Pediatric case conference Present Patient Data n n







- Slides: 59

Pediatric case conference Present: 江泳昇 醫師
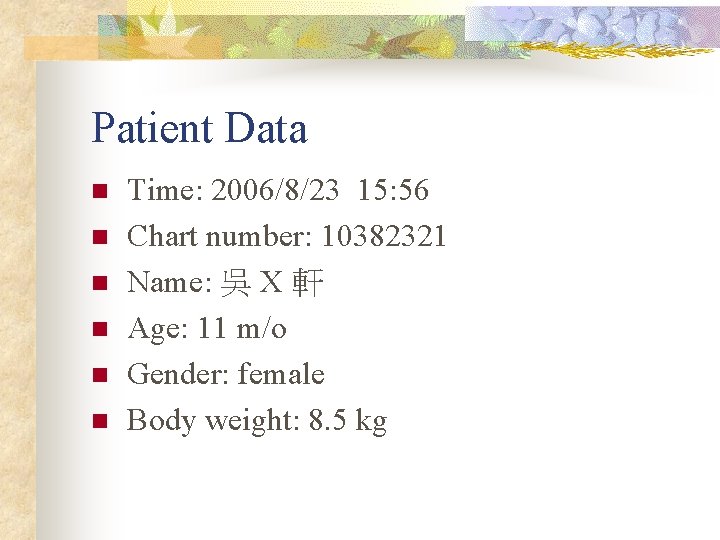
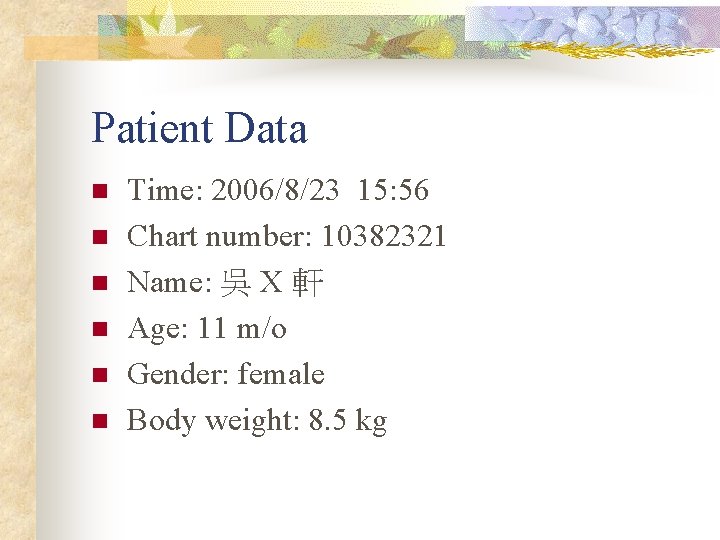
Patient Data n n n Time: 2006/8/23 15: 56 Chart number: 10382321 Name: 吳 X 軒 Age: 11 m/o Gender: female Body weight: 8. 5 kg
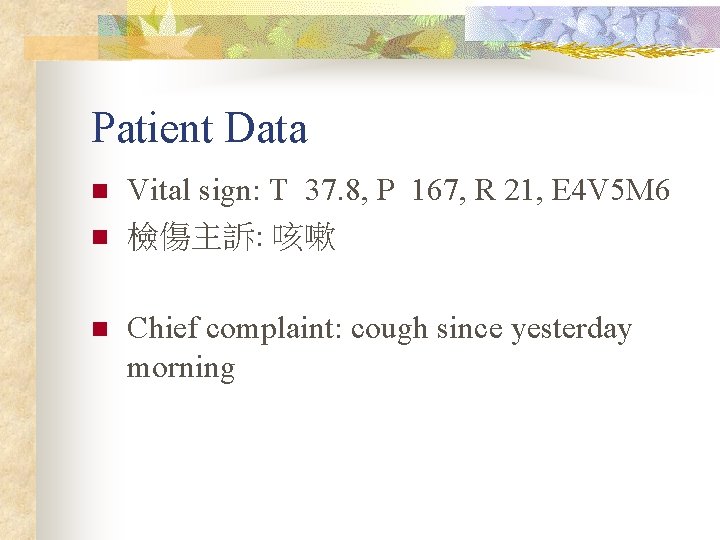
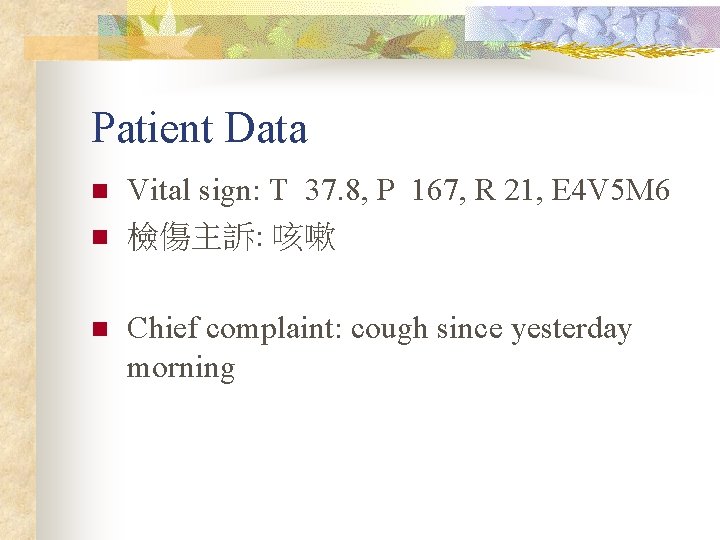
Patient Data n n n Vital sign: T 37. 8, P 167, R 21, E 4 V 5 M 6 檢傷主訴: 咳嗽 Chief complaint: cough since yesterday morning
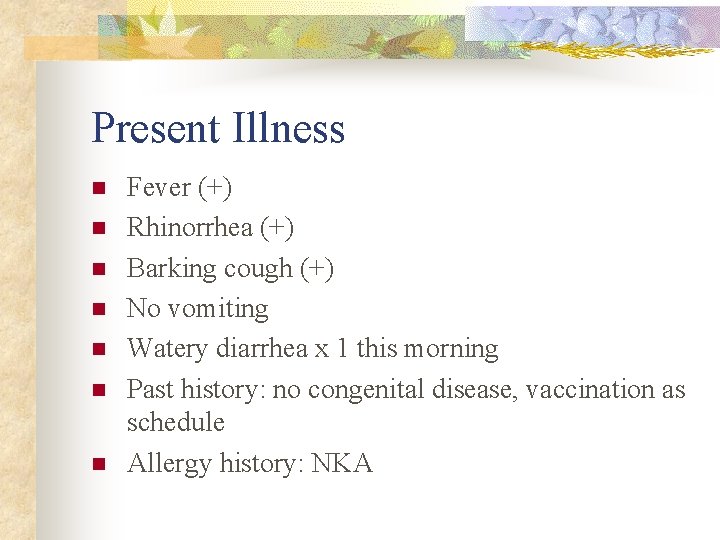
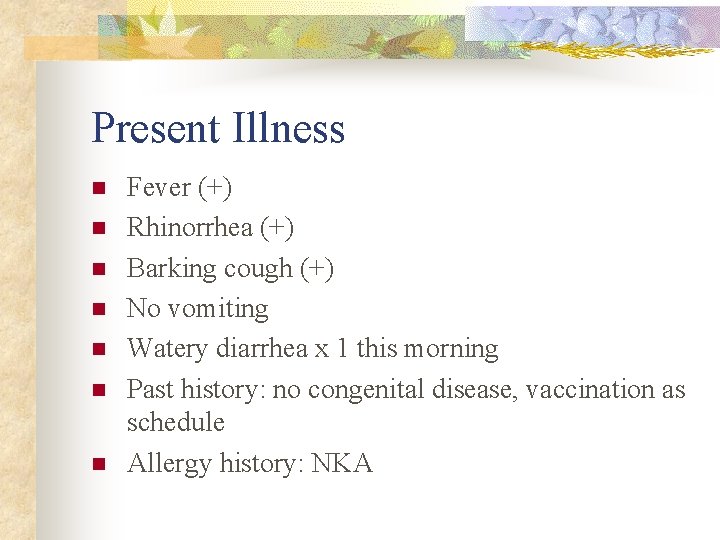
Present Illness n n n n Fever (+) Rhinorrhea (+) Barking cough (+) No vomiting Watery diarrhea x 1 this morning Past history: no congenital disease, vaccination as schedule Allergy history: NKA
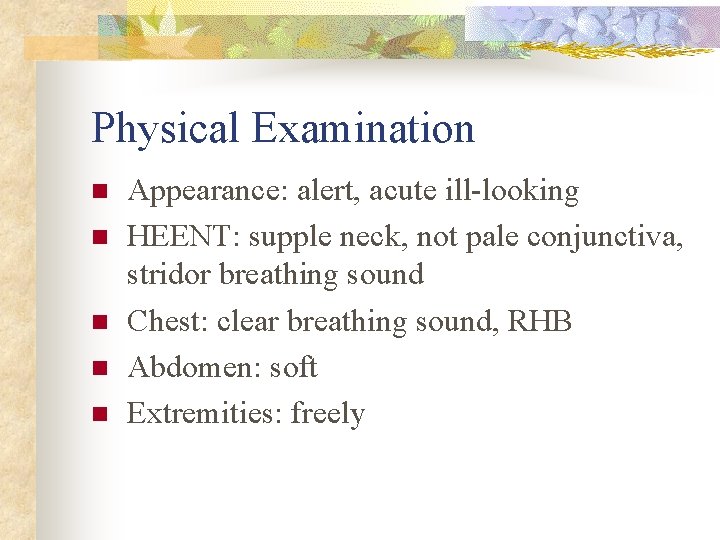
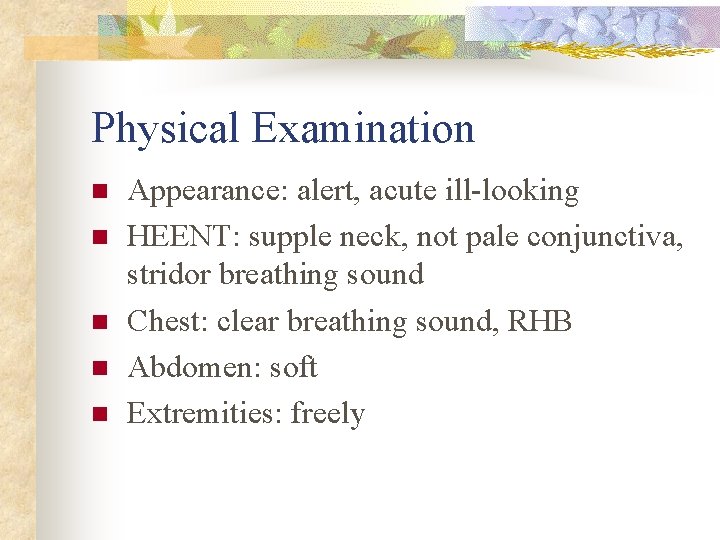
Physical Examination n n Appearance: alert, acute ill-looking HEENT: supple neck, not pale conjunctiva, stridor breathing sound Chest: clear breathing sound, RHB Abdomen: soft Extremities: freely
Initial Impression n Croup
Initial order (11 min) n n Dexamethasone 1 PC IM stat, Bosmin 1 PC inhalation stat CXR, C-spine extension lateral view


Further order n n Further order (2 hr 24 min): Bosmin 1 PC inhalation stat Further order (3 hr 14 min): Consult ENT (drooling)
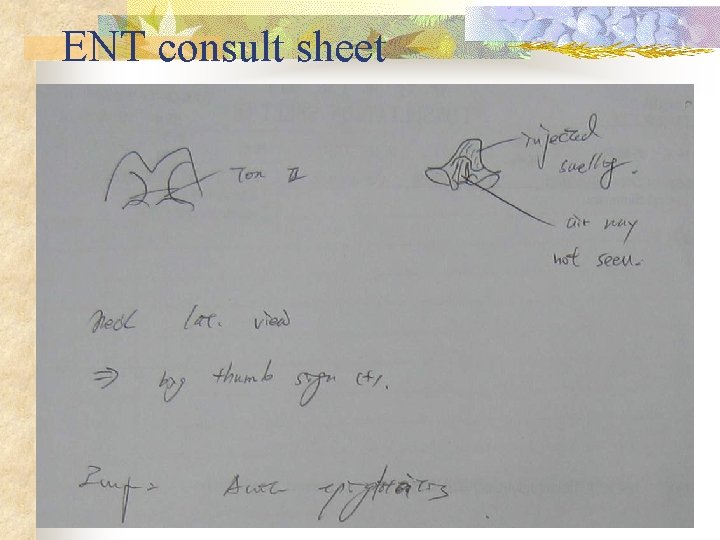
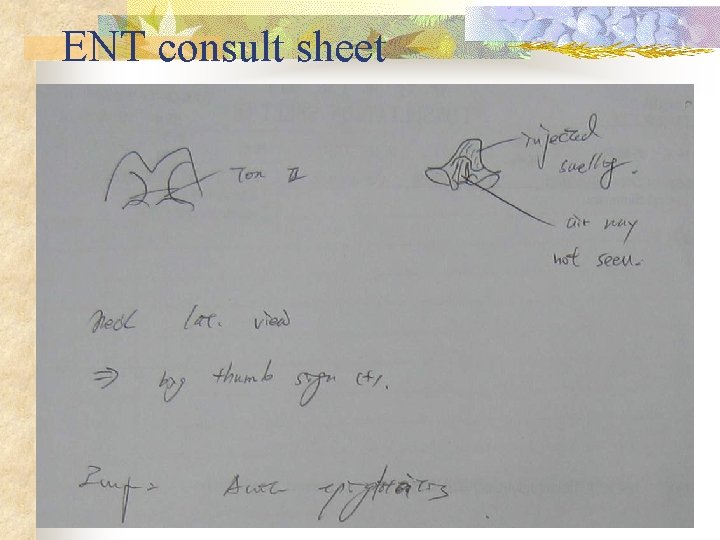
ENT consult sheet
Further order n n n Admit to PICU 9 A 963 Rocephin 200 mg IV stat CBC/DC, CRP, B/C, BUN, Sugar, IV with D 5 S 1/4 run 40 ml/hr
Case 2 n n n Chart number: 20900544 Name: 林 X 南 Age: 11 w/o Gender: male Body weight: 6. 6 kg
Case 2 n n Chief Complaint: Shortness of breath and cough for 1 week
Present Illness n n n Fever up to 38 C on 7/10 Cough, Poor appetite, Poor activity 7/11 Dr 林如立's OPD URI was diagnosed 7/18 Shortness of breathing and cough LMD laryngiomalacia was told Shortness of breath and cough became more severe Dr朱世明's OPD admission
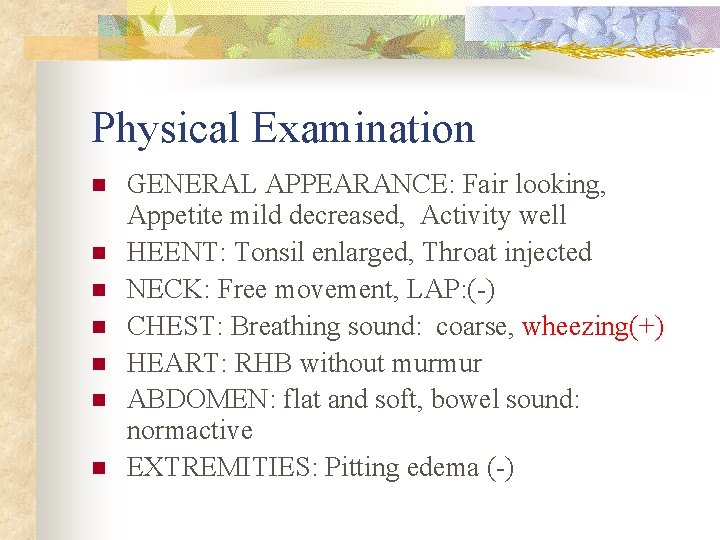
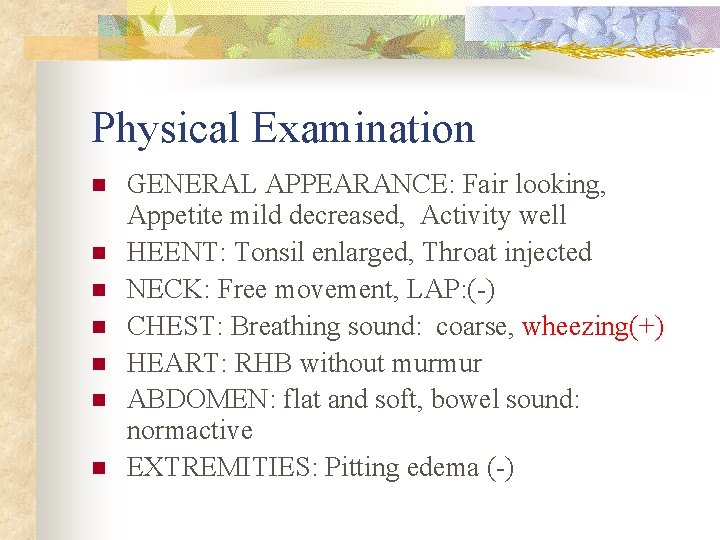
Physical Examination n n n GENERAL APPEARANCE: Fair looking, Appetite mild decreased, Activity well HEENT: Tonsil enlarged, Throat injected NECK: Free movement, LAP: (-) CHEST: Breathing sound: coarse, wheezing(+) HEART: RHB without murmur ABDOMEN: flat and soft, bowel sound: normactive EXTREMITIES: Pitting edema (-)
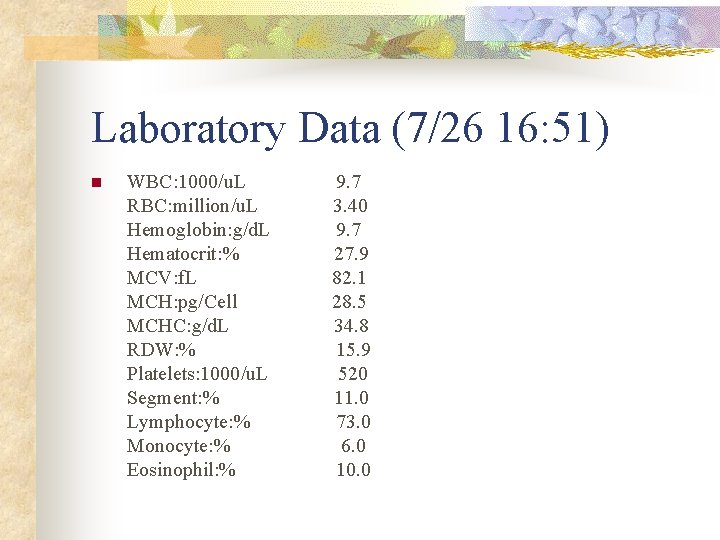
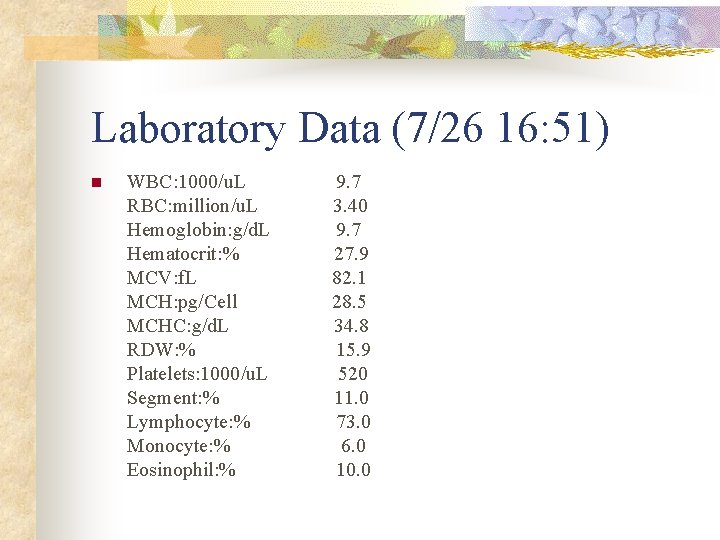
Laboratory Data (7/26 16: 51) n WBC: 1000/u. L RBC: million/u. L Hemoglobin: g/d. L Hematocrit: % MCV: f. L MCH: pg/Cell MCHC: g/d. L RDW: % Platelets: 1000/u. L Segment: % Lymphocyte: % Monocyte: % Eosinophil: % 9. 7 3. 40 9. 7 27. 9 82. 1 28. 5 34. 8 15. 9 520 11. 0 73. 0 6. 0 10. 0
Impression n n R/O bronchiolitis R/O asthma
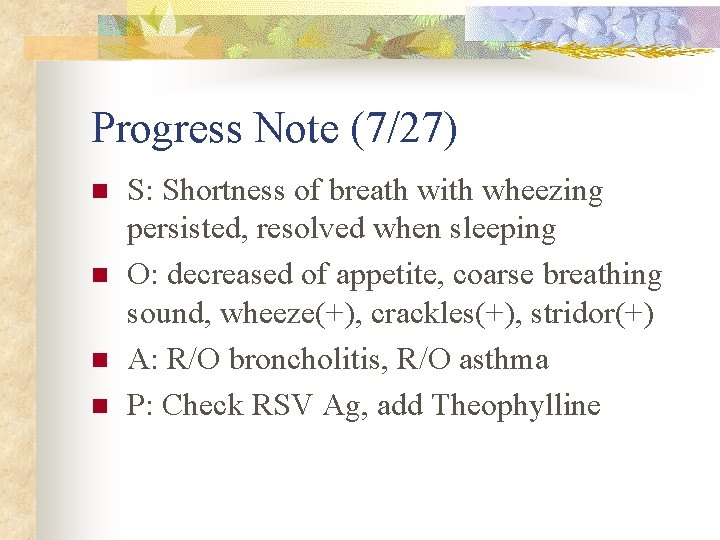
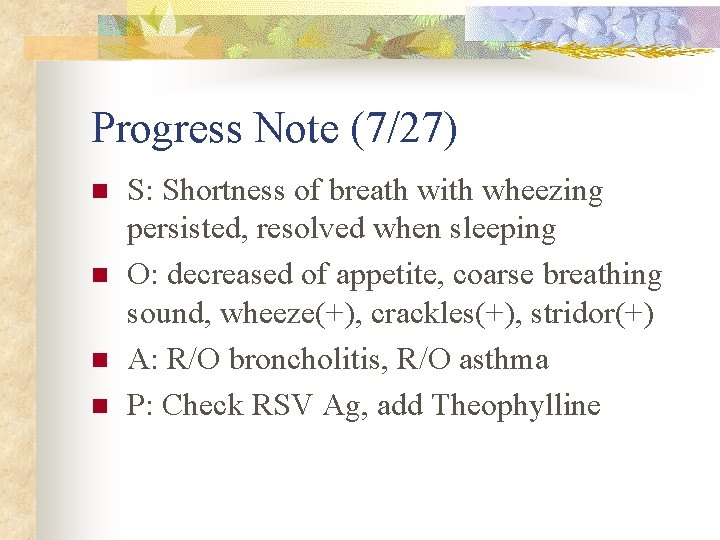
Progress Note (7/27) n n S: Shortness of breath with wheezing persisted, resolved when sleeping O: decreased of appetite, coarse breathing sound, wheeze(+), crackles(+), stridor(+) A: R/O broncholitis, R/O asthma P: Check RSV Ag, add Theophylline
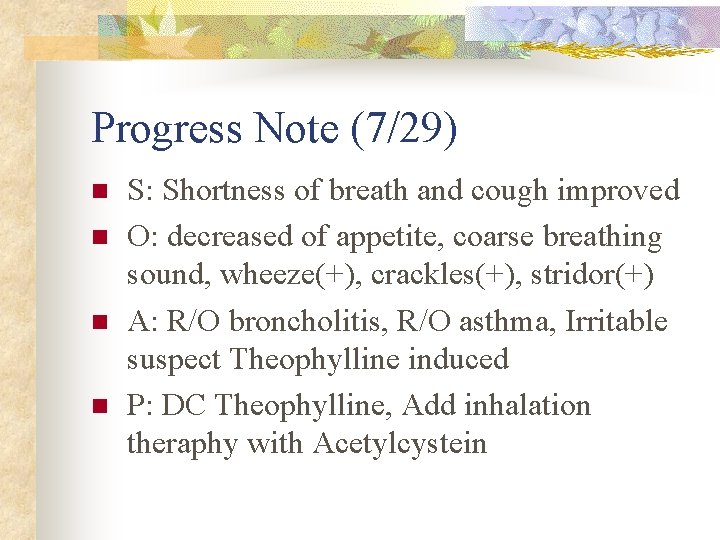
Progress Note (7/29) n n S: Shortness of breath and cough improved O: decreased of appetite, coarse breathing sound, wheeze(+), crackles(+), stridor(+) A: R/O broncholitis, R/O asthma, Irritable suspect Theophylline induced P: DC Theophylline, Add inhalation theraphy with Acetylcystein
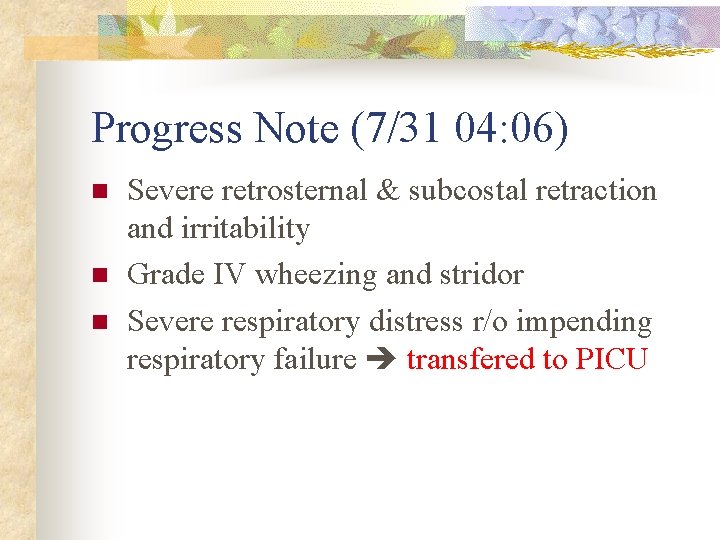
Progress Note (7/31 04: 06) n n n Severe retrosternal & subcostal retraction and irritability Grade IV wheezing and stridor Severe respiratory distress r/o impending respiratory failure transfered to PICU
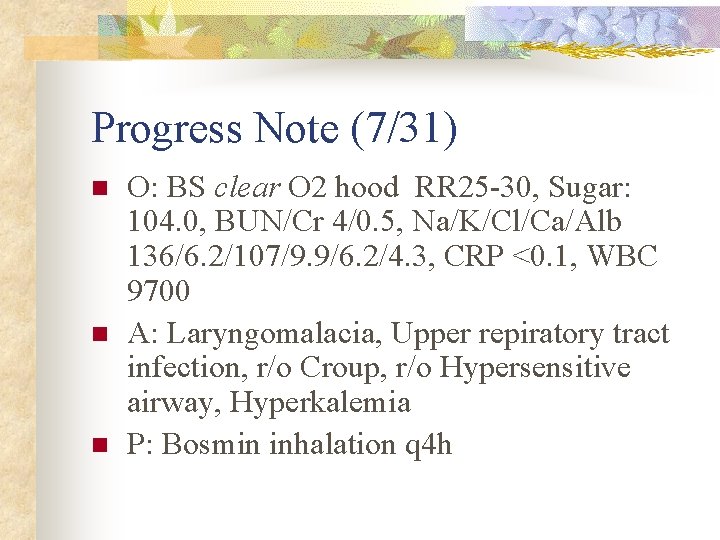
Progress Note (7/31) n n n O: BS clear O 2 hood RR 25 -30, Sugar: 104. 0, BUN/Cr 4/0. 5, Na/K/Cl/Ca/Alb 136/6. 2/107/9. 9/6. 2/4. 3, CRP <0. 1, WBC 9700 A: Laryngomalacia, Upper repiratory tract infection, r/o Croup, r/o Hypersensitive airway, Hyperkalemia P: Bosmin inhalation q 4 h
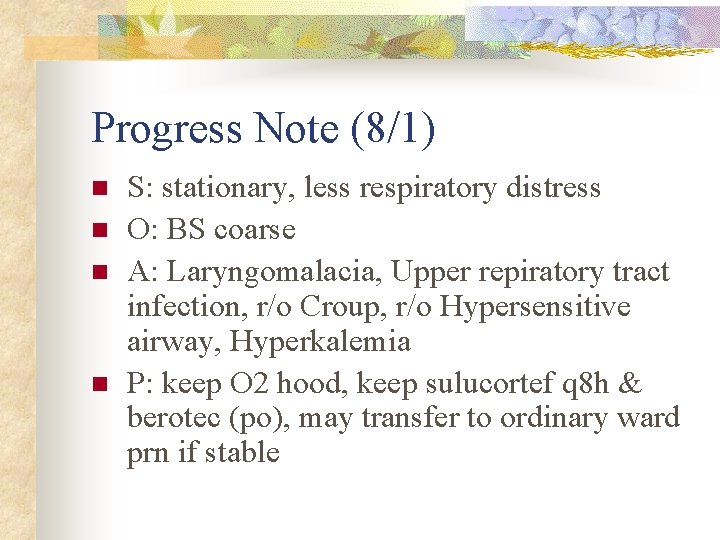
Progress Note (8/1) n n S: stationary, less respiratory distress O: BS coarse A: Laryngomalacia, Upper repiratory tract infection, r/o Croup, r/o Hypersensitive airway, Hyperkalemia P: keep O 2 hood, keep sulucortef q 8 h & berotec (po), may transfer to ordinary ward prn if stable
Progress Note (8/1) n n n respiratory condition gradually stablized bronchospasm with crying desaturation was still noted sometimes relatively stable condition transfer to ordinary ward
Progress Note (8/2) n n S: still SOB O: coarse breathing sound, stridor(+) A: 1. Acute bronchiolitis 2. Stridor r/o upper airway anomaly r/o infection-related upper airway obstruction P: 1. Bosmin inhalatin and chest care 2. solucortef treatment 3. check virus isolation, pertussis PCR, and chlamydia Ag
Progress Note (8/3) n n S: still intermittent SOB while irritable crying O: coarse breathing sound, stridor(+), rhonchi(+) A: 1. Acute bronchiolitis 2. Stridor r/o upper airway anomaly r/o infection-related upper airway obstruction P: 1. Bosmin inhalatin and chest care 2. solucortef treatment 3. Arrange 3 D CT for airway structure survey
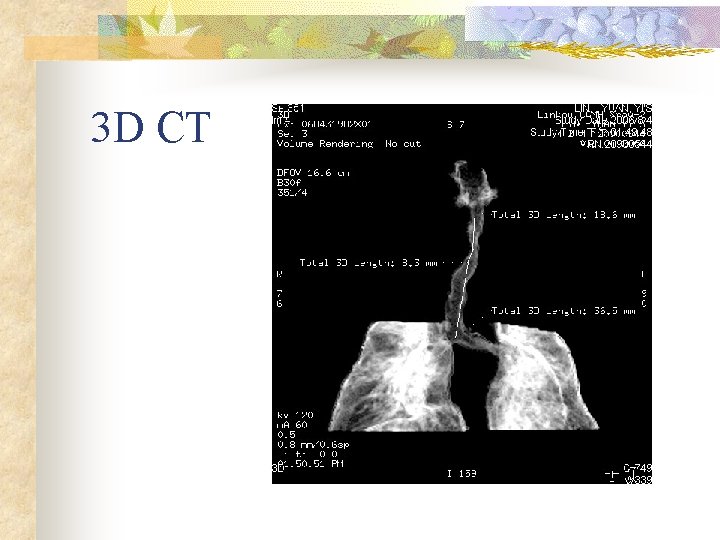
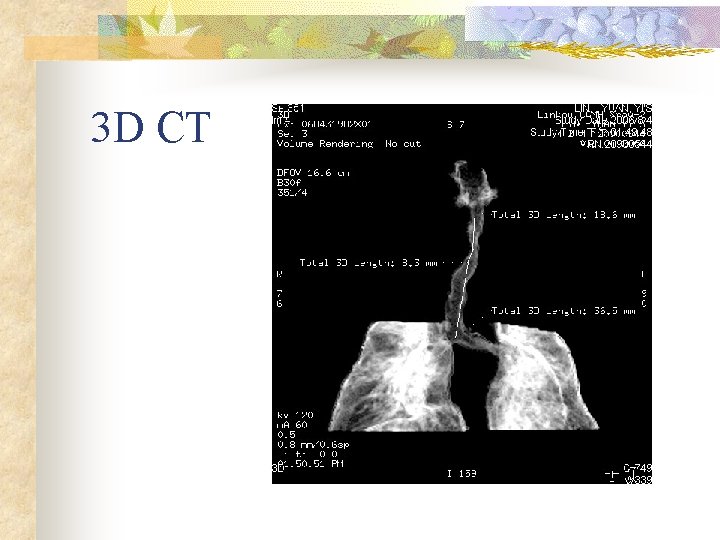
3 D CT
3 D CT n n n Subglottic tracheal stenosis Segmental 18. 6 mm from cord to steonsis area Stenosis severity 74% consult CVS and Chest
CVS consultation sheet n n Dilatation and tracheal stenting were indicated After discuss with patient’s mother, conservative treatment is preferred
Chest consultation sheet n n Bronchoscopy is indicated If the parents agree the examination, notify us
Progress Note (8/10) n n S: fair activity and appetite, No SOB or retraction if not crying, family refuse further evaluation (bronchoscopy) or treatment (operation) O: coarse breathing sound, wheeze(-), crackles(-), stridor(-), rhonchi(-) A: 1. Acute bronchiolitis, 2. subglottic tracheal stenosis, segmental, 3. left hydronephrosis P: supportive treatment
Final Diagnosis (8/12) n n 1. Acute bronchiolitis 2. subglottic tracheal stenosis, segmental
Discussion Stridor assessment: n n A thorough clinical history, a complete physical examination Tests: radiography, pulmonary function testing, and even airway visualization
Stridor assessment Age: n Congenital disorders (eg, vocal cord paralysis, laryngomalacia, and tracheomalacia) present in the first few weeks of life n Foreign body aspiration above six months of age (incidence peaking around two to three years of age )
Stridor assessment Age: n Retropharyngeal abscesses less than four years of age n Epiglottitis (past) between two and seven years of Age H. influenzae type B vaccine present (now) greater than seven years n Peritonsillar abscess older than 10 years of age
Stridor assessment Onset and severity: n Foreign body aspiration sudden onset of stridor, with or without respiratory distress, and without other physical findings n bacterial infections rapidly progressive respiratory distress, drooling, and gasping for air accompanied by other upper respiratory symptoms
Stridor assessment Onset and severity: n Severe allergic reactions (anaphylaxis and laryngeal edema) abrupt and severe onset n Viral croup a more insidious way, with steady, progressive respiratory distress, more than 90 percent of all cases of stridor
Stridor assessment n n n Chronic or recurrent stridor foreign body, subglottic stenosis, vascular rings, or a tumor Asthma recurrent noisy breathing associated with cough and exercise intolerance Vocal cord dysfunction intermittent episodes of stridor or wheezing in which the onset and cessation are abrupt
Stridor assessment Associated symptoms: n more serious bacterial infections appear ill or toxic (fever can neither diagnoses nor excludes, 25% afebrile) n Drooling and a muffled voice supraglottic obstruction n Drooling and dysphagia foreign body or a mass compresses the anterior esophageal wall
Stridor assessment Associated symptoms: n A change in the voice tone with stridor a laryngeal lesion such as vocal cord injury due to inflammation (eg, croup) or paralysis n Respiratory distress and stridor related to feeding swallowing dysfunction or gastroesophageal reflux induced aspiration
Stridor assessment Associated symptoms: n Rash, hypotension, and wheezing with acute onset of stridor allergic reaction with angioedema
Stridor assessment Physical examination: n Surgical scars around the upper chest or neck vocal cord lesion, or tracheal or subglottic stenosis n Neck edema accompanied by fever retropharyngeal or peritonsillar abscess n Clubbing an underlying congenital heart disease or bronchiectasis
Stridor assessment Physical examination: n Cafe au lait spots head and neck neurofibromas, which can involve the airway n Auscultation placed over the child's mouth and neck to determine the origin of the stridor
Stridor assessment Physical examination: n Snoring nasal, nasopharyngeal, or oropharyngeal obstruction n Inspiratory stridor obstruction above the glottis n Expiratory stridor intrathoracic obstruction
Stridor assessment Physical examination: n Biphasic stridor either critical obstruction (at any level), or an obstruction in the area between the glottis and subglottis
Stridor assessment Neck radiographs: n Retropharyngeal abscesses a retropharyngeal space greater than 7 mm anterior to the inferior border of the second cervical vertebral body, or a retrotracheal space greater than 14 mm in children anterior to the inferior border of the sixth cervical vertebral body
Stridor assessment Neck radiographs: n Croup AP view steeple sign subglottic arch becomes edematous n Croup lateral view distended hypopharynx and subglottic haziness
Stridor assessment Neck radiographs: n epiglottitis lateral view an edematous epiglottis with the thumb sign, enlarged aryepiglottic folds, and a ballooned hypopharyngeal airway n 70 percent of all patients with epiglottitis have radiographic findings interpreted as normal
Stridor assessment Chest radiographs: n Vascular rings a right aortic arch n Foreign body aspiration mediastinal shift, unilateral hyperinflation, atelectasis, or the actual foreign body
Stridor assessment Other studies: n Barium swallow to identify swallowing dysfunction, vascular rings, mediastinal masses, GERD, or esophageal abnormalities
Stridor assessment Other studies: n CT scan 1. retropharyngeal cellulitis with compression of the pyriform sinuses and an anterior deviation of the trachea. 2. look for enlarged lymph nodes, tumors, aberrant arteries, and vascular rings. 3. show narrowing of the airway suggestive of tracheal stenosis.
Stridor assessment Other studies: n Nasopharyngoscopy epiglottitis, bacterial tracheitis, laryngomalacia, and anatomic defects between the nose and pharynx, as well as in the assessment of vocal cord movement
Stridor assessment Other studies: n Flexible bronchoscopy to identify abnormalities in airway dynamics. n Rigid laryngoscopy and bronchoscopy the gold standard for evaluation and diagnosis of subglottic, tracheal, and central airway lesions.
Stridor assessment Other studies: n Rigid bronchoscope allows to take biopsy samples, remove foreign bodies, and dilate stenosed airways if necessary.




Thanks for Your Attention !!