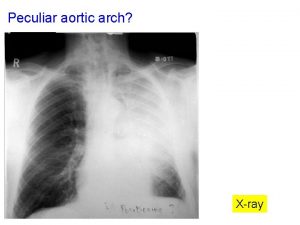
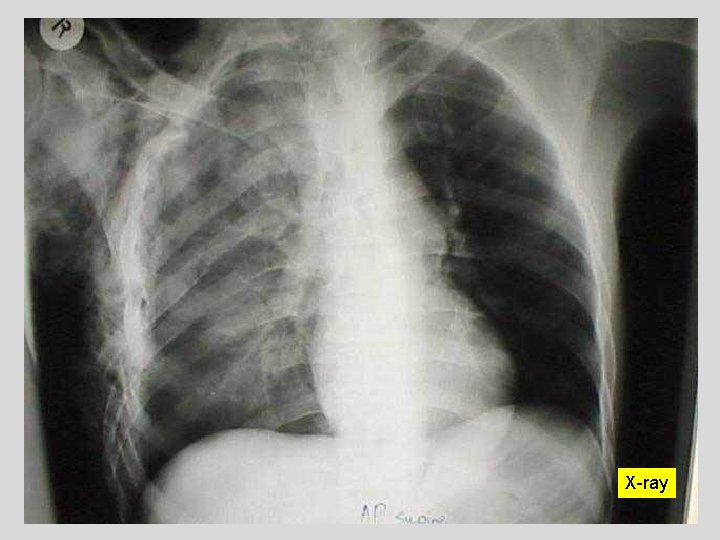
Xray Peculiar aortic arch arlllckkkh Peculiar aortic arch





- Slides: 64
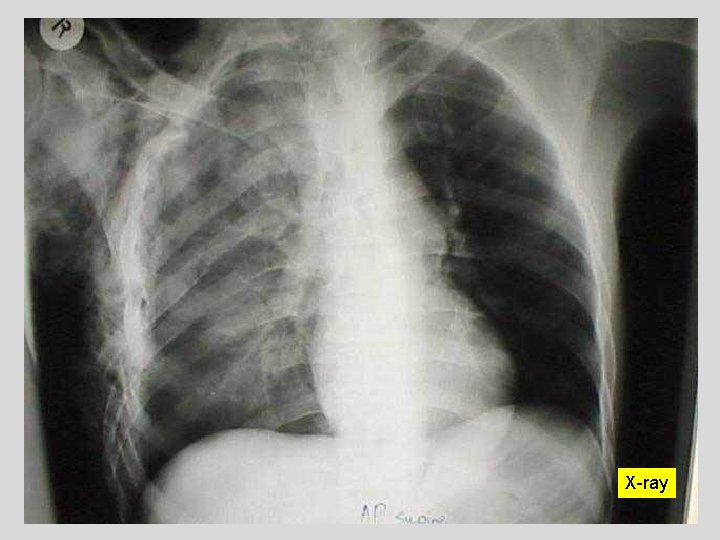
X-ray
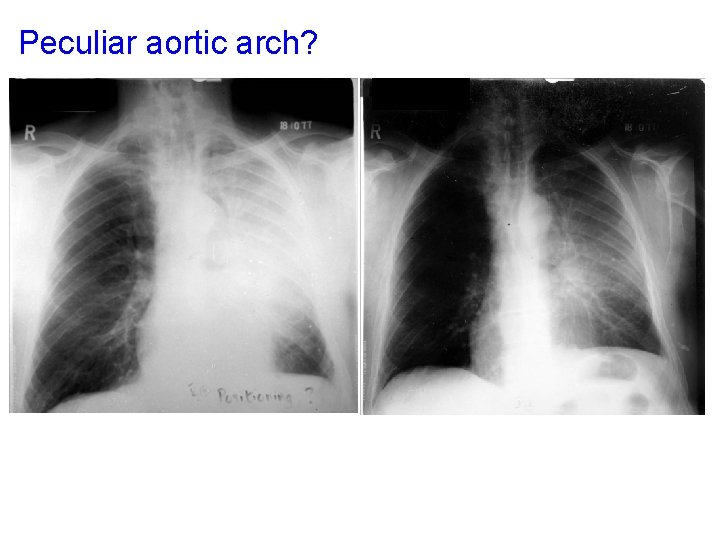
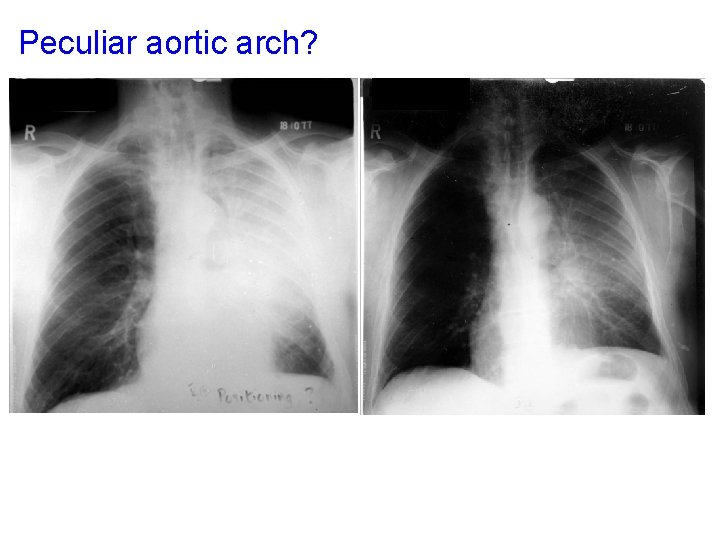
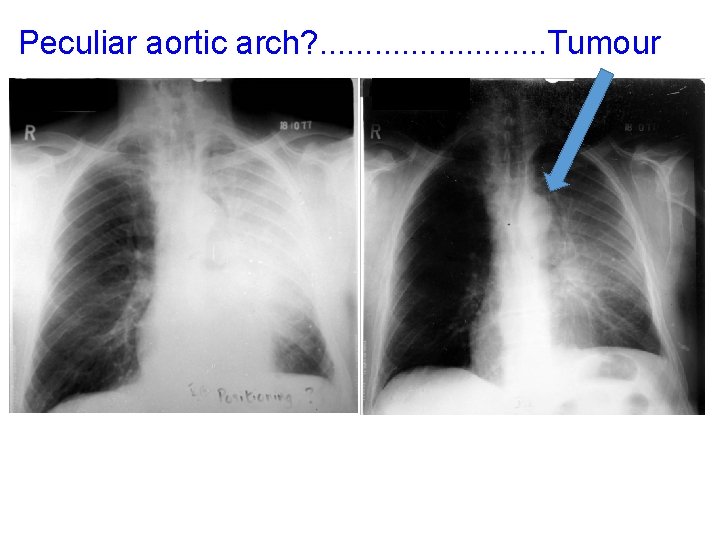
Peculiar aortic arch? arlllckkkh
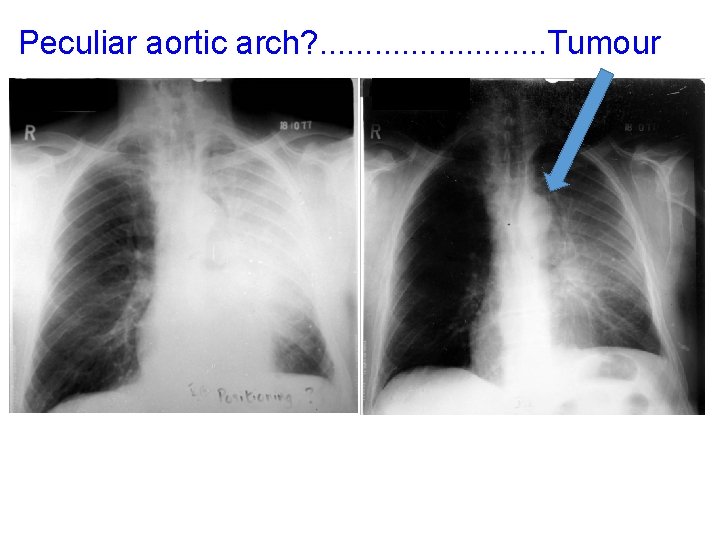
Peculiar aortic arch? . . . Tumour arlllckkkh
PT to increase lung volume • (Pain management) • Positioning • Neurophysiological facilitation of respiration • Deep breathing • Manual hyperinflation
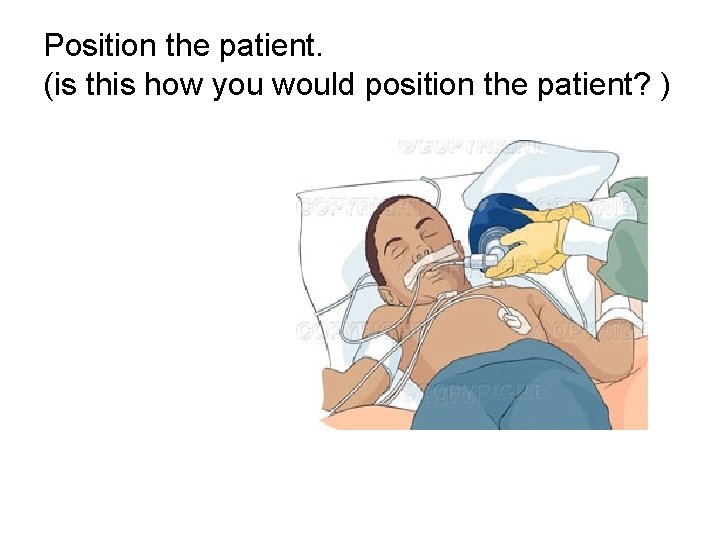
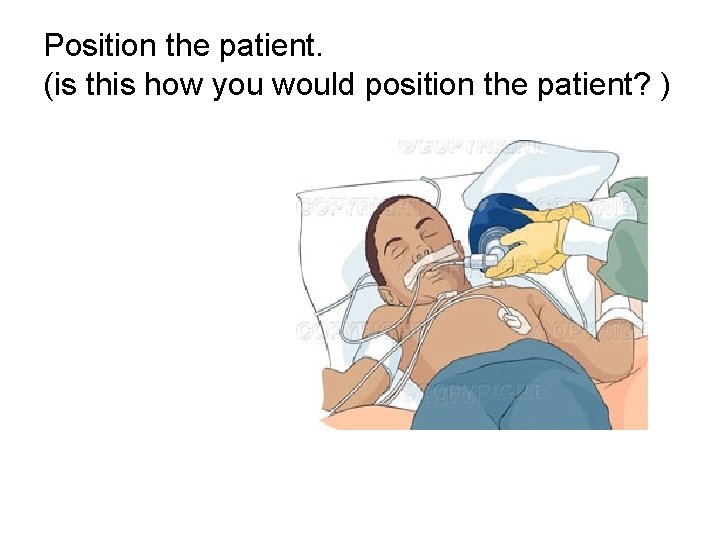
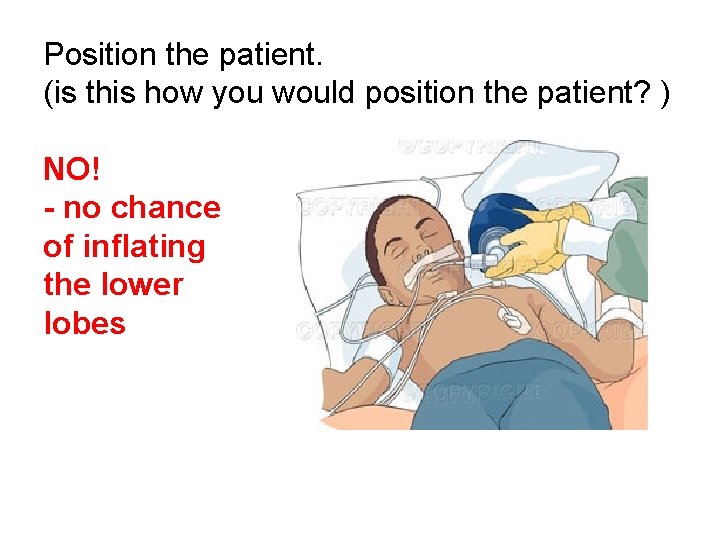
Position the patient. (is this how you would position the patient? )
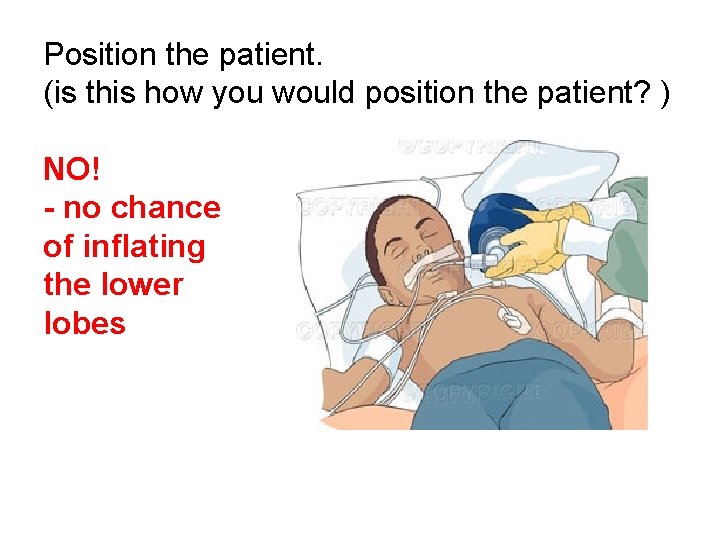
Position the patient. (is this how you would position the patient? ) NO! - no chance of inflating the lower lobes
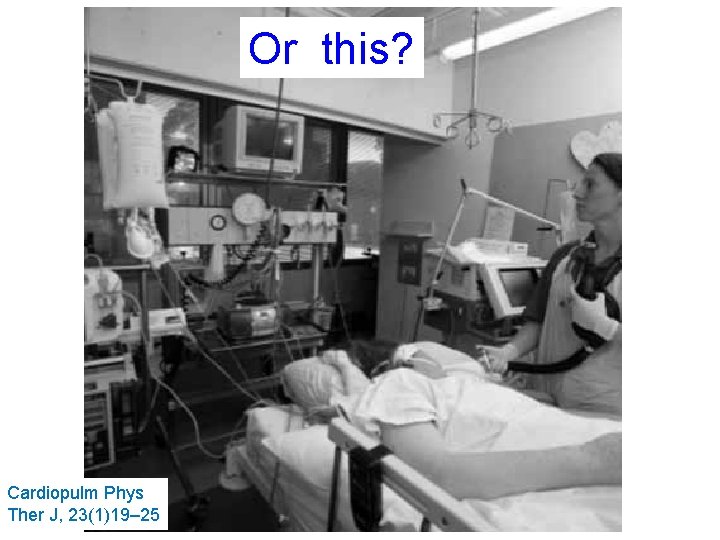
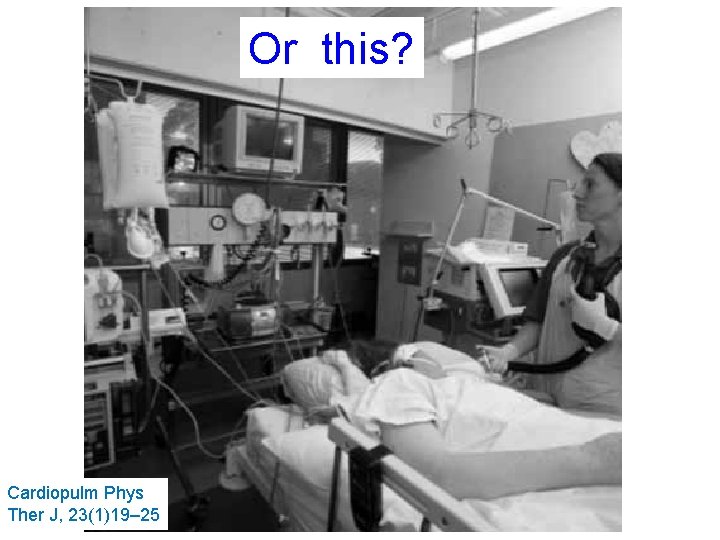
Or this? Cardiopulm Phys Ther J, 23(1)19– 25
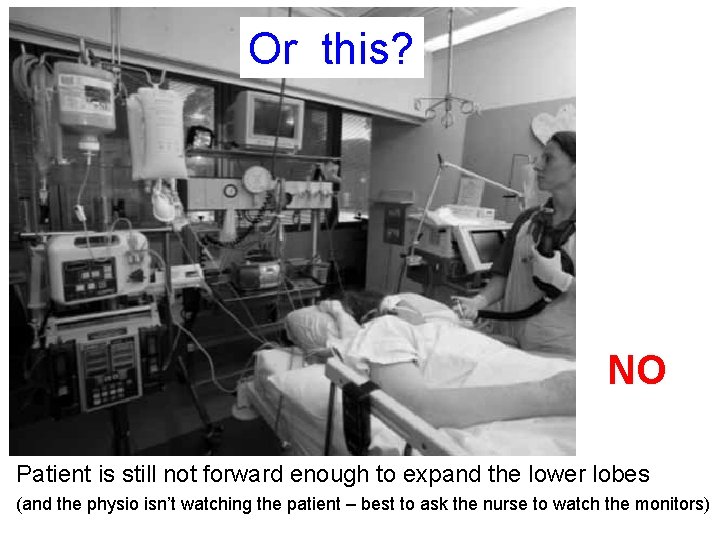
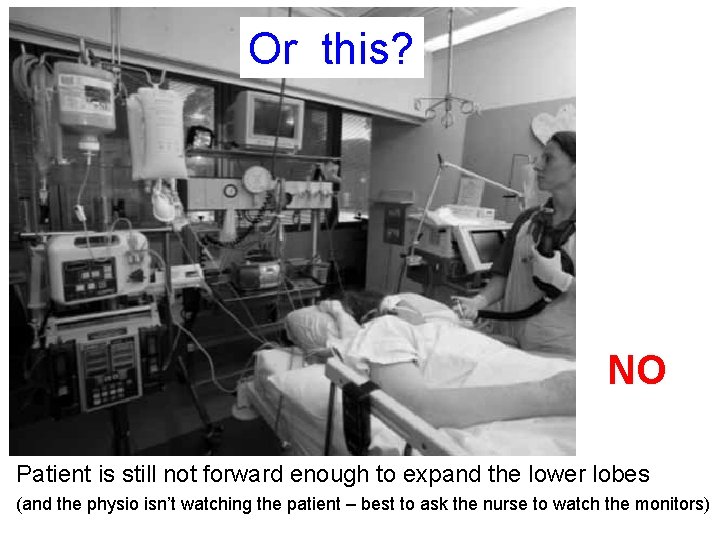
Or this? NO Patient is still not forward enough to expand the lower lobes (and the physio isn’t watching the patient – best to ask the nurse to watch the monitors)
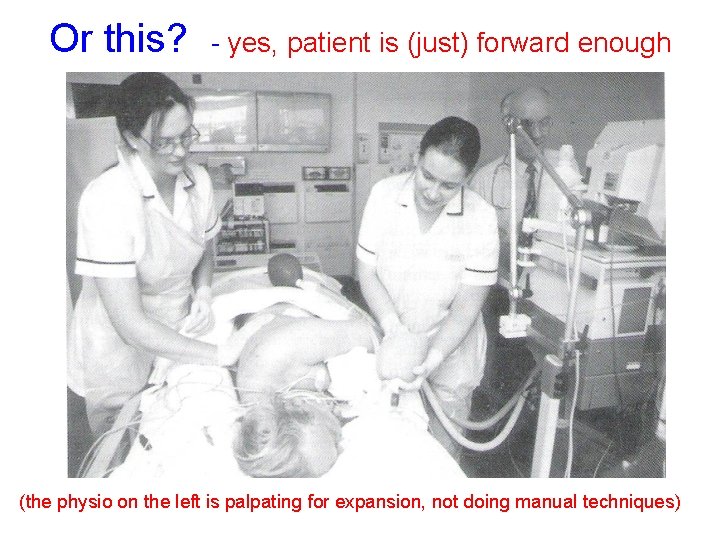
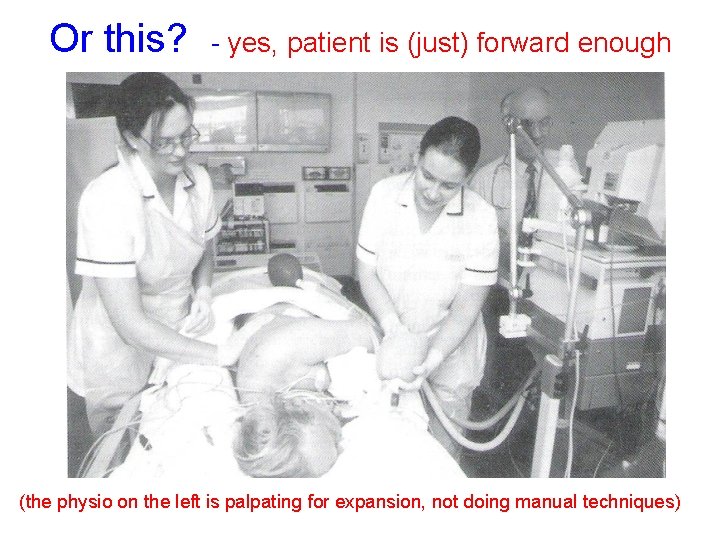
Or this? - yes, patient is (just) forward enough (the physio on the left is palpating for expansion, not doing manual techniques)
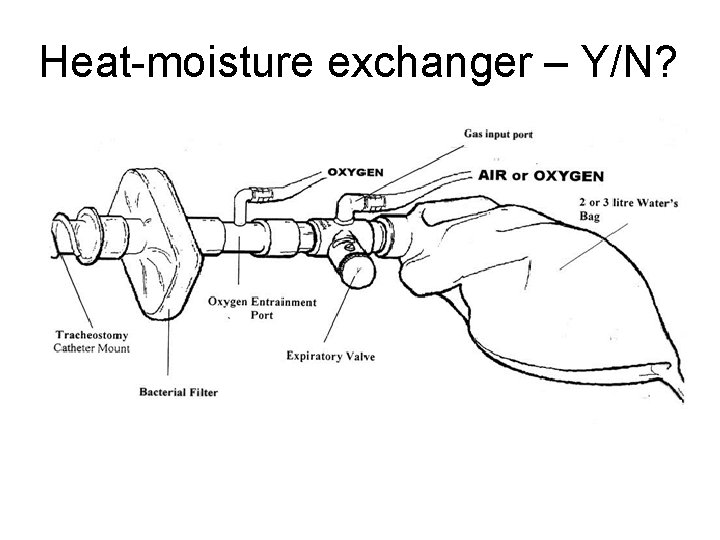
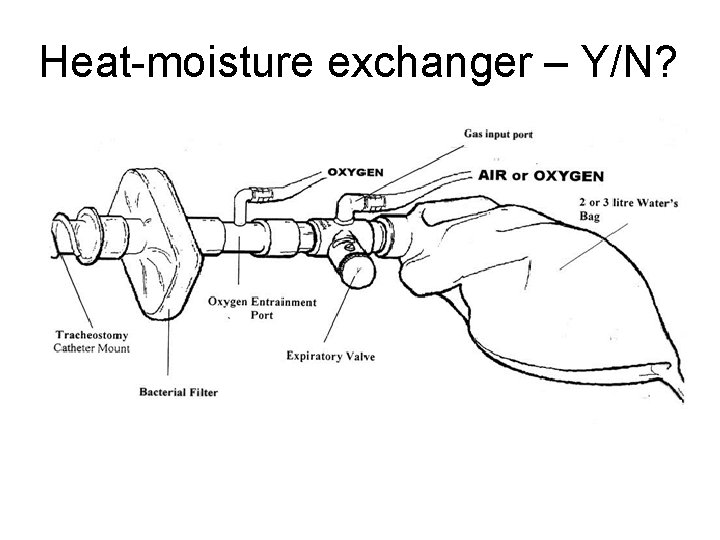
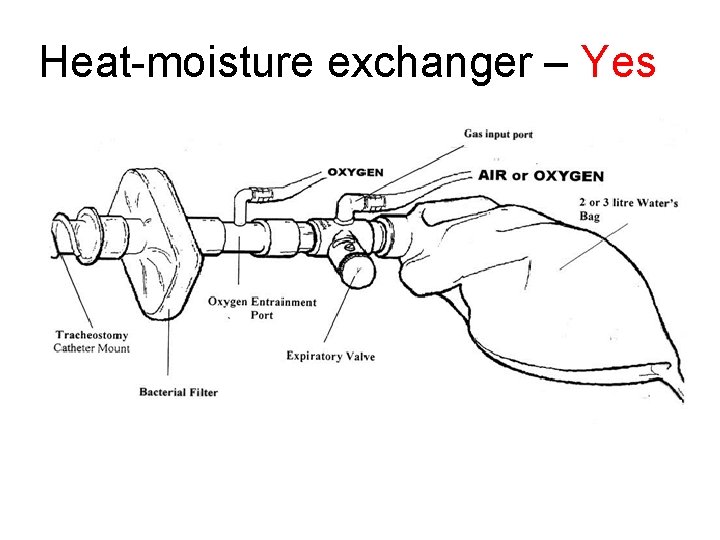
Heat-moisture exchanger – Y/N?
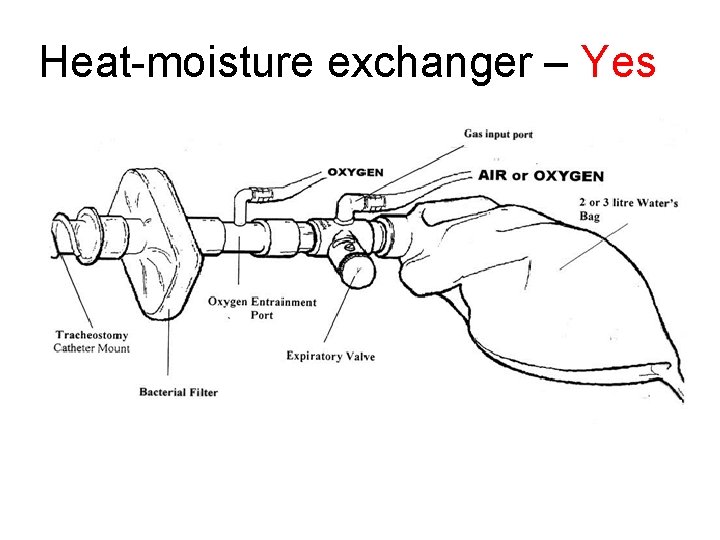
Heat-moisture exchanger – Yes
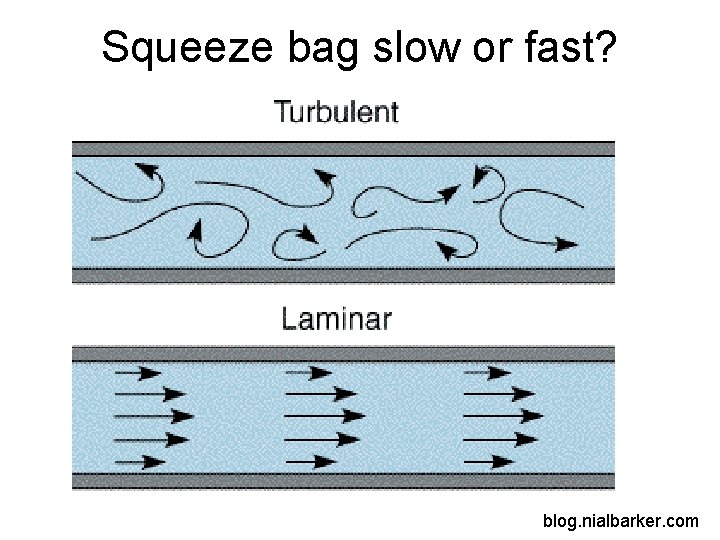
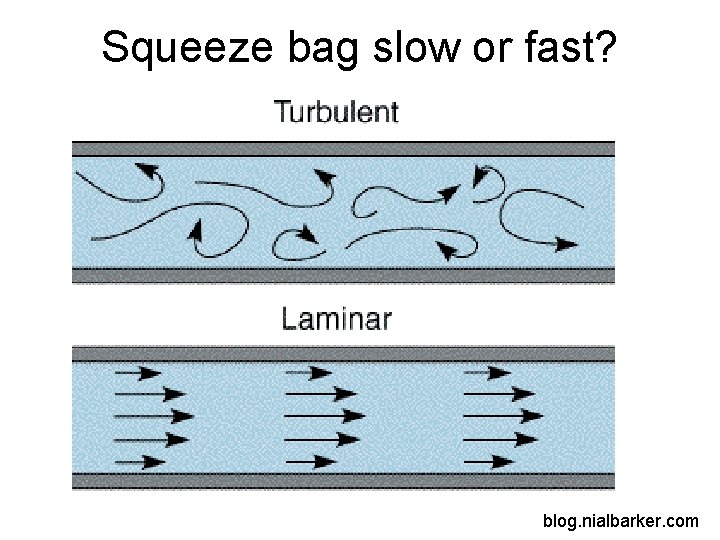
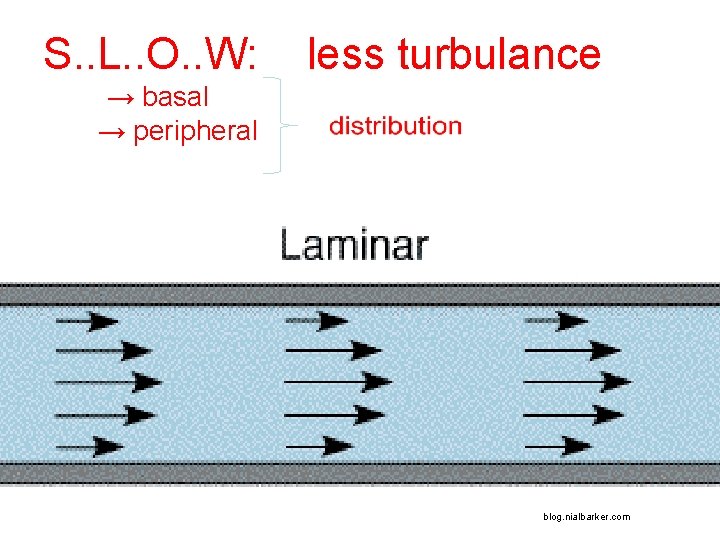
Squeeze bag slow or fast? blog. nialbarker. com
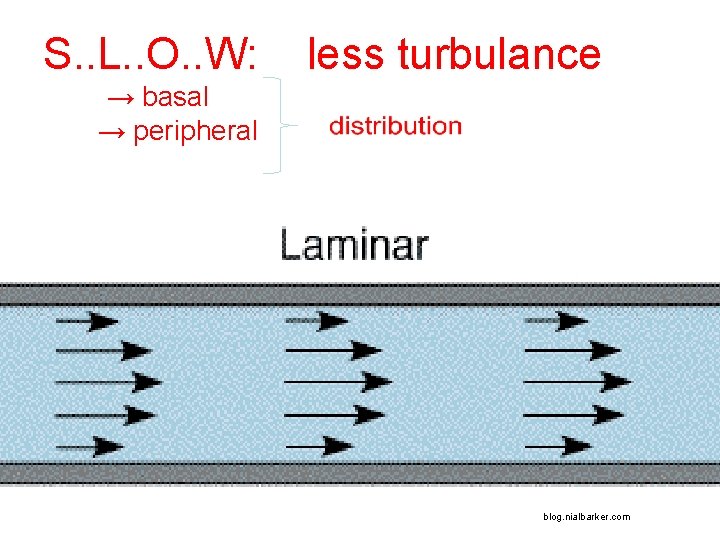
S. . L. . O. . W: a less turbulance → basal → peripheral blog. nialbarker. com
FIRST FEW BREATHS – TIDAL VOLUME q or DEEP BREATH q
FIRST FEW BREATHS – TIDAL VOLUME or DEEP BREATH x
TO JUDGE VOLUME. . . .
TO JUDGE VOLUME. . . . observe.
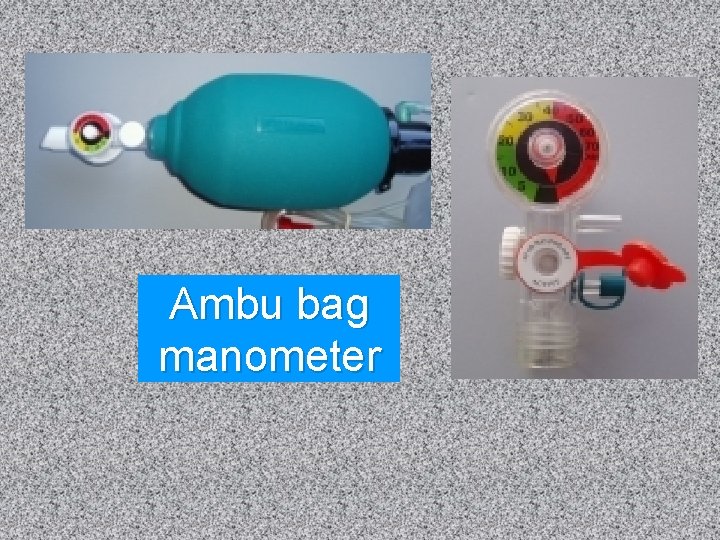
TO JUDGE PRESSURE. . .

Manometer

Manometer
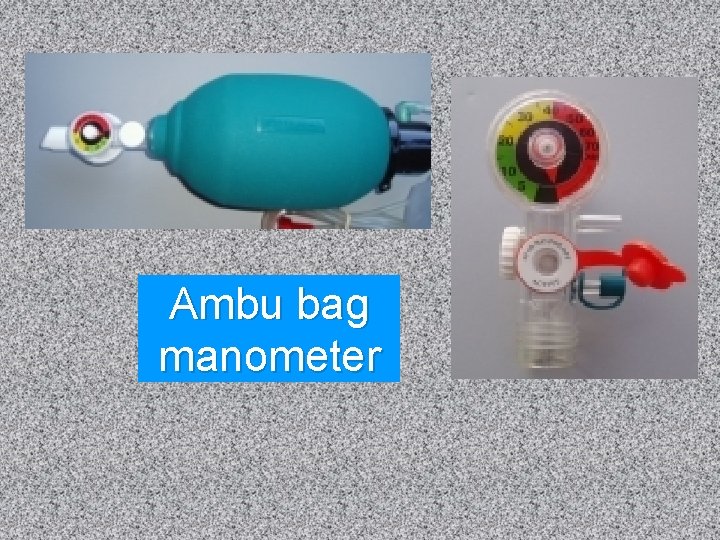
Ambu bag manometer
Maximum safe pressure (normal lungs)……
Maximum safe pressure (normal lungs)…… Some studies have stated that 60 cm. H 2 O is OK
Maximum safe pressure (normal lungs)…… But many clinicians say that 40 cm. H 2 O is best
Maximum safe pressure (damaged lungs)…… NO SAFE PRESSURE identified in the literature
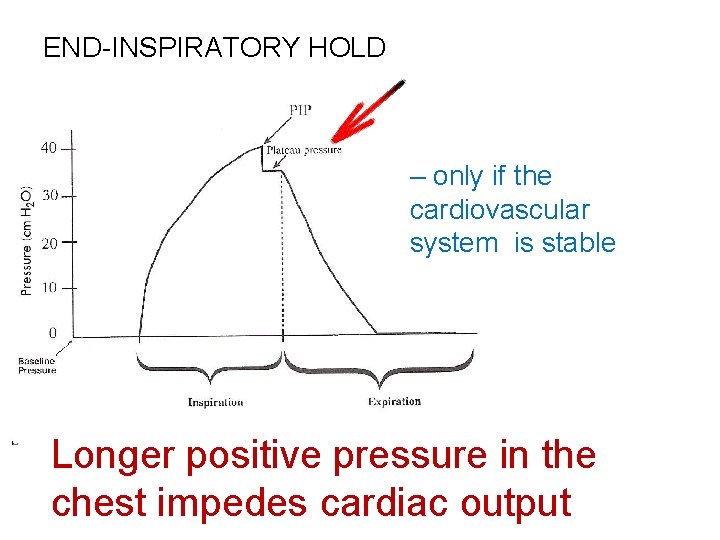
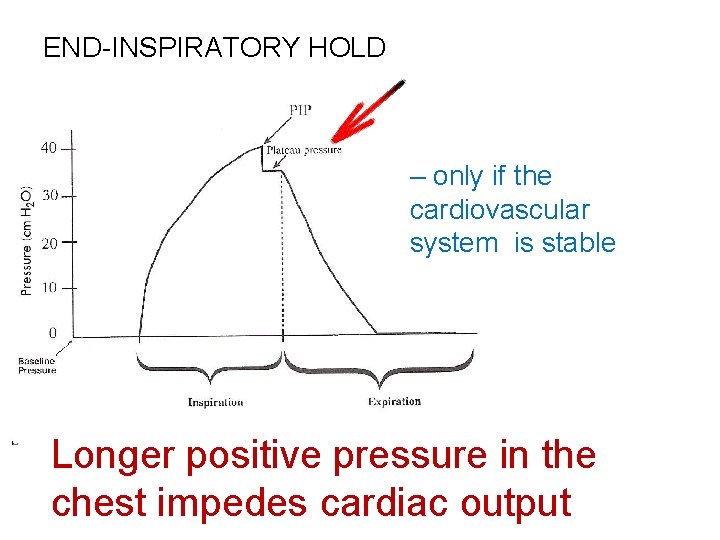
END-INSPIRATORY HOLD – only if the cardiovascular system is stable Longer positive pressure in the chest impedes cardiac output
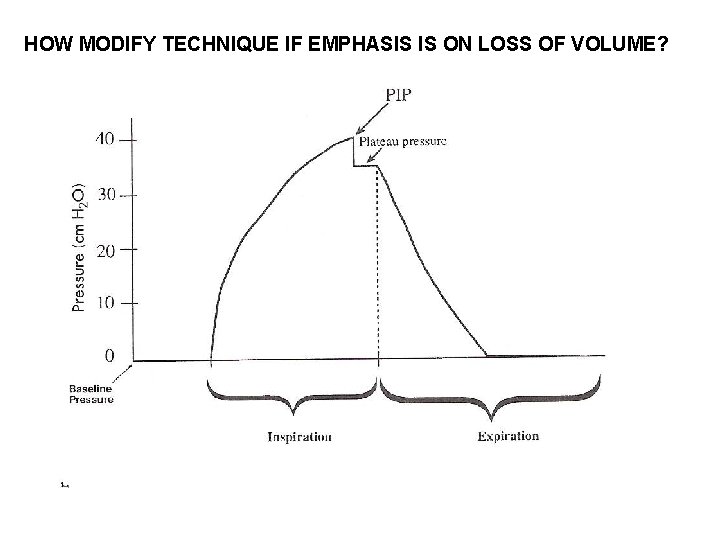
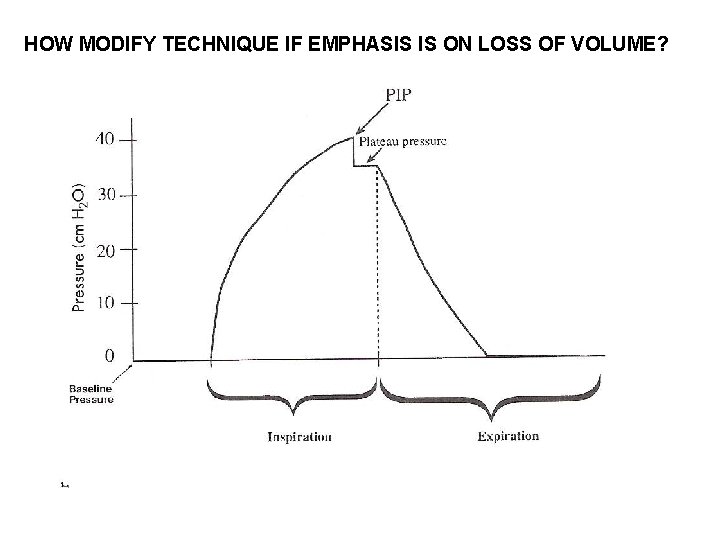
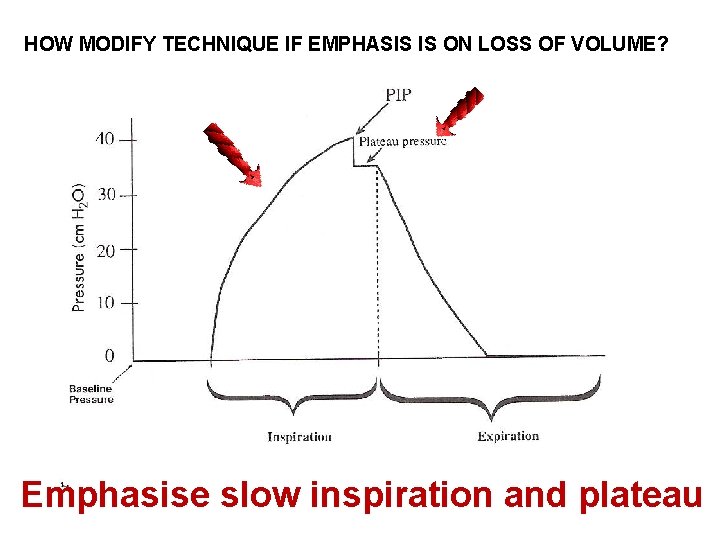
HOW MODIFY TECHNIQUE IF EMPHASIS IS ON LOSS OF VOLUME?
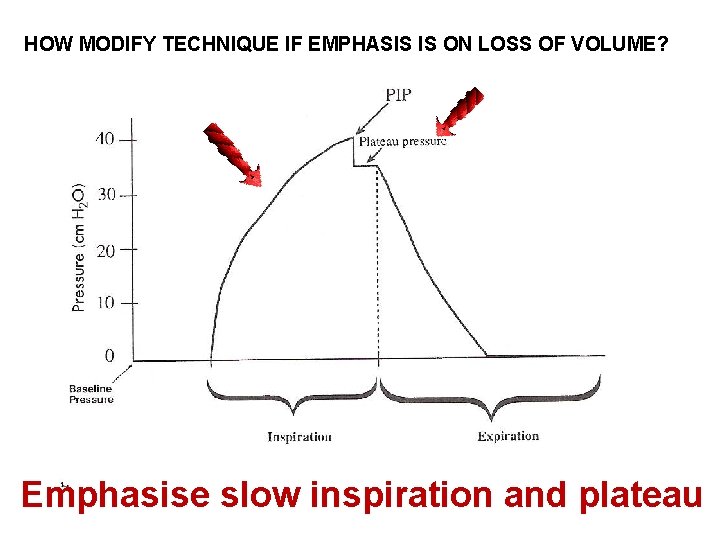
HOW MODIFY TECHNIQUE IF EMPHASIS IS ON LOSS OF VOLUME? Emphasise slow inspiration and plateau
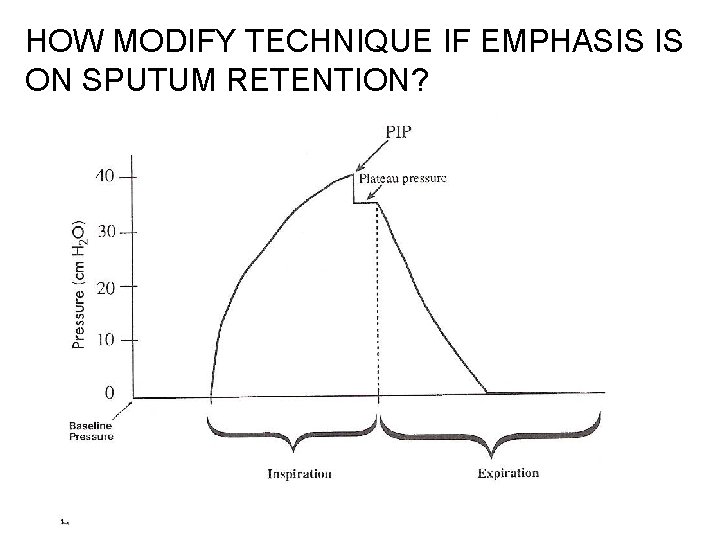
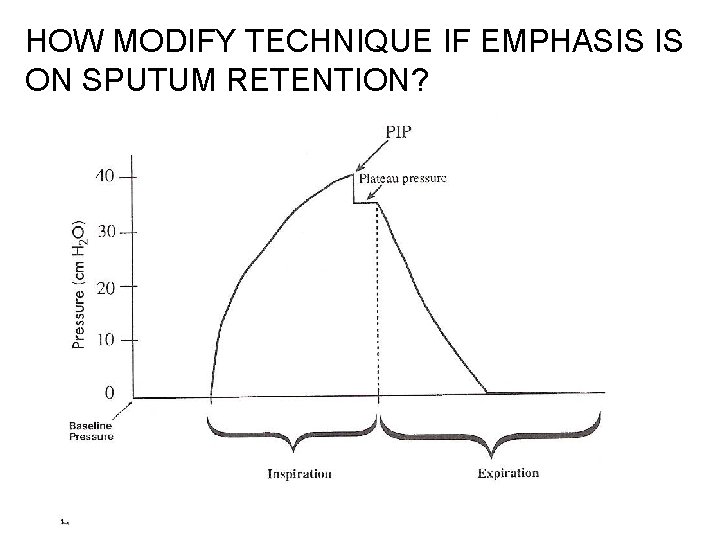
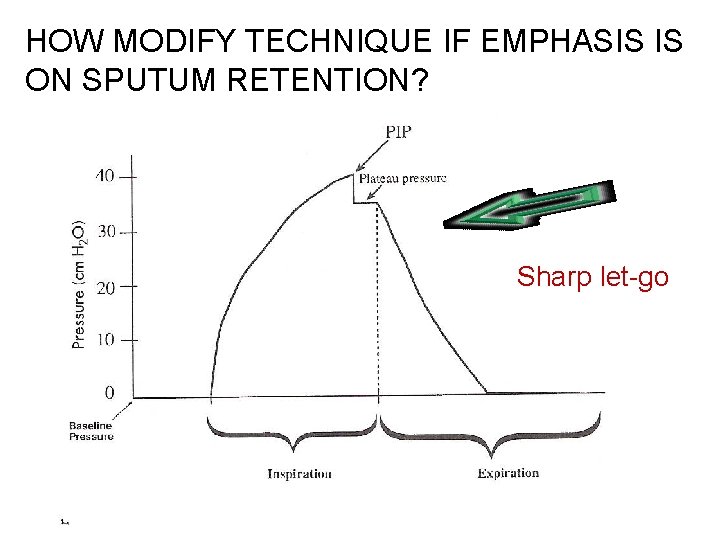
HOW MODIFY TECHNIQUE IF EMPHASIS IS ON SPUTUM RETENTION?
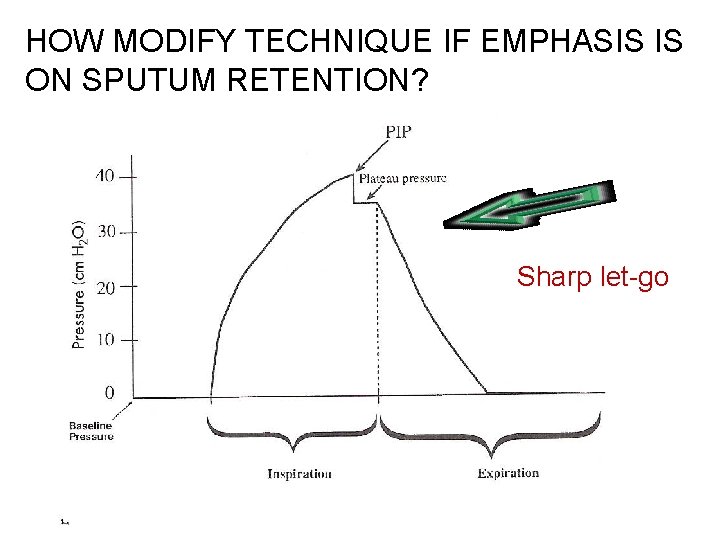
HOW MODIFY TECHNIQUE IF EMPHASIS IS ON SPUTUM RETENTION? Sharp let-go
THROUGHOUT, OBSERVE: …patient’s face……(to ensure patient is not distressed) …abdomen…. (to ensure patient not resisting the breath) …monitors…. (to ensure no adverse objective effects) …expansion…. (to ensure technique is effective)
THROUGHOUT, OBSERVE: …patient’s face……(to ensure patient is not distressed) …abdomen…. (to ensure patient not resisting the breath) …monitors…. (to ensure no adverse objective effects) …expansion…. (to ensure technique is effective) If secretions mobilised, stop MH, suction.
AFTER – CHECK: • •
AFTER – CHECK: • Breath sounds / added sounds
AFTER – CHECK: • Breath sounds / added sounds • breathing pattern • monitors • pt comfort
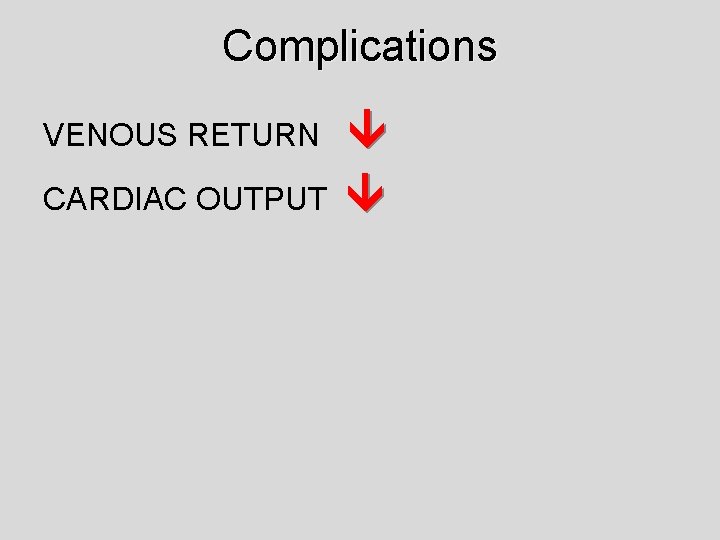
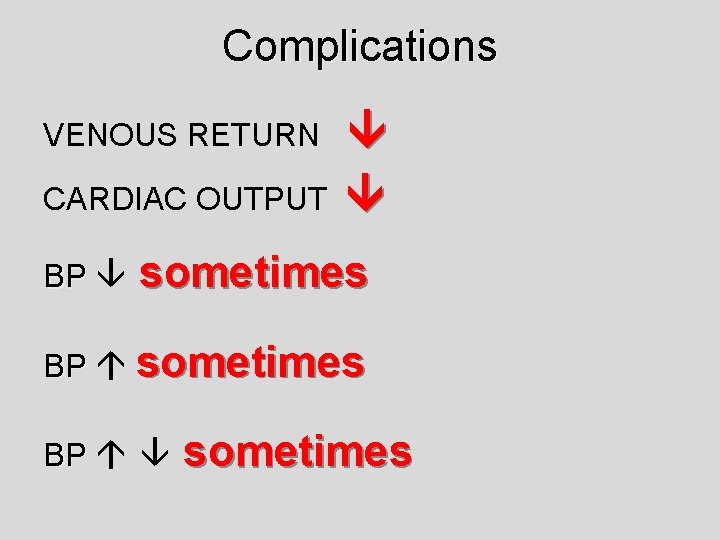
Complications
Complications VENOUS RETURN CARDIAC OUTPUT
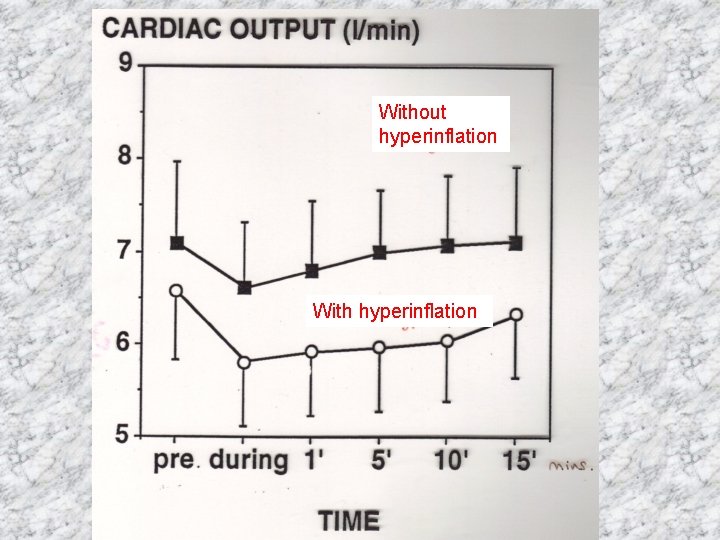
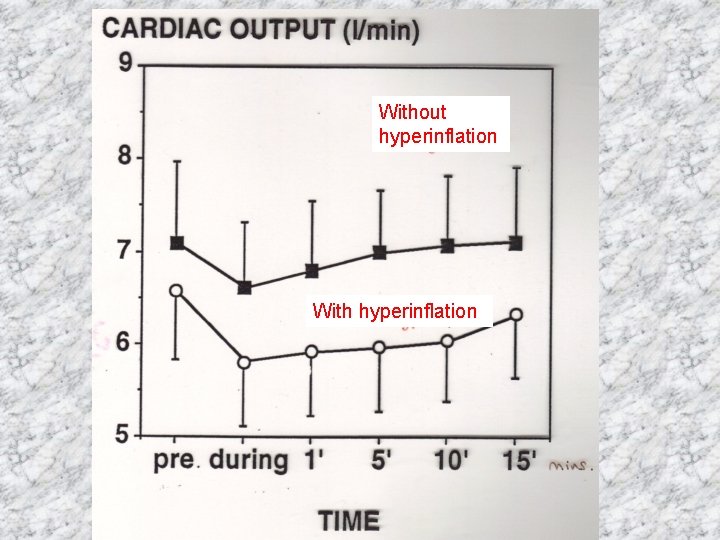
Without hyperinflation With hyperinflation
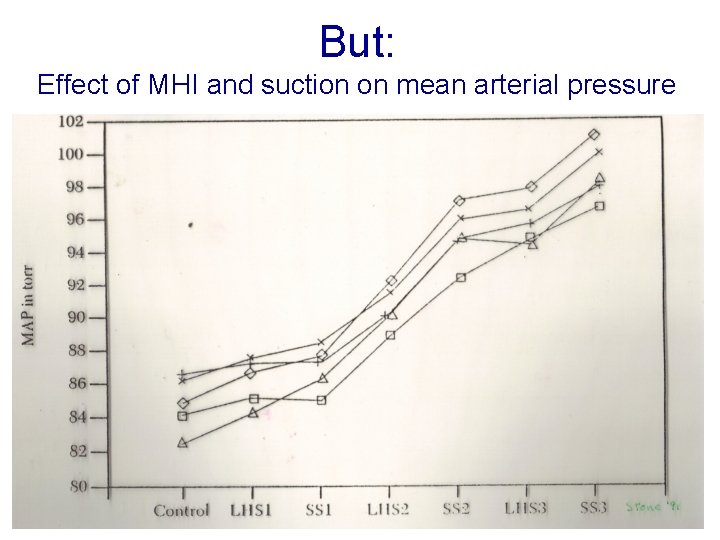
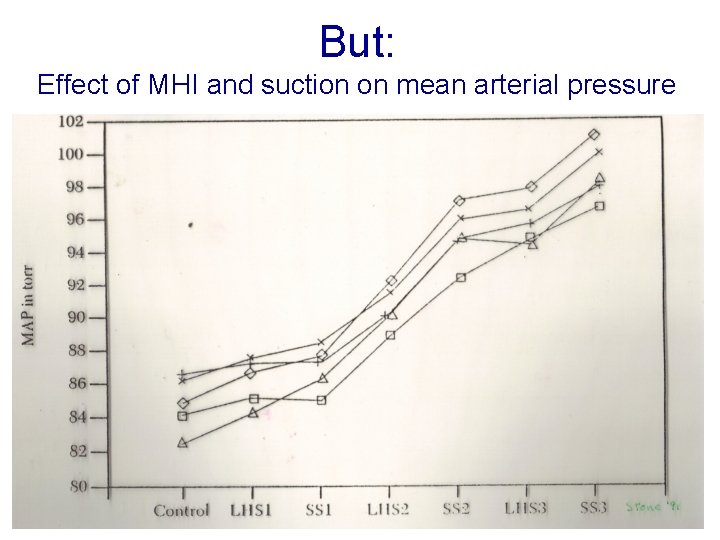
But: Effect of MHI and suction on mean arterial pressure
Complications VENOUS RETURN CARDIAC OUTPUT BP sometimes BP sometimes
Distress Modify by technique and communication
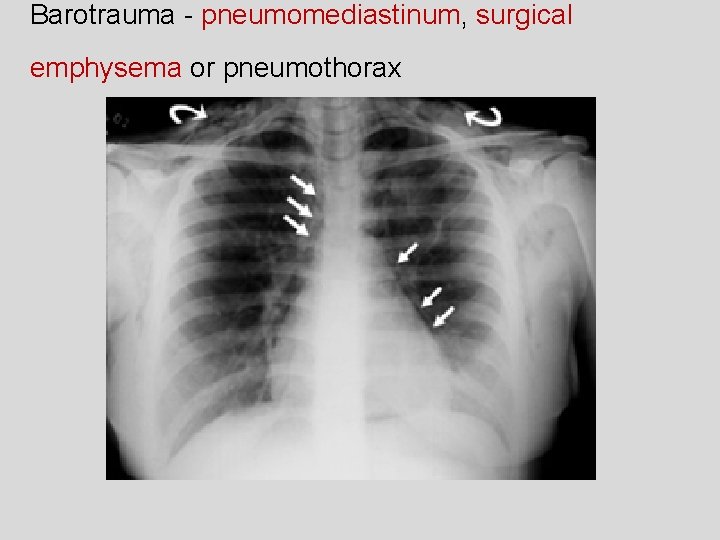
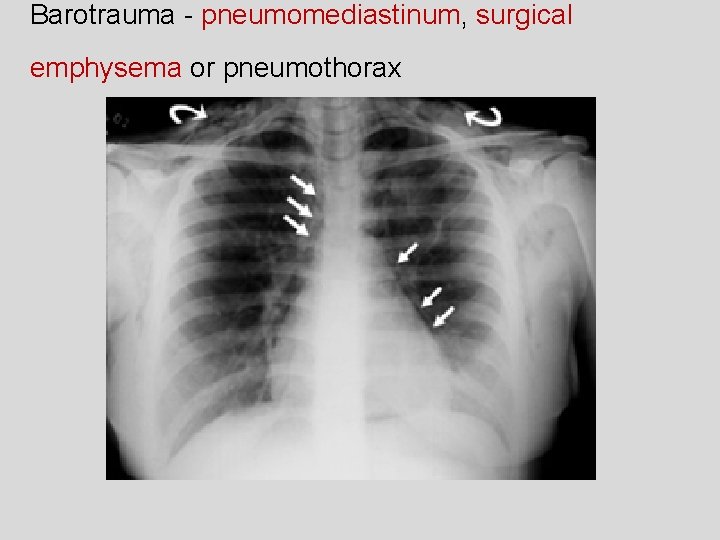
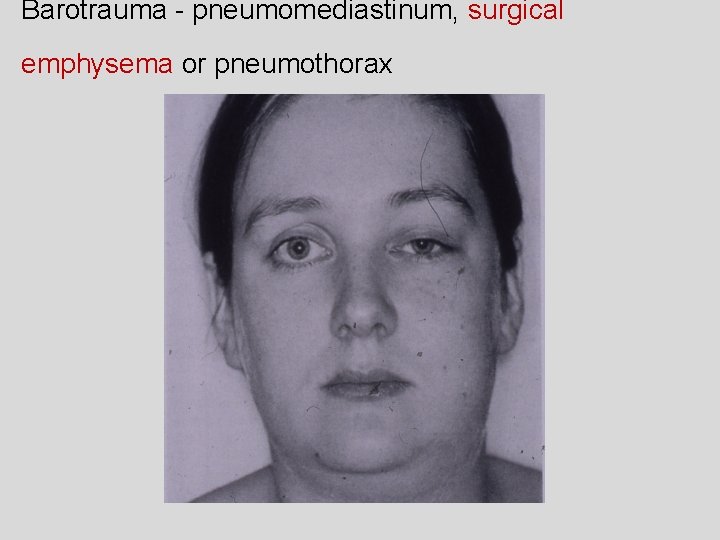
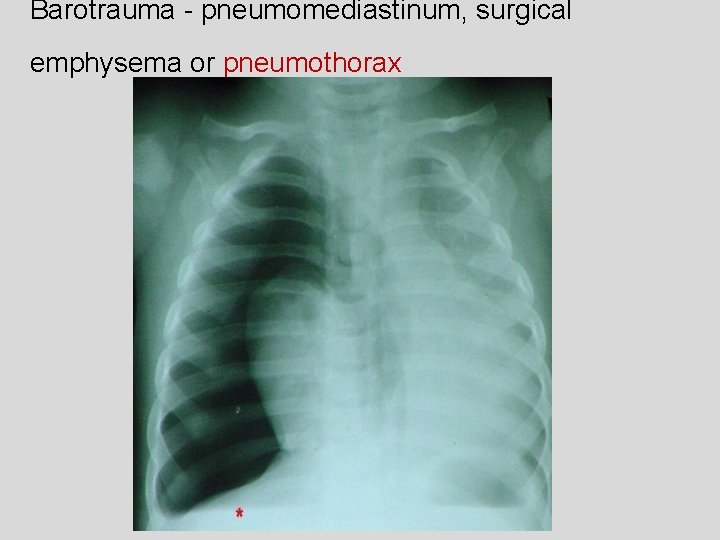
Barotrauma - pneumomediastinum, surgical emphysema or pneumothorax
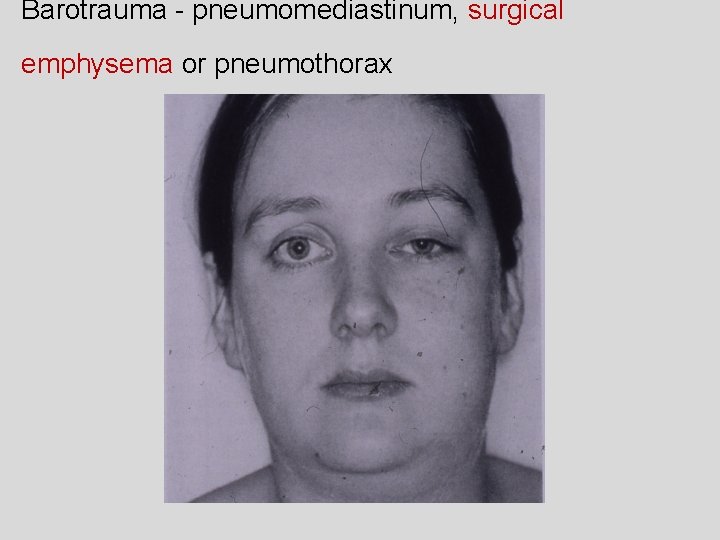
Barotrauma - pneumomediastinum, surgical emphysema or pneumothorax
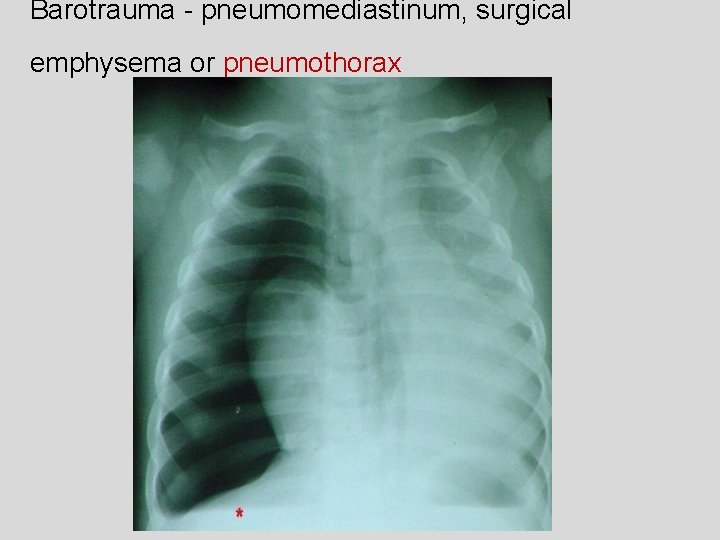
Barotrauma - pneumomediastinum, surgical emphysema or pneumothorax
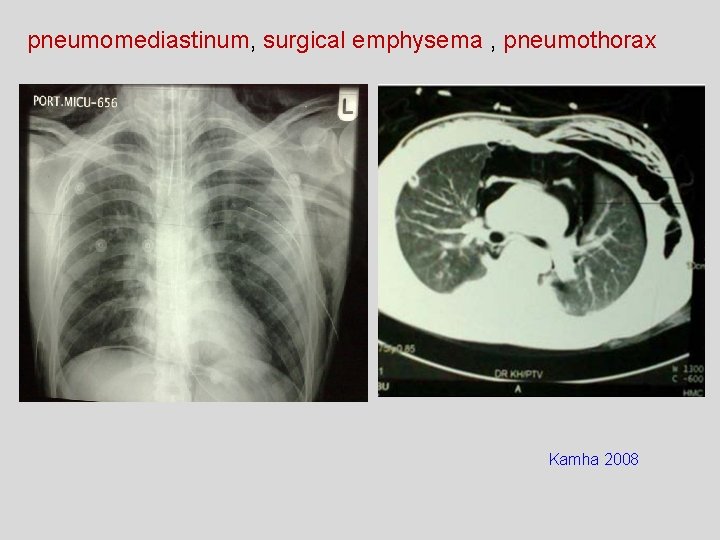
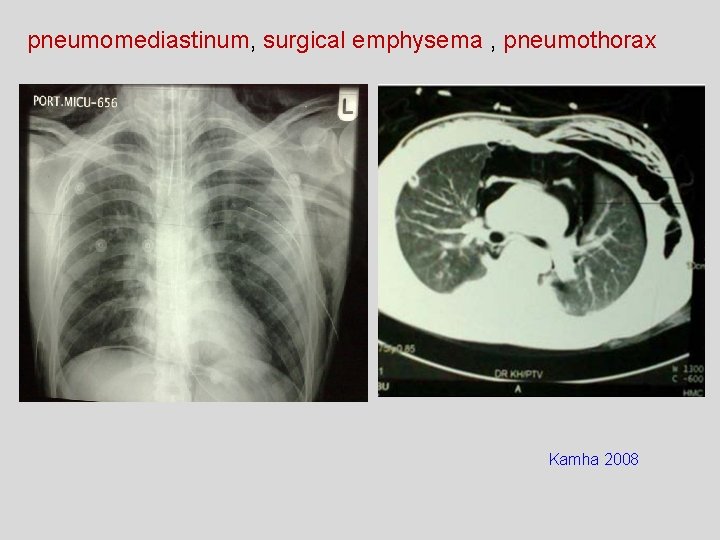
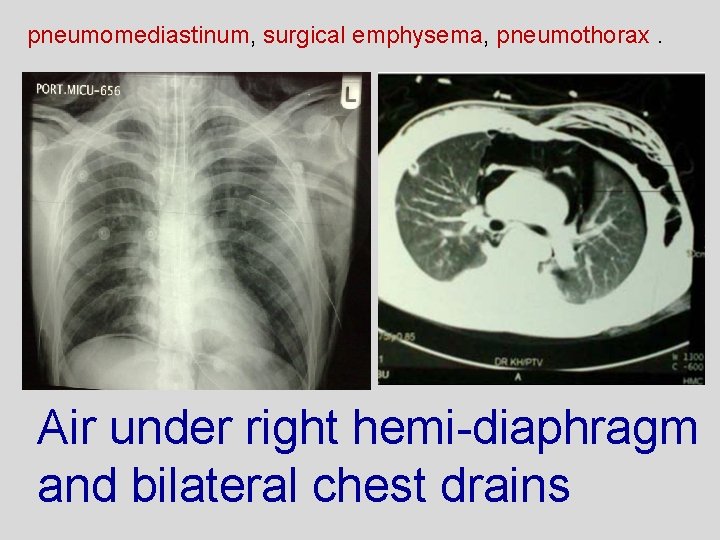
pneumomediastinum, surgical emphysema , pneumothorax Kamha 2008
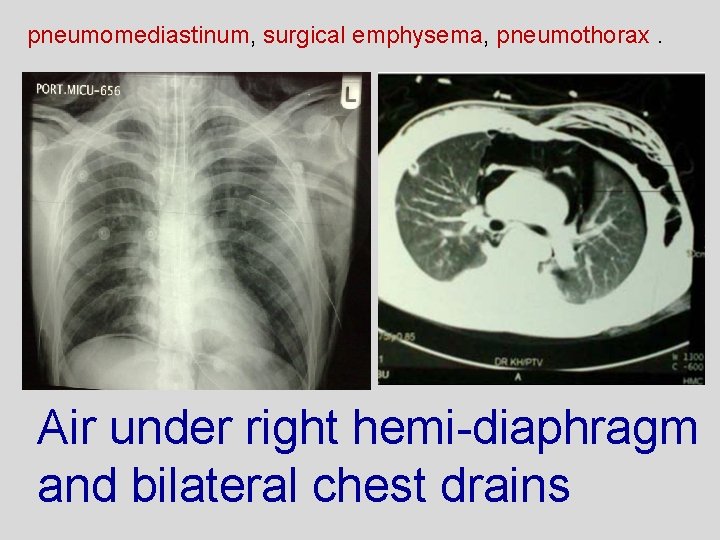
pneumomediastinum, surgical emphysema, pneumothorax. Air under right hemi-diaphragm and bilateral chest drains
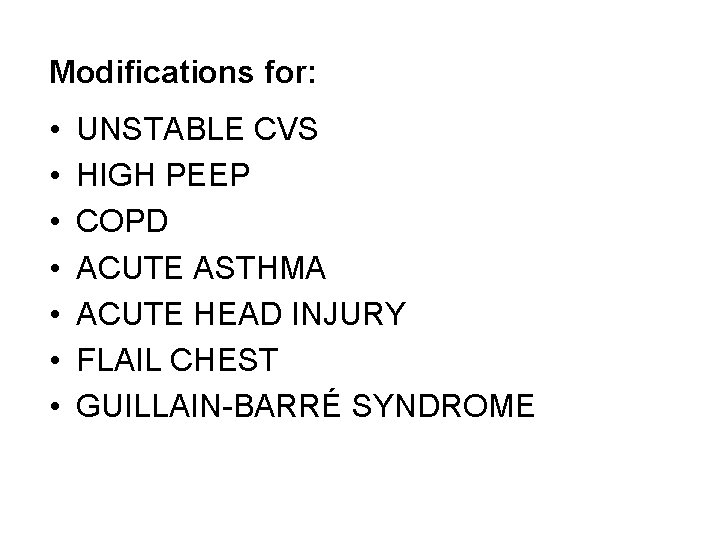
Modifications for: • • UNSTABLE CVS HIGH PEEP COPD ACUTE ASTHMA ACUTE HEAD INJURY FLAIL CHEST GUILLAIN-BARRÉ SYNDROME
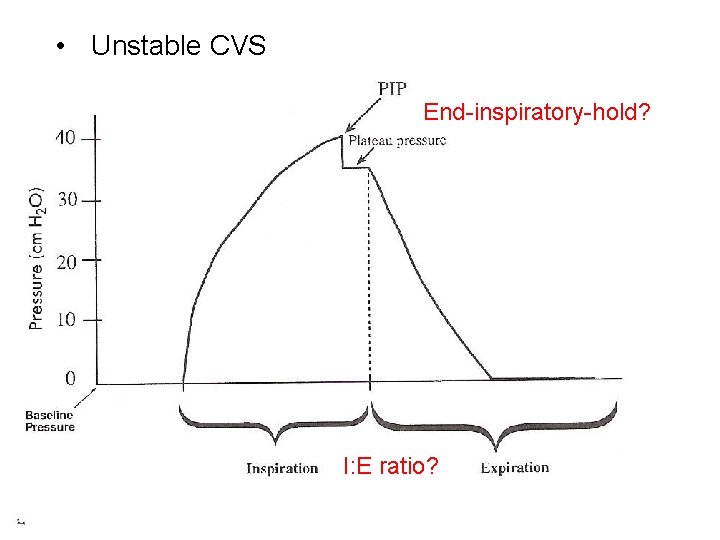
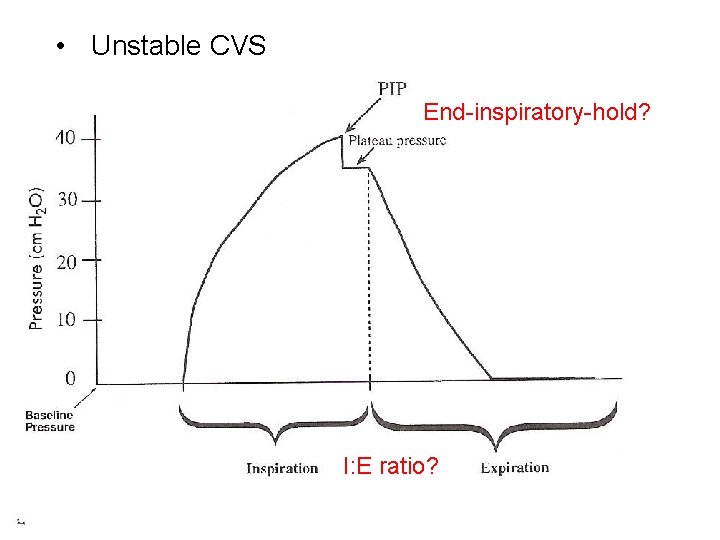
• Unstable CVS End-inspiratory-hold? I: E ratio?
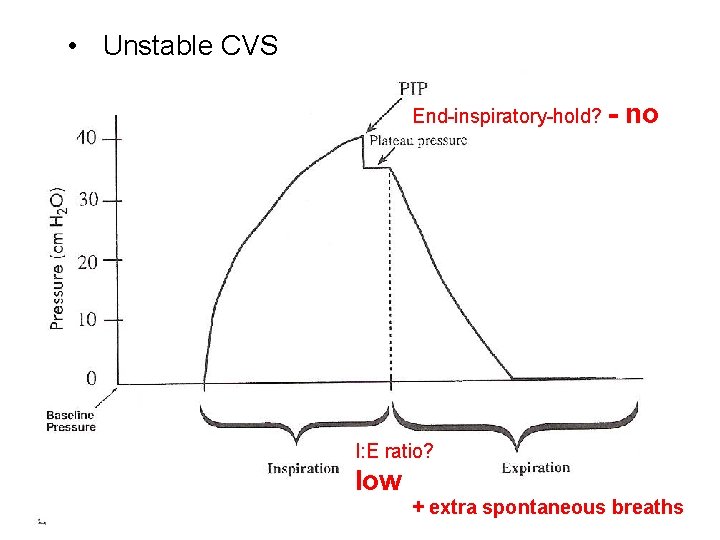
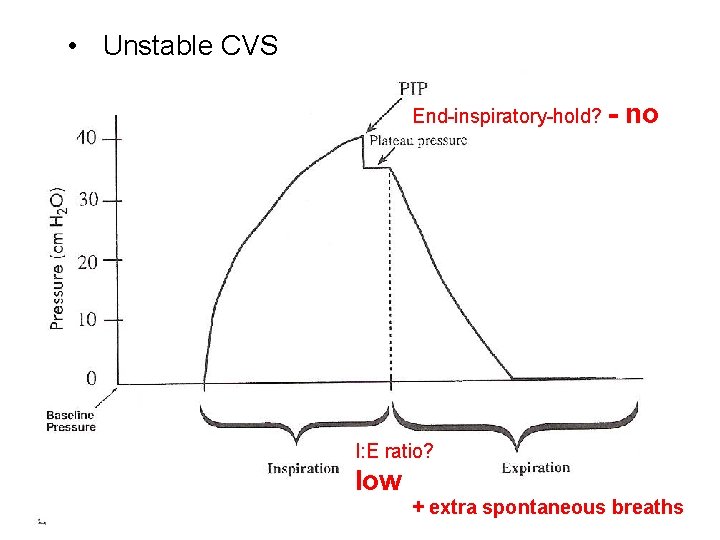
• Unstable CVS End-inspiratory-hold? - no I: E ratio? low + extra spontaneous breaths
• High PEEP (> 5)
High PEEP (> 5) • Ventilator hyperinflation • Manual PEEP: don’t let bag empty • PEEP valve

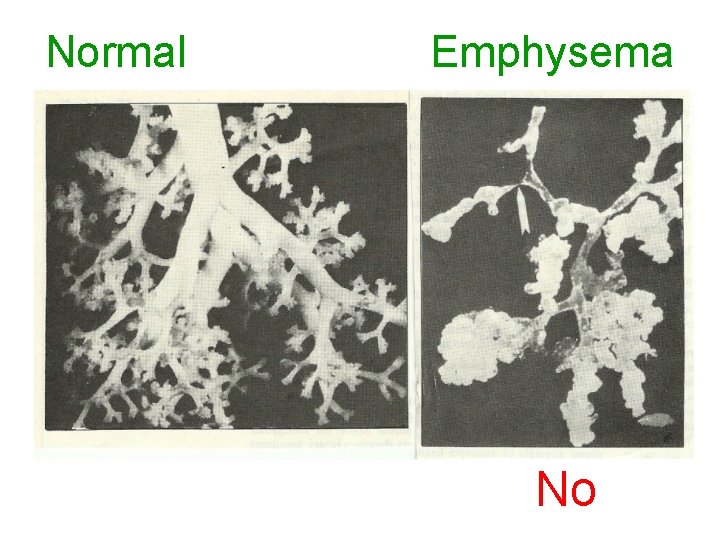
ACUTE ASTHMA ↓ NO
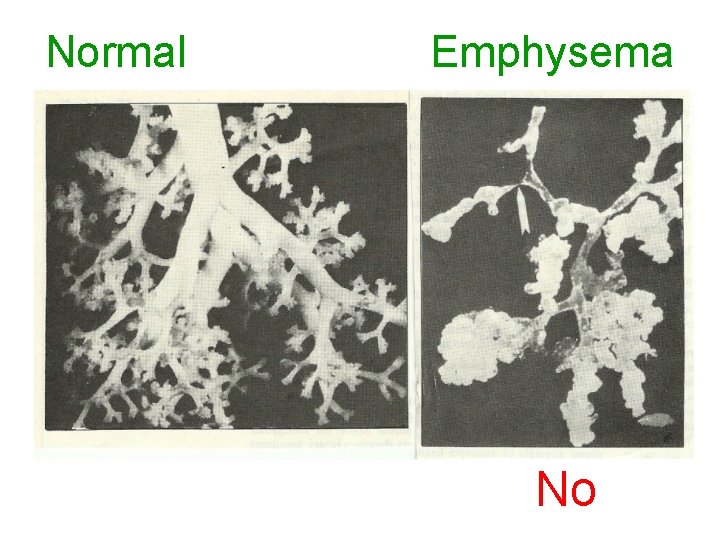
Normal Emphysema No
• Acute asthma
• ACUTE BRAIN INJURY
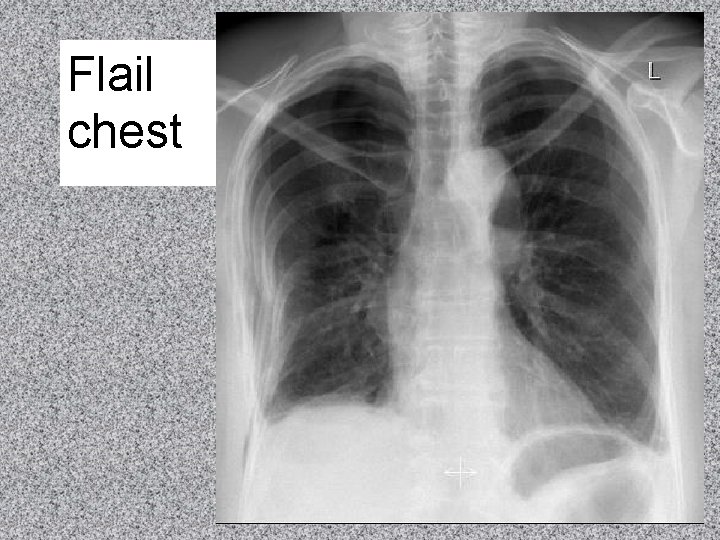
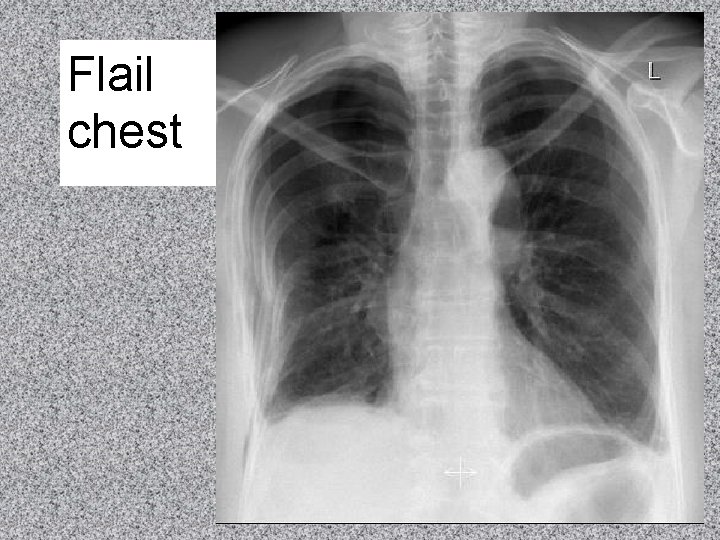
Flail chest
COPD - Type II c/o inspired gas + preferably no MHI because probably some emphysema
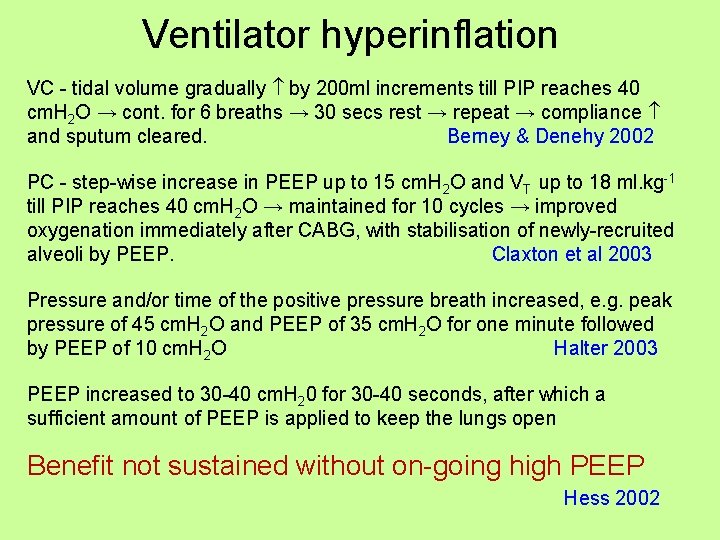
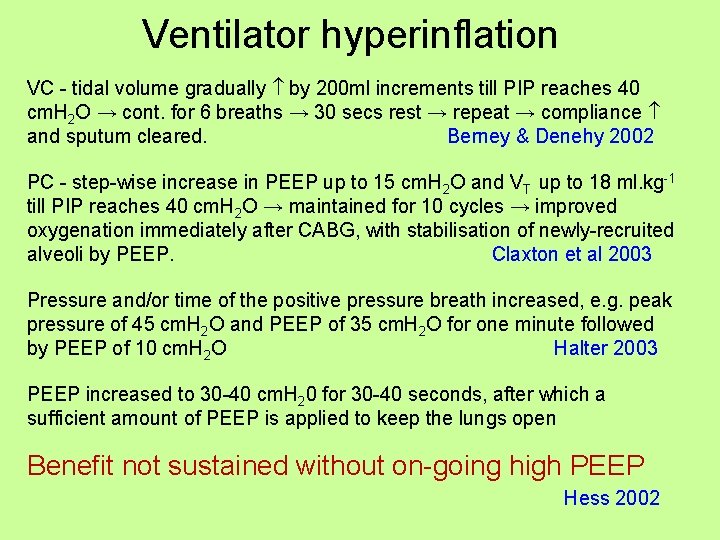
Ventilator hyperinflation VC - tidal volume gradually by 200 ml increments till PIP reaches 40 cm. H 2 O → cont. for 6 breaths → 30 secs rest → repeat → compliance and sputum cleared. Berney & Denehy 2002 PC - step-wise increase in PEEP up to 15 cm. H 2 O and VT up to 18 ml. kg-1 till PIP reaches 40 cm. H 2 O → maintained for 10 cycles → improved oxygenation immediately after CABG, with stabilisation of newly-recruited alveoli by PEEP. Claxton et al 2003 Pressure and/or time of the positive pressure breath increased, e. g. peak pressure of 45 cm. H 2 O and PEEP of 35 cm. H 2 O for one minute followed by PEEP of 10 cm. H 2 O Halter 2003 PEEP increased to 30 -40 cm. H 20 for 30 -40 seconds, after which a sufficient amount of PEEP is applied to keep the lungs open Benefit not sustained without on-going high PEEP Hess 2002
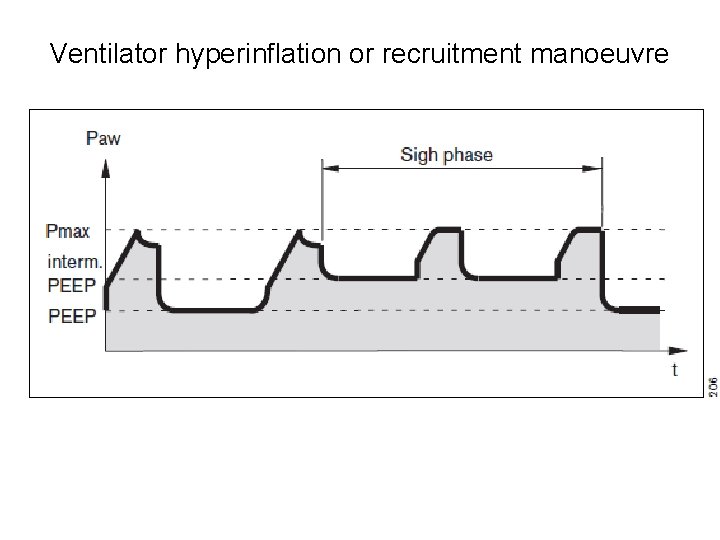
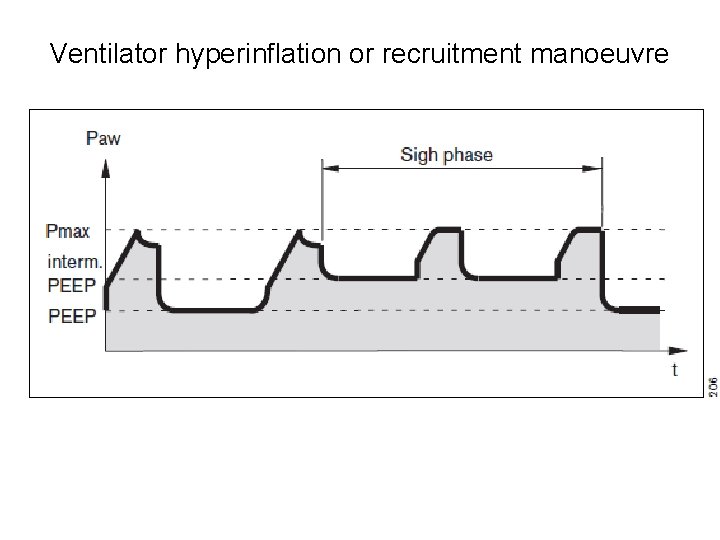
Ventilator hyperinflation or recruitment manoeuvre


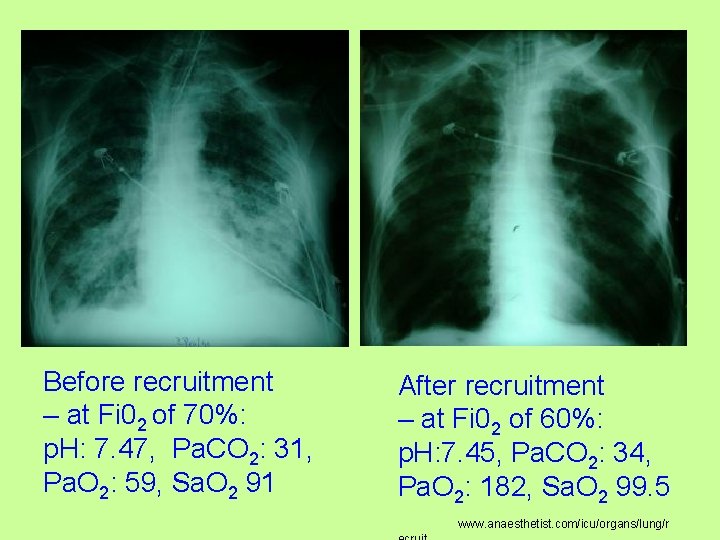
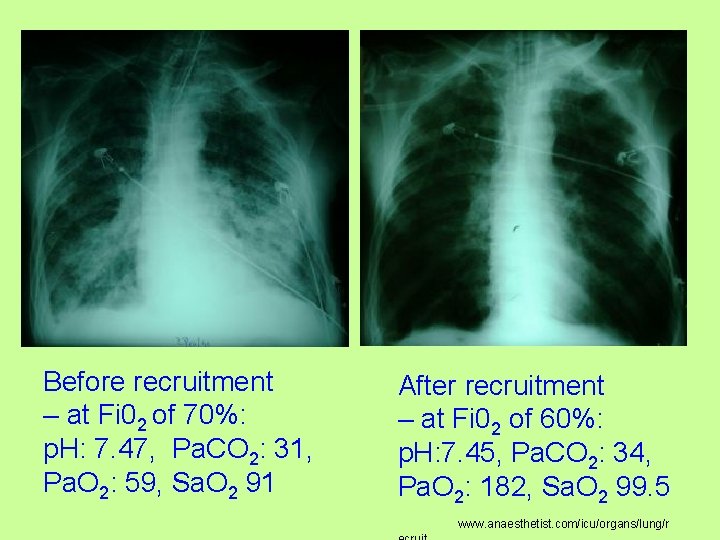
Before recruitment – at Fi 02 of 70%: p. H: 7. 47, Pa. CO 2: 31, Pa. O 2: 59, Sa. O 2 91 After recruitment – at Fi 02 of 60%: p. H: 7. 45, Pa. CO 2: 34, Pa. O 2: 182, Sa. O 2 99. 5 www. anaesthetist. com/icu/organs/lung/r
Good relationships required
PT to increase lung volume SUMMARY • (Pain management) • Positioning • Neurophysiological facilitation of respiration • Deep breathing • Manual hyperinflation
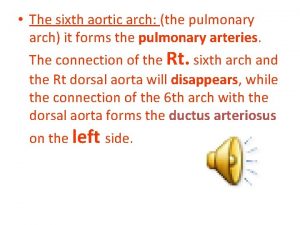
 Recurrent laryngeal nerve
Recurrent laryngeal nerve Brachial pulses
Brachial pulses Art-labeling activity: figure 19.26b (4 of 4)
Art-labeling activity: figure 19.26b (4 of 4) Branches off aortic arch
Branches off aortic arch Interruption of the aortic arch
Interruption of the aortic arch Major arteries of the ascending aorta and aortic arch
Major arteries of the ascending aorta and aortic arch Define peculiar institution
Define peculiar institution Superlative adjectives comfortable
Superlative adjectives comfortable Peculiar institution apush
Peculiar institution apush The crucible unit test
The crucible unit test Hd 101065
Hd 101065 Haustra xray
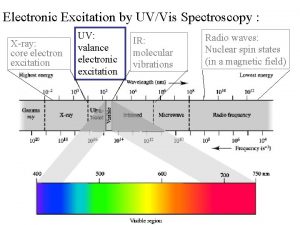
Haustra xray Xray spectrometer
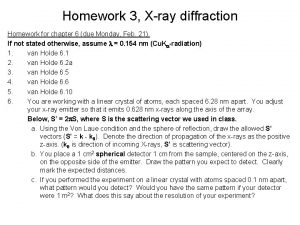
Xray spectrometer Bravais lattices
Bravais lattices Xray training
Xray training V/q scan pulmonary embolism
V/q scan pulmonary embolism Michigan xray
Michigan xray 't zand
't zand Causes of rickets
Causes of rickets Picker xray
Picker xray Bga xray
Bga xray Xray lithography
Xray lithography Xray laser
Xray laser Xray file cabinet
Xray file cabinet Properties of xray
Properties of xray Signo rigler
Signo rigler Pnuemothorax xray
Pnuemothorax xray Xray technique chart
Xray technique chart Thumbprinting on xray
Thumbprinting on xray The label side of the dental film packet
The label side of the dental film packet Sza xray
Sza xray Xray laser
Xray laser Xray laser
Xray laser Yxlon xray
Yxlon xray Xray waves examples
Xray waves examples First xray ever taken
First xray ever taken Mmc xray
Mmc xray Foreshortening and elongation
Foreshortening and elongation Xray photoelectron spectroscopy
Xray photoelectron spectroscopy Pulmonary embolism x ray
Pulmonary embolism x ray Ellis curve pleural effusion
Ellis curve pleural effusion Facial bone xray
Facial bone xray Inertia xray
Inertia xray Scotch tape x ray
Scotch tape x ray Gimp xray
Gimp xray Thumb sign
Thumb sign Emulsion peel x ray
Emulsion peel x ray In capacitor/condenser discharge mobile units,
In capacitor/condenser discharge mobile units, Jfk skull
Jfk skull Supine chest xray
Supine chest xray Kub xray
Kub xray Xray laser
Xray laser Xray laser
Xray laser Xray neck lateral view
Xray neck lateral view Xray telescope
Xray telescope Noi toi poi doi
Noi toi poi doi Bacterial tracheitis xray
Bacterial tracheitis xray Spectrum xray
Spectrum xray Who invented x ray
Who invented x ray X ray orbit
X ray orbit Atom xray
Atom xray Omegascans
Omegascans L
L Xray laser
Xray laser Xray searches
Xray searches