Acute Pulmonary Edema During Emergence from Anesthesia Liu


![Negative-pressure Pulmonary Edema in a Child with Hiccups during Induction [CASE REPORTS] Anesthesiology, 93(1): Negative-pressure Pulmonary Edema in a Child with Hiccups during Induction [CASE REPORTS] Anesthesiology, 93(1):](https://slidetodoc.com/presentation_image/77d2d6ba51a331a71a037b7e93baa3ef/image-21.jpg)
![Negative-pressure Pulmonary Edema in a Child with Hiccups during Induction [Correspondence] Anesthesiology, 94(2): 378 Negative-pressure Pulmonary Edema in a Child with Hiccups during Induction [Correspondence] Anesthesiology, 94(2): 378](https://slidetodoc.com/presentation_image/77d2d6ba51a331a71a037b7e93baa3ef/image-22.jpg)

- Slides: 24
Acute Pulmonary Edema During Emergence from Anesthesia Liu, Chih-Min 2003 -9 -22
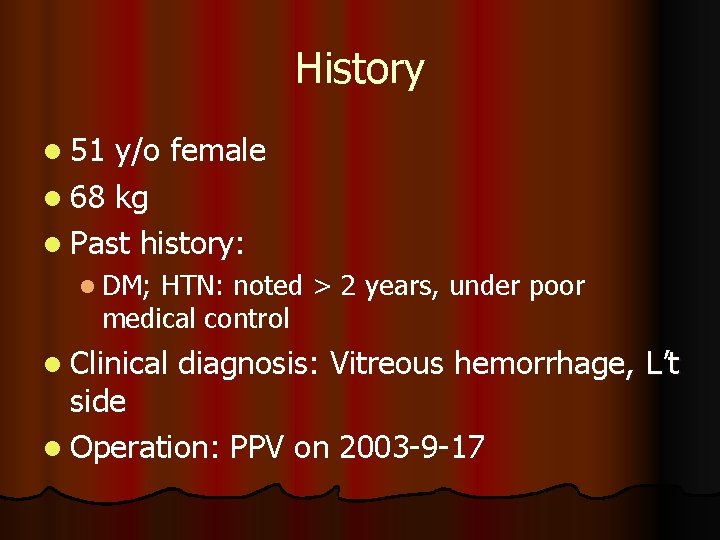
History l 51 y/o female l 68 kg l Past history: l DM; HTN: noted > 2 years, under poor medical control l Clinical diagnosis: Vitreous hemorrhage, L’t side l Operation: PPV on 2003 -9 -17

ASA class lll. E l BP: 237/134 mm. Hg at the OR l Past history: l DM; HTN: noted > 2 years, under poor medical control
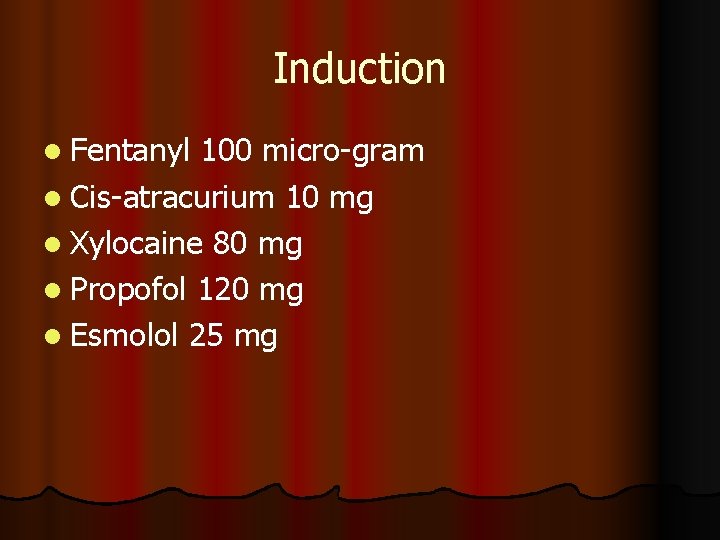
Induction l Fentanyl 100 micro-gram l Cis-atracurium 10 mg l Xylocaine 80 mg l Propofol 120 mg l Esmolol 25 mg
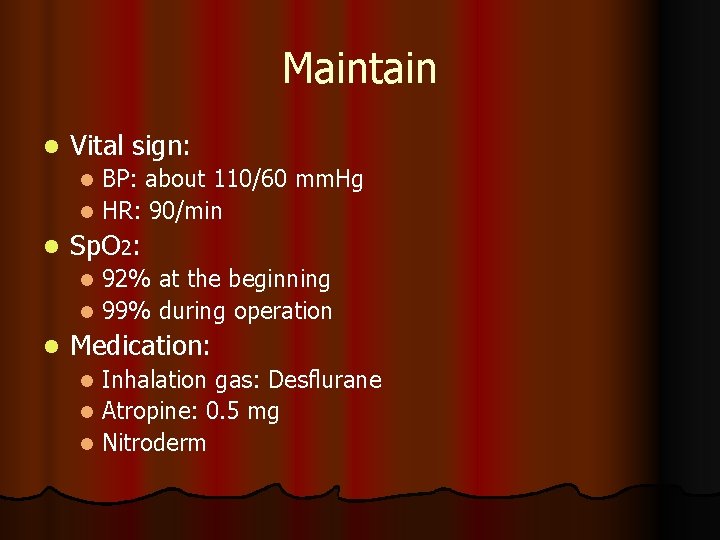
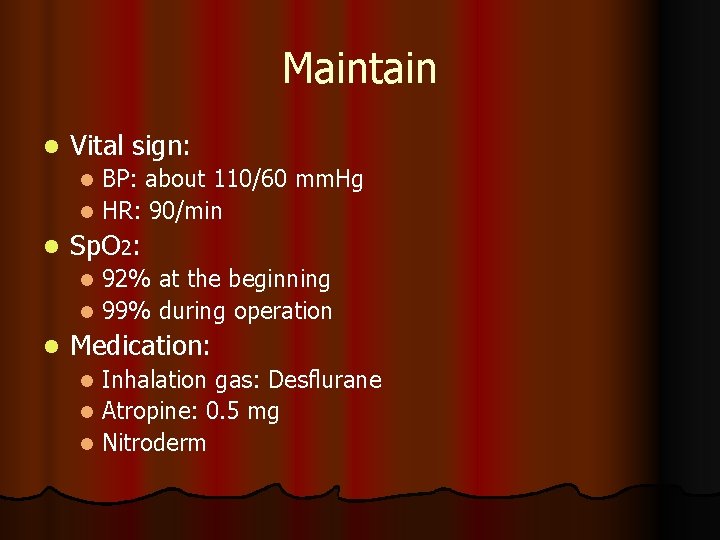
Maintain l Vital sign: BP: about 110/60 mm. Hg l HR: 90/min l l Sp. O 2: 92% at the beginning l 99% during operation l l Medication: Inhalation gas: Desflurane l Atropine: 0. 5 mg l Nitroderm l
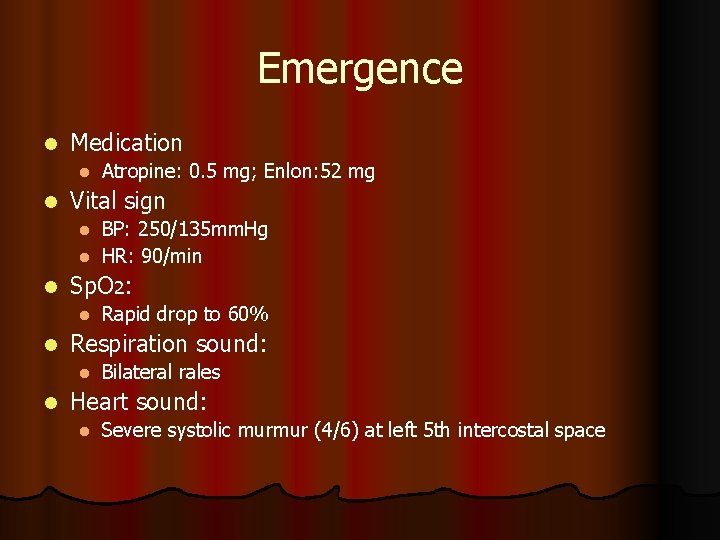
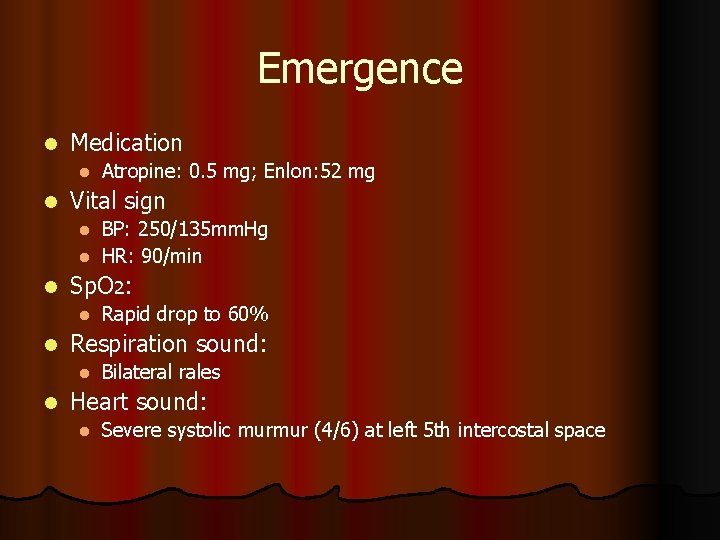
Emergence l Medication l l Atropine: 0. 5 mg; Enlon: 52 mg Vital sign BP: 250/135 mm. Hg l HR: 90/min l l Sp. O 2: l l Respiration sound: l l Rapid drop to 60% Bilateral rales Heart sound: l Severe systolic murmur (4/6) at left 5 th intercostal space
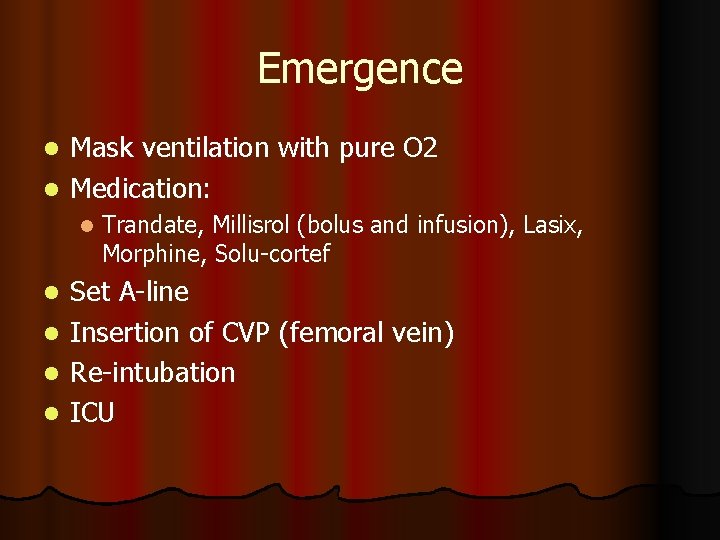
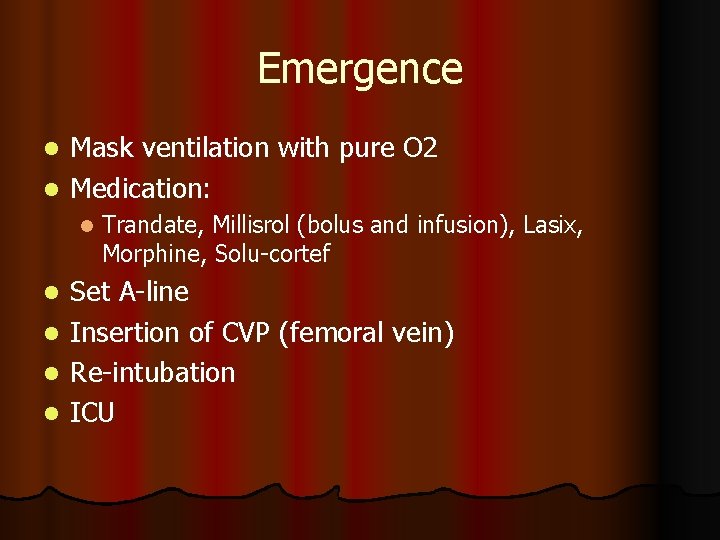
Emergence Mask ventilation with pure O 2 l Medication: l l Trandate, Millisrol (bolus and infusion), Lasix, Morphine, Solu-cortef Set A-line l Insertion of CVP (femoral vein) l Re-intubation l ICU l
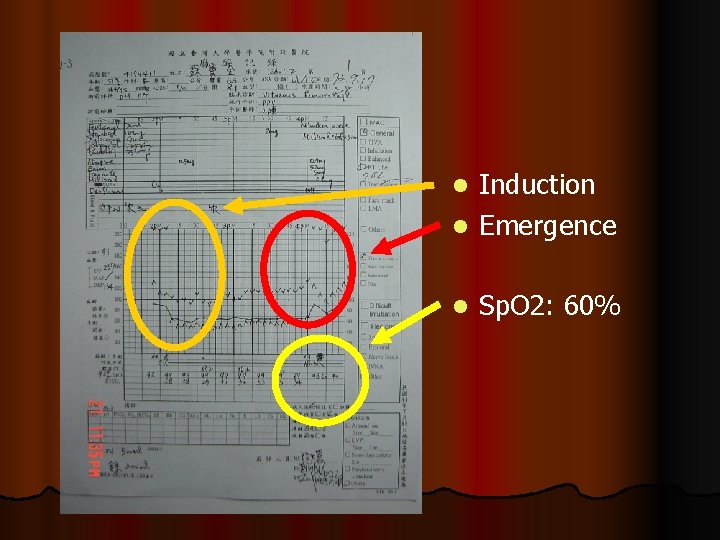
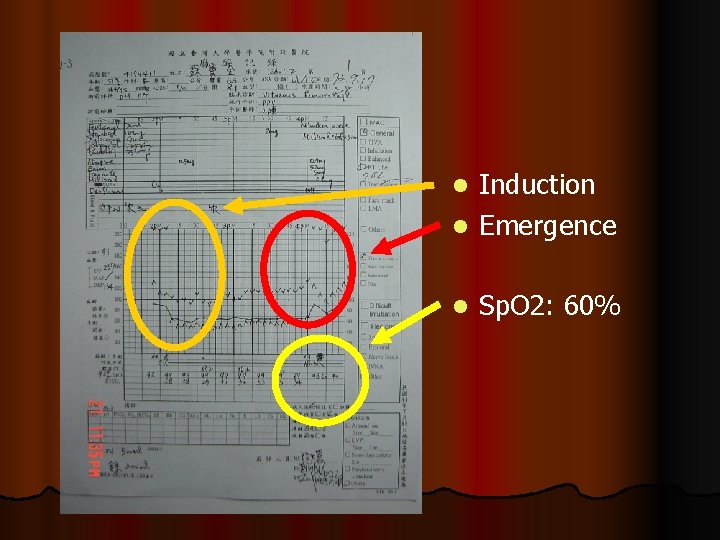
Induction l Emergence l l Sp. O 2: 60%
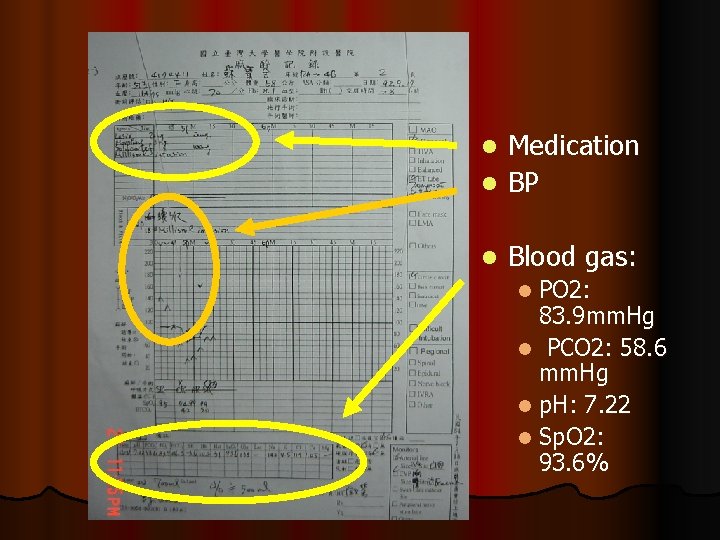
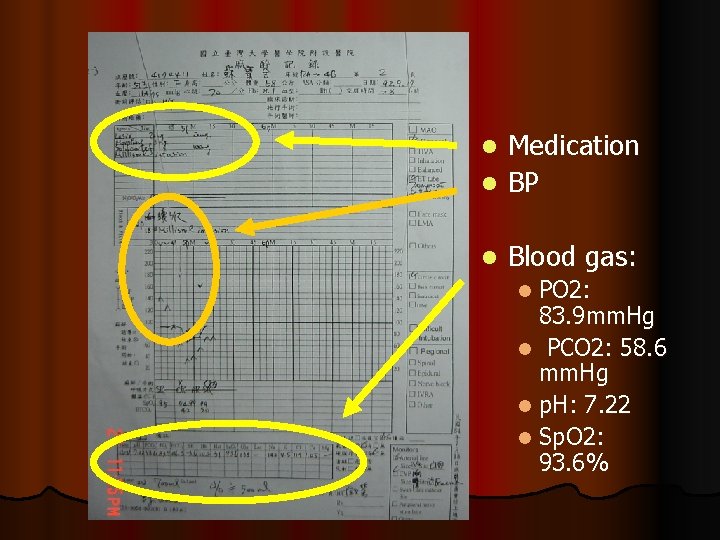
Medication l BP l l Blood gas: PO 2: 83. 9 mm. Hg l PCO 2: 58. 6 mm. Hg l p. H: 7. 22 l Sp. O 2: 93. 6% l
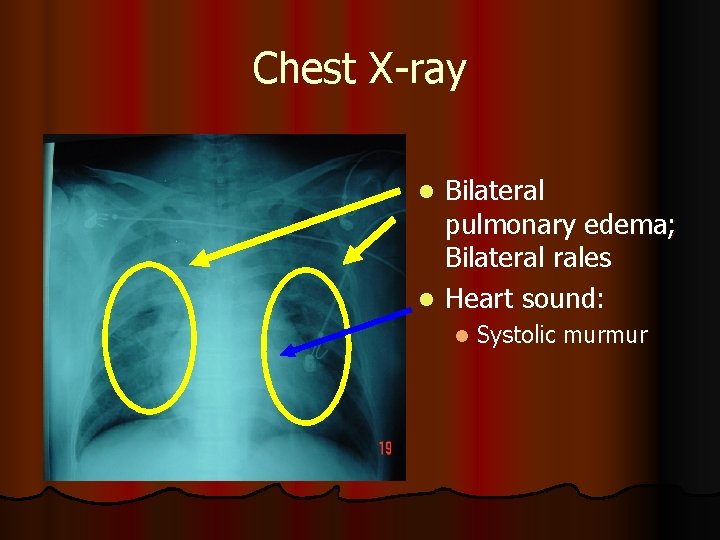
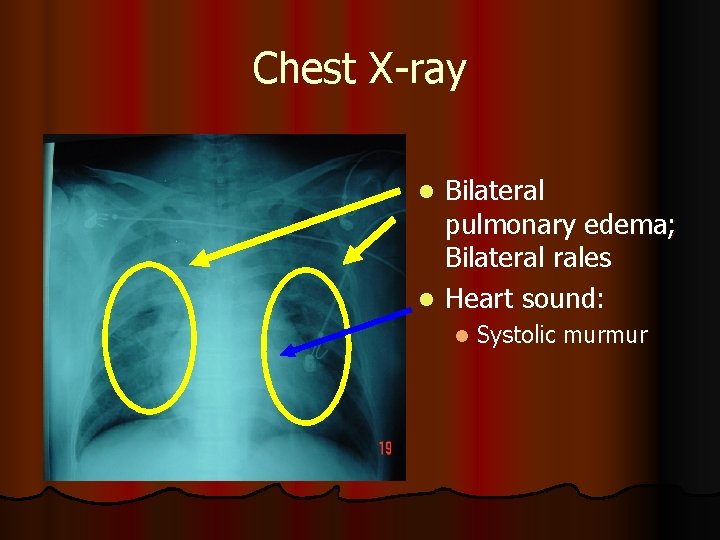
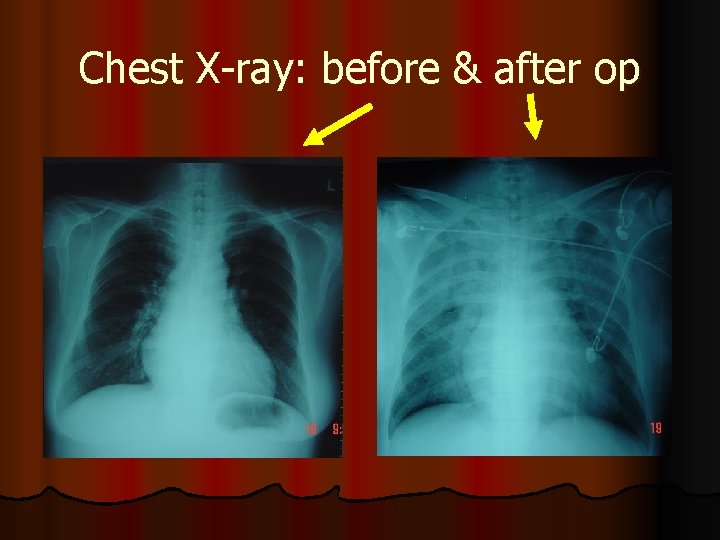
Chest X-ray Bilateral pulmonary edema; Bilateral rales l Heart sound: l l Systolic murmur
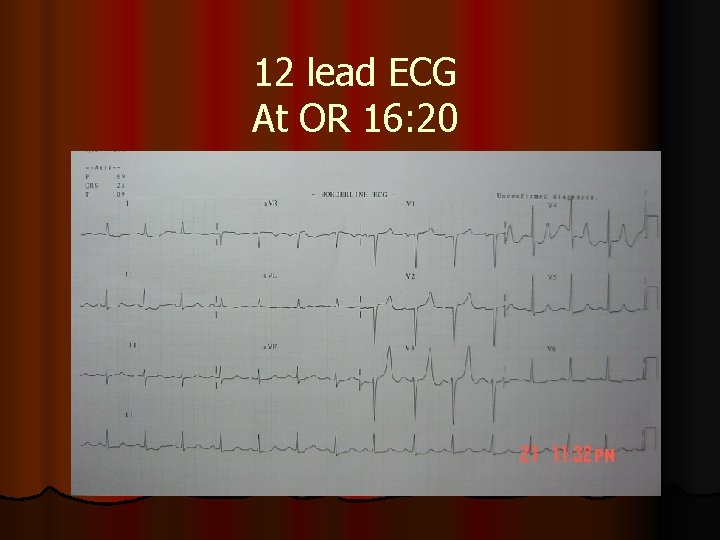
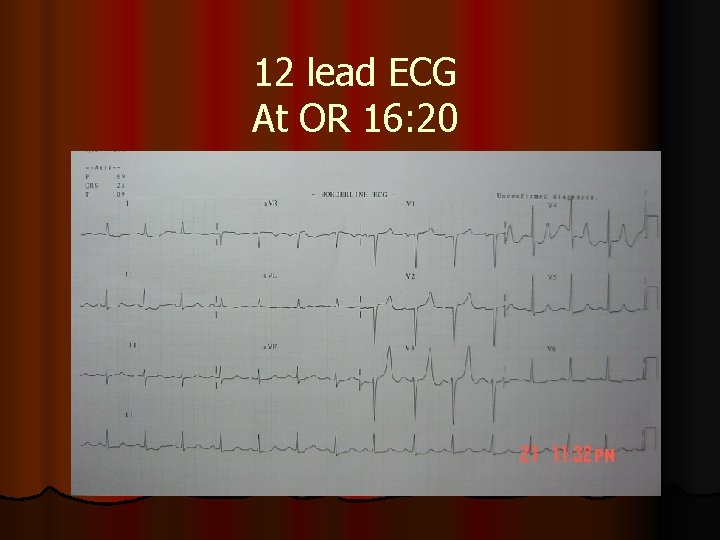
12 lead ECG At OR 16: 20
Send to ICU l Ventilator l SIMV l PEEP l Sedation
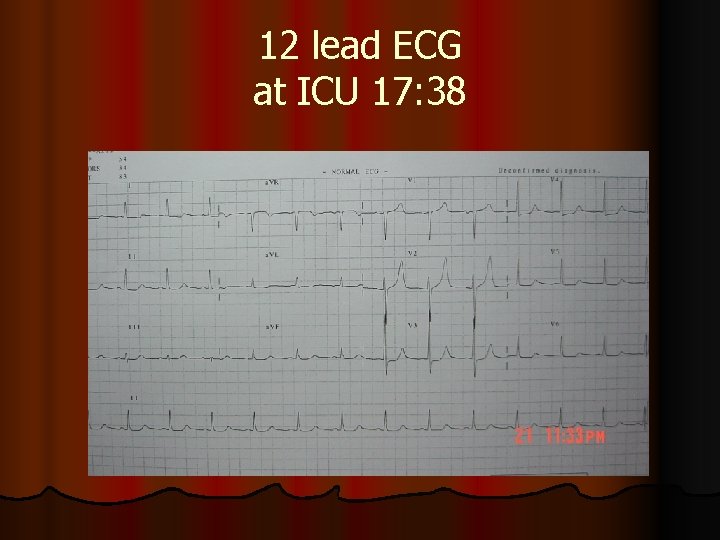
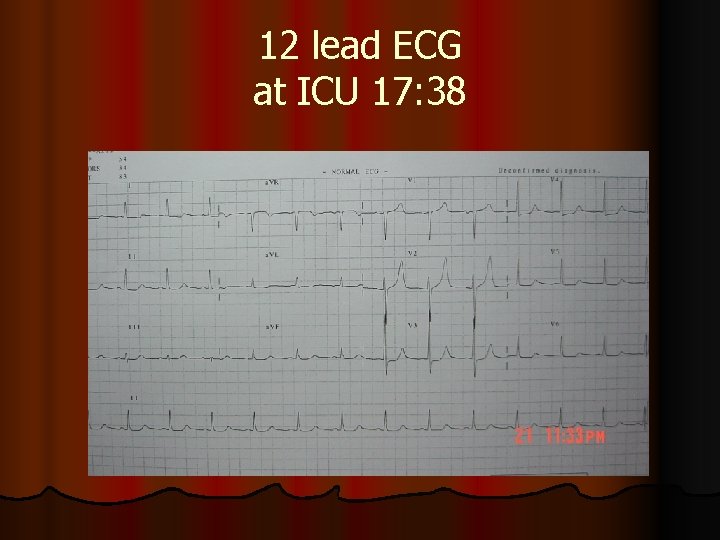
12 lead ECG at ICU 17: 38
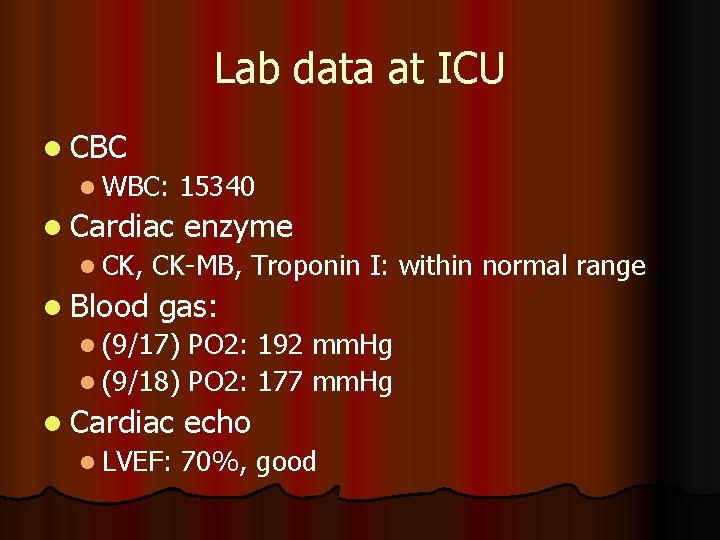
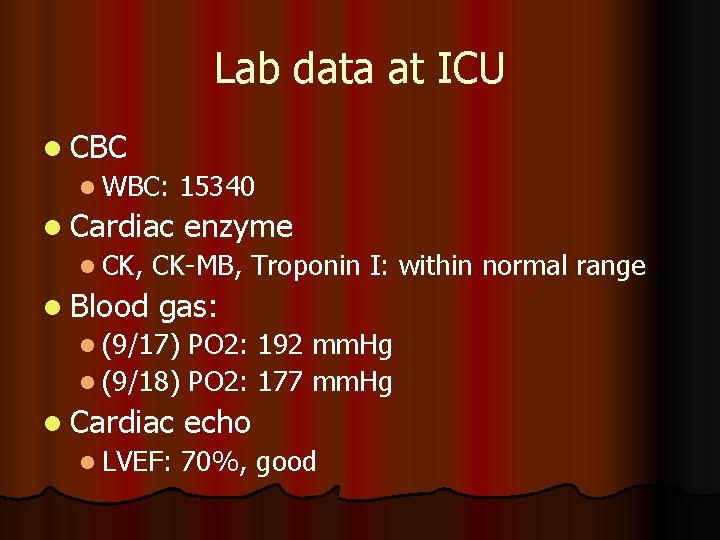
Lab data at ICU l CBC l WBC: 15340 l Cardiac l CK, l Blood enzyme CK-MB, Troponin I: within normal range gas: l (9/17) PO 2: 192 mm. Hg l (9/18) PO 2: 177 mm. Hg l Cardiac l LVEF: echo 70%, good

Discussion
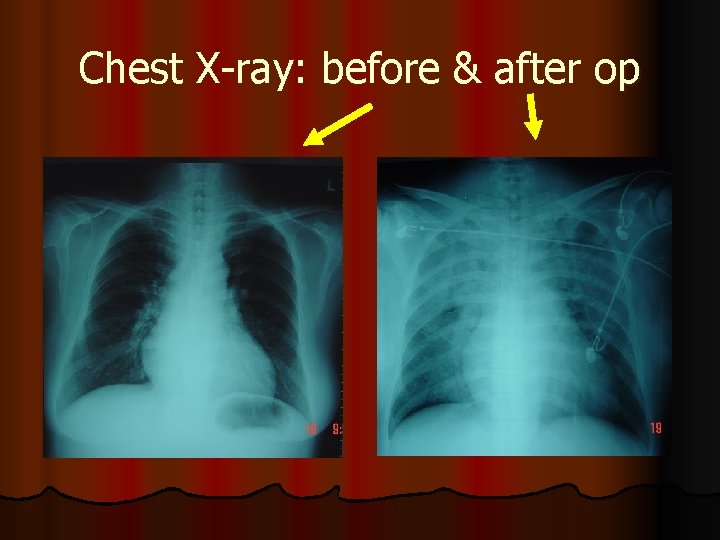
Chest X-ray: before & after op
What happened? Pulmonary Edema
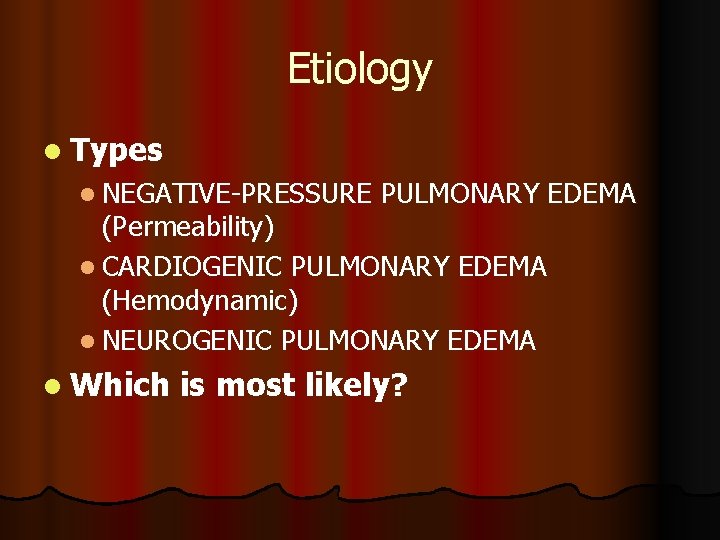
Etiology l Types l NEGATIVE-PRESSURE PULMONARY EDEMA (Permeability) l CARDIOGENIC PULMONARY EDEMA (Hemodynamic) l NEUROGENIC PULMONARY EDEMA l Which is most likely?
NEGATIVE-PRESSURE PULMONARY EDEMA l l l Also known as postobstructive pulmonary edema Characterized by its rapid onset and short-lived course Large, negative intrapleural pressures are the pathophysiologic hallmark of negative-pressure pulmonary edema Various types of airway obstruction, including croup, epiglottitis, laryngospasm after tonsillectomy, hanging, and tumors have been reported Symptoms commonly resolve within 12 to 24 hours Suction mechanism
l NEUROGENIC PULMONARY EDEMA The exact cause of neurogenic pulmonary edema is unknown l Increased capillary hydrostatic pressure and increased capillary permeability l With a history of head trauma or intracranial pathology l l CARDIOGENIC PULMONARY EDEMA Develops when Pcap is excessively high, overwhelming the ability of the lymphatic system to resorb fluid. l Left-to-right shunting lesions, such as a patent ductus arteriosus or a ventricular septal defect l Ventricular function l
![Negativepressure Pulmonary Edema in a Child with Hiccups during Induction CASE REPORTS Anesthesiology 931 Negative-pressure Pulmonary Edema in a Child with Hiccups during Induction [CASE REPORTS] Anesthesiology, 93(1):](https://slidetodoc.com/presentation_image/77d2d6ba51a331a71a037b7e93baa3ef/image-21.jpg)
Negative-pressure Pulmonary Edema in a Child with Hiccups during Induction [CASE REPORTS] Anesthesiology, 93(1): 282 -4 Negative-pressure pulmonary edema (NPPE) occurs soon after relief of acute or chronic obstruction of the upper airway. It is commonly reported after laryngospasm during induction or emergence from anesthesia. l Markedly negative intrapleural pressures during airway occlusion cause increased venous return and increased left ventricular afterload. The increased hydrostatic pressure gradient in the pulmonary capillaries leads to transsudation of fluid into the alveoli. Hypoxemia and a hypoxia-induced hyperadrenergic state further promote edema formation. l It is likely that more cases of unexplained perioperative hypoxemia are related to unrecognized NPPE. l
![Negativepressure Pulmonary Edema in a Child with Hiccups during Induction Correspondence Anesthesiology 942 378 Negative-pressure Pulmonary Edema in a Child with Hiccups during Induction [Correspondence] Anesthesiology, 94(2): 378](https://slidetodoc.com/presentation_image/77d2d6ba51a331a71a037b7e93baa3ef/image-22.jpg)
Negative-pressure Pulmonary Edema in a Child with Hiccups during Induction [Correspondence] Anesthesiology, 94(2): 378 -9 l NPPE v. s. CPE: l l Echo: l l The most specific method for differentiating NCPE from CPE is the demonstration of increased alveolar–capillary permeability, which is characteristic of NCPE. Alternatively, pulmonary capillary wedge pressure measurement could be useful to differentiate CPE from NCPE. An echocardiogram shows normal left ventricular systolic and diastolic function in NCPE X-ray l Centrally distributed pulmonary edema could be suggestive of cardiogenic origin
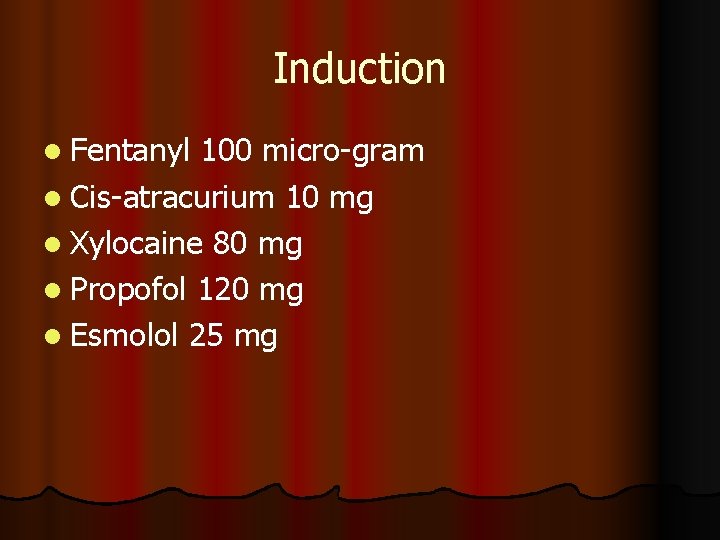
Pulmonary oedema associated with airway obstruction Canadian Journal of Anaesthesia. 37(2): 210 -8, 1990 Mar l Pathogenesis of pulmonary oedema associated with upper airway obstruction is multifactorial l negative intrapleural pressure is the dominant pathophysiological mechanism involved in the genesis of pulmonary oedema associated with upper airway obstruction l The majority of cases present within minutes Resolution is typically rapid, over a period of a few hours. l Maintenance of a patent airway, supplemental oxygen, mechanical ventilation and positive end-expiratory pressure l

Thanks for your attention
 Pulmonary edema
Pulmonary edema Cardiogenic vs noncardiogenic pulmonary edema
Cardiogenic vs noncardiogenic pulmonary edema Heart failure cells are seen in lungs
Heart failure cells are seen in lungs Barrel chest with emphysema
Barrel chest with emphysema Alex liu cecilia liu
Alex liu cecilia liu Líu líu lo lo ta ca hát say sưa
Líu líu lo lo ta ca hát say sưa Emergence of scaling in random networks
Emergence of scaling in random networks The emergence of new values
The emergence of new values Emergence of entrepreneurial class
Emergence of entrepreneurial class The emergence of mass society
The emergence of mass society Landmarks in emergence of corporate governance
Landmarks in emergence of corporate governance Speech emergence
Speech emergence Plan emergence madagascar 2019-2023 pdf
Plan emergence madagascar 2019-2023 pdf Ion storm
Ion storm The emergence of mass society
The emergence of mass society Plan emergence madagascar 2019-2023 pdf
Plan emergence madagascar 2019-2023 pdf Emergence profile
Emergence profile Speech emergence examples
Speech emergence examples Emergence netflix
Emergence netflix Emergence theory
Emergence theory So&e
So&e Dependent edema
Dependent edema Triada de virchow
Triada de virchow Edema paru non kardiogenik
Edema paru non kardiogenik Edeme
Edeme