Pulmonary edema Dr Akhilesh Chhaya Professor Dept of

- Slides: 36
Pulmonary edema Dr. Akhilesh Chhaya, Professor, Dept. of Anaesthesia, S. B. K. S. M. I. R. C. , Piparia
Definition • Pulmonary edema is a condition characterized by fluid accumulation in the lungs caused by extravasation of fluid from pulmonary vasculature in to the interstitium and alveoli of the lungs
The extent to which fluid accumulates in the interstitium of the lung depends on the balance of hydrostatic and oncotic forces within the pulmonary capillaries and in the surrounding tissue. • Hydrostatic pressure favors movement of fluid from the capillary into the interstitium • Oncotic pressure favors movement of fluid into the vessel • Maintenance lymphatic in the tissue carry away the small amounts of protein that may leak out tight junction of endothelium are impermeable to protein
Pathophysiology • imbalance of starling force • increase pulmonary capillary pressure • decrease plasma oncotic pressure • increase negative interstitial pressure • damage to alveolar- capillary barrier • lymphatic obstruction • Disruption of endothelial barrier allow protein to escape capillary bed and enhance movement of fluid in to the tissue of the lung • idiopathic or unknown
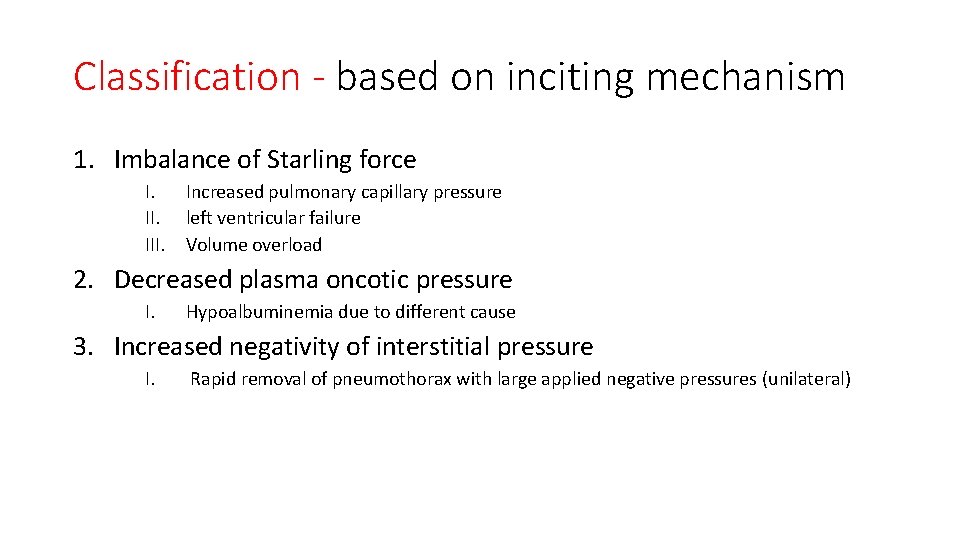
Classification - based on inciting mechanism 1. Imbalance of Starling force I. III. Increased pulmonary capillary pressure left ventricular failure Volume overload 2. Decreased plasma oncotic pressure I. Hypoalbuminemia due to different cause 3. Increased negativity of interstitial pressure I. Rapid removal of pneumothorax with large applied negative pressures (unilateral)
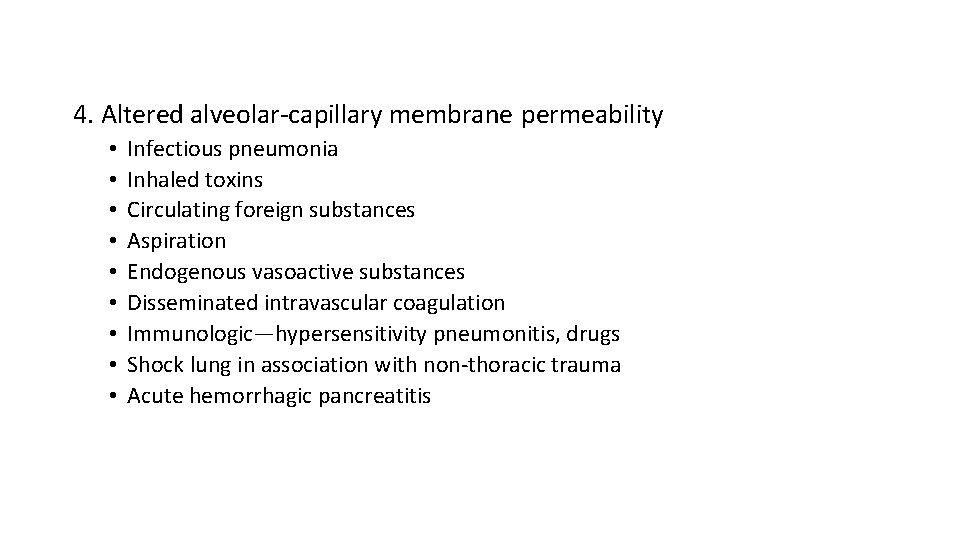
4. Altered alveolar-capillary membrane permeability • • • Infectious pneumonia Inhaled toxins Circulating foreign substances Aspiration Endogenous vasoactive substances Disseminated intravascular coagulation Immunologic—hypersensitivity pneumonitis, drugs Shock lung in association with non-thoracic trauma Acute hemorrhagic pancreatitis
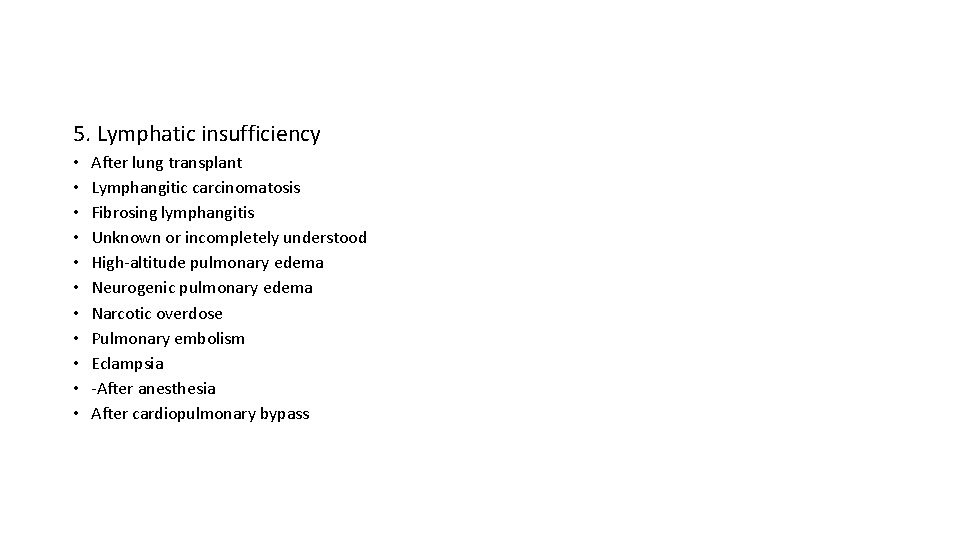
5. Lymphatic insufficiency • • • After lung transplant Lymphangitic carcinomatosis Fibrosing lymphangitis Unknown or incompletely understood High-altitude pulmonary edema Neurogenic pulmonary edema Narcotic overdose Pulmonary embolism Eclampsia -After anesthesia After cardiopulmonary bypass
Classification Base on underlining cause. . • Cardiogenic pulmonary edema • Non-cardiogenic pulmonary edema
Cardiogenic pulmonary edema Is Pulmonary edema due to increased pressure in the pulmonary capillaries because of cardiac abnormalities that lead to an increase in pulmonary venouspressure. Hydrostatic pressure is increased rate and fluid exit capillary at
Basic pathophysiology: A rise in pulmonary venous and pulmonary capillary pressures pushes fluid into the pulmonary alveoli and interstitium. CXR: B/L perihilar bat’s wing appearance, symmetric opacification of lung fields
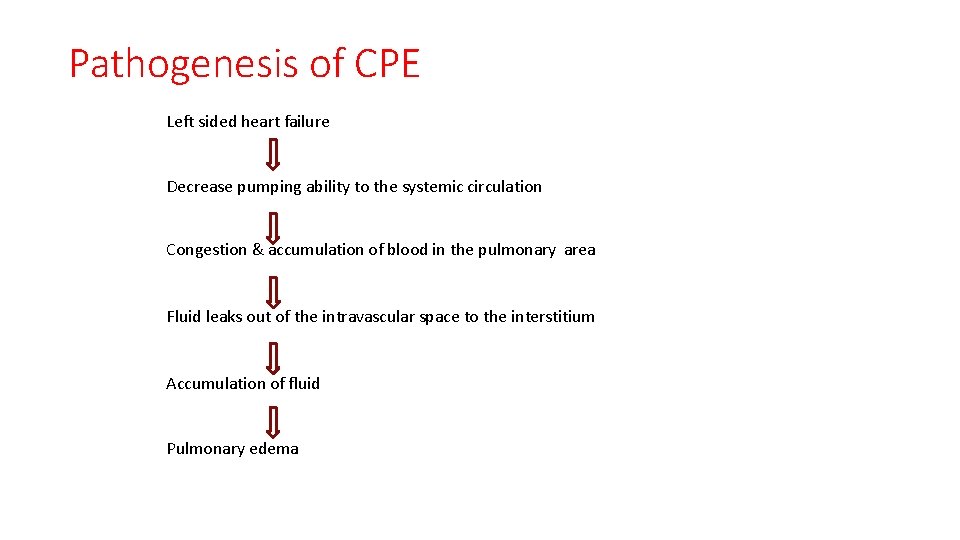
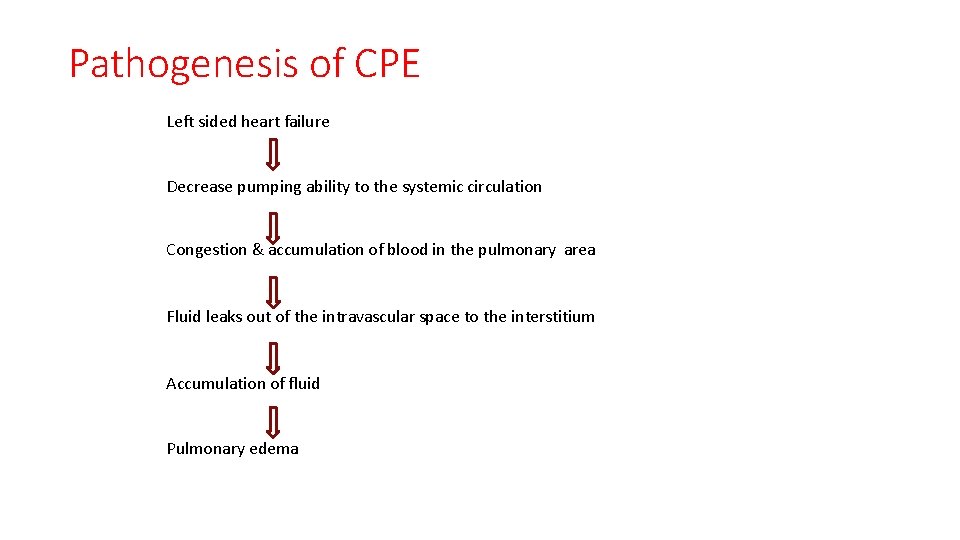
Pathogenesis of CPE Left sided heart failure Decrease pumping ability to the systemic circulation Congestion & accumulation of blood in the pulmonary area Fluid leaks out of the intravascular space to the interstitium Accumulation of fluid Pulmonary edema
Causes of Cardiogenic PE • LV failure is the most common cause. • Dysrhythmia • LV hypertrophy and cardiomyopathy • LV volume over load • Myocardia infarction • left ventricular outflow obstruction
Non cardiogenic pulmonary edema • It is defined as the evidence of alveolar fluid accumulation with out hemodynamic evidence that suggest a cardiogenic etiology. • Hydrostatic pressure is normal • Leakage of protein and other molecule into the tissue
• Associated with dysfunction of surfactant lining the alveoli, increased surface force and a propensity for the alveoli to collapse at low volume. • Characterized by intra pulmonary shunt with hypoxemia and decrease lung compliance
Non cardiogenic pulmonary edema Mechanism include: • Increased alveolar–capillary membrane permeability • Decreased plasma oncotic pressure • Increased negativity of pulmonary interstitial pressure • Lymphatic insufficiency or obstruction
Non- cardiogenic PE cause • Direct injury to the lung • Hematogenous injury to the lung • possible lung injury plus elevated hydrostatic pressure
Staging of PE Three stages of PE can be distinguished based on the degree of fluid accumulation: Stage-1 : all excess fluid can still be cleared by lymphatic drainage. Stage-2 : characterized by the presence of interstitial edema. Stage-3 : characterized by alveolar edema due to altered alveolorcapillary permeabilitya
• Mild: Only engorgement of pulmonary vasculature is seen. • Moderate: There is extravasation of fluid into the interstitial space due to changes in oncotic pressure. • Severe: Alveolar filling occurs
Unusual type pulmonary edema Neurogenic pulmonary edema • Patients with central nervous system disorders and without apparent preexisting LV dysfunction Re-expansion pulmonary edema • Develops after removal of air or fluid that has been in pleural space for some time, post- thoracentesis • Patients may develop hypotension or oliguria resulting from rapid fluid shifts into lung.
Unusual type pulmonary edema High altitude pulmonary edema • occurs in young people who have quickly ascended to altitudes above 2700 m and who then engage in strenuous physical exercise at that altitude, before they have become acclimatized. • Reversible (in less than 48 hours)
Symptom of pulmonary edema ACUTE • Shortness of breath • A Feeling of suffocating • Anxiety , restlessness • Cough-frothy sputum that may be tinged withblood • excessive sweating • pale skin • chest pain if PE is cause by cardiac abnormality • palpitation
Symptom…… Loang term(chronic) • Paraxosomal nocturnal dyspnea • orthopnea • Rapid weight gain • Loss of appetite • fatigue • ankle and leg swelling
Signs • • • Tachycardia Tachypnea Confusion Agitation Anxious Diaphoric Hypertension Cool extremities Rales Wheezing CVS findings, S 3 , accentuation of pulmonic component of S 2, jugular venous distention…. .
Complications • • • leg swelling(edema), abdominal swelling(ascites), Pleural effusion, Congestion & swelling of liver, acute heart attack (myocardial infarction [MI]), cardiogenic shock, arrhythmias, electrolyte disturbances, mesenteric insufficiency, protein enteropathy, respiratory arrest, and death.
Distinguishing Cardiogenic from Non-cardiogenic Pulmonary edema Finding suggesting cardiogenic edema • • • S 3 gallop elevated JVP Peripheral edema Findings suggesting non-cardiogenic edema • Pulmonary findings may be relatively normal in the early stages
Distinguishing …. . • Chest radiography • A cardiogenic cause is favoured with • Cardiomegaly • Kerley B lines and loss of distinct vascular margins • Cephalization: engorgement of vasculature to the apices • Perihilar alveolar infiltrate • Pleural effusion Non cardiogenic cause • Heart size is normal • Uniform alveolar infiltrate • pleural effusion is uncommon • lack of cephalization
Distinguishing…. . Hypoxemia 1. Cardiogenic • • due to ventilation perfusion miss match respond to administration of oxygen 2. Non cardiogenic • • due to intrapulmonary shunting persist despite oxygen supplimentation
INVESTIGATIONS • CXR-PA view: unilateral or bilateral involvement, cardiogenic pattern or non cardiogenic pattern(air bronchogram signs, fluffy opacities, asymmetrical inhomogenous involvement), lobar involvement in post infectious PE. • ABG analysis: hypoxia and hypocapnia initially with respi. alkalois hypercapnea in later stage with respi and metabolic acidosis • Hemodynamic measurement with Swan-Ganz catheter • Blood work up and septic screen
Management strategy • Treat underlying cause : Sepsis, heart failure, high altitude hypoxia, obstruction, fluid overload, hypoproteinemia etc. • Respi support: NIV vs Intubation f/b venti support Indication for intubation f/b venti support • • • Refractive hypoxia Excessive work of breathing : rate > 35/min , MV>12 L/min Hemodynamic instability Inability to protect airway Anticipated rapid clinical deterioration
Management strategy…. . • NIV support: CPAP Reasonable initial venti settings are EPAP 7 cm. H 2 O and IPAP of around 15 cm H 2 O with adjustment according to patient tolerance and maintaining Sa. O 2>90% • Decreases work of breathing, FRC is increased, collapse of alveoli due to edema fluid is prevented and helps in opening up of already collapsed alveoli • Good response is generally observed in 30 minutes, if not so or worsening is seen, consider elective intubation f/b venti support
Management stretagy… Principles of mechanical ventilation. Two fundamental principles • Prevention of overdistension of alveoli-limiting tidal volume or inspiratory pressure • Choose the level of PEEP sufficiently high to prevent derecruitment of alveoli at end of expiration
• Limiting tidal volume High TV 12 -15 ml per kg are dangerous in patient with PE can lead to VOLUTRAUMA • Tidal volume kept at 6 -8 ml per kg to start with in patient of PE • Then adjusted to keep the plateau pressure below 30 cm of H 2 O
2. Use of PEEP • Recruits collapsed alveoli, prevents collapse, improves V/Q mismatch, decreases shunt and venous admixture, increases FRC, reduces pathological dead space • Can allow adequate oxygenation at lower Fi. O 2, protects from oxygen toxicity • Most patients with ARDS will need PEEP of more than 10 cm H 2 O at Fi. O 2<0. 6 • If high level of PEEP causes hemodynamic instability, use of pressure controlled – inverse ratio ventilation , prone posture can be beneficial • Inverse ratio venti: changes inspiration-expiration ratio, lower peak pressure can be achieved, auto- PEEP develops, higher mean alveolar pressure with low peak pressure
Treatment in special conditions High altitude pulmonary edema • Slow ascent , prophylactically tab. nifedipine 20 mg sustained release 8 hrly, or tab dexamethasone 8 mg 12 hrly, or inhaled salmeterol • Descent and supplemental O 2 are definitive Rx • If descent not possible and O 2 not available, start pharmacotherapy to reduce pulmonary artery • Tab nifedipine 10 mg sublingual f/b 20 mg SR tab • Also hydralazine, inhaled nitrous oxide • acetazolamide are helpful pressure 6 hrly
Post Aspiration PE • Preop gastric emptying by physical means(ryle’s tube aspiration) or pharmacological means(perinorm, atropine, glocopyrolate) • Anti ematics ondensatron, granisatron injectable • Induction in lateral position • Head low position • Bronchoscopic removal of particulate aspirate material • NO BRONCHO-ALVEOLAR LAVAGE-removes surfactant and promotes collapse • Supportive sterids • PEEP and mechanical venti till edema clears

Thank You!!
 Cardiogenic vs noncardiogenic pulmonary edema
Cardiogenic vs noncardiogenic pulmonary edema Pulmonary edema
Pulmonary edema Chhaya kapilashrami
Chhaya kapilashrami Dr akhilesh dubey indore
Dr akhilesh dubey indore Promotion from associate professor to professor
Promotion from associate professor to professor Worcester building dept
Worcester building dept Tabella chemical shift c13
Tabella chemical shift c13 Central islip fire dept
Central islip fire dept Hoe dept
Hoe dept Dept. name of organization
Dept. name of organization La geaux biz
La geaux biz Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services Dept nmr spectroscopy
Dept nmr spectroscopy Gome dept
Gome dept Dept ind onegov
Dept ind onegov Dept. name of organization
Dept. name of organization Pt dept logistik
Pt dept logistik Dss rowan county
Dss rowan county Firefighter interview tips
Firefighter interview tips Ohio dept of dd
Ohio dept of dd Oxford dept of continuing education
Oxford dept of continuing education Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services Department of agriculture consumer services
Department of agriculture consumer services Nyttofunktion
Nyttofunktion Albany county dept of social services
Albany county dept of social services Dept of education
Dept of education Mn dept of education
Mn dept of education Nys department of homeland security
Nys department of homeland security Maine dept of agriculture
Maine dept of agriculture Vaginal dept
Vaginal dept Nebraska dept of agriculture
Nebraska dept of agriculture Poster affiliation
Poster affiliation Dept a
Dept a Finance departments
Finance departments Gome dept
Gome dept Liz welch mississippi
Liz welch mississippi Affiliate disclodures
Affiliate disclodures