Reproductive Health of Young Adults Contraception Pregnancy and


- Slides: 95
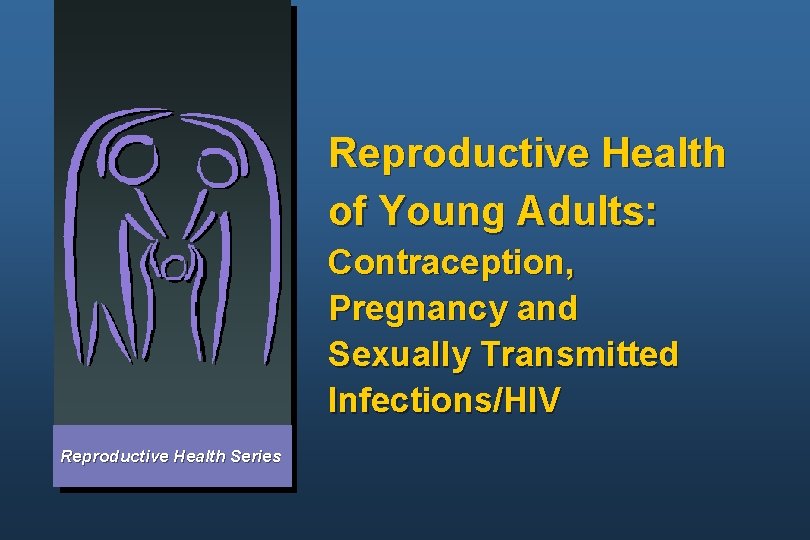
Reproductive Health of Young Adults: Contraception, Pregnancy and Sexually Transmitted Infections/HIV Reproductive Health Series
Reproductive Health Issues of Young Adults Topics to be covered l l l Why focus on young adults Defining young adults Characteristics of young adults Reproductive health risks and consequences STI/HIV risks and consequences
Why Focus on the Reproductive Health of Young Adults? More than 1 of every 4 persons worldwide is between ages 10 and 24 years
Youth Are Assets Youth are a great potential resource
Reproductive Health Risks and Consequences for Young Adults Risks: l Unintended and too-early pregnancy l STIs, including HIV/AIDS l Unsafe abortion Consequences: l Sexual violence l Medical and unwanted l Psychological sexual activity l Social l Economic
HIV/AIDS Risk for Youth About half of all new HIV infections are among youth l l l HIV/AIDS epidemic among youth remains largely invisible to adults Stopping HIV/AIDS requires working with youth in a comprehensive way Young women are several times more likely to get infected than young men Today’s young people are the AIDS generation
Transition from Childhood to Adulthood Involves physiological, psychological, cognitive, social and economic changes Universal process that varies by individual and culture
Defining Young Adults Terms used: adolescents, young people, young adults, teenagers, youth Age Range: 10 -24 years
Factors Affecting the Reproductive Health Needs of Young Adults l l l Age Marital status Gender norms l l l l Sexual activity School status Childbearing status Economic/social status Rural/urban Peer pressure Political/cultural
Married and Unmarried Youth Common Characteristics: l Biological l Need for accurate information Differences: l Access to services l Contraceptive needs
Gender Affects the Reproductive Health of Youth Gender involves roles and relationships that are determined by society and culture. Gender affects: l l l Expectations of sexual activity of boys and girls Views regarding responsibility for contraception Social consequences of pregnancy Degree of risk for HIV/AIDS infection Cultural acceptance of harmful behaviors and practices Client-provider interactions
Gender Affects HIV/AIDS, Other Risks l l Males have more ability to use a condom than females, for cultural reasons Culture accepts harmful behaviors and practices against females
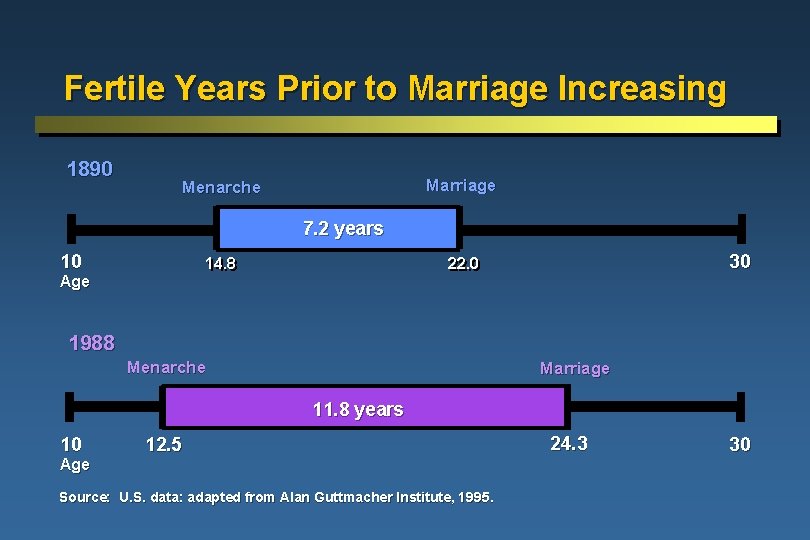
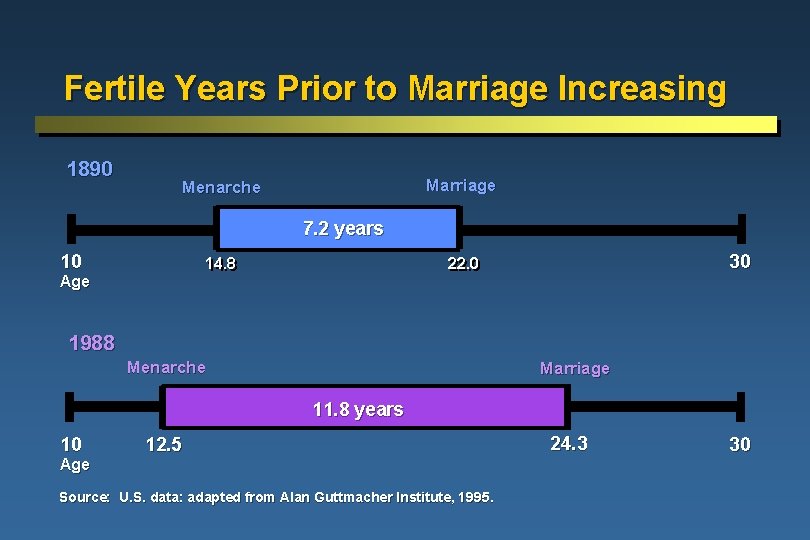
Fertile Years Prior to Marriage Increasing 1890 Marriage Menarche 7. 2 years 10 14. 8 Age 30 22. 0 1988 Menarche Marriage 11. 8 years 10 12. 5 Age Source: U. S. data: adapted from Alan Guttmacher Institute, 1995. 24. 3 30
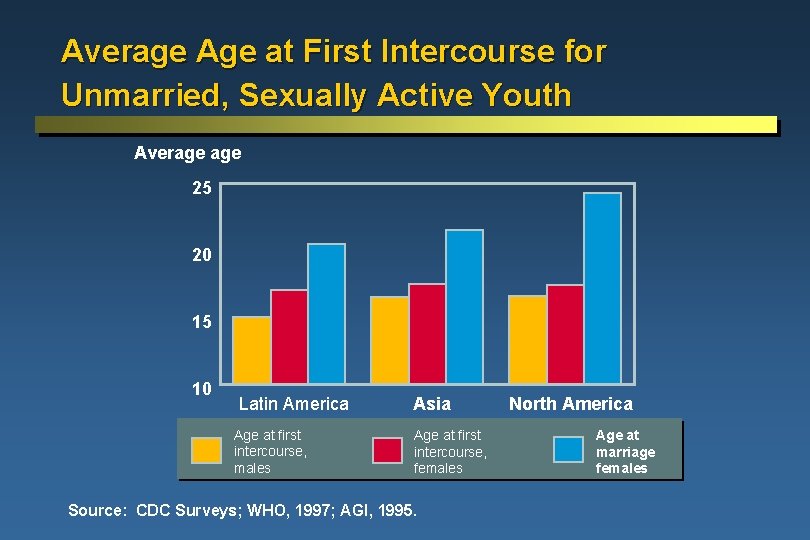
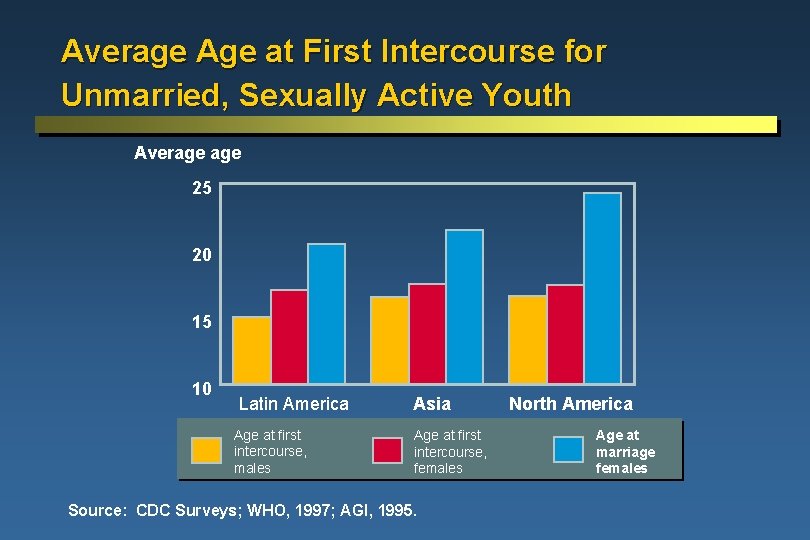
Average Age at First Intercourse for Unmarried, Sexually Active Youth Average 25 20 15 10 Latin America Age at first intercourse, males Asia Age at first intercourse, females Source: CDC Surveys; WHO, 1997; AGI, 1995. North America Age at marriage females
Young Adults and Contraceptive Use l l l Few married youth use contraceptives before first birth After becoming sexually active, unmarried youth delay use of contraceptives about a year Common reasons for non-use of contraceptives among unmarried youth: - did not expect to have sex - lacked information about contraception - lacked access to contraceptives
Limited Contraceptive Use: Characteristics of Youth l l l l Tend not to plan ahead or anticipate consequences Think they are not at risk Feel invulnerable Lack confidence or motivation to use Embarrassed or not assertive Lack power and skill to negotiate use Social or cultural expectations or beliefs
Limited Contraceptive Use: Barriers to Access Lack of access to services or methods: l Clinics not designed to be inviting to youth l Providers reluctant to serve unmarried youth l Laws/policy may prohibit provision to unmarried youth Youth may: l Lack transportation to clinic or money for contraceptives or services l Fear judgment or discovery l Be concerned about having pelvic exam
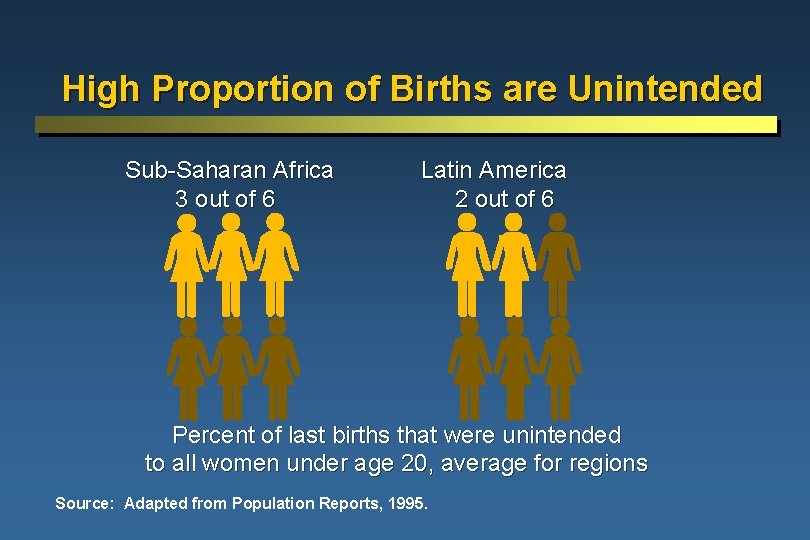
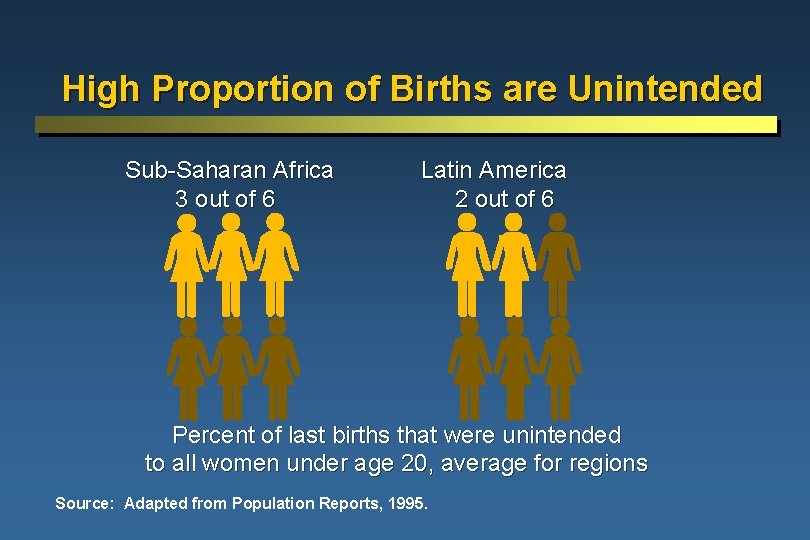
High Proportion of Births are Unintended Sub-Saharan Africa 3 out of 6 Latin America 2 out of 6 Percent of last births that were unintended to all women under age 20, average for regions Source: Adapted from Population Reports, 1995.
Psychological and Social Consequences of Pregnancy for Unmarried Youth l l l l Social stigmas for unmarried mothers and children Limited education Fewer career or job opportunities Heavy economic burden Depression, loss of self-confidence and lack of hope Consequences more severe for young women than men Children of young parents may face psychological, social and economic obstacles
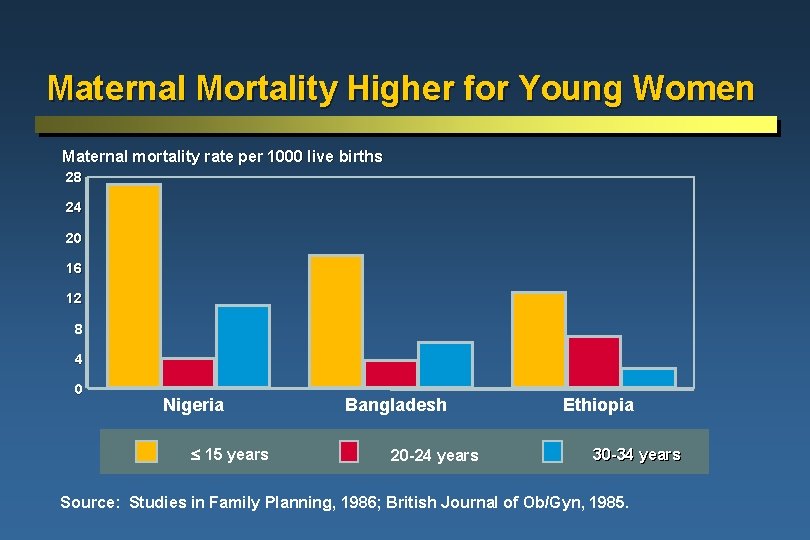
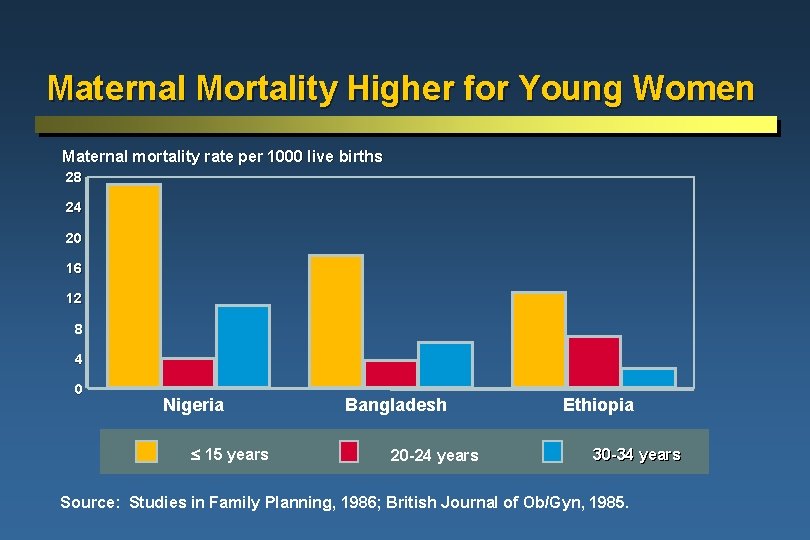
Maternal Mortality Higher for Young Women Maternal mortality rate per 1000 live births 28 24 20 16 12 8 4 0 Nigeria 15 years Bangladesh 20 -24 years Ethiopia 30 -34 years Source: Studies in Family Planning, 1986; British Journal of Ob/Gyn, 1985.
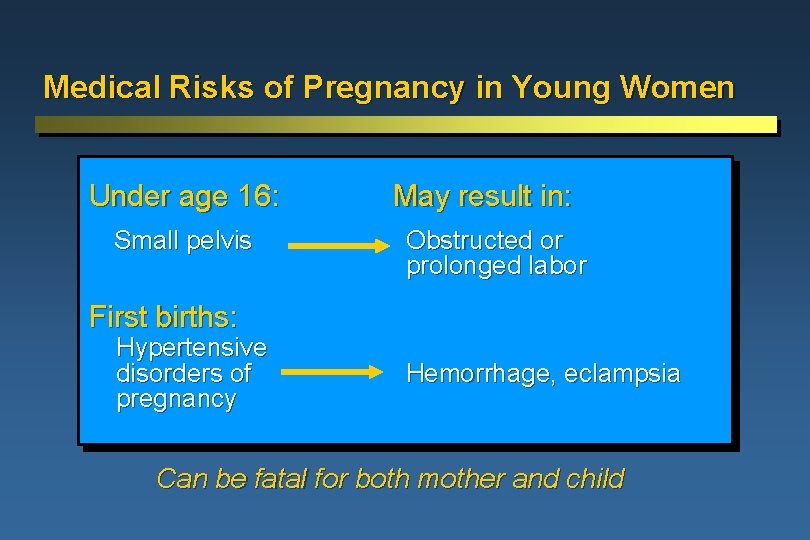
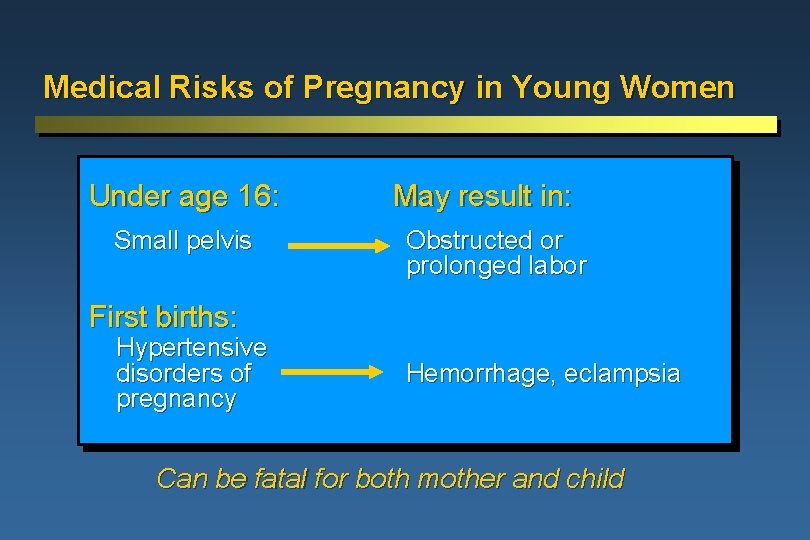
Medical Risks of Pregnancy in Young Women Under age 16: Small pelvis May result in: Obstructed or prolonged labor First births: Hypertensive disorders of pregnancy Hemorrhage, eclampsia Can be fatal for both mother and child
Maternity Care Prenatal Care: l To educate young women on proper pregnancy care and assess risk for complications Delivery: l To monitor for possible complications Prenatal and postpartum: l To provide information on contraception, breastfeeding, childcare skills and child health
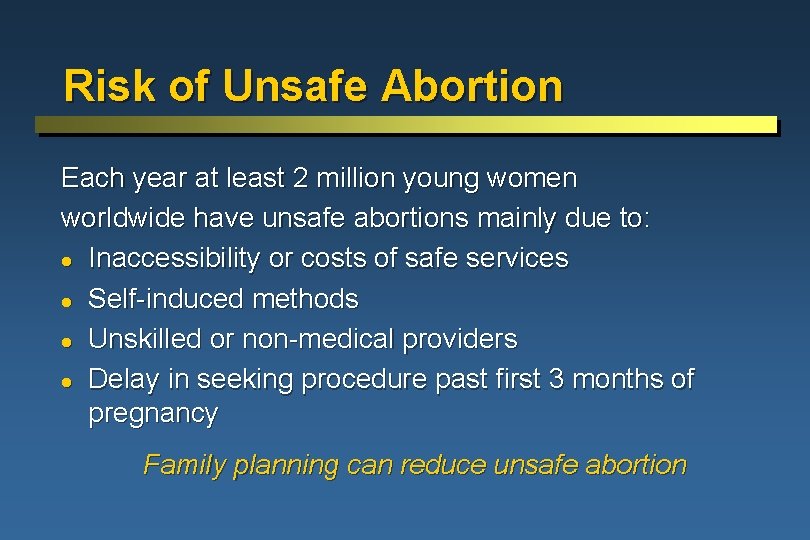
Risk of Unsafe Abortion Each year at least 2 million young women worldwide have unsafe abortions mainly due to: l Inaccessibility or costs of safe services l Self-induced methods l Unskilled or non-medical providers l Delay in seeking procedure past first 3 months of pregnancy Family planning can reduce unsafe abortion
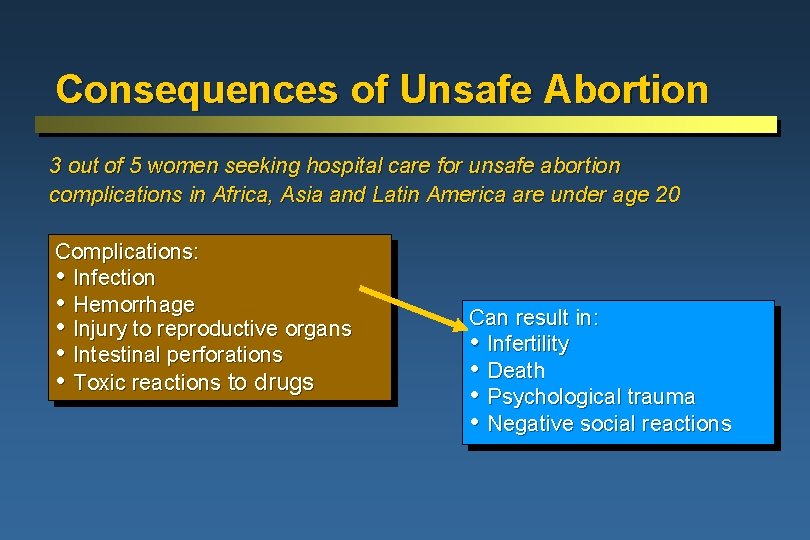
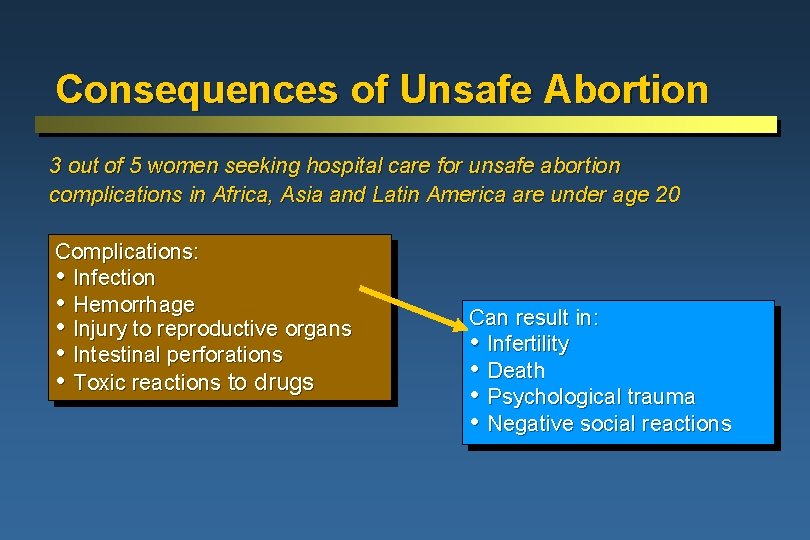
Consequences of Unsafe Abortion 3 out of 5 women seeking hospital care for unsafe abortion complications in Africa, Asia and Latin America are under age 20 Complications: • Infection • Hemorrhage • Injury to reproductive organs • Intestinal perforations • Toxic reactions to drugs Can result in: • Infertility • Death • Psychological trauma • Negative social reactions
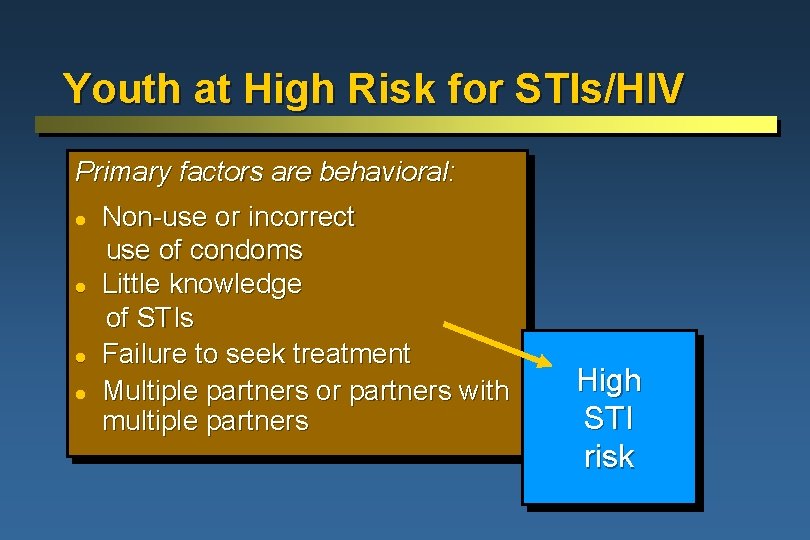
Youth at High Risk for STIs/HIV Primary factors are behavioral: l l Non-use or incorrect use of condoms Little knowledge of STIs Failure to seek treatment Multiple partners or partners with multiple partners High STI risk
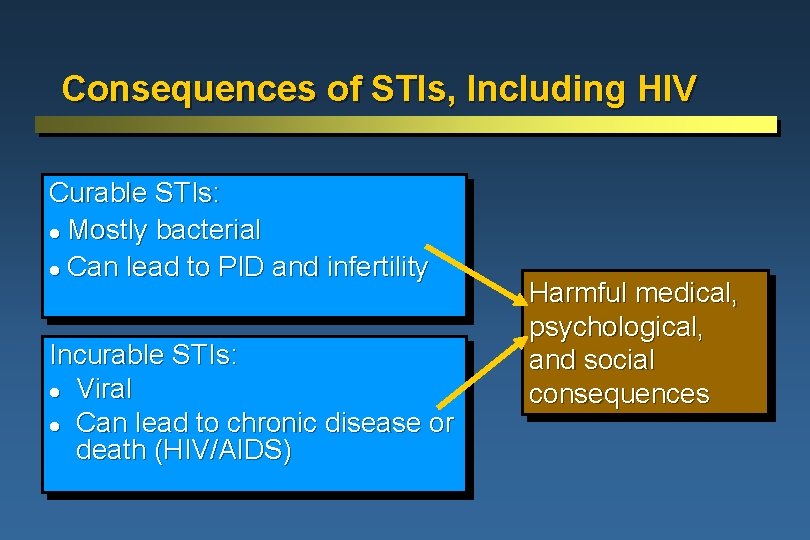
Consequences of STIs, Including HIV Curable STIs: l Mostly bacterial l Can lead to PID and infertility Incurable STIs: l Viral l Can lead to chronic disease or death (HIV/AIDS) Harmful medical, psychological, and social consequences
Risks and Consequences of Sexual Abuse Rape, sexual assault, involuntary prostitution can result in: l Physical injury l Unintended pregnancy l STIs l Psychological trauma l Increased likelihood of high-risk sexual behavior
Summary and Next Steps Young adults face high risks of pregnancy and STIs To address this: Young adults need information, skills, and access to services Policy-makers and providers need to know how and where to reach youth, and what contraceptive and STI/HIV services are needed
How to Reach Young Adults Topics to be covered l l l Who provides information and services to young adults l What reproductive health information is needed by is needed young adults by young adults Where services for young areadults best provided l Where services for adults young are best provided l
Youth Involvement Is Critical l Involve perspective of target audience l Work with youth, rather than for youth l Draw on youth’s energy, hope, eagerness to learn and resilience Youth “should be involved from the start as full partners…. ” ¾ World Health Organization, 2001
Who Provides Information and Services to Youth? Teachers To offer a range of services, various providers need to be involved Doctors Peer Educators Nurses Community Workers
Provider Attitudes Often Negative Toward Young Adults I wouldn't want mychild to get contraception. I don't want to talk about sexuality; it may encourage them. . . Anyone that age who is sexually active must be a bad person.
Sexuality: Open Discussions Are Important l l Difficult topic to discuss openly for both youth and adults Includes a wide range of issues, such as peer pressure, sexual identity, sexual orientation, sexual capability, sexual coercion Helps youth understand express their feelings Promotes responsible sexual behavior, helps prevent unintended pregnancy and STIs
Communication Skills Needed by Providers l l Reflective listening Open-ended questions Positive body language Characteristics that help communication: - sincerity, honesty, non-judgment, respect, sense of humor Confidentiality is critical in serving youth
Provider Training Needed l l l Technical knowledge Knowledge of issues facing young adults Gender awareness Counseling skills For some: how to train young people in communication skills
What Reproductive Health Information and Education Do Youth Need? Young adults need information and skills to be able to take responsibility for their sexuality. l Risks and consequences of sexual activity l Contraceptives and STIs l Sex education l Fertility issues for men and women l Gender issues Information and education should be age-specific
Research Shows Sex Education Helps Sex education: l Does not lead to earlier or increased sexual activity l Can give young people skills to delay sexual activity l Can increase contraceptive use It is important to begin sex education early Source: WHO, 1993.
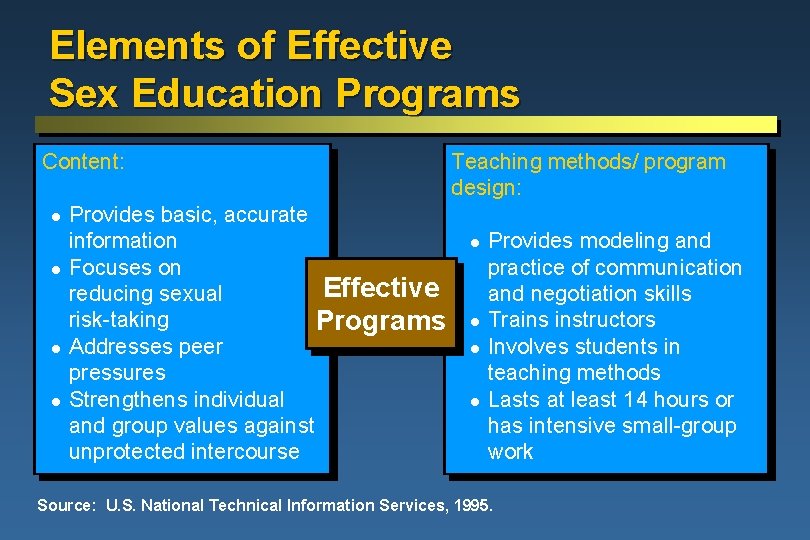
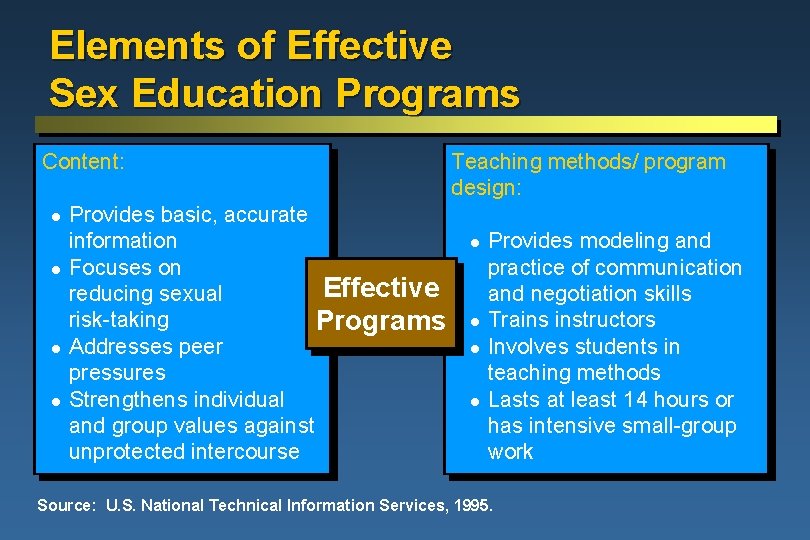
Elements of Effective Sex Education Programs Content: l l Provides basic, accurate information Focuses on Effective reducing sexual risk-taking Programs Addresses peer pressures Strengthens individual and group values against unprotected intercourse Teaching methods/ program design: l l Provides modeling and practice of communication and negotiation skills Trains instructors Involves students in teaching methods Lasts at least 14 hours or has intensive small-group work Source: U. S. National Technical Information Services, 1995.
Sexuality: What Youth Need to Know Includes issues of identity, societal roles, human relationships, biological development Youth need to learn: l How their bodies, minds and feelings are changing l How to communicate about sexuality l How to handle societal and peer pressures l How to make responsible decisions about sexual activity, including abstinence
Ways of Expressing Sexuality Young people need to know alternatives to risky sexual behavior l Holding hands l Hugging l Dry kissing l Body rubbing l Masturbation l Mutual masturbation l Sexual intercourse with a condom
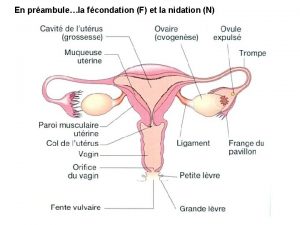
Fertility Awareness Involves education about: l The reproductive system l Fertility l The menstrual cycle l How pregnancy occurs l Attitudes and cultural norms about fertility, the use of contraception and childbearing Important for both males and females
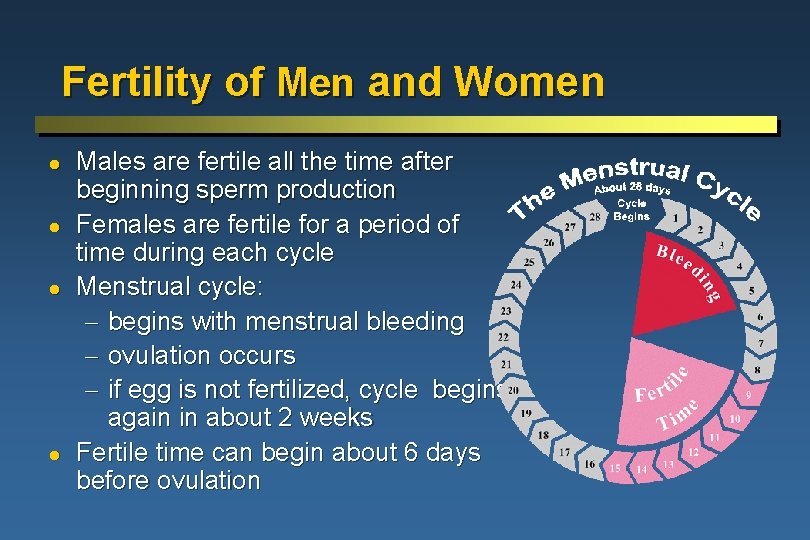
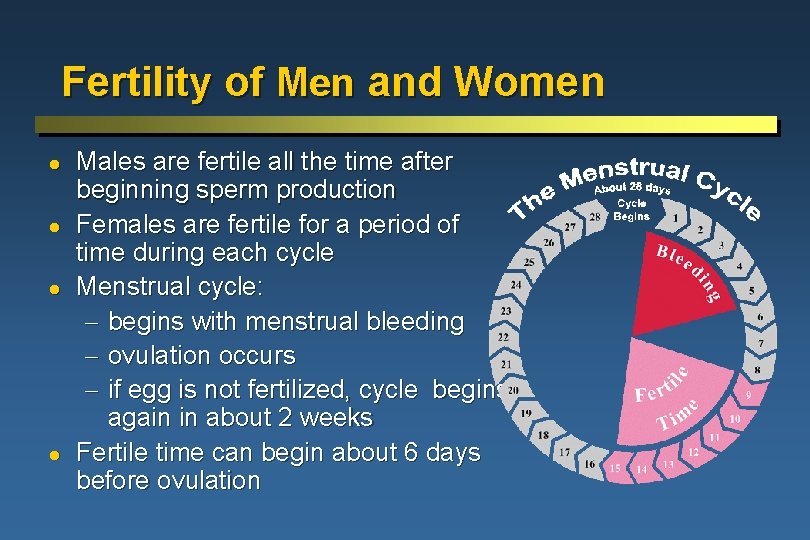
Fertility of Men and Women l l Males are fertile all the time after beginning sperm production Females are fertile for a period of time during each cycle Menstrual cycle: - begins with menstrual bleeding - ovulation occurs - if egg is not fertilized, cycle begins again in about 2 weeks Fertile time can begin about 6 days before ovulation
Gender Awareness for Youth Important to emphasize communication and shared responsibility between boys and girls
Where Can Information and Services for Youth Be Provided? l l l Home Health clinics School-based programs Community-based youth organizations Mass media
Effective Programs for Young Adults Identify target group, analyze assets and needs Incorporate evaluation Make services accessible, as identified by youth Involve youth Work with community, including family members Use materials designed by and for youth

Youth-Adult Partnerships Elements of good partnerships: l Organizational commitment and capacity l Attitude shifts among adults and youth l Selection, recruitment and retention of youth l Substantive levels of youth participation
Family Involvement l l Many youth want to talk to family members about sexuality Crucial elements: - availability of family members - attitudes and knowledge - communications skills Programs needed to help parents learn necessary skills and information Family members can support youth in seeking services and information
Health Clinics Designed for Youth l Separate units for youth l Outreach clinics with specially trained staff l Mobile clinics l Special hours l Convenient and safe locations l Youth-to-youth promotion l Low or no-cost services
Traditional Health Clinics: An Opportunity to Reach Youth l l Providers can take advantage of existing opportunities for providing information to young adults With every client, the provider should ask: “If you are sexually active, what are you doing to prevent pregnancy and STIs? ” l Referrals to other services and providers
Elements of School-Based Programs Large numbers of youth can be reached efficiently at schools l Family life education curricula l School-based or linked clinical services l Training of instructors and administrators l Involvement of families and community
Community-Based Youth Organizations l l Multi-service organizations: recreation, sports teams, vocational training, tutoring Workplace and religious groups: information and services Peer promoters or educators: information, counseling and condoms Youth centers for pregnant and parenting teens: continuing education and skills training
Mass Media and Other Creative Outreach l l l Mass media: radio, television, film, comic books Telephone hotlines Entertainment: drama groups, puppet shows, concerts Computer technology: Web sites, CD ROMS, distance learning Social marketing
Summary Lessons learned: l Sex education is valuable for young adults l Education needs to focus on skills and attitudes as well as information l Programs need to involve youth in the design l Forming effective youth-adult partnerships influences attitude changes
Contraceptive Options for Young Adults Topics to be covered l Contraceptive methods l Emergency contraception l Dual method use l Postpartum and postabortion contraception
Contraceptive Issues for Young Adults Non-medical issues: l High-risk behavior l Lack of accurate information l May not use methods consistently and correctly l Have unplanned and sporadic sexual activity l Lack of knowledge or access to emergency contraception
Complete Abstinence l l l Most effective way to prevent pregnancy and STIs No sexual intercourse May include other forms of sexual expression Option for all youth, including those who have begun sexual activity Requires high motivation, selfcontrol, communication and social support
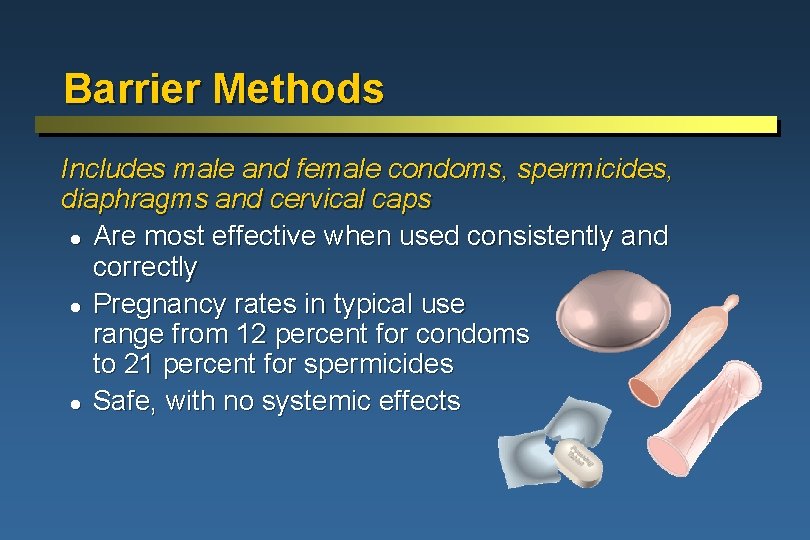
Barrier Methods Includes male and female condoms, spermicides, diaphragms and cervical caps l Are most effective when used consistently and correctly l Pregnancy rates in typical use range from 12 percent for condoms to 21 percent for spermicides l Safe, with no systemic effects
Barrier Methods: Advantages l l l Male condom is the most effective method for STI/HIV prevention Female condom is an alternative to male condom Most methods are accessible and available Good for infrequent sexual activity User-controlled Easily initiated and discontinued
Barrier Methods: Counseling Successful use requires: l Partner participation and negotiation skills l High level of motivation, self-confidence, self-control Key messages: l Always carry with you, so barrier methods are available when needed l Communication and shared responsibility are vital l Consistent and correct use are key to effectiveness
Male Condom l Use for pregnancy protection and if at risk for STIs l Use with other methods for STI protection l Incorporate into sexual activities l Use can result in delayed ejaculation
Male Condom: Use When using: l Open package carefully l Do not unroll before putting it on l Hold rim of condom during withdrawal l Use only water-based lubricants
Oral Contraceptives l l l l Very safe and effective when used consistently and correctly Many non-contraceptive health benefits Rapid return to fertility Use independent of sexual intercourse Can be used without partner’s knowledge Usually requires visit to clinic or other trained provider No STI protection
Oral Contraceptives: Counseling l l l Contraceptive benefit wears off quickly Pills must be taken daily Possible side effects include nausea or breakthrough bleeding Link pill-taking to a daily routine Encourage use of condoms for backup if pills not taken correctly or if at risk for STIs
Injectables and Implants l l l Very effective against pregnancy Non-contraceptive health benefits No daily action required or supplies needed at home Use independent of sexual intercourse and can be used without partner knowledge Require clinic visit No STI protection
Injectables and Implants: Counseling Progestin-only injectables and implants: l Bleeding irregularities likely l Return to fertility - delayed with injectables - immediate upon removal of implants l Use condoms if at risk for STIs Implants: l Appropriate for those wanting long-term method
Intrauterine Devices (IUDs) l l l Very effective at pregnancy prevention Use independent of intercourse Quick return to fertility Requires clinic visit for insertion and removal No STI protection
Intrauterine Devices (IUDs): Counseling Eligibility: l Not usually recommended for young women at increased risk for STIs l Not recommended for those with recent or current STIs l Under age 20 and nulliparous women may have increase risk of expulsion Counseling messages: l IUDs are not appropriate for those with high-risk behavior l Important to check for signs of expulsion
Lactational Amenorrhea Method (LAM) Temporary and effective method for breastfeeding women For LAM to be effective the woman must be: l Fully or nearly fully breastfeeding l Amenorrheic l Within the first six months postpartum LAM provides no protection against STIs
Traditional Methods Periodic abstinence and withdrawal: l Always available l Can promote reproductive health awareness l High pregnancy rates in typical use l No STI protection l Require considerable motivation l Periodic abstinence is difficult for young women with irregular menstrual cycles l Training about fertility awareness essential
Sterilization Generally not an appropriate method for young adults
Emergency Contraception l l l l Prevents pregnancy after unprotected intercourse Not meant to be a regular method After use, a regular method should be initiated or resumed Can be used at any time during cycle Does not protect against STIs Most effective when used early after unprotected intercourse Method options: - combined oral contraceptive pills - progestin-only contraceptive pills
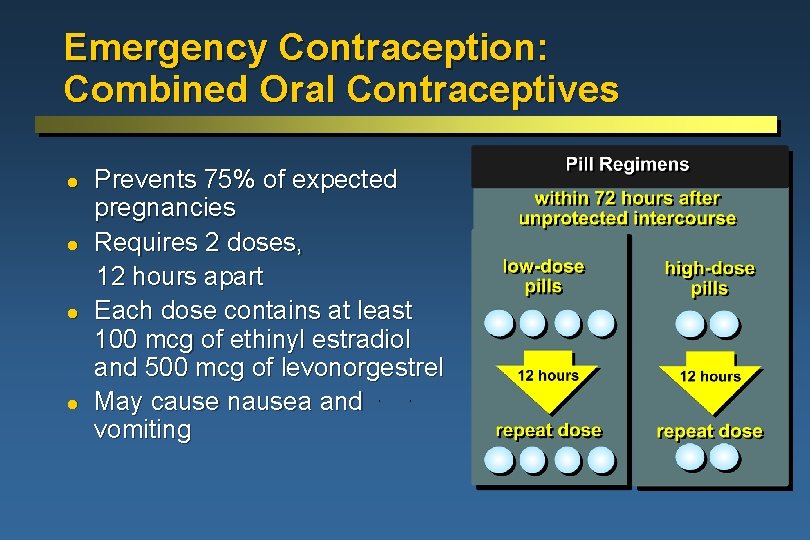
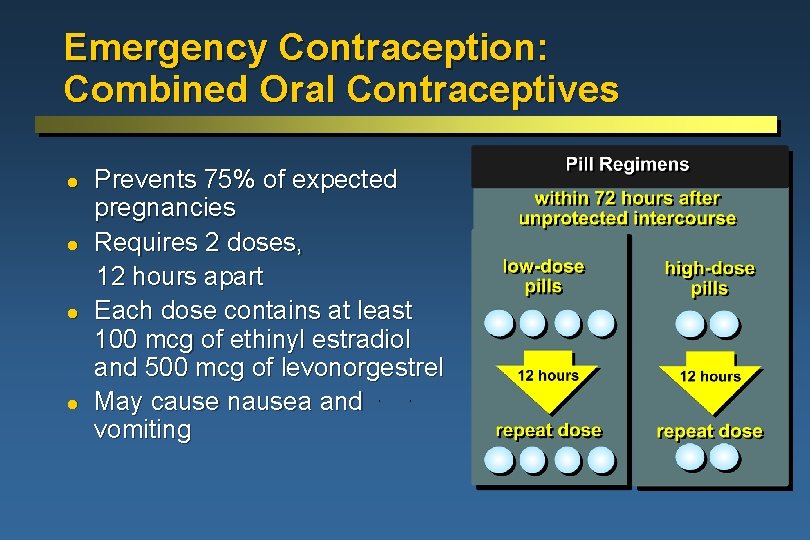
Emergency Contraception: Combined Oral Contraceptives l l Prevents 75% of expected pregnancies Requires 2 doses, 12 hours apart Each dose contains at least 100 mcg of ethinyl estradiol and 500 mcg of levonorgestrel May cause nausea and vomiting
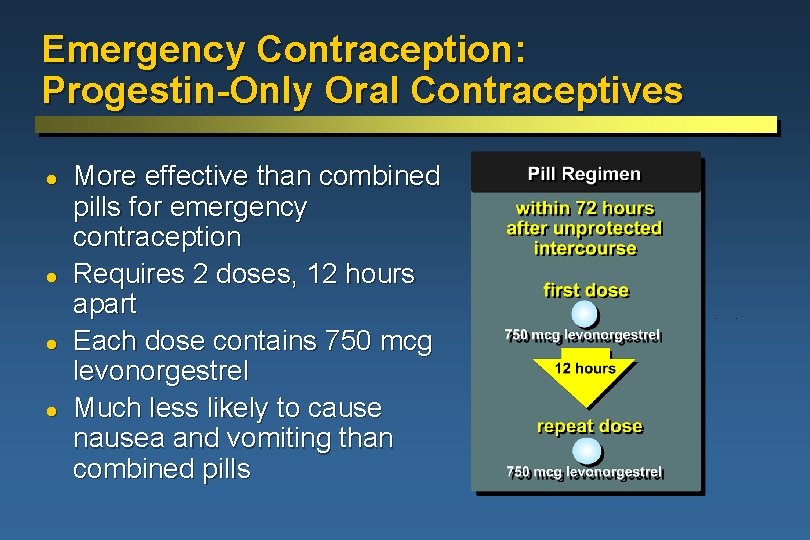
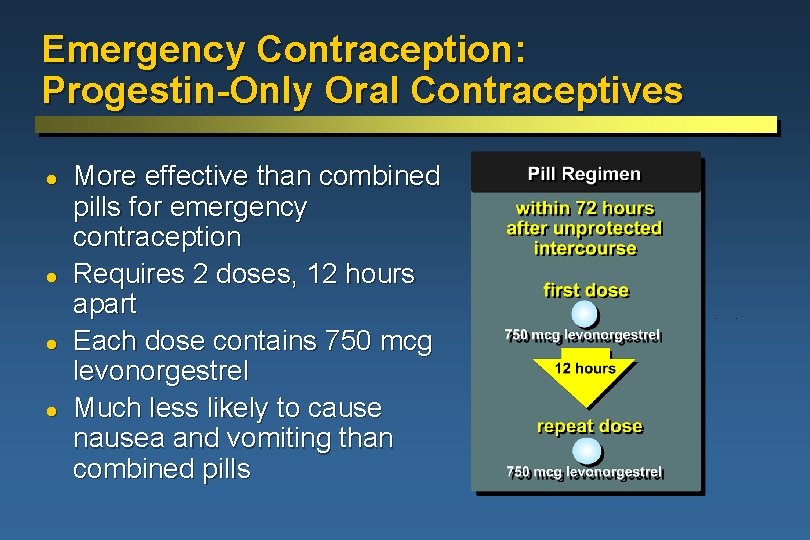
Emergency Contraception: Progestin-Only Oral Contraceptives l l More effective than combined pills for emergency contraception Requires 2 doses, 12 hours apart Each dose contains 750 mcg levonorgestrel Much less likely to cause nausea and vomiting than combined pills
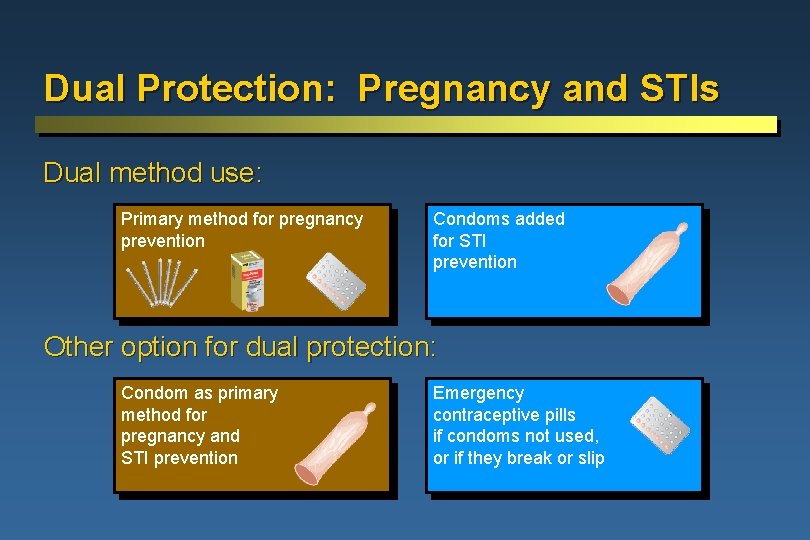
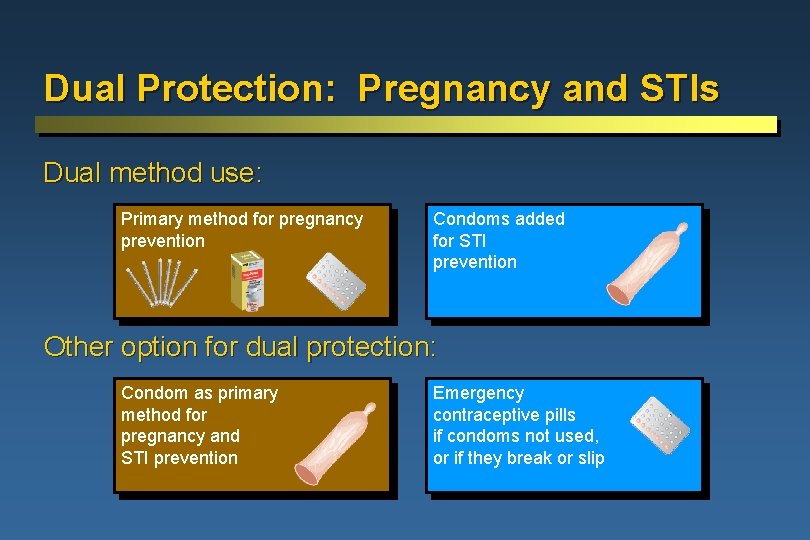
Dual Protection: Pregnancy and STIs Dual method use: Primary method for pregnancy prevention Condoms added for STI prevention Other option for dual protection: Condom as primary method for pregnancy and STI prevention Emergency contraceptive pills if condoms not used, or if they break or slip
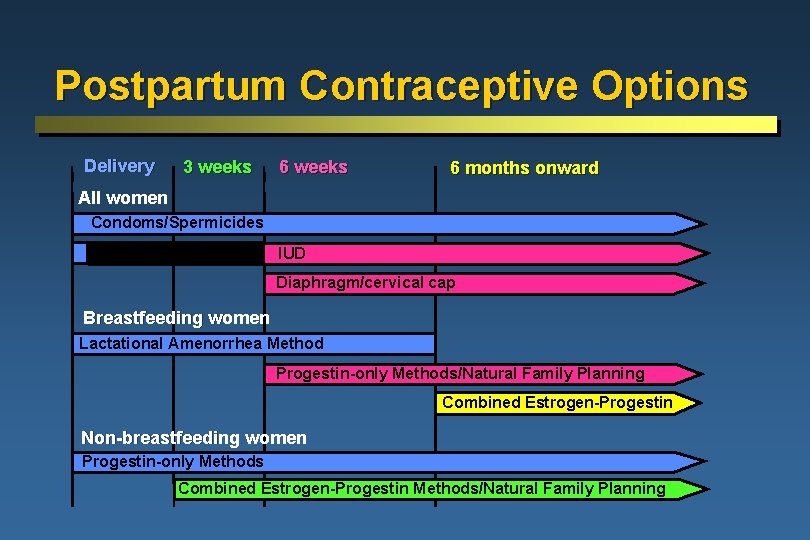
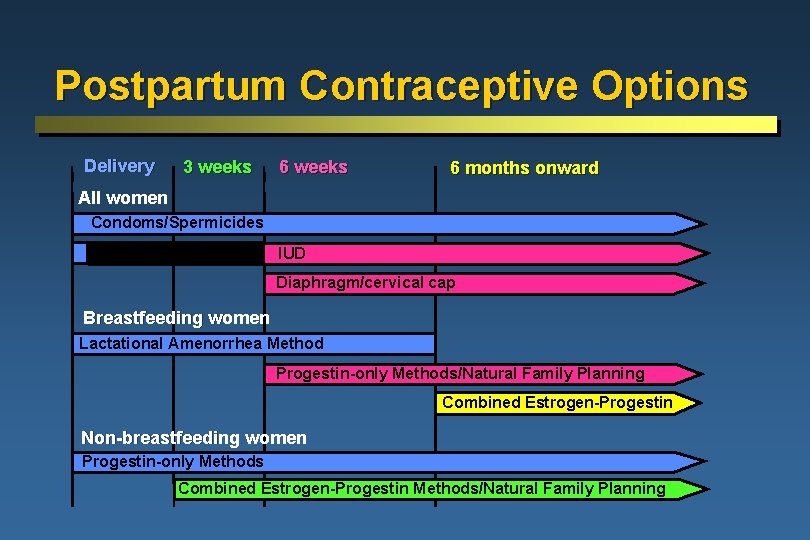
Postpartum Contraceptive Options Delivery 3 weeks 6 months onward All women Condoms/Spermicides IUD Diaphragm/cervical cap Breastfeeding women Lactational Amenorrhea Method Progestin-only Methods/Natural Family Planning Combined Estrogen-Progestin Non-breastfeeding women Progestin-only Methods Combined Estrogen-Progestin Methods/Natural Family Planning
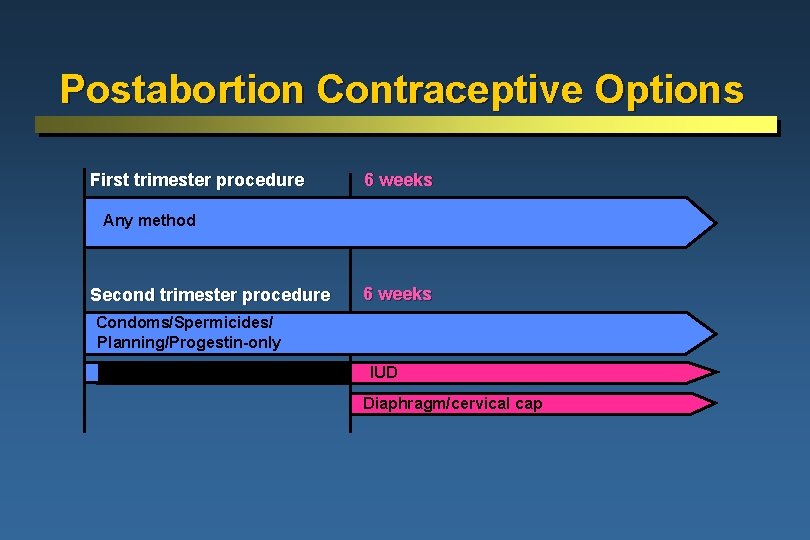
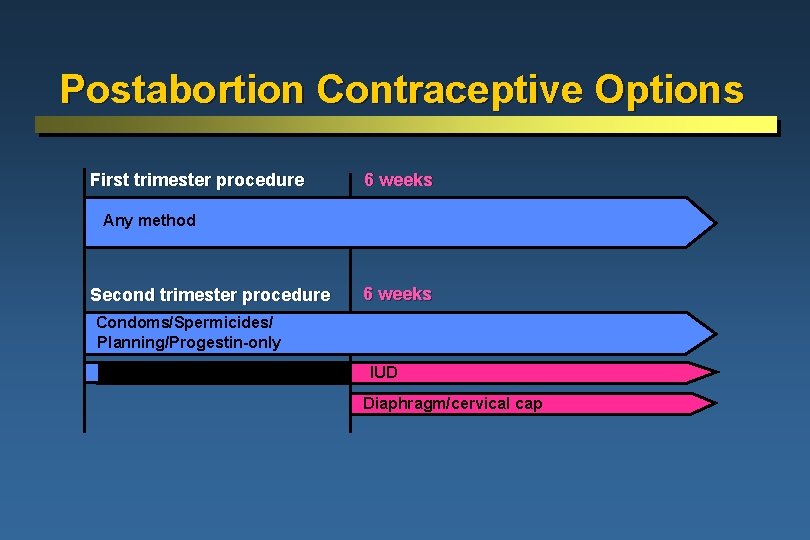
Postabortion Contraceptive Options First trimester procedure 6 weeks Any method Second trimester procedure 6 weeks Condoms/Spermicides/Combined Estrogen-Progestin/Natural Family Planning/Progestin-only IUD Diaphragm/cervical cap
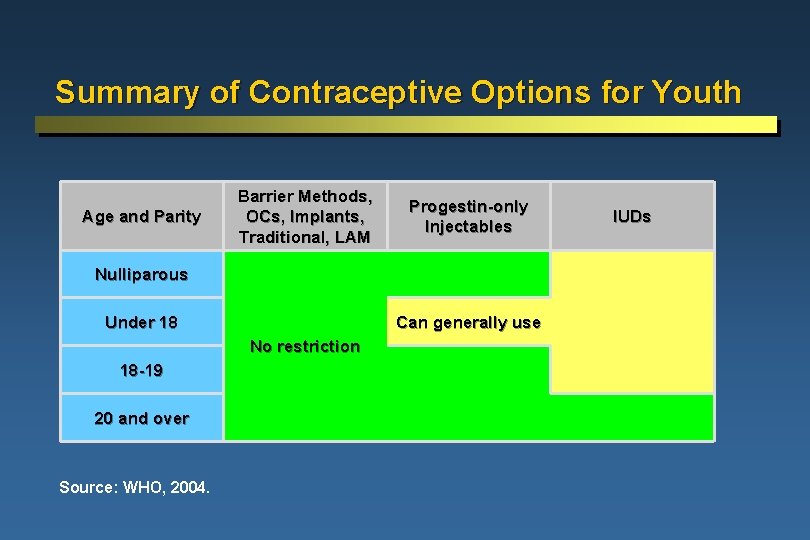
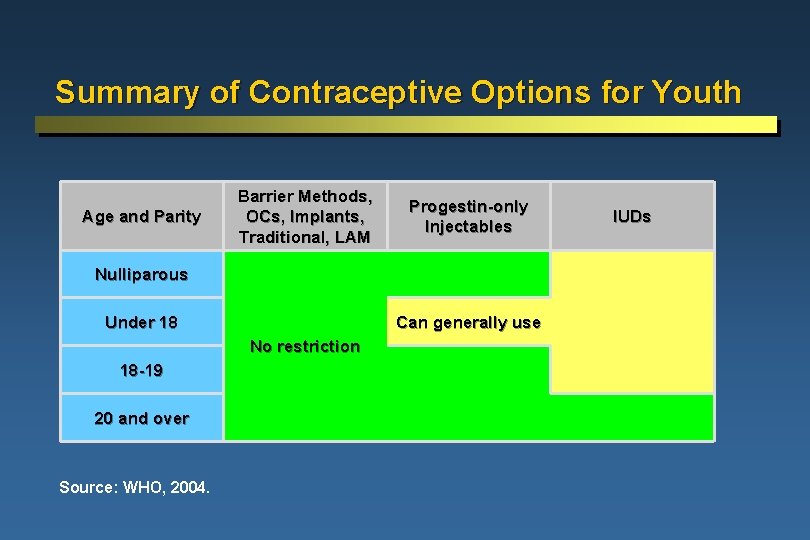
Summary of Contraceptive Options for Youth Age and Parity Barrier Methods, OCs, Implants, Traditional, LAM Progestin-only Injectables Nulliparous Under 18 Can generally use No restriction 18 -19 20 and over Source: WHO, 2004. IUDs
STI/HIV Prevention and Treatment: Priority for Young Adults Topics to be covered l STI/HIV risks and consequences l Most common STIs, including HIV l STI/HIV prevention l STI/HIV counseling l Voluntary counseling and testing l Risk assessment l STI/HIV management and treatment

STI/HIV Risk Higher in Young Adults Behavioral susceptibility: Youth feel invulnerable, don’t believe it could happen to them l Condoms not used consistently or correctly l Have multiple partners, or partners with multiple partners l Other factors such as drug and alcohol use l Biological susceptibility in young women: l Cervical ectopy
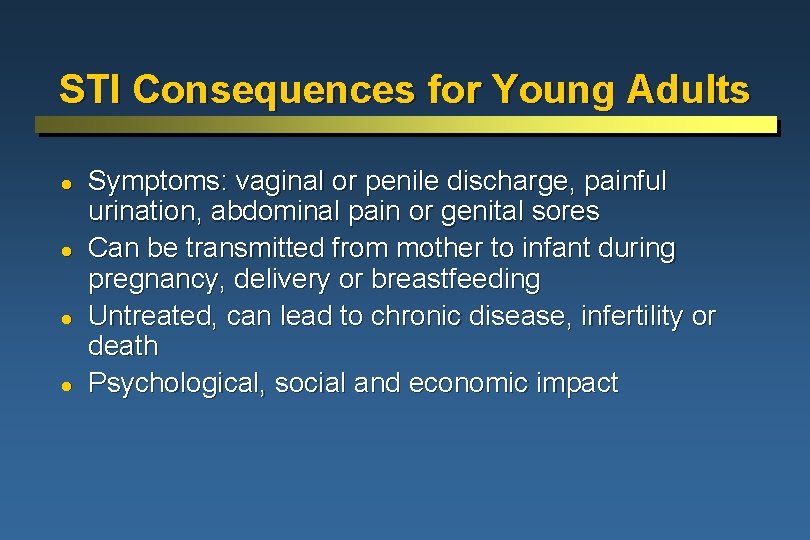
STI Consequences for Young Adults l l Symptoms: vaginal or penile discharge, painful urination, abdominal pain or genital sores Can be transmitted from mother to infant during pregnancy, delivery or breastfeeding Untreated, can lead to chronic disease, infertility or death Psychological, social and economic impact
Most Common STIs Providers need to know STI prevalence in their areas Curable (mostly bacterial) Trichomoniasis, chlamydia, gonorrhea, syphilis Incurable (viral) HIV/AIDS, human papilloma virus (HPV), hepatitis B, herpes
Curable STIs l l l Curable with antibiotics Access to treatment services important opportunity Often asymptomatic and hard to diagnose Can lead to PID and infertility Some can be transmitted during childbirth or result in adverse pregnancy outcomes Increases risk of HIV transmission
Most Common Curable STIs Trichomoniasis: l Estimated to be most common STI globally l Associated with adverse pregnancy outcomes Chlamydia and gonorrhea: l High rates in young adults l May lead to PID l Can infect newborn during childbirth Syphilis: l High risk of congenital infection
HIV: High Risk for Young Adults Half of all infections worldwide are in people under 25 years of age l New infections concentrated in young women HIV can be transmitted through semen, vaginal fluids, blood, breastmilk or in utero l No vaccine exists l Prevention strategies are essential l
Other Viral STIs Human papilloma virus (HPV): l Causes genital warts l Highly associated with cervical cancer Hepatitis B: l Causes liver damage l Vaccine available Herpes: l Symptomatic or asymptomatic l Widespread among young adults
Addressing the HIV Epidemic: Youth Central to Strategies l l l Build support among leaders to speak out Use education and communication Address cultural, social and gender norms Promote condoms Make services youth-friendly Reach out to vulnerable youth
Orphans and Vulnerable Children (OVC) l l By 2010, more than 25 million children will have lost one or both parents to AIDS Needs to address: - Whether orphans should know their serostatus - Increased risk of sexual exploitation - Stable family structure, educational opportunities - Mental health supports, such as memory books - Reproductive health and HIV prevention
STI Prevention Should be part of all reproductive health programs l l Provide information on STIs Counsel clients about safe sexual behaviors Assess risk for STIs Promote and distribute condoms
STI Counseling Messages for youth: l All sexual activity puts them at risk for STIs/HIV l Safest sexual behavior is abstinence l For those sexually active, safe sexual behaviors include: - Assessing if partner is infected - Mutual monogamy - Reducing number of sexual partners - Using condoms
Voluntary Counseling and Testing (VCT) l l l Where HIV prevalence is high, young people want to know their status VCT can help young adults use safer sexual practices and reduce rates of STIs VCT presents challenges: - Recruitment - Preservation of confidentiality - Stigma
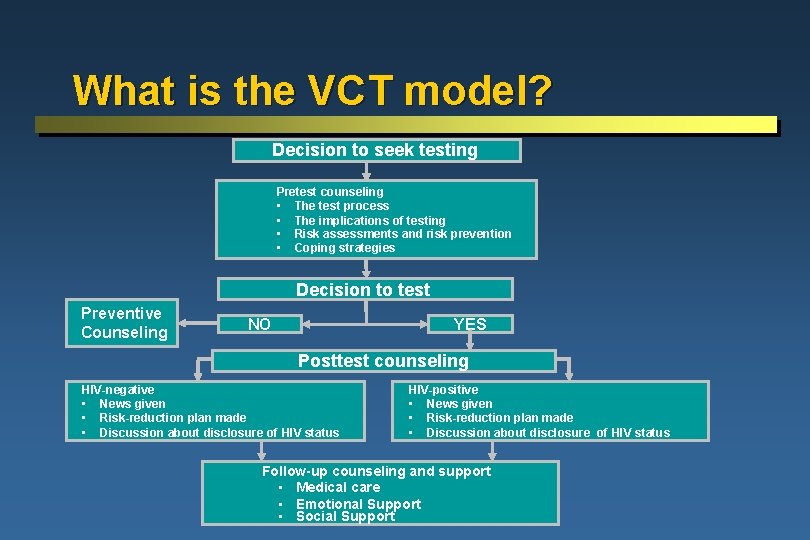
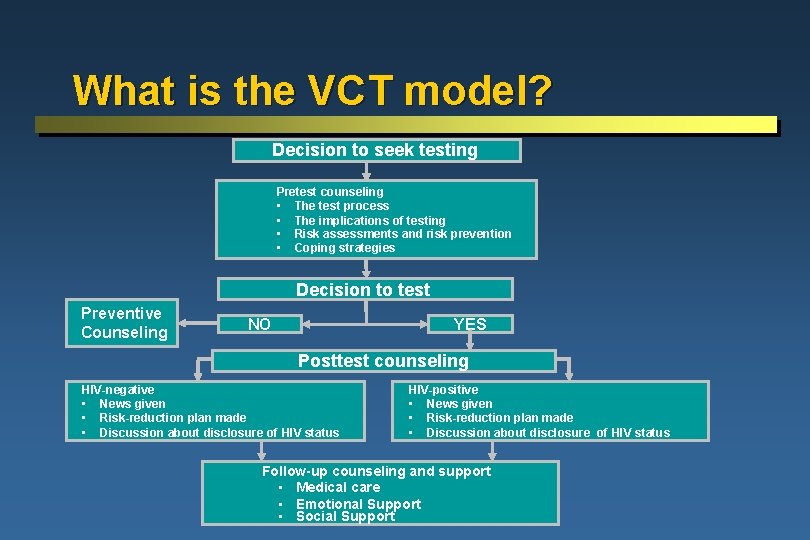
What is the VCT model? Decision to seek testing Pretest counseling • The test process • The implications of testing • Risk assessments and risk prevention • Coping strategies Decision to test Preventive Counseling NO YES Posttest counseling HIV-negative • News given • Risk-reduction plan made • Discussion about disclosure of HIV status HIV-positive • News given • Risk-reduction plan made • Discussion about disclosure of HIV status Follow-up counseling and support • Medical care • Emotional Support • Social Support
Assessment of STI Risk STI symptoms include: - Vaginal or penile discharge, painful urination, abdominal pain, or genital sores Risk factors include: - Number of sexual partners - Client’s age - Recent new partner - Previous STI infection - Partner has other partners or STI symptoms
STI Management: Diagnosis and Treatment Using laboratory tests: l Expensive and require client to return to clinic Using syndromic approach: l Based on a person’s symptoms and signs and the local epidemiology l Works well for ulcers and male urethral discharge; does not work as well for vaginal discharge syndrome During treatment, counseling should emphasize partner notification
Summary STI prevention and treatment – a priority for those working with youth l l Young women in particular need attention since HIV rates are increasing most rapidly among this group Good counseling can help all youth avoid STI infection
Youth Are Our Future
 Molar pregnancy
Molar pregnancy Female reproductive system pregnancy
Female reproductive system pregnancy Ogn and pgn in contraception
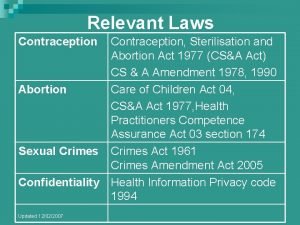
Ogn and pgn in contraception Contraception sterilisation and abortion act 1977
Contraception sterilisation and abortion act 1977 Fdic money smart for young adults
Fdic money smart for young adults Victorian era birth control
Victorian era birth control Cape cervicale caya
Cape cervicale caya Contraception for over 40s
Contraception for over 40s Contraception
Contraception Diaphragme contraception caya
Diaphragme contraception caya Voluntary surgical contraception
Voluntary surgical contraception Lam contraception method
Lam contraception method Nidation
Nidation Mental health and older adults
Mental health and older adults Mental health and older adults
Mental health and older adults Older adults mental health
Older adults mental health Components of rch phase 1
Components of rch phase 1 Role of nurse in rch phase 2
Role of nurse in rch phase 2 Inguinal hernia are a female reproductive health issue
Inguinal hernia are a female reproductive health issue Definition of reproductive health
Definition of reproductive health Interconception definition
Interconception definition Height of fundus during pregnancy
Height of fundus during pregnancy Picme2.0
Picme2.0 The art and science of helping adults learn
The art and science of helping adults learn Adhd treatment plan
Adhd treatment plan Type 1 diabetes in adults diagnosis and management
Type 1 diabetes in adults diagnosis and management Unit 11 safeguarding adults and promoting independence
Unit 11 safeguarding adults and promoting independence Office of aging and adults services
Office of aging and adults services Oaas
Oaas Nice guidelines diarrhoea and vomiting in adults
Nice guidelines diarrhoea and vomiting in adults Health and social care component 3 health and wellbeing
Health and social care component 3 health and wellbeing When might you receive a blood transfusion brainpop
When might you receive a blood transfusion brainpop Normal ast and alt levels in pregnancy
Normal ast and alt levels in pregnancy Chapter 4 prenatal care and adaptations to pregnancy
Chapter 4 prenatal care and adaptations to pregnancy Lesson 20.2 the male reproductive system
Lesson 20.2 the male reproductive system Chapter 13 anatomy and physiology of pregnancy
Chapter 13 anatomy and physiology of pregnancy Pregnancy and fetal development brainpop answers
Pregnancy and fetal development brainpop answers Kode icd 10 persalinan kembar dua
Kode icd 10 persalinan kembar dua With whom did shilpi and her husband discuss pregnancy?
With whom did shilpi and her husband discuss pregnancy? Chapter 4 prenatal care and adaptations to pregnancy
Chapter 4 prenatal care and adaptations to pregnancy Breast tenderness early pregnancy
Breast tenderness early pregnancy Selective mutism in adults
Selective mutism in adults C
C Normal vital signs of newborn
Normal vital signs of newborn Bluegrass billbugs overwinter as adults
Bluegrass billbugs overwinter as adults Love language example
Love language example Apical radial pulse
Apical radial pulse Examples of problem solving scenarios for adults
Examples of problem solving scenarios for adults Amoebiasis stool color for adults
Amoebiasis stool color for adults Self advocacy worksheets
Self advocacy worksheets Pyloric stenosis adults treatment
Pyloric stenosis adults treatment Oppositional defiant disorder in adults
Oppositional defiant disorder in adults Nonverbal learning disorder symptoms in adults
Nonverbal learning disorder symptoms in adults Grading of jaundice in neonates
Grading of jaundice in neonates Hobbs and holt token economy
Hobbs and holt token economy David howe ent
David howe ent Flask shaped
Flask shaped Hep b vaccine schedule for adults
Hep b vaccine schedule for adults Unhealthy relationship scenarios
Unhealthy relationship scenarios Testul gama
Testul gama Riddles about fruits
Riddles about fruits Male and female skeleton differences
Male and female skeleton differences Placement of aed pads on adults
Placement of aed pads on adults Adult fetal alcohol syndrome
Adult fetal alcohol syndrome Hpv vaccine schedule adults
Hpv vaccine schedule adults Oppositional defiant disorder in adults
Oppositional defiant disorder in adults Cpr in physical education
Cpr in physical education Adjective: 'bad' (superlative of superiority).
Adjective: 'bad' (superlative of superiority). Comparative small
Comparative small Childlike behavior in adults
Childlike behavior in adults Adderall dosage by weight
Adderall dosage by weight Altered cognition in older adults is commonly attributed to
Altered cognition in older adults is commonly attributed to Hyperammonemia causes
Hyperammonemia causes Burn management formula
Burn management formula The silence of adults bdo
The silence of adults bdo Pulse check in unresponsive victim
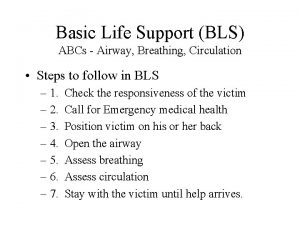
Pulse check in unresponsive victim Abcs of bls
Abcs of bls Ocd symptoms in adults
Ocd symptoms in adults Anticipatory guidance for elderly
Anticipatory guidance for elderly Normal range for vital signs
Normal range for vital signs Compression to ventilation ratio adults
Compression to ventilation ratio adults Is a child's urine the same as an adults
Is a child's urine the same as an adults Tana brown
Tana brown Pediatric medication administration guidelines
Pediatric medication administration guidelines Conclusion of physical examination
Conclusion of physical examination Train adults
Train adults Dose calculation formula for adults
Dose calculation formula for adults Adults in scouting
Adults in scouting Wiltshire safeguarding training
Wiltshire safeguarding training Adults spend about ______% of their sleep in rem sleep.
Adults spend about ______% of their sleep in rem sleep. Schistosoma
Schistosoma Teaching phonics to adults
Teaching phonics to adults Assessment strategies for adults
Assessment strategies for adults Older adults
Older adults Hampshire safeguarding adults board
Hampshire safeguarding adults board Covids older adults
Covids older adults