Trauma initial assessement and management Pawe Grala Klinika


- Slides: 22
Trauma – initial assessement and management. Paweł Grala Klinika Chirurgii Urazowej, Leczenia Oparzeń, Chirurgii Plastycznej AM w Poznaniu Kierownik Kliniki: Prof. dr hab. med. Krzysztof Słowiński
“Trauma” - expression comprising a spectrum of severity of mechanical violation of tissues, from a little scratch to a multiply injured patient. - also surgical intervention.
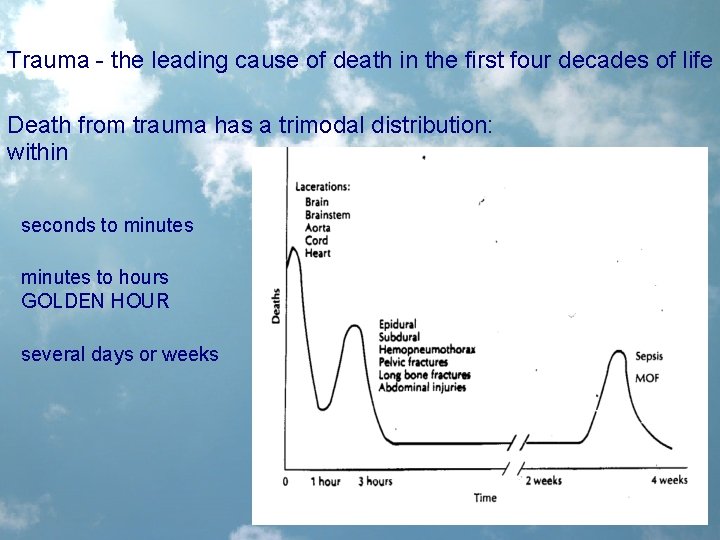
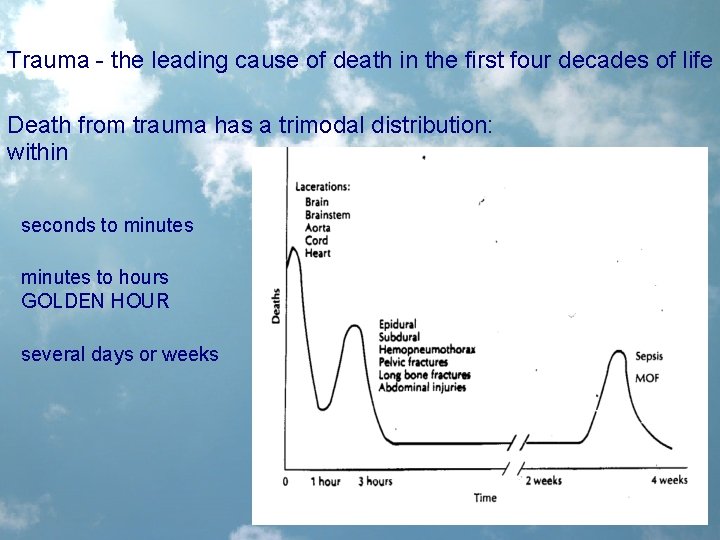
Trauma - the leading cause of death in the first four decades of life Death from trauma has a trimodal distribution: within seconds to minutes to hours GOLDEN HOUR several days or weeks
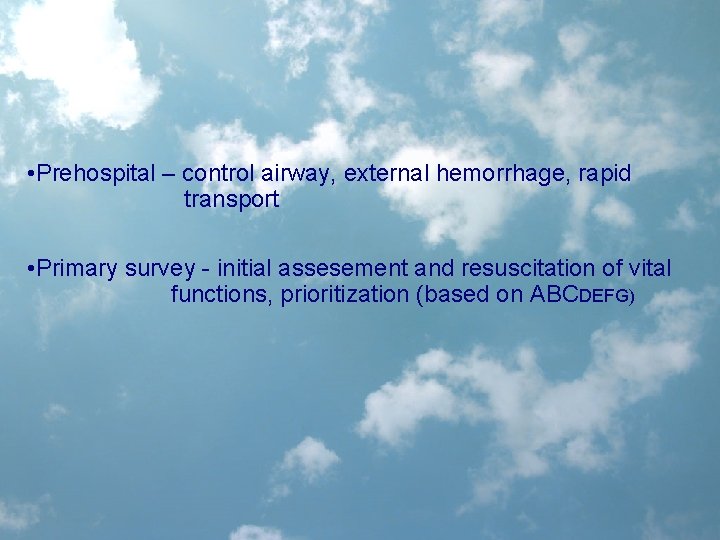
• Prehospital – control airway, external hemorrhage, rapid transport • Primary survey - initial assesement and resuscitation of vital functions, prioritization (based on ABCDEFG)
An organized consistent approach to the trauma patient optimal outcome. The Advanced Trauma Life Support (ATLS) adopted by the American College of Surgeons in 1979. The primary focus of ATLS is on the first hour of trauma management - rapid assessment and resuscitation THE GOLDEN HOUR
The primary survey – life threatening conditions are identified and management is begun simultaneously! • A - Airway maintenance with cervical spine control • B - Breathing and ventilation • C - Circulation with hemorrhage control • D - Disability: neurological status • E - Exposure: completely undress the patient
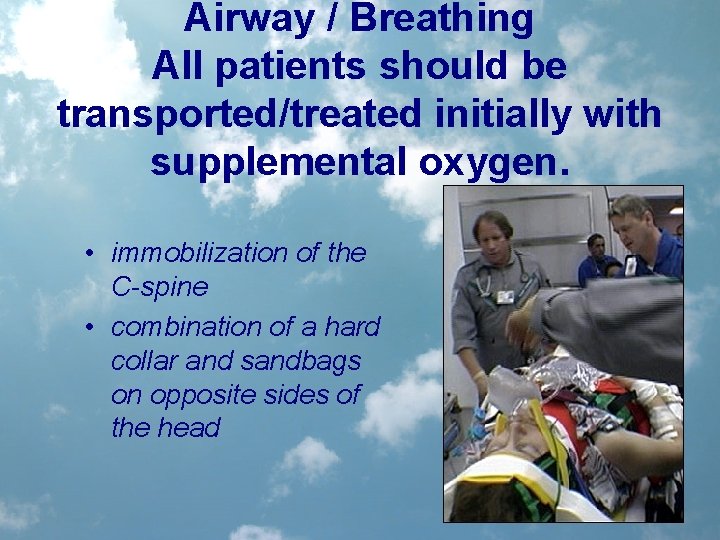
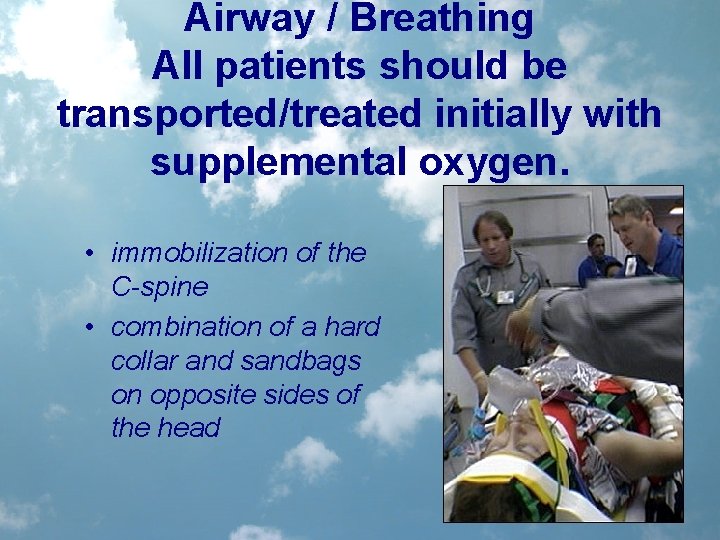
Airway / Breathing All patients should be transported/treated initially with supplemental oxygen. • immobilization of the C-spine • combination of a hard collar and sandbags on opposite sides of the head
Airway / Breathing • establishing verbal contact with the patient clear phonation by the patient establishes that the airway is patent. • further intervention depends on: - neurologic stability - adequacy of gas exchange and the potential for airway compromise
Neurological Stability • decreased level of consciousness is considered to be intracranial pathology until proven otherwise (drugs, alkohol) • brief neuro exam (done during the primary survey): A - Alert V - responds to Verbal stimuli P - responds to Painful stimuli U - Unresponsive • Glasgow Coma Scale (GCS): GCS < 8 requires definite airway intervention to prevent aspiration pneumonitis, to insure adequate oxygen delivery and to avoid hypercarbia. If a patient is responding only to painful stimuli or is unresponsive/unconscious, the GCS is or has a high likelihood of being less than 8.
Adequacy of Gas Exchange • airway patency does not insure adequate ventilation LOOK • nature of the injury: maxillofacial trauma/airway burns - potential for airway compromise, obvious airway or chest trauma (sucking chest wounds, flail segments), cyanosis • tachypnea, use of accessory muscles of respiration or evidence of tracheal shift
Adequacy of Gas Exchange • • LISTEN stridor upper airway compromise. hyperresonance to percussion/lack of air entry pneumothorax dullness to percussion/lack of air entry hemothorax. bowel sounds in the chest ruptured diaphragm.
Adequacy of Gas Exchange FEEL • hand over the mouth - feel for air exchange. • Insertion of a finger - sweep to clear the mouth of any foreign bodies (especially dislodged teeth) and to evaluate for evidence of maxillofacial trauma. LAB • pulse oximetry - haemoglobin saturation; immediate feedback pitfalls - motion, peripheral vasoconstriction, carboxy/methaemoglobinemia. • ABG`s - more complete picture of the patient; feedback on oxygenation, ventilation and tissue perfusion pitfalls - a defined waiting period (institution dependent). .
Securing the Airway - endotracheal intubation (inspection of th airway, suction of blood and secretions, bag mask ventillation) - possible spinal cord or direct traumatic tracheal injuries surgical airway - translaryngeal intubation • Immediate - apnea • Emergent - hypoventilation, significant head injury, cyanosis • Urgent - burns, maxillofacial injury and cervical hematomas will likely require a secure airway to prevent upper airway obstruction; chest wall and pulmonary injuries are usually initially well compensated but may eventually require mechanical ventilation there is often time for a history, appropriate physical exam and cervical radiographs
Securing the Airway Blind nasotracheal intubation vs direct orotracheal intubation Determined by the experience of the physician Blind nasotracheal intubation: requires a spontaneously breathing unconscious or cooperative conscious patient, unacceptable failure rate (35%) - requires 3. 7 vs. 1. 3 oral attempts, contraindicated if basal skull or midface fracture. can precipitate epistaxis (may interfere with subsequent alternative attempts at intubation if unsuccessful). high incidence of sinusitis if a tube is left in place greater than 72 hours.

Assume the cervical spine to be unstable until proven otherwise • up to 50% of patients sustaining C-spine trauma develop neurologic abnormalities (nerve root compression and weakness to quadri- plegia and death). • 10% of patients with C-spine injury are initially neurologically intact, but develop deficits during the course of emergency care • risks of airway management
C-spine evaluation • bone and soft tissue • X-ray exam: „one view is no view”, L-all 7 C+Th 1 (30% inj. C 7 Th 1), AP-vertical alignment of the spinous and articular process and abnormalities in joint and disc spaces, open mouth view integrity of the atlanto-occipital and atlanto-axial joints, the odontoid process, oblique – intervert. foramina • CT • lateral cervical spine - sensitivity of about 85% 92% in a three view series 100% when selective CT scanning is employed

Circulation • BP • HR Alghevar scheme - quantification of shock: SBP / HR >1 no or minor clinical symptoms <1 major shock • Pulses • Indirect signs: UA, skin, tachypnoe, altered consciousness, „empty” periferal veins Large bore IV lines
Circulation • warmed intravenous infusions Control: • external hemorrhage • internal hemorrhage: MAST (PASG) suit Pelvic binders Surgery stabilisation secondary survey
Initial assessement • • • Chest and abd. PE Orthopaedic PE Periferial Neurologic PE Labs X-rays, US, CT
tertiary trauma survey • ACS definition - a patient evaluation that identifies and catalogues all injuries after the initial resuscitation and operative intervention • 2 - 50% of combined life threatening and non-life threatening injuries are missed during primary and secondary surveys • timing is institution specific (typically occurs within 24 h after admission and is repeated when the patient is awake, responsive, and able to communicate any complaints). • is a comprehensive review of the medical record with emphasis on the mechanism of injury and pertinent comorbid factors such as age, includes the repetition of the primary and secondary surveys, a review of all laboratory data, and a review of radiographic studies with an attending radiologist
 Kim był święty piotr
Kim był święty piotr Dr paweł grala
Dr paweł grala Grala transport
Grala transport Jolanta grala-michalak
Jolanta grala-michalak Klinikaxp
Klinikaxp Neurológiai klinika szeged
Neurológiai klinika szeged Zan mitrev klinika
Zan mitrev klinika Neurologická klinika nitra
Neurologická klinika nitra Lowestoft polska klinika
Lowestoft polska klinika Veterinārā klīnika liepājā
Veterinārā klīnika liepājā Semmelweis egyetem konzerváló fogászati klinika budapest
Semmelweis egyetem konzerváló fogászati klinika budapest Semmelweis egyetem szemészeti klinika budapest
Semmelweis egyetem szemészeti klinika budapest Acromion klinika
Acromion klinika Szeged klinika mri vizsgálat
Szeged klinika mri vizsgálat Laringotraheobronhitis
Laringotraheobronhitis Dominika szalewska
Dominika szalewska Klinika za psihijatriju beograd
Klinika za psihijatriju beograd Klinika prawa definicja
Klinika prawa definicja Mia klinika
Mia klinika Klinika za rehabilitaciju dr miroslav zotović
Klinika za rehabilitaciju dr miroslav zotović Multimed
Multimed Digestivna hirurgija skopje
Digestivna hirurgija skopje Thm klinika
Thm klinika