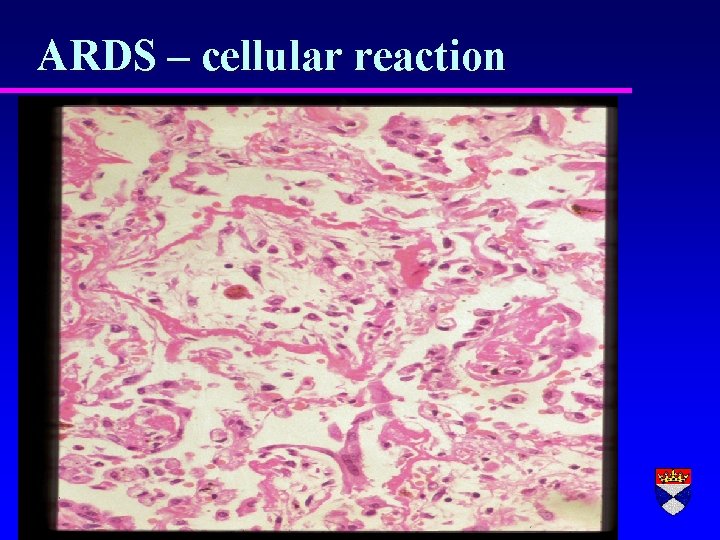
ARDS – cellular reaction
Outcome of ARDS r Death r Resolution r Fibrosis (chronic restrictive lung disease
Neonatal RDS r Premature infants r Deficient in surfactant (type 2 alveolar lining cells r Increased effort in expanding lung physical damage to cells
Embolus r. A detached intravascular mass carried by the blood to a site in the body distant from its point of origin r Most emboli are thrombi – others include gas, fat, foreign bodies and tumour clumps
Pulmonary Embolus r Common r Often subclinical r An important cause of sudden death and pulmonary hypertension 95% + of emboli are thromboemboli
Source of most pulmonary emboli…. . r Deep limbs venous thrombosis (DVT) of lower

Risk factors for PE are those for DVT…. 1. 2. 3. Factors in vessel wall (eg endothelial hypoxia) Abnormal blood flow (venous stasis) Hypercoaguable blood (cancer patients, post-MI etc) - Virchow’s triad
Effects of PE r Sudden death r Severe chest pain/dyspnoea/haemoptysis r Pulmonary infarction r Pulmonary hypertension
Effects of PE depend on… r Size of embolus r Cardiac function r Respiratory function
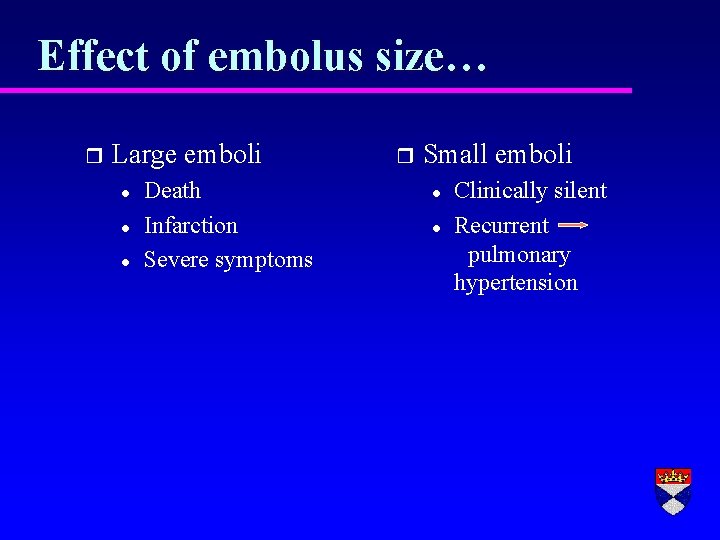
Effect of embolus size… r Large emboli l l l Death Infarction Severe symptoms r Small emboli l l Clinically silent Recurrent pulmonary hypertension
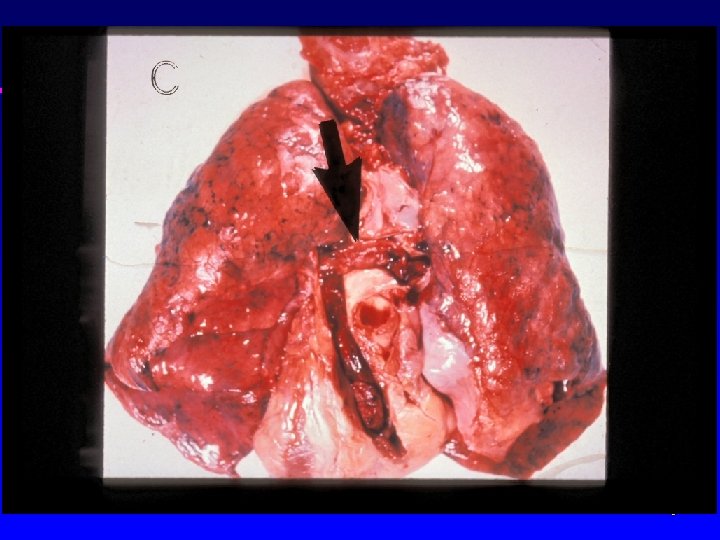
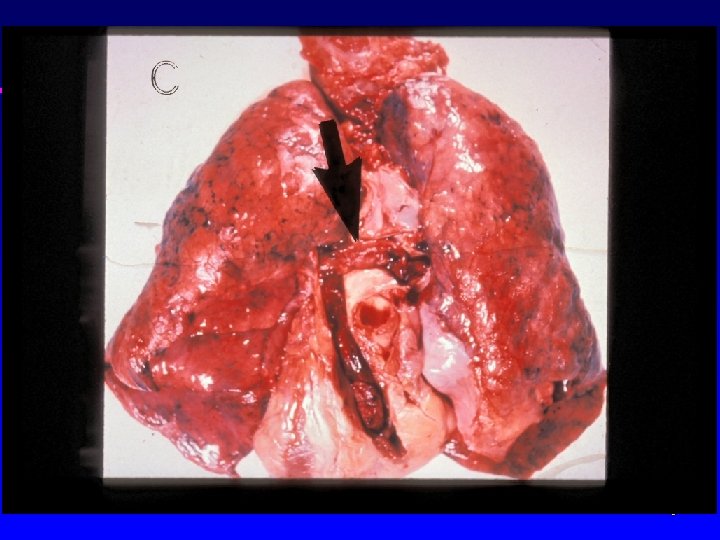
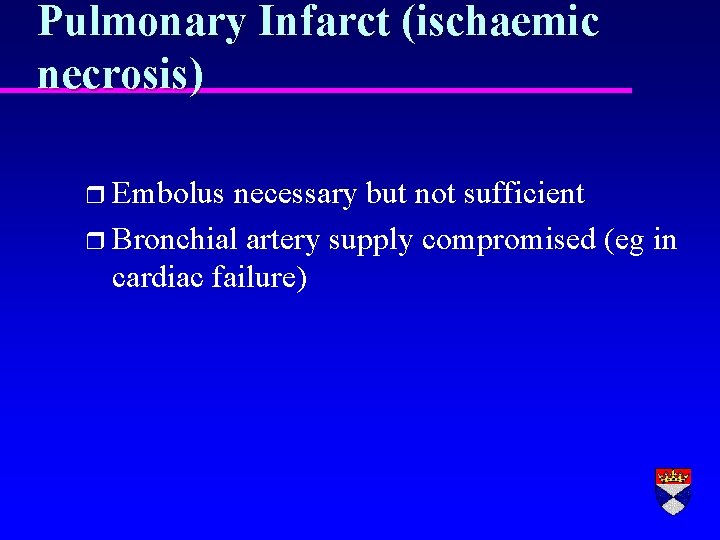
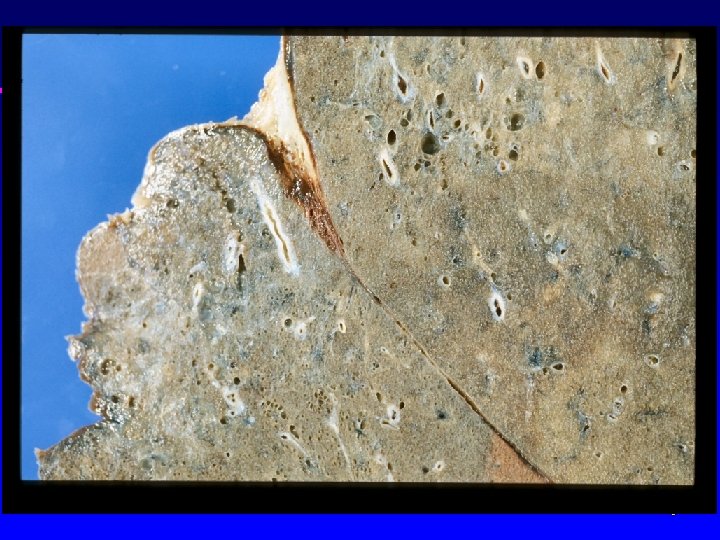
Pulmonary Infarct (ischaemic necrosis) r Embolus necessary but not sufficient r Bronchial artery supply compromised (eg in cardiac failure)
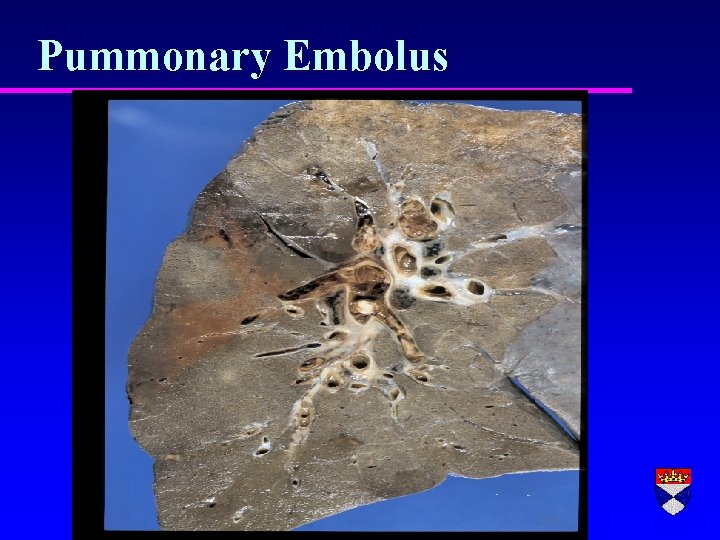
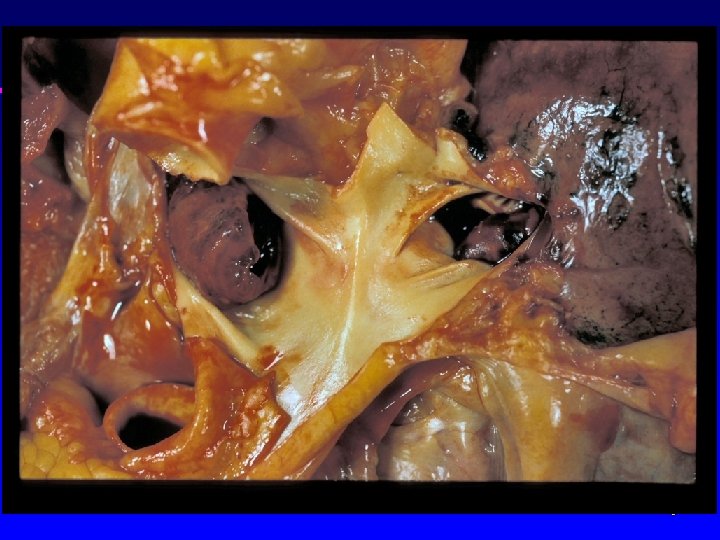
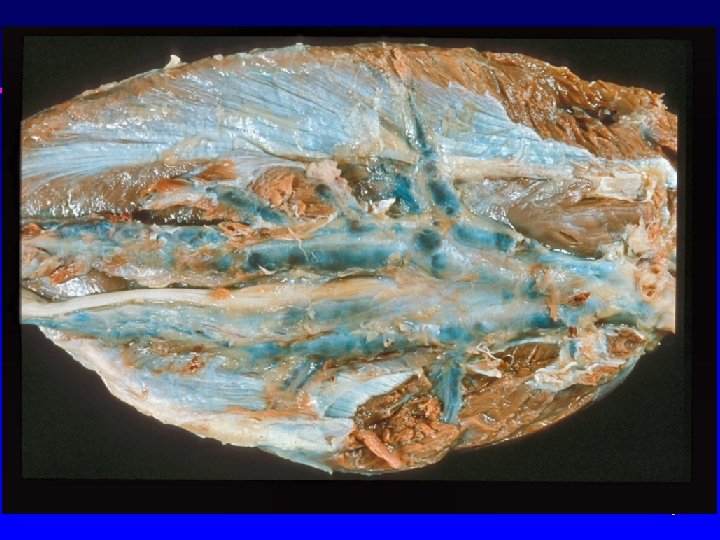
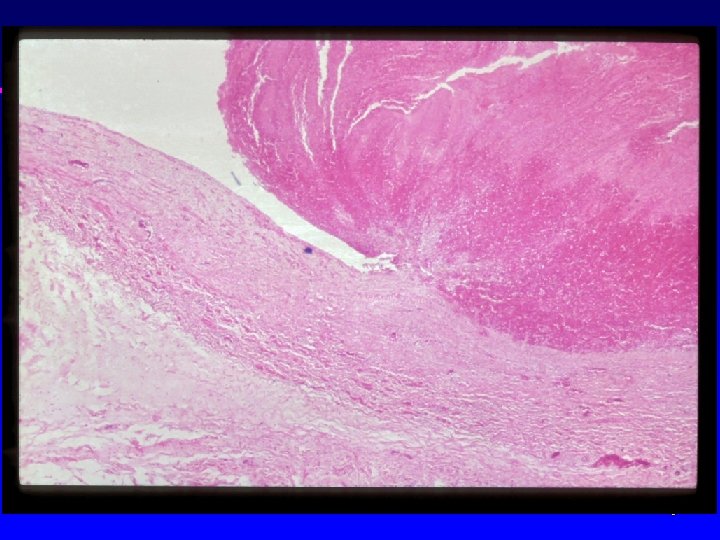
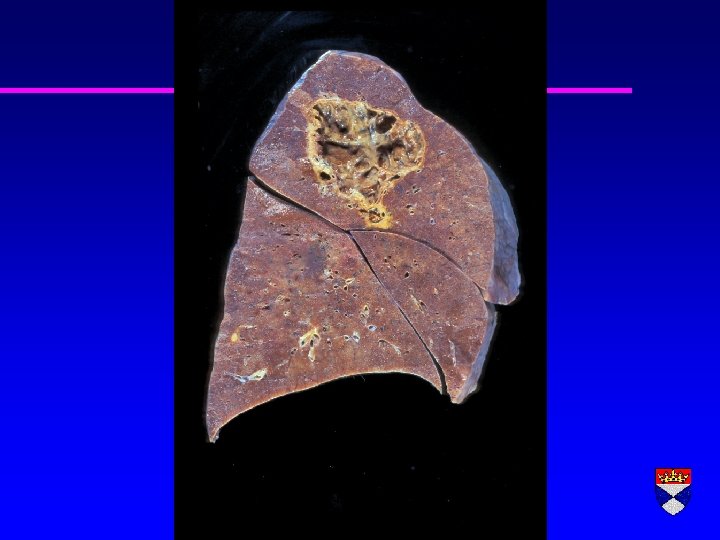
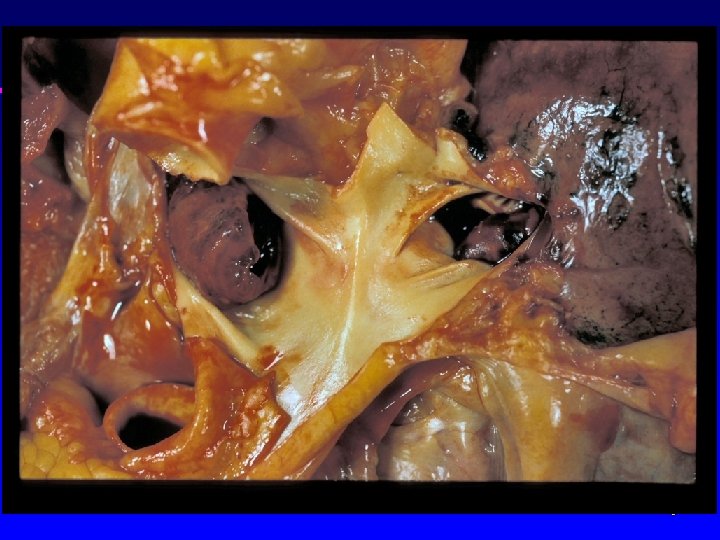
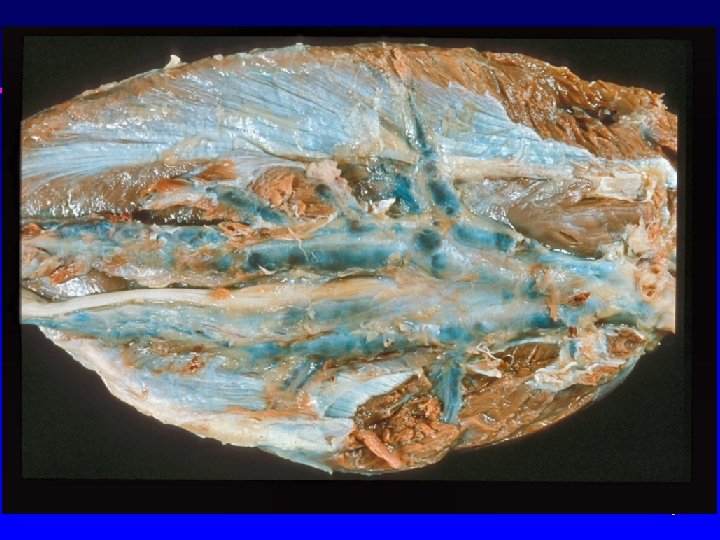
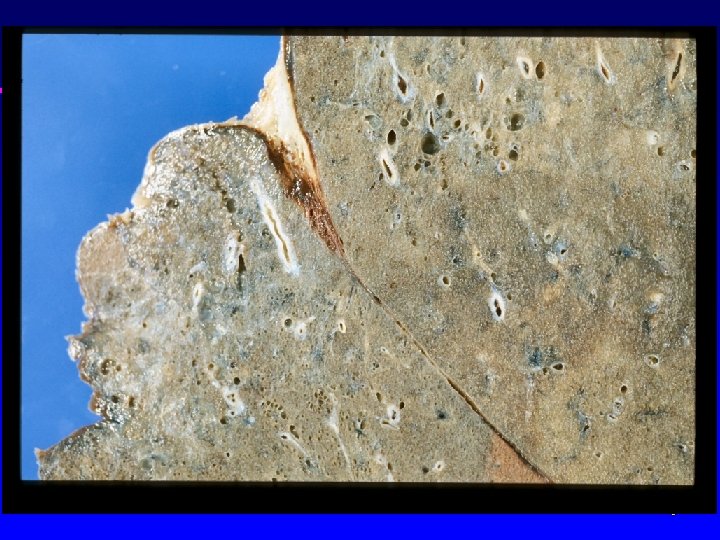
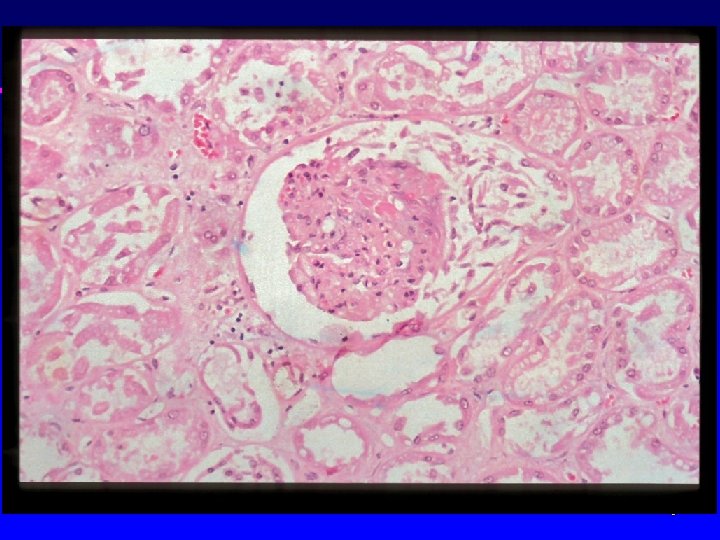
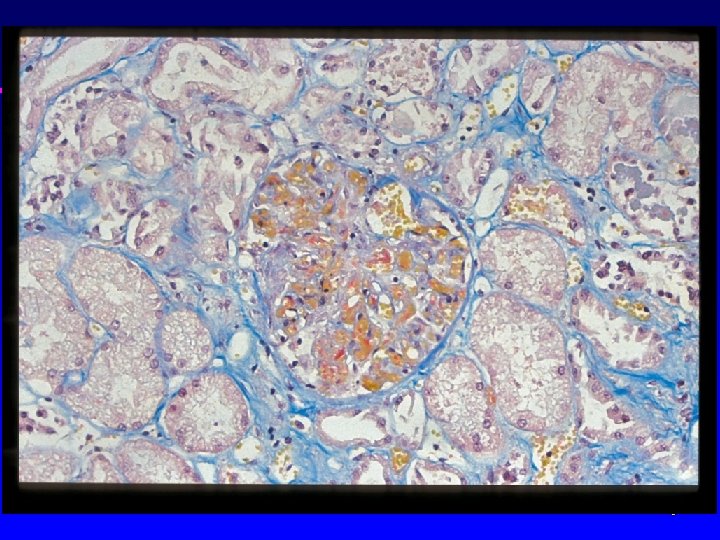
Pummonary Embolus

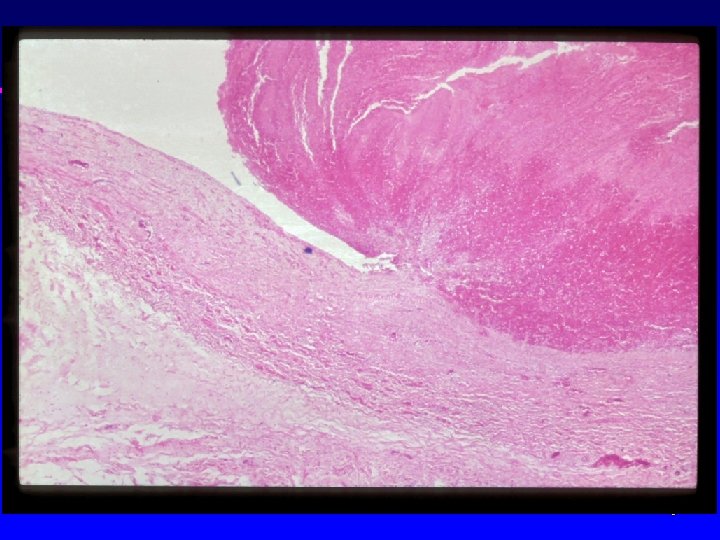
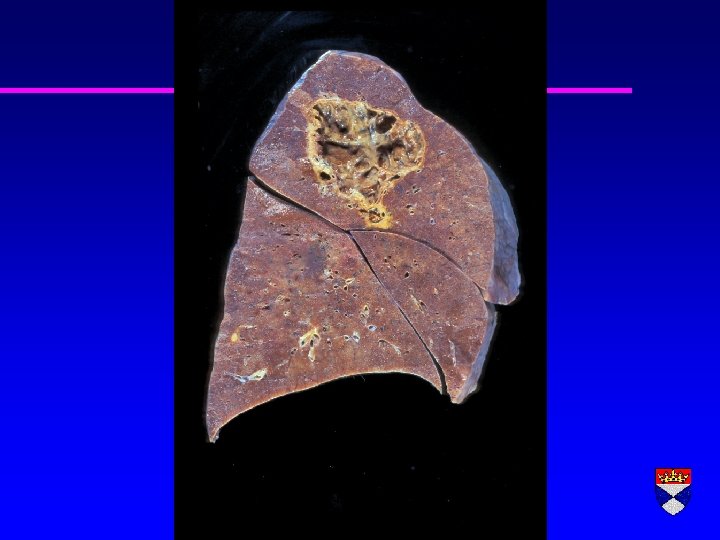
Pulmonary infarct – tumour embolus
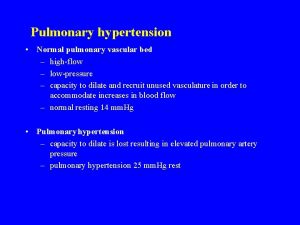
Pulmonary Hypertension r Primary (rare, young women) r Secondary
Pulmonary Hypertension (mechanisms) r Hypoxia (vascular constriction) r Increased flow through pulmonary circulation (congenital heart disease) r Blockage (PE) or loss (emphysema) of pulmonary vascular bed r Back pressure from left sided heart failure
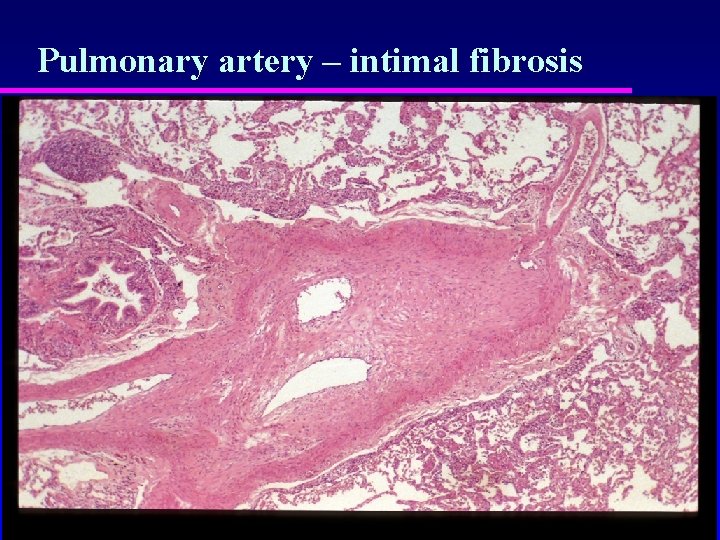
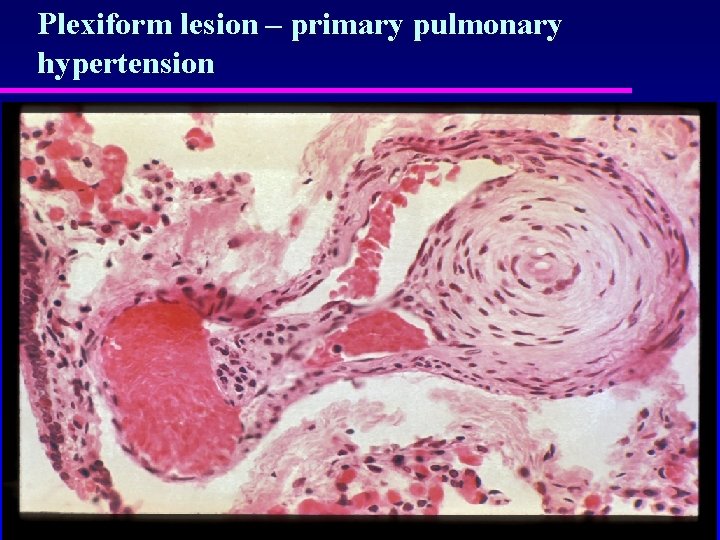
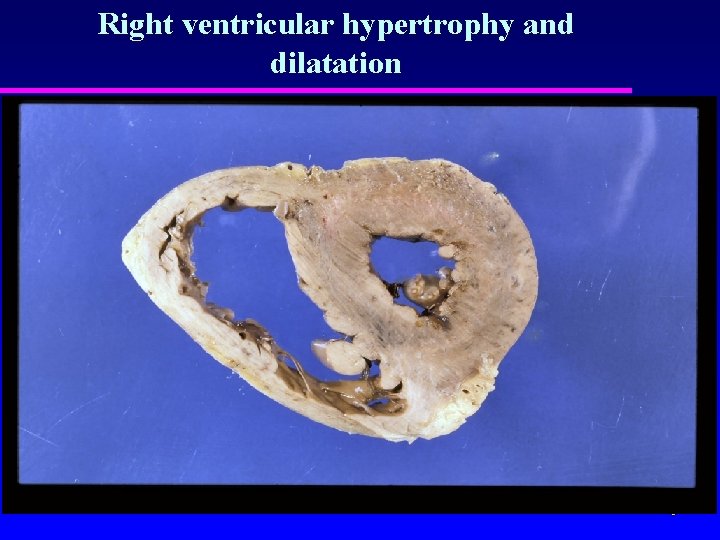
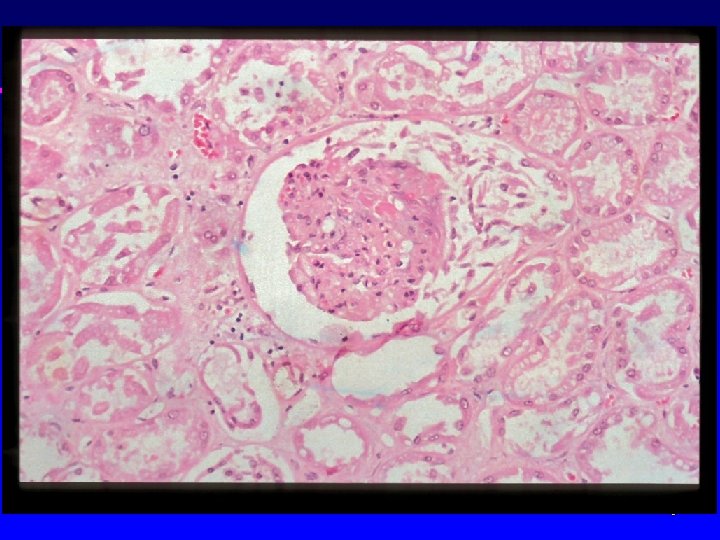
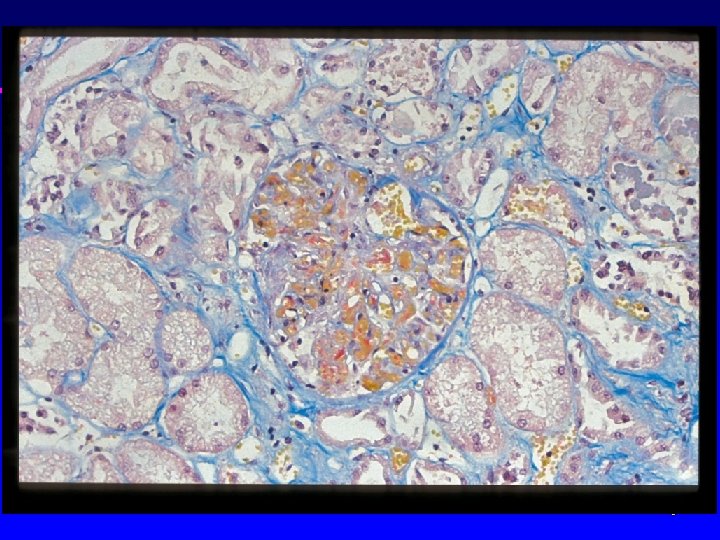
Morphology of pulmonary hypertension r Medial hypertrophy of arteries r Intimal thickening (fibrosis) r Atheroma r Right ventricular hypertrophy r Extreme cases (congenital heart disease, primary pulmonary hypertension) – plexogenic change/necrosis
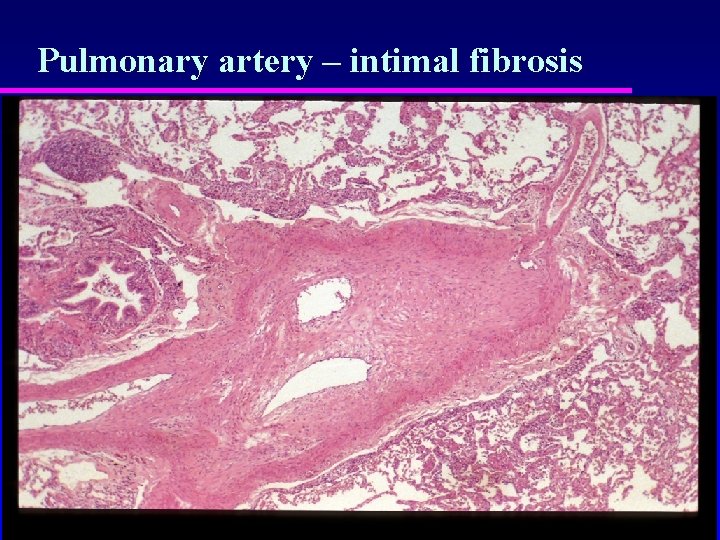
Pulmonary artery – intimal fibrosis
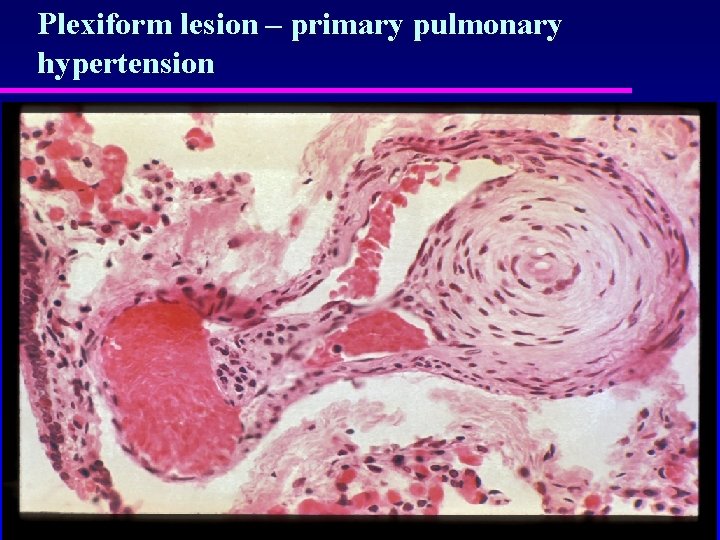
Plexiform lesion – primary pulmonary hypertension
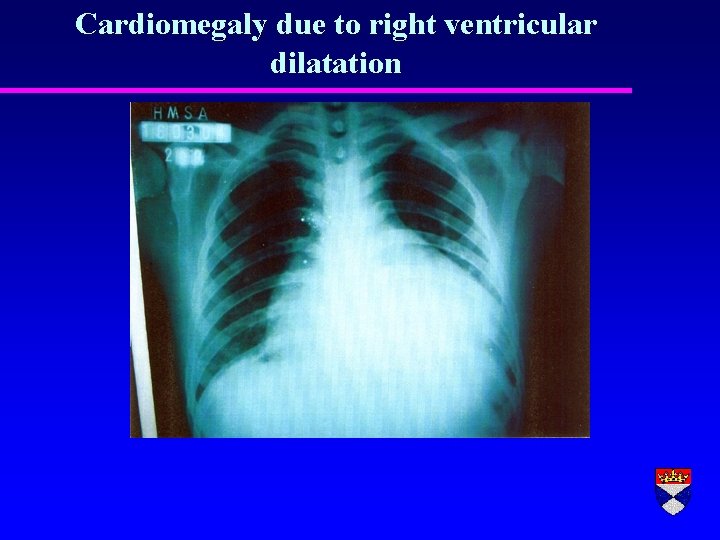
“Cor Pulmonale” r Pulmonary hypertension complicating lung disease r Right ventricular hypertrophy r Right ventricular dilatation r Right heart failure (swollen legs, congested liver etc)
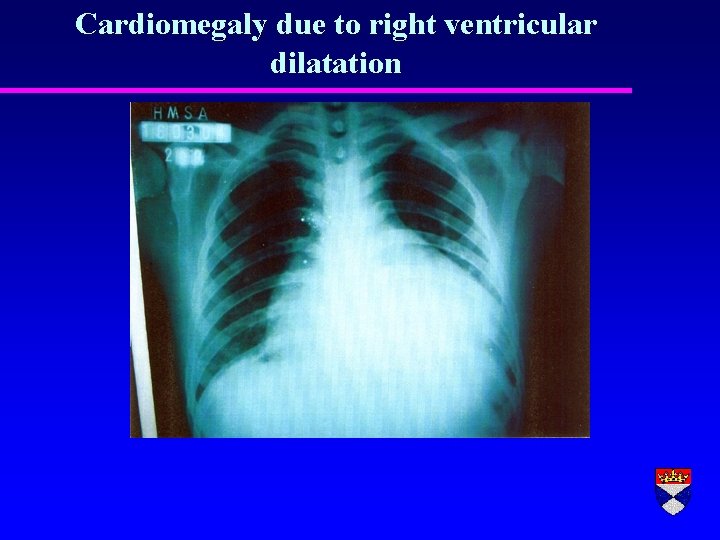
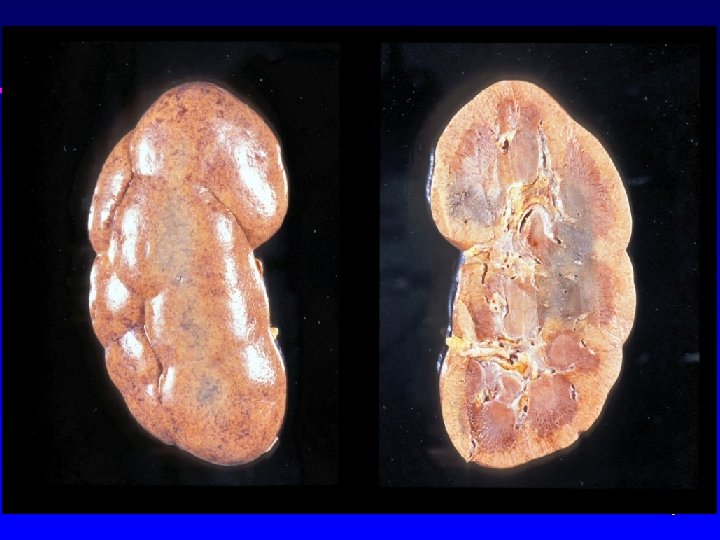
Cardiomegaly due to right ventricular dilatation
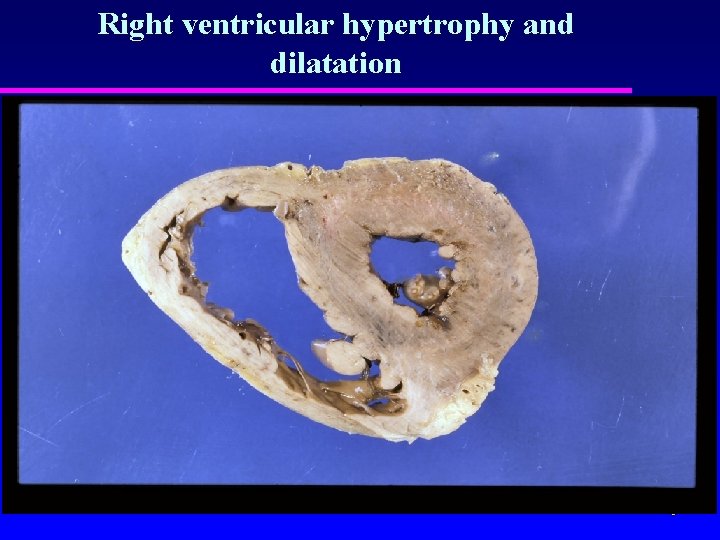
Right ventricular hypertrophy and dilatation
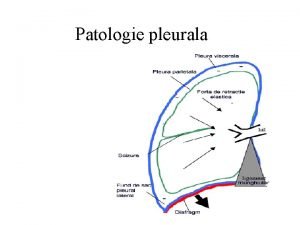
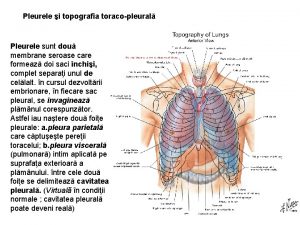
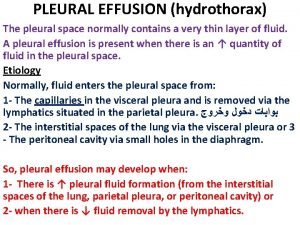
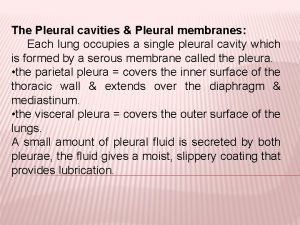
The Pleura r. A mesothelial surface lining the lungs and mediastinum r Mesothelial cells designed for fluid absorption r Hallmark of disease is the effusion
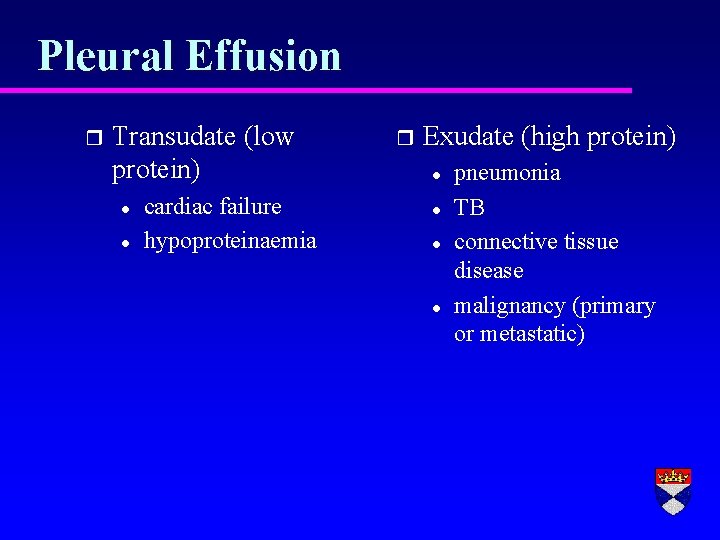
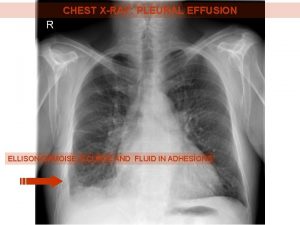
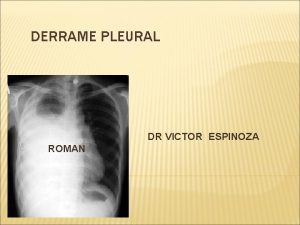
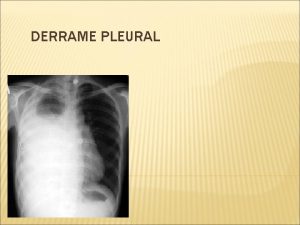
Pleural Effusion r Transudate (low protein) l l cardiac failure hypoproteinaemia r Exudate (high protein) l l pneumonia TB connective tissue disease malignancy (primary or metastatic)
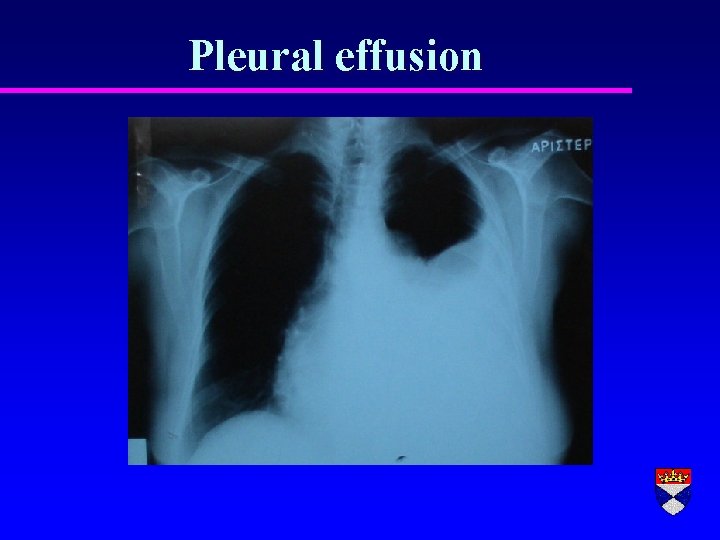
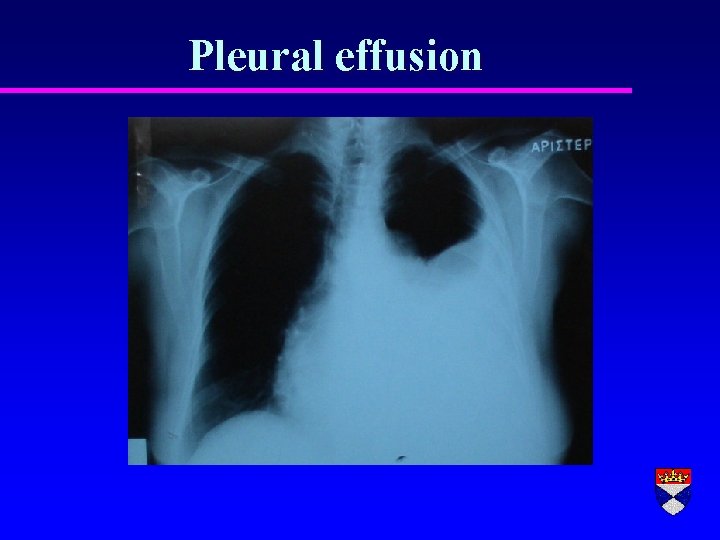
Pleural effusion
Purulent Effusion Full of acute inflammatory cells r Empyema r Can become chronic
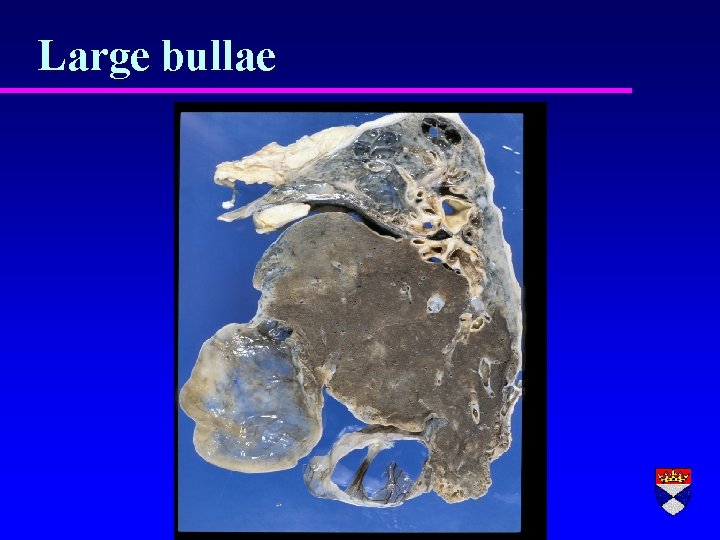
Pneumothorax Air in pleural space r Trauma r Rupture of bulla
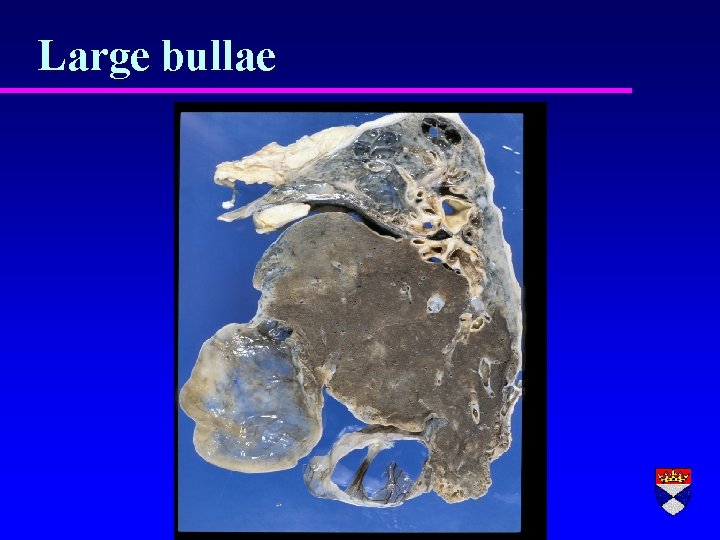
Large bullae
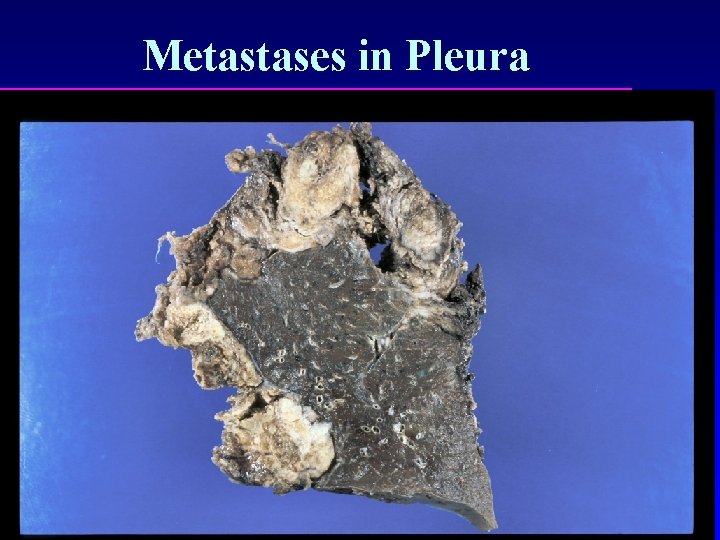
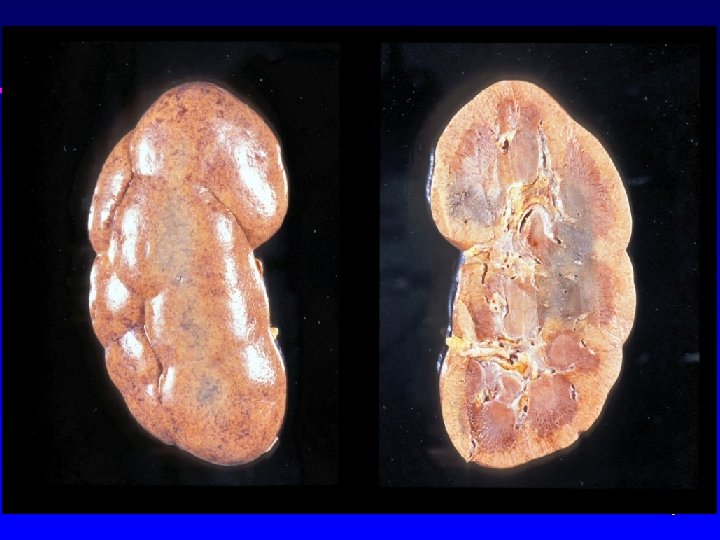
Pleural Neoplasia r Primary l l benign (rare) malignant mesothelioma r Secondary l common (adenocarcinomas - lung, GIT, ovary)
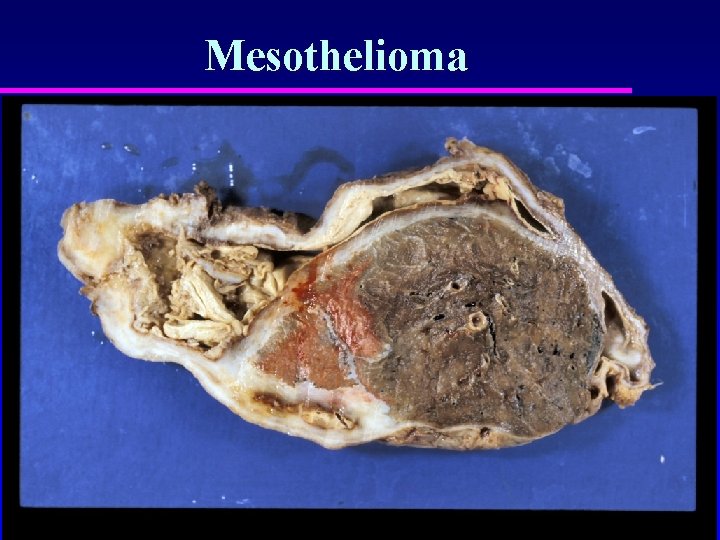
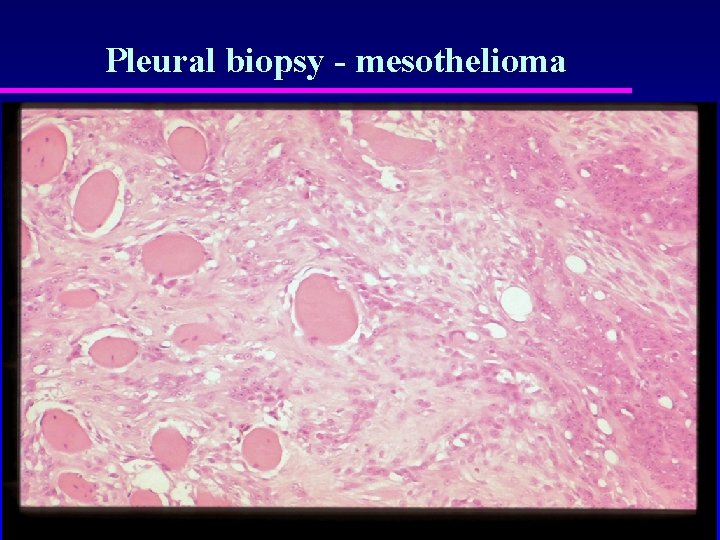
Mesothelioma r Asbestosis related r Increasing incidence r Mixed epithelial/mesenchymal differentiation r Dismal prognosis
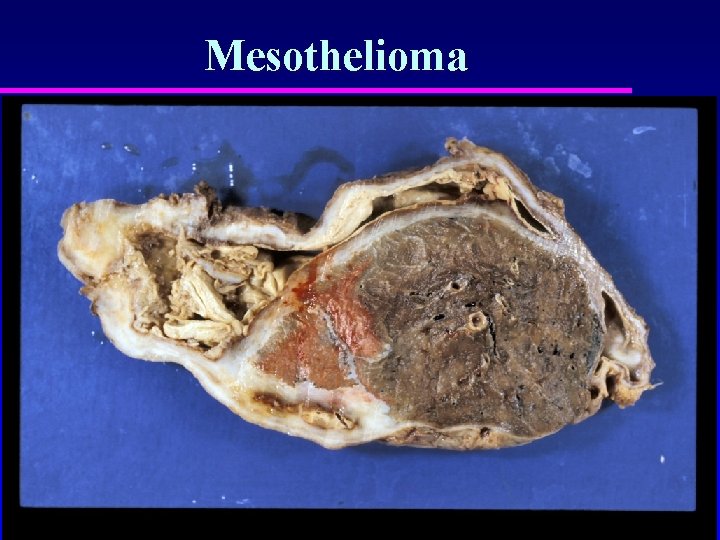
Mesothelioma
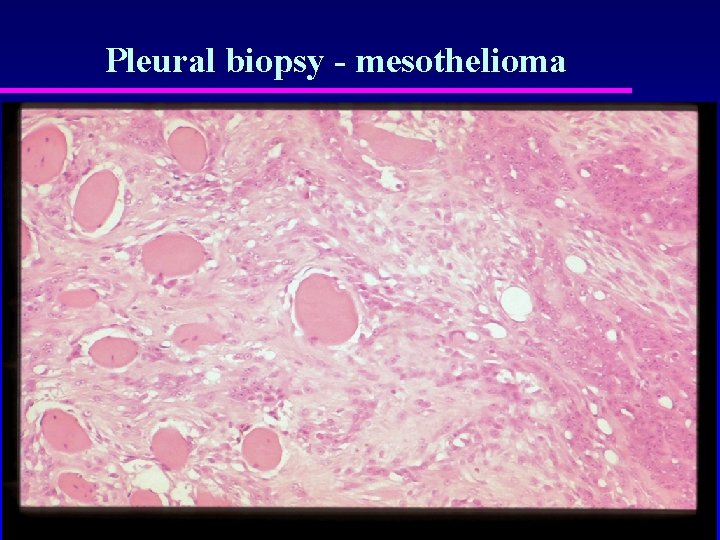
Pleural biopsy - mesothelioma
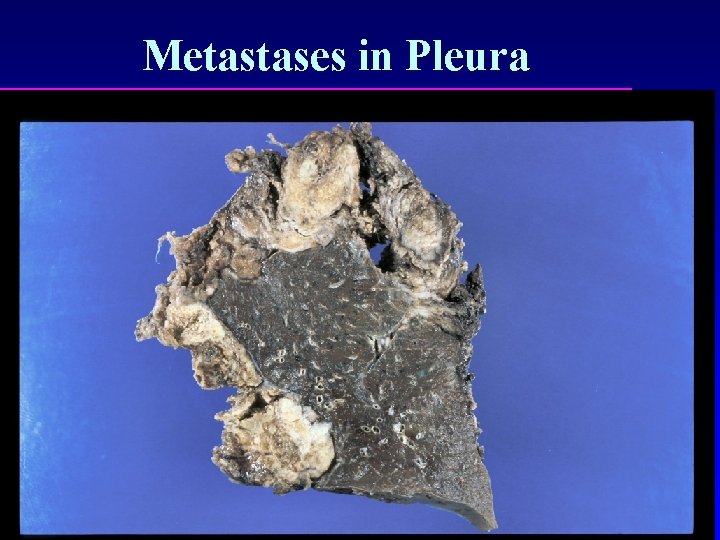
Metastases in Pleura
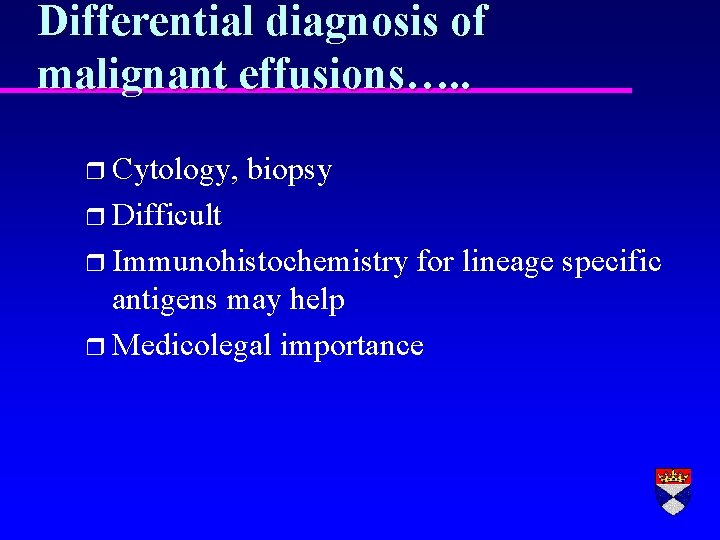
Differential diagnosis of malignant effusions…. . r Cytology, biopsy r Difficult r Immunohistochemistry for lineage specific antigens may help r Medicolegal importance


 Svr calculation
Svr calculation How to calculate systemic vascular resistance
How to calculate systemic vascular resistance Normal pulmonary vascular resistance
Normal pulmonary vascular resistance How to calculate pulmonary vascular resistance
How to calculate pulmonary vascular resistance Non vascular vs vascular plants
Non vascular vs vascular plants Life cycle of seedless plants
Life cycle of seedless plants Vascular and non vascular difference
Vascular and non vascular difference Copd means
Copd means Pulmonary disease definition
Pulmonary disease definition Vascular bundles definition
Vascular bundles definition Bharathi viswanathan
Bharathi viswanathan Diferença de exsudato e transudato
Diferença de exsudato e transudato Kerley b lines
Kerley b lines Infarto pulmonar
Infarto pulmonar Lung
Lung Pleural rub
Pleural rub Cardiac notch
Cardiac notch Pleural fluid color chart
Pleural fluid color chart Pleural effusion abg results
Pleural effusion abg results Cloisonnement pleural
Cloisonnement pleural Pleural effusion concept map
Pleural effusion concept map Pleural fissures
Pleural fissures Serosangineous
Serosangineous Exsudat transudat
Exsudat transudat Difference between transudate and exudate
Difference between transudate and exudate Foita parietala
Foita parietala Sonda de pleurostomia
Sonda de pleurostomia Pleural membrane
Pleural membrane Pleural tapping notes
Pleural tapping notes Chest expansion test
Chest expansion test Pleura
Pleura Hydrothorax causes
Hydrothorax causes Neumotorax hemotorax hidrotorax piotorax
Neumotorax hemotorax hidrotorax piotorax Angulos costofrenicos
Angulos costofrenicos Chylous ascites lymphoma
Chylous ascites lymphoma Criterios de light derrame pleural
Criterios de light derrame pleural Ellis s curve pleural effusion
Ellis s curve pleural effusion Bourse drain thoracique
Bourse drain thoracique Pleural recesses
Pleural recesses Grados de hemotorax
Grados de hemotorax Ecografa
Ecografa Pleural effusion color chart
Pleural effusion color chart Diaphragmatic impression
Diaphragmatic impression Antonio cuñarro
Antonio cuñarro Cavidade pleural
Cavidade pleural Micronoduli centrolobulari
Micronoduli centrolobulari Fremitus lungs
Fremitus lungs Liquido pleural color marron
Liquido pleural color marron Light's criteria
Light's criteria Hemoneumotorax
Hemoneumotorax Pleural empyema
Pleural empyema Dr kelechi okoli
Dr kelechi okoli Light criterios
Light criterios Pleural effusion ellis curve
Pleural effusion ellis curve Quilotorax y pseudoquilotorax
Quilotorax y pseudoquilotorax