www drsarma in Novel Cardio Vascular Risk Factors

- Slides: 58
www. drsarma. in Novel Cardio Vascular Risk Factors Makers and Markers of CVD Prof. Dr. Sarma VSN Rachakonda M. D (Medicine). , M. Sc. , (Canada), FCGP, FICP, FIMSA, FRCP (G), FCCP (USA), FACP (USA) Hon. National Professor of Medicine, IMA – CGP, India Senior Consultant Physician & Cardio-metabolic Specialist Adjunct Professor, Tamilnadu Dr. MGR Medical University, Chennai
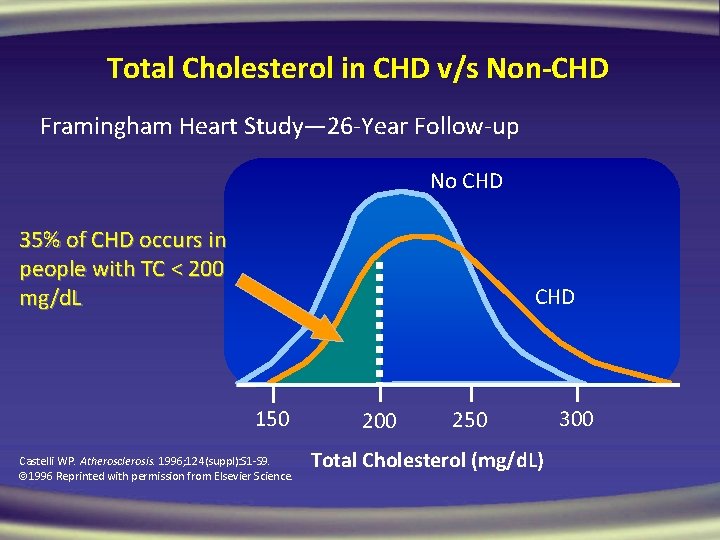
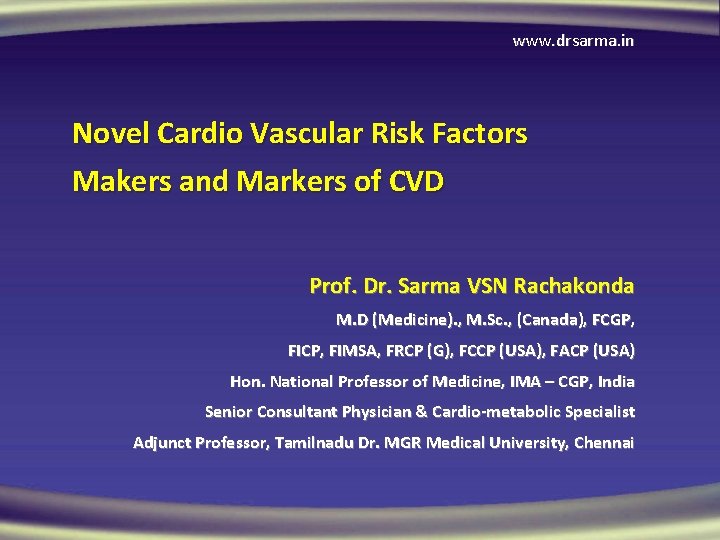
Total Cholesterol in CHD v/s Non-CHD Framingham Heart Study— 26 -Year Follow-up No CHD 35% of CHD occurs in people with TC < 200 mg/d. L CHD 150 Castelli WP. Atherosclerosis. 1996; 124(suppl): S 1 -S 9. 1996 Reprinted with permission from Elsevier Science. 200 250 Total Cholesterol (mg/d. L) 300
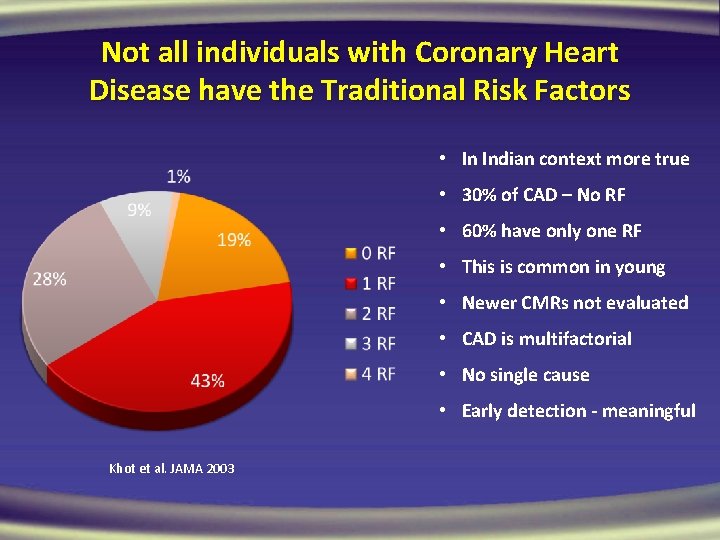
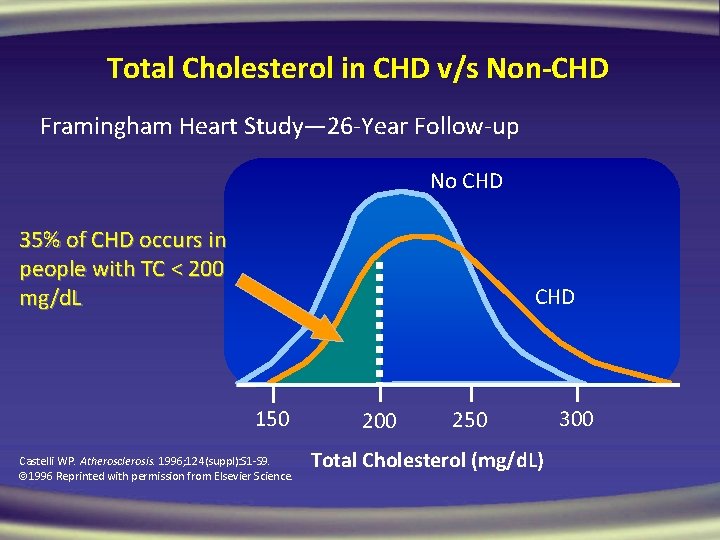
Not all individuals with Coronary Heart Disease have the Traditional Risk Factors • In Indian context more true • 30% of CAD – No RF • 60% have only one RF • This is common in young • Newer CMRs not evaluated • CAD is multifactorial • No single cause • Early detection - meaningful Khot et al. JAMA 2003
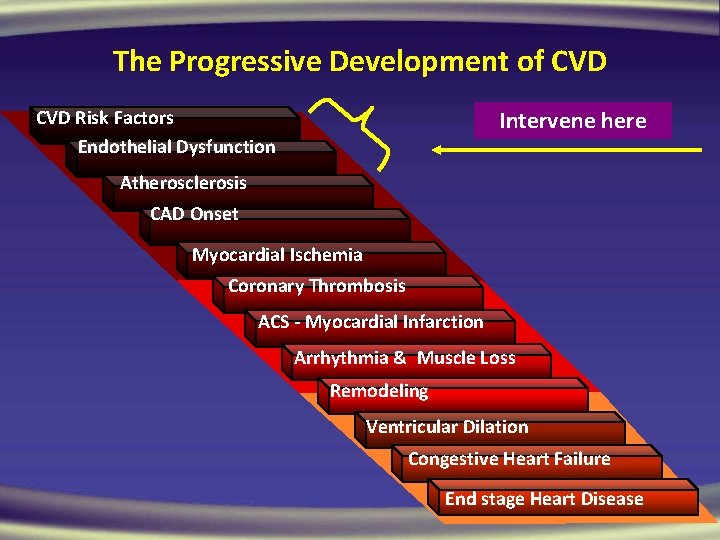
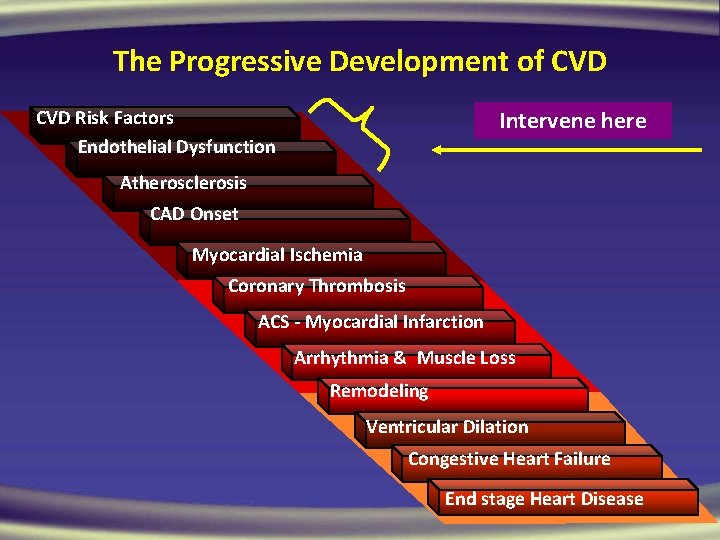
The Progressive Development of CVD Risk Factors Endothelial Dysfunction Intervene here Atherosclerosis CAD Onset Myocardial Ischemia Coronary Thrombosis ACS - Myocardial Infarction Arrhythmia & Muscle Loss Remodeling Ventricular Dilation Congestive Heart Failure End stage Heart Disease
www. drsarma. in 5
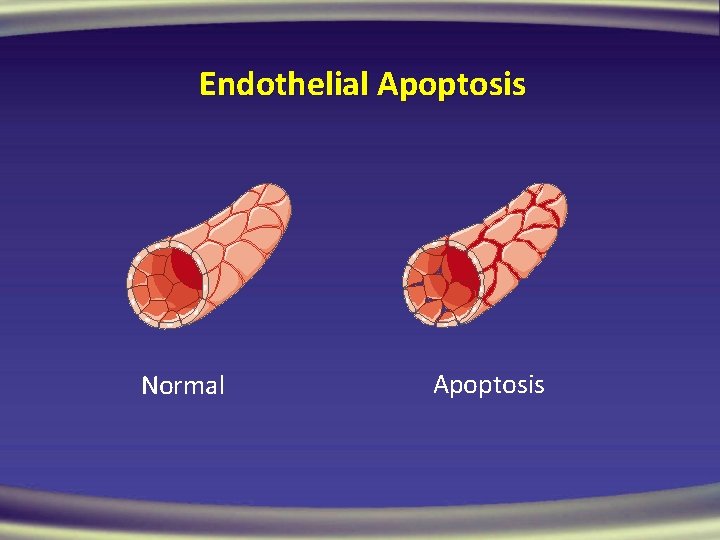
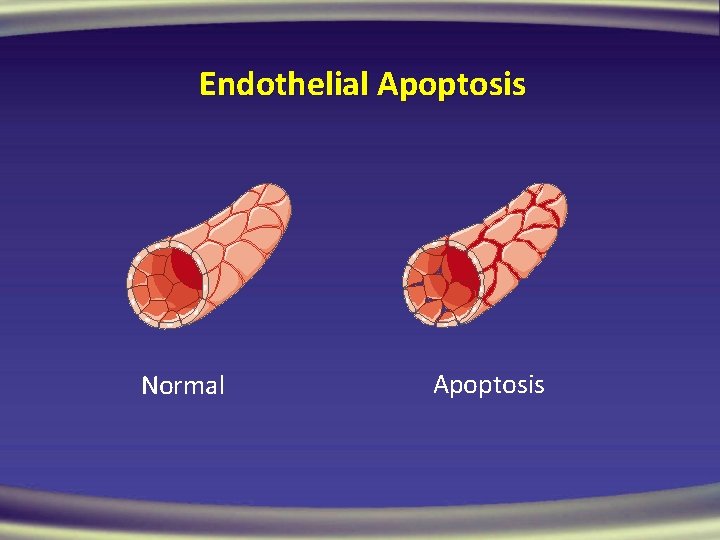
Endothelial Apoptosis Normal Apoptosis
Vasodilation NO, PGI 2, EDHF, BK, C-NP Thrombolysis t. PA, Protein C, TF-I, v. WF Vasoconstrictio n. ROS, ET-1, Tx. A 2, A-II, PGH 2 Thrombosis PAI-1, TF-α, Tx-A 2 Endothelial. Platelet dysfunction Adhesion is the. Molecules basis of CVD Disaggregation CAMs, P, E Selectins NO, PGI 2 Antiproliferation Growth Factors NO, PGI 2, TGF- , Hep ET-1, A-II, PDGF, ILs Lipolysis Inflammation LPL ROS, NF- B
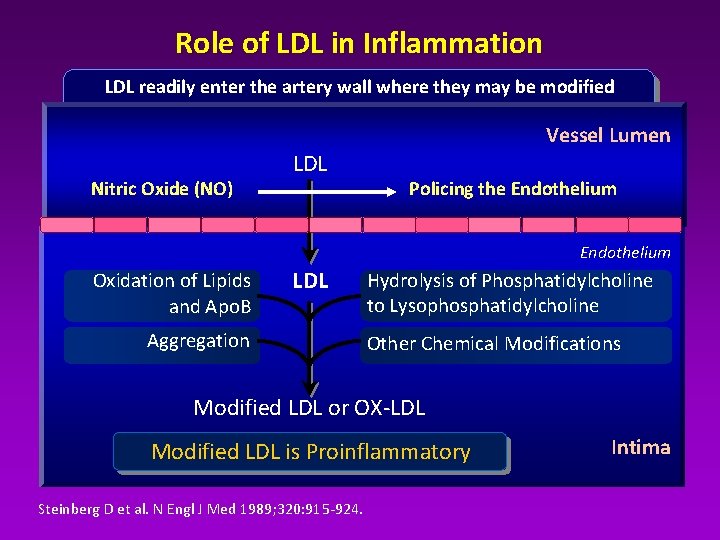
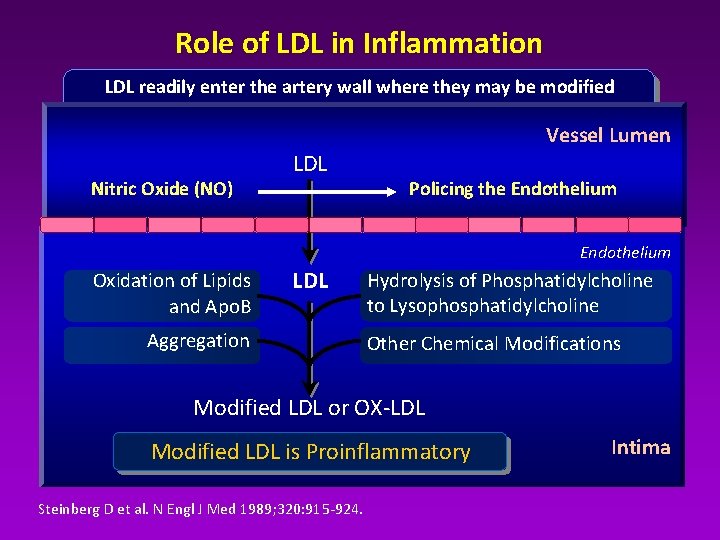
Role of LDL in Inflammation LDL readily enter the artery wall where they may be modified Vessel Lumen Nitric Oxide (NO) LDL Policing the Endothelium Oxidation of Lipids and Apo. B LDL Aggregation Hydrolysis of Phosphatidylcholine to Lysophosphatidylcholine Other Chemical Modifications Modified LDL or OX-LDL Modified LDL is Proinflammatory Steinberg D et al. N Engl J Med 1989; 320: 915 -924. Intima
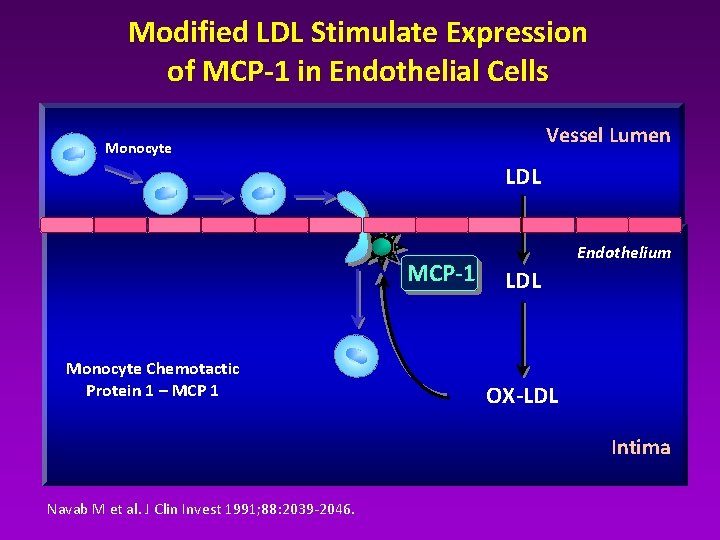
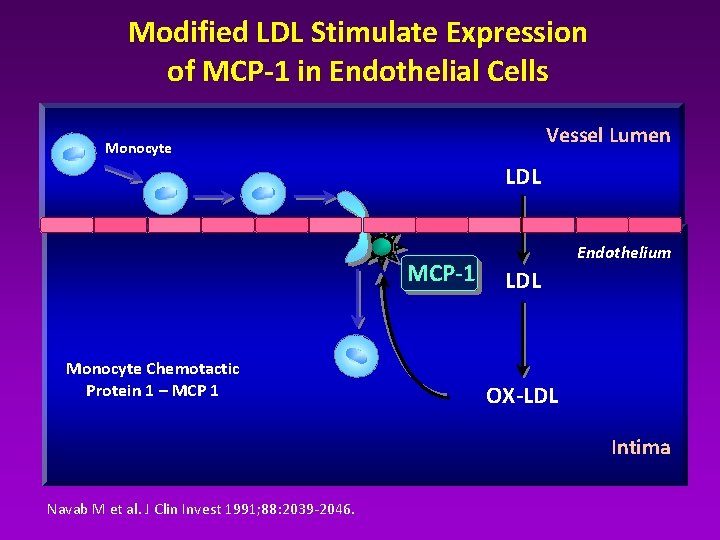
Modified LDL Stimulate Expression of MCP-1 in Endothelial Cells Vessel Lumen Monocyte LDL MCP-1 Monocyte Chemotactic Protein 1 – MCP 1 Endothelium LDL OX-LDL Intima Navab M et al. J Clin Invest 1991; 88: 2039 -2046.
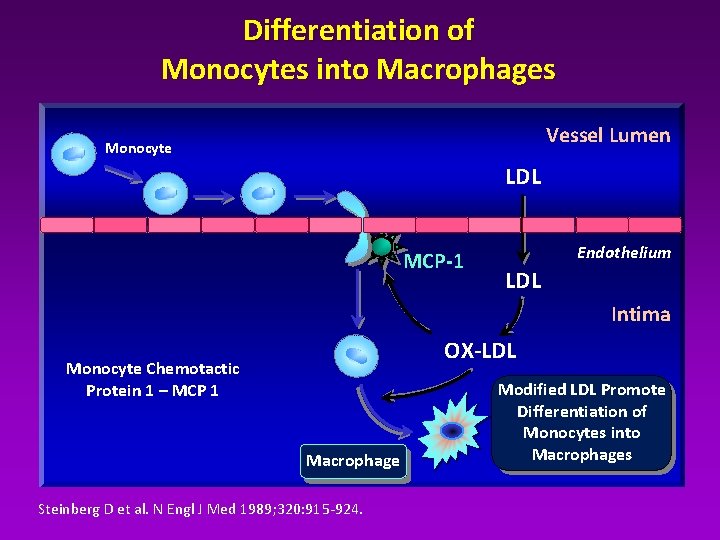
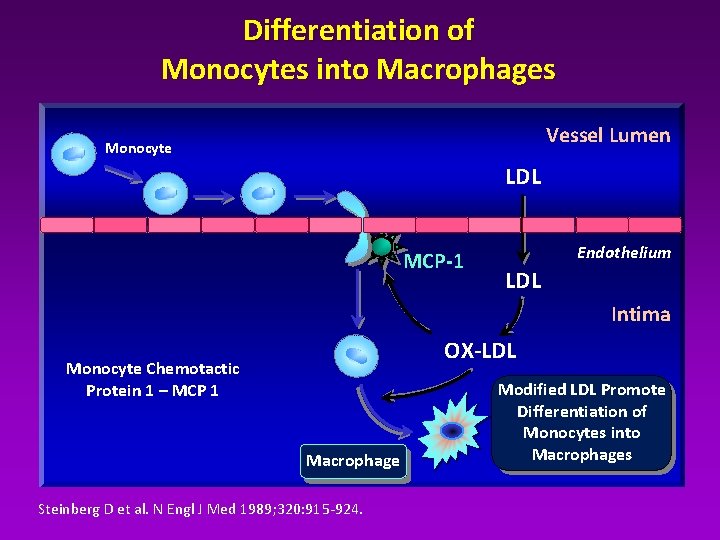
Differentiation of Monocytes into Macrophages Vessel Lumen Monocyte LDL MCP-1 Endothelium LDL Intima OX-LDL Monocyte Chemotactic Protein 1 – MCP 1 Macrophage Steinberg D et al. N Engl J Med 1989; 320: 915 -924. Modified LDL Promote Differentiation of Monocytes into Macrophages
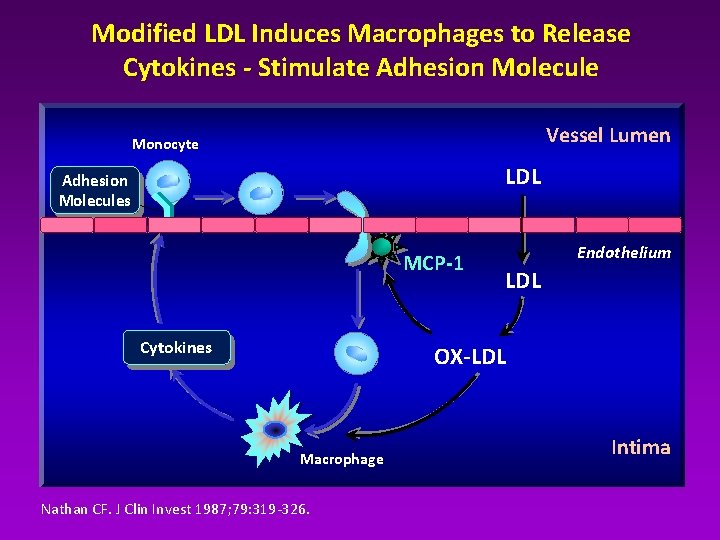
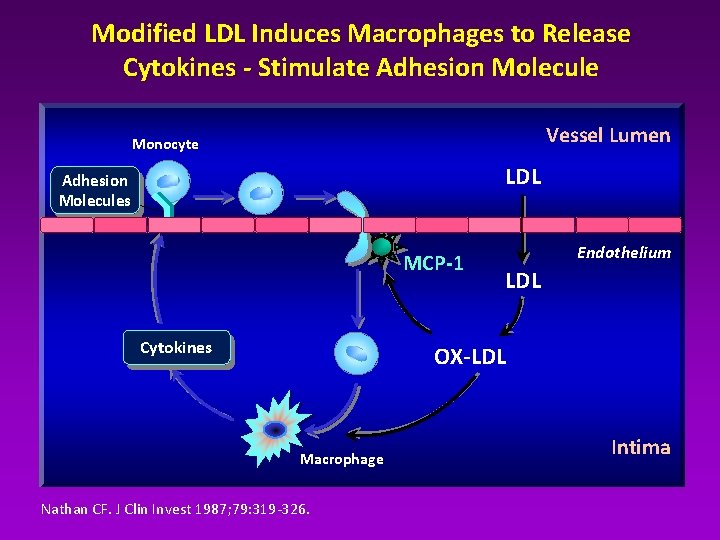
Modified LDL Induces Macrophages to Release Cytokines - Stimulate Adhesion Molecule Vessel Lumen Monocyte LDL Adhesion Molecules MCP-1 Cytokines Endothelium LDL OX-LDL Macrophage Nathan CF. J Clin Invest 1987; 79: 319 -326. Intima
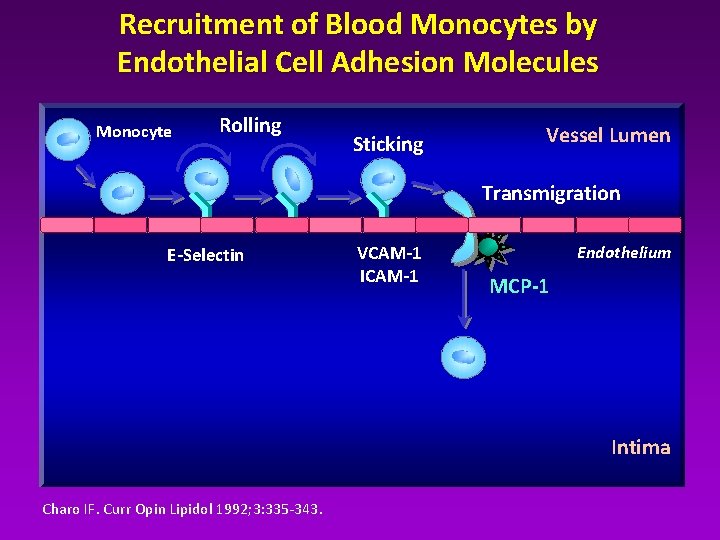
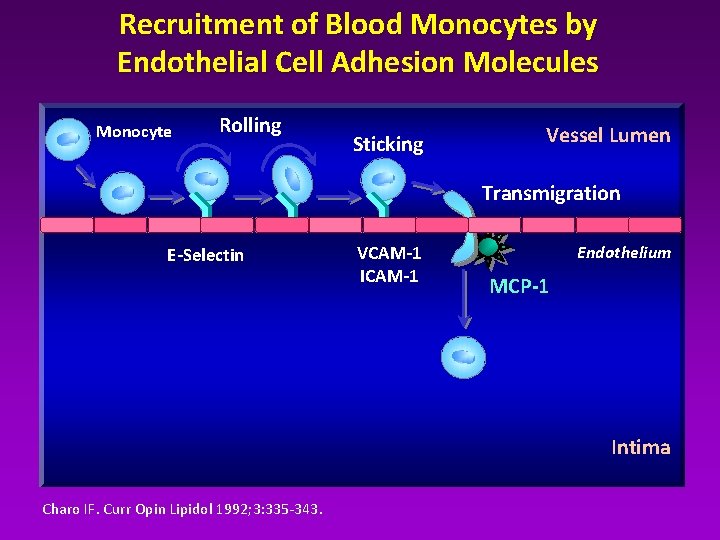
Recruitment of Blood Monocytes by Endothelial Cell Adhesion Molecules Monocyte Rolling Sticking Vessel Lumen Transmigration E-Selectin VCAM-1 ICAM-1 Endothelium MCP-1 Intima Charo IF. Curr Opin Lipidol 1992; 3: 335 -343.
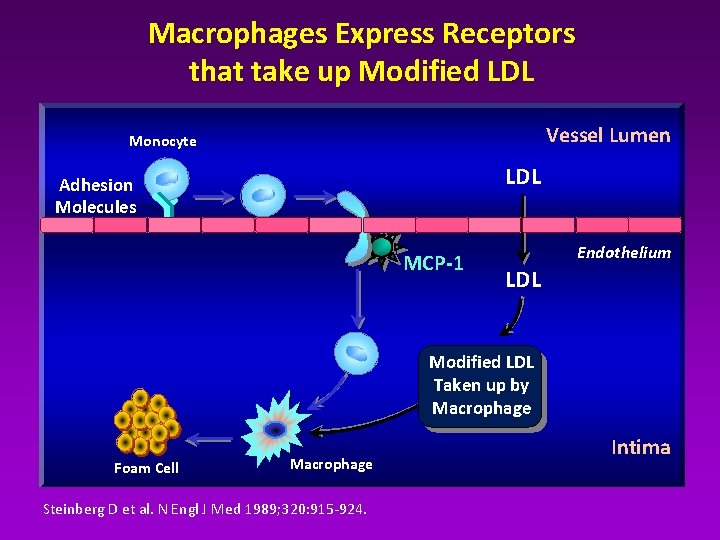
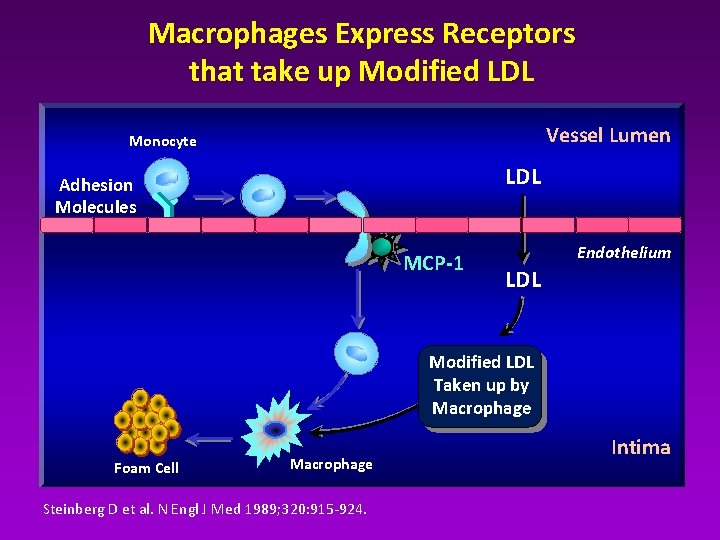
Macrophages Express Receptors that take up Modified LDL Vessel Lumen Monocyte LDL Adhesion Molecules MCP-1 Endothelium LDL Modified LDL Taken up by Macrophage Foam Cell Macrophage Steinberg D et al. N Engl J Med 1989; 320: 915 -924. Intima
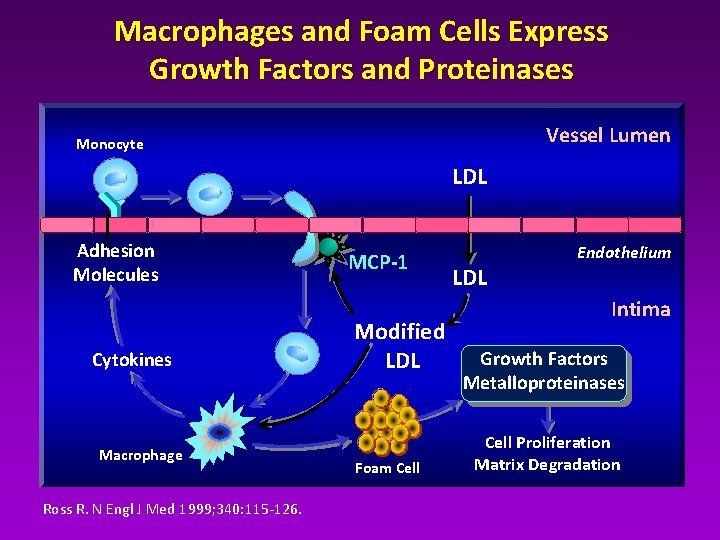
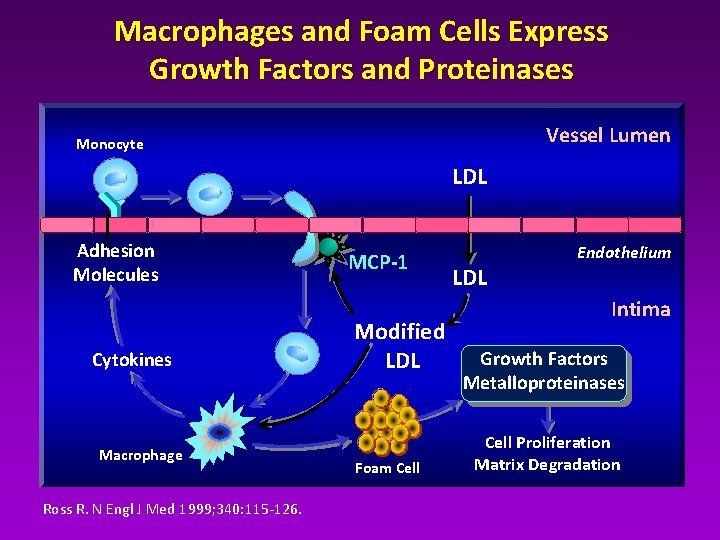
Macrophages and Foam Cells Express Growth Factors and Proteinases Vessel Lumen Monocyte LDL Adhesion Molecules Cytokines Macrophage Ross R. N Engl J Med 1999; 340: 115 -126. MCP-1 Modified LDL Foam Cell LDL Endothelium Intima Growth Factors Metalloproteinases Cell Proliferation Matrix Degradation
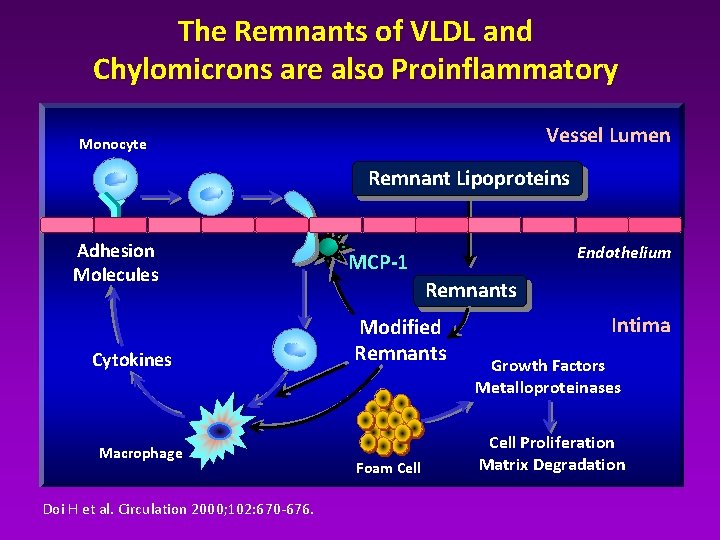
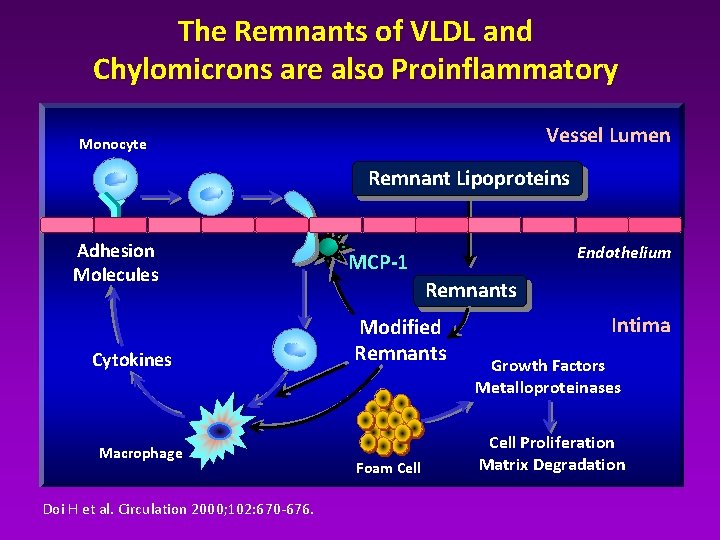
The Remnants of VLDL and Chylomicrons are also Proinflammatory Vessel Lumen Monocyte Remnant Lipoproteins Adhesion Molecules Cytokines Macrophage Doi H et al. Circulation 2000; 102: 670 -676. Endothelium MCP-1 Remnants Modified Remnants Foam Cell Intima Growth Factors Metalloproteinases Cell Proliferation Matrix Degradation
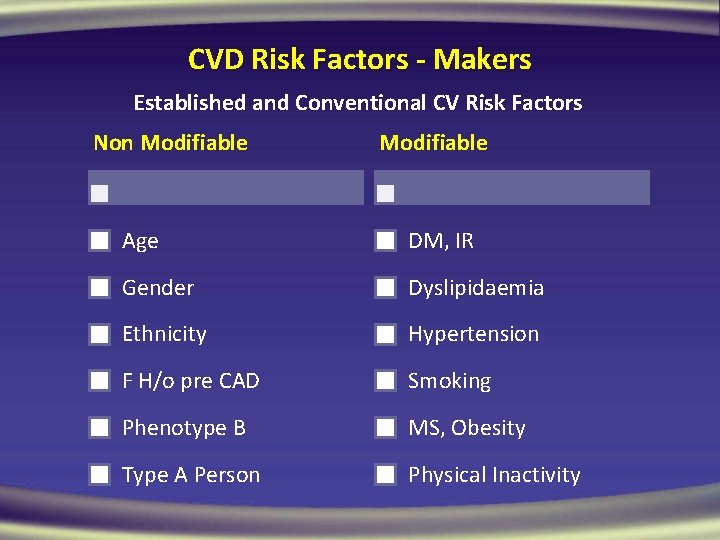
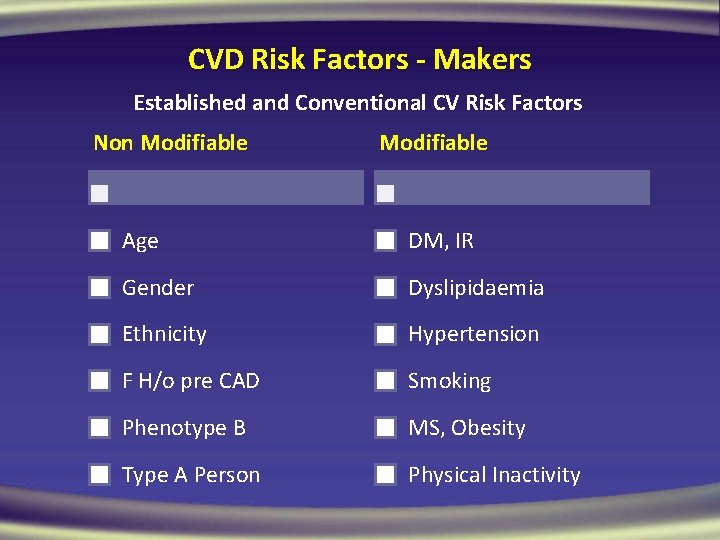
CVD Risk Factors - Makers Established and Conventional CV Risk Factors Non Modifiable Age DM, IR Gender Dyslipidaemia Ethnicity Hypertension F H/o pre CAD Smoking Phenotype B MS, Obesity Type A Person Physical Inactivity
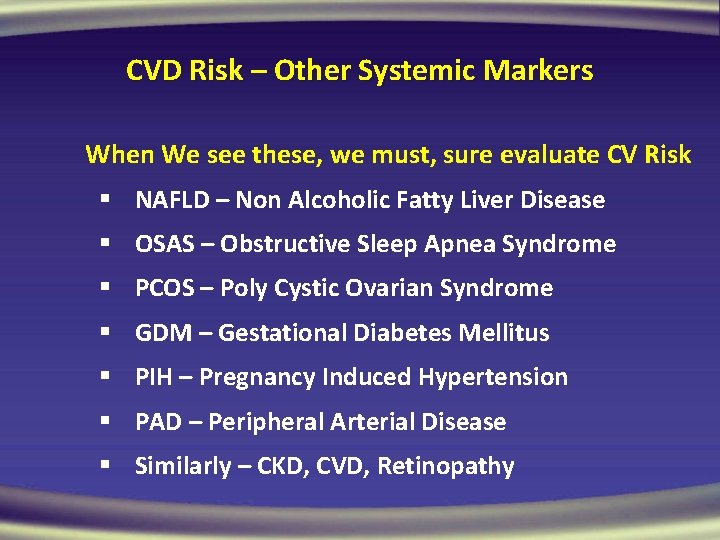
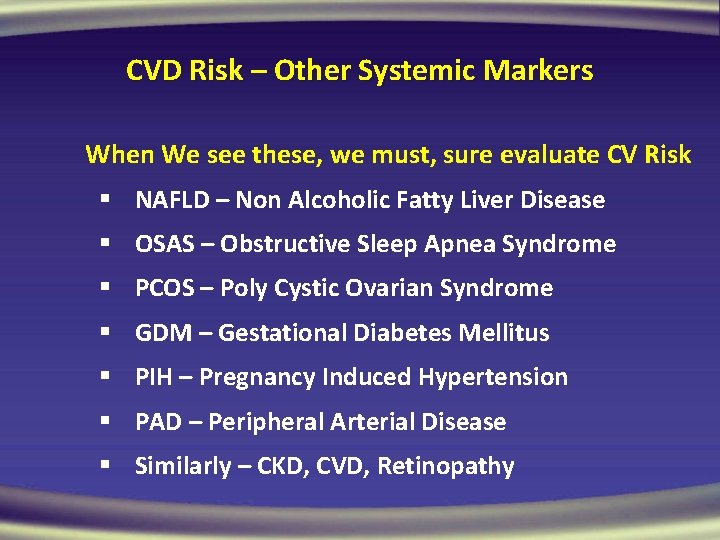
CVD Risk – Other Systemic Markers When We see these, we must, sure evaluate CV Risk § NAFLD – Non Alcoholic Fatty Liver Disease § OSAS – Obstructive Sleep Apnea Syndrome § PCOS – Poly Cystic Ovarian Syndrome § GDM – Gestational Diabetes Mellitus § PIH – Pregnancy Induced Hypertension § PAD – Peripheral Arterial Disease § Similarly – CKD, CVD, Retinopathy
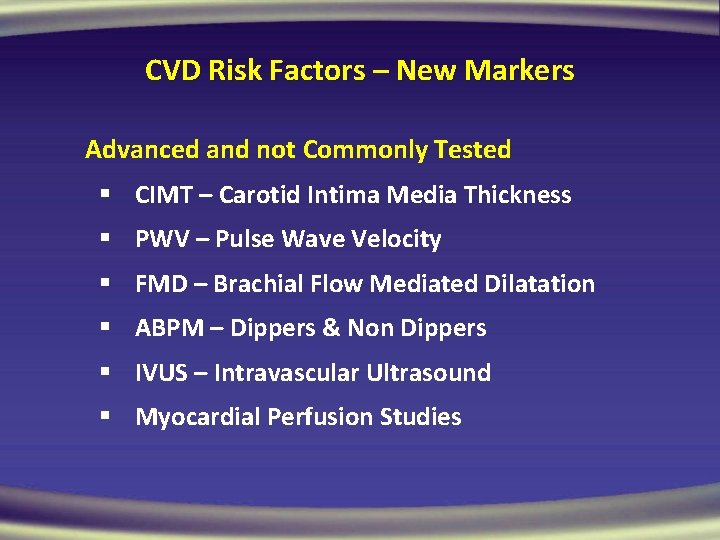
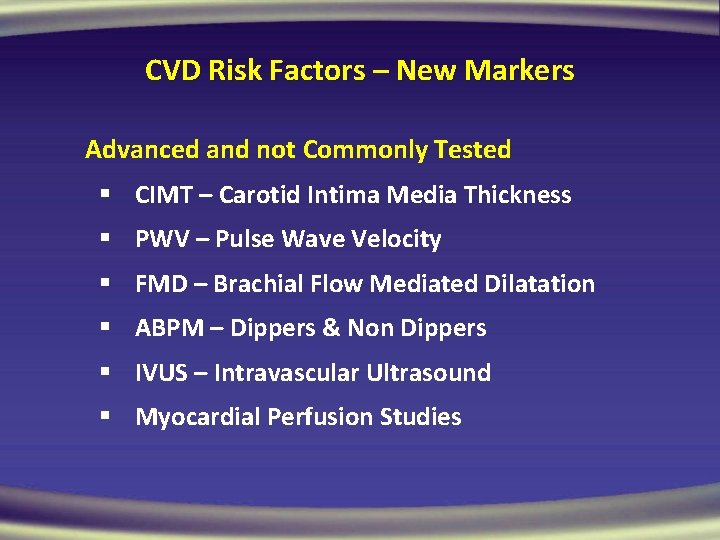
CVD Risk Factors – New Markers Advanced and not Commonly Tested § CIMT – Carotid Intima Media Thickness § PWV – Pulse Wave Velocity § FMD – Brachial Flow Mediated Dilatation § ABPM – Dippers & Non Dippers § IVUS – Intravascular Ultrasound § Myocardial Perfusion Studies
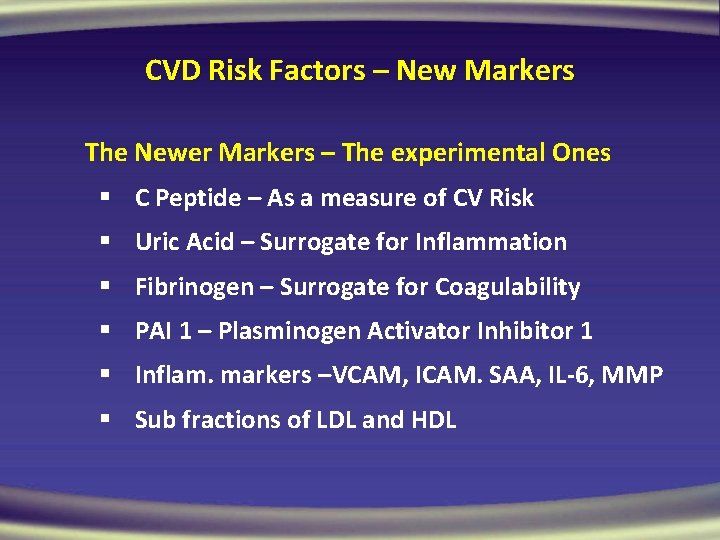
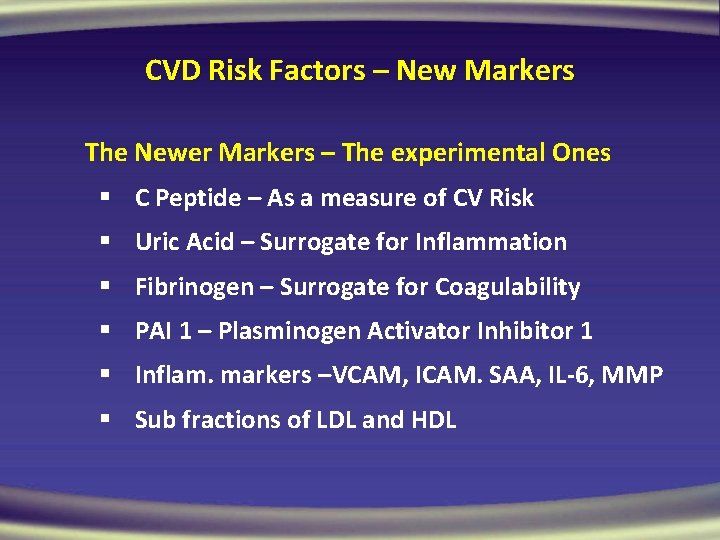
CVD Risk Factors – New Markers The Newer Markers – The experimental Ones § C Peptide – As a measure of CV Risk § Uric Acid – Surrogate for Inflammation § Fibrinogen – Surrogate for Coagulability § PAI 1 – Plasminogen Activator Inhibitor 1 § Inflam. markers –VCAM, ICAM. SAA, IL-6, MMP § Sub fractions of LDL and HDL
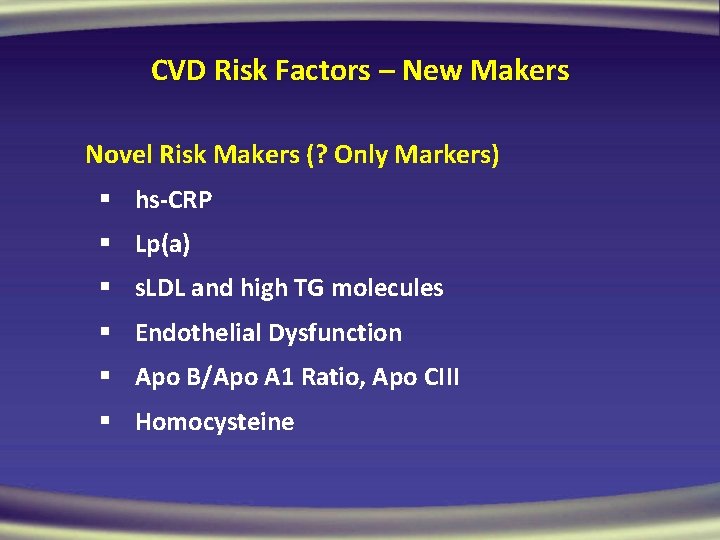
CVD Risk Factors – New Makers Novel Risk Makers (? Only Markers) § hs-CRP § Lp(a) § s. LDL and high TG molecules § Endothelial Dysfunction § Apo B/Apo A 1 Ratio, Apo CIII § Homocysteine
CVD Risk - Clinical Markers Very Simple, we need to apply in practice § WC – Waist Circumference – Are we using? § MAU – Micro Albuminuria – ACR § ABI – Ankle Brachial Index, IC, Pedal pulse § LVH – By Echocardiography, ECG § ED – Erectile Dysfunction; ED = ED § PP – Pulse Pressure – Importance of ISH
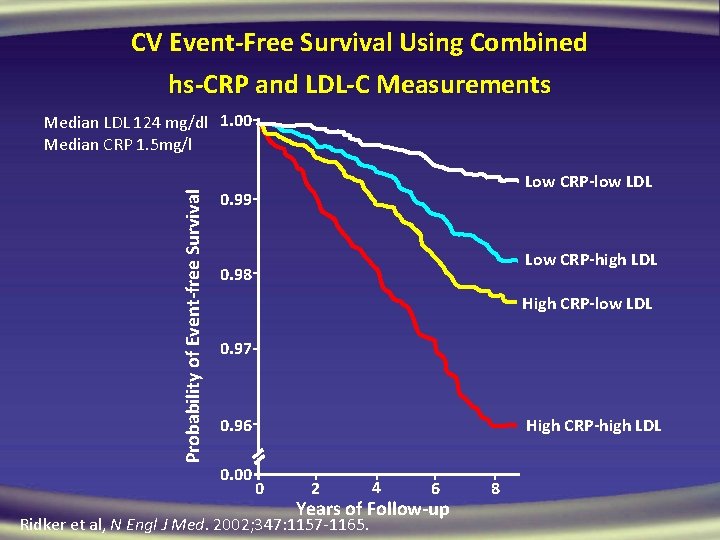
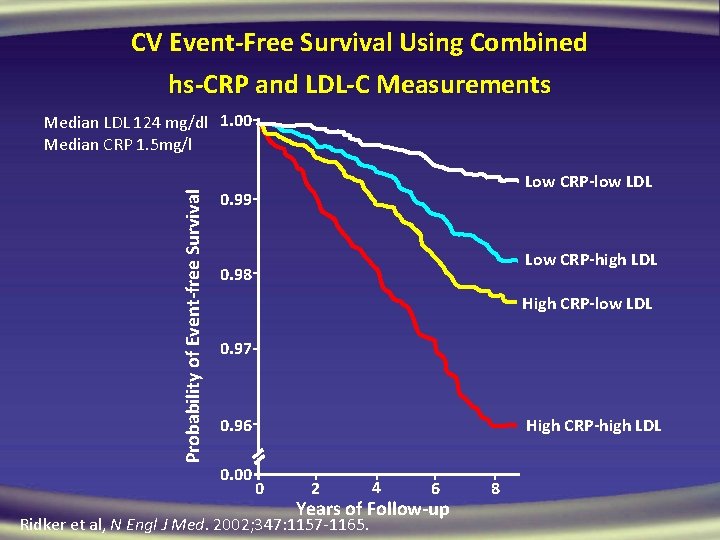
CV Event-Free Survival Using Combined hs-CRP and LDL-C Measurements Probability of Event-free Survival Median LDL 124 mg/dl 1. 00 Median CRP 1. 5 mg/l Low CRP-low LDL 0. 99 Low CRP-high LDL 0. 98 High CRP-low LDL 0. 97 0. 96 0. 00 High CRP-high LDL 0 2 4 6 Years of Follow-up Ridker et al, N Engl J Med. 2002; 347: 1157 -1165. 8
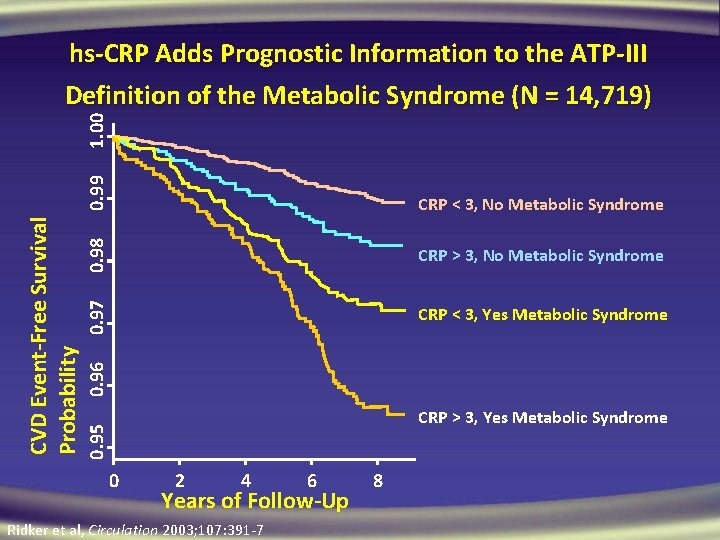
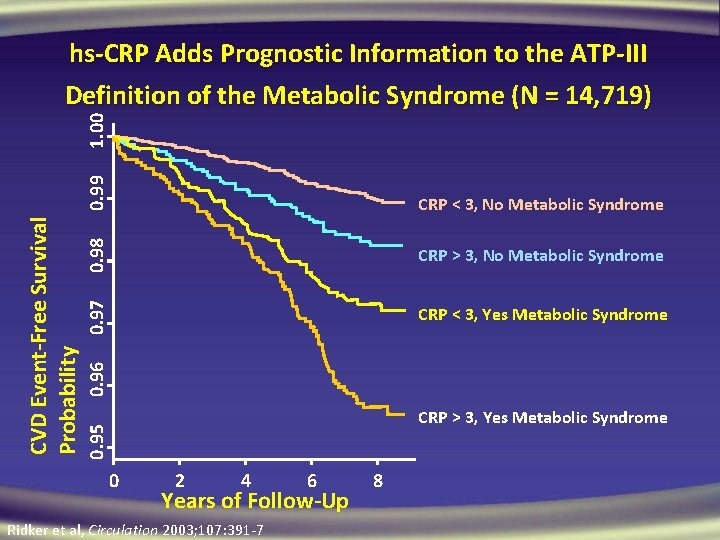
0. 99 0. 98 CRP > 3, No Metabolic Syndrome 0. 97 CRP < 3, Yes Metabolic Syndrome 0. 96 CRP < 3, No Metabolic Syndrome CRP > 3, Yes Metabolic Syndrome 0. 95 CVD Event-Free Survival Probability 1. 00 hs-CRP Adds Prognostic Information to the ATP-III Definition of the Metabolic Syndrome (N = 14, 719) 0 2 4 6 Years of Follow-Up Ridker et al, Circulation 2003; 107: 391 -7 8
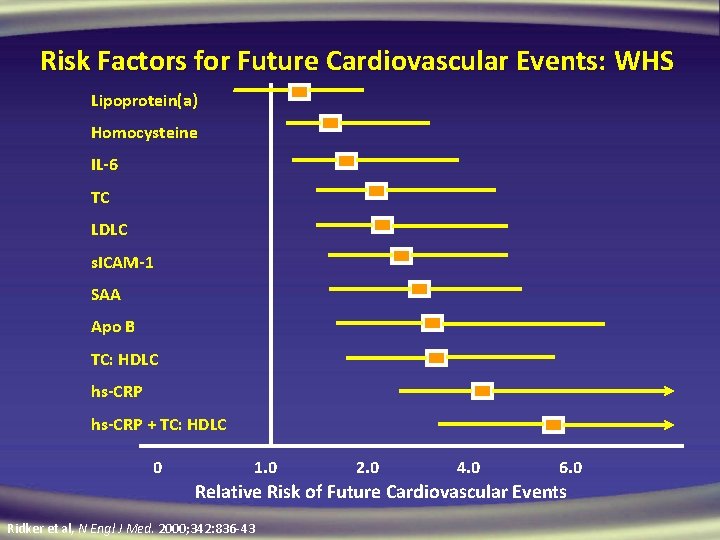
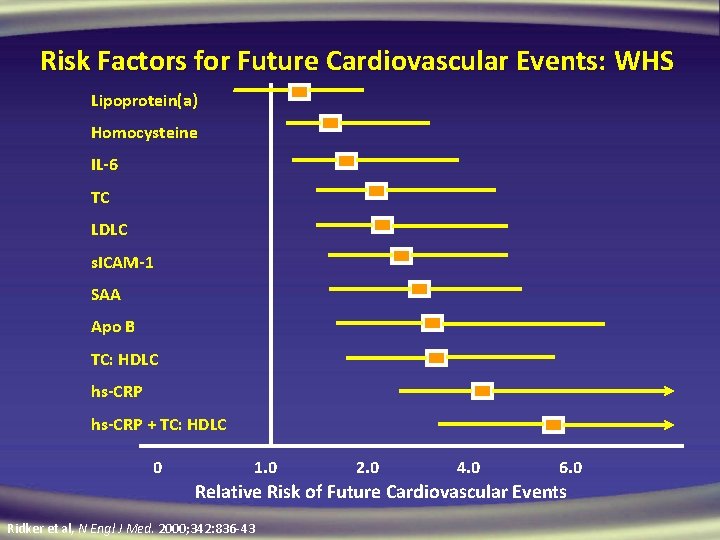
Risk Factors for Future Cardiovascular Events: WHS Lipoprotein(a) Homocysteine IL-6 TC LDLC s. ICAM-1 SAA Apo B TC: HDLC hs-CRP + TC: HDLC 0 1. 0 2. 0 4. 0 6. 0 Relative Risk of Future Cardiovascular Events Ridker et al, N Engl J Med. 2000; 342: 836 -43
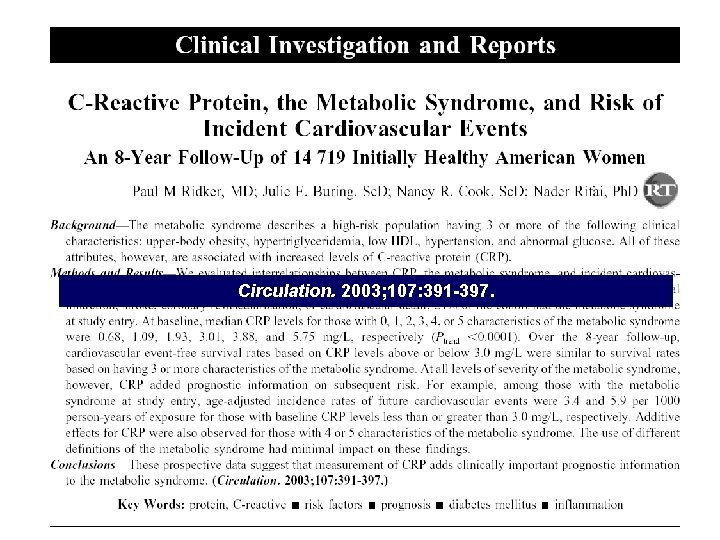
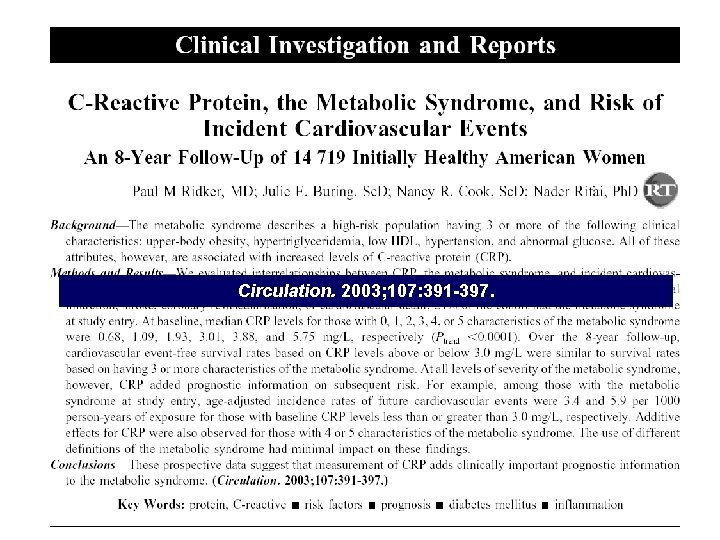
Circulation. 2003; 107: 391 -397.
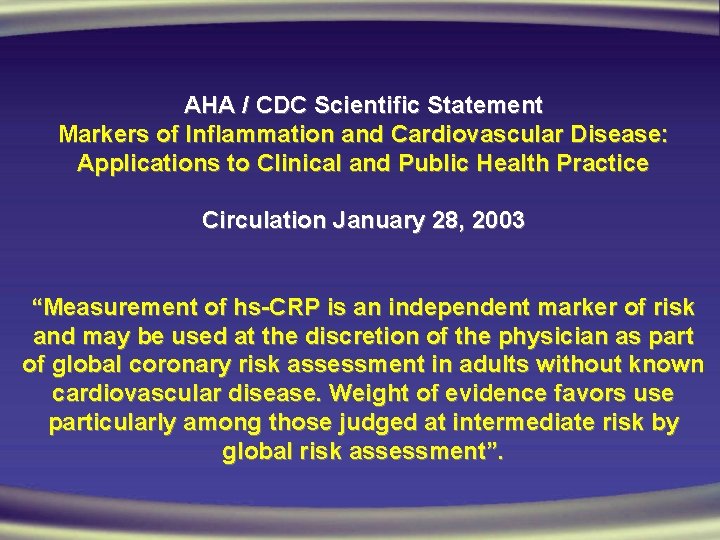
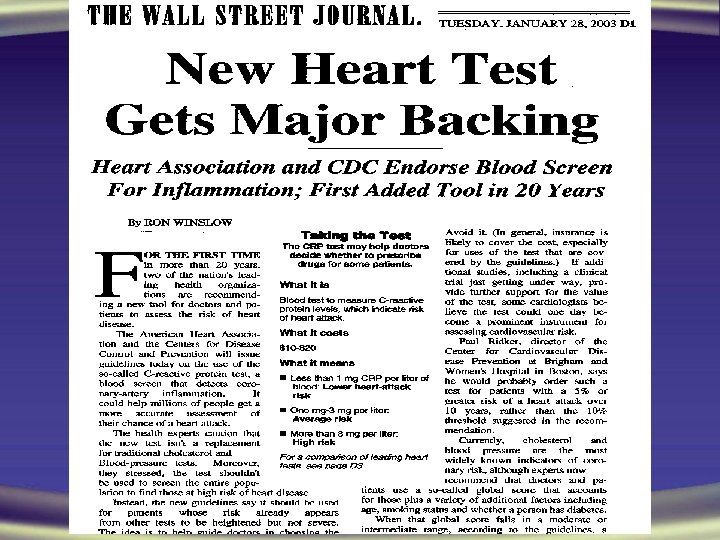
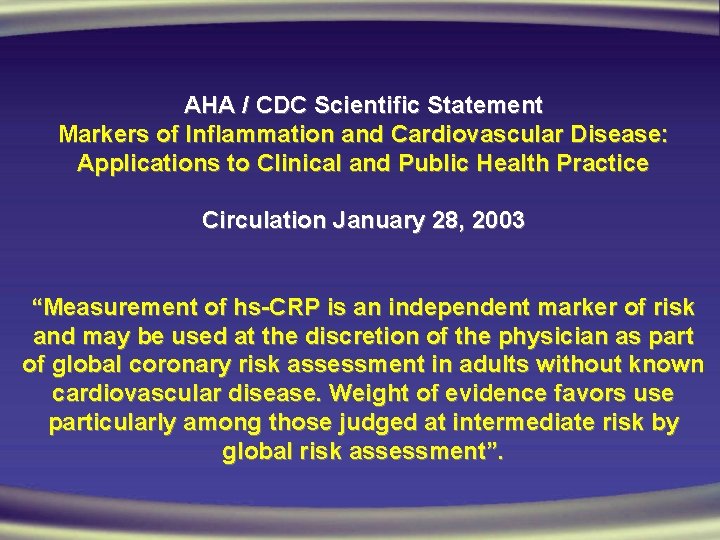
AHA / CDC Scientific Statement Markers of Inflammation and Cardiovascular Disease: Applications to Clinical and Public Health Practice Circulation January 28, 2003 “Measurement of hs-CRP is an independent marker of risk and may be used at the discretion of the physician as part of global coronary risk assessment in adults without known cardiovascular disease. Weight of evidence favors use particularly among those judged at intermediate risk by global risk assessment”.
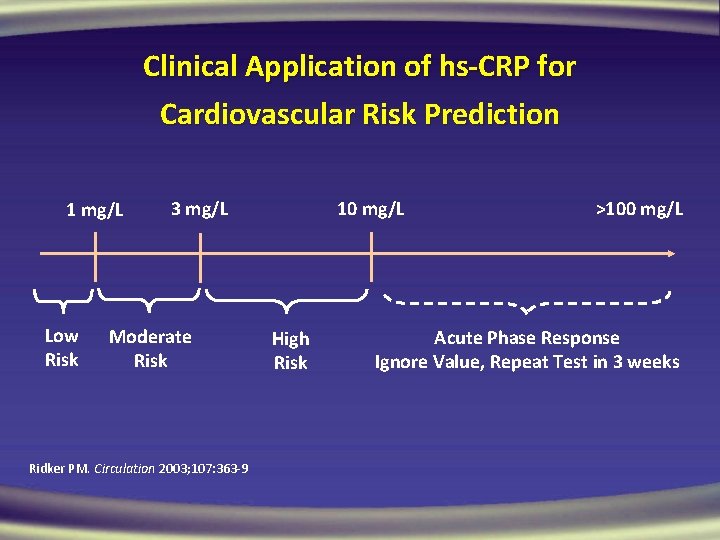
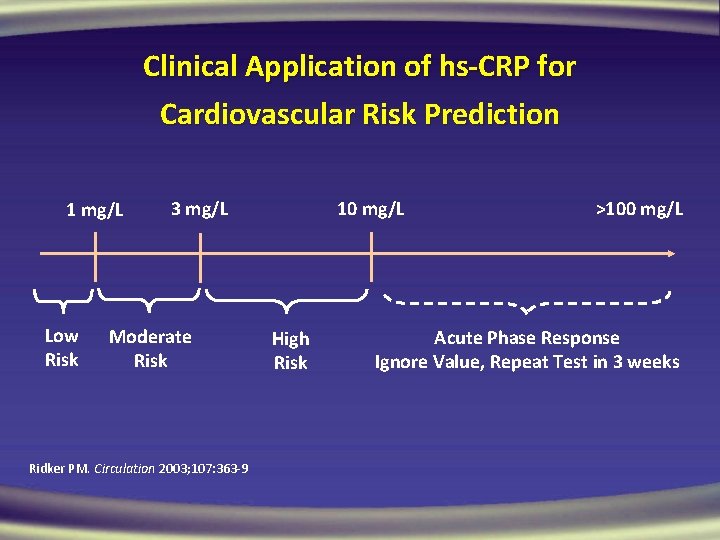
Clinical Application of hs-CRP for Cardiovascular Risk Prediction 1 mg/L Low Risk 3 mg/L Moderate Risk Ridker PM. Circulation 2003; 107: 363 -9 10 mg/L High Risk >100 mg/L Acute Phase Response Ignore Value, Repeat Test in 3 weeks
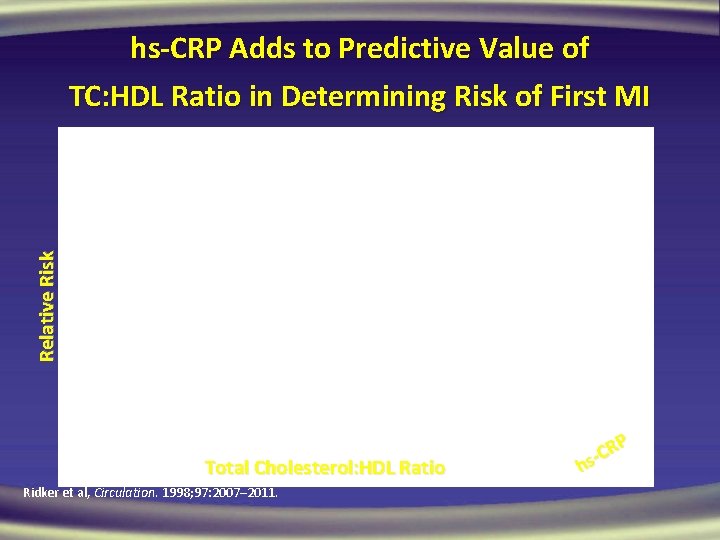
Relative Risk hs-CRP Adds to Predictive Value of TC: HDL Ratio in Determining Risk of First MI Total Cholesterol: HDL Ratio Ridker et al, Circulation. 1998; 97: 2007– 2011. RP C hs
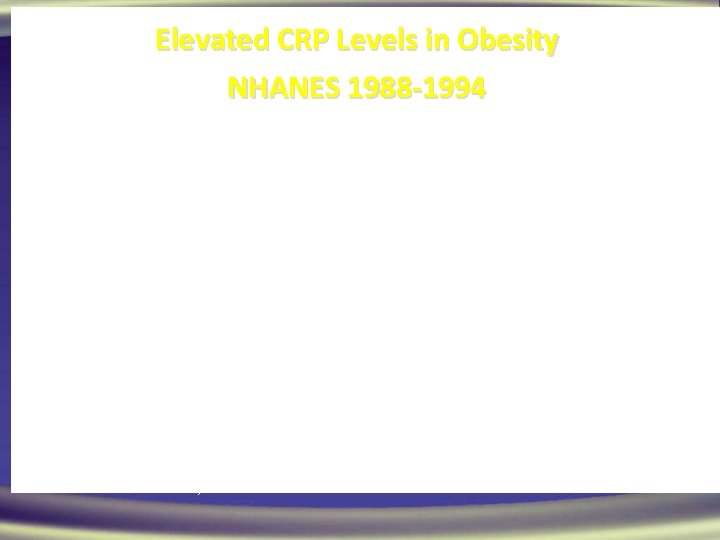
Percent with CRP 0. 22 mg/d. L Elevated CRP Levels in Obesity NHANES 1988 -1994 Normal Visser M et al. JAMA 1999; 282: 2131 -2135. Overweight Obese
31
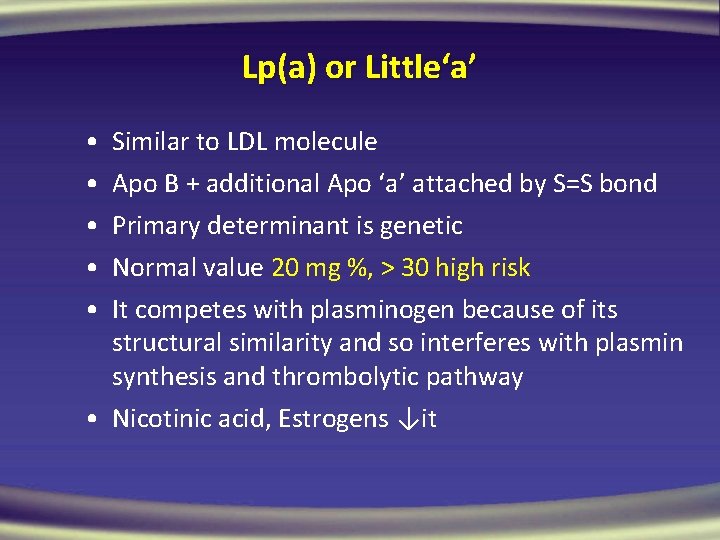
Lp(a) or Little‘a’ • • • Similar to LDL molecule Apo B + additional Apo ‘a’ attached by S=S bond Primary determinant is genetic Normal value 20 mg %, > 30 high risk It competes with plasminogen because of its structural similarity and so interferes with plasmin synthesis and thrombolytic pathway • Nicotinic acid, Estrogens ↓it
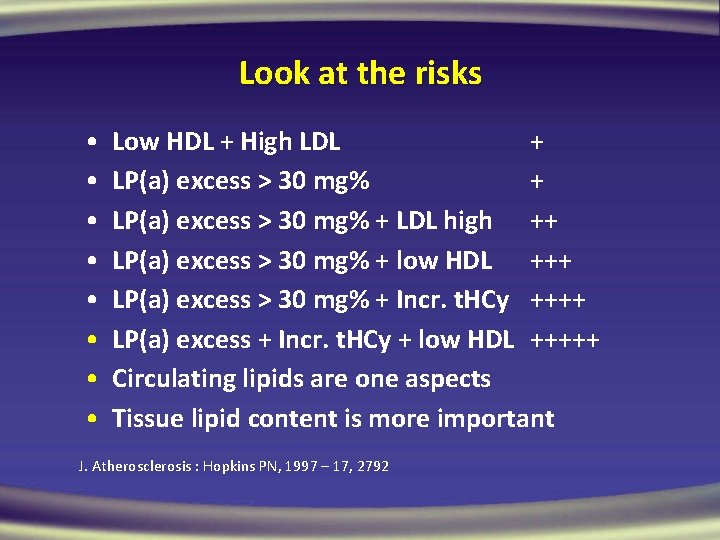
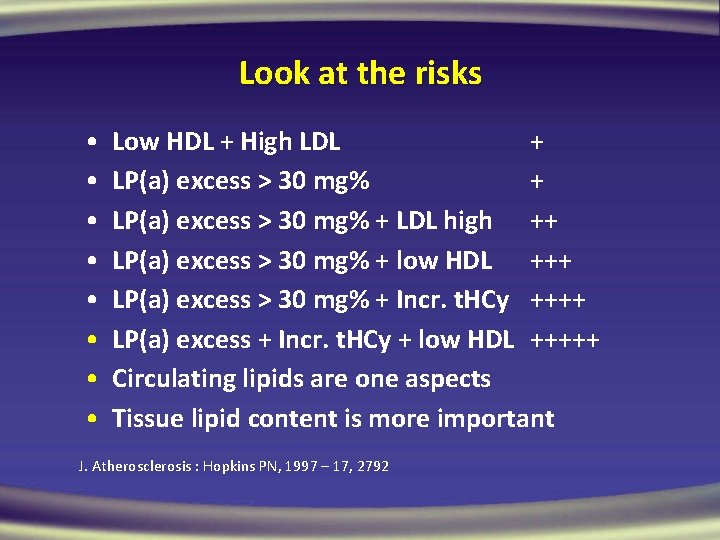
Look at the risks • • Low HDL + High LDL + LP(a) excess > 30 mg% + LDL high ++ LP(a) excess > 30 mg% + low HDL +++ LP(a) excess > 30 mg% + Incr. t. HCy ++++ LP(a) excess + Incr. t. HCy + low HDL +++++ Circulating lipids are one aspects Tissue lipid content is more important J. Atherosclerosis : Hopkins PN, 1997 – 17, 2792
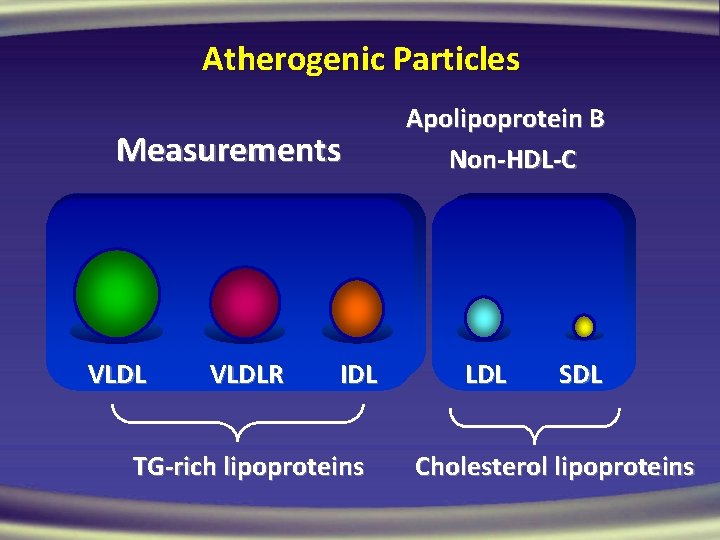
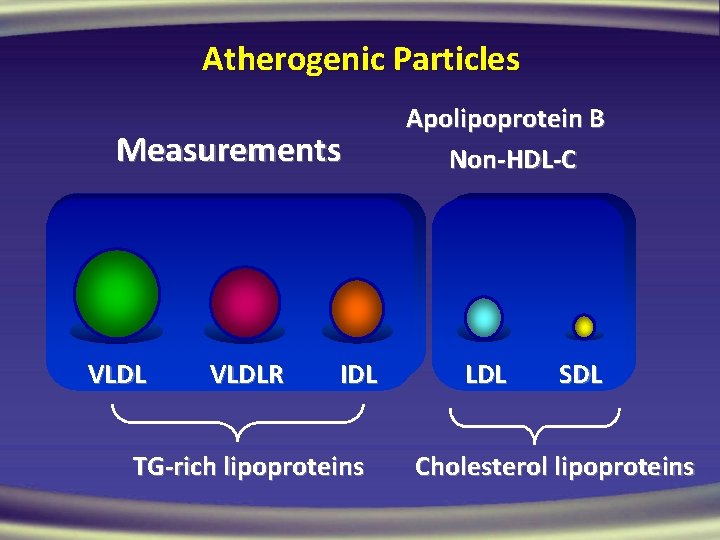
Atherogenic Particles Measurements VLDLR IDL TG-rich lipoproteins Apolipoprotein B Non-HDL-C LDL SDL Cholesterol lipoproteins
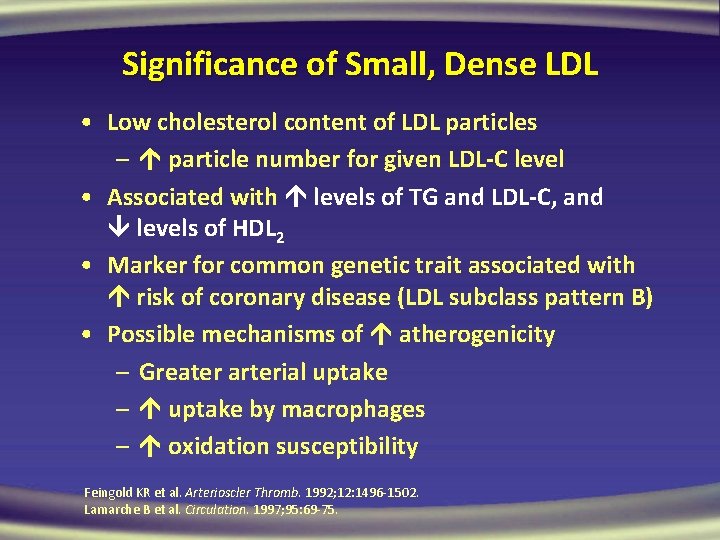
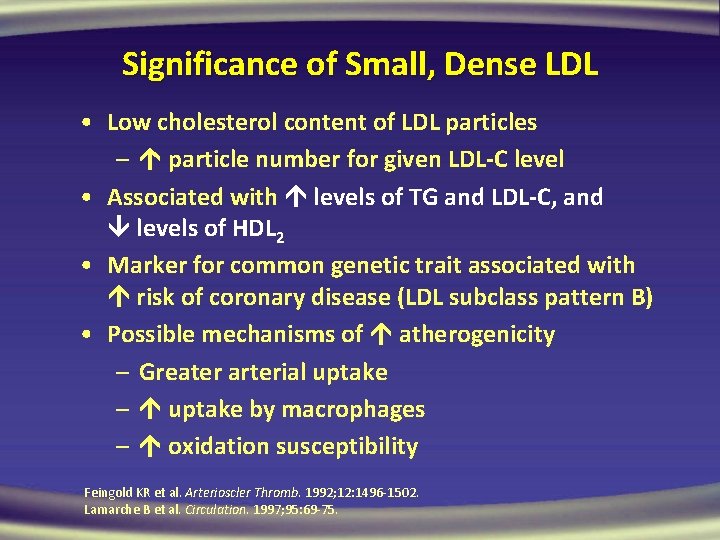
Significance of Small, Dense LDL • Low cholesterol content of LDL particles – particle number for given LDL-C level • Associated with levels of TG and LDL-C, and levels of HDL 2 • Marker for common genetic trait associated with risk of coronary disease (LDL subclass pattern B) • Possible mechanisms of atherogenicity – Greater arterial uptake – uptake by macrophages – oxidation susceptibility Feingold KR et al. Arterioscler Thromb. 1992; 12: 1496 -1502. Lamarche B et al. Circulation. 1997; 95: 69 -75.
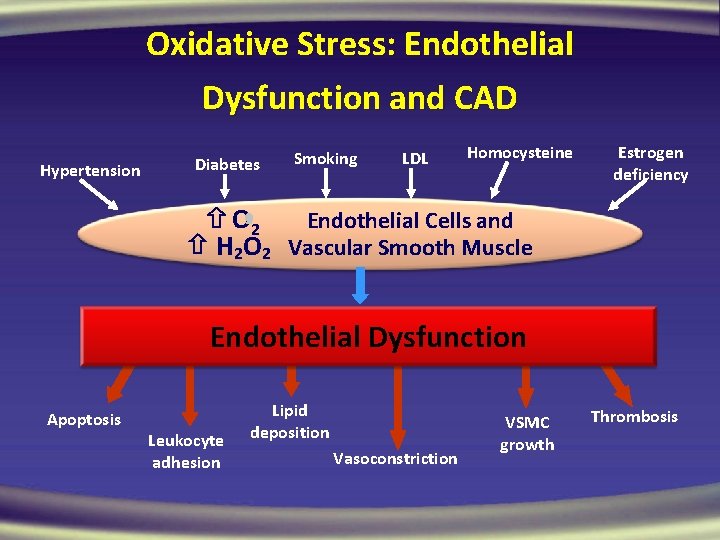
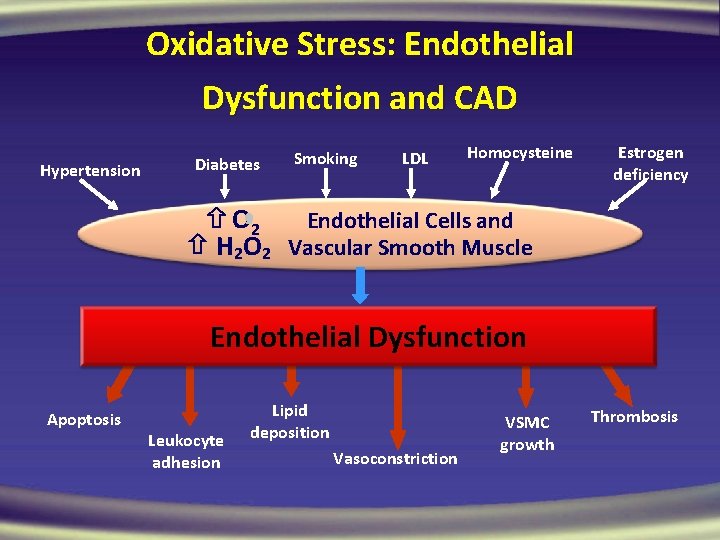
Oxidative Stress: Endothelial Dysfunction and CAD Hypertension Diabetes Smoking LDL Homocysteine Estrogen deficiency O 2 Endothelial Cells and H 2 O 2 Vascular Smooth Muscle Endothelial Dysfunction Apoptosis Leukocyte adhesion Lipid deposition Vasoconstriction VSMC growth Thrombosis
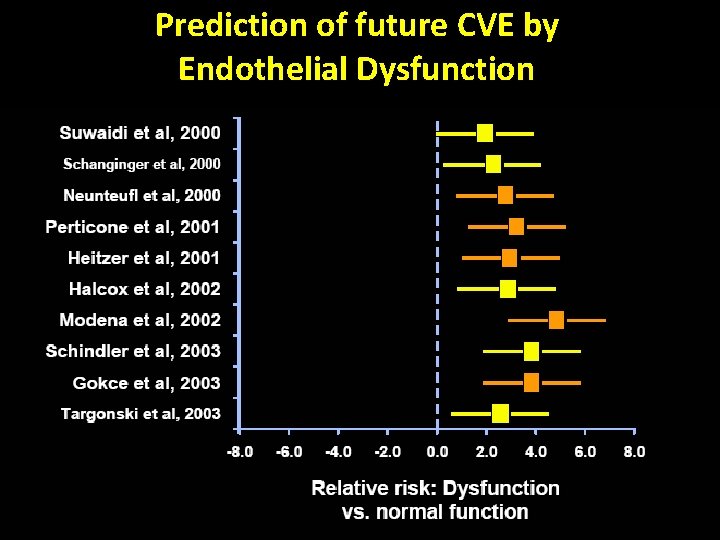
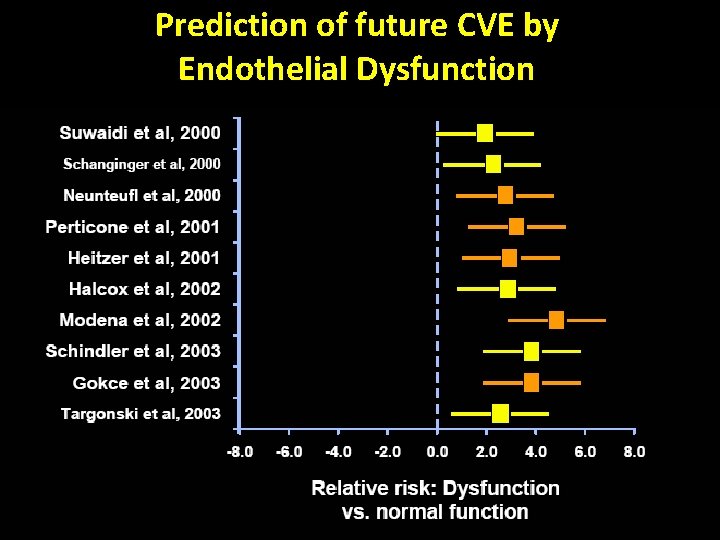
Prediction of future CVE by Endothelial Dysfunction 37
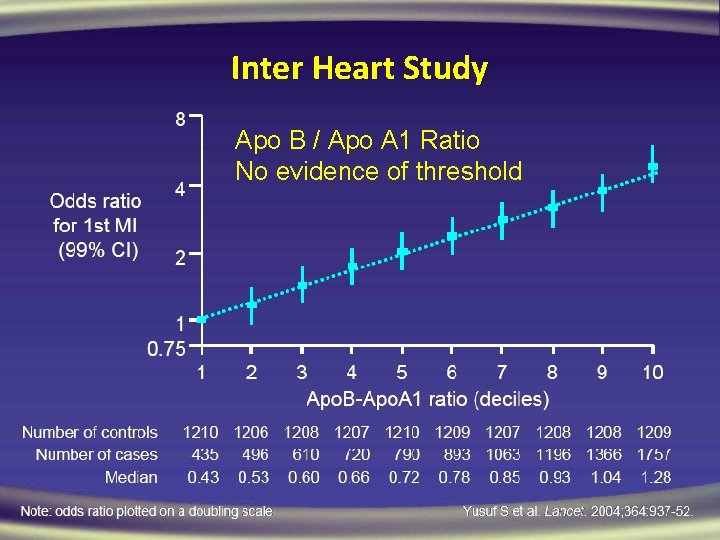
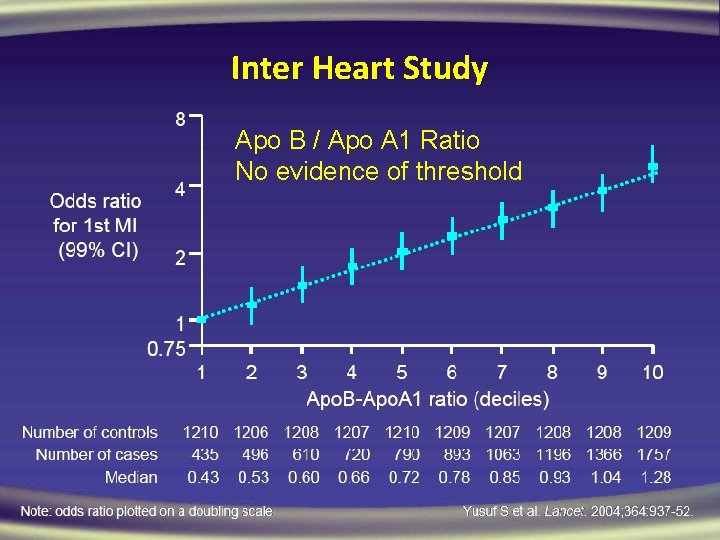
Inter Heart Study Apo B / Apo A 1 Ratio No evidence of threshold
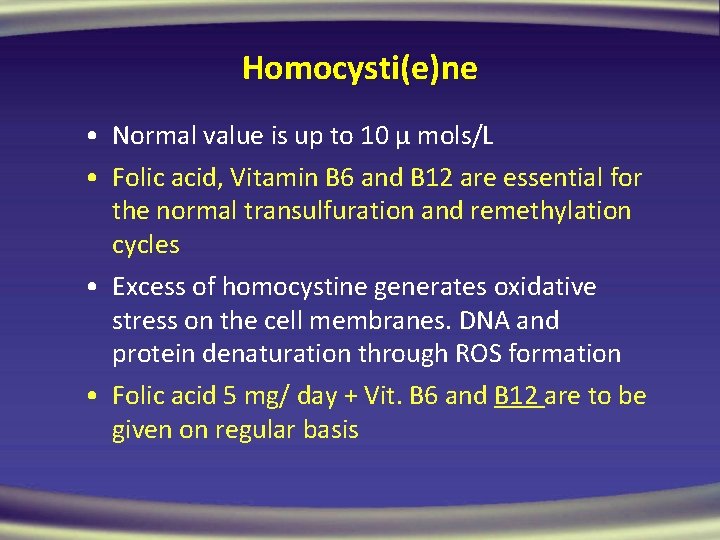
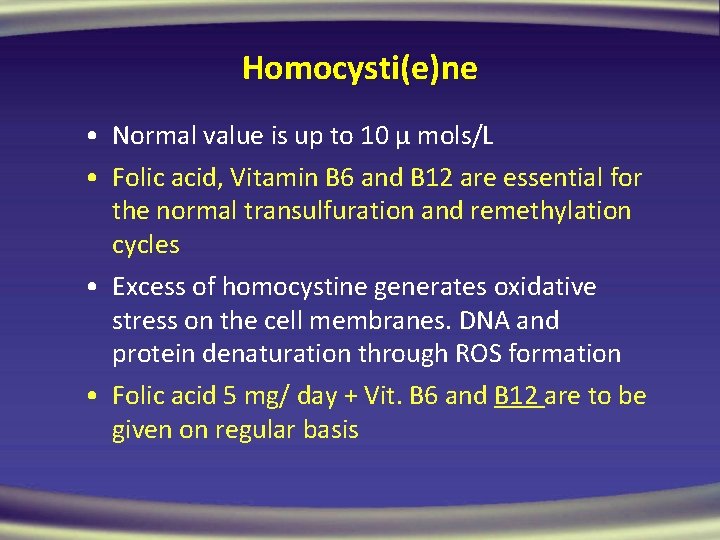
Homocysti(e)ne • Normal value is up to 10 μ mols/L • Folic acid, Vitamin B 6 and B 12 are essential for the normal transulfuration and remethylation cycles • Excess of homocystine generates oxidative stress on the cell membranes. DNA and protein denaturation through ROS formation • Folic acid 5 mg/ day + Vit. B 6 and B 12 are to be given on regular basis
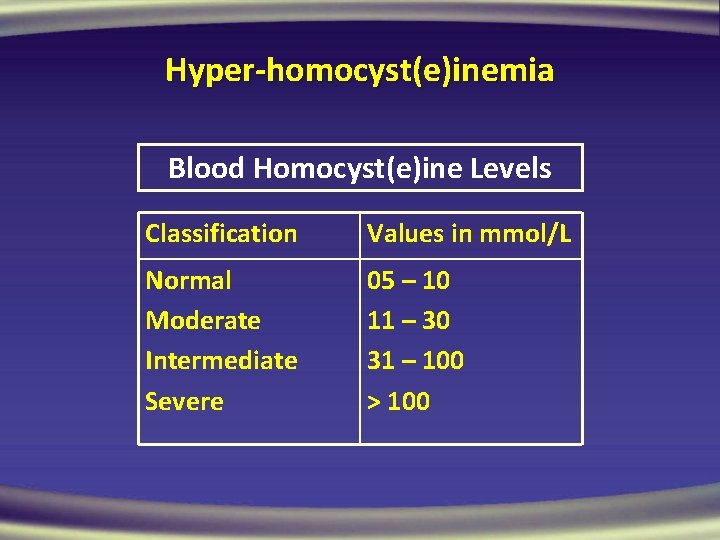
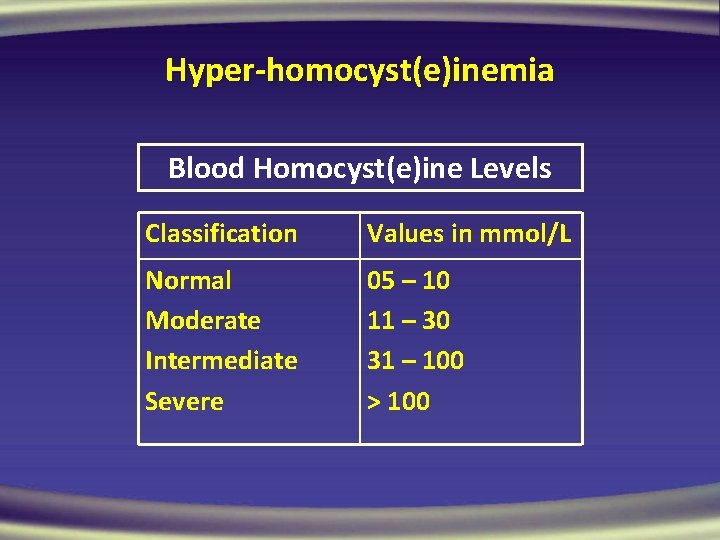
Hyper-homocyst(e)inemia Blood Homocyst(e)ine Levels Classification Values in mmol/L Normal Moderate Intermediate Severe 05 – 10 11 – 30 31 – 100 > 100
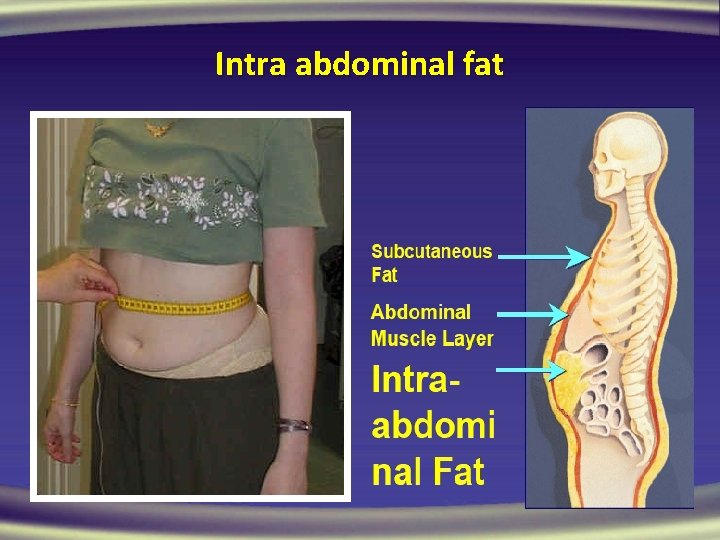
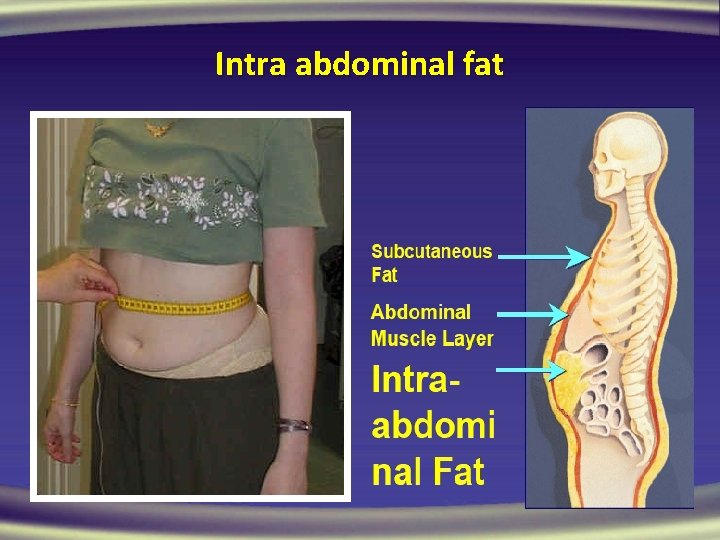
Intra abdominal fat
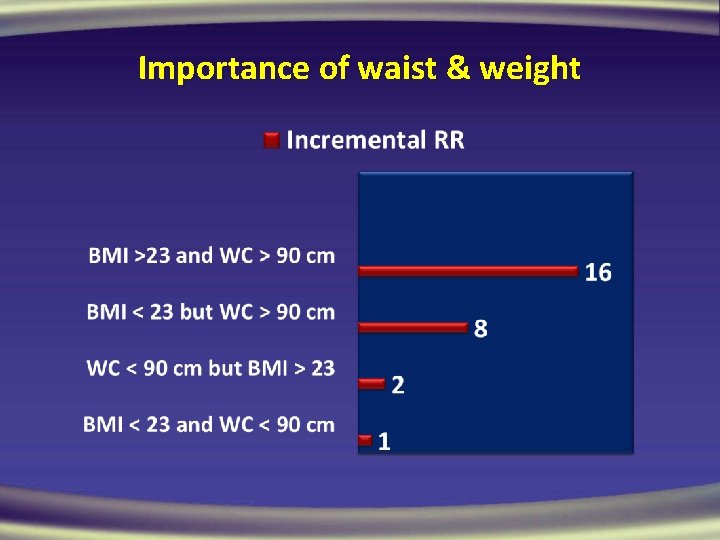
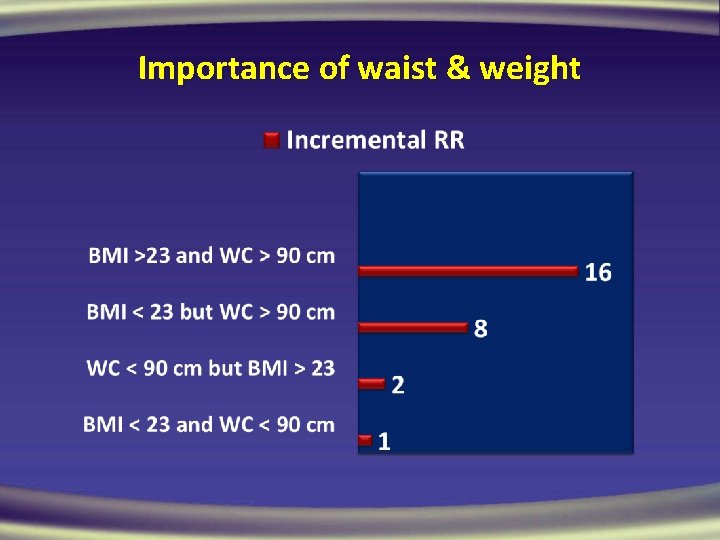
Importance of waist & weight
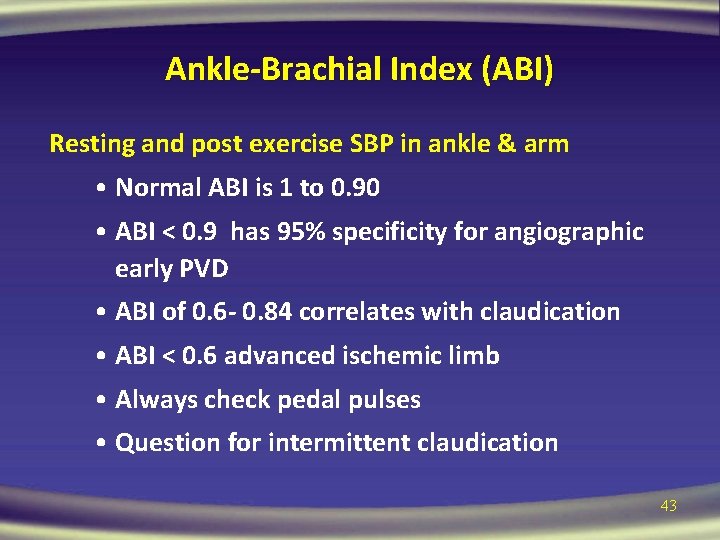
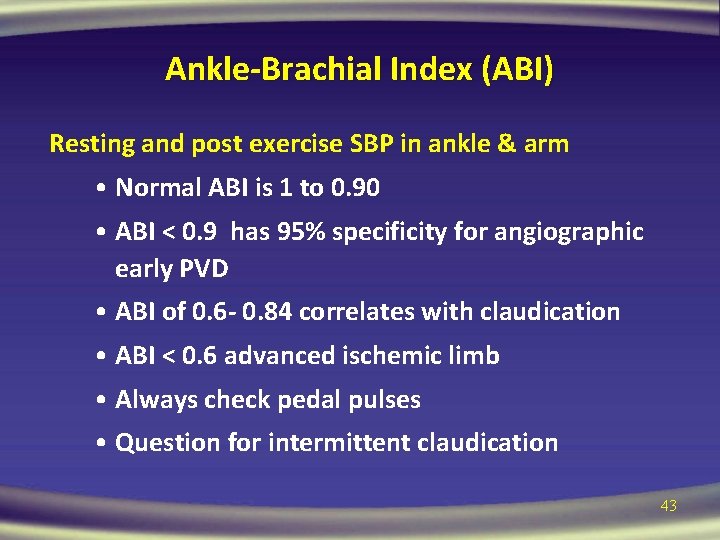
Ankle-Brachial Index (ABI) Resting and post exercise SBP in ankle & arm • Normal ABI is 1 to 0. 90 • ABI < 0. 9 has 95% specificity for angiographic early PVD • ABI of 0. 6 - 0. 84 correlates with claudication • ABI < 0. 6 advanced ischemic limb • Always check pedal pulses • Question for intermittent claudication 43
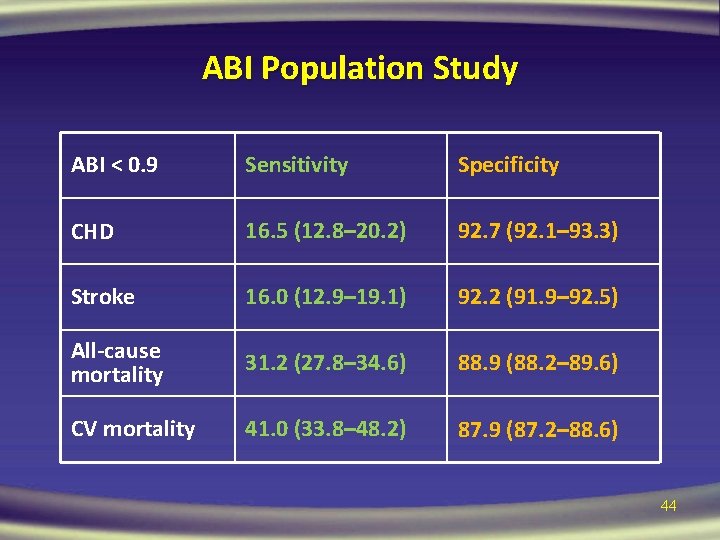
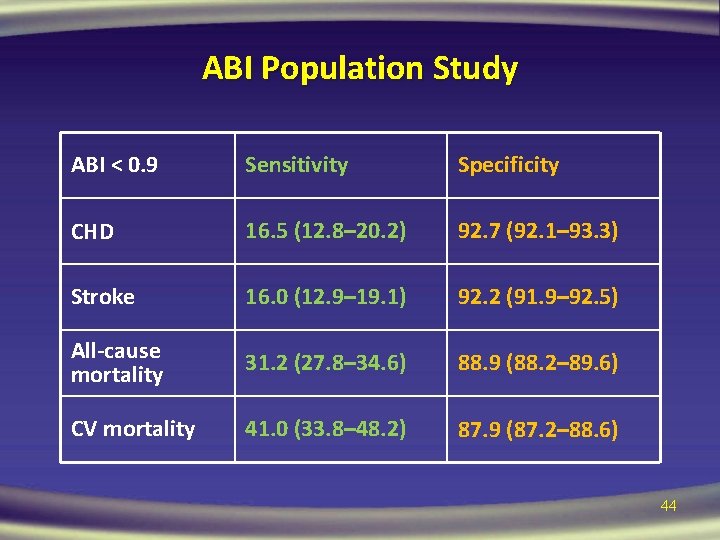
ABI Population Study ABI < 0. 9 Sensitivity Specificity CHD 16. 5 (12. 8– 20. 2) 92. 7 (92. 1– 93. 3) Stroke 16. 0 (12. 9– 19. 1) 92. 2 (91. 9– 92. 5) All-cause mortality 31. 2 (27. 8– 34. 6) 88. 9 (88. 2– 89. 6) CV mortality 41. 0 (33. 8– 48. 2) 87. 9 (87. 2– 88. 6) 44
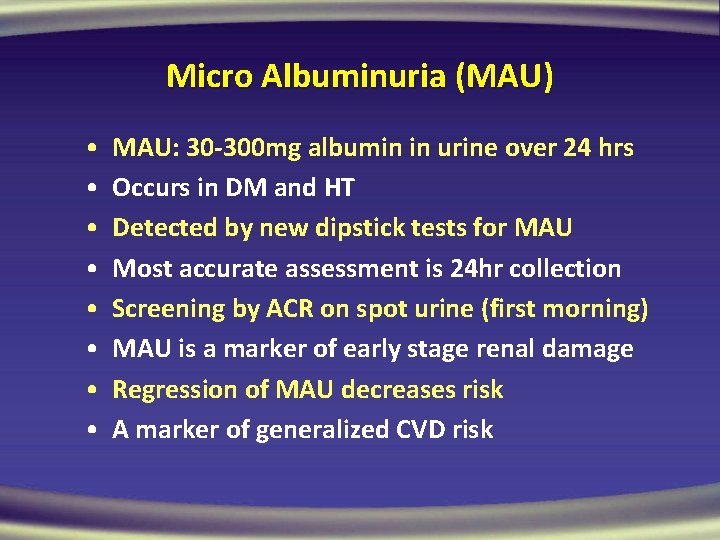
Micro Albuminuria (MAU) • • MAU: 30 -300 mg albumin in urine over 24 hrs Occurs in DM and HT Detected by new dipstick tests for MAU Most accurate assessment is 24 hr collection Screening by ACR on spot urine (first morning) MAU is a marker of early stage renal damage Regression of MAU decreases risk A marker of generalized CVD risk
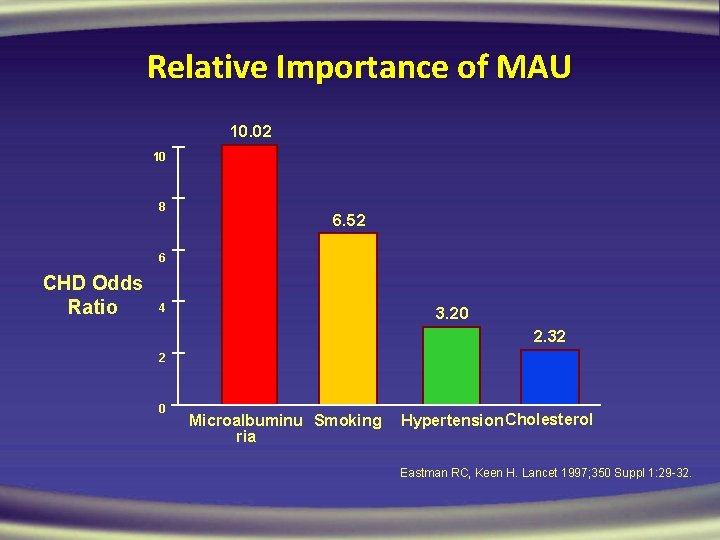
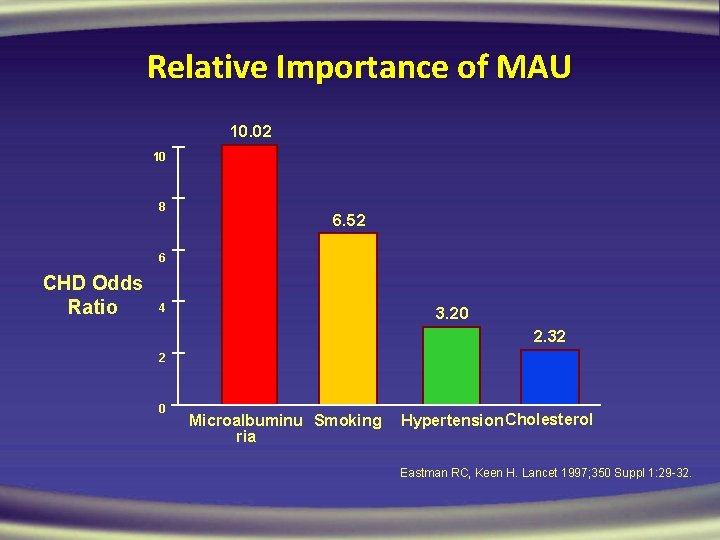
Relative Importance of MAU 10. 02 10 8 6. 52 6 CHD Odds Ratio 4 3. 20 2. 32 2 0 Microalbuminu Smoking ria Hypertension Cholesterol Eastman RC, Keen H. Lancet 1997; 350 Suppl 1: 29 -32.
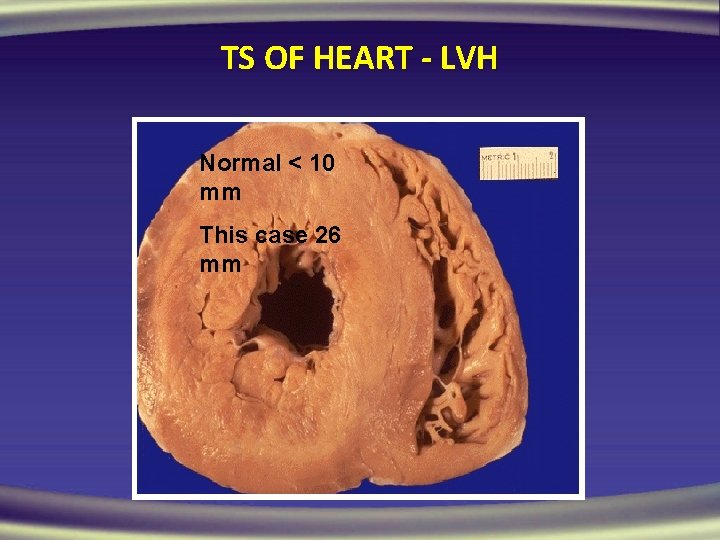
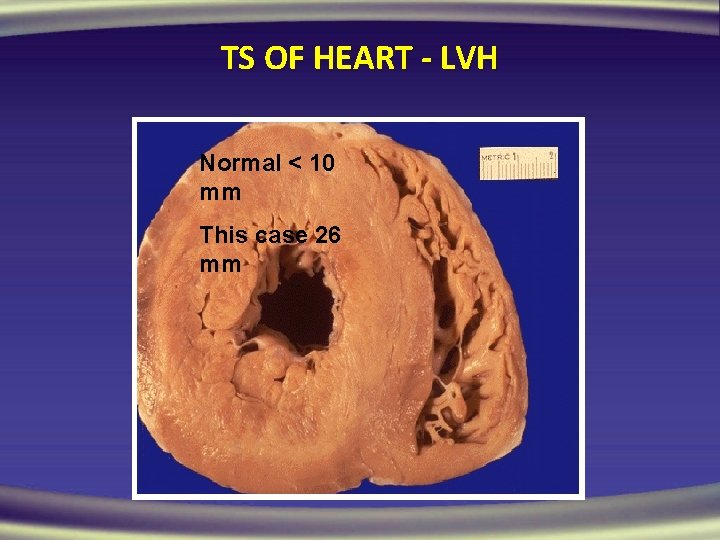
TS OF HEART - LVH Normal < 10 mm This case 26 mm
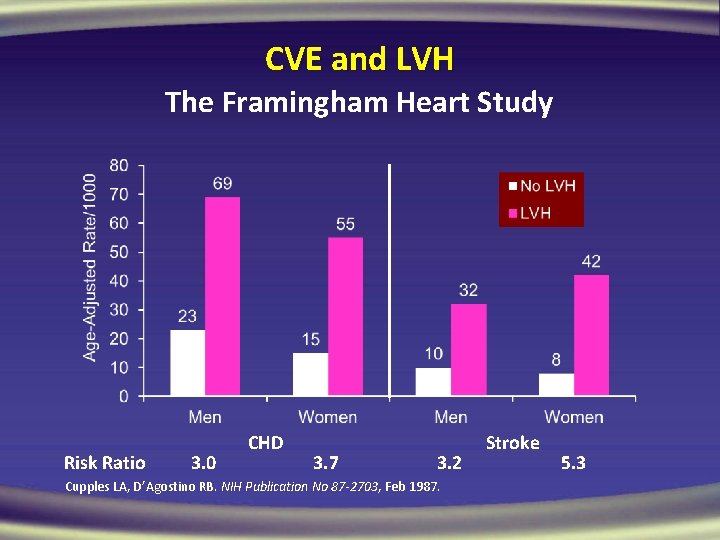
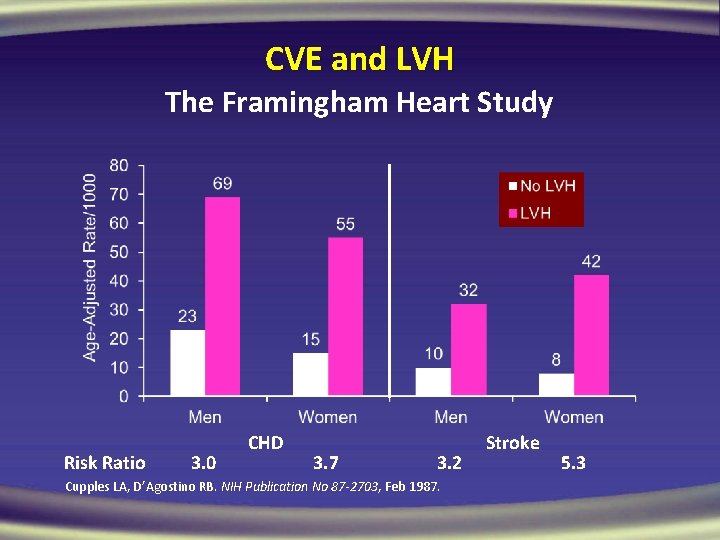
CVE and LVH The Framingham Heart Study Risk Ratio 3. 0 CHD 3. 7 3. 2 Cupples LA, D’Agostino RB. NIH Publication No 87 -2703, Feb 1987. Stroke 5. 3
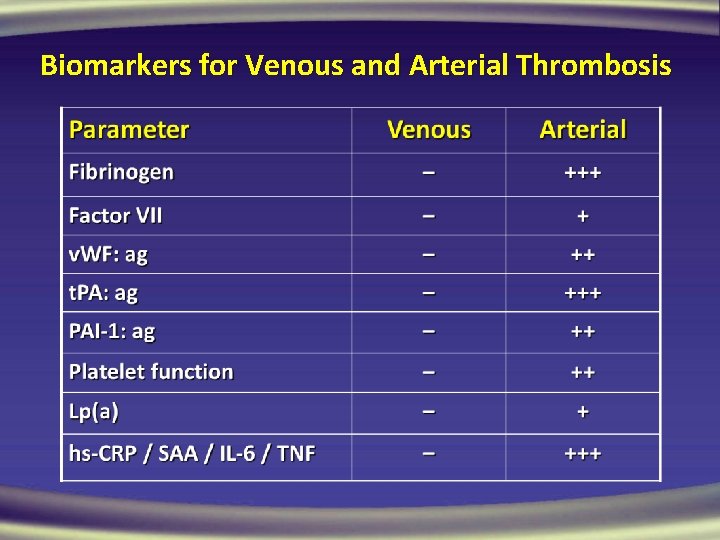
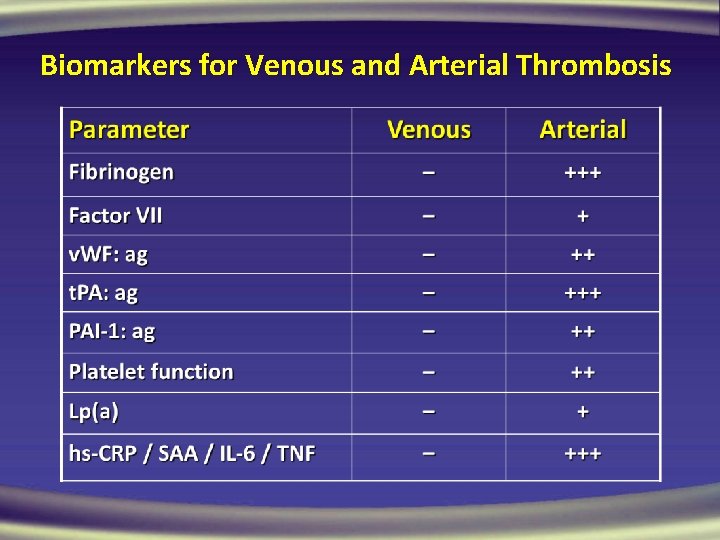
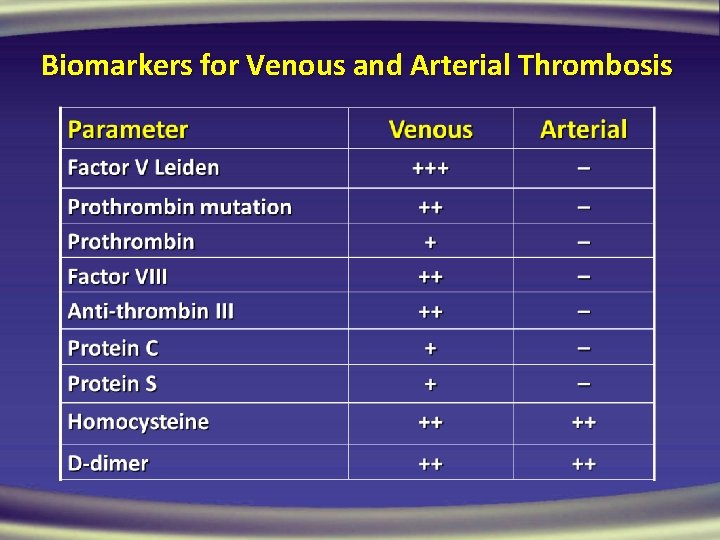
Biomarkers for Venous and Arterial Thrombosis
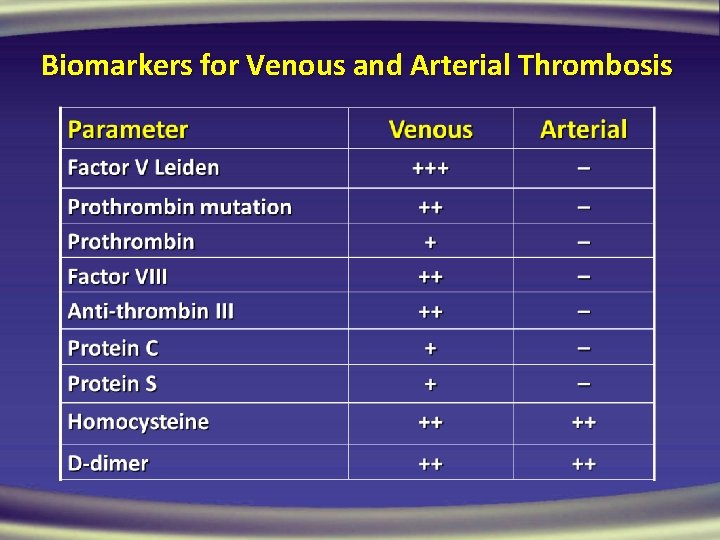
Biomarkers for Venous and Arterial Thrombosis
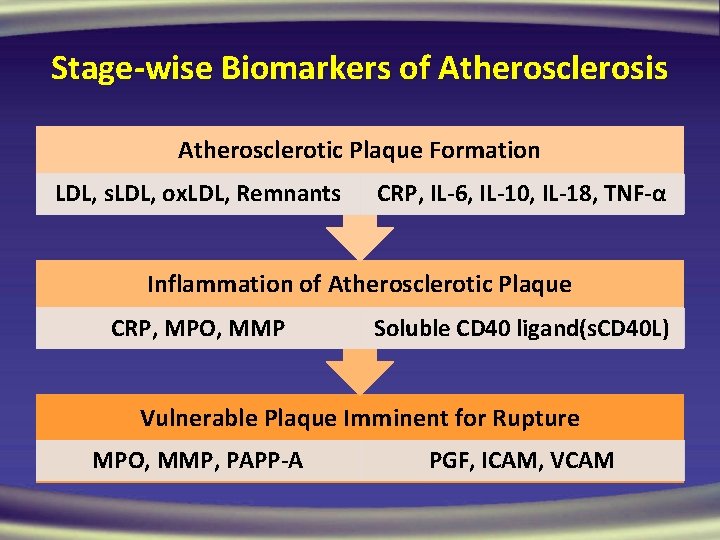
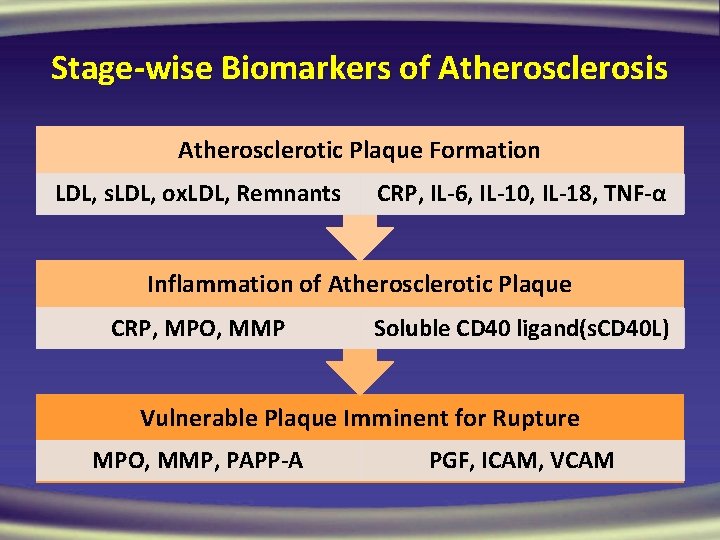
Stage-wise Biomarkers of Atherosclerosis Atherosclerotic Plaque Formation LDL, s. LDL, ox. LDL, Remnants CRP, IL-6, IL-10, IL-18, TNF-α Inflammation of Atherosclerotic Plaque CRP, MPO, MMP Soluble CD 40 ligand(s. CD 40 L) Vulnerable Plaque Imminent for Rupture MPO, MMP, PAPP-A PGF, ICAM, VCAM
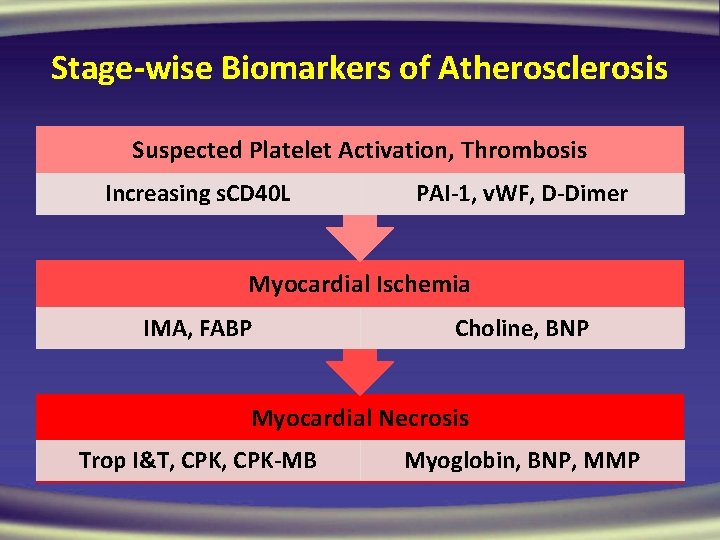
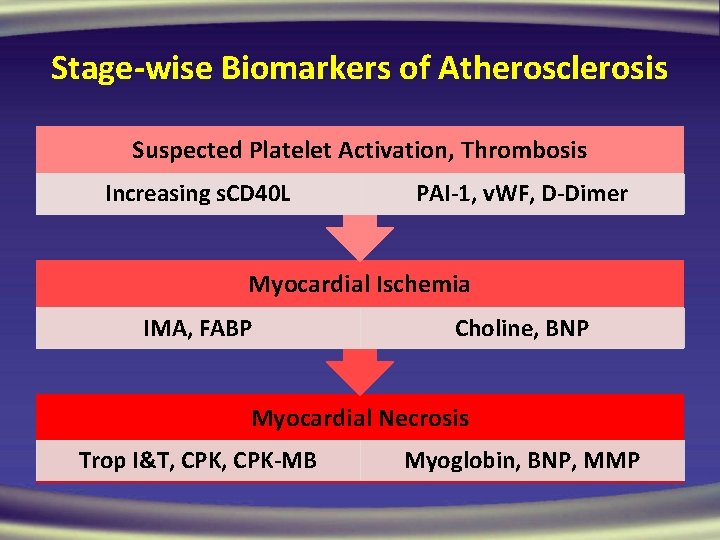
Stage-wise Biomarkers of Atherosclerosis Suspected Platelet Activation, Thrombosis Increasing s. CD 40 L PAI-1, v. WF, D-Dimer Myocardial Ischemia IMA, FABP Choline, BNP Myocardial Necrosis Trop I&T, CPK-MB Myoglobin, BNP, MMP
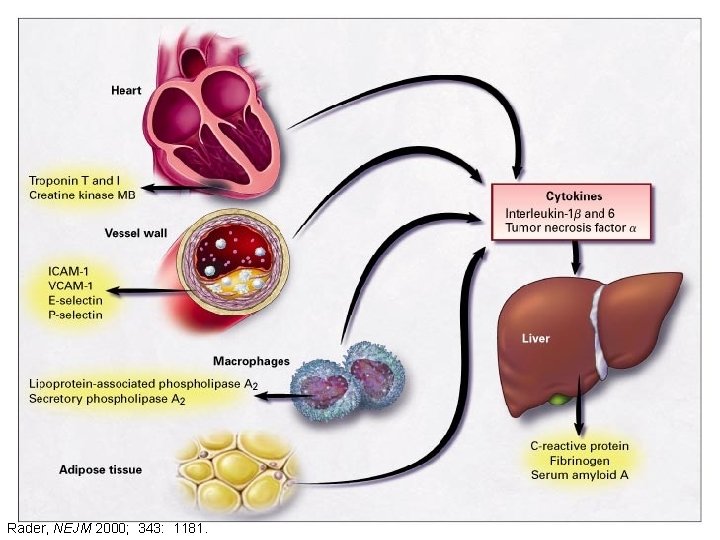
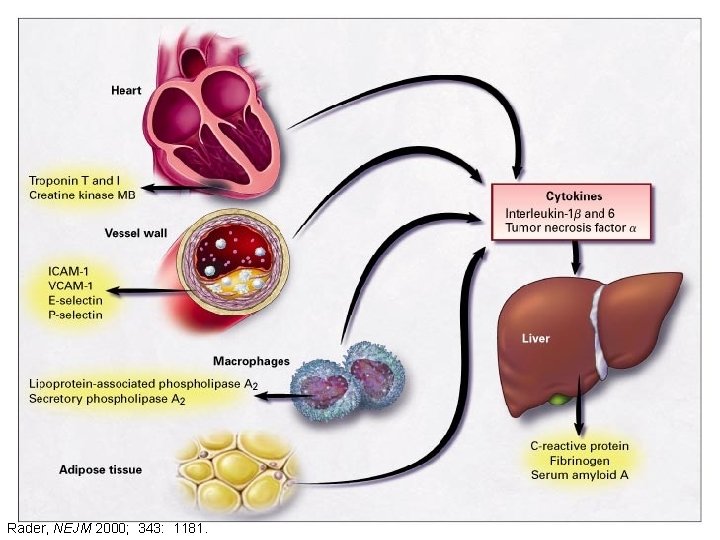
Rader, NEJM 2000; 343: 1181.
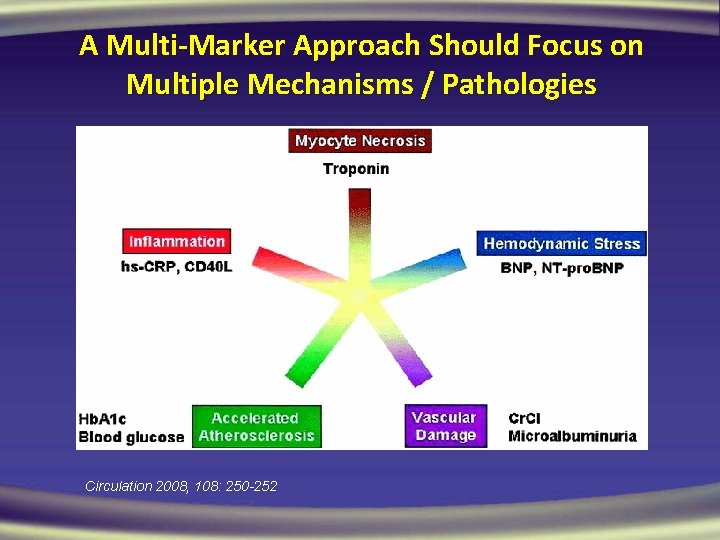
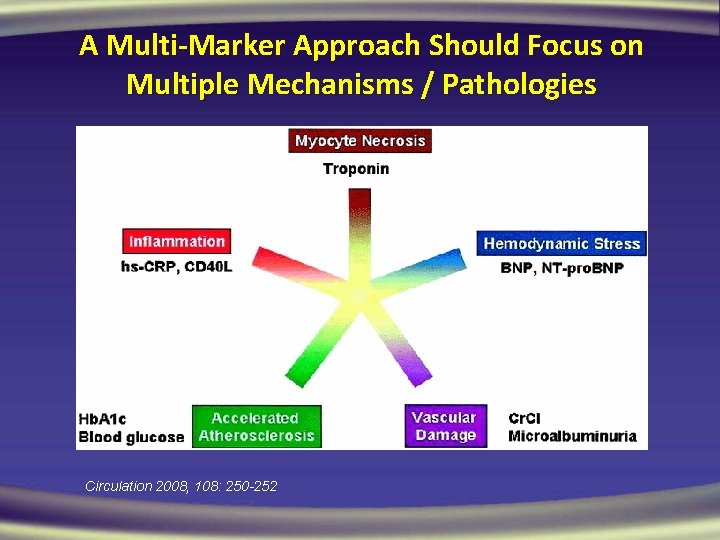
A Multi-Marker Approach Should Focus on Multiple Mechanisms / Pathologies Circulation 2008, 108: 250 -252
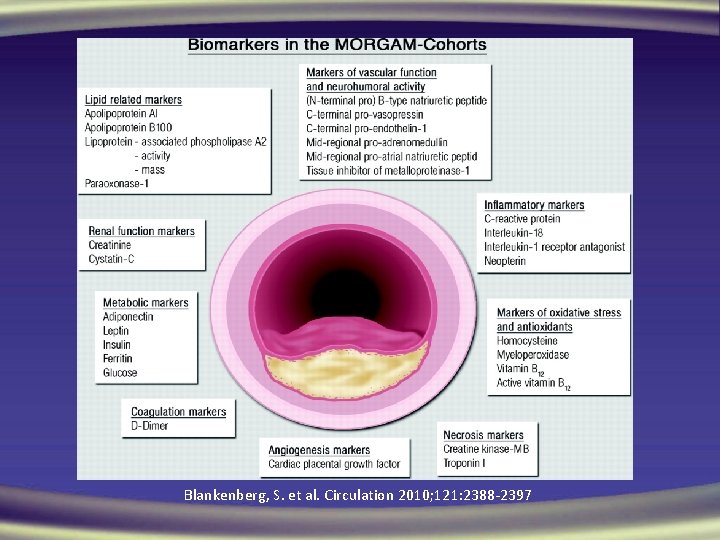
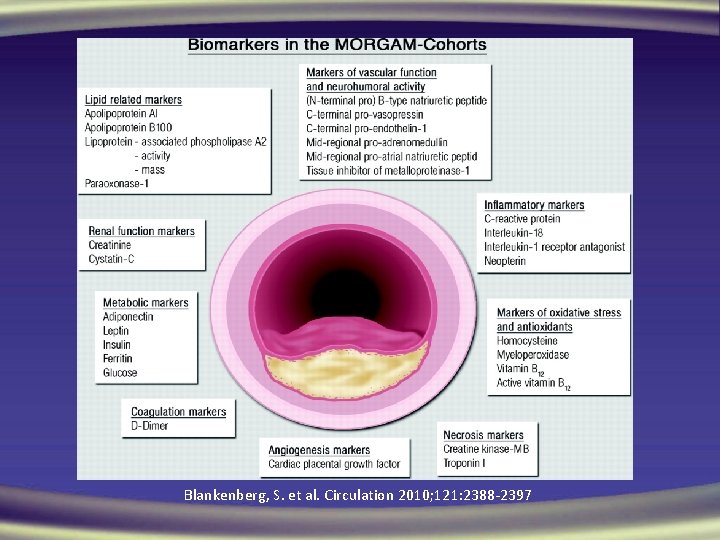
Blankenberg, S. et al. Circulation 2010; 121: 2388 -2397
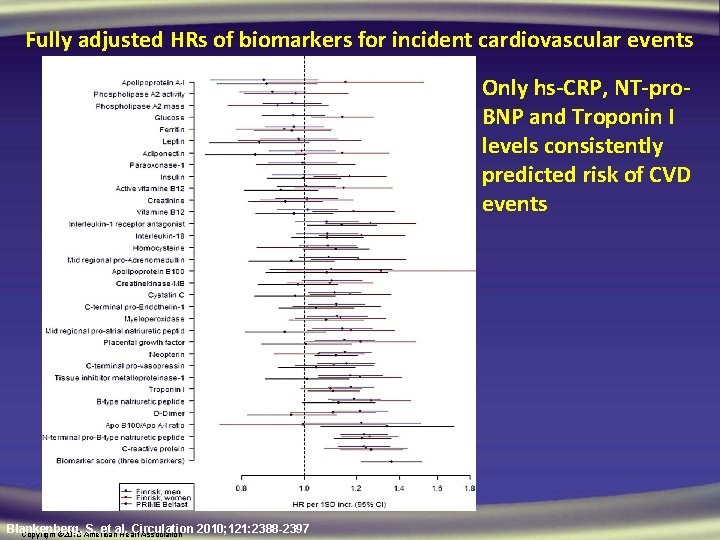
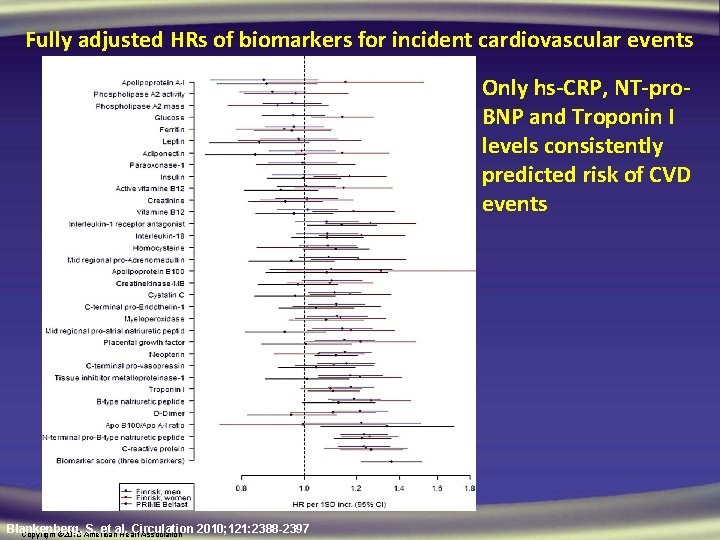
Fully adjusted HRs of biomarkers for incident cardiovascular events Only hs-CRP, NT-pro. BNP and Troponin I levels consistently predicted risk of CVD events Blankenberg, S. et al. Circulation 2010; 121: 2388 -2397 Copyright © 2010 American Heart Association
Conclusions • Conventional Risk Factors do not predict global risk well • Measurement of certain biomarkers such as hs-CRP may be useful in conjunction with global risk assessment to improve risk classification. • Insufficient data at the present time to recommend novel biomarkers to screen the population at large, but in selected intermediate risk groups may be appropriate. • Individual biomarkers do not markedly improve risk assess. • None of these are ready for day-to-day clinical application • Cost-effectiveness and outcome studies needed

THANK YOU ALL
 Non vascular plants
Non vascular plants Non vascular plant
Non vascular plant Vascular and non vascular difference
Vascular and non vascular difference Liquidity measures
Liquidity measures Vddi pharmaceuticals
Vddi pharmaceuticals Stopul cardio respirator definitie
Stopul cardio respirator definitie Sindrom velo cardio facial
Sindrom velo cardio facial Index cardio thoracique
Index cardio thoracique Index cardio thoracique
Index cardio thoracique Lordotic chest x ray
Lordotic chest x ray Cardio vision
Cardio vision Apex poumon
Apex poumon Cauze reversibile de stop cardio-respirator
Cauze reversibile de stop cardio-respirator Abdomen bdi
Abdomen bdi Cardio clearance meaning
Cardio clearance meaning Cardio sense
Cardio sense Thorax bréviligne
Thorax bréviligne Sufijo grama
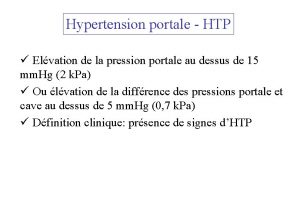
Sufijo grama Hypertension portale
Hypertension portale Cardiomems video
Cardiomems video Barorécepteur et chémorécepteur
Barorécepteur et chémorécepteur кардио софт
кардио софт Cardio map
Cardio map Investigator photos
Investigator photos Trusight cardio
Trusight cardio 4tech cardio
4tech cardio Discovery cardio care programme
Discovery cardio care programme Pickwickian syndrome wiki
Pickwickian syndrome wiki Electro cardio gram
Electro cardio gram Atl cardio
Atl cardio Cardio alex
Cardio alex Risk projection
Risk projection Risk mitigation avoidance
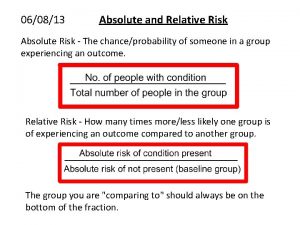
Risk mitigation avoidance Absolute risk vs relative risk
Absolute risk vs relative risk Residual risk and secondary risk pmp
Residual risk and secondary risk pmp Tracing vs vouching
Tracing vs vouching Absolute risk vs relative risk
Absolute risk vs relative risk The stock market game activity sheet 2 answers
The stock market game activity sheet 2 answers Medium risk examples
Medium risk examples Risk financing transfer adalah
Risk financing transfer adalah The biggest risk is not taking any risks
The biggest risk is not taking any risks Key risk indicators template
Key risk indicators template Business risk audit
Business risk audit Business risk vs financial risk capital structure
Business risk vs financial risk capital structure Attributable risk formula
Attributable risk formula Risk map risk management
Risk map risk management Relative risk and attributable risk
Relative risk and attributable risk Low sodium symptoms
Low sodium symptoms Dynamic risk factors
Dynamic risk factors Anaphylactic shock risk factors
Anaphylactic shock risk factors Central eight risk factors
Central eight risk factors What are examples of risk factors?
What are examples of risk factors? Dynamic risk factors
Dynamic risk factors Macrosomia
Macrosomia Central eight risk factors
Central eight risk factors Stratum basale
Stratum basale 135 meq/l
135 meq/l Rules of halves in hypertension
Rules of halves in hypertension Hiv risk factors
Hiv risk factors