EDEMA PROF DR YESAR KARTER 1 75 of







- Slides: 32
EDEMA PROF. DR. YESARİ KARTER 1
75 % of total body weight is water - 50 % - Intracellular volume - 20 % - Interstitial volume - 5 % - Intravascular volume 2
EDEMA Increasing of fluid volume in tissues. -It is usually used to define the increasing of extracellular and extravascular fluid volume 3

EDEMA – Local (Pulmonary, cerebral, pharyngeal - Disseminated (Increasing of interstitial fluid volume) 4
Intraperitoneal - Ascites Intrapleural - Hydrothorax 5

PATHOGENESIS OF EDEMA 1) Capillary permeability 2) Hydrostatic pressure of intracapillary fluid 3) Oncotic pressure of intracapillary fluid 4) Oncotic pressure of interstitial fluid 5) Tissue resistance 6) Lymphatic drainnage 7) Renal hormonal factors 8) Atrial natriüretic peptide 6
Capillary permeability Water, electrolytes, gases – Diffusion Proteins - Filtration Chemical, bacterial, thermal, mechanical factors may cause the increasing of permeability – inflamatory edema / angioedema 7
Hydrostatic pressure: It forces the blood fluid pass into the tissues through the capillary wall. It is 32 mm. Hg at the arteriolar end of the capillary, and 12 mm. Hg at the venule hand. 8

Oncotic pressure: Formed by plasma proteins (especially albumin) It tries to keep the fluid in the capillary The oncotic pressure of the capillary is 24 mm. Hg. 9

Plasma protin content > İnterstitial protein content Plasma oncotic pressure > ınterstitial oncotic pressre Effective oncotic pressure = Plasma oncotic pressure – Interstitium oncotic pressure Effective oncotic pressure decreases: - As the decreasing of plasma oncotic pressure ( cirrhosis, malnutrition, nephrotic syndrome, protein loosing ent. ) - As the increasing of interstitium oncotic pressure (Increasing of permeability – inflamatory / allergy) 10
Arteriolar end: Hydrostatic pressure > Oncotic pressure Fluid passes into interstitium Venule end: Oncotic pressure > Hydrostatic pressure Fluid returns capillary bed * The increase of pressure at the venule end Fluid cannot return capillary and stay at the interstitium 11
Oncotic pressure of the interstitium: The amount of protein is nearly 0. 3 % g / dl and it is not so important 12
Lymph drainege: Some of the fluid in the interstitium and a few amount of protein diffused into interstitium is carried by lymph vessels. Obstruction of the vessels causes edema. 13
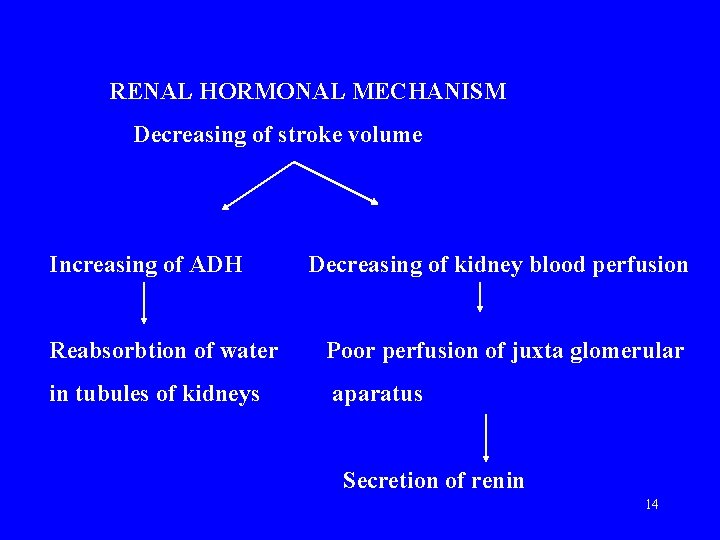
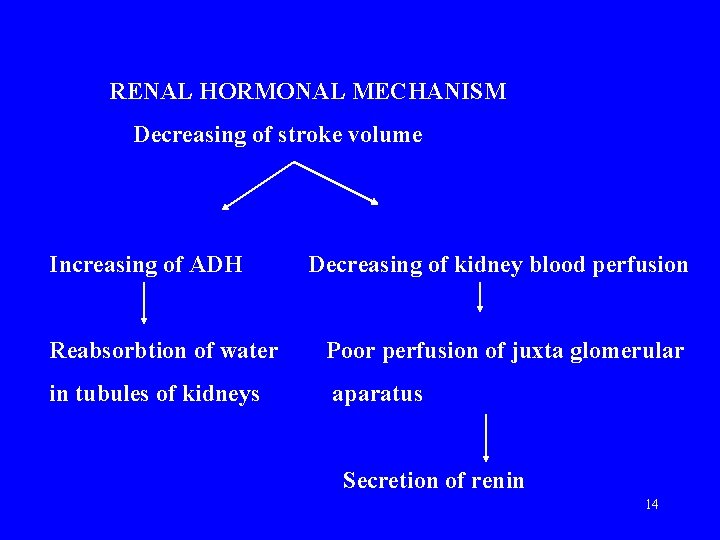
RENAL HORMONAL MECHANISM Decreasing of stroke volume Increasing of ADH Decreasing of kidney blood perfusion Reabsorbtion of water Poor perfusion of juxta glomerular in tubules of kidneys aparatus Secretion of renin 14
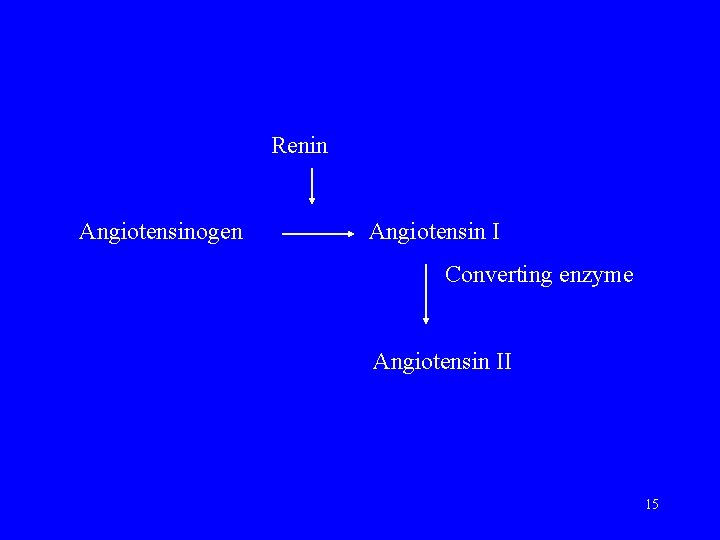
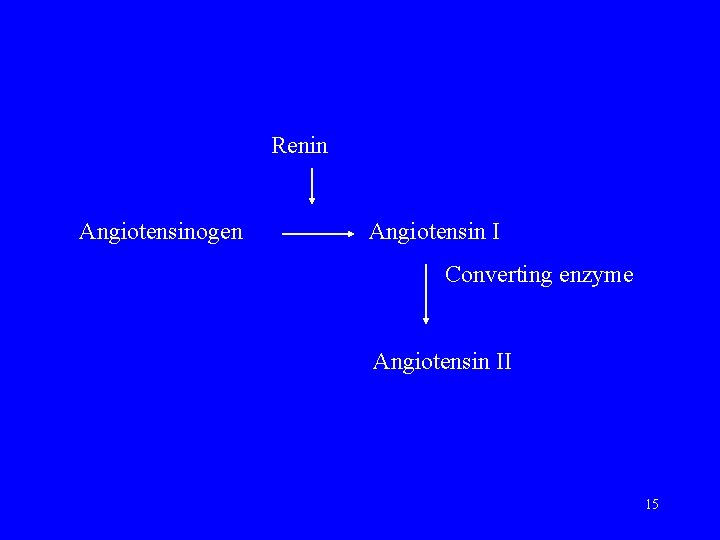
Renin Angiotensinogen Angiotensin I Converting enzyme Angiotensin II 15
Angiotensin II: 1) Causes vasoconstriction 2) Increases the secretion of aldosteron from adrenal gland ( seconder hyperaldosteronism) – İncreases sodium reabsorbtion in distal tubules 16
ATRIAL NATRURETIC PEPTIDE -Secreted by the secretory granules in the atrium -Secretion is stimulated by atrial enlargement ( plasma volume increases) -Increases diuresis and sodium output. -Causes vasodilatation -Inhibits renin and angiotensin release 17
EDEMA -Dısseminated edema -Local edema 18
Disseminated Edema • • Edema due to cardiac failure Nephritic edema Nephrotic edema Edema caused by liver failure Nutritional edema (inadequate intake) Protein loss through gastrointestinal system Edema due to endocrine pathologies Edema during pregnancy 19
Local edema - Traumatic - Inflammatory edema - Obstriction of venous circulation - Thrombophlebitis - Compression of veins -Lymphatic edema -Angioneurotic edema 20
Cardiac Insufficiency - Blood volume per minute decreases Water is conserved by renal and hormonal mechanisms - Hydrostatic pressure increases 21
Nephritic Edema Mild and hard edema is seen in acute glomerulonephritis Glomerular filtration decreases, but tubular reabsorbtion is not disturbed. (glomerulotubular inbalance) Capillaritis (generalized capillary disorder) 22

Nephrotic Edema -It is very soft and in anasarca type -Low oncotic pressure due to protein loss -Secondary hyperaldosteronism 23

Cirrhotic Edema • It is usually seen with ascites • Albumin synthesis in liver decreases • Some blood proteins are excreted in feces due to portal hypertension • Aldosteron breakdown in liver decreases ; secretion by adrenal gland increases (secondary hyperaldosteronism) 24
Nutritional edema • • Kwashiworker Malabsobtion Syndromes Gastrectomy Cancer 25
Edema due to endocrine pathologies • Mixedema • Premenstrual edema • Pregnancy 26
Iatrogenic Edema • • Mineralocorticoid Corticosteroid Androgen ADH 27
Inflammatory Edema Due tu increased permeability - Microorganisms - Connective tissue disorders 28
Venous Edema • Thrombophlebitis: Local inflamations cause thrombus venous obstriction -Large and hard edema - Erythema, hotness, pain • Compression of veins -Ganglion, tumor, ascites • Edema related to varices High hydrostatic pressure in veins 29
Lymphatic Edema • Due to obstruction of lymph vessels, plasma proteins cannot be taken from the interstitium 30
Angioneurotic Edema (Quincke’s edema) Vessels insubcutaneous tissue enlarge due to local histamine discharge and extravasation from capillaries occurs -Food allergy -Drug allergy -Infections -Emotional 31

References • • • Anand IS et al: Studies of body water andsodium, renal function, , hemadynamic indexes, and plasma hormones in untreated congestive heart failure. Circulation 1989; 80: 299 Abassi Z et al: Control of extracelluler fluid volume and the pathophysiology of edema formation. The kidney. 7 th ed, BM Brenner (ed). Philedelphia, Saunders, 2004 ; pp 777, 856. Braunwald E: Edema in the Harrison’s Principles of Internal Medicine, 16 th edition, Braunwald (ed). USA Mc. Graw –Hill Companies, 2005, pp 212 -216 Braunwald E: Edema in the Harrison’s Principles of Internal Medicine, 14 th edition, Braunwald (ed). USA Mc. Graw –Hill Companies, 1998, pp 210 -214 Chertow GM: Approach to the patient with edema. Cardiolgy for the Primary Care Phsician. Braunwald E, Goldman L (eds) 2 nd ed, Philedelphia, Saunders, 2003, pp 117128. 32