Outpatient Management of COPD Ryan Nall MD Learning










- Slides: 39
Outpatient Management of COPD Ryan Nall MD
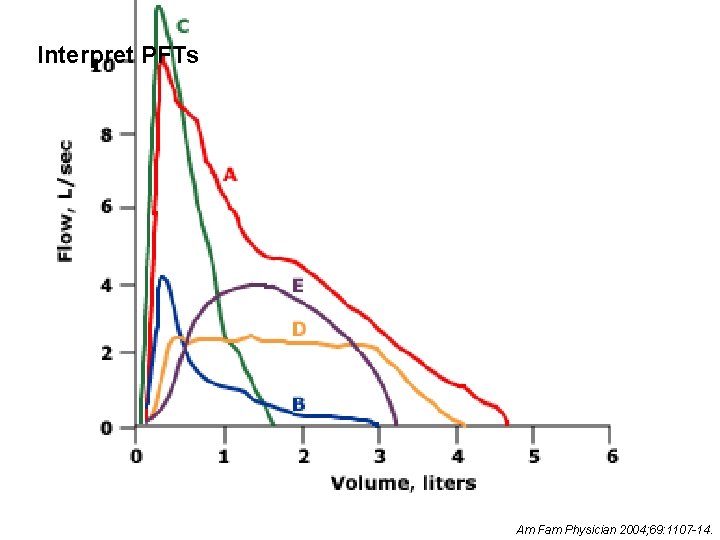
Learning Objectives • • • Understand the pathophysiology of COPD Interpret pulmonary function tests Diagnose and Stage COPD Understand management of stable COPD Recognize complications of COPD
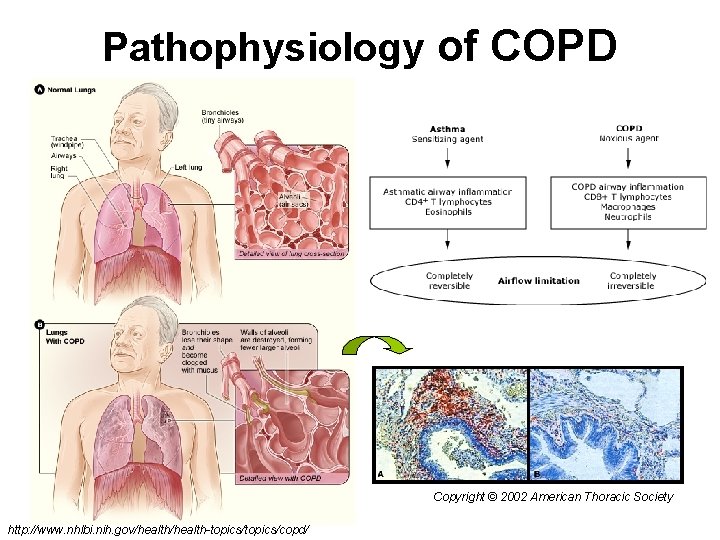
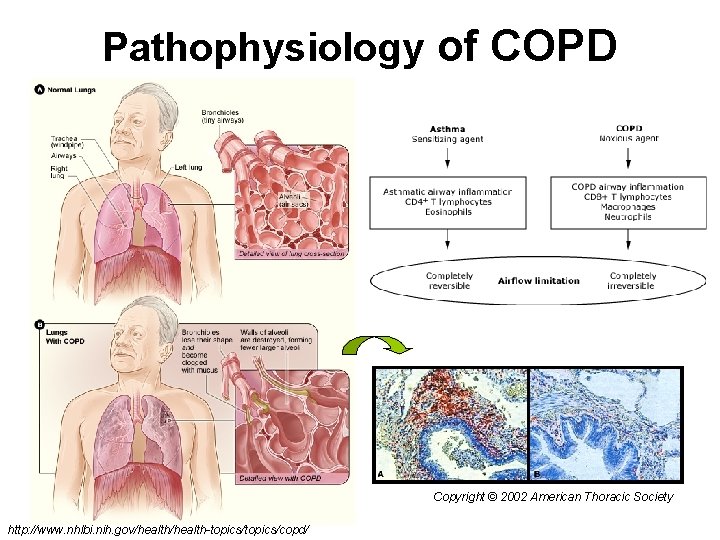
Pathophysiology of COPD Copyright © 2002 American Thoracic Society http: //www. nhlbi. nih. gov/health-topics/copd/


Case 48 yo healthy man presents with a number of episodes of shortness of breath in the past six months. Episodes are primarily with exertion, and often associated with windy or cold weather. These episodes typically will last for only a few minutes after he stops to rest. In general, the patient can go up and down two flights of stairs without difficulty. Walking on flat ground is not limited by shortness of breath. He has no nocturnal respiratory symptoms. He denies chronic cough and hemoptysis. He has no symptoms of chest tightness. He denies recent fever and chills. He has had no ankle swelling.
Case Vitals: BP 132/70, P 68, RR 16 Gen: thin, middle- aged man in no acute distress HEENT: pupils are equal, round and reactive and there is no scleral icterus. There is no erythema or thrush in the pharynx and the oral mucosa is moist. There is no supraclavicular, cervical or axillary lymphadenopathy. The skin is negative for rash and for ecchymosis. Tissue turgor is normal Neck: There is no jugular venous distension nor thyromegaly Chest: The chest is resonant to percussion and symmetrical on expansion with a moderate decrease in breath sounds at the bases. There are no wheezes or rales and the I/E ratio is 1/1. The point of maximal impulse is not displaced. S 1 and S 2 are soft. There is no gallop or murmur and the pulmonic component of the second heart sound is not accentuated. Abdomen: The abdomen revealed active bowel sounds. The liver and spleen are not palpable and there are no abdominal masses, guarding or tenderness. Ext: There is no clubbing, cyanosis or edema of the extremities.
Diagnosis and Staging • History – Dyspnea, Cough, Wheezing, Chest illnesses – Risk Factors • Family hx, Smoking hx, Environmental Hx • Physical (findings present with severe disease) – Overdistention of lungs, decreased intensity of heart/lung sounds, pursed lip breathing, accessory respiratory muscles, prolonged expiratory phase – Hoover’s Sign – Is clubbing associated with COPD? – Lower Extremity Edema
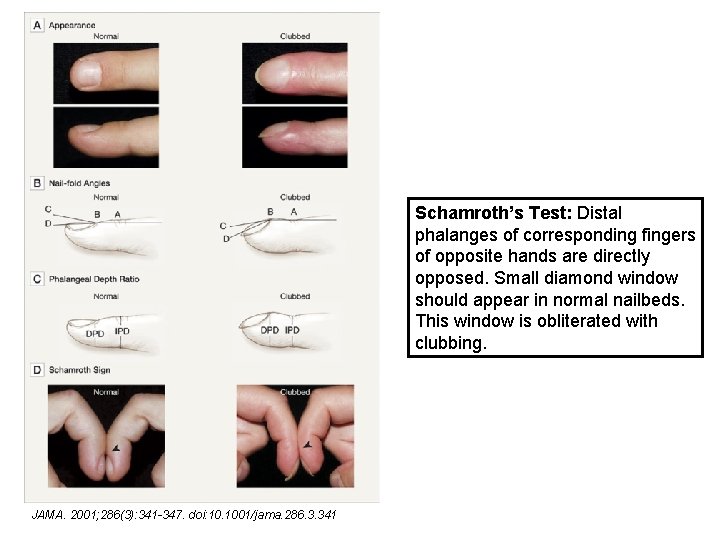
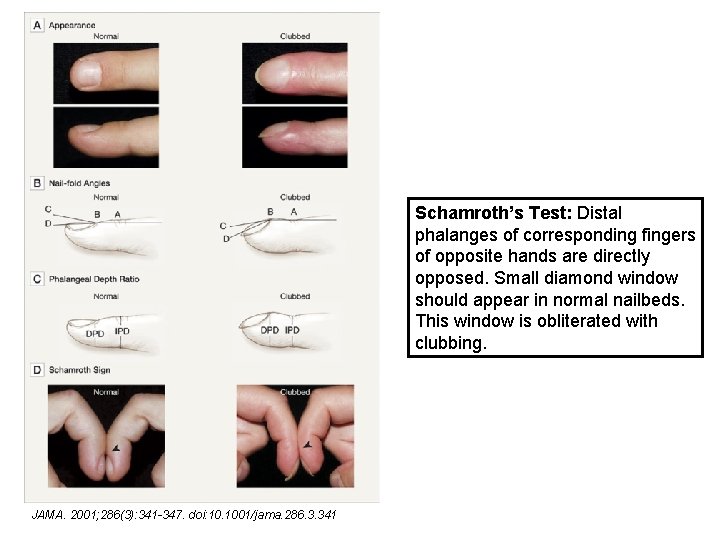
Schamroth’s Test: Distal phalanges of corresponding fingers of opposite hands are directly opposed. Small diamond window should appear in normal nailbeds. This window is obliterated with clubbing. JAMA. 2001; 286(3): 341 -347. doi: 10. 1001/jama. 286. 3. 341
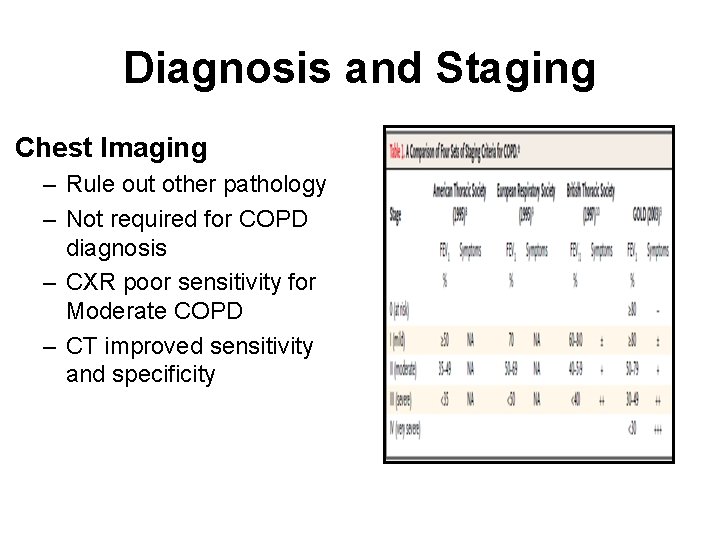
Diagnosis and Staging Chest Imaging – Rule out other pathology – Not required for COPD diagnosis – CXR poor sensitivity for Moderate COPD – CT improved sensitivity and specificity
Diagnosis and Staging Spirometry
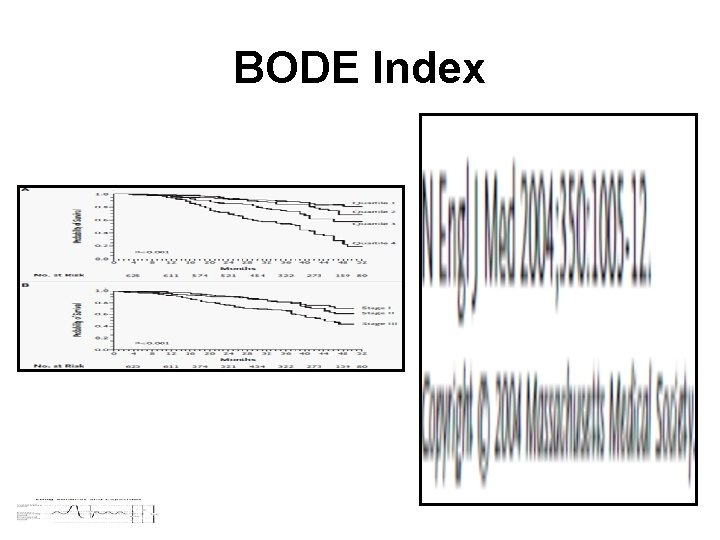
BODE Index

Am Fam Physician 2004; 69: 1107 -14.
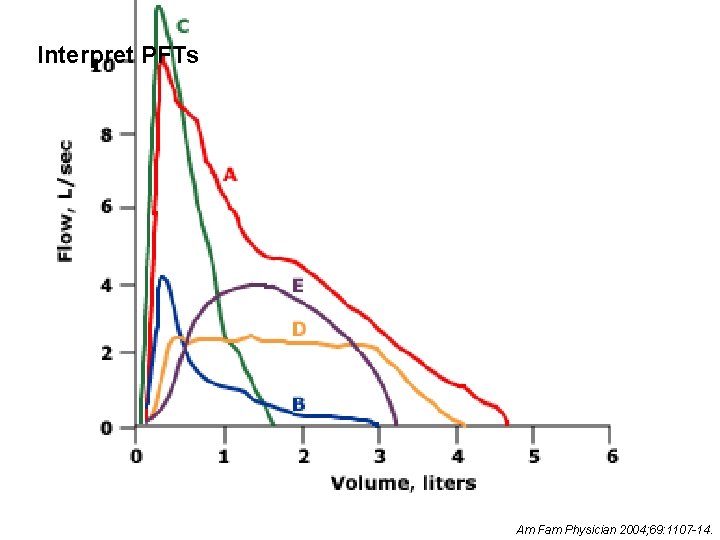
Interpret PFTs Am Fam Physician 2004; 69: 1107 -14.
Flow-Volume Variations www. uptodate. com
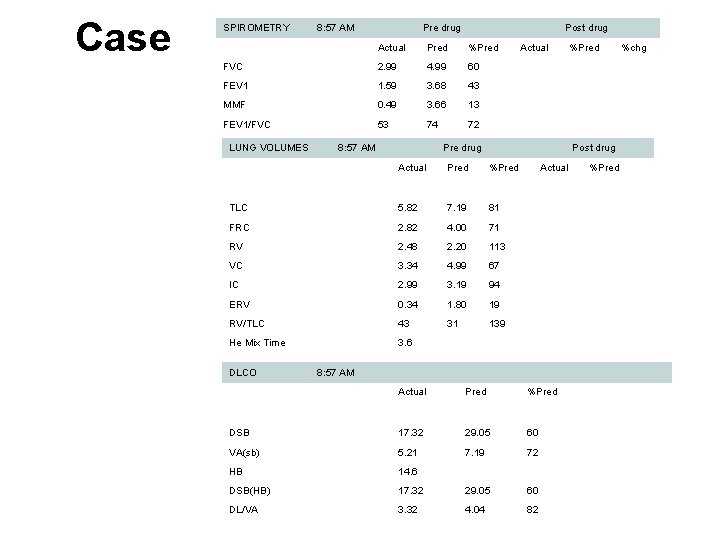
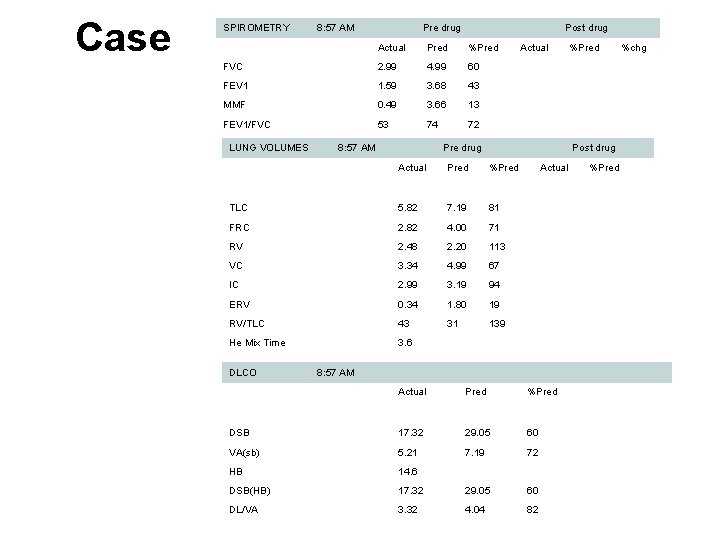
Case SPIROMETRY 8: 57 AM Pre drug Post drug Actual Pred %Pred Actual %Pred %chg FVC 2. 99 4. 99 60 FEV 1 1. 59 3. 68 43 MMF 0. 49 3. 66 13 FEV 1/FVC 53 74 72 LUNG VOLUMES 8: 57 AM Pre drug Post drug Actual Pred %Pred Actual %Pred TLC 5. 82 7. 19 81 FRC 2. 82 4. 00 71 RV 2. 48 2. 20 113 VC 3. 34 4. 99 67 IC 2. 99 3. 19 94 ERV 0. 34 1. 80 19 RV/TLC 43 31 139 He Mix Time 3. 6 DLCO 8: 57 AM Actual Pred %Pred DSB 17. 32 29. 05 60 VA(sb) 5. 21 7. 19 72 HB 14. 6 DSB(HB) 17. 32 29. 05 60 DL/VA 3. 32 4. 04 82

Case


Outpatient Management of COPD • Health Care Maintenance • Drug Therapy • Supplemental Therapy
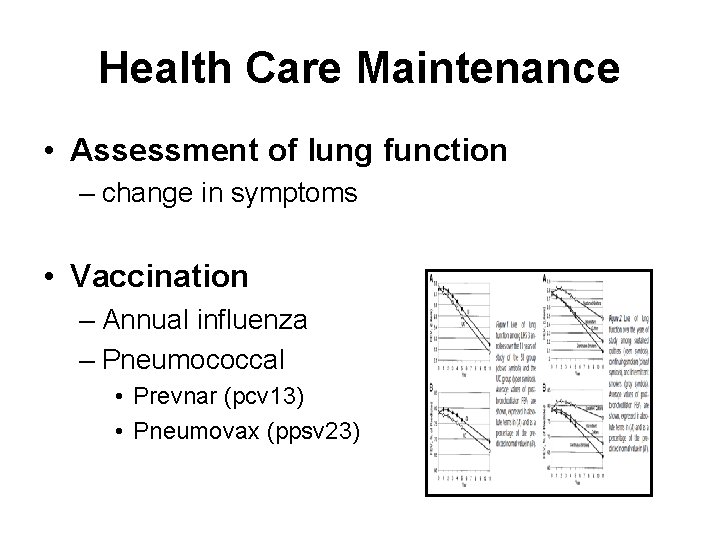
Health Care Maintenance • Assessment of lung function – change in symptoms • Vaccination – Annual influenza – Pneumococcal • Prevnar (pcv 13) • Pneumovax (ppsv 23)
Health Care Maintenance • Smoking Cessation – 50% reduction in the rate of lung-function decline in patients with COPD – ONLY intervention known to modify disease
Drug Therapy • • Inhaled Bronchodilators Inhaled Corticosteroids Oral Corticosteroids Prophylactic Azithromycin
Drug Therapy Inhaled Bronchodilators Foundation of pharmacotherapy for COPD – Alleviate Symptoms – Decrease Exacerbations – Improve quality of life – NO documented change in mortality
Mild COPD • Single short-acting inhaled bronchodilator as needed for symptoms • Two Options – Albuterol Sulfate - Beta 2 Agonist – Ipratropium Bromide - Cholinergic-Receptor Antagonist • 4 -6 hours action • Equally effective
Moderate COPD • Most patients with moderate airflow limitation when diagnosed • Long acting bronchodilator – Superior to short-acting in reducing symptoms, exacerbations, quality of life • Options: – formoterol fumarate and salmeterol xinafoate (8 -12 hours) – tiotropium bromide (24 hours ) – OR combination of both Are long acting anticholingeric antagonists and Beta-2 agonists equal?


Moderate to Severe COPD • Add inhaled corticosteroid if symptoms not controlled with optimal bronchodilator therapy • Oral Corticosteroids – No role in management of stable COPD

How do you use an inhaler?
Supplemental Therapy • Pulmonary Rehabilitation • Oxygen • Surgery
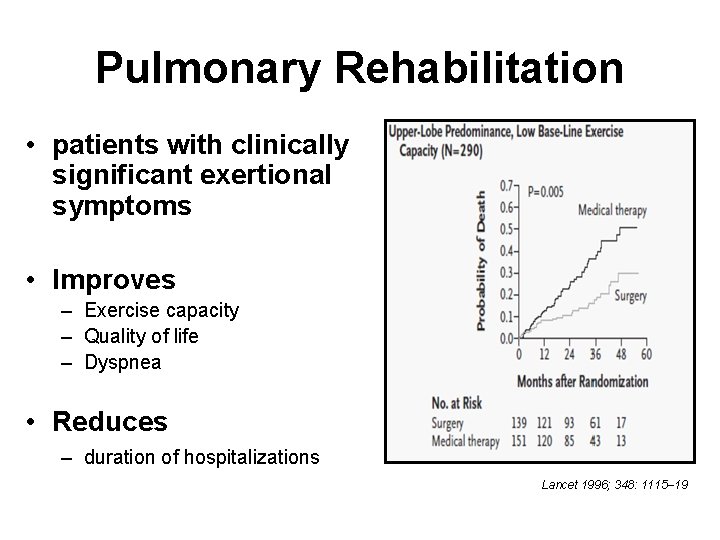
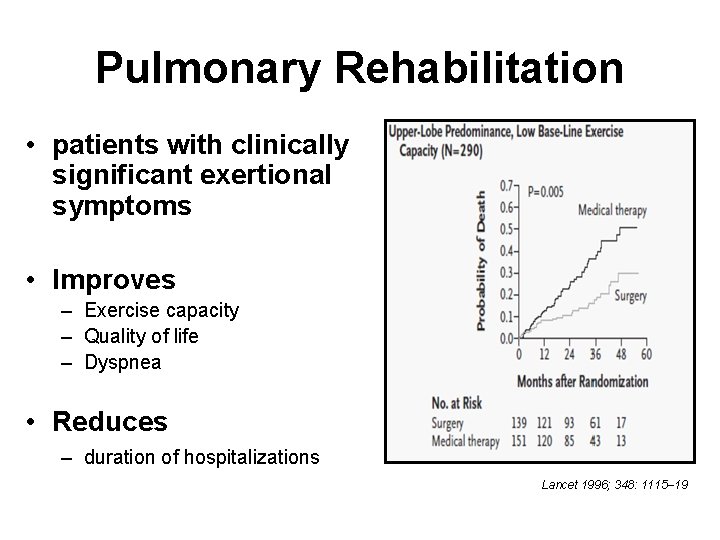
Pulmonary Rehabilitation • patients with clinically significant exertional symptoms • Improves – Exercise capacity – Quality of life – Dyspnea • Reduces – duration of hospitalizations Lancet 1996; 348: 1115– 19
Oxygen Therapy • Hypoxemia develops as ventilationperfusion mismatch worsens • Clinical trials have shown decreased mortality with supplemental oxygen for 15 or more hours per day • Medicare guidelines – Partial pressure of arterial oxygen < 55 mm. Hg – Oxygen saturation 88% or less
Surgery • Lung volume reduction – Resection of severely emphysematous tissue from upper lobes – RCT • without mortality benefit • subgroup with predominant upper lobe disease showed mortality benefit • improved lung function, exercise capacity and respiratory quality of life • Transplant – Median survival 5 years – No RCT
Air Travel • Pre-Flight Assessment – definitely need oxygen • Spo 2<92% or already use o 2 – unlikely to require oxygen • Spo 2 >95% or >92% without risk factors such as severe COPD, hypercapnia, recent exacerbation – indeterminate • Spo 2 between 92 and 95% with risk factors • Need hypoxic challenge test • In-Flight Oxygen Therapy – Increase by 2 L/min Thorax 2003; 58: 729– 732
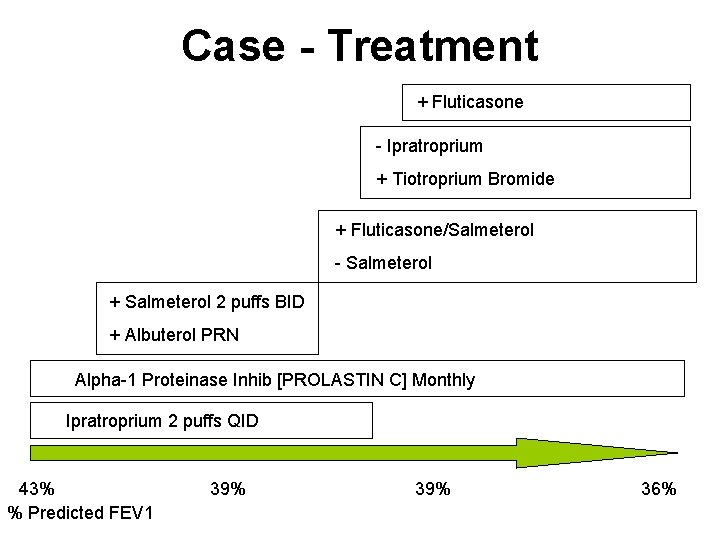
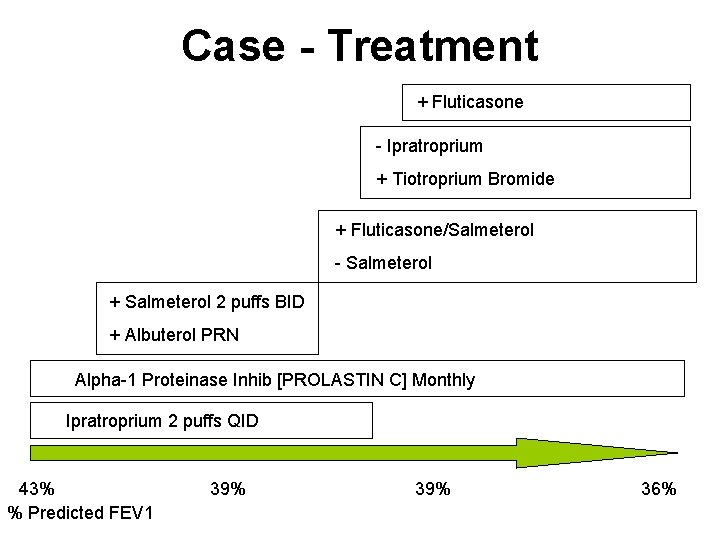
Case - Treatment + Fluticasone - Ipratroprium + Tiotroprium Bromide + Fluticasone/Salmeterol - Salmeterol + Salmeterol 2 puffs BID + Albuterol PRN Alpha-1 Proteinase Inhib [PROLASTIN C] Monthly Ipratroprium 2 puffs QID 43% 39% 36% % Predicted FEV 1
COPD complications • Exacerbations – May cause permanent loss of lung function – Antibiotics decrease RR of treatment failure by 50% • Most effective when cough and sputum purulence present – Systemic corticosteroids decrease RR of treatment failure by 30% • • Chronic steroid exposure Social Isolation Depression Anxiety
Take Home Points • Smoking cessation is the only intervention shown to change COPD disease progression • Therapy approached in stepwise fashion with bronchodilators serving as the backbone • Monitor closely for hypoxemia as oxygen therapy shown to reduce mortality • Improved quality of life, exercise capacity with pulmonary rehab • Antibiotics and systemic steroids substantially reduce the risk of treatment failure in COPD exacerbation • High rates of anxiety/depression associated with COPD

 Outpatient clinical documentation improvement
Outpatient clinical documentation improvement Methods of drug distribution
Methods of drug distribution Outpatient medical center leesville la
Outpatient medical center leesville la Outpatient cdi
Outpatient cdi Outpatient parenteral antimicrobial therapy (opat)
Outpatient parenteral antimicrobial therapy (opat) Torrance memorial transitional care unit
Torrance memorial transitional care unit Document services
Document services Slidetodoc.com
Slidetodoc.com Ryan dougherty md
Ryan dougherty md Barrel chest
Barrel chest Copd exacerbation nursing management
Copd exacerbation nursing management Pulmonary disease definition
Pulmonary disease definition Cuadro comparativo de e-learning
Cuadro comparativo de e-learning Ipassthebaton
Ipassthebaton Spirometry
Spirometry Interstitialis rajzolat a tüdőben
Interstitialis rajzolat a tüdőben Niv modes and settings
Niv modes and settings Cat score copd
Cat score copd Blue and white inhaler
Blue and white inhaler Tam chứng anthonisen
Tam chứng anthonisen Gina asthma
Gina asthma Non pharmacological treatment for copd
Non pharmacological treatment for copd Conditietraining amsterdam oost
Conditietraining amsterdam oost Copd vs asthma
Copd vs asthma Lets be copd
Lets be copd Sbar copd
Sbar copd Copd 저농도 산소
Copd 저농도 산소 Copd national action plan
Copd national action plan Bitemporal wasting in copd
Bitemporal wasting in copd Copd abcd assessment
Copd abcd assessment Ibratropium
Ibratropium Exacerbatie copd
Exacerbatie copd Terminale copd
Terminale copd Copd stervensfase
Copd stervensfase Copd pink puffer
Copd pink puffer Sputum colour chart
Sputum colour chart Chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease Copd full form
Copd full form Copd types
Copd types Fever in copd
Fever in copd