CONTRACEPTION DEFINITION Any methods or system that allow


![VAGINAL SPONGE[TODAY] Soft disposable foam sponge made of polyurethane, saturated with Nanoxynol-9 Attached with VAGINAL SPONGE[TODAY] Soft disposable foam sponge made of polyurethane, saturated with Nanoxynol-9 Attached with](https://slidetodoc.com/presentation_image_h/7efeb3ac45350115e9f101c1a4c4c157/image-31.jpg)


- Slides: 103
CONTRACEPTION
DEFINITION �Any methods or system that allow inter course yet prevent conception called contraception. �IDEAL CONTRACEPTIVE: �Safe �Effective �Acceptable �Simple to administer �Inexpensive �Reversible �Independent of coitus �Long lasting
�Present approach to the family planning programme is the cafeteria approach. Measurement of contraceptive efficiency Pearl index; This is expressed pregnancy rate per 100 women years and is calculated by the formula. Pregnancy rate per HWY= total accidental pregnancies× 1200÷total months of exposure to un intended pregnancy. Total month of exposure is obtained by deducting from the period under review those methods during which for extrinsic reasons contraception was not possible. 10 months are deducted from the a full term pregnancy and 4 months from abortion. Life table technique: To over come the bias of the pearl index this is used. This estimates probability of being pregnant while using any methods during the fixed period. Pregnancy rate is expressed as X per HWY. This method gives information about the method failure and patient failure.
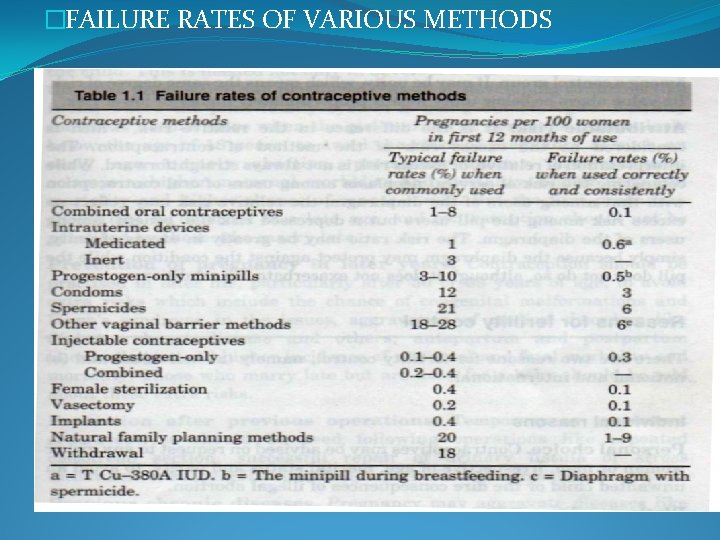
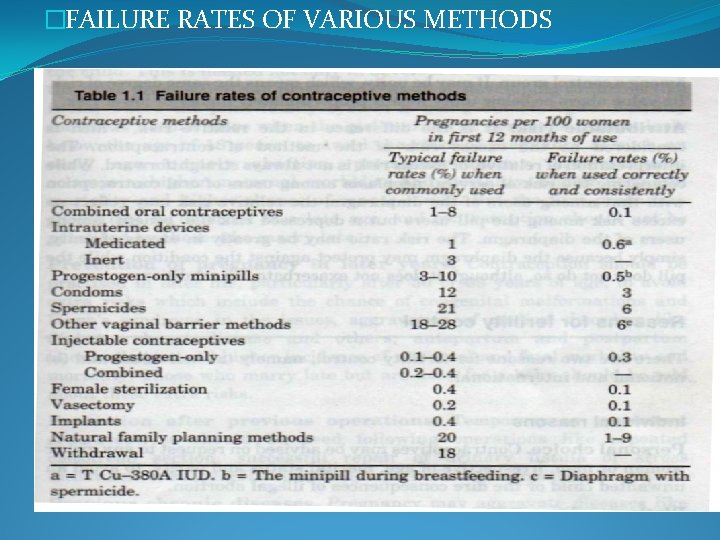
�FAILURE RATES OF VARIOUS METHODS
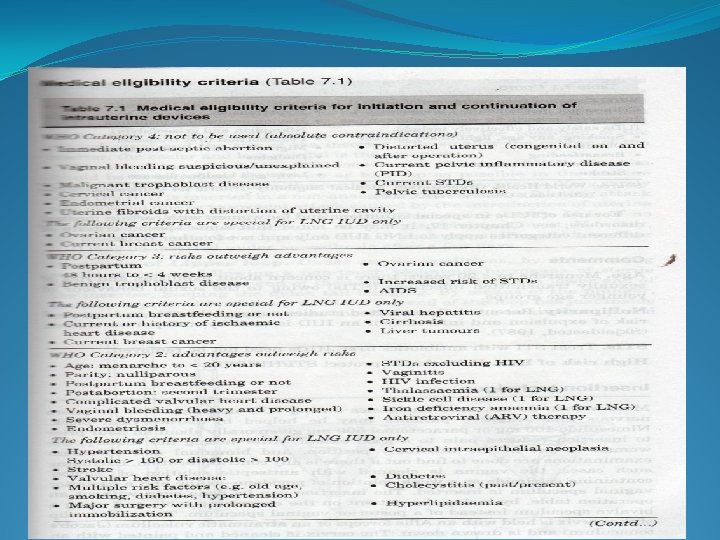
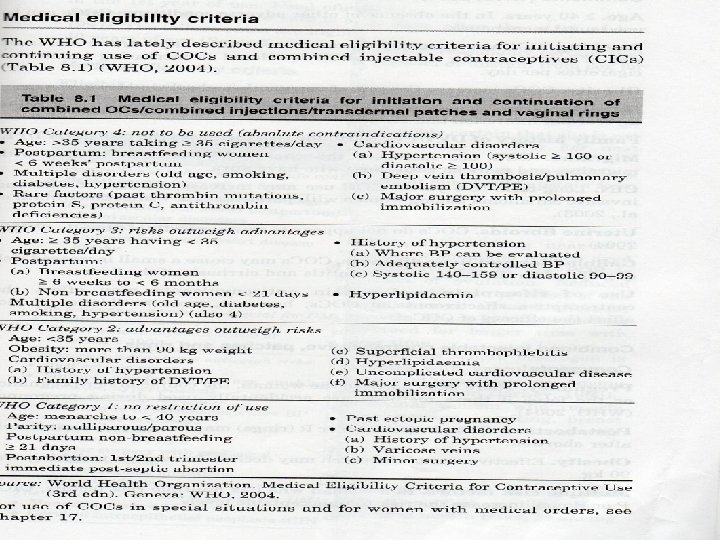
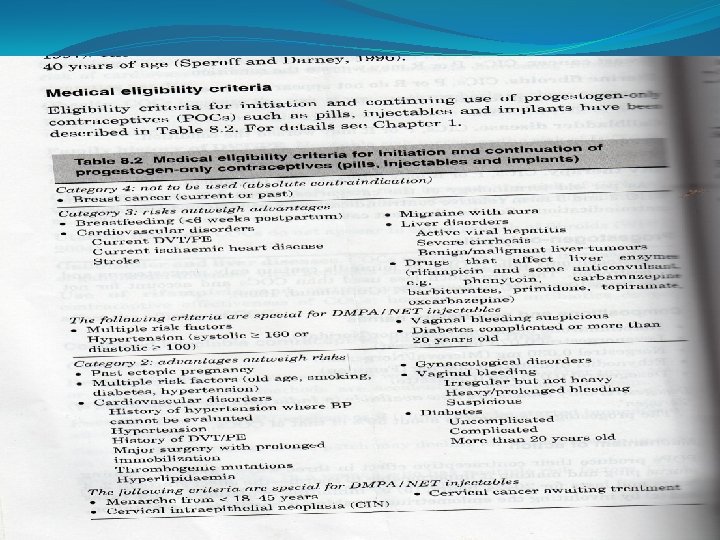
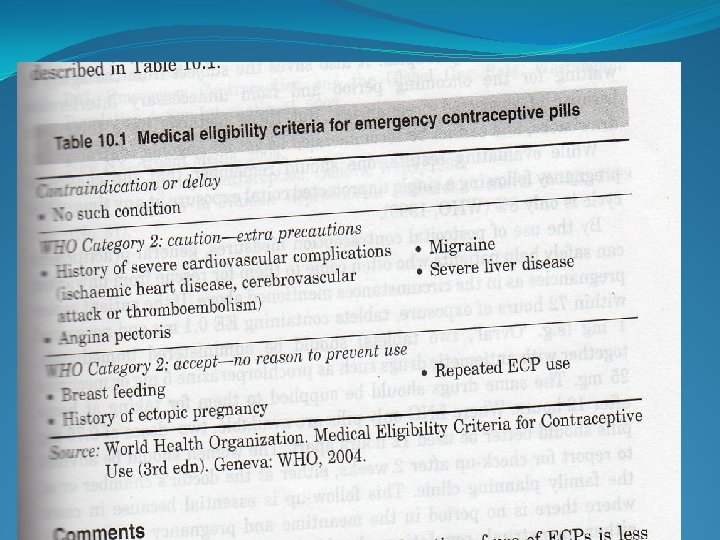
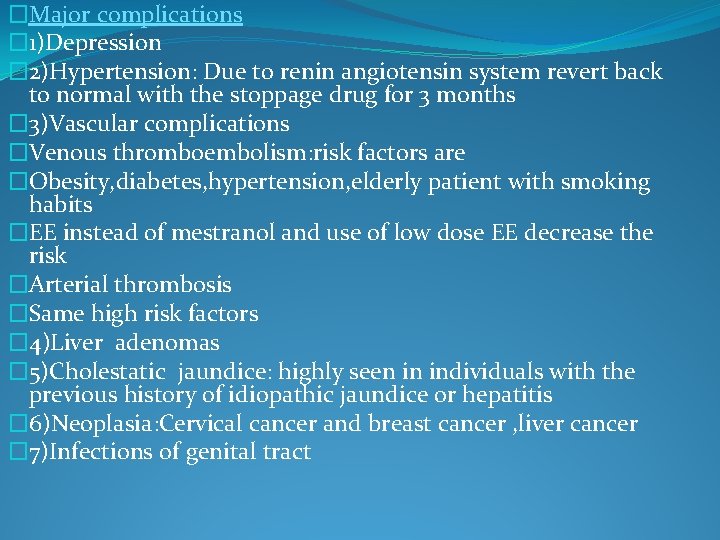
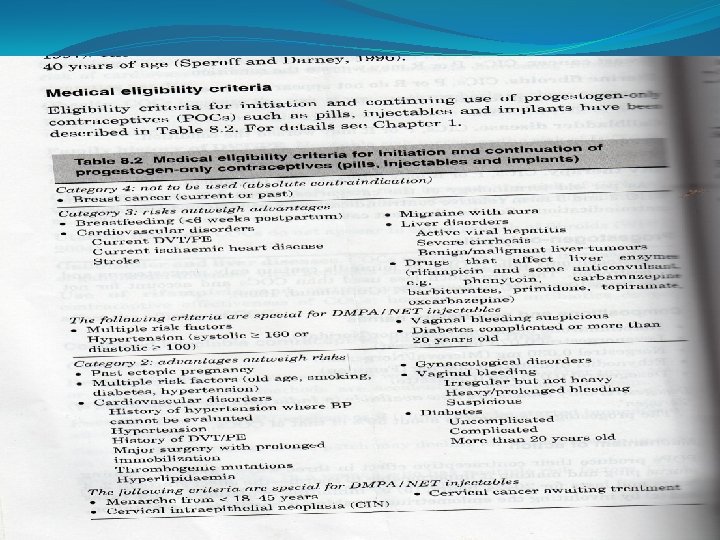
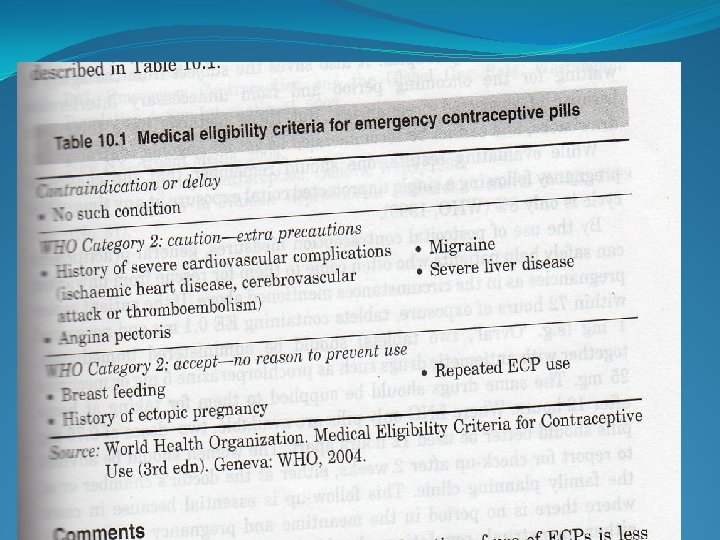
�MEDICAL ELIGIBILITY CRITERIA �WHO in 2004 published this for initiation and continuing use of contraceptives on the basis of the thorough review of the latest clinical and epidemiological information taking into account the risks and benefits of using such method. �Eligibility criteria for reversible contraceptives �Category 1 - no restrictions for use. �Category 2 -advantages of using this over weigh theoretical or proven risks. �Category 3 -therotical or proven risks out weigh the advantages of this method. �Category 4 -use of this methods presents un acceptable health risks.
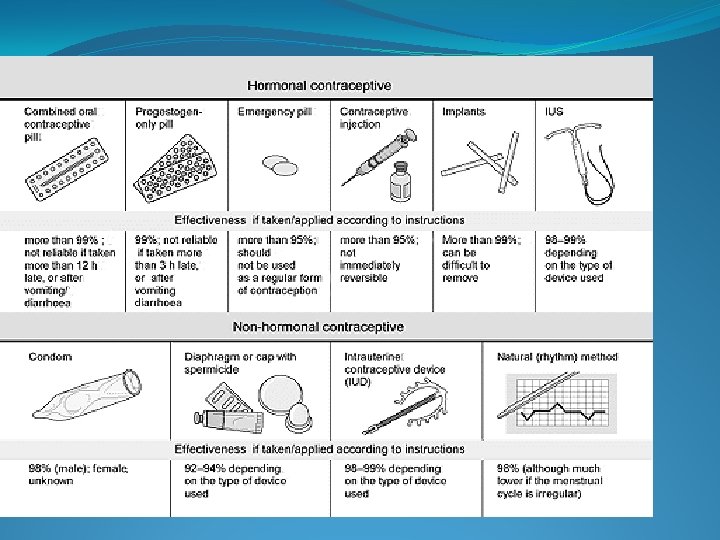
METHODS OF CONTRACEPTION A) TEMPORARY METHODS � Natural methods �Barrier methods �IUCDS �Steroidal contraceptives B) PERMANENT METHODS �Female: Tubal occlusion �Male: Vasectomy
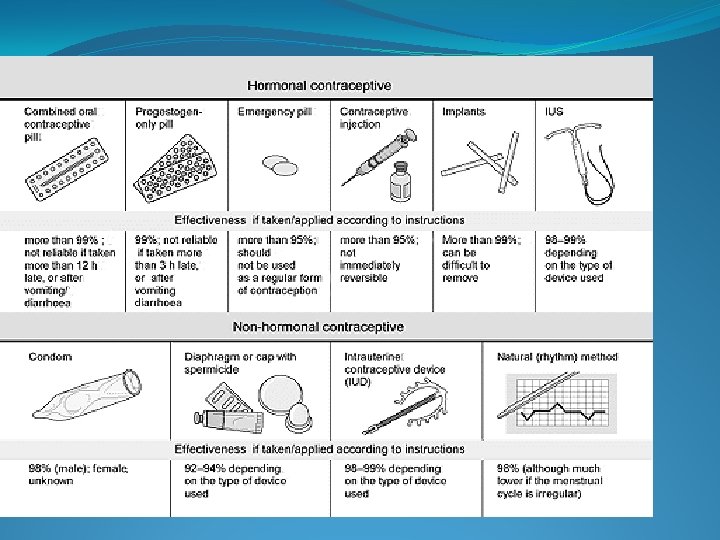
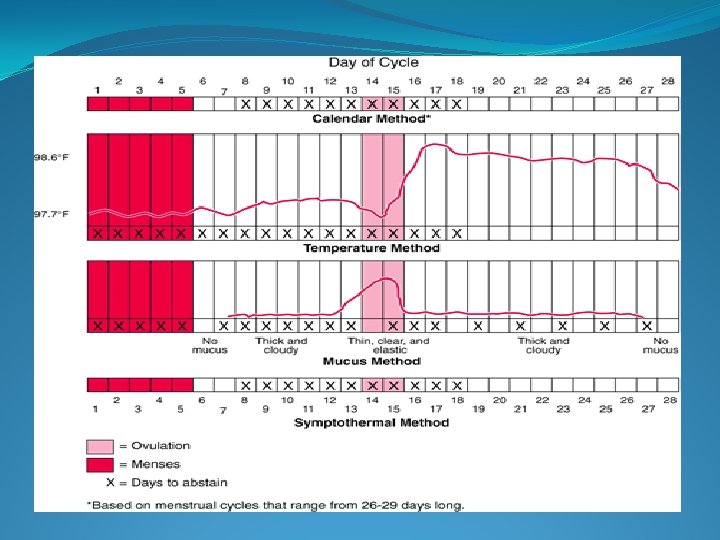
�Natural methods of contraception � DEFINITION : methods that do not use the application of medicine. �FERTILITY AWARENESS BASED METHODS �Method of planning and preventing pregnancy by observing signs and symptoms of the fertile phase and voidance of the coitus during the fertile phase if pregnancy to be avoided. �METHODS ARE: �Rhythm method �Basal body temperature method �Cervical mucus method �Sympothermal method �Standard days method
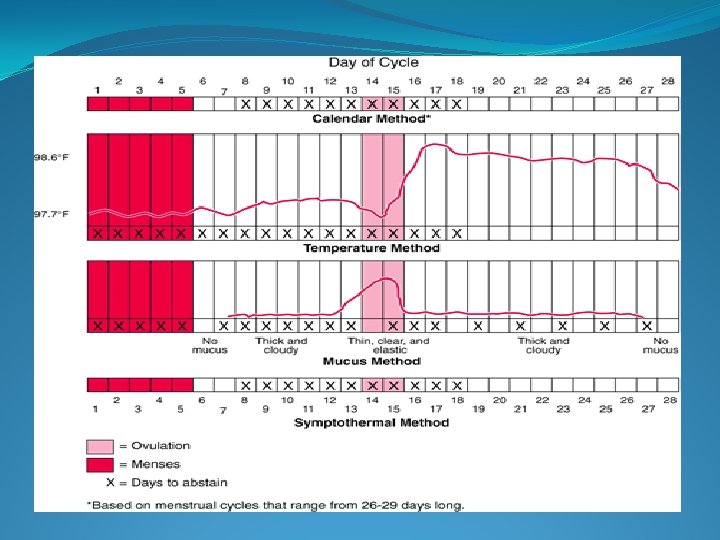
�Rhythm method/Calendar method �Based on OGINOS theory that ovulation takes place between 14+2 days that is between D 7 -D 21 �Irregular cycles (shortest cycle-18) and (longest cycles 11) �Basal _Body Temperature Method �Principle: There is the rise in BBT soon after the ovulation due to progesterone rise. �Rise in temp 0. 5 -0. 8˚F/0. 2 -0. 4˚C. . �Couples are advised to avoid coitus 3 day after the temp rise in the post- ovulatory period. �preovulatory safe period cannot be decided so this is not effective.
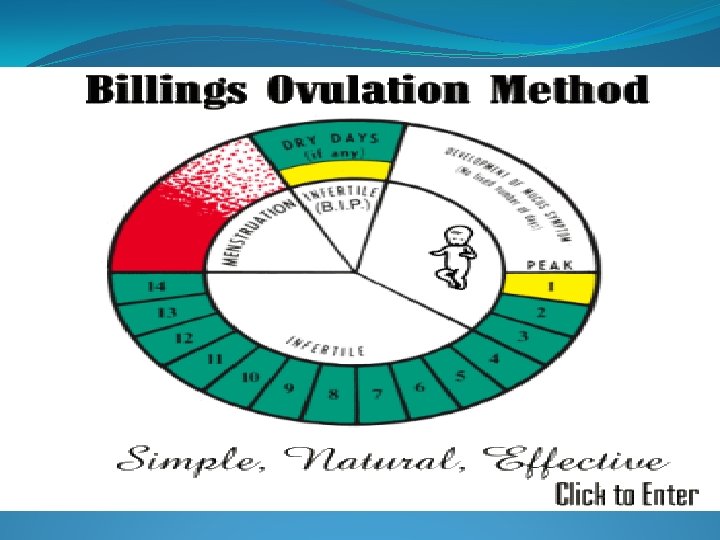
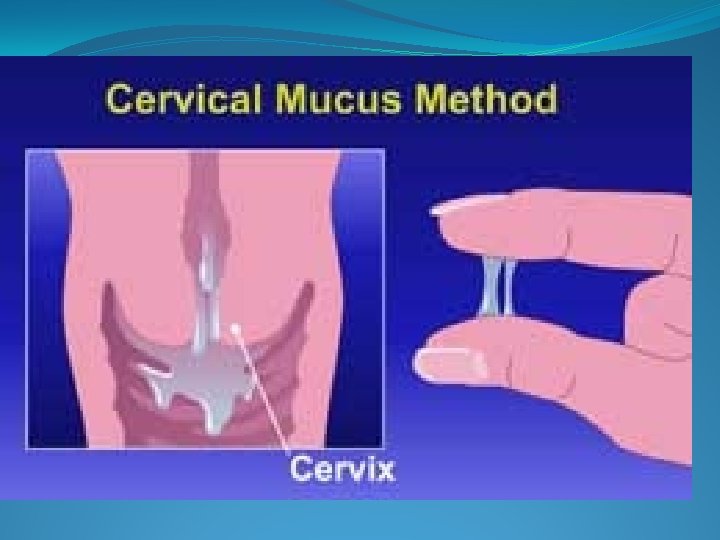
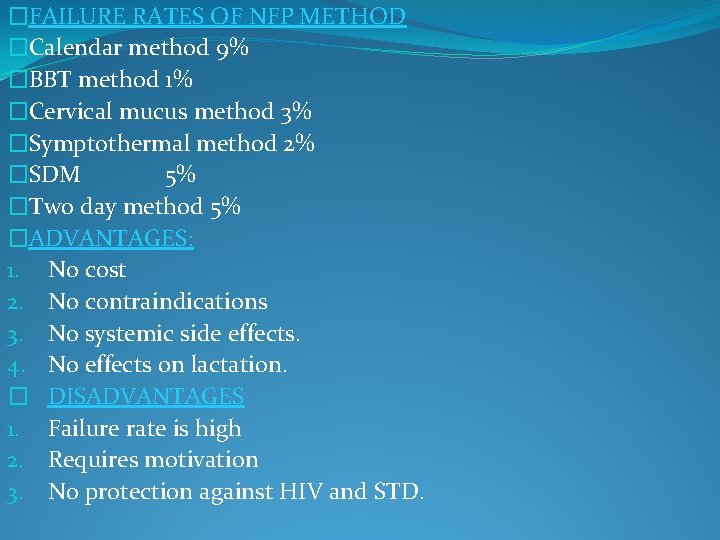
�Cervical mucus method/Ovulationmethod/ BILLINGS METHOD �PRINCIPLE: Changes in the cervical mucus is due to oestrogen and progesterone. �Due to oestrogen mucus appear profuse slippery discharge. �Progesterone produces scanty and thick mucus. �Inter course can be practiced during mensturation and alternate days following mensturation ie during the dry days. The couple should abstain as soon as the first mucus appears in the pre ovulatory phase and during the wet days in the ovulatory phase days)and 3 days after the peak mucus day. (last day of the wet mucus is called the peak day). �This method is un suitable for those with abnormal white discharge.
�SYMPTO THERMAL METHOD �Observation of the basal body temperature, cervical mucus changes, and the manifestations of the fertile period such as the mid cycle pain , mid cycle light spotting breast tenderness. �Noted in the sympto thermal chart. �The practice of the inter course is same as that Billings method. �STANDARD DAY METHODS �By using cycle beads(string of colour coded beads that represent a woman's menstural cycle) � 1 day black thread across the red bead /every day one bead will be added/when the ring is on the brown beads pregnancy is unlikely/white beads chance to become pregnant �It also helps to calculate the length of her cycle �If she gets period before moving to the brown beads her cycle is less than 26 days. �If moves to the last baeds then also period has not yet started her cycle is longer than 32 days.
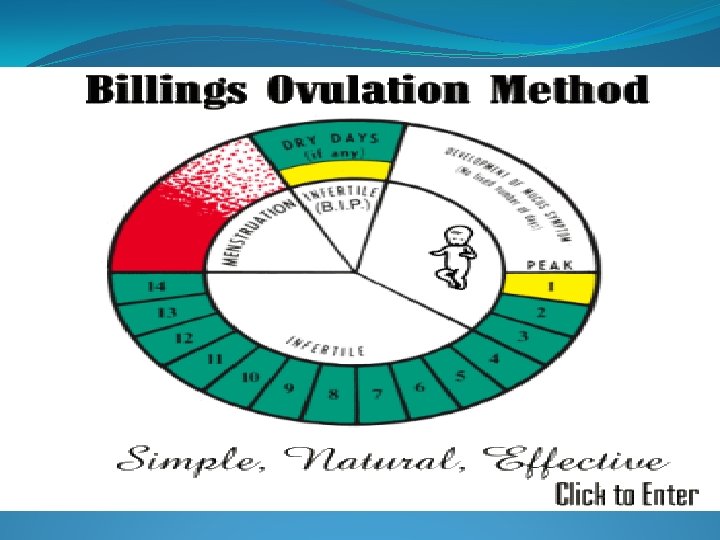
�FAILURE RATES OF NFP METHOD �Calendar method 9% �BBT method 1% �Cervical mucus method 3% �Symptothermal method 2% �SDM 5% �Two day method 5% �ADVANTAGES: 1. No cost 2. No contraindications 3. No systemic side effects. 4. No effects on lactation. � DISADVANTAGES 1. Failure rate is high 2. Requires motivation 3. No protection against HIV and STD.


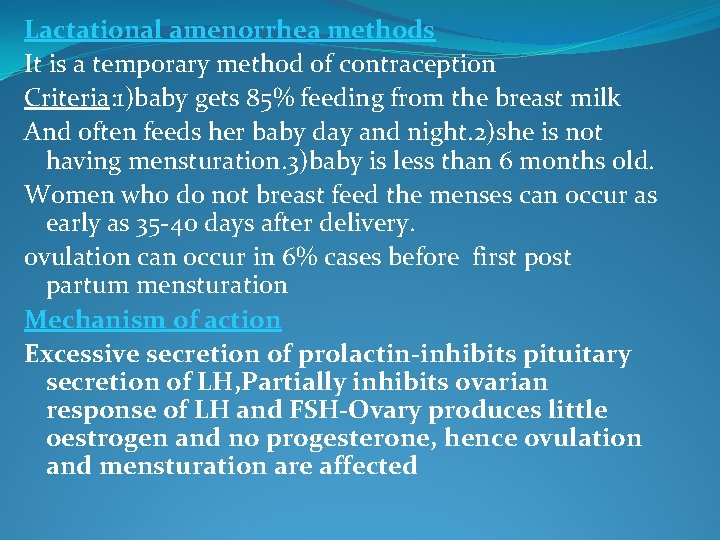
Lactational amenorrhea methods It is a temporary method of contraception Criteria: 1)baby gets 85% feeding from the breast milk And often feeds her baby day and night. 2)she is not having mensturation. 3)baby is less than 6 months old. Women who do not breast feed the menses can occur as early as 35 -40 days after delivery. ovulation can occur in 6% cases before first post partum mensturation Mechanism of action Excessive secretion of prolactin-inhibits pituitary secretion of LH, Partially inhibits ovarian response of LH and FSH-Ovary produces little oestrogen and no progesterone, hence ovulation and mensturation are affected
�ANTIINFERTILITY EFFECTS OF PROLACTl. N �Anovulatory cycles with short luteal cycles, impaired luteal competence, interference with implantation. �Either due to itself or due to suckling induced oxytocin release. �ABSOLUTE CONTRA INDICATION �cannot fully breast fed the baby �Menstruation starts(bleeding for atleast 2 days after 8 weeks of child birth) �Mother treated with mood altering drugs �Viral hepatitis of the mother �Mother has HIV/AIDS �DRAWBACK �Super involution of the uterus �Persistent hyper prolactinemia �Prolonged amenorrhoea/oligo
Failure rate-0. 5 -1. 5 % Advantages-Effectively prevents pregnancy -No hormonal side effects Disadvantages-Inconvenient to working mothers -No protection against STD’S WITHDRAWAL METHODS/COITUS INTERRUPTUS Coitus takes place in the normal manner but penis is withdrawn before the ejaculation Failure rate is 25 per 100 women years
BARRIER CONTRACEPTIVES Acts as barriers which prevent union of sperms and ovum TYPES 1. Condoms 2. Occlusive caps 3. Vaginal sponge 4. Spermicides 5. Female condoms
1. CONDOMS �Types-Fine latex rubber Circular cylinders, 15 -20 cm in length, 3 -3. 5 cm diameter, 0. 003 -0. 007 cm thickness, closed at one end and open at the other end with a rim �Available in dry ; semidry ; prelubricated forms. �Spermicidal condoms are coated with nonoxynol-9 both inner and the outer surfaces. In India dry condoms manufactured and supplied free of cost under the brand name NIRODH. �Non latex condoms. �Made of poly urethane. �Longer shelf life and can be used with oil lubricants which damages latex condoms. �Average life span is 5 years from the date of manufacturer.
�Advantages �Protection against STDS and AIDS �Following vasectomy for 12 ejaculates �Immunologic infertility in males �In later months of pregnancy protect against amniotic fluid infections. �When used more than 5 years reduces the chance of cervical dysplasia and cervical cancer �Disadvantages �Hyper sensitization �Severe allergy to the latex �Ultra thin condoms prone for breakage Failure rate is 10 -14 per HWY due to bursting or slipping or due to compliance.
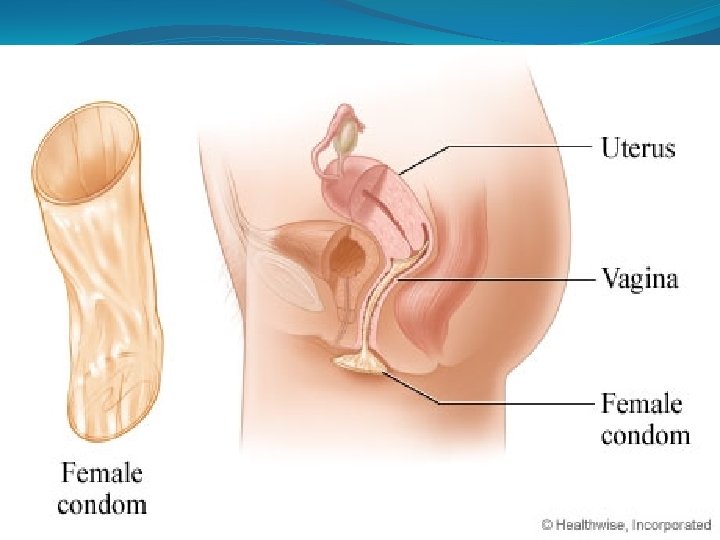
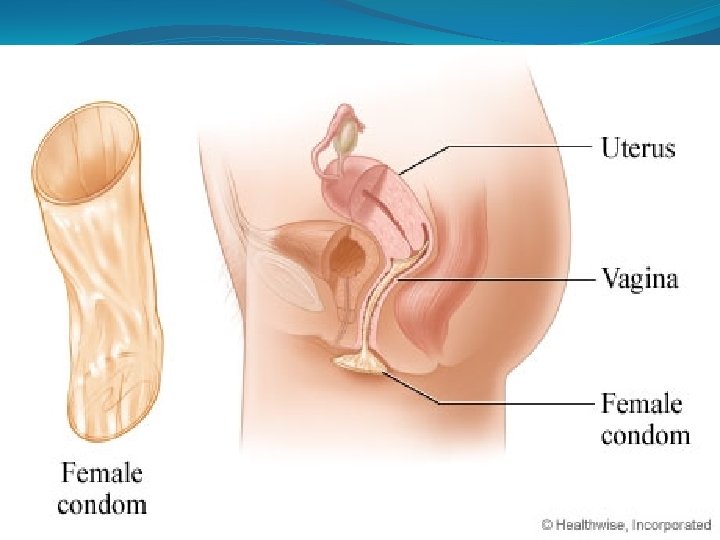
FEMALE CONDOM Soft loose fitting polyurethane sac-15 cm long and 7 cm diameter lubricated with silicone based lubricant (DIAMETHICONE). It is a woman controlled method. Advantages It is a woman controlled method It prevent STDS and HIV It is not damaged by oils and chemicals. Disadvantages Needs high motivation Intercourse is noisy and slippage can occur It is expensive method. Failure rate-21%
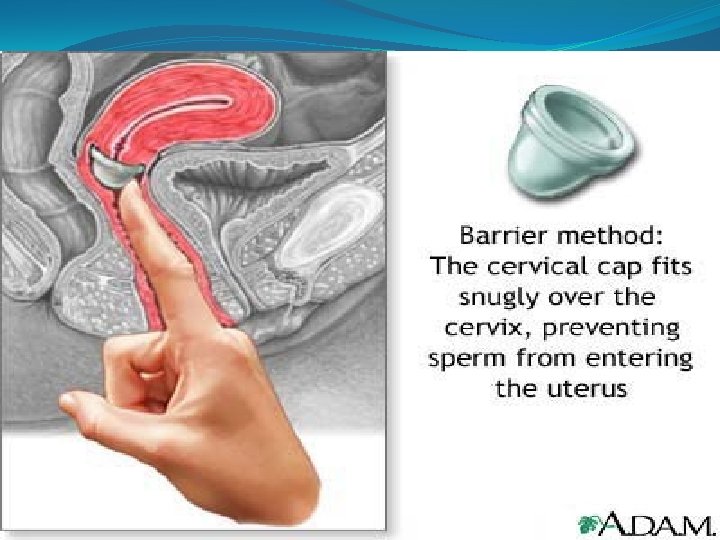
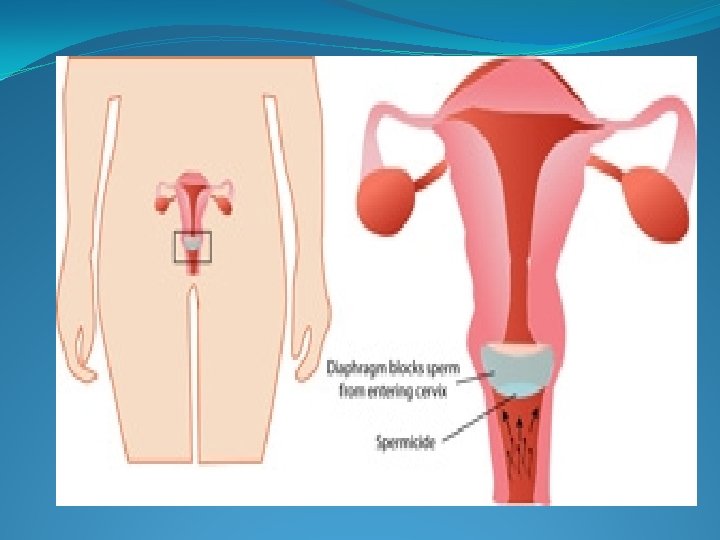
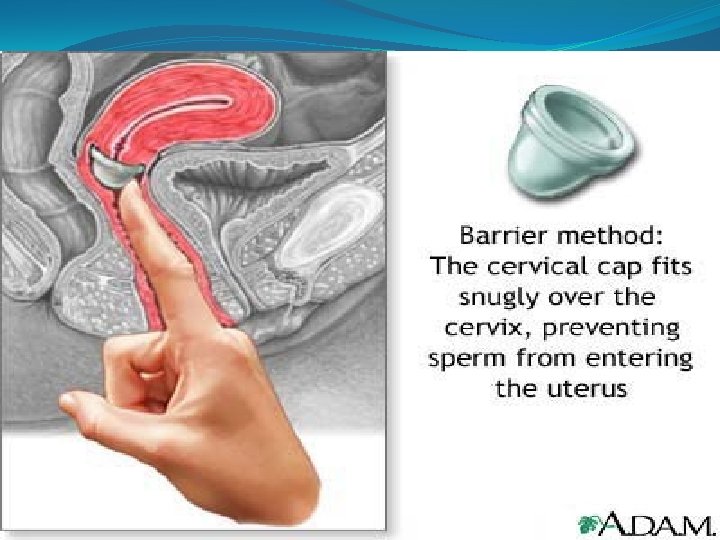
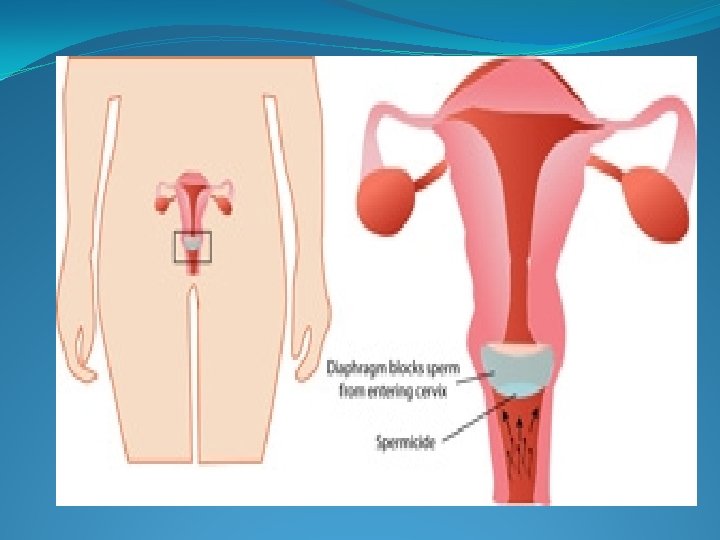
�OCCLUSIVE CAPS �These provide barrier in the vagina against direct insemination. �This is effective when used along with the spermicides. �TYPES �Dutch cap/diaphragm �Cervical cap �Vault cap �Vinule cap
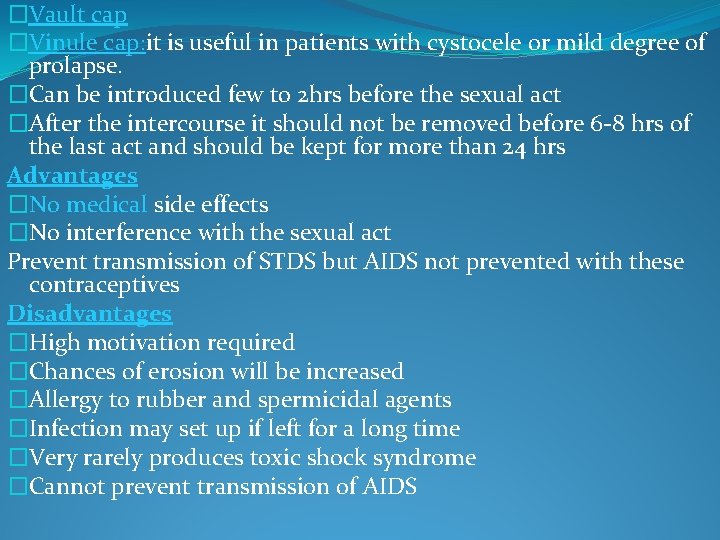
�Dutch cap/diaphragm �It is easiest type of cap for use �It fits obliquely just behind the pubic symphysis to the posterior fornix and covers the cervix �It is held in position by the tension of the metal spring. �Contra indications for diaphragm �Prolapse/cystocele/rectocele/ �Recurrent urinary tract infections �allergy to rubber or spermicidal agents Failure rate is 4 per HWY Cervical cap/ check pessary Thimble/dome shaped held in position by the suction Contra indications Chronic cervicitis, cervical erosion, cervical lacerations In a woman with prolapse of uterus or vagina this is preffered to diaphragm
�Vault cap �Vinule cap: it is useful in patients with cystocele or mild degree of prolapse. �Can be introduced few to 2 hrs before the sexual act �After the intercourse it should not be removed before 6 -8 hrs of the last act and should be kept for more than 24 hrs Advantages �No medical side effects �No interference with the sexual act Prevent transmission of STDS but AIDS not prevented with these contraceptives Disadvantages �High motivation required �Chances of erosion will be increased �Allergy to rubber and spermicidal agents �Infection may set up if left for a long time �Very rarely produces toxic shock syndrome �Cannot prevent transmission of AIDS
![VAGINAL SPONGETODAY Soft disposable foam sponge made of polyurethane saturated with Nanoxynol9 Attached with VAGINAL SPONGE[TODAY] Soft disposable foam sponge made of polyurethane, saturated with Nanoxynol-9 Attached with](https://slidetodoc.com/presentation_image_h/7efeb3ac45350115e9f101c1a4c4c157/image-31.jpg)
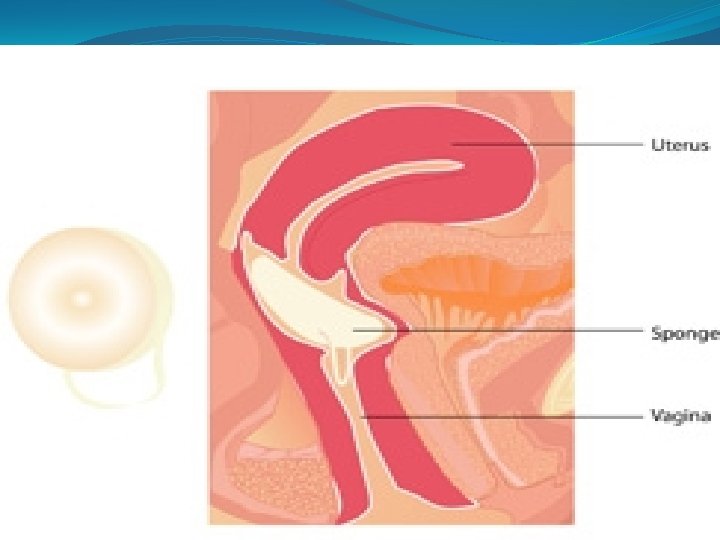
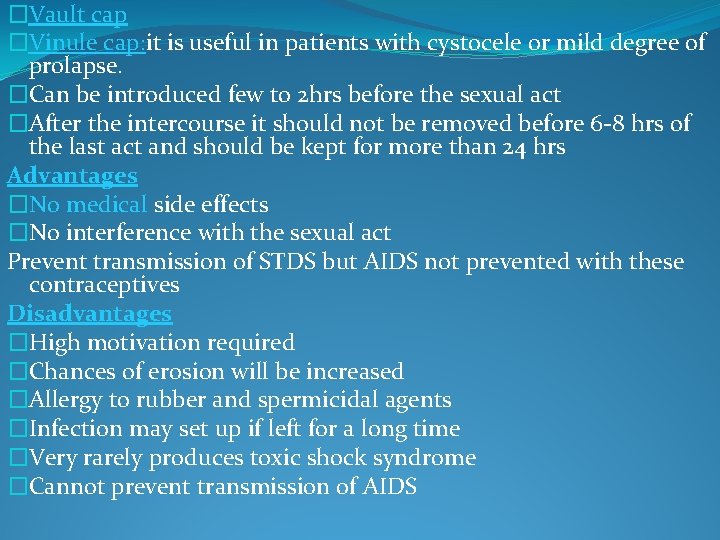
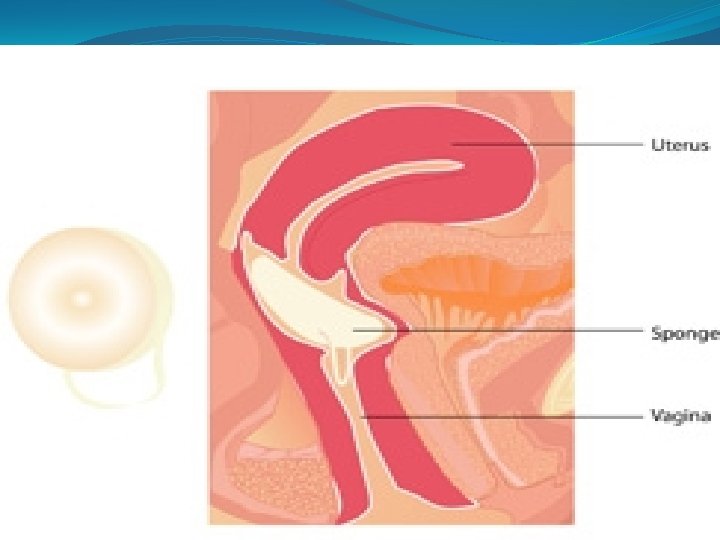
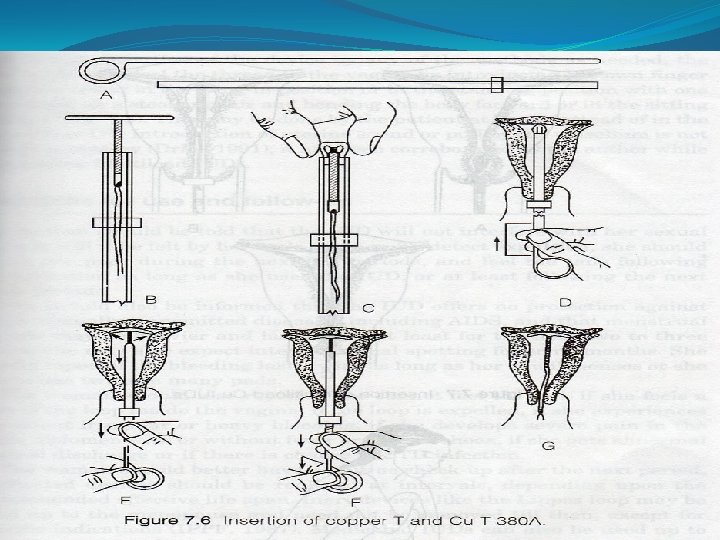
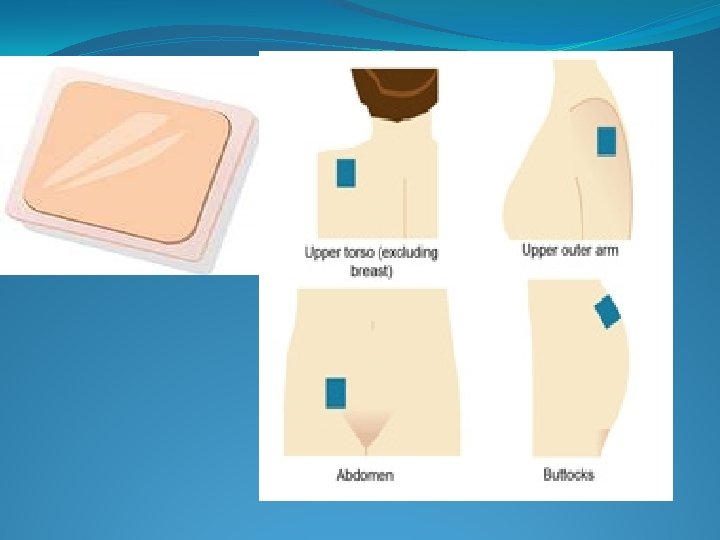
VAGINAL SPONGE[TODAY] Soft disposable foam sponge made of polyurethane, saturated with Nanoxynol-9 Attached with nylon loop Effective for 24 hrsit must be removed and thrown away after 8 -24 hrs and not before 6 hrs Disadvantage-High pregnancy rate -Toxic Shock Syndrome Allergic reactions/vaginal dryness/soreness/damage vaginal epithelium and cause transmission of HIV SPERMICIDES Non ionic surfactants which alters sperm surface membrane permeability Contains Nonoxynol-9 Used to improve contraceptive effect of barrier method
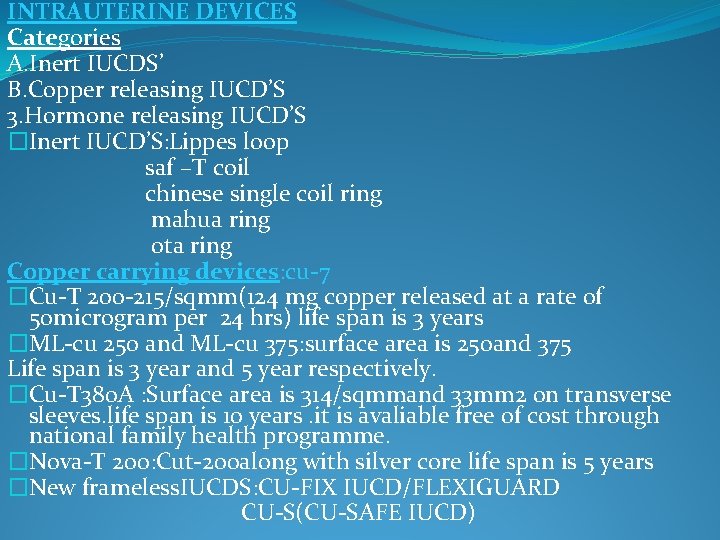
Types 1. Chemical suppositories 2. Contraceptive creams and jellies 3. Foam tablets 4. Aerosols or Foams 5. C-Films FAILURE RATE-21%
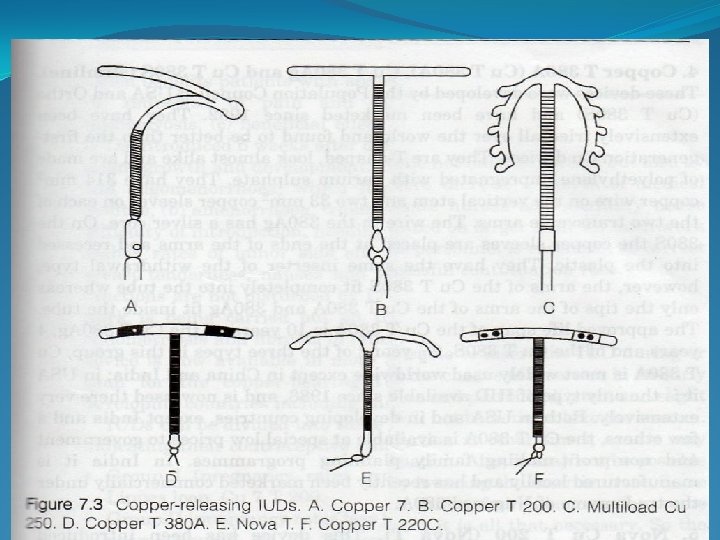
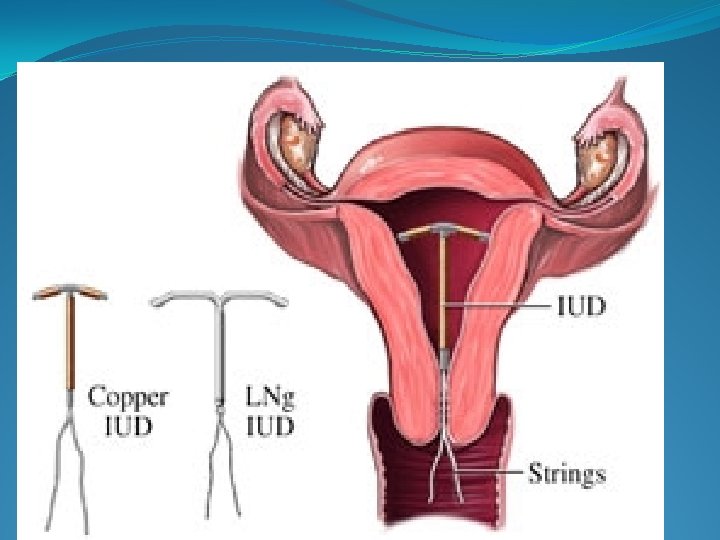
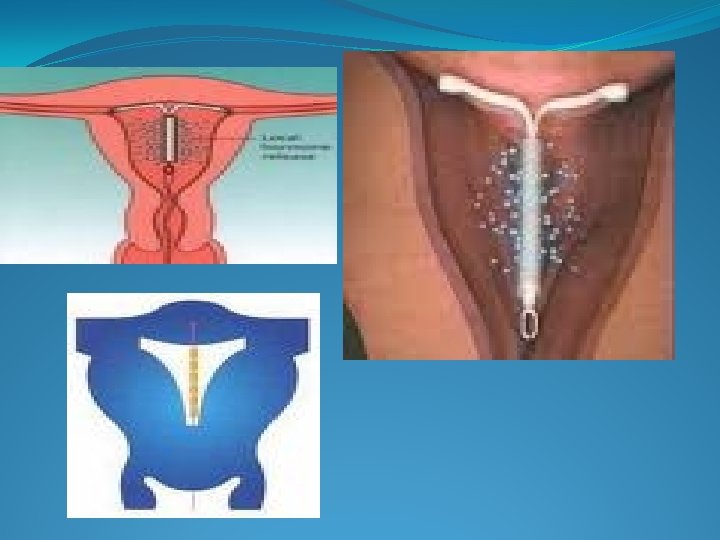
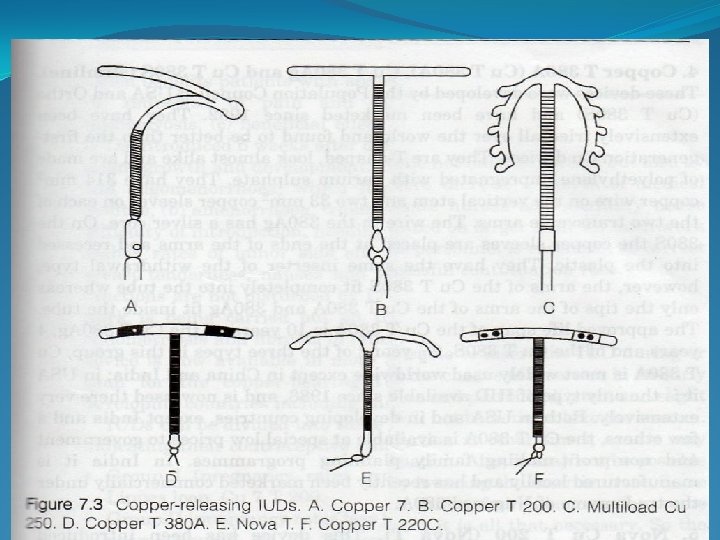
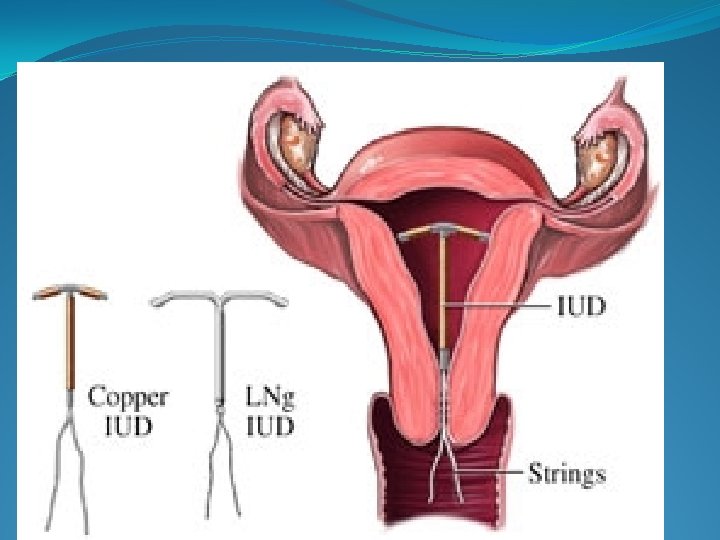
INTRAUTERINE DEVICES Categories A. Inert IUCDS’ B. Copper releasing IUCD’S 3. Hormone releasing IUCD’S �Inert IUCD’S: Lippes loop saf –T coil chinese single coil ring mahua ring ota ring Copper carrying devices: cu-7 �Cu-T 200 -215/sqmm(124 mg copper released at a rate of 50 microgram per 24 hrs) life span is 3 years �ML-cu 250 and ML-cu 375: surface area is 250 and 375 Life span is 3 year and 5 year respectively. �Cu-T 380 A : Surface area is 314/sqmmand 33 mm 2 on transverse sleeves. life span is 10 years. it is avaliable free of cost through national family health programme. �Nova-T 200: Cut-200 along with silver core life span is 5 years �New frameless. IUCDS: CU-FIX IUCD/FLEXIGUARD CU-S(CU-SAFE IUCD)
�Intra uterine devices �They are divided into three groups according to the pregnancy rates �Group I: pregnancy rates more than 2 per 100 women years(lippes loop, CU 7 T 200) �Group II pregnancy rates less than 2 but more than 1 per 100 women years. Nova-T, MLCu-250, Cu-T 220 C �Group III pregnancy rates less than 1 per 100 women years. Cu-T 380 A, Cu. T 380 S, ML Cu-375, LNG 20
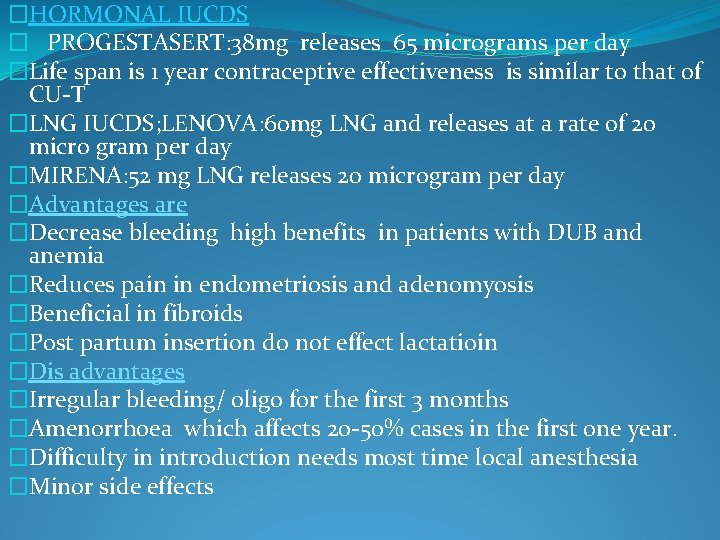
�HORMONAL IUCDS � PROGESTASERT: 38 mg releases 65 micrograms per day �Life span is 1 year contraceptive effectiveness is similar to that of CU-T �LNG IUCDS; LENOVA: 60 mg LNG and releases at a rate of 20 micro gram per day �MIRENA: 52 mg LNG releases 20 microgram per day �Advantages are �Decrease bleeding high benefits in patients with DUB and anemia �Reduces pain in endometriosis and adenomyosis �Beneficial in fibroids �Post partum insertion do not effect lactatioin �Dis advantages �Irregular bleeding/ oligo for the first 3 months �Amenorrhoea which affects 20 -50% cases in the first one year. �Difficulty in introduction needs most time local anesthesia �Minor side effects
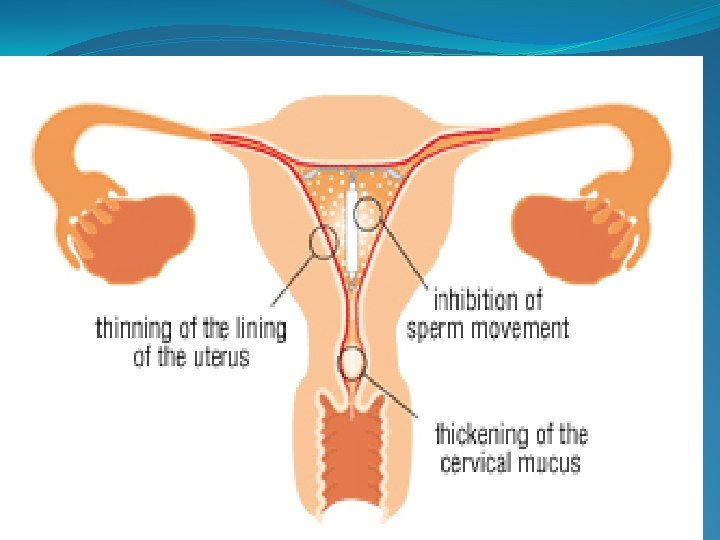
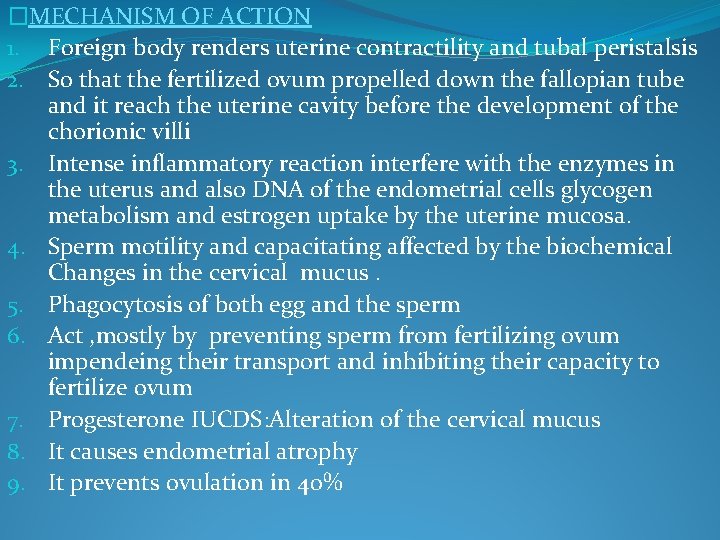
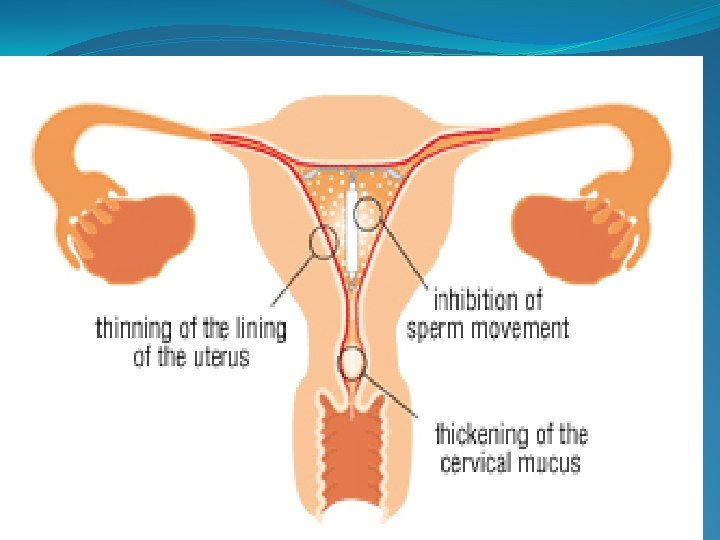
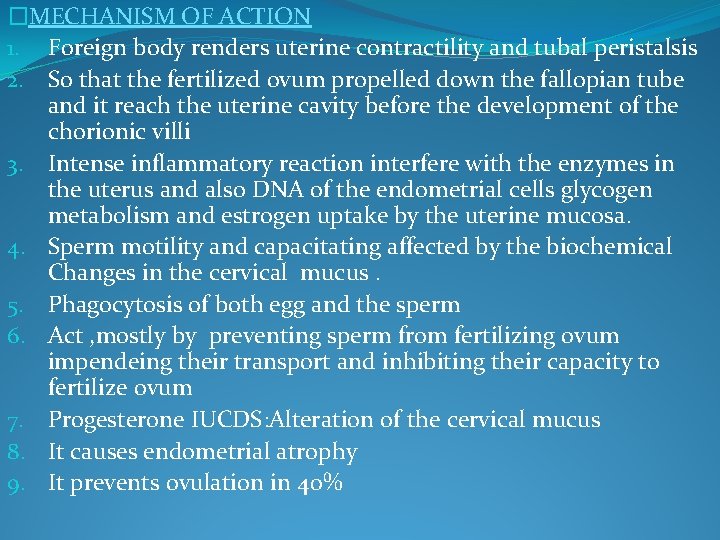
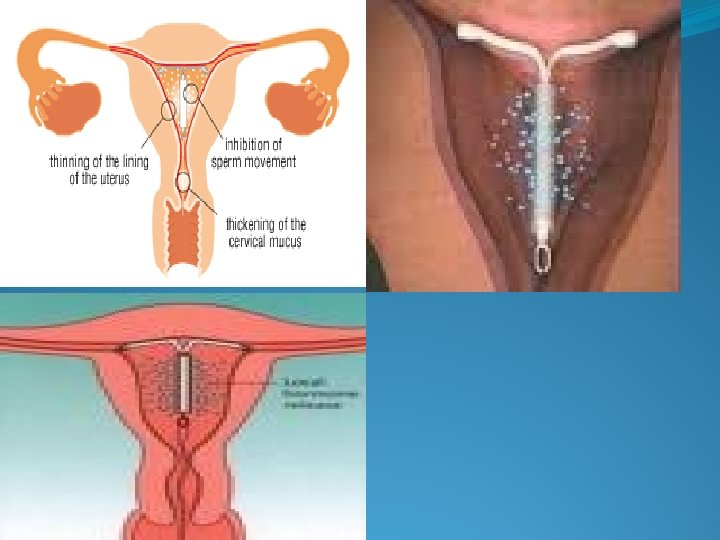
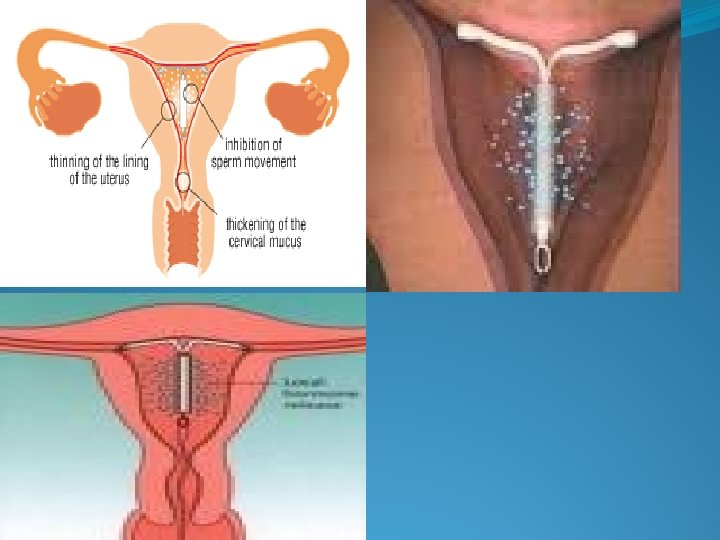
�MECHANISM OF ACTION 1. Foreign body renders uterine contractility and tubal peristalsis 2. So that the fertilized ovum propelled down the fallopian tube and it reach the uterine cavity before the development of the chorionic villi 3. Intense inflammatory reaction interfere with the enzymes in the uterus and also DNA of the endometrial cells glycogen metabolism and estrogen uptake by the uterine mucosa. 4. Sperm motility and capacitating affected by the biochemical Changes in the cervical mucus. 5. Phagocytosis of both egg and the sperm 6. Act , mostly by preventing sperm from fertilizing ovum impendeing their transport and inhibiting their capacity to fertilize ovum 7. Progesterone IUCDS: Alteration of the cervical mucus 8. It causes endometrial atrophy 9. It prevents ovulation in 40%
�Patient selection �Low risk STDS �Monogamous relationship �Multiparous women �Long term reversible method required �Unreliable user of OCPS/barrier methods �Uses of IUCDS �Contraception �Emergency contraception �After excision of the uterine septum/ asherman syndrome �Hormonal IUCDS menorrhagia/DUB �CONTRINDICATIONS �Suspected pregnancy �Pelvic inflammatory disease �Fibroids �Diabetic women �Heart disease
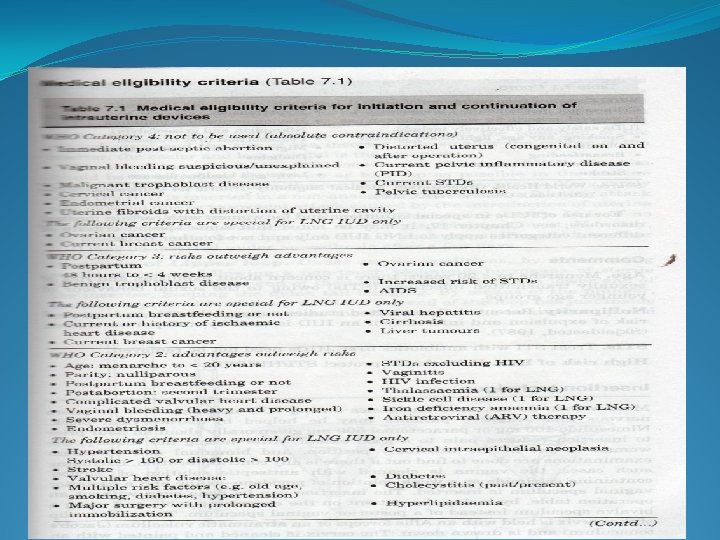
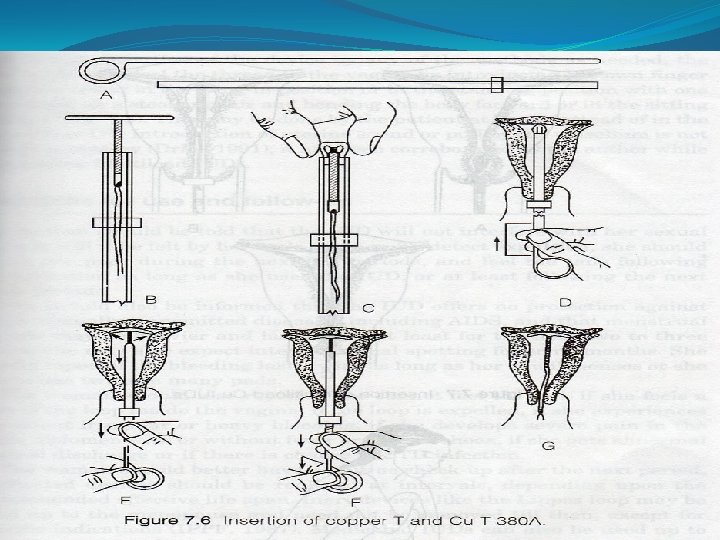
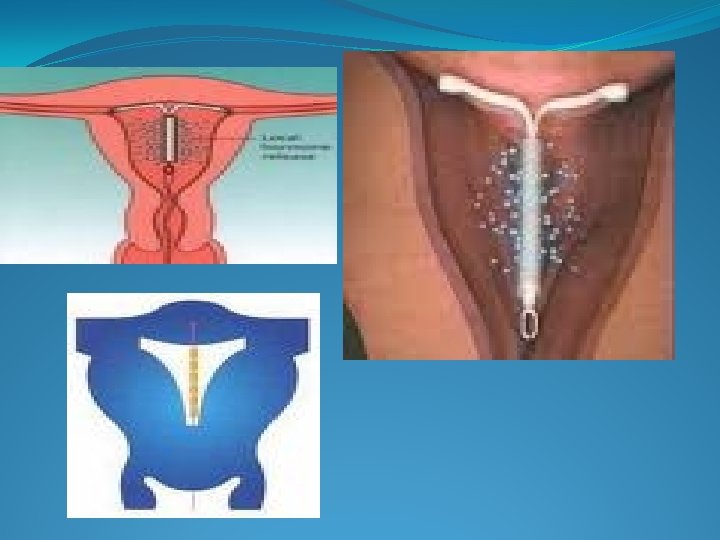
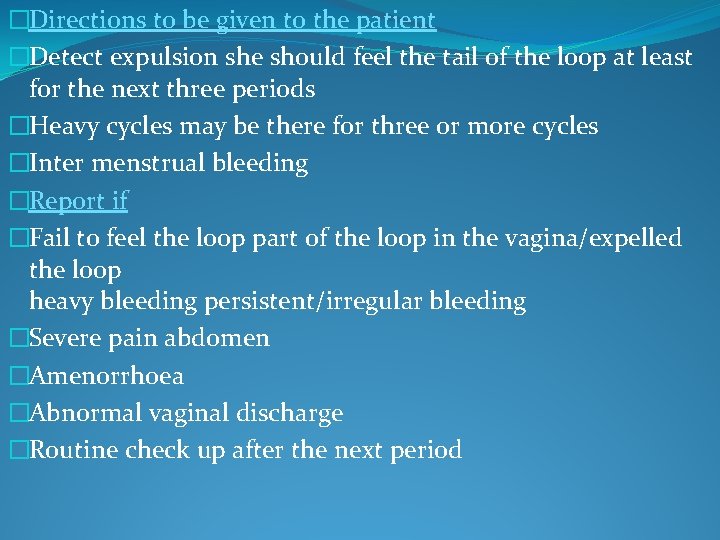
�Previous ectopic �scarred uterus �In nulliparous due to high risk of PID �LNG IUCD in breast cancer �Timing for insertion of IUCDS �Mensturation : soon after it �Post coital; emergency contraception up to 5 days. �Post abortal: following MTP/spontaneous abortion m/c after first trimester abortion but not after the second trimester. �Post partum: 6 weeks after the normal vaginal delivery and 12 months after the c section other wise high rate of expulsion. �Insertion of IUCDS
�Before insertion counsel the patient �Method is no touch technique �That is loading the IUCD into the inserter without opening the sterile packet �Not touch the speculum and the posterior vaginal wall �First do the pelvic examination �Inspect vagina and the cervix calculate the length of the uterine cavity with the uterine sound.
�Directions to be given to the patient �Detect expulsion she should feel the tail of the loop at least for the next three periods �Heavy cycles may be there for three or more cycles �Inter menstrual bleeding �Report if �Fail to feel the loop part of the loop in the vagina/expelled the loop heavy bleeding persistent/irregular bleeding �Severe pain abdomen �Amenorrhoea �Abnormal vaginal discharge �Routine check up after the next period
�Indications for removal �pelvic pain/cramping �Abnormal excessive persistent bleeding �Expiry of the effective life span. �Displacement of the devices either inside the uterus or outside �Menopause 1 year after �Uterine or cervical malignancy �Desire for pregnancy �Complications �Immediate: cramp like pain � syncopal attack � Partial or complete perforation �Remote : pain � abnormal menstural bleeding �Pelvic infection �Spontaneous expulsion �Perforation of the uterus
� Menstrual problem Increased bleeding: normal loss is 30 -40 ml Inert loss up to 70 -80 ml Cu-T 50 -60 ml Removal in about 2 -10/100 women years Due to increase in the plasminogen activating enzymes /increased vascularity/hormonal asynchronisation. Inter menstrual bleeding due to the damage to the endometrium Scanty bleed with LNG-20 � Pain Due to uterine cramp subsides in a week Persistent pelvic pain: PID/ectopic abnormal position perforation expulsion disparity between uterine size and IUCD Investigate and remove the IUCD
�Expulsion �Most common in the nulliparous women �, , lippes loop than with cu-t �Immediate post partum �Technical fault �High expulsion the first three months high during mensturation �MOA due to contraction of the uterus and disparity in the size �Cousel the patient to check the thread �Clinician should feel the thread with the uterine sound if the tail is not visible �Ski graph/usg if the tail is not felt in the uterus �If expelled it should be re inserted there is high chance for retainment
�Vaginal discharge due to foreign body reactions. � perforation �m/c seen at the time of insertion �m/c with the push out technique in lippes and cu-7 than with the withdrawal technique used in the cu-t �Clinical features �m/c asymptomatic �Sharp pain at the time of insertion �Disappearance of the tail �Post insertion bleeding �Cut transverse stem can perforate the cervix and can lie in the vagina and produce dysparuenia �In the peritoneal cavity �Can produce adhesions of omental mass �Progesterone can produce intra peritoneal bleeding �Plain x-ray/pelvic usg
hys teroscopy In the uterine cavity it can be removed with hysteroscope/curette/shirodkar hook Perforated laprotomy Infections m/c in nulliparous women High in first 20 days after insertion Infection introduced at the time off insertion Flaring up of un diagnosed infections Fresh STI Increase volume and duration of the cycle Doxycycline 200 mg/azithromycin 500 mg If within 24 hours no subsidence of the symtoms then remove iucd m/c infection is due to actinomycosis
�Pregnancy �Once confirmed IUCD should be removed to high chance of infections/miscarriage/pre term labor. �If thread not seen MTP advised as there is high chance of infections/leave it like that only and explain about the risk of continuation of pregnancy. �Pregnancy rate with LNG 0. 2/HWY and cu-T 380 A is 0. 8/HWY. �Ectopic pregnancy � 0. 25 -11. 5/HWY �IUCDS protect against uterine pregnancy but not against ectopic. �Increase incidence of the ovarian pregnancy with progesterone device. �As the action limited to the local effect on endometrium and cervical mucus.
�Advantages �Coital independent. �One time insertion long time effect. �No systemic side effects. �No adverse effect on lactation. �No decrease fertility after removal: 75% return within 1 month � 90% within 6 months. �Failure rate is 3% at the end of one year and 1% at the end of 5 years.
�Hormonal contraceptives �Oral pills: combined pills � progesterone only pills � post coital pill � once a month pill � male pill �Depot /slow release formulations �Injectables �Sub cutaneous implants �Vaginal rings �COMBINED ORAL PILLS � monophasic pills � multi phasic pills �It contains ethinyl estradiol/3 - methyl ester that is mestranol that is metabolised to ethinyl estradiol
�It also contains progestins they are the pro gestational agents that produce the secretory changes in the estrogen primed endometrium. �High progestational activity �norgesterel. >ethynodiol diacetate>norethisterone actate>nor ethisterone �Nor ethisterone group: nor ethisterone, ne acetate, ethyniodiol acetate, lynesterol �Pills containing this group are calleed first generation pills �Norgestrel group; activity due to levo form , high progestational activity and high androgenic activity �Pills containing called second generation pills � 19 nor testosterone derivative �Desogestrol, gestodene, norgestimate �No estrogenic activity, high progestational activity, high anti estrogenic action, anti ovulatory action, minimal androgenic action �These change protect against the CVS disease but venous thromboembolism high than other progestins.
�Spironolactone analogue �Anti androgenic action and anti mineralocorticoid action �EE 30 mcg along with DRSP 3 mg �YASMIN �CALLED THIRD GENERATION PILLS 1. MONOPHASIC PILL these pills contain estrogen and progesterone in they same amount in each pill They are divided into two groups Low dose pills containing EE less than 0. 05 mg Very low dose pills containing EE 0. 015 -0. 025 mg �MALA –D: D-NORGESTREL 0. 15 mg+EE 0. 03 mg �MALA-N : LNG 0. 15 mg+EE 0. 03 mg �NOVELON : DESOGESTREL 0. 15 mg+EE 0. 03 mg �Mala-N provided free of cost by the govt of India; �FEMILON: DESOGESTREL 0. 15 mg+EE 0. 02 mg �YASMIN; DROSPERINONE 3 mg+EE 0. 03 mg
�MULTI PHASIC) �These formulations employ low doses and variable amounts of estrogen and progesterone in two(biphasic) or three(triphasic) periods within the menstural cycle. �The dose of progesterone low in the beginning of the cycle and higher at the end and estrogen remains almost constant or rises slightly in the cycle. �BIPHASIC PILLS �EE 0. 035 mg+low dose progesterone for the first 10 days and higher dose of progesterone for the next 11 days �They have high failure rates and also not avaliable in a India �TRIPHASIC PILLS �EE 0. 03 mg+0. 05 mg L-Norgestrel for the first 6 days �EE 0. 03 mg+0. 075 mg LNG for the next 5 days �EE 0. 03 mg+0. 125 mg. LNG for the last 10 days �tota; l 0. 68 mg. EE and 1. 92 mg LNG �They can be administered easily to the individuals as they do not interfere with the carbohydrate and lipid metabolism
�MOA �Inhibition of ovulation �By suppressing the release of the gonadotrophic releasing hormones from the hypothalamus is prevented by the negative feed back mechanism. �No LH surge and release of FSH is also affected �Therefore follicular growth does not occur �Producing static endometrial hypoplasia �Stromal edema, decidual reaction and regression of the glands �Rendering unsuitable for implantation �Alteration of the character of the cervical mucus �Thick scanty and viscus interfere with the sperm penetration �Interfere with the motility and the secretions of the fallopian tube �Estrogen inhibit FSH rise and prevents follicular growth �Progestin an ovulatory effect by inhibiting LH surge �And also counteract the effects of estrogen on the endometrium
�Selection of the patient �History �General physical examination �Pelvic examination �Pregnancy must be excluded �How to use the pill �New users should begin their pill packet on the first day of their cycle �One tab is taken preferentially at the bed time for the consecutive 21 days and there is 7 days break �Next pack should be started on the 8 day irrespective of the bleeding �Woman can also start the pill on the 5 day o their cycle but that should use a condom for the 7 days �The pill can be started on the day of abortion �In the non lactating women it can be taken after 3 weeks �In lactating they are with held fore 6 months
�Follow up �Patient should be examined every 3 months then every 6 months and then yearly �The patient aged above 35 years should be examined very frequently �Missed pills �Normally there is the return of the pitutary and the ovarian function during the pill free interval �Lengthening of the PFI due to omissions malabsorption, or vomiting at the beginning or at the end of the packet increases the break through ovulation and the chance for pregnancy �Management if the women forgets to take the one pill she should take the pill at once and continue the rest of the schedule �When misses 2 pills in the first 7 days she should take 2 pill one each of the next 2 days and then continue the rest of the schedule �If 2 pills are missed in the third week if more than 2 pills are missed at any time of the cycle then another form of contraception should be started

�Additional contraception �When broad spectrum antibiotics like ampicillin amoxicillin, tetracycline , doxycycline used as they impair the absorption of EE. �When enzyme inducing drugs are used high dose pills to be used. � interfere with the metabolism �Indications for the withdrawal �Severe migraine �Visual and speech disturbances �Sudden chest pain �Un explained fainting attack �Excessive weight gain �Severe depression �Patients under going surgery it should be with held for 6 weeks
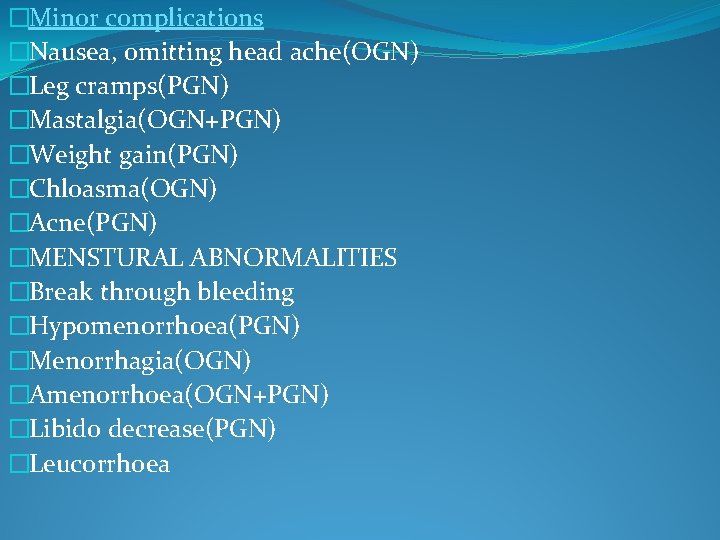
�Benefits of C OCPs �Contraceptive benefits �Protection against the unwanted pregnancy(failure rate is 0. 1/100 women years) �Not intercourse related �Reversibility �Improving maternal and child health �Non contraceptive benefits �Improvement of menstural abnormalities �Protection against health disorders �PID, ectopic pregnancy, endometriosis, fibroid uterus, hirsutism, acne, functional ovarian cysts, benign breast disease, osteopenia, auto immune disorders of thyroid, rhuematoid arthritis �Prevention of , malignancies: endometrial cancer(50%). ovarian cancer(40%), colorectal cancer(40%)
�Minor complications �Nausea, omitting head ache(OGN) �Leg cramps(PGN) �Mastalgia(OGN+PGN) �Weight gain(PGN) �Chloasma(OGN) �Acne(PGN) �MENSTURAL ABNORMALITIES �Break through bleeding �Hypomenorrhoea(PGN) �Menorrhagia(OGN) �Amenorrhoea(OGN+PGN) �Libido decrease(PGN) �Leucorrhoea
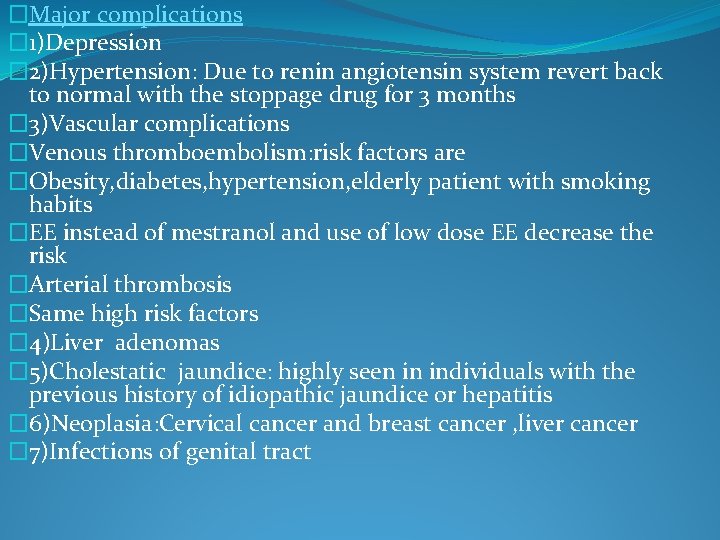
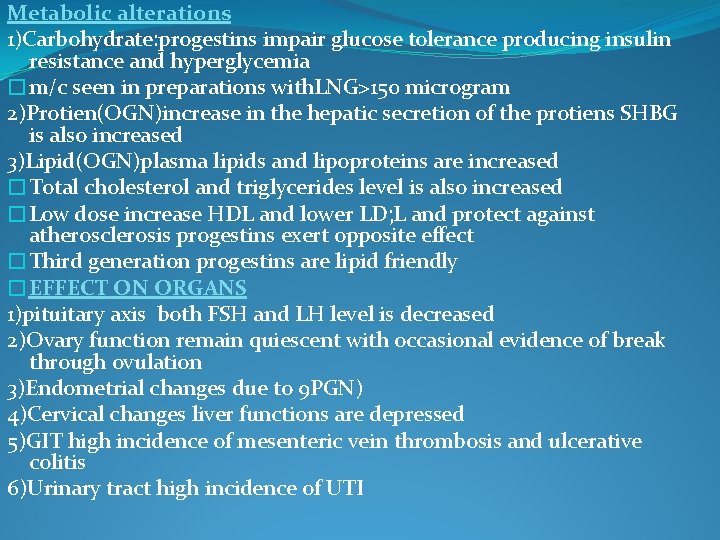
�Major complications � 1)Depression � 2)Hypertension: Due to renin angiotensin system revert back to normal with the stoppage drug for 3 months � 3)Vascular complications �Venous thromboembolism: risk factors are �Obesity, diabetes, hypertension, elderly patient with smoking habits �EE instead of mestranol and use of low dose EE decrease the risk �Arterial thrombosis �Same high risk factors � 4)Liver adenomas � 5)Cholestatic jaundice: highly seen in individuals with the previous history of idiopathic jaundice or hepatitis � 6)Neoplasia: Cervical cancer and breast cancer , liver cancer � 7)Infections of genital tract
Metabolic alterations 1)Carbohydrate: progestins impair glucose tolerance producing insulin resistance and hyperglycemia �m/c seen in preparations with. LNG>150 microgram 2)Protien(OGN)increase in the hepatic secretion of the protiens SHBG is also increased 3)Lipid(OGN)plasma lipids and lipoproteins are increased �Total cholesterol and triglycerides level is also increased �Low dose increase HDL and lower LD; L and protect against atherosclerosis progestins exert opposite effect �Third generation progestins are lipid friendly �EFFECT ON ORGANS 1)pituitary axis both FSH and LH level is decreased 2)Ovary function remain quiescent with occasional evidence of break through ovulation 3)Endometrial changes due to 9 PGN) 4)Cervical changes liver functions are depressed 5)GIT high incidence of mesenteric vein thrombosis and ulcerative colitis 6)Urinary tract high incidence of UTI
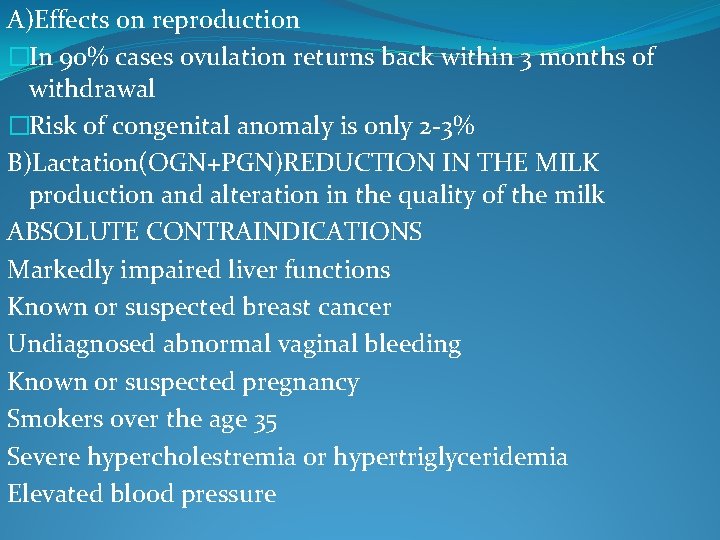
A)Effects on reproduction �In 90% cases ovulation returns back within 3 months of withdrawal �Risk of congenital anomaly is only 2 -3% B)Lactation(OGN+PGN)REDUCTION IN THE MILK production and alteration in the quality of the milk ABSOLUTE CONTRAINDICATIONS Markedly impaired liver functions Known or suspected breast cancer Undiagnosed abnormal vaginal bleeding Known or suspected pregnancy Smokers over the age 35 Severe hypercholestremia or hypertriglyceridemia Elevated blood pressure
�Relative contraindications �Migraine �Hypertension �Uterine lieomyoma �Gestational diabetes �Diabetes mellitus �Seizure disorder �Obstructive jaundice in pregnancy �Sickle cell disease �Gall bladder disease �MVP �SLE Smoking Hepatic disease
Progestin only contraception Progesterone only pills �Contains only progesterone and no estrogen �Compositions –Nor etindrone 0. 350 mg-(micronovar) �LNG 0. 075 mg (Neogest) �Norgesterl 0. 030 mg (Microoval/Norgeston) �Ethynidiol diacetate 0. 500 mg (Femuleon) �Desogestrel (zerogen) �MOA-thickening of the mucus plug �Effects starts 2 -4 hours and last for 20 -24 hrs �Involution of the endometrium �Administration � 6 weeks after the delivery �Should be started within 5 days of the cycle �It should be taken at the same time every day �Minipill taken 3 hrs later back up method is used for 48 hrs
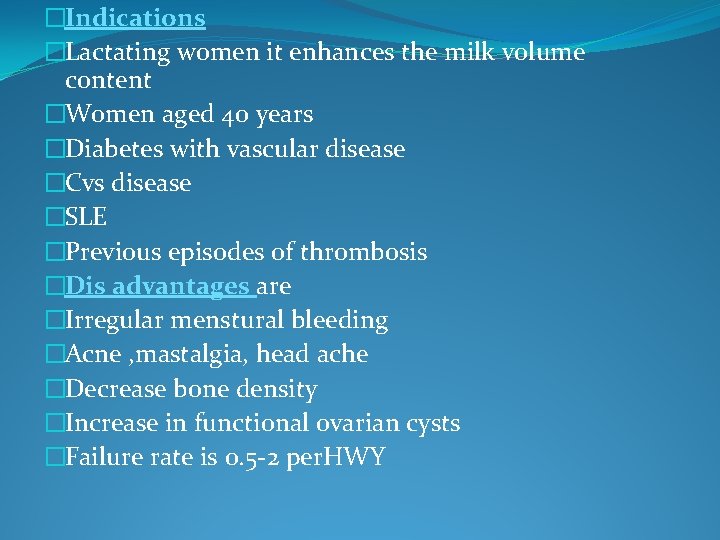
�Indications �Lactating women it enhances the milk volume content �Women aged 40 years �Diabetes with vascular disease �Cvs disease �SLE �Previous episodes of thrombosis �Dis advantages are �Irregular menstural bleeding �Acne , mastalgia, head ache �Decrease bone density �Increase in functional ovarian cysts �Failure rate is 0. 5 -2 per. HWY
�Centchroman �Non hormonal chemically synthetic once a week oral contraceptive. �Saheli (centchroman) contains 30 mg �Recommended dose is one tabtwice weekly starting from the first day of the menses for the first 3 months and then once a week irrespective of mensturation. �Weak estrogenic and potent anti estrogenic action, acting mostly on the endometrium there by interfering with the nidation of the embryo. �It has no progestational androgenic or anti androgenic actions. �Continous use ocps �Seasonale : contains 0. 15 mg LNG and 0. 03 mg EE women take pill every day for 84 days and then hormone free pills for 7 days �This results in 4 withdrawal bleed per year than 12 It decrases the migraine mood changes heavy painful beeding with the OCPS
�RU-486/MIFEPRISTONE �Anti progesterone compound which prevents hormone action at the receptor level. �Given orally in the mid cycle can inhibit mid cycle LSH surge. �In the late luteal phase can cause menstruation

�PROGESTOGEN ONLY CONTRACEPTIVE INJ �Depot medroxy progesterone acetate: �Prepared in the micro crystalline suspension that delays the absorption of the hormone after an injection administered in 150 mg once in every 3 months± 14 days. �Norethisterone enanthate �NET-EN/noristerat, used as oily solution � 200 mg every 2 months± 14 days. �Effectiveness depends on the �Timing of the injection �Injection technique �Regularity of the inj at proper intervals
�Advantages �No need of regular medications as that of oral pills �Can be used safely in lactation �No estrogen related side effects �Menstrual symptoms decreases �Protective against endometrial cancer �Interim contraception before vasectomy �Decrease PID, endometriosis, ectopic and ovarian ca �DMPA prevents sickling best in sickle cell anemia �Best in seizure dis order �Disadvantages �Irregular menstrual bleeding �Weight gain �Impaired glucose tolerance �Delay in return of fertility it takes 5. 6 months in comparison to 3 months with that of ocp �High chance of invasive ca cervix DMPA>5 years �Bone density changes
�Combined injectables �It contains long acting progestins and short acting estrogen �DMPA 25 mg+Esradiolcypionate 5 mg(cyclofem) �NET-EN 50 mg+estradiolvalerate 5 mg(mesigna) �Absolute contraindications �Breast feeding within 6 weeks �Confirmed or suspected pregnancy �Ca breast or liver �Past or present thrombo embolism, heat disease or stroke �HTN>160/100 mmhg �Migraine with aura �Complicated diabetes �New DMPA S. C injections �Injected under the skin � 104 mg DMPA � 3 months interval �Upper thigh and abdomen
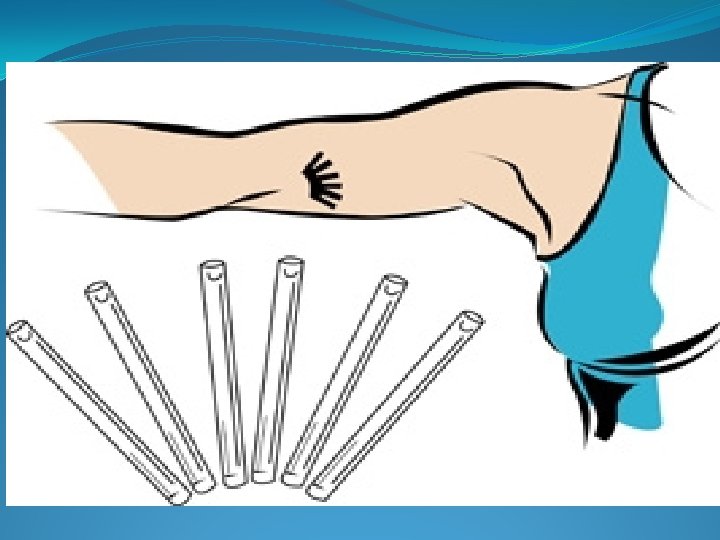
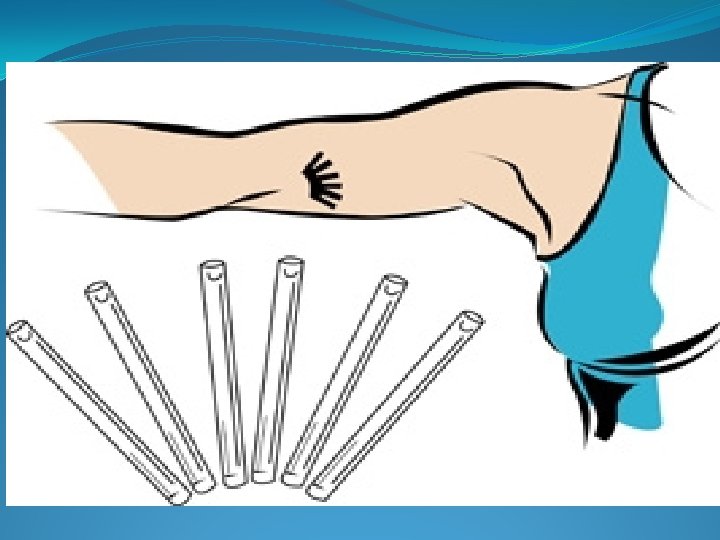
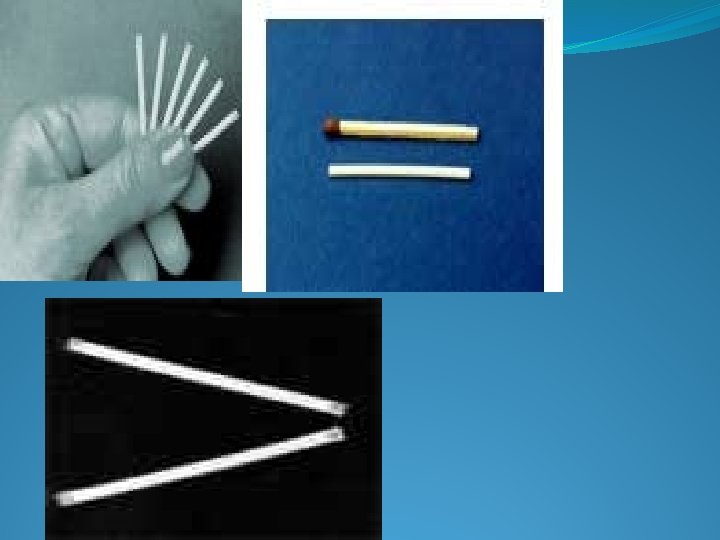
�Implants �Failure rate is 0. 2/ HWY �NORPLANT : 6 sialistic cap LNG(36 mg) life span 5 years. Initially releases 85 micro gram and later 30 microgram �Norplant. II /JADELLE : 2 sialistic cap LNG(70 mg/rod)30 microgram/day life span 3 years �UNIPLANT 1 : sialistic norgesterol 55 mg with release of about 100 microgram per day. life span 1 year �ST 1435: 1 sialistic cap nestirone life span 2 years �Implanon : ethinyl vinyl acetate contains 68 mg 3 ketodeogesterl , life span 3 years, intially releases 67 microgram then reduces to 30 micro gram per day �Biodegradable implants : capronor single capsule releases LNG from the polymer E-caprolactone at a rate 10 times faster than the silastic the longer cap contains 26 mg LNG and inhibits ovulation in 50%. contraceptive efficiency similar to that of NORPLANT. it starts to disappear within 12 months
�Capsules are inserted subdermally in the inner aspect of the non dominant arm. 6 -8 cm above the elbow fold. it is done under local anesthesia. it is ideally inserted immediately after abortion , on the first day of mensturation, three weeks after post partum Advantage Highly effective individuals requiring long term use Who completed the family and do not want permanent contraception Women who have contraindications for estrogen contraceptives Intend to breast feed Disadvantages Surgical procedure Menstrual irregularity Weight gain Acne and breast tenderness Functional ovarian cyst Head ache and mood changes No protection against sexually transmitted diseases
�CONTRAINDICATIONS �Active thrombophlebitis/thromboembolism �Undiagnosed genital bleeding �Active liver disease �Benign or malignant liver tumors �Known or suspected breast cancer
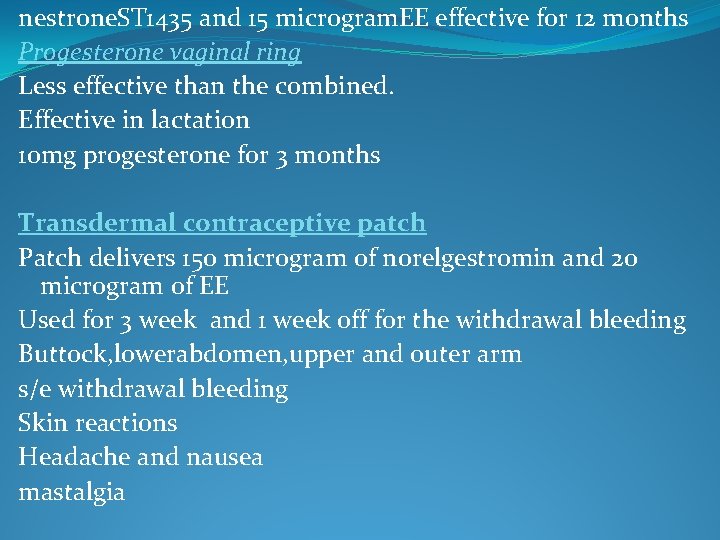
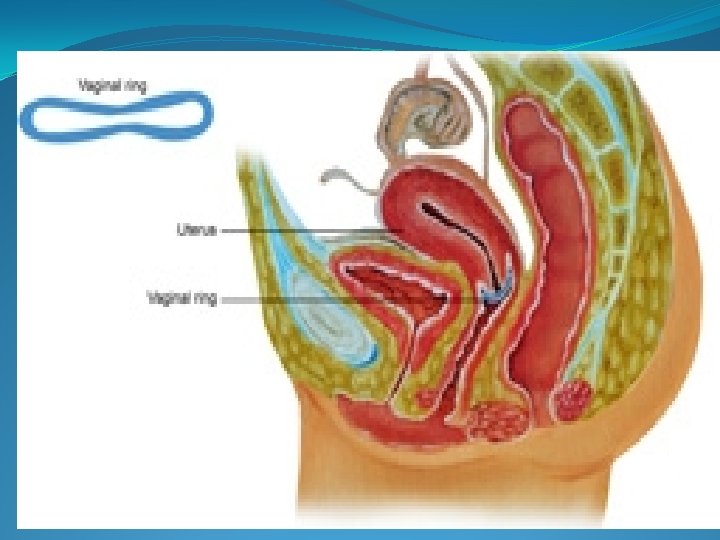
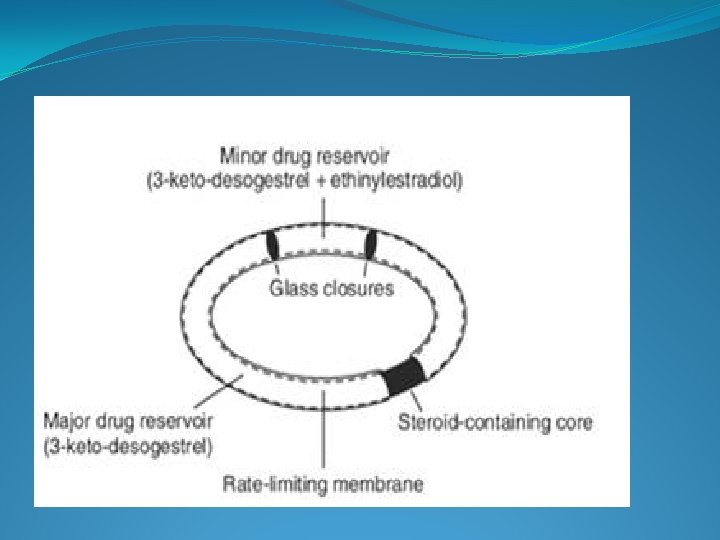
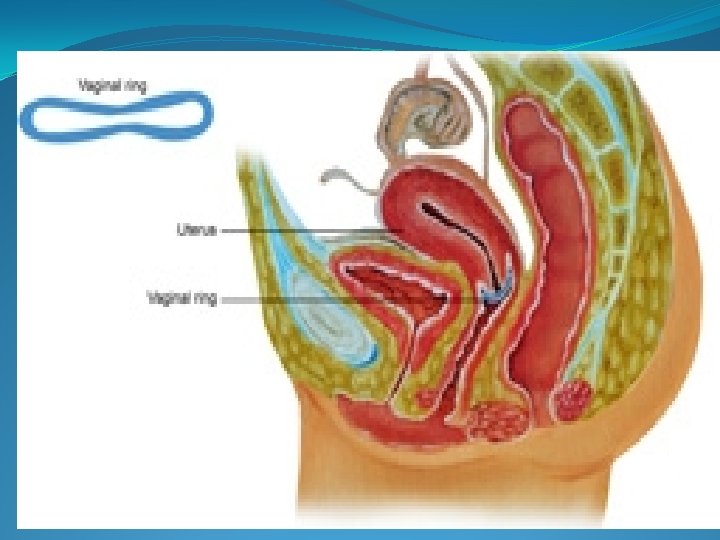
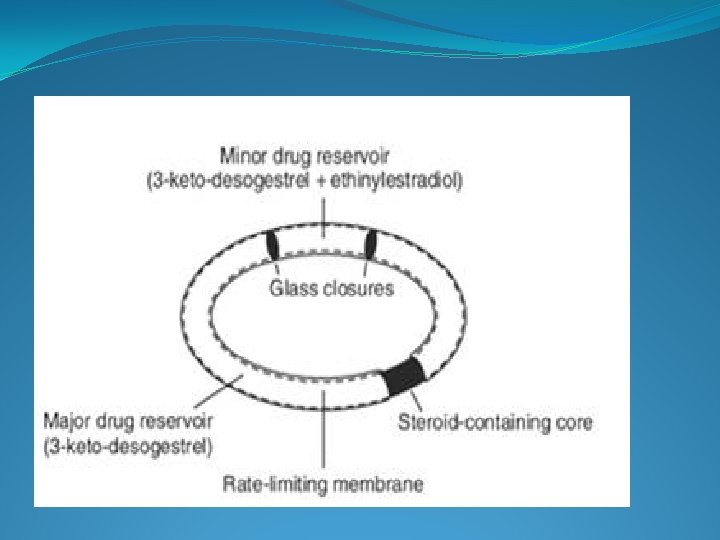
�Vaginal rings �Containing LNG covered by sialistic tubing they are 5 -6 cm diameter and delivers LNG 20 microgram per day to maintain constant blood level like that of norplant. �Ring replaced every 90 days. �Pregnancy rate is 3 per 100 women years. �Combined rings –NUVA RING. �Soft transparent ethylene vinyl ring releases EE 15 microgram and etonorgesterl metabolite of desogestrel 0. 12 mg daily over a period of 21 days. It is then removed and after 1 week a new ring is inserted. �Pearl index is 0. 65 and cycle control is good �Advantages �Avoidance of GITdisturbances �Rapid return of ovulation �Easy to insert and remove �Disadvantages �Headache, leucorrhoea, vaginitis, expulsion
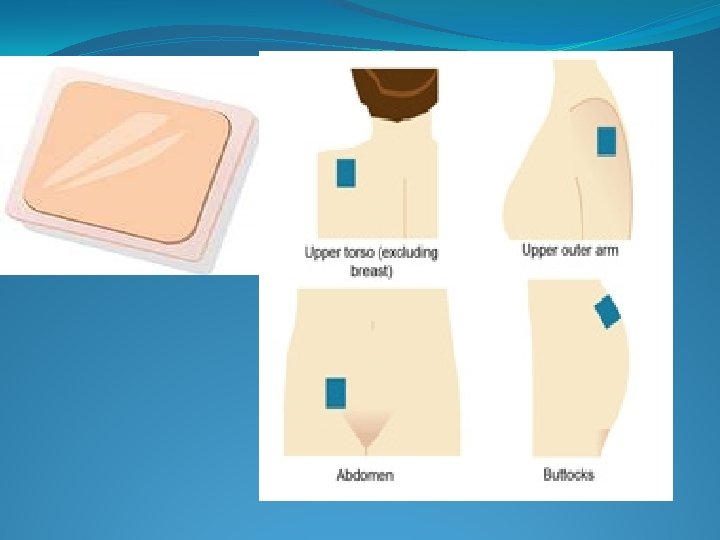
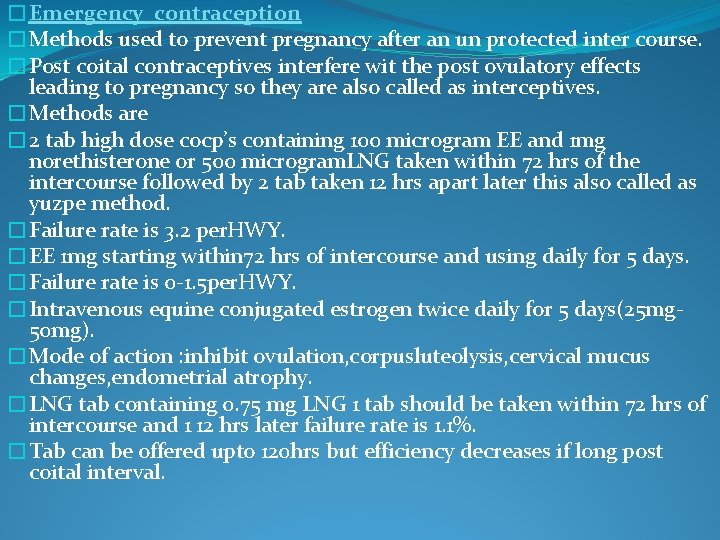
nestrone. ST 1435 and 15 microgram. EE effective for 12 months Progesterone vaginal ring Less effective than the combined. Effective in lactation 10 mg progesterone for 3 months Transdermal contraceptive patch Patch delivers 150 microgram of norelgestromin and 20 microgram of EE Used for 3 week and 1 week off for the withdrawal bleeding Buttock, lowerabdomen, upper and outer arm s/e withdrawal bleeding Skin reactions Headache and nausea mastalgia
�Emergency contraception �Methods used to prevent pregnancy after an un protected inter course. �Post coital contraceptives interfere wit the post ovulatory effects leading to pregnancy so they are also called as interceptives. �Methods are � 2 tab high dose cocp’s containing 100 microgram EE and 1 mg norethisterone or 500 microgram. LNG taken within 72 hrs of the intercourse followed by 2 tab taken 12 hrs apart later this also called as yuzpe method. �Failure rate is 3. 2 per. HWY. �EE 1 mg starting within 72 hrs of intercourse and using daily for 5 days. �Failure rate is 0 -1. 5 per. HWY. �Intravenous equine conjugated estrogen twice daily for 5 days(25 mg 50 mg). �Mode of action : inhibit ovulation, corpusluteolysis, cervical mucus changes, endometrial atrophy. �LNG tab containing 0. 75 mg LNG 1 tab should be taken within 72 hrs of intercourse and 1 12 hrs later failure rate is 1. 1%. �Tab can be offered upto 120 hrs but efficiency decreases if long post coital interval.
�Centchroman/saheli �Synthetic non steroidal taken as 30 mg started on the first day of the menses and taken twice weekly for 12 week �MOA: it has weak estrogenic and strong anti estrogenic action �It is not a teratogenic nor a carcinogenic no pharmacological effect on any organs �s/e are prolonged cycles or oligomennorhea �Head ache nausea vomitting gain in weight �Does not protect against HIV and AIDS �Contra indications �During 6 months of lactation �PCOD, hepatic dysfunction
�RU-486 Mifepristone �A single dose 10 mg is sufficient to prevent pregnancy �Centchroman � 2 tab 60 mg take twice within 24 hrs of the intercourse can prevent pregnancy �Prostaglandins �Self administered vaginal suppository containing PG following an intercourse by its luteolytic effect on the ovary and its increased motility effect on the fallopian tubes and the uterus can prevents implantation and brings about mensturation �Mechanical emergency contraception �Iucds can be used post coitally upto 5 days
�MALE CONTRACEPTION �Condoms �Natural methods �Hormonal methods �Androgens ; Testesterone enanthate Testesterone buciliate Progestogen DMPA Anti androgen and progestogen: cyproterone acetate Testesterone undedecanoate MOA By inhibiting LH which supresses spermatogenesis and FSH which testesterone production. They produce azoospermia in 40 -70% cases and oligospermia in the rest Anti spermatogenic effect is reversible. No short term bad effects except that decrease in the testesterone level may effect the male organs functions
�Testosterone enanthate �Decreases the testosterone level �Weekly inj 200 mg once azoospermia men is infertile for 12 months �Testosterone buciliate �They suppress the gonando tropins, effect for 12 weeks �Testosterone undeconate �Needed bi monthly or monthly �Progestogen pill with anti androgenic property �CYA: low dose 12. 5 mg/day+testosterone inj 100 mg per week for 16 weeks produce complete azoospermia in about 9 -10 weeks
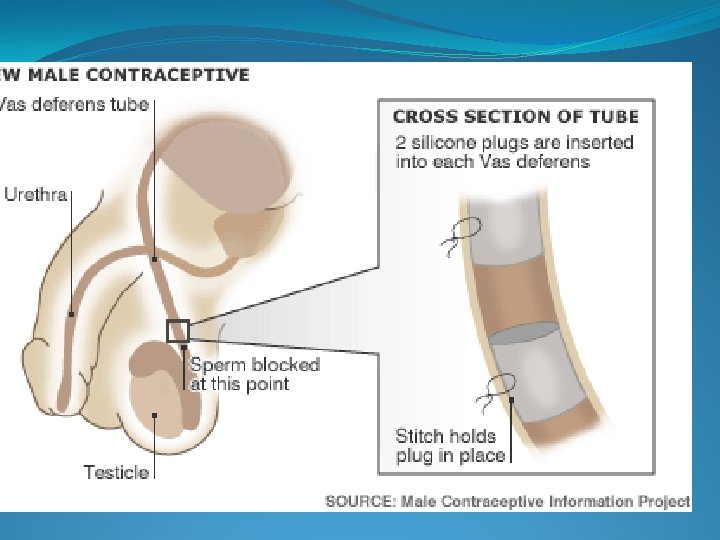
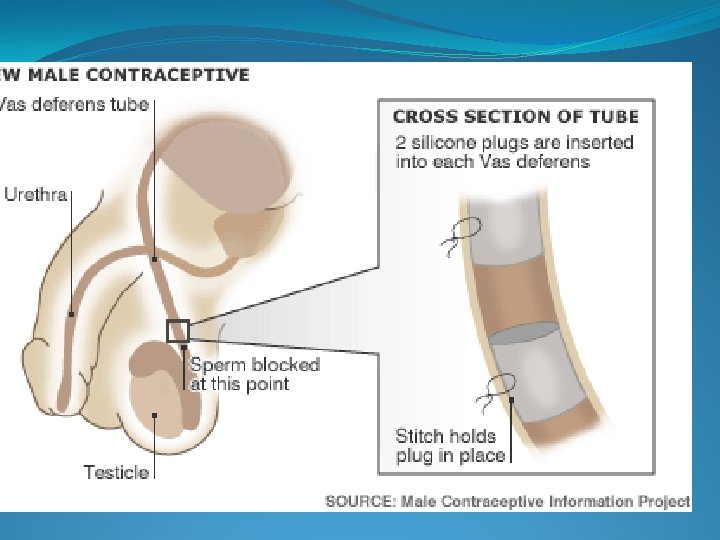
�Non hormonal agents �Gossypol �Effect by decreasing spermatogenesis. decrease the epididymal sperm motility, and affecting conversion of proacrosin tpo acrosin �Most severe side effect is hypokalemic peridic paralysis �RISUG �Reversible inhibition of the sperm under guidance �Clear polymer gelmade of styrene mallic hydrochloride �Injected into the vas it partially obstructs the vas and prevent the sperm entering to the ejaculate. �Intr vas device �Orginally called SHUG that is implanted into the vas. two plugs implanted int 2 vas �Introduction similar to that of no scalpel method �Plant compound pills �Male vaccines
�Permanent methods �Male sterilization �Conventional vasectomy �No scalpel vasectomy