Normal Hemostasis Galila Zaher Consultant Hematologist KAUH Function















- Slides: 39
Normal Hemostasis Galila Zaher Consultant Hematologist KAUH

Function of Haemostasis Prevention of blood loss from intact vessels Arrest of bleeding from damaged vessels Blood vessel reaction to injury Platelet plug formation at site of damage
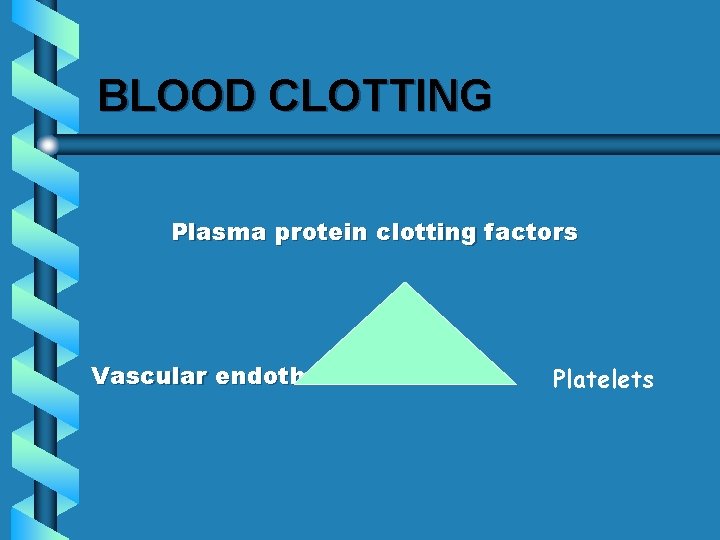
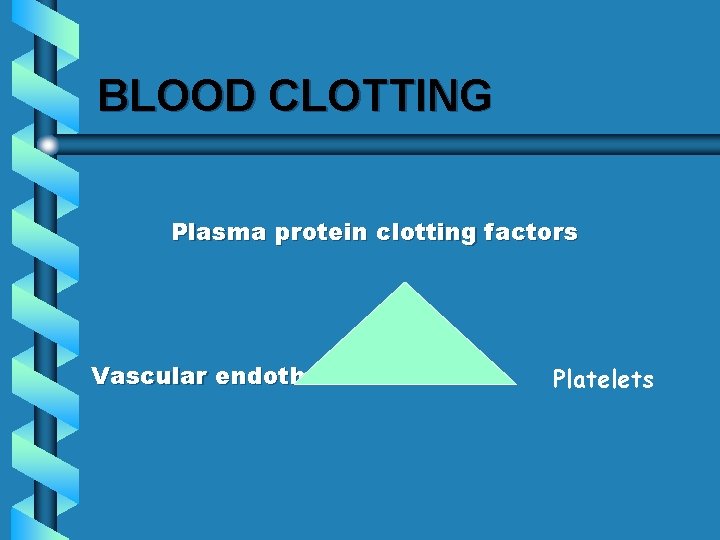
BLOOD CLOTTING Plasma protein clotting factors Vascular endothelium Platelets

COAGULOPATHIES Bleeding Clotting factors platelets Thrombosis Natural anticoagulant
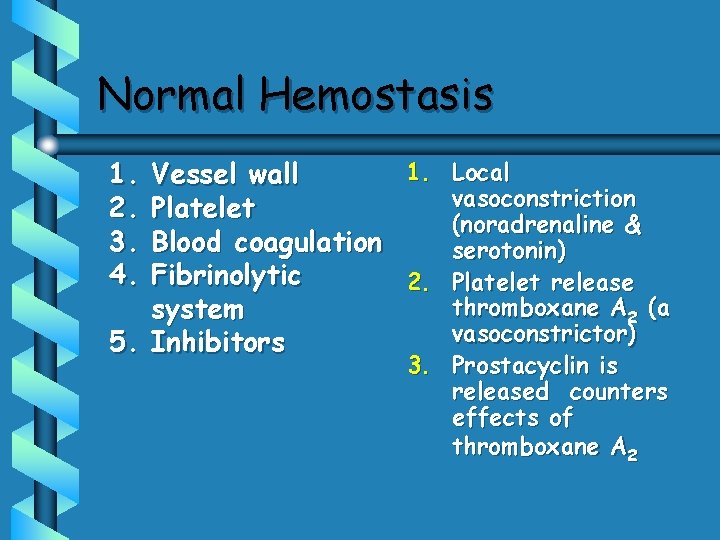
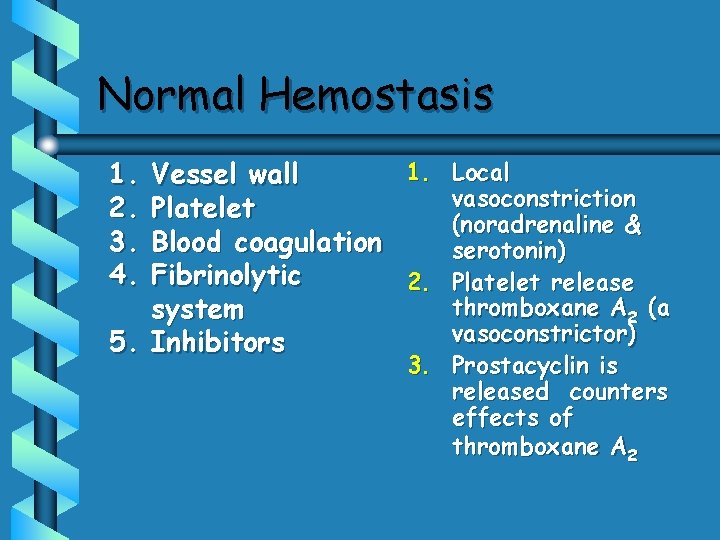
Normal Hemostasis 1. 2. 3. 4. 1. Local Vessel wall vasoconstriction Platelet (noradrenaline & Blood coagulation serotonin) Fibrinolytic 2. Platelet release thromboxane A 2 (a system vasoconstrictor) 5. Inhibitors 3. Prostacyclin is released counters effects of thromboxane A 2
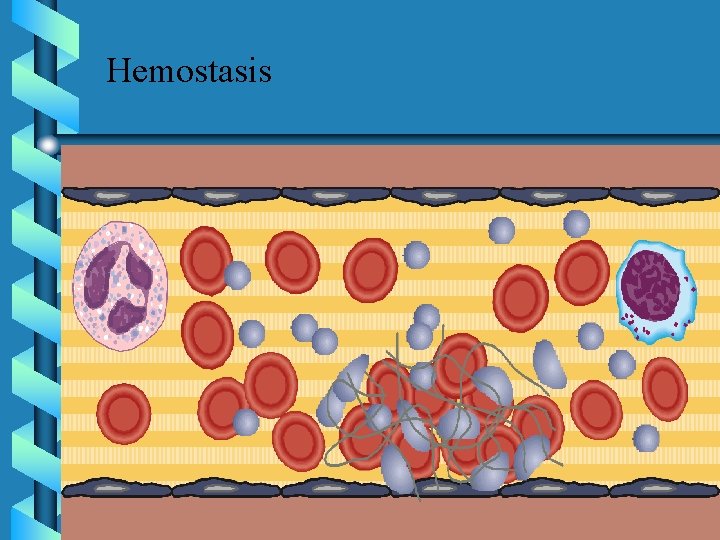
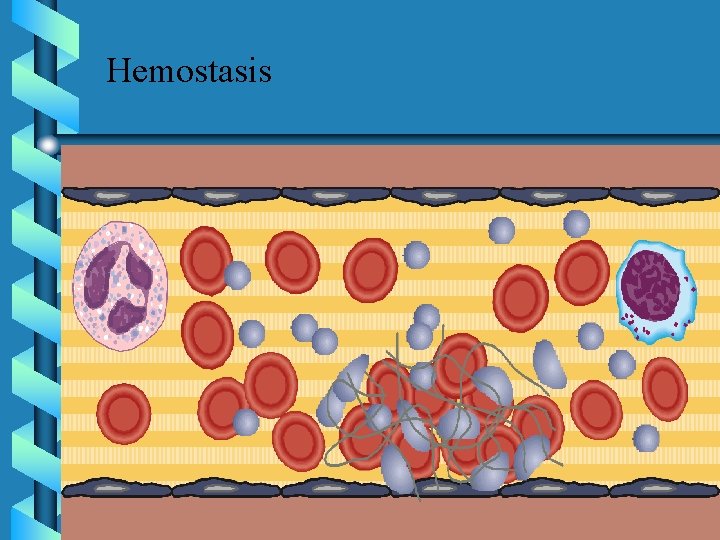
Hemostasis

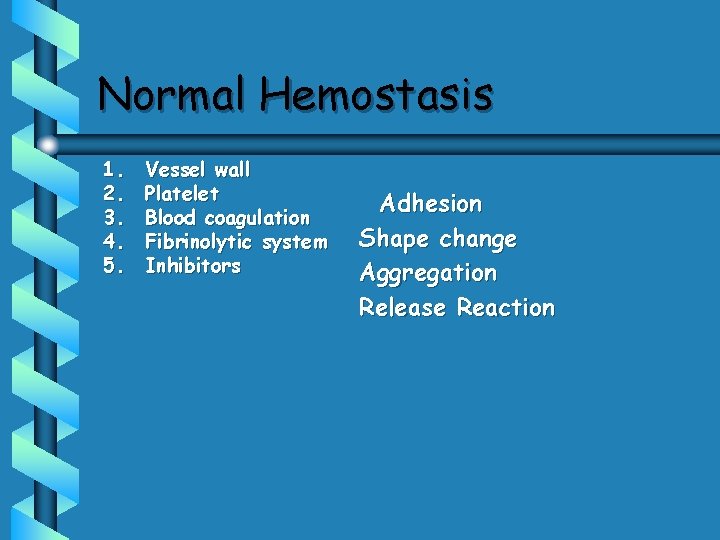
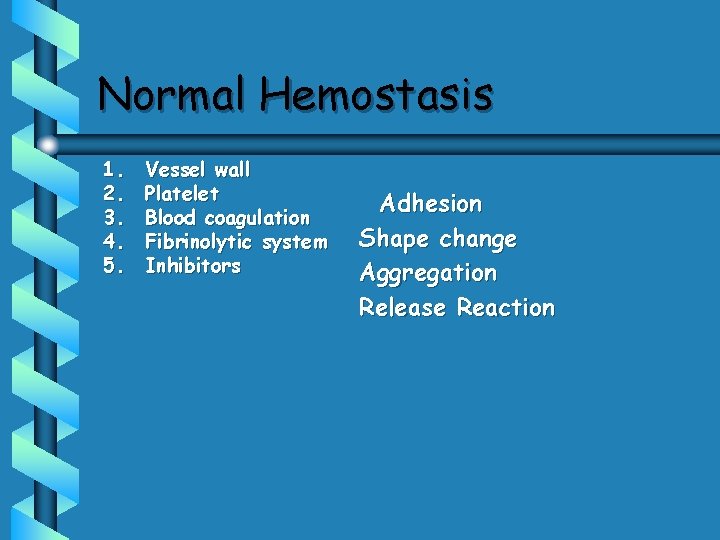
Normal Hemostasis 1. 2. 3. 4. 5. Vessel wall Platelet Blood coagulation Fibrinolytic system Inhibitors Adhesion Shape change Aggregation Release Reaction
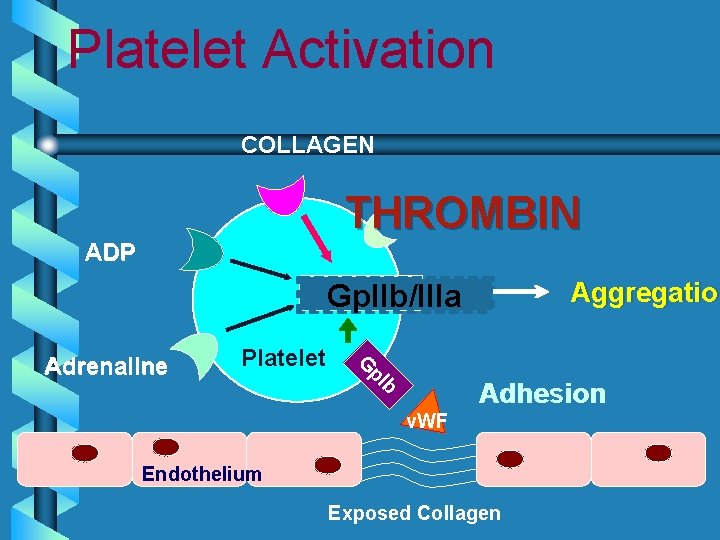
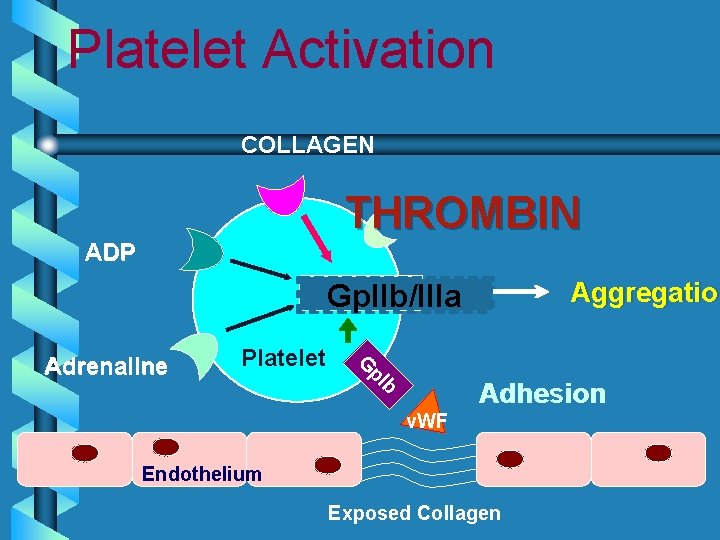
Platelet Activation COLLAGEN THROMBIN ADP Aggregation Aggregatio Gp. IIb/IIIa Platelet G p. I Adrenaline b Adhesion v. WF Endothelium Exposed Collagen




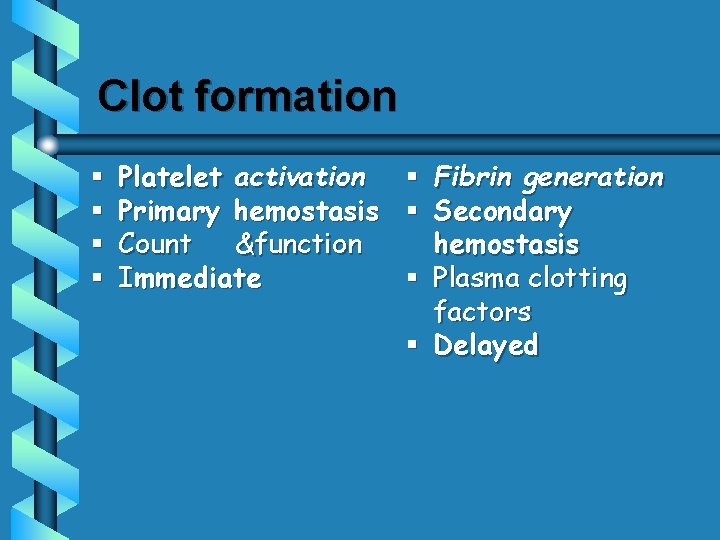
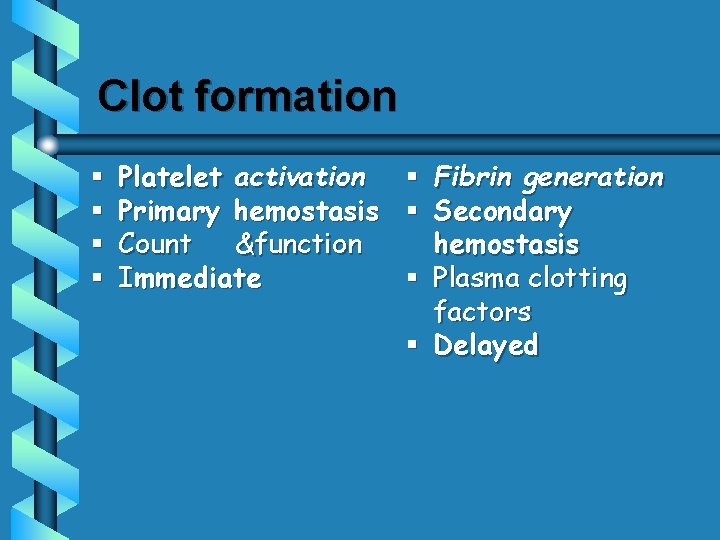
Clot formation § § Platelet activation Primary hemostasis Count &function Immediate § Fibrin generation § Secondary hemostasis § Plasma clotting factors § Delayed


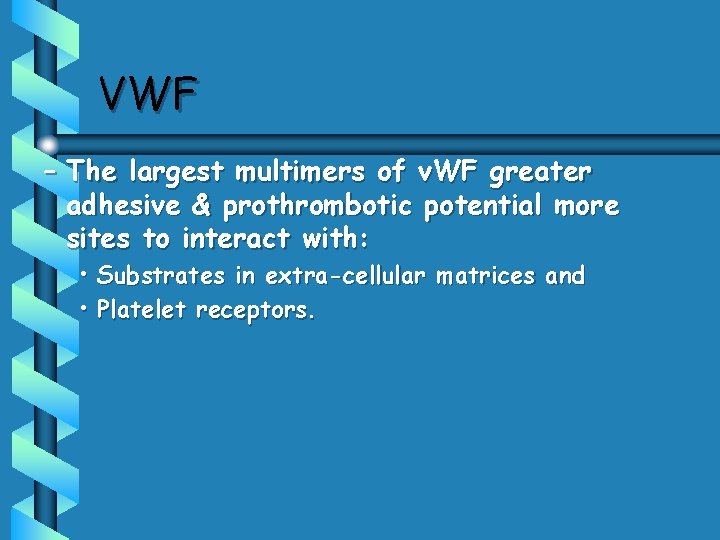
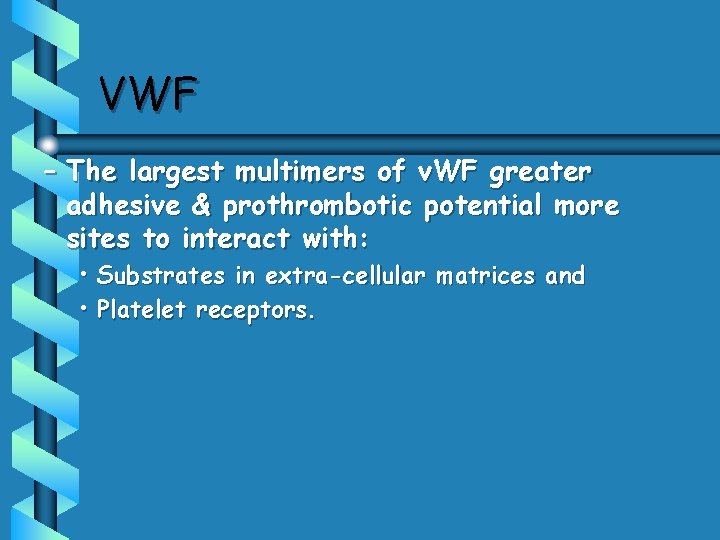
VWF – The largest multimers of v. WF greater adhesive & prothrombotic potential more sites to interact with: • Substrates in extra-cellular matrices and • Platelet receptors.
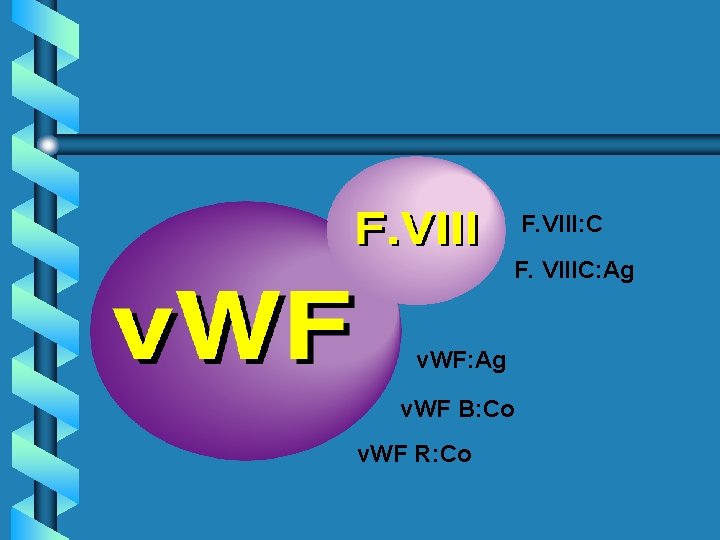
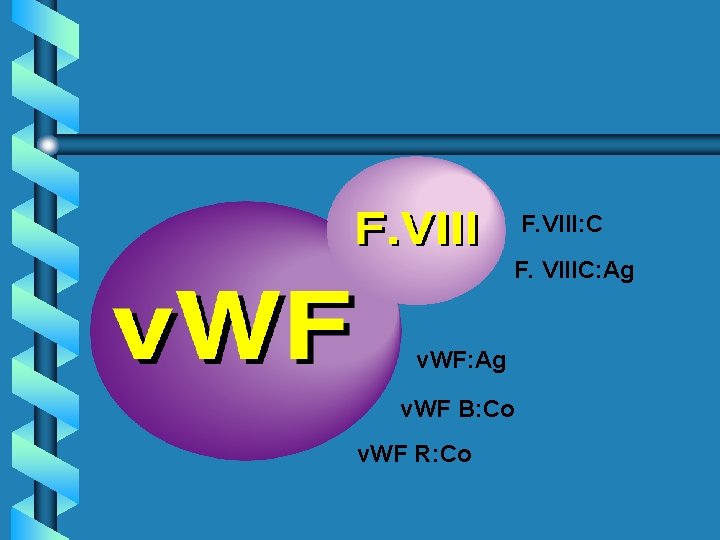
F. VIII: C F. VIIIC: Ag v. WF B: Co v. WF R: Co

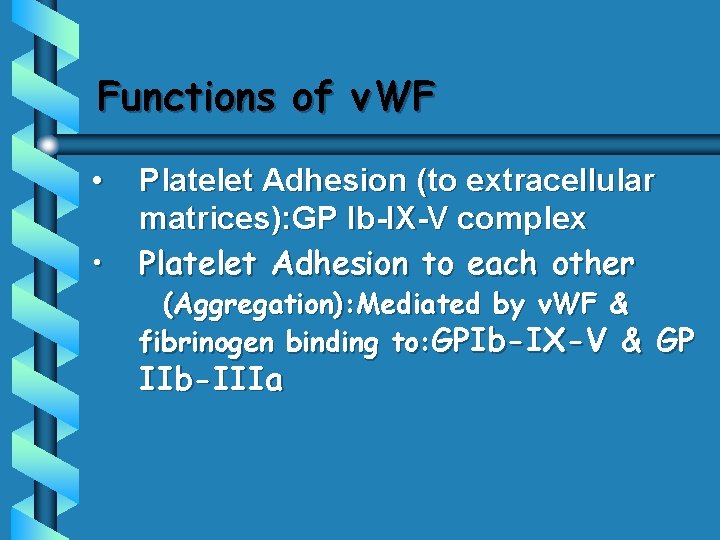
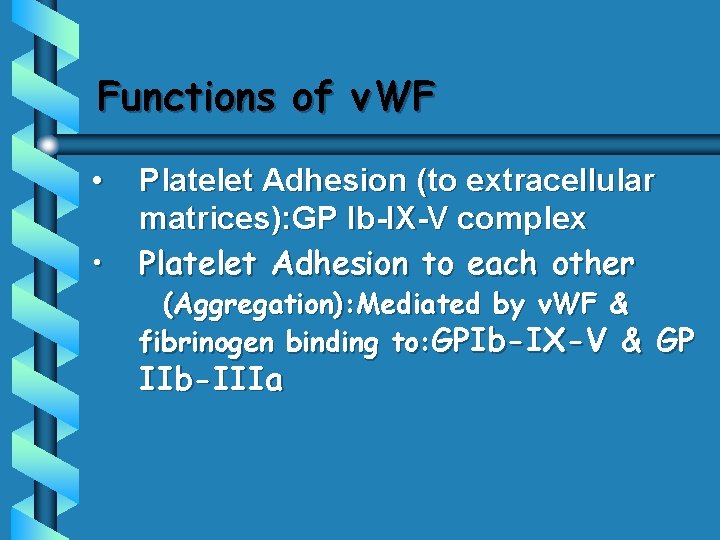
Functions of v. WF • • Platelet Adhesion (to extracellular matrices): GP Ib-IX-V complex Platelet Adhesion to each other (Aggregation): Mediated by v. WF & fibrinogen binding to: GPIb-IX-V & GP IIb-IIIa
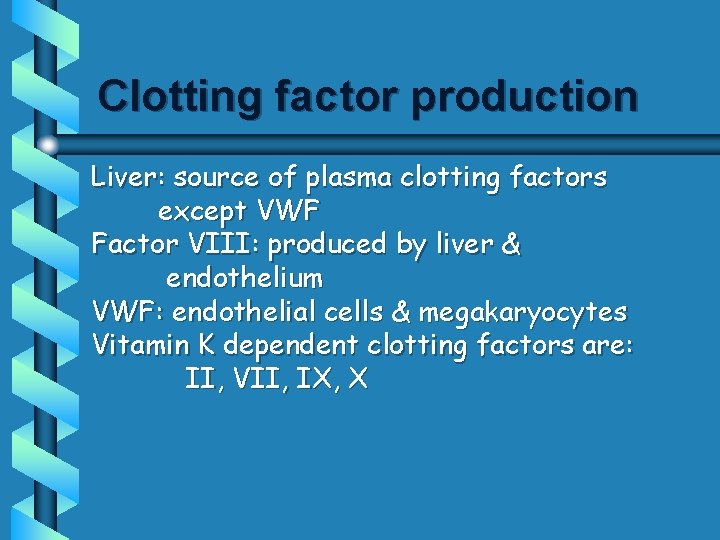
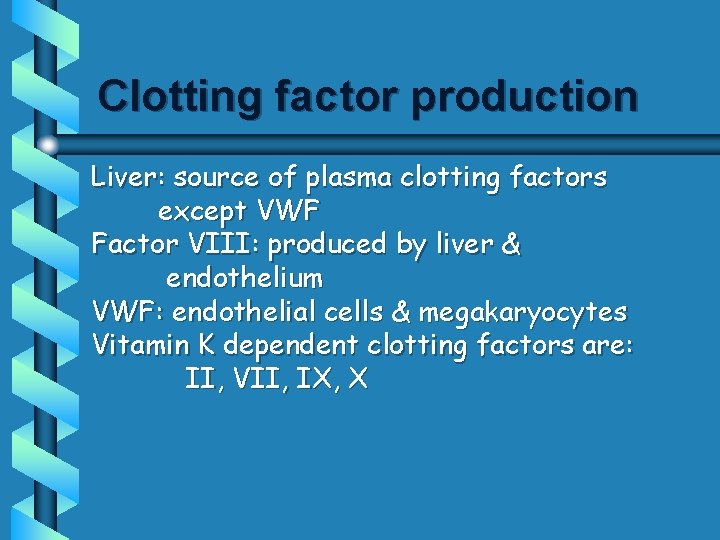
Clotting factor production Liver: source of plasma clotting factors except VWF Factor VIII: produced by liver & endothelium VWF: endothelial cells & megakaryocytes Vitamin K dependent clotting factors are: II, VII, IX, X
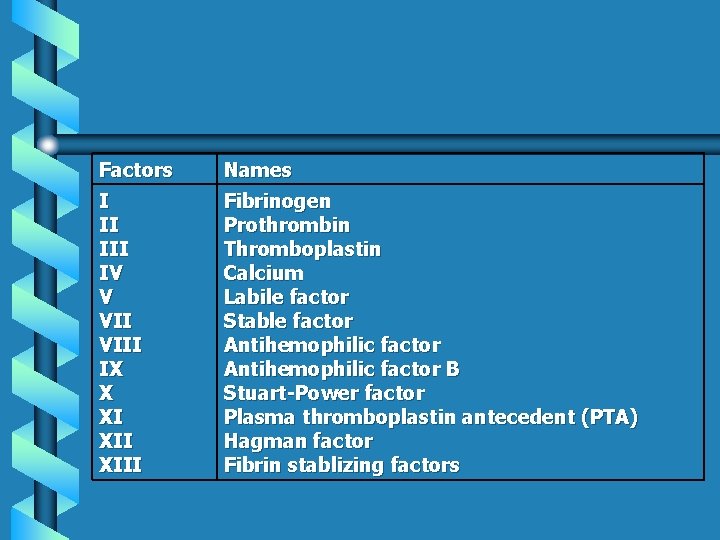
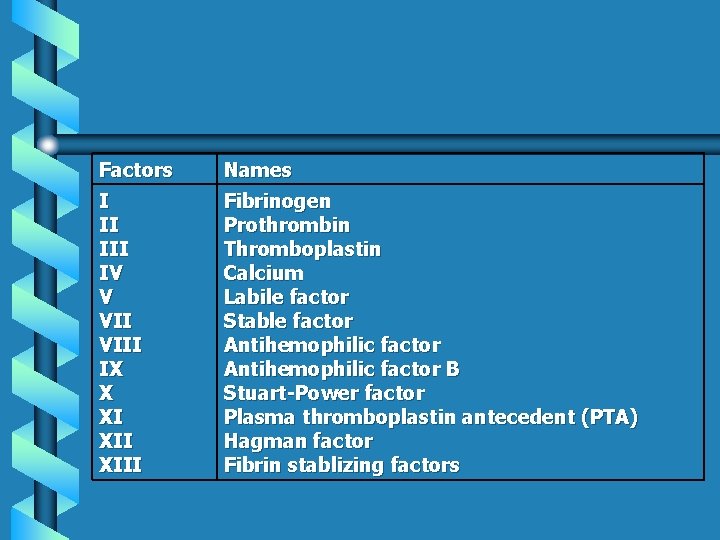
Factors Names I II IV V VIII IX X XI XIII Fibrinogen Prothrombin Thromboplastin Calcium Labile factor Stable factor Antihemophilic factor B Stuart-Power factor Plasma thromboplastin antecedent (PTA) Hagman factor Fibrin stablizing factors
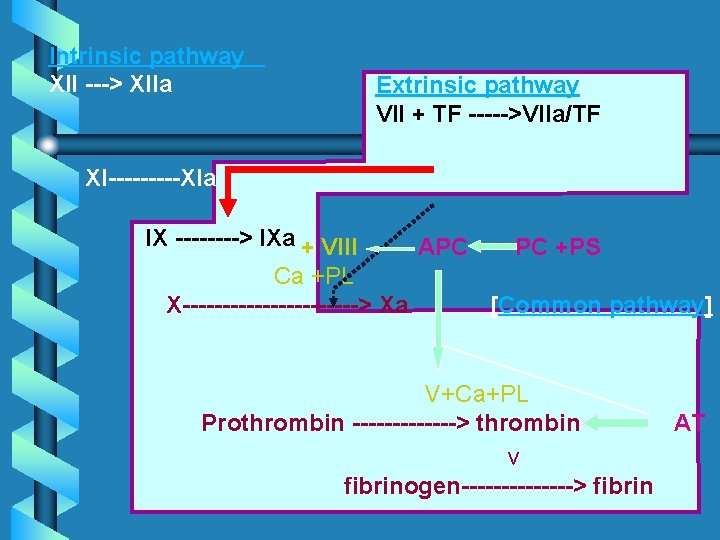
COAGULATION PATHWAYS Intrinsic & extrinsic pathways “conclude” in the common pathway Intrinsic pathway clotting factors Extrinsic pathway clotting factors Common pathway clotting factors
Intrinsic Pathway § All clotting factors are within the blood vessels § Clotting slower § Activated partial thromboplastin test (a. PTT) Extrinsic Pathway § Initiating factor is outside blood vessels - tissue factor § Clotting faster § Prothrombin test (PT)

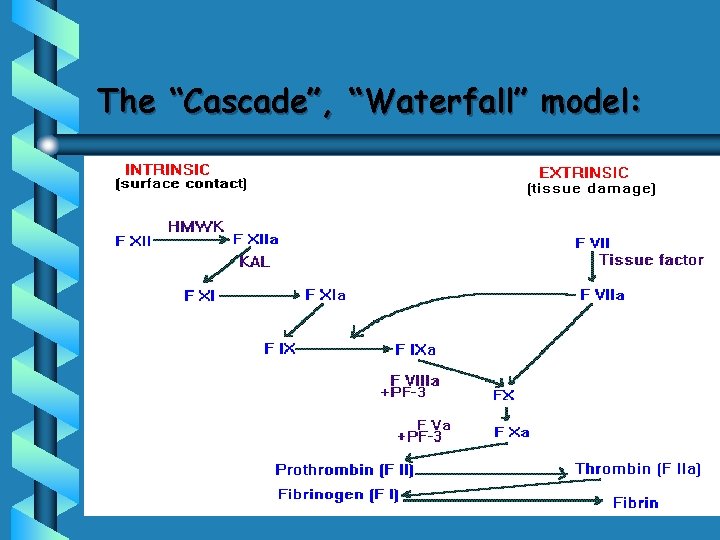
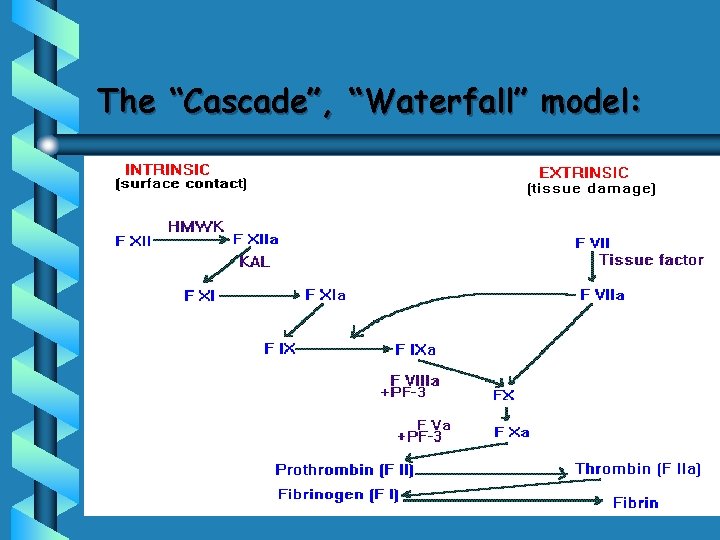
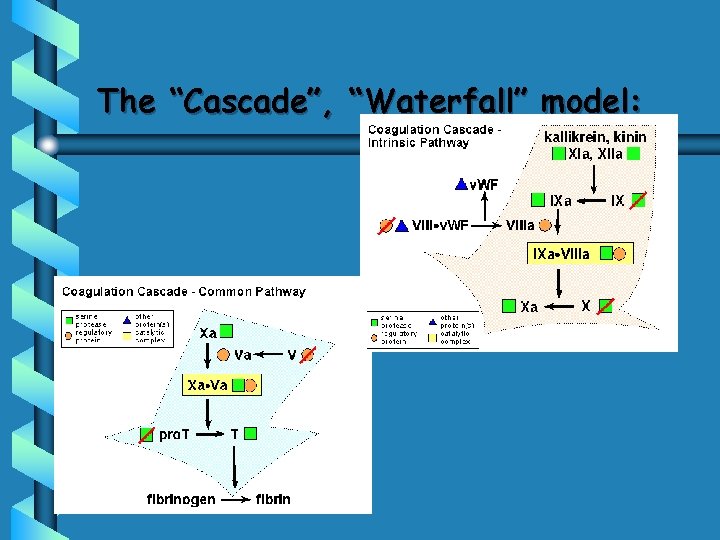
The “Cascade”, “Waterfall” model:
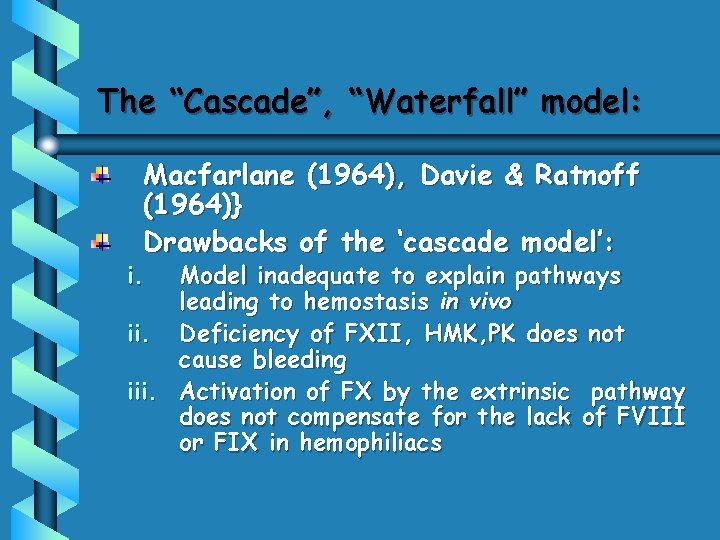
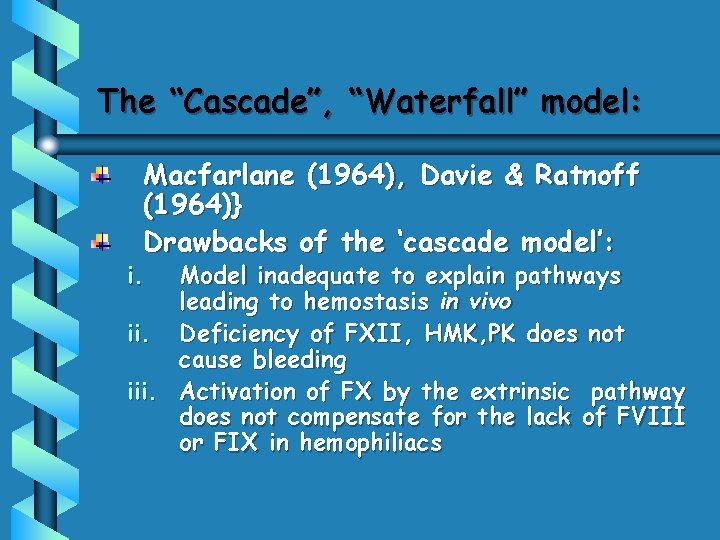
The “Cascade”, “Waterfall” model: Macfarlane (1964), Davie & Ratnoff (1964)} Drawbacks of the ‘cascade model’: i. Model inadequate to explain pathways leading to hemostasis in vivo ii. Deficiency of FXII, HMK, PK does not cause bleeding iii. Activation of FX by the extrinsic pathway does not compensate for the lack of FVIII or FIX in hemophiliacs
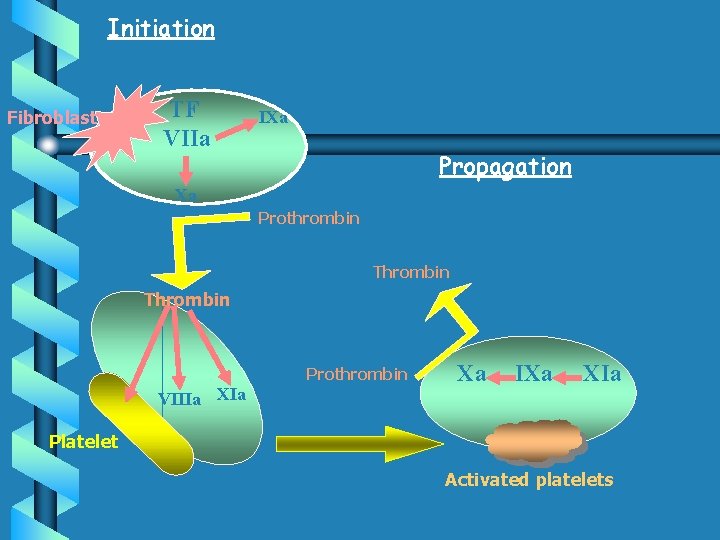
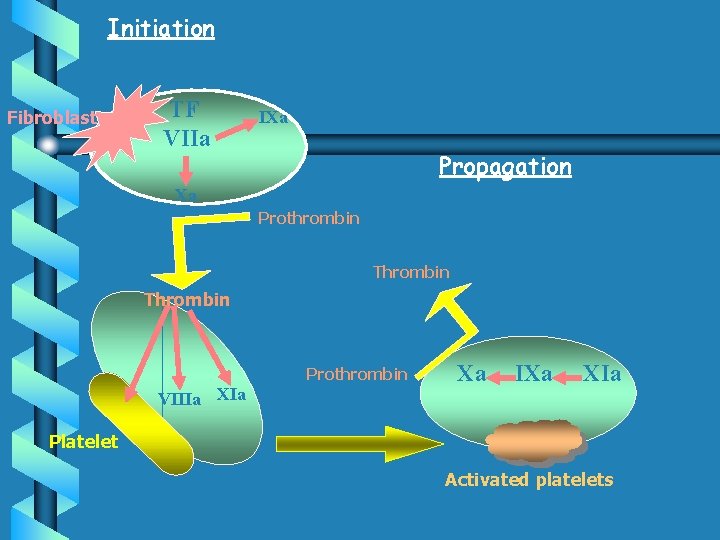
Initiation Fibroblast TF VIIa IXa Propagation Xa Prothrombin Thrombin Prothrombin VIIIa Xa IXa XIa Platelet Activated platelets Amplification
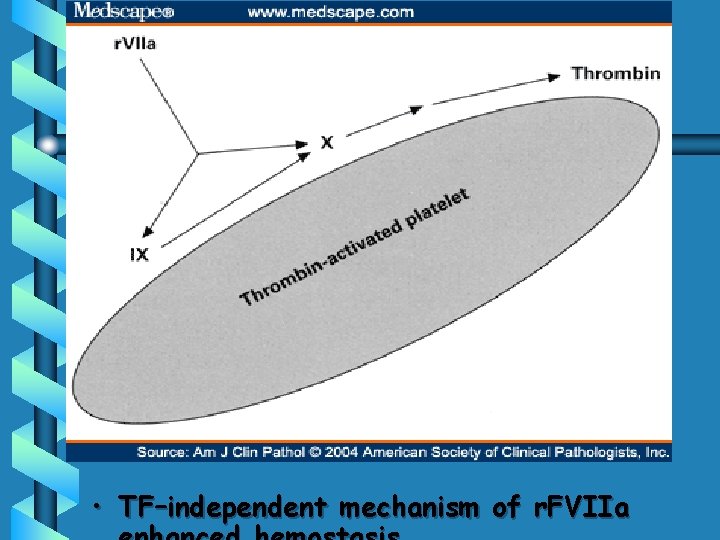
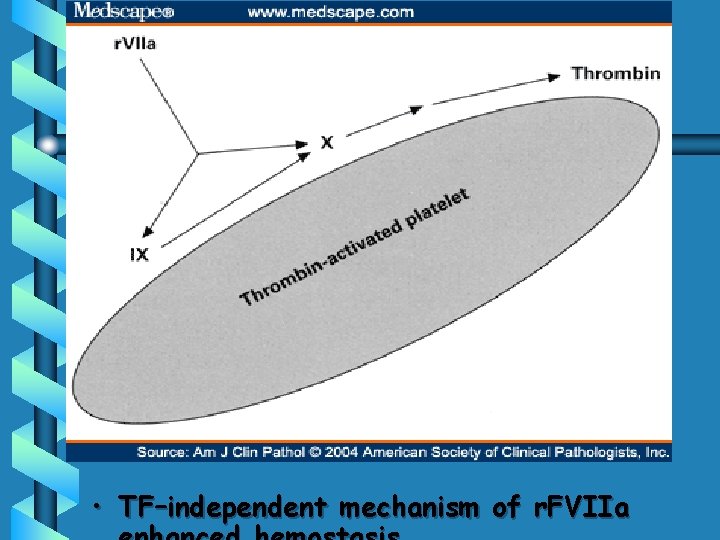
• TF–independent mechanism of r. FVIIa

Alternative (Cell-based) Model • • • The initiation phase: Commences on TF-bearing cells (fibroblasts) FXa, IXa & thrombin Initiation of the coagulation process The amplification phase: Coagulation moves from TF-bearing cells to activated platelets, The propagation phase: The active proteases combine with cofactors on platelet surface to generate thrombin; End-result is fibrin polymerization

Fibrinolysis 1. 2. 3. 4. 5. Vessel wall Platelet Blood coagulation Fibrinolytic system Inhibitors 1. 2. Fibrin is digested by enzymes from plasma and from cells. Endothelium replaces the fibrin
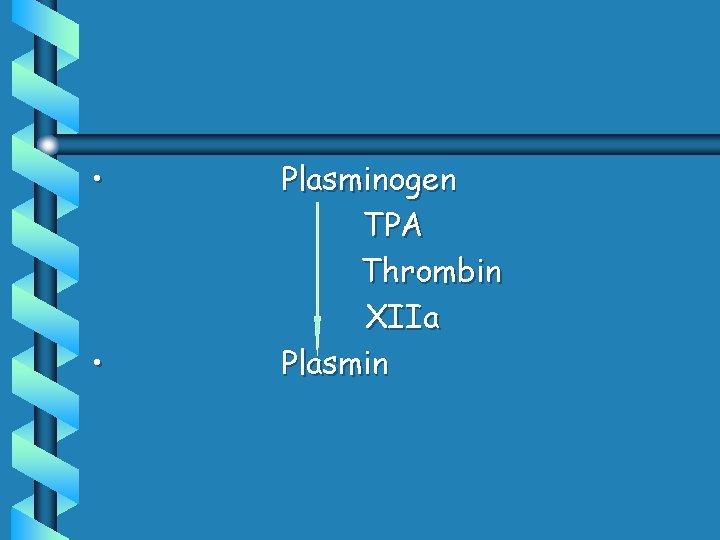
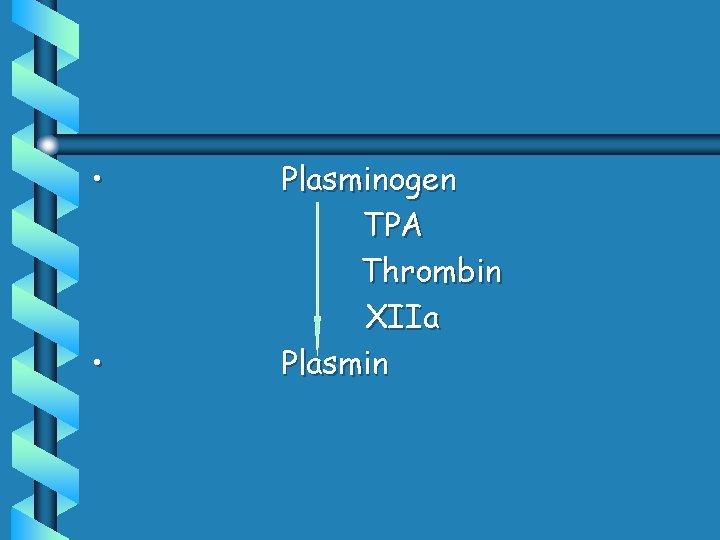
• • Plasminogen TPA Thrombin XIIa Plasmin

Activation of fibrinolysis damaged cells thrombin mental/physical stress PAI inflammation trauma t-PA plasminogen plasmin fibrinogen FDP (X, Y, D, E) extrinsic pathway antiplasmin cross-linked fibrin X-FDP (D-Dimer, cross-linked oligomers, DD/E. . . )
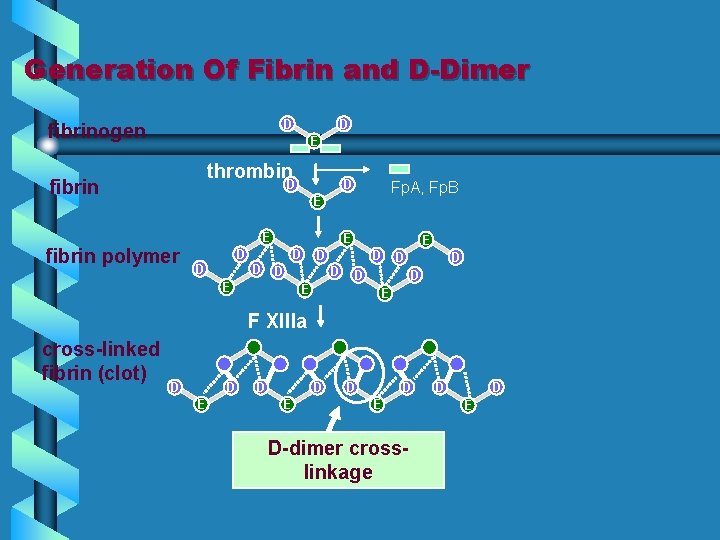
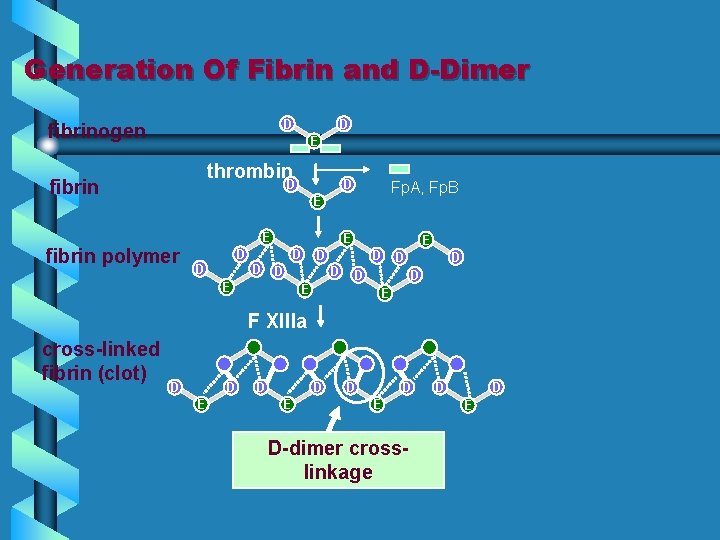
Generation Of Fibrin and D-Dimer D fibrinogen D EE thrombin fibrin D D Fp. A, Fp. B E E EE E fibrin polymer D D D D EE F XIIIa E D EE E D D D EE E cross-linked fibrin (clot) D D EE D-dimer crosslinkage D D E
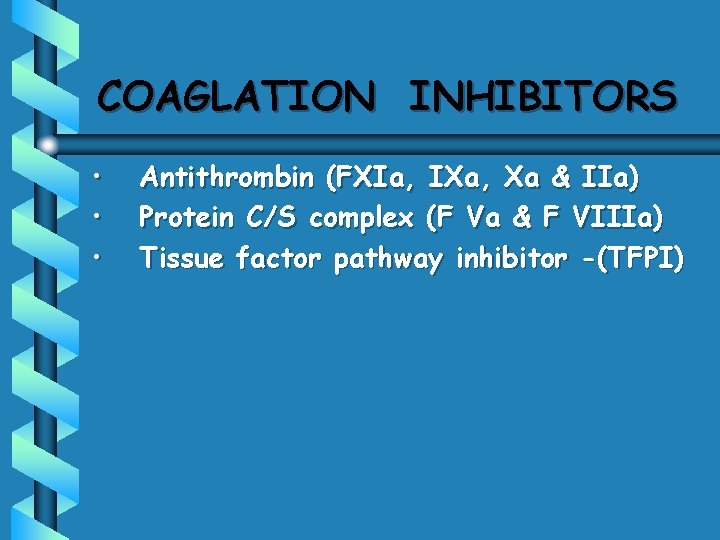
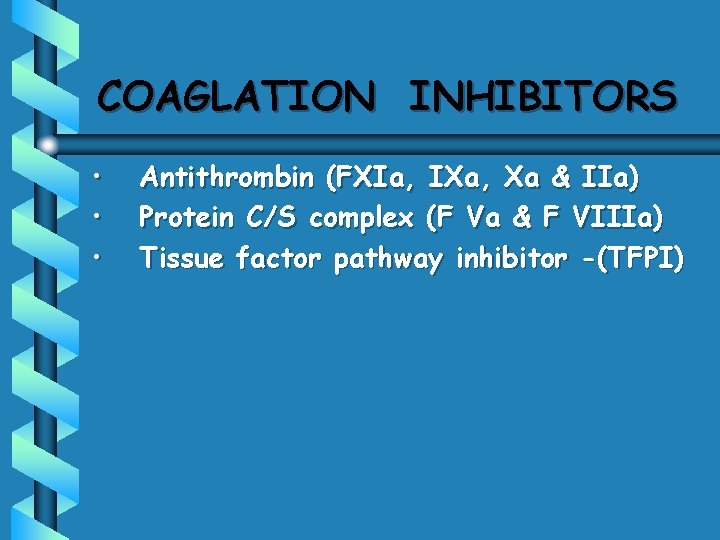
COAGLATION INHIBITORS • • • Antithrombin (FXIa, IXa, Xa & IIa) Protein C/S complex (F Va & F VIIIa) Tissue factor pathway inhibitor -(TFPI)
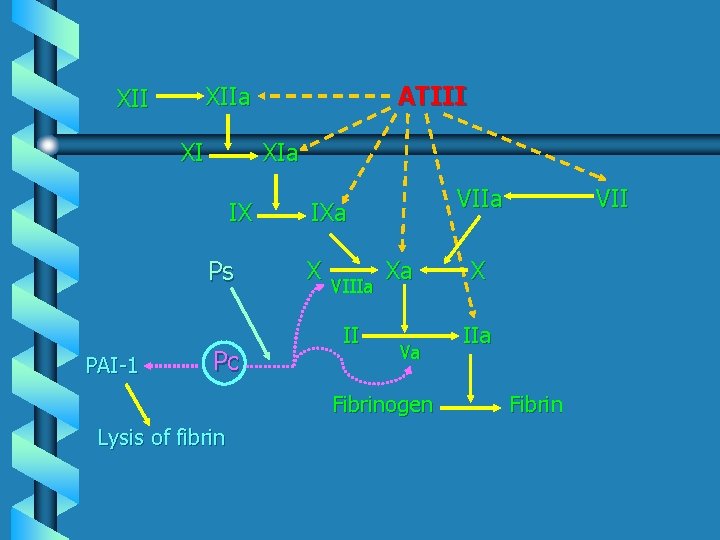
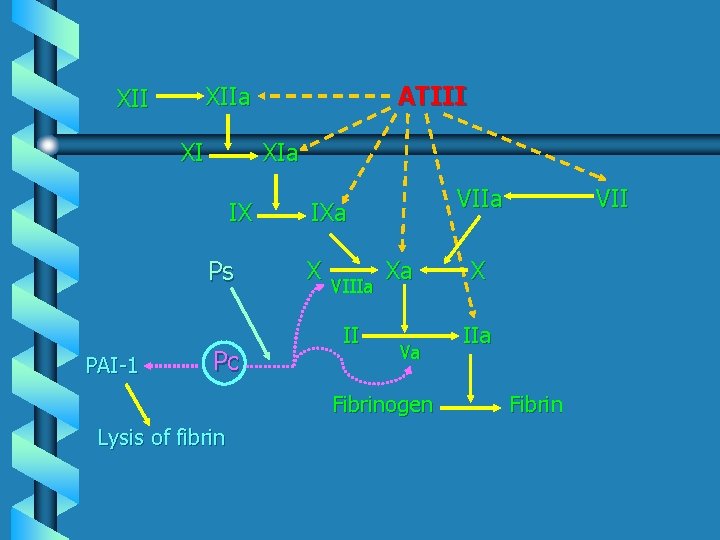
XI XIa IX Ps PAI-1 ATIII XIIa XII Pc VIIa IXa X VIIIa II Xa Va Fibrinogen Lysis of fibrin VII X IIa Fibrin

Tissue factor + Factor VIIa Factor IXa -FVIIIa TFPI Factor Xa +FVa Anti Thrombin III Protein C Factor XIa Factor IIa (thrombin) Fibrinogen Fibrin
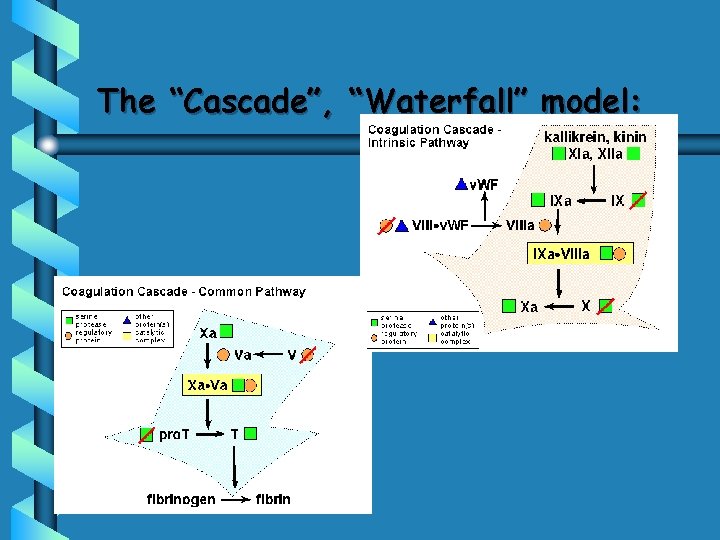
The “Cascade”, “Waterfall” model:
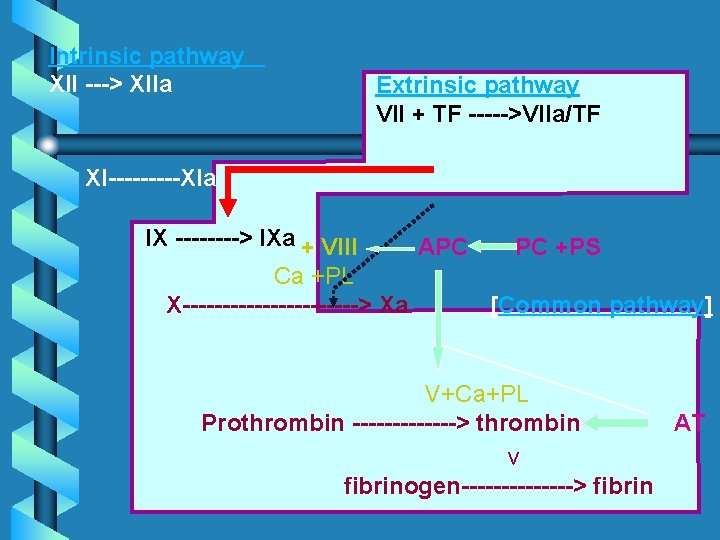
Intrinsic pathway XII ---> XIIa Extrinsic pathway VII + TF ----->VIIa/TF XI-----XIa IX ----> IXa + VIII Ca +PL X-----------> Xa APC PC +PS [Common pathway] V+Ca+PL Prothrombin -------> thrombin AT v fibrinogen-------> fibrin