Too Well Too Sick or Just Right for




- Slides: 58
“Too Well, Too Sick, or Just Right” for Advanced Heart Failure Therapies Todd D. Edwards MD FACC FACP FASNC

Too Sick Too Well Just Right Cardiologist Looking for Mr. /Mrs. Right
Disclosures I have nothing to disclose (unfortunately)
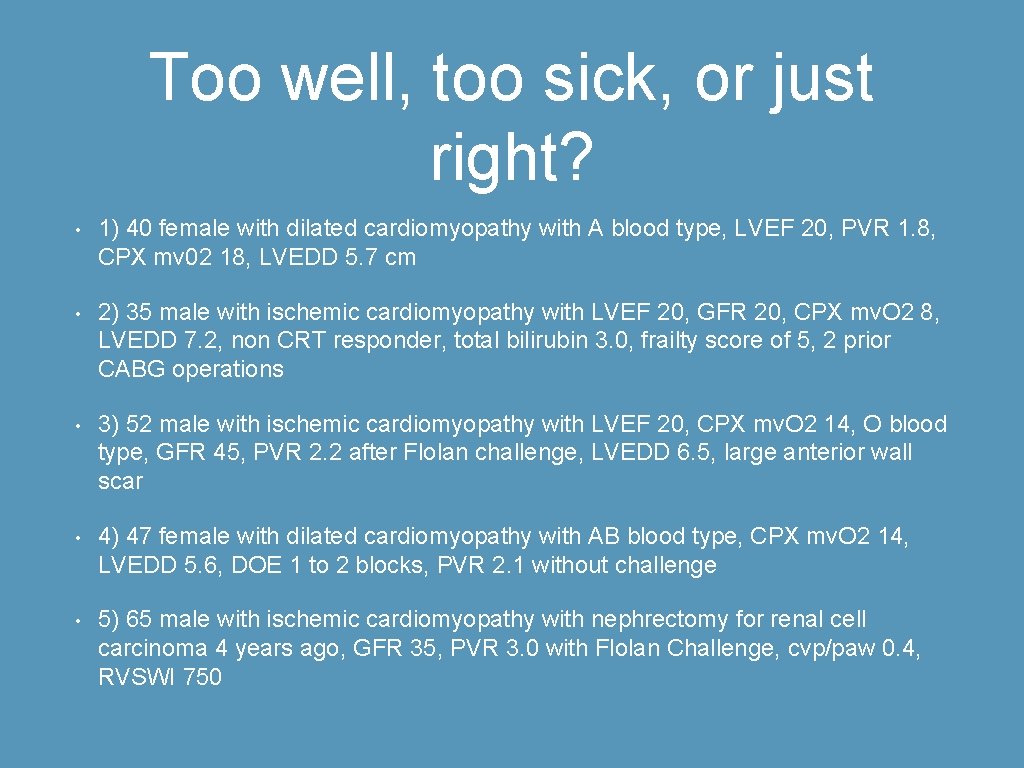
Too well, too sick, or just right? • 1) 40 female with dilated cardiomyopathy with A blood type, LVEF 20, PVR 1. 8, CPX mv 02 18, LVEDD 5. 7 cm • 2) 35 male with ischemic cardiomyopathy with LVEF 20, GFR 20, CPX mv. O 2 8, LVEDD 7. 2, non CRT responder, total bilirubin 3. 0, frailty score of 5, 2 prior CABG operations • 3) 52 male with ischemic cardiomyopathy with LVEF 20, CPX mv. O 2 14, O blood type, GFR 45, PVR 2. 2 after Flolan challenge, LVEDD 6. 5, large anterior wall scar • 4) 47 female with dilated cardiomyopathy with AB blood type, CPX mv. O 2 14, LVEDD 5. 6, DOE 1 to 2 blocks, PVR 2. 1 without challenge • 5) 65 male with ischemic cardiomyopathy with nephrectomy for renal cell carcinoma 4 years ago, GFR 35, PVR 3. 0 with Flolan Challenge, cvp/paw 0. 4, RVSWI 750
Assumptions 1) This presentation predominantly focused on systolic CHF with LVEF less than or equal to 25%
Assumptions 2. In this subset , I assume that patients are already treated with: A. Ace inhibitors and if intolerant an ARB B. Beta blockers (carvedilol/metoprolol/bisoprolol) C. appropriate diuretics to control congestive symptoms D. Aldosterone antagonists (spironolactone/eplerenone) with Class II to IV symptoms
Assumptions E. Nitrates/Hydralazine for patient intolerant of ACE and ARB’s and for African Americans with continued Class II to IV symptoms despite the above standard therapy F. Typical heart failure therapy required for elective advance heart therapies for 45 of the preceding 60 days or IABP for 7 days
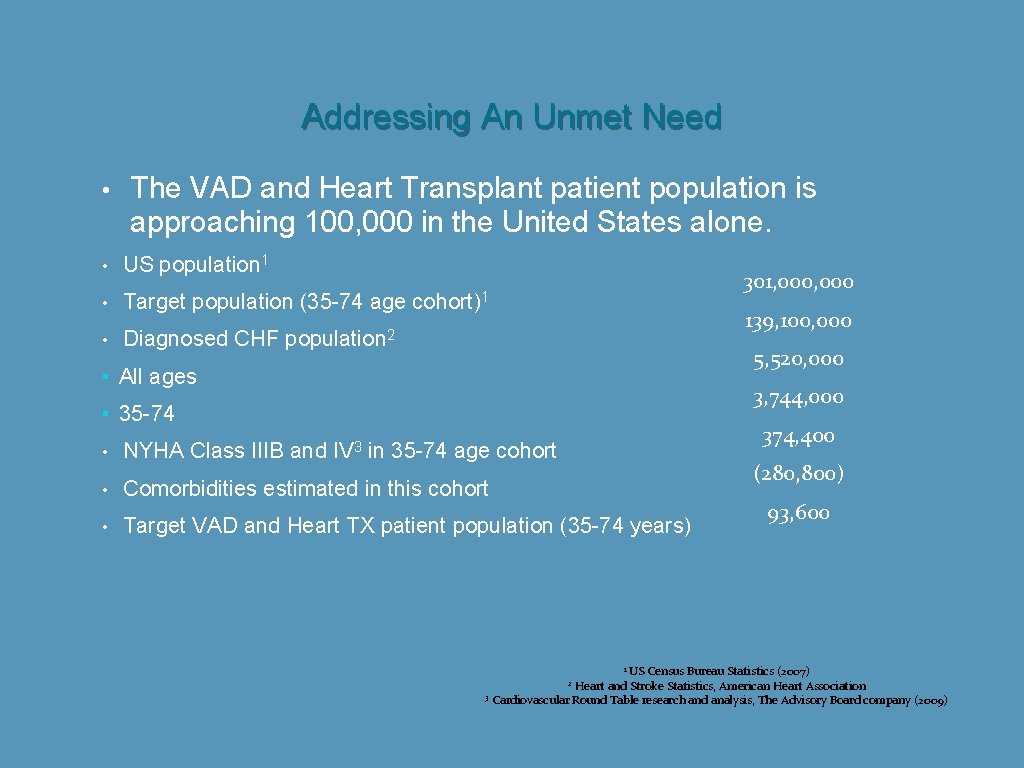
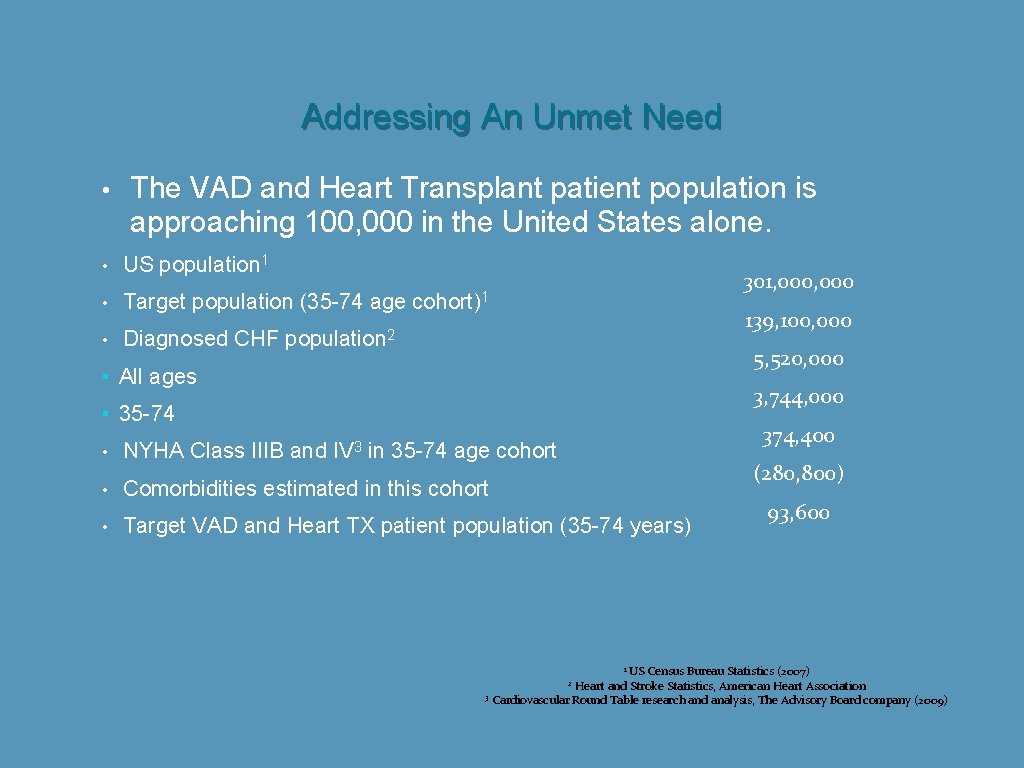
Addressing An Unmet Need • • The VAD and Heart Transplant patient population is approaching 100, 000 in the United States alone. US population 1 Target population (35 -74 age Diagnosed CHF 301, 000 cohort)1 139, 100, 000 population 2 5, 520, 000 ▪ All ages 3, 744, 000 ▪ 35 -74 IV 3 374, 400 • NYHA Class IIIB and in 35 -74 age cohort • Comorbidities estimated in this cohort • Target VAD and Heart TX patient population (35 -74 years) (280, 800) 93, 600 US Census Bureau Statistics (2007) Heart and Stroke Statistics, American Heart Association 3 Cardiovascular Round Table research and analysis, The Advisory Board company (2009) 1 2
Physical Exam The most prognostic findings are A. JVP B. S 3 gallop
• JVP and a S 3 gallop in SOLVD (Drazner et al, NEJM 2001) proved to be the most prognostic signs for death and CHF hospitalization (RR 1. 30 for JVP and RR 1. 22 for S 3)
Physical Exam Far less helpful signs include A. rales (very specific for PAW over 18 if present but not sensitive for PAW over 18 with one study showing only 9 of 37 (24%) having rales with known PAW over 18 at RHC B. peripheral edema (not specific for CHF with many other possible diagnoses)
Imaging A. CXR can be very characteristic but also can be nondiagnostic—Intersititial edema has a sensitivity of 60%/specificity of 73%/PPV 78%/NPV 53% for elevated PAW B. ECHO is the most information dense test we have and is essential to classify CHF C. If severe systolic CHF present with LVEF less than 25%, cardiac catheterization to assess coronary anatomy is preferred to stress imaging which can be falsely negative or falsely positive in this population.
Lab 1. BNP helps to separate CHF patients from other causes of dyspnea but can be elevated in other cardiac conditions (afib /pulmonary hypertension) High BNP levels do not prove a diagnosis of acute heart failure. BNP elevation suggests CHF when pretest probability likely. A low BNP suggests alternative diagnoses. The BNP decreases with increasing BMI and decreases with obesity. 2. GFR is a sign of both venous congestion and inadequate cardiac output. One needs to look at “minor changes”. There is an increased 1. 5 relative risk of pump failure when comparing patients with Cr less than 1. 5 versus Cr 1. 5 to 2. 0 in multivariate analysis. 3. Total billirubin is marker for hepatic congestion (MELD score and modified MELD score for those on Warfarin) MELD score can be done with calculator app with age, creatinine, bilirubin, INR, and yes/no concerning HD twice in past week. Modified MELD substitutes albumin value for INR on those taking Warfarin.
Lab • Sodium-increase risk of mortality with levels less than 135 and greater than 145 (Optimize HF registry) • Hematocrit-increase risk of mortality with levels less than 12. 8 and greater than 15. 8
EKG • Assess cardiac rhythm and conduction • Detect LVH • Evaluate QRS duration for candidates for biventricular pacing/resynchronization • Detect evidence of myocardial ischemia
Severity Assessment Although many scoring models exist (Forrester HF class, Framingham CHF criteria, Killip Class, Stevenson HF class, and Valiant HF risk score), 4 scoring models are used in advance CHF 1. NYHA Functional CLASS 2. Seattle Heart Failure Model 3. Heart Failure Survival Score
Severity Assessment 4. INTERMACS Class
NYHA Functional Class I no limitation with activity Class II mild limitation of activity Class III marked limitation of activity Class IV rest symptoms or with minimal activity
Seattle Heart Failure Model Can be done quickly with computer model algorithm on largely well known and easily retrieved data. Caveats for use are that SHFM tends to underestimate risk/overestimate survival and based on an outpatient broad (less sick) population. SHFM incorporates treatment data in contrast to HFSS
Seattle Heart Failure Model Variables required for score include age, LVEF, SBP, weight, gender, NYHA Class, etiology, diuretic type and dose, allopurinol use, statin use, ACE use, beta blocker use, ARB use, K sparing diuretic, devices, sodium level, total cholesterol, hemoglobin, lymphocytes, and uric acid. Uric acid is felt to be a sign of oxidative stress.
Seattle Heart Failure Model This calculation yields an anticipated 1 year, 2 year, and 5 year survival. Calculation with the proper app take less than 2 minutes.
Heart Failure Survival Score This score developed for more sick patients with Class III and IV CHF to help with transplant listing but only has 7 variables to plug into an online risk calculator. Caveats are that this score tends to overestimate risk and requires a MVO 2 from a CPX treadmill
Heart Failure Survival Score The variables include presence/absence of CAD, resting heart rate, LVEF, mean arterial BP, presence absence of IVCD on EKG, serum sodium, and peak VO 2
Heart Failure Survival Score The calculation give you a result of risk in three groups 1. low risk HFSS greater than 8. 10 (88% 1 yr survival) 2. Moderate risk HFSS 7. 20 to 8. 09 (60% 1 yr survival) 3. High risk HFSS less then 7. 20 (35% 1 yr survival)
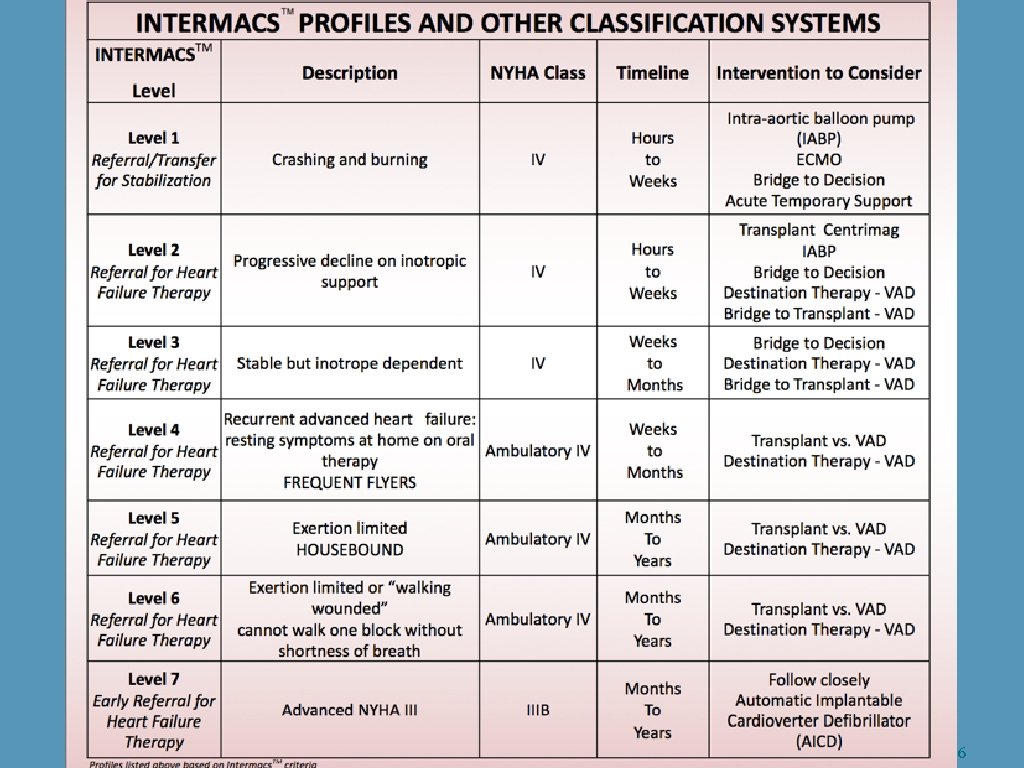
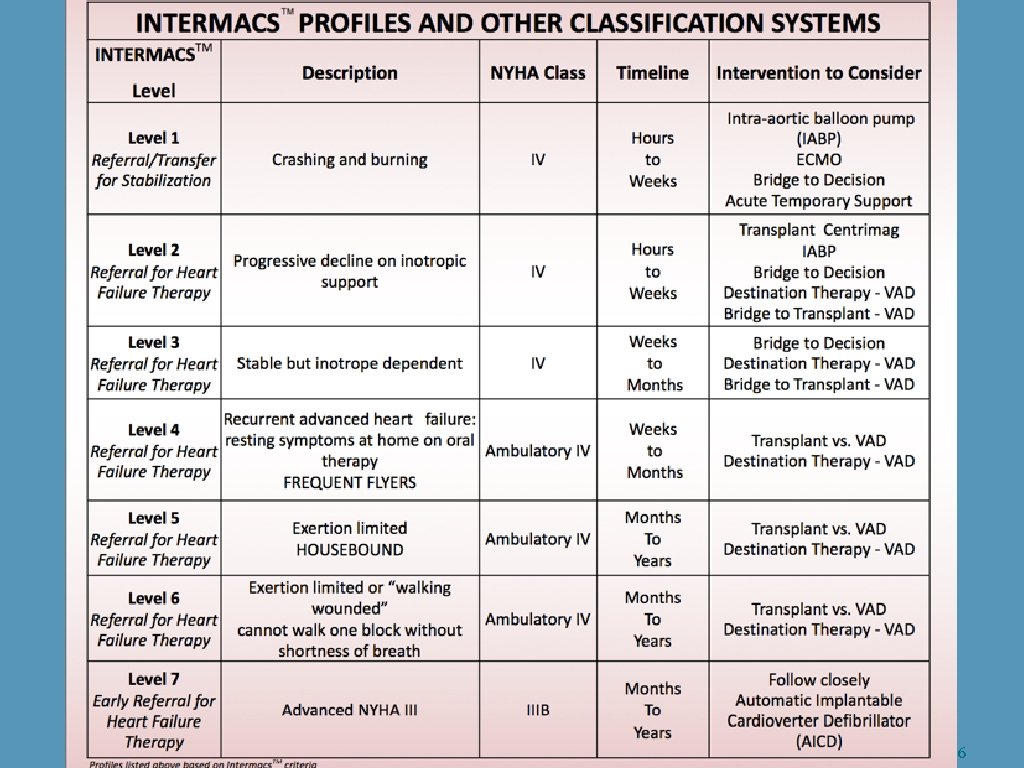
Intermacs Profiles • Seven different profiles developed to allow optimal selection of patients for medical/pacing therapies, transplant and MCS (Stevenson et al, ISHLT 2009) • Intermacs profiles are divided into 3 Class IV profiles, 3 ambulatory Class IV profiles and 1 advanced Class III categories.
6
Assessment of the Advanced Heart Failure Patient 1. Are they sick enough to benefit? 2. How far along are they in their disease? 3. Do we have time to wait or do they need workup now? 4. What are the non cardiac issues? 5. Do they have adequate social, psychologic and financial support?
Assessment of the Advance Heart Failure Patient 6. Are the “well enough” not to die?
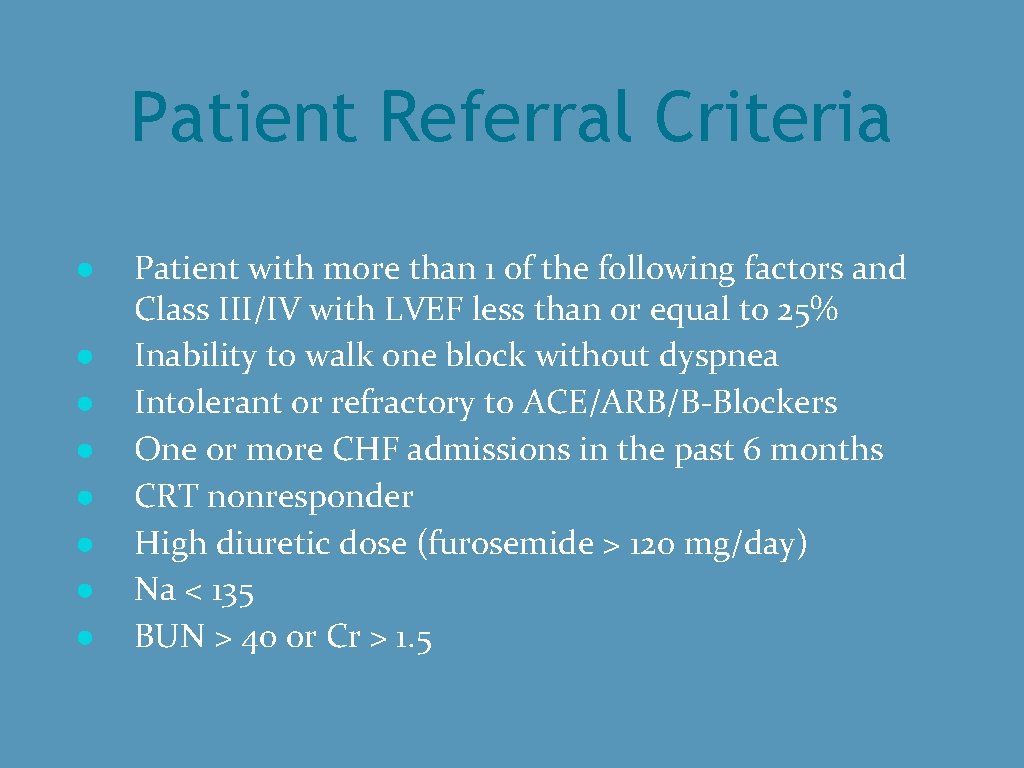
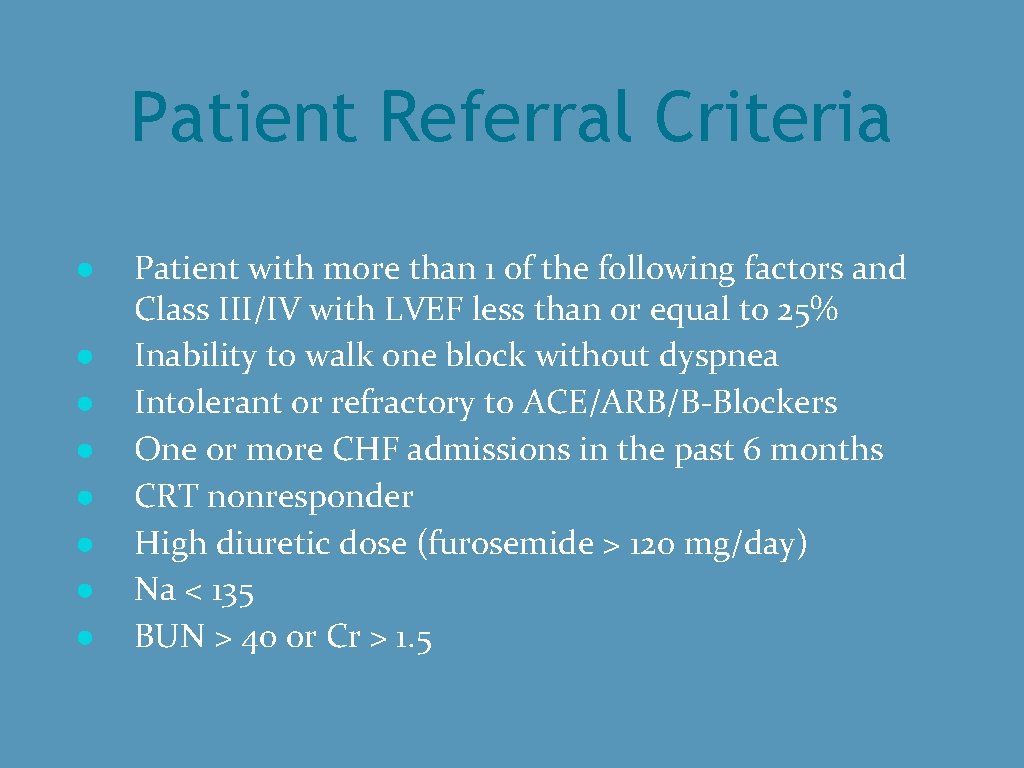
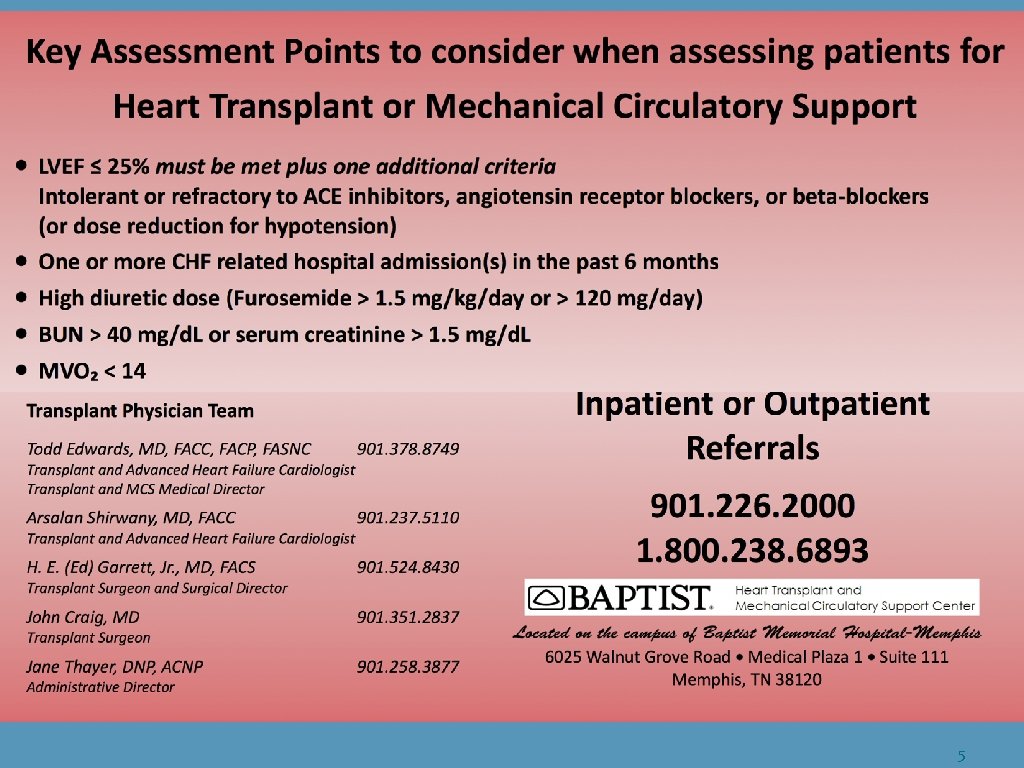
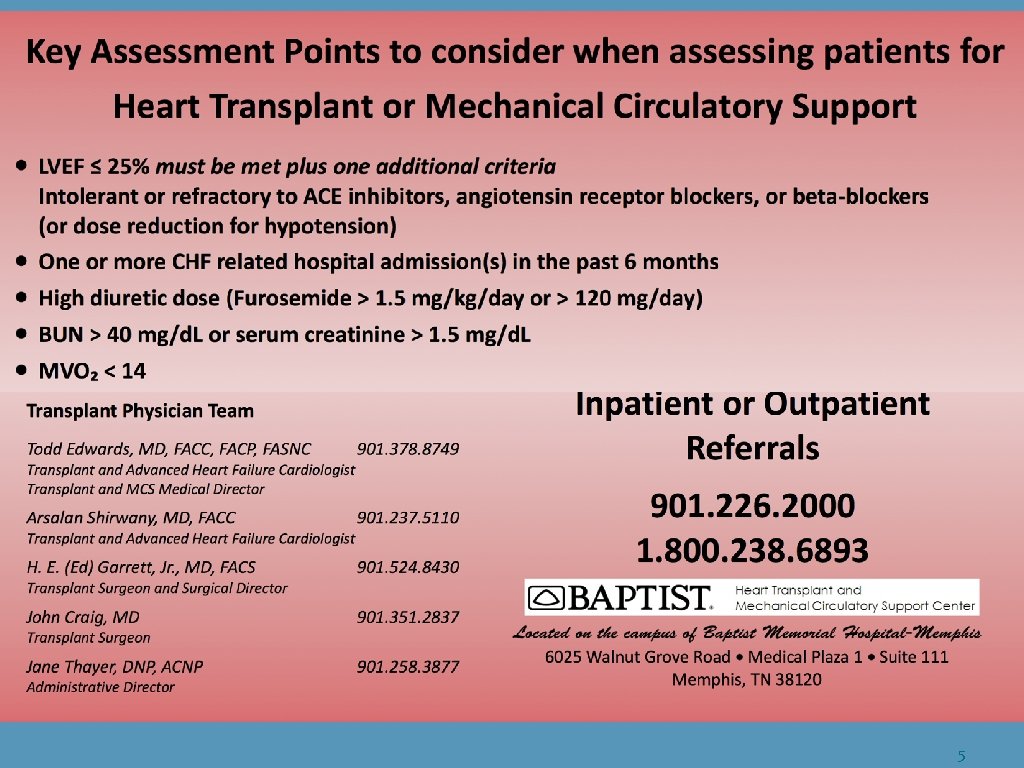
Patient Referral Criteria ● ● ● ● Patient with more than 1 of the following factors and Class III/IV with LVEF less than or equal to 25% Inability to walk one block without dyspnea Intolerant or refractory to ACE/ARB/B-Blockers One or more CHF admissions in the past 6 months CRT nonresponder High diuretic dose (furosemide > 120 mg/day) Na < 135 BUN > 40 or Cr > 1. 5
5
Starting Points 1. ABO blood type/body size 2. Recent ECHO 3. CPX treadmill 4. Right heart catheterization (addition of left heart cath if not recently done)
ABO blood type and body size • Since O blood type is the universal donor, finding hearts for O blood type is the most difficult. AB recipients are the easiest to find donors as the universal recipient and are among the few that can be transplanted from home as Status 2. • Donors should be roughy no more than 20% over ideal body weight and no less then 40% under the ideal body weight of the recipient. • Therefore, the “big O recipient ” is the most difficult to transplant and often use LVAD as bridge to transplant
ECHO • 2 D and Doppler/Color flow is the single most useful test in the evaluation of heart failure • In addition to a full exam, attention to LV dilatation is important. Those patients with larger LV’s have increased wall tension (Law of Laplace) and more likely to “fall” off the Frank Starling Curve. The LV compensation of dilatation is deleterious.

LV dilatation • LV wall stress =LV pressure X radius divided by 2 x LV wall thickness • French astronomer and mathematician Pierre Simone Laplace

LV dilatation Law of Laplace • Increase wall stress and neurohormonal activation drive the remodeling process favoring LV dilatation and deterioration in function until a new equilibrium is reached between forces exerted by the extracellular matrix and distending forces that promote LV dilatation
CPX • CPX gives objective determination of functional capacity impairment • For systolic CHF patients, the key variables are work effort, maximal oxygen capacity, and ventilatory equivalent for CO 2 • Work effort grouped as maximal, submaximal, and poor. 1)maximal (RER greater than 1. 1 WR max) 2) submaximal (RER less than 1. 1 and greater than 0. 9 WR max. ) 3) poor (RER less than 0. 9 WRmax)
CPX • Respiratory exchange ratio (RER) —-related to but not equivalent to its cellular counterpart, the respiratory quotient, and is defined as the ratio of CO 2 to O 2 • Maximal oxygen capacity (Vo 2 max)—value achieved with O 2 remains stable despite a progressive increase in the intensity of exercise —synonymous with peak aerobic capacity. The anaerobic threshold is the highest oxygen uptake without a sustained incase in blood lactate concentration and lactate/pyruvate ratio
CPX • Ventilation/carbon dioxide production ratio (Ve/VCO 2 slope)-also known as the ventilatory equivalent for CO 2 and represents a respiratory control function that reflects chemoreceptor, sensitivity, acid-bace balance, and ventilatory efficiency
CPX • Assuming maximal effort, a MVO 2 less than 14 ml/kg/min will call for advance CHF therapies. A MVO 2 less than 10 ml/kg/min is a higher risk group. • A VE/VCO 2 slope over 30 has a decreased survival. In general, a VE/VCO 2 slope over 35 qualifies for advance CHF therapies. A VE/VCO 2 over 40 is high risk
CPX • Suggest CPX in those patients with LV dysfunction with a LVEF less or equal to 25% to be sure adequate treatment. If MVO 2 over 14 ml/kg/min and VE/VC 02 slope less than 35, it is proper to continue optimal pharmacologic therapy including the proper EP directed therapies for prevention of sudden death and biventricular pacing.
Right Heart Cath • Pulmonary hypertension—defined as mean PAP of 25 or greater—can be venous, arterial, or both • Transpulmonary gradient —PA mean minus the PAW mean. Normal TPG 10 or less. If TPG greater than 10, then at least some pulmonary arterial component • Pulmonary vascular resistance (PVR) —expressed in Wood units—acceptable is 2. 3 Wood units or less here—if TPG 10 or less, then accept up to 2. 7 Wood units.
Right Heart Cath • Can use IV Nipride, inhaled Flolan, IV Flolan, or IV adenosine for vasodilator challenge if initial PVR over these levels • RA pressure—-want less than 10 pre LVADincrease risk of venous hepatic and renal congestion • CVP/PAW ratio —want less than 0. 63—sign of significant RV dysfunction if higher than 0. 63
Right Heart Cath • RV stroke work index (RVSWI)—RV stroke volume (cardiac index in ml/heart rate) multiplied times the difference between the PA mean and RA mean. RVSWI greater than 600 suggests adequate RV 2) RVSWI greater than 900 suggests excellent RV 3) RVSWI less than 400 suggests failing RV and high risk for RV failure with LVAD alone.
Multidisciplinary approach to selection • cardiologist-symptoms, echo, cath data, cpx, • CV surgeon-operative risk, vascular issues • pulmonologist- operative risk for pulmonary complication • nephrologist- acceptable preop renal function • infectious disease -infectious risks • hematologist- anemia and hypercoagulability issues • Pharm. D- compliance with obtaining and taking med correctly
Multidisciplinary approach to selection • coordinators- risk score tabulations, survival statistics, compliance assessment • social worker- personal responsibility, family support, financial ability • psychologist-psychiatric disease, compliance assessment, educational level assessment • supportive care- expectations and life/death issues • dietician-obesity, diet, diabetes control • physical therapist-fraility, ability to rehab • financial administrator- insurance approval and ongoing coverage
Too well, too sick, or just right? • 1) 40 female with dilated cardiomyopathy with A blood type, LVEF 20, PVR 1. 8, CPX mv 02 18, LVEDD 5. 7 cm
Responses • 1) Too well • 2) Too sick • 3) Just right
Too well, too sick, or just right? • 2) 35 male with ischemic cardiomyopathy with LVEF 20, GFR 20, CPX mv. O 2 8, LVEDD 7. 2, non CRT responder, total bilirubin 3. 0, frailty score of 5, 2 prior CABG operations
Responses • 1) Too well • 2) Too sick • 3) Just right
Too well, too sick, or just right? • 3) 52 male with ischemic cardiomyopathy with LVEF 20, CPX mv. O 2 14, O blood type, GFR 45, PVR 2. 2 after Flolan challenge, LVEDD 6. 5, large anterior wall scar
Responses • 1) Too well • 2) Too sick • 3) Just right
Too well, too sick, or just right? • 4) 47 female with dilated cardiomyopathy with AB blood type, CPX mv. O 2 14, LVEDD 5. 6, DOE 1 to 2 blocks, PVR 2. 1 without challenge
Responses • 1) Too well • 2) Too sick • 3) Just right
Too well, too sick, or just right? • 5) 65 male with ischemic cardiomyopathy with nephrectomy for renal cell carcinoma 4 years ago, GFR 35, PVR 3. 0 with Flolan Challenge, cvp/paw 0. 4, RVSWI 750
Responses • 1) Too well • 2) Too sick • 3) Just right

I would like to thank my tech support.