PHARMACODYNAMIC Dwi Indria Anggraini 1 Rovina Ruslami 2












- Slides: 38
PHARMACODYNAMIC Dwi Indria Anggraini 1; Rovina Ruslami 2

Definitions Pharmacogenetic Pharmacotherapeutic Pharmacology Pharmacoeconomic • Pharmacokinetic • Pharmacodynamic Pharmacy Clinical Pharmacology Pharmacognosy
Pharmacodynamics • The study of biochemical and physiological effects of drugs and their mechanism of action • What the drugs do to the body How drugs act? = mechanism of action 1. General principles 2. Molecular aspects

Overview General principles: Interaction between drug with living systems • binding drugs to the cells • desensitization and tachyphilaxis Molecular aspects: • target for the drug action • receptor protein • ion channels as drug targets • control for receptor expression • receptor and disease

PHARMACODYNAMIC General principles
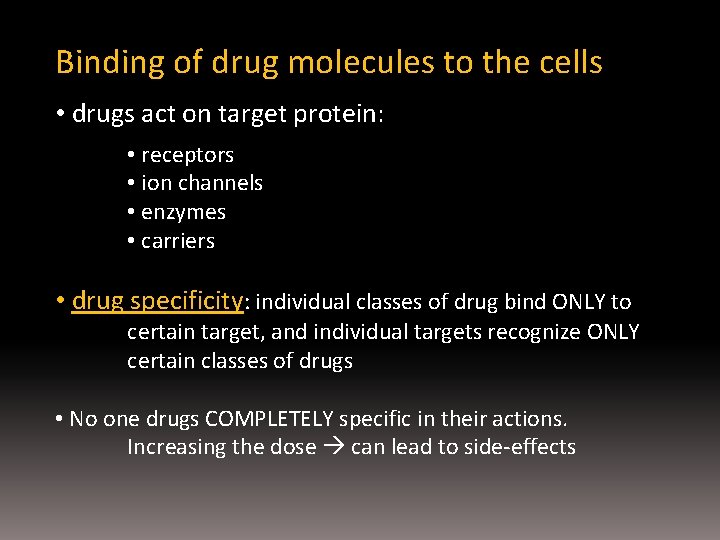
Binding of drug molecules to the cells • drugs act on target protein: • receptors • ion channels • enzymes • carriers • drug specificity: individual classes of drug bind ONLY to certain target, and individual targets recognize ONLY certain classes of drugs • No one drugs COMPLETELY specific in their actions. Increasing the dose can lead to side-effects
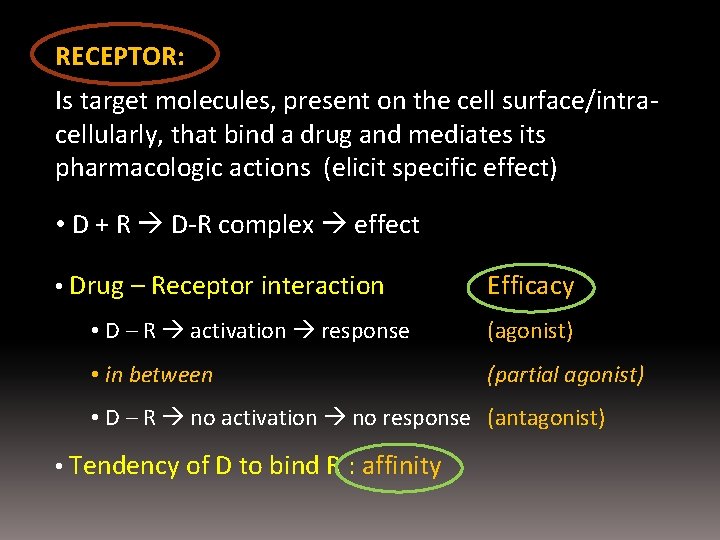
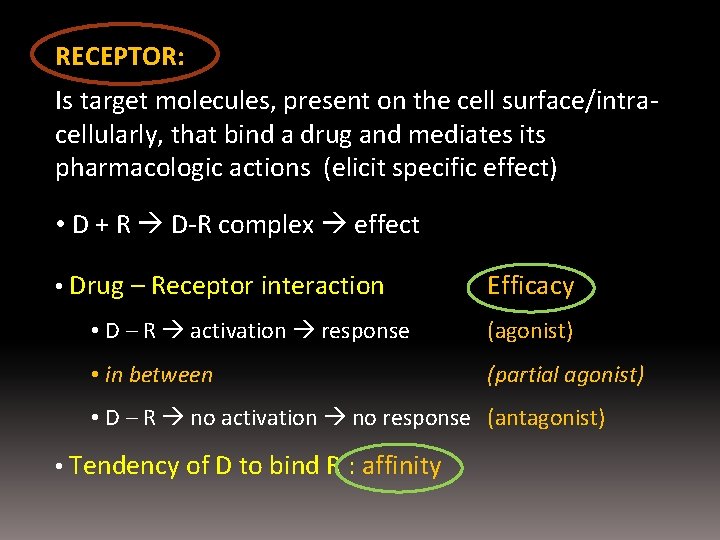
RECEPTOR: Is target molecules, present on the cell surface/intracellularly, that bind a drug and mediates its pharmacologic actions (elicit specific effect) • D + R D-R complex effect • Drug – Receptor interaction Efficacy • D – R activation response (agonist) • in between (partial agonist) • D – R no activation no response (antagonist) • Tendency of D to bind R : affinity
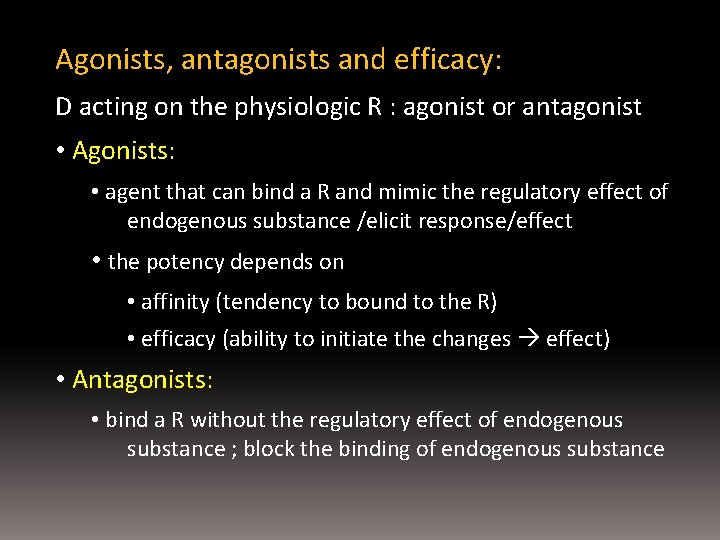
Agonists, antagonists and efficacy: D acting on the physiologic R : agonist or antagonist • Agonists: • agent that can bind a R and mimic the regulatory effect of endogenous substance /elicit response/effect • the potency depends on • affinity (tendency to bound to the R) • efficacy (ability to initiate the changes effect) • Antagonists: • bind a R without the regulatory effect of endogenous substance ; block the binding of endogenous substance
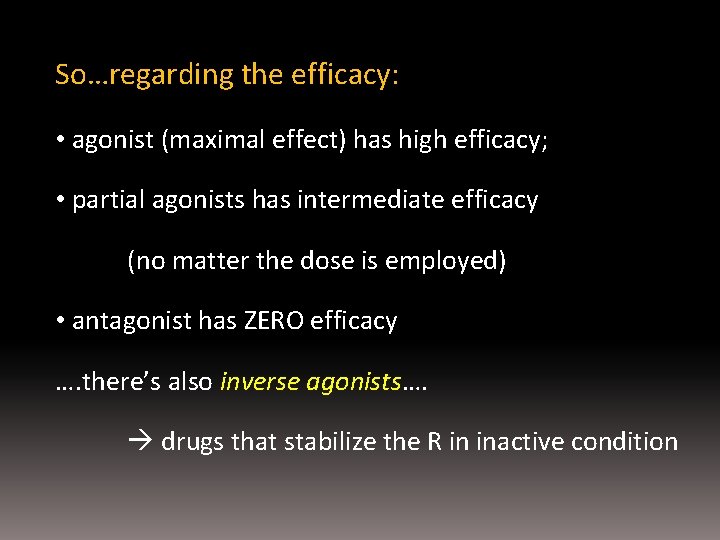
So…regarding the efficacy: • agonist (maximal effect) has high efficacy; • partial agonists has intermediate efficacy (no matter the dose is employed) • antagonist has ZERO efficacy …. there’s also inverse agonists…. drugs that stabilize the R in inactive condition
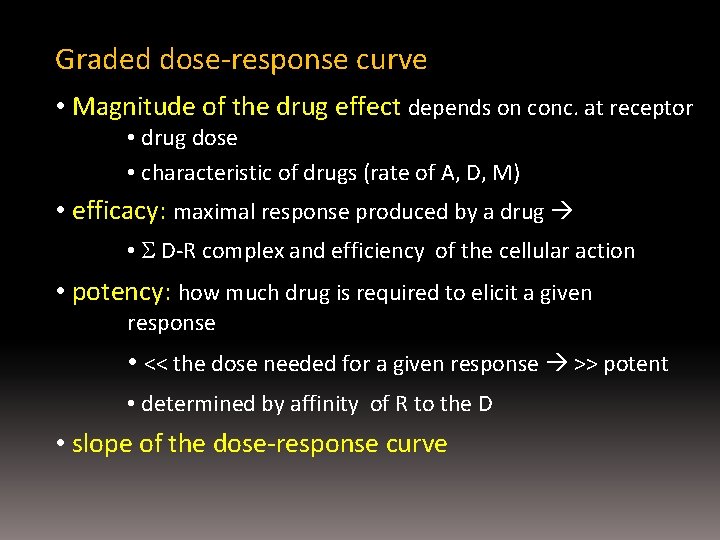
Graded dose-response curve • Magnitude of the drug effect depends on conc. at receptor • drug dose • characteristic of drugs (rate of A, D, M) • efficacy: maximal response produced by a drug • D-R complex and efficiency of the cellular action • potency: how much drug is required to elicit a given response • << the dose needed for a given response >> potent • determined by affinity of R to the D • slope of the dose-response curve

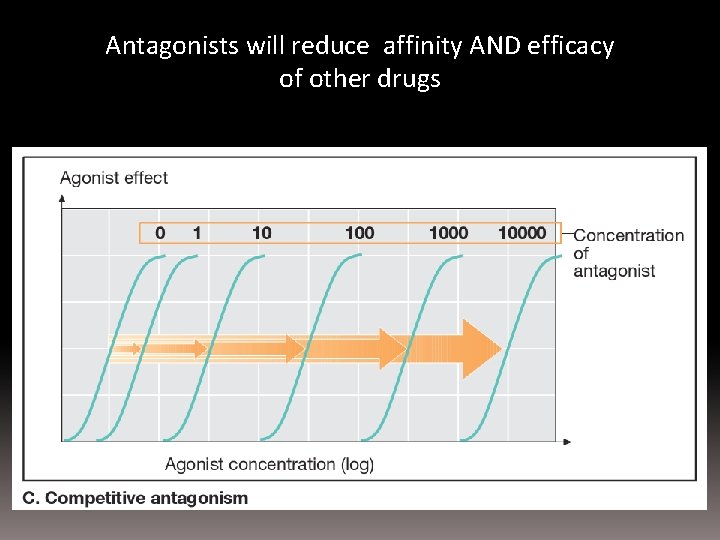
Binding of D to the R: • If >2 D compete for the same R each will reduce affinity of the other • Drug antagonism if the effect of one drug is diminished in the presence of another drug a. chemical antagonism (interaction in solution) b. PK antagonism (affecting A, D, M, E) c. antagonism by R block ( both drugs bind to the same R); d. non-competitive antagonism (drug interrupt R - effector) e. Physiological antagonism (2 drugs produce opposing physiologic effect)
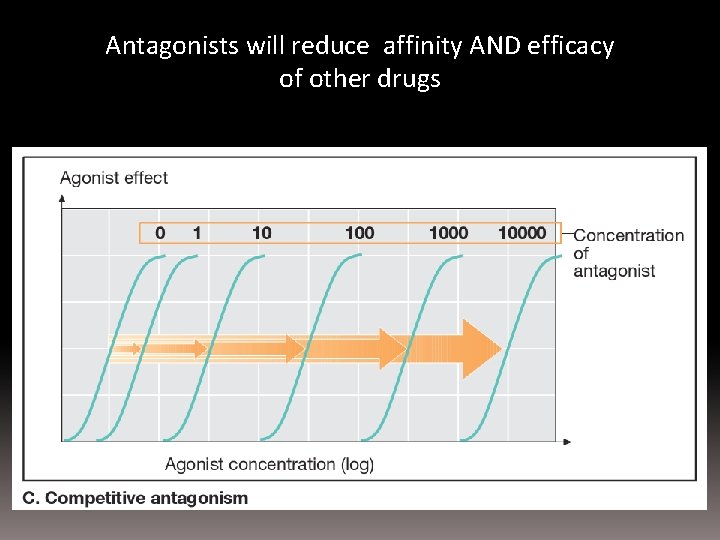
Antagonists will reduce affinity AND efficacy of other drugs
Desensitization & Tachyphylaxis • The loss of a drug’s effect, esp. if it’s given repeatedly /continuously • It takes time to happen & to recover (days – weeks) • Mechanism involved: a. changes in R b. loss of R c. exhaustions of mediators d. enhanced D metabolism e. compensatory physiological mechanism f. extrusion of D from the cells (resistance)
a. Change in R: • usually happen to R directly coupled to ion channels • exp: neurotransmitter to it’s R b. Loss of R = down regulation • prolong exposure to agonist of R • (R are taken by the cells by endocytosis) • exp: B-adrenoceptor c. Exhaustion of mediators • essential mediators is depleted • exp: amphetamine release amine from nerve terminal • if the amine stores is depleted tachyphylaxis

d. Increased metabolic degradation: • tolerance to some drugs: repeated administration of the same dose lower plasma conc. • exp: barbiturate e. Physiological adaptation • effect is nullified by homeostatic response • exp: prolong use of HCT activates RAA system
PHARMACODYNAMIC Molecular aspects
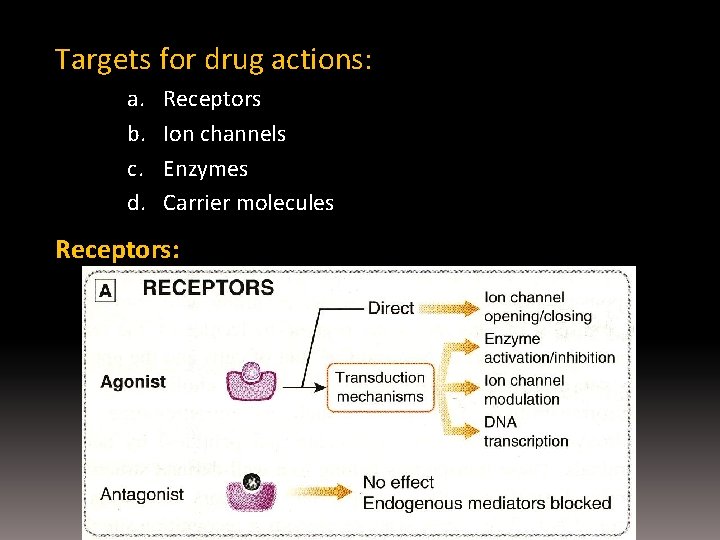
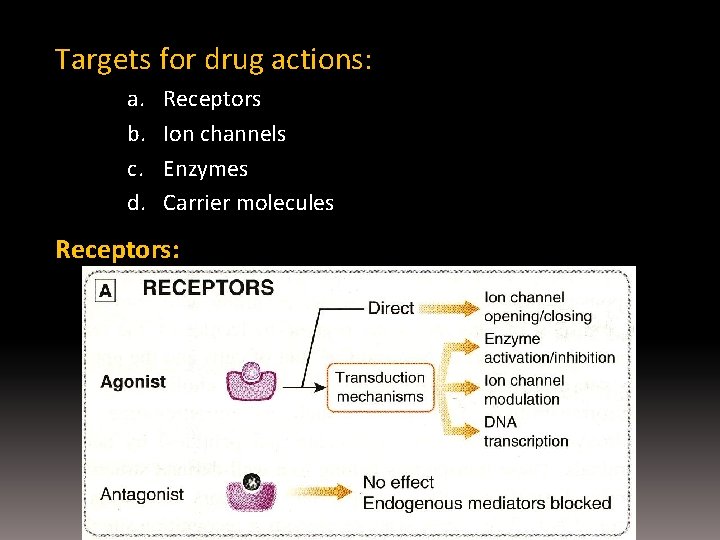
Targets for drug actions: a. b. c. d. Receptors Ion channels Enzymes Carrier molecules Receptors:
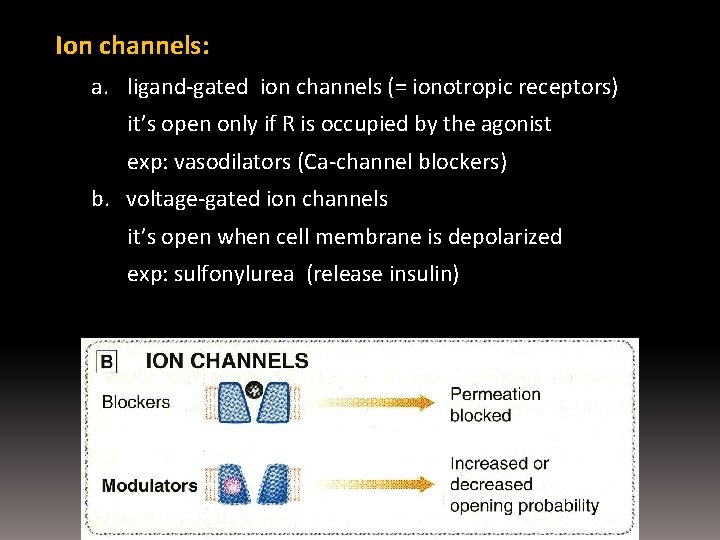
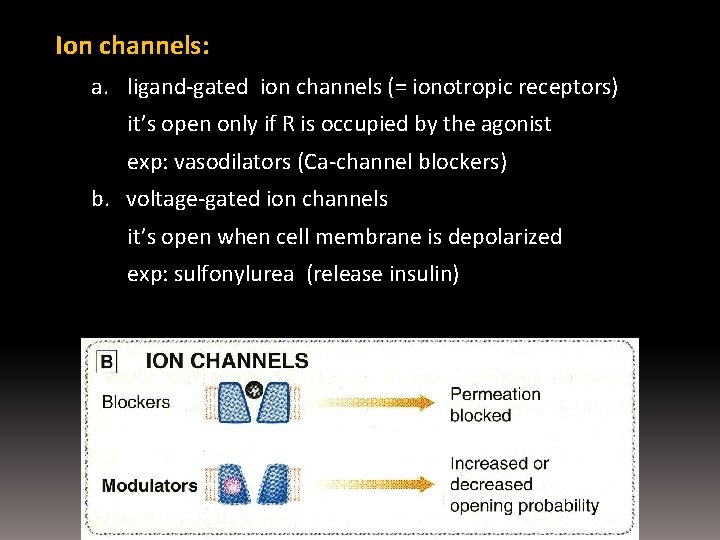
Ion channels: a. ligand-gated ion channels (= ionotropic receptors) it’s open only if R is occupied by the agonist exp: vasodilators (Ca-channel blockers) b. voltage-gated ion channels it’s open when cell membrane is depolarized exp: sulfonylurea (release insulin)
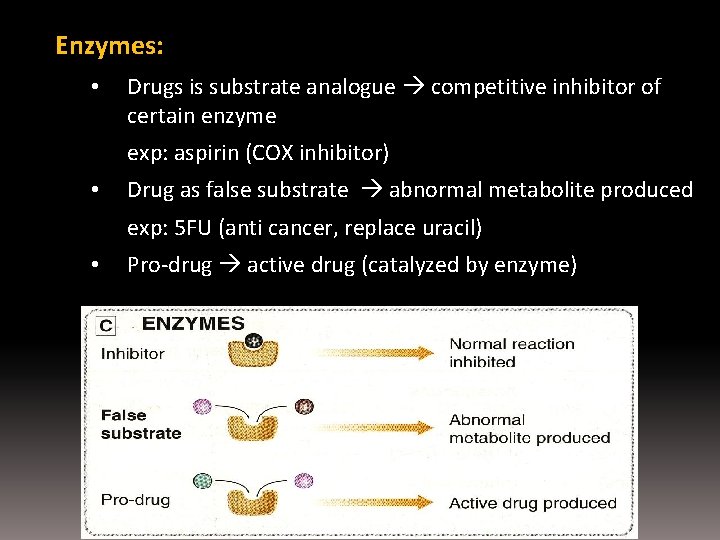
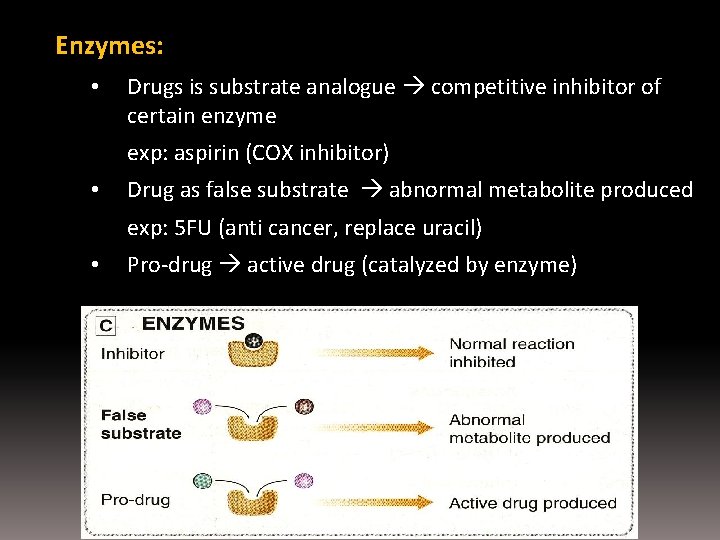
Enzymes: • Drugs is substrate analogue competitive inhibitor of certain enzyme exp: aspirin (COX inhibitor) • Drug as false substrate abnormal metabolite produced exp: 5 FU (anti cancer, replace uracil) • Pro-drug active drug (catalyzed by enzyme)
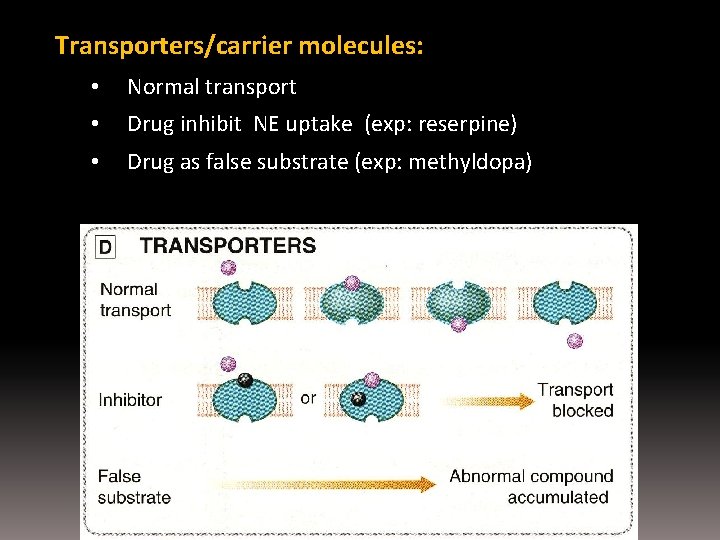
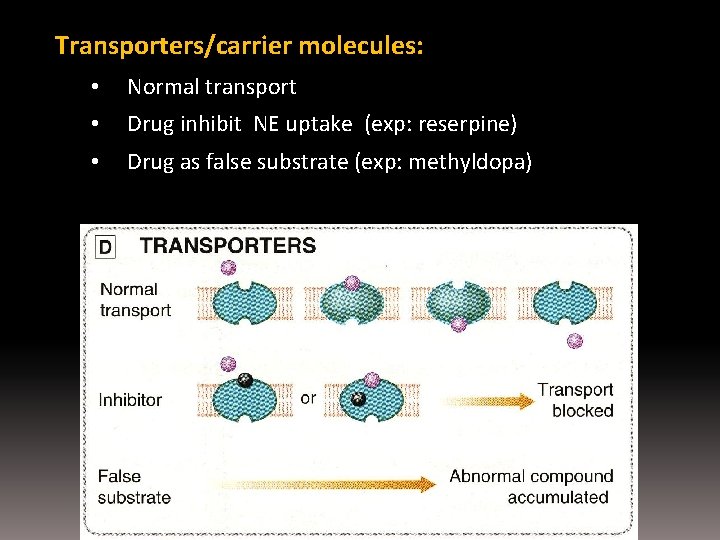
Transporters/carrier molecules: • Normal transport • Drug inhibit NE uptake (exp: reserpine) • Drug as false substrate (exp: methyldopa)
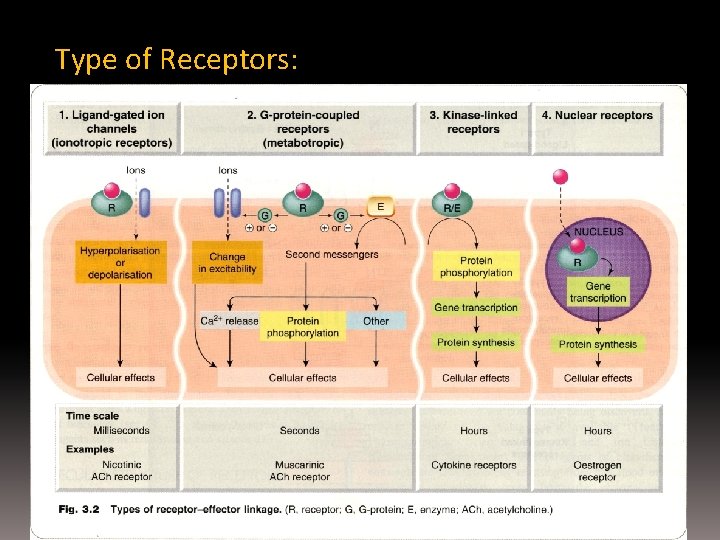
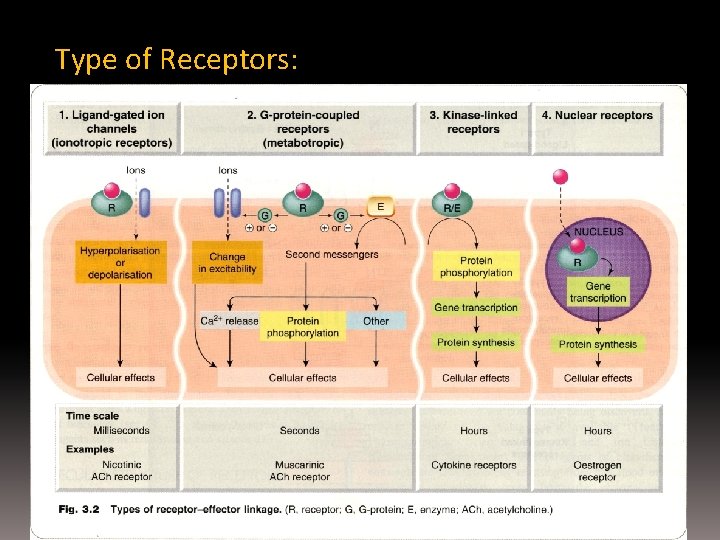
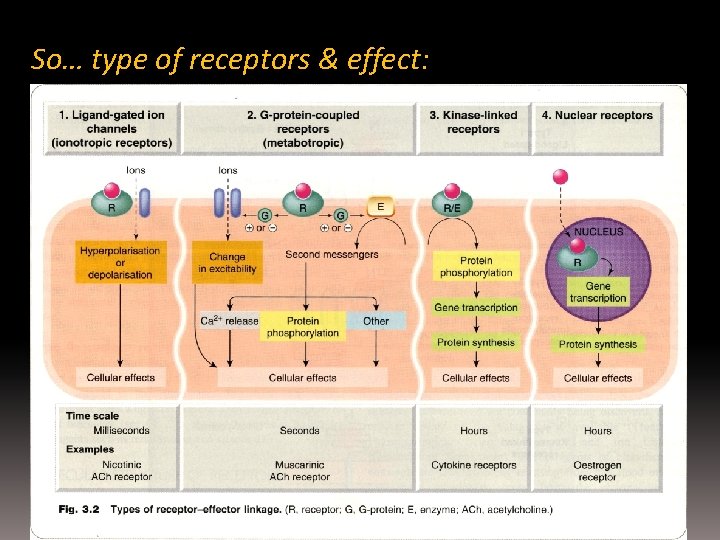
Type of Receptors:
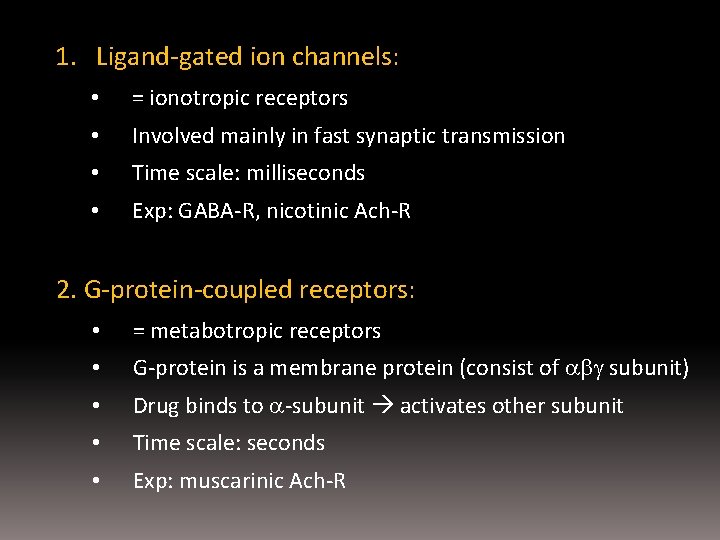
1. Ligand-gated ion channels: • = ionotropic receptors • Involved mainly in fast synaptic transmission • Time scale: milliseconds • Exp: GABA-R, nicotinic Ach-R 2. G-protein-coupled receptors: • = metabotropic receptors • G-protein is a membrane protein (consist of subunit) • Drug binds to -subunit activates other subunit • Time scale: seconds • Exp: muscarinic Ach-R

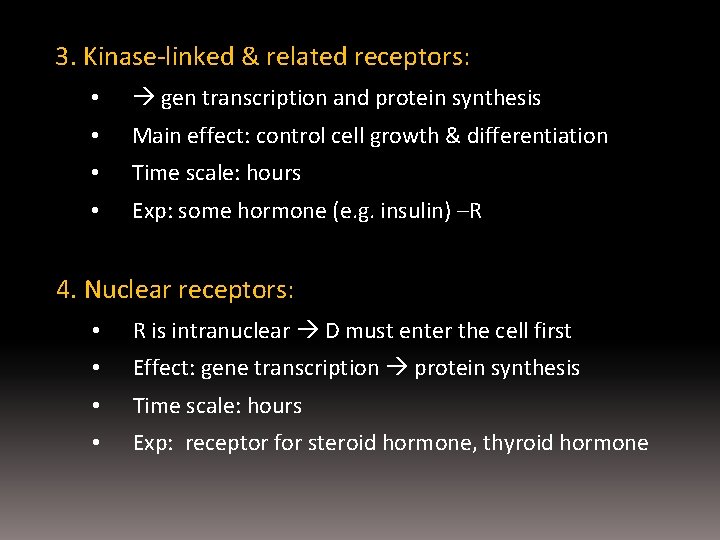
3. Kinase-linked & related receptors: • gen transcription and protein synthesis • Main effect: control cell growth & differentiation • Time scale: hours • Exp: some hormone (e. g. insulin) –R 4. Nuclear receptors: • R is intranuclear D must enter the cell first • Effect: gene transcription protein synthesis • Time scale: hours • Exp: receptor for steroid hormone, thyroid hormone


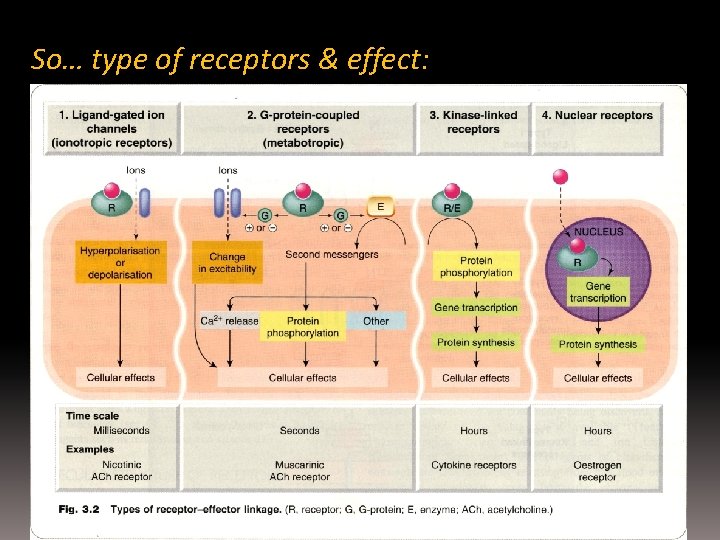
So… type of receptors & effect:
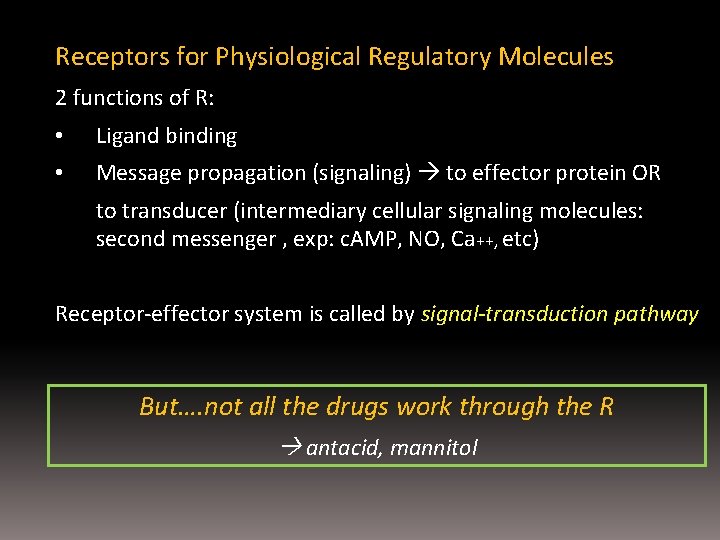
Receptors for Physiological Regulatory Molecules 2 functions of R: • Ligand binding • Message propagation (signaling) to effector protein OR to transducer (intermediary cellular signaling molecules: second messenger , exp: c. AMP, NO, Ca++, etc) Receptor-effector system is called by signal-transduction pathway But…. not all the drugs work through the R antacid, mannitol

Regulation of R: Regulation of synthesis & degradation • Multiple mechanism • From other R OR from feedback regulation by their own signaling output Includes: • Desensitization: cont stimulation of cells by agonist • = down regulation = adaptation = refractoriness • The phenomenon is called by TACHYPHILAXIS !!!
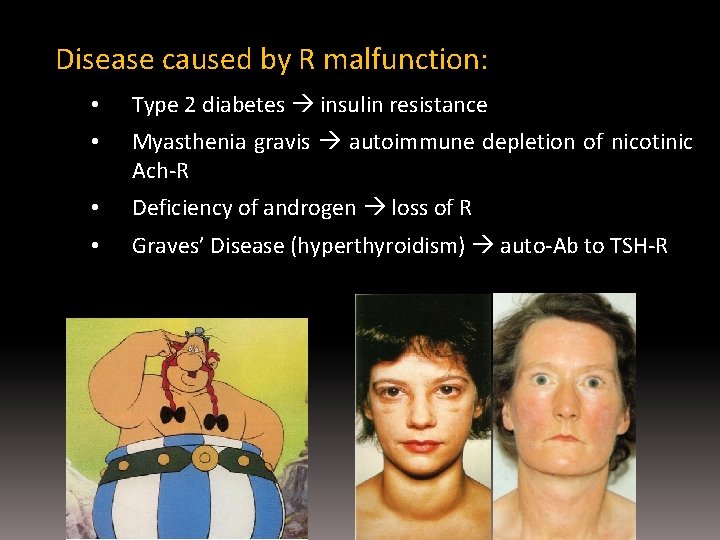
Disease caused by R malfunction: • Type 2 diabetes insulin resistance • Myasthenia gravis autoimmune depletion of nicotinic Ach-R • Deficiency of androgen loss of R • Graves’ Disease (hyperthyroidism) auto-Ab to TSH-R
PHARMACODYNAMIC VARIABILITY

Concentration-effect relationship 4 characteristic variables: • Potency • Maximal efficacy • Slope • Individual variation PD variability: • Between subjects AND Within subject • Factors affecting: internal and external • • Genetic Age Disease Other drugs Alter PK of the drug effect • sub-theraputic • therapeutic • toxicity
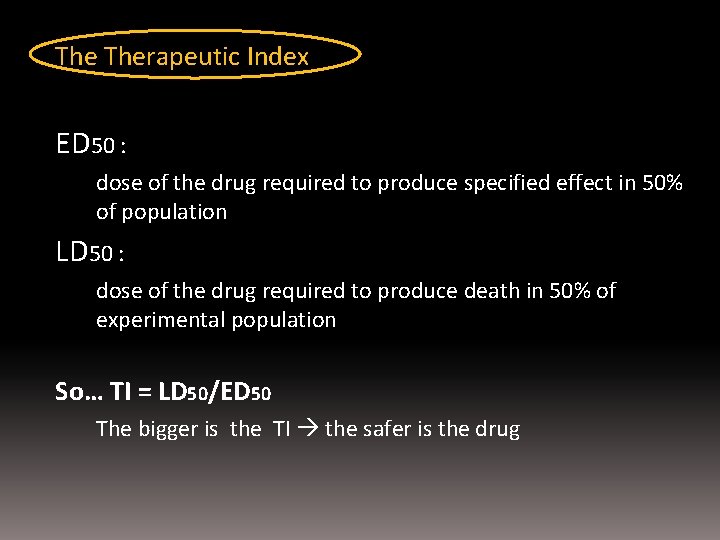
The Therapeutic Index ED 50 : dose of the drug required to produce specified effect in 50% of population LD 50 : dose of the drug required to produce death in 50% of experimental population So… TI = LD 50/ED 50 The bigger is the TI the safer is the drug

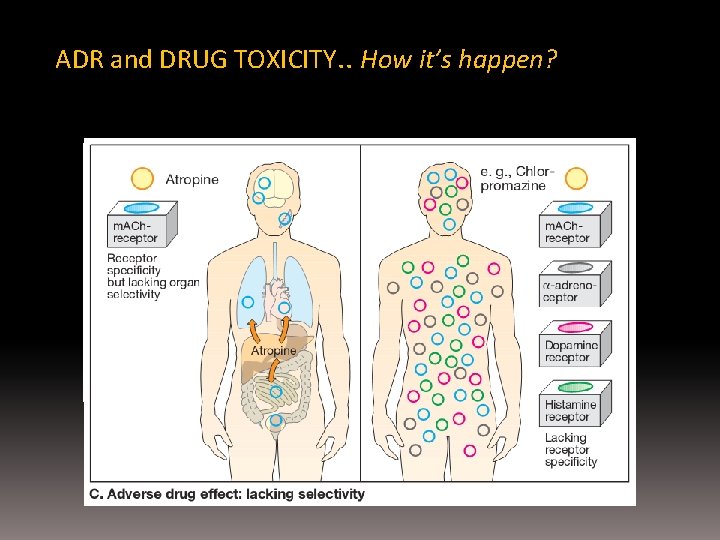
ADR and DRUG TOXICITY ADR (Adverse Drug Reaction) > any drug has potential to do harm > it is the common cause of iatrogenic disease! > idiosyncratic: if it’s encountered infrequently - mechanism-based (angioedema) OR - off-target action (anaphylaxis to penicillin)
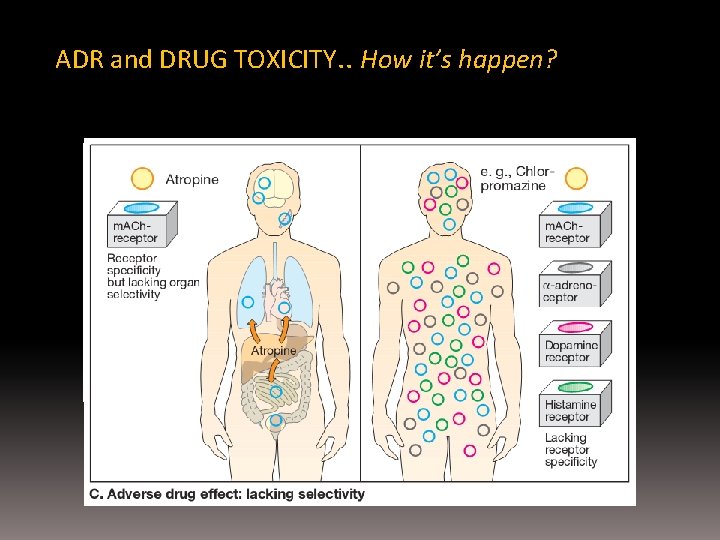
ADR and DRUG TOXICITY. . How it’s happen?

Therapeutic Drug Monitoring …Many factors that alter drug disposition …need TDM (in special case) > drug with narrow therapeutic window (range of plasma conc. between required for efficacy – toxicity occurs) > drug with low TI > drug with effect (+ or -) that is difficult to monitor > drug with large variability of plasma conc.
Be careful with using drugs. . .
 Dr dwi indria anggraini
Dr dwi indria anggraini Pharmacodynamic definition
Pharmacodynamic definition Panca budhindriya
Panca budhindriya Mikturisi
Mikturisi Peristiwa bersejarah epidemiologi wabah diare di london
Peristiwa bersejarah epidemiologi wabah diare di london Dyah anggraini gunadarma
Dyah anggraini gunadarma Ica puspita dewi anggraini
Ica puspita dewi anggraini Dea anggraini viral
Dea anggraini viral Ica puspita dewi anggraini
Ica puspita dewi anggraini Interpretasi timpanometri
Interpretasi timpanometri Ica puspita dewi anggraini
Ica puspita dewi anggraini Frontalna rovina
Frontalna rovina Morfolgia
Morfolgia Odchýlky od vetnej stavby
Odchýlky od vetnej stavby Naklonená rovina
Naklonená rovina Kolmica dopadu
Kolmica dopadu Středosibiřská vysočina mapa
Středosibiřská vysočina mapa Regio hypochondriaca
Regio hypochondriaca Naklonená rovina príklady
Naklonená rovina príklady Nakloněná rovina prezentace
Nakloněná rovina prezentace Naklonená rovina 4 ročník
Naklonená rovina 4 ročník Znelé a neznelé spoluhlásky
Znelé a neznelé spoluhlásky Jednoduche stroje priklady
Jednoduche stroje priklady Operace symetrie
Operace symetrie Průčelná poloha
Průčelná poloha Nakloněná rovina příklady v praxi
Nakloněná rovina příklady v praxi Typy krajiny podle nadmořské výšky
Typy krajiny podle nadmořské výšky αεα
αεα Anatomické roviny
Anatomické roviny Psak 71 dwi martani
Psak 71 dwi martani Rumus dwi koordinat
Rumus dwi koordinat Psak 72
Psak 72 Dwi hartanto
Dwi hartanto Dwi rita kusumawati
Dwi rita kusumawati Dwi marta nurjaya
Dwi marta nurjaya Klasifikasi dehidrasi pada anak
Klasifikasi dehidrasi pada anak Contoh perhitungan psak 73
Contoh perhitungan psak 73 Psak 16 dwi martani
Psak 16 dwi martani Drg dwi imbang lestari
Drg dwi imbang lestari