Contraception in the over 40s Why do over

- Slides: 19

Contraception in the over 40’s
Why do over 40’s need separate guidance? � Method choice may be affected by age and risk factors; eg obesity, breast and gynaecological cancers. � When � How can the method be discontinued? is the menopause diagnosed?
Typical scenario. . 49 yr old Debbie , on progesterone only pill. Amenorrhoea 2+ yrs. Having some hot flushes, reduced libido, mood swings. She wonders if this may be due to the menopause. Can she have a blood test? Does she need to continue contraception?
Transition to menopause ( 40 -50) � Intermittent ovulation/anovulation with variable FSH levels. � Typically last 4 -5 years � Cycle length may reduce or increase. � Amenorrhoea not a reliable indicator of menopause when using hormonal contraception � FSH levels; not an exact science!
Contraceptive method. � No method is contraindicated by age alone up to 50 yrs. � Some methods become less safe but this is dependent on other risk factors. � Need to use UKMEC guidance but if there are multiple risk factors this may affect advice.
Sexual health in the over 40’s
Sexual health in over 40’s � Average divorce in women is 41 yrs. � New relationships common. � The number of live births in 40+ has doubled from 2000 to 2015 ; now approx 30, 000 pa ( England/Wales) � 2015; 28% pregancies in over 40’s resulted in � Older women may not be well informed regarding sexual health and contraception.
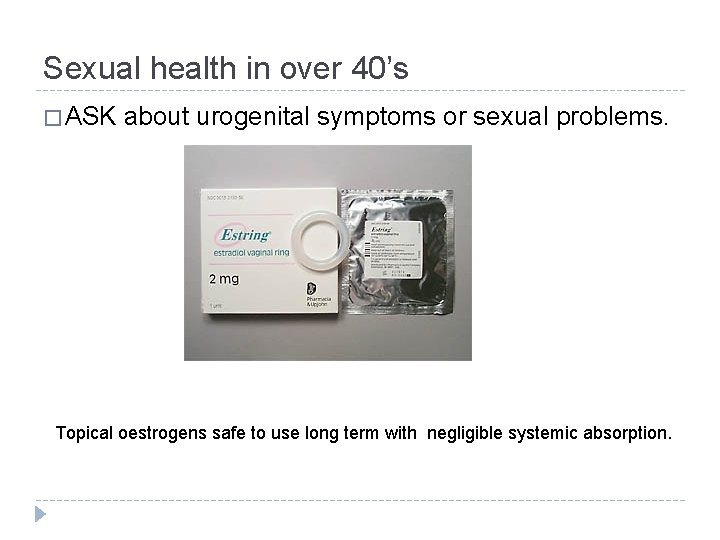
Sexual health in over 40’s � ASK about urogenital symptoms or sexual problems. Topical oestrogens safe to use long term with negligible systemic absorption.
Other vaginal lubricants. � Silicone based preparations more effective.
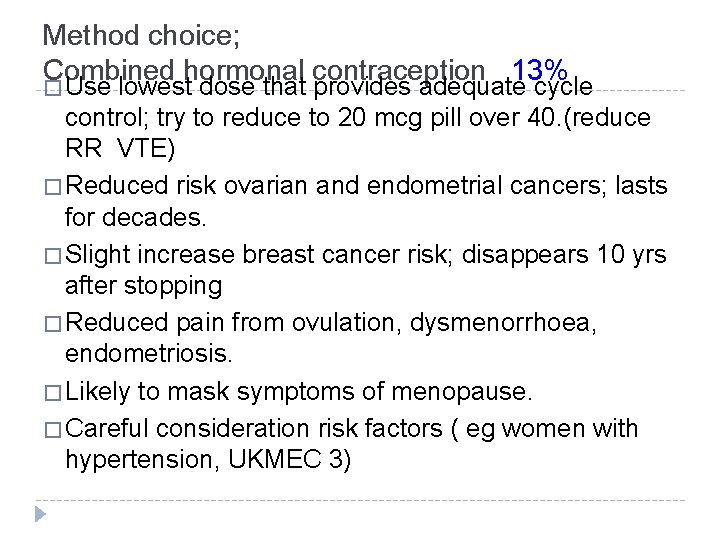
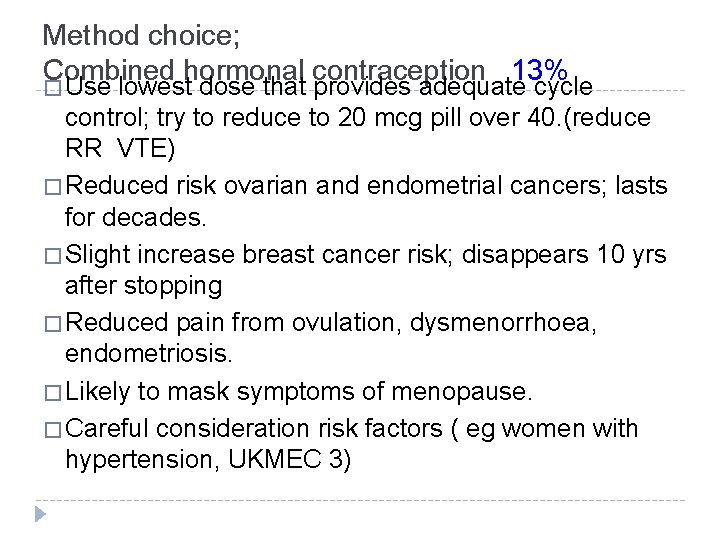
Method choice; Combined hormonal contraception 13% � Use lowest dose that provides adequate cycle control; try to reduce to 20 mcg pill over 40. (reduce RR VTE) � Reduced risk ovarian and endometrial cancers; lasts for decades. � Slight increase breast cancer risk; disappears 10 yrs after stopping � Reduced pain from ovulation, dysmenorrhoea, endometriosis. � Likely to mask symptoms of menopause. � Careful consideration risk factors ( eg women with hypertension, UKMEC 3)
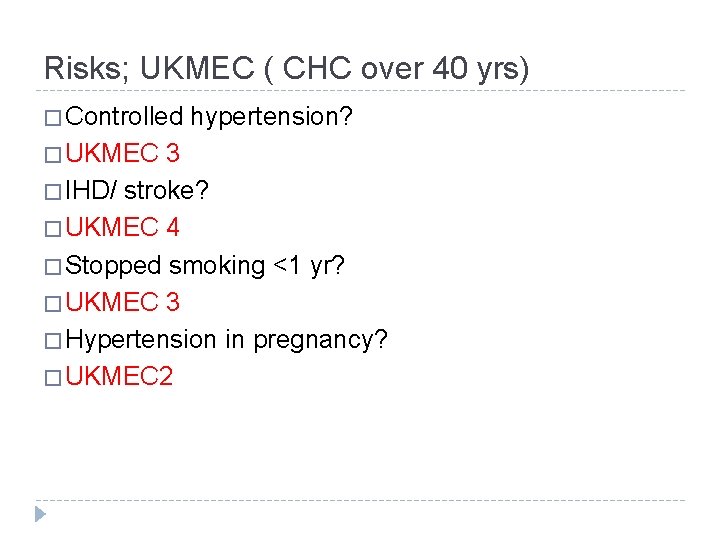
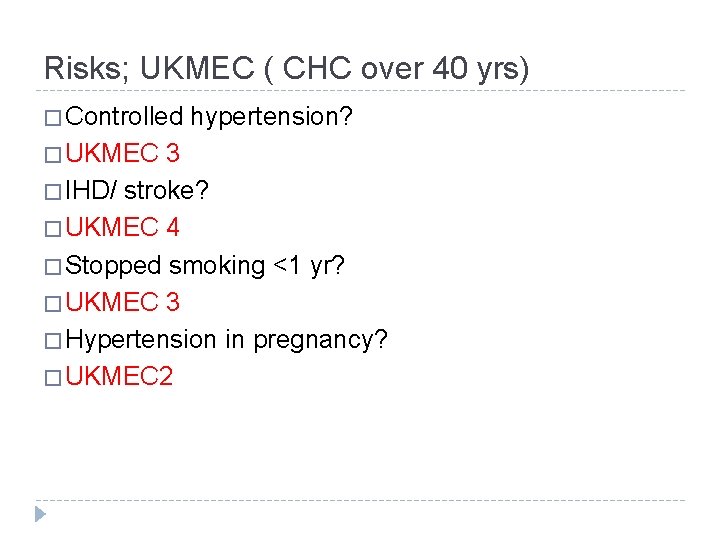
Risks; UKMEC ( CHC over 40 yrs) � Controlled � UKMEC hypertension? 3 � IHD/ stroke? � UKMEC 4 � Stopped smoking <1 yr? � UKMEC 3 � Hypertension in pregnancy? � UKMEC 2
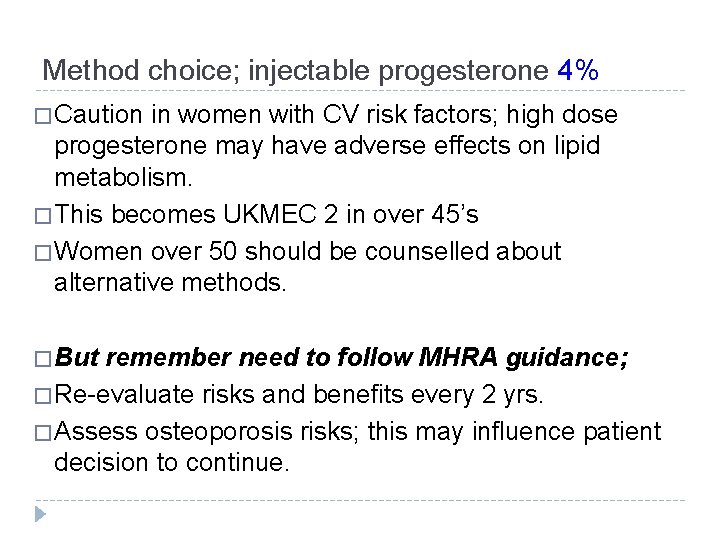
Method choice; injectable progesterone 4% � Caution in women with CV risk factors; high dose progesterone may have adverse effects on lipid metabolism. � This becomes UKMEC 2 in over 45’s � Women over 50 should be counselled about alternative methods. � But remember need to follow MHRA guidance; � Re-evaluate risks and benefits every 2 yrs. � Assess osteoporosis risks; this may influence patient decision to continue.
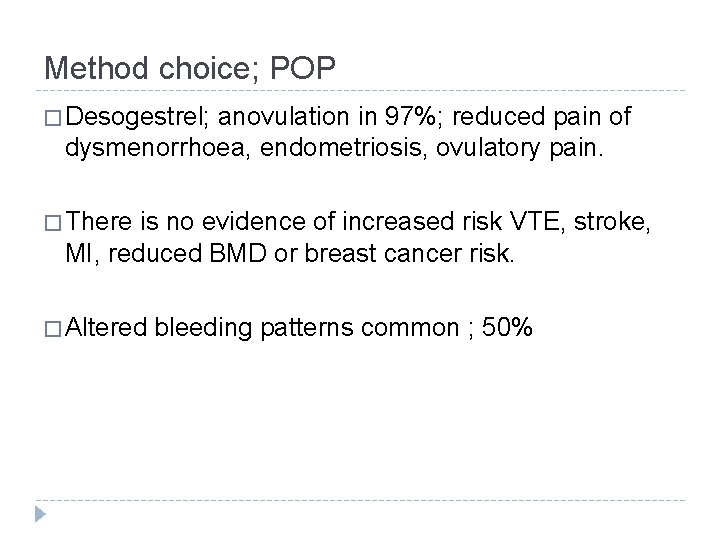
Method choice; POP � Desogestrel; anovulation in 97%; reduced pain of dysmenorrhoea, endometriosis, ovulatory pain. � There is no evidence of increased risk VTE, stroke, MI, reduced BMD or breast cancer risk. � Altered bleeding patterns common ; 50%
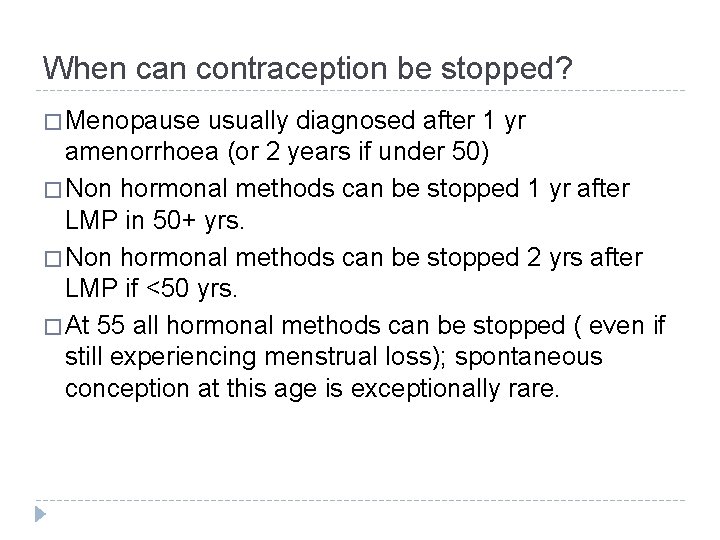
When can contraception be stopped? � Menopause usually diagnosed after 1 yr amenorrhoea (or 2 years if under 50) � Non hormonal methods can be stopped 1 yr after LMP in 50+ yrs. � Non hormonal methods can be stopped 2 yrs after LMP if <50 yrs. � At 55 all hormonal methods can be stopped ( even if still experiencing menstrual loss); spontaneous conception at this age is exceptionally rare.
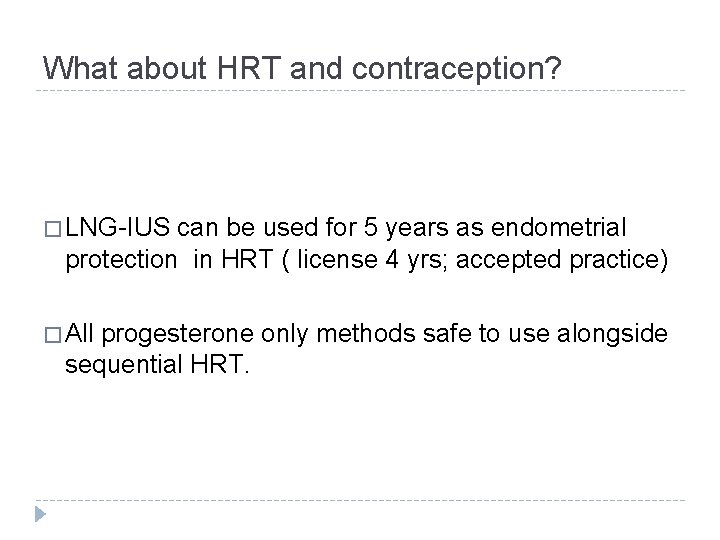
What about HRT and contraception? � LNG-IUS can be used for 5 years as endometrial protection in HRT ( license 4 yrs; accepted practice) � All progesterone only methods safe to use alongside sequential HRT.
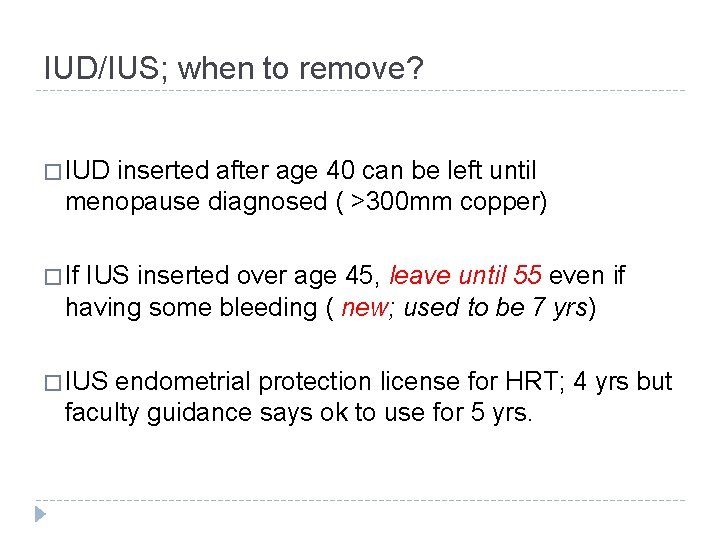
IUD/IUS; when to remove? � IUD inserted after age 40 can be left until menopause diagnosed ( >300 mm copper) � If IUS inserted over age 45, leave until 55 even if having some bleeding ( new; used to be 7 yrs) � IUS endometrial protection license for HRT; 4 yrs but faculty guidance says ok to use for 5 yrs.
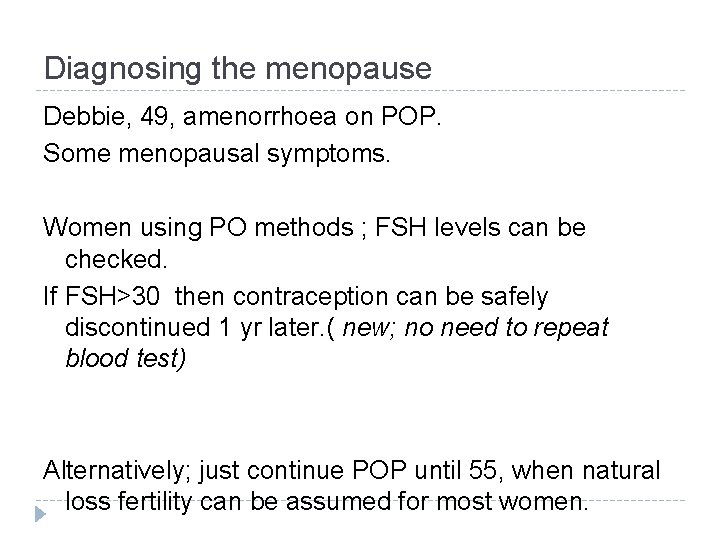
Diagnosing the menopause Debbie, 49, amenorrhoea on POP. Some menopausal symptoms. Women using PO methods ; FSH levels can be checked. If FSH>30 then contraception can be safely discontinued 1 yr later. ( new; no need to repeat blood test) Alternatively; just continue POP until 55, when natural loss fertility can be assumed for most women.
Women using CHC. � FSH is not a reliable indicator of ovarian failure in women using combined hormones, even if measured during the hormone-free interval. � At age 50 switch to non hormonal or PO method. � Prepare for the worst. . . .
Time for HRT? ? ?