Inherited Coagulation Disorders Dr Galila Zaher Consultant Hematologist








- Slides: 41
Inherited Coagulation Disorders Dr Galila Zaher Consultant Hematologist KAUH
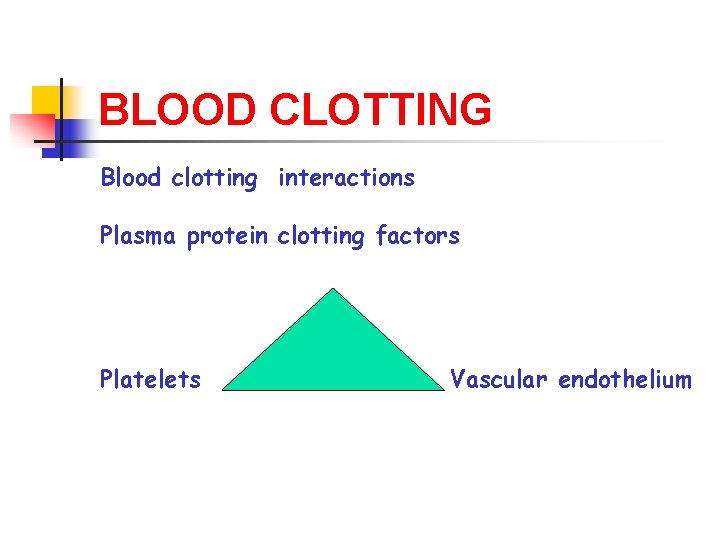
BLOOD CLOTTING Blood clotting interactions Plasma protein clotting factors Platelets Vascular endothelium
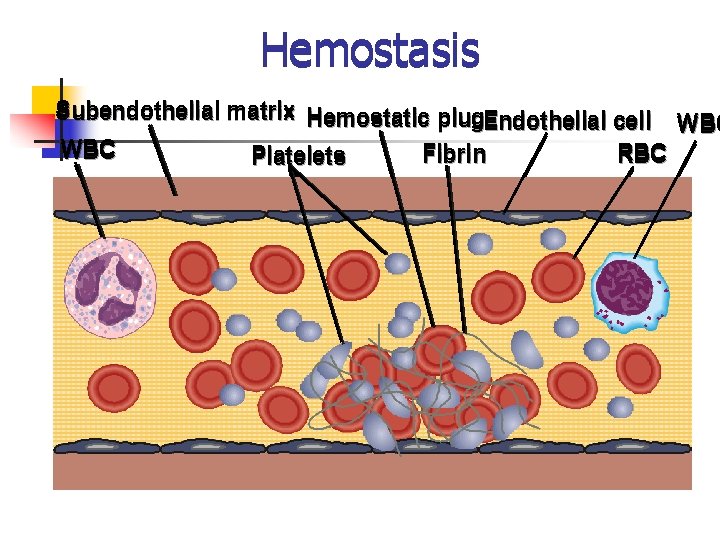
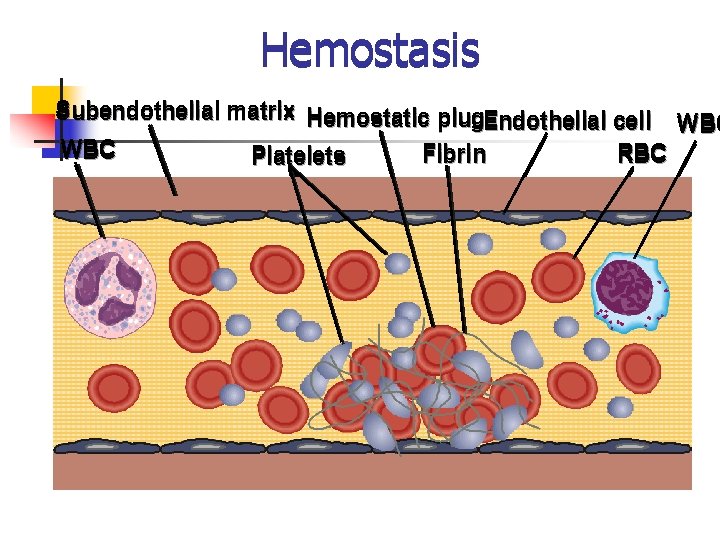
Hemostasis Subendothelial matrix Hemostatic plug. Endothelial cell WBC Fibrin RBC Platelets
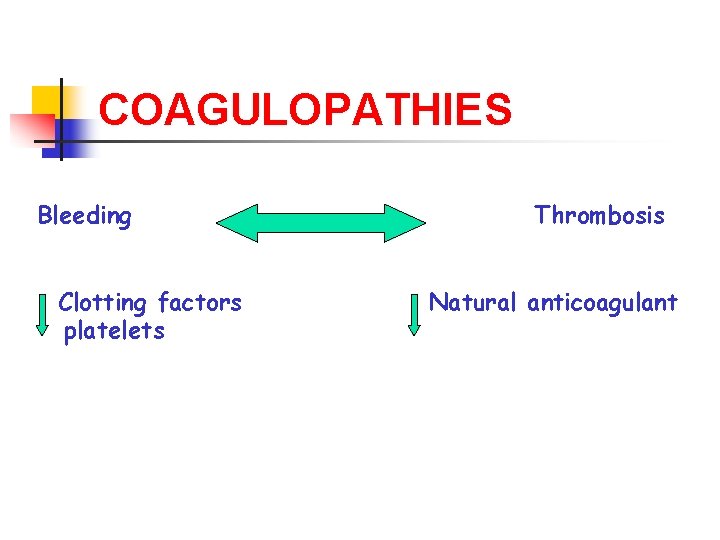
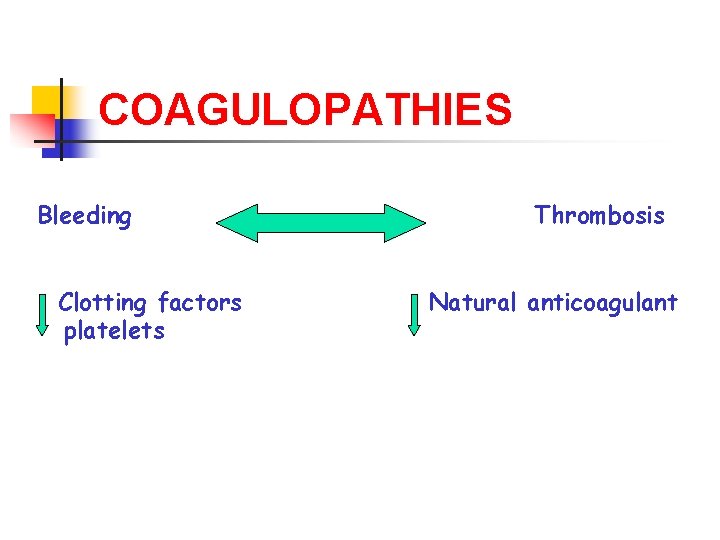
COAGULOPATHIES Bleeding Clotting factors platelets Thrombosis Natural anticoagulant

Clot formation Platelet activation No &count Fibrin generation plasma clotting factors Primary hemostasis (immediate) Secondary hemostasis (delayed)
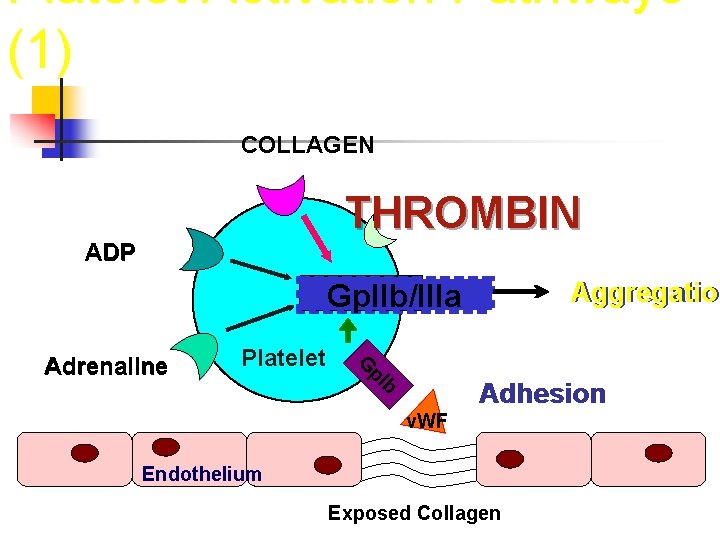
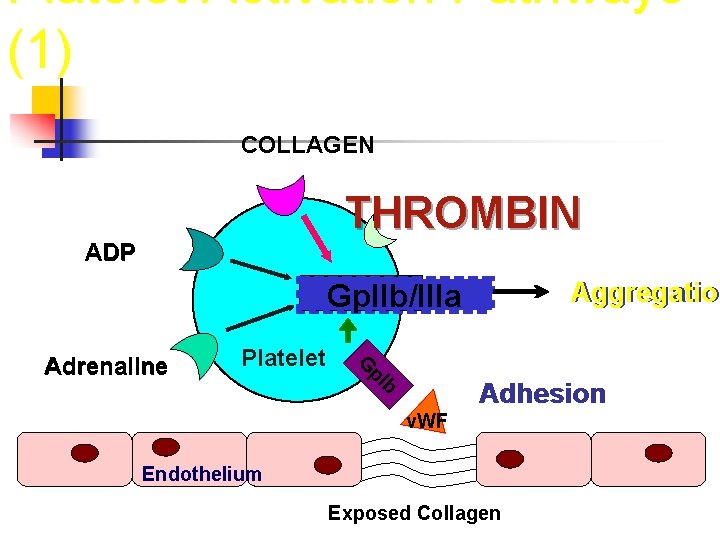
Platelet Activation Pathways (1) COLLAGEN THROMBIN ADP Aggregation Aggregatio Gp. IIb/IIIa Platelet G p. I Adrenaline b Adhesion v. WF Endothelium Exposed Collagen
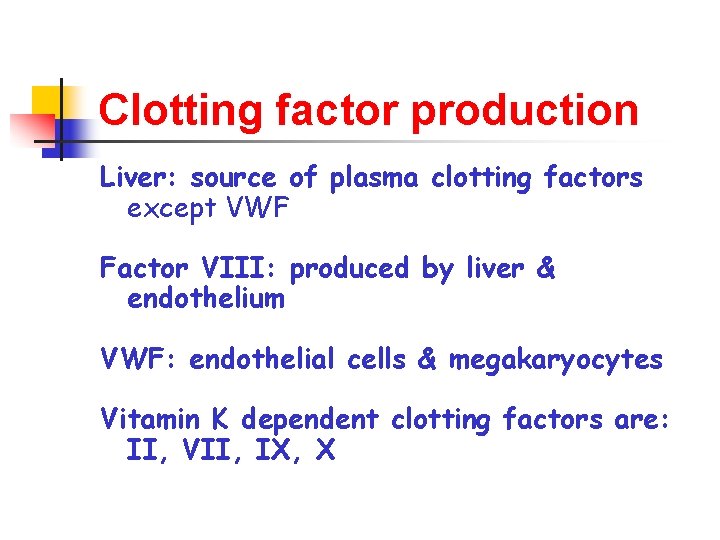
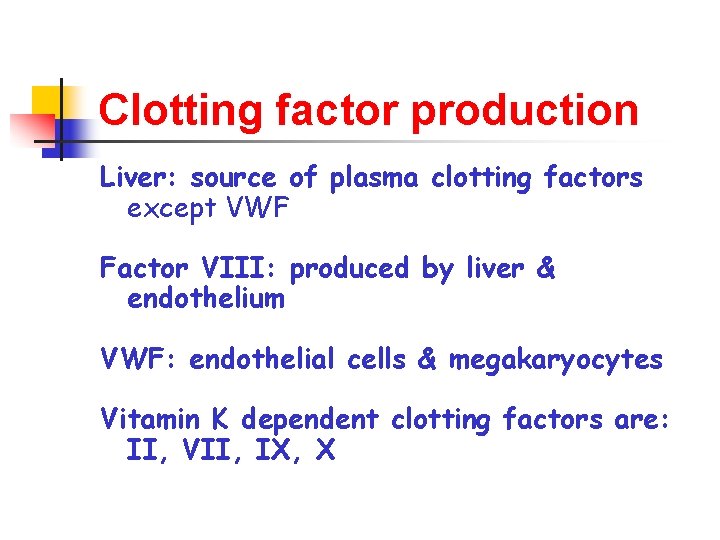
Clotting factor production Liver: source of plasma clotting factors except VWF Factor VIII: produced by liver & endothelium VWF: endothelial cells & megakaryocytes Vitamin K dependent clotting factors are: II, VII, IX, X
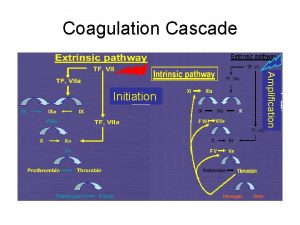
COAGULATION PATHWAYS Intrinsic & extrinsic pathways “conclude” in the common pathway Intrinsic pathway clotting factors Extrinsic pathway clotting factors Common pathway clotting factors
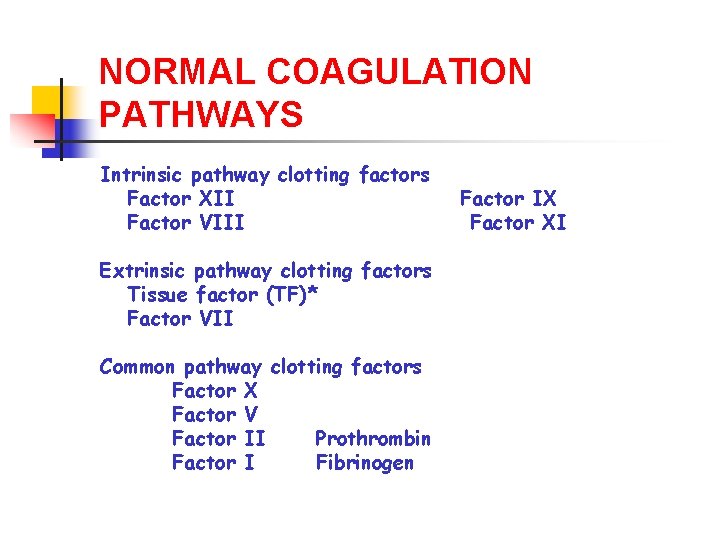
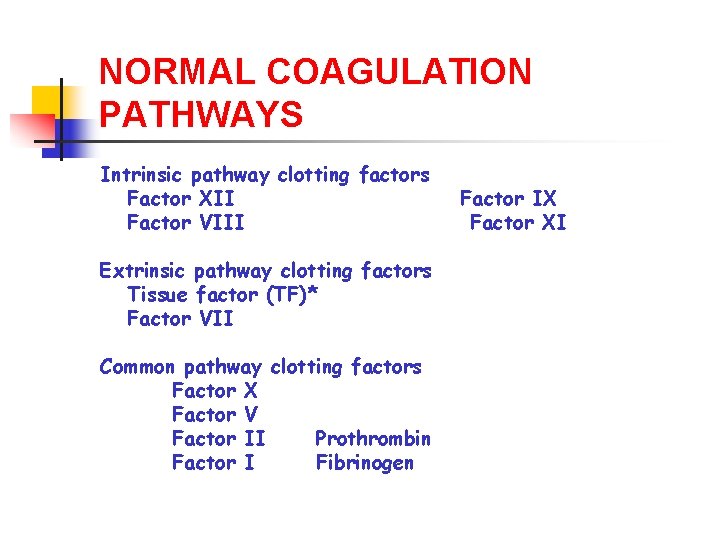
NORMAL COAGULATION PATHWAYS Intrinsic pathway clotting factors Factor XII Factor VIII Extrinsic pathway clotting factors Tissue factor (TF)* Factor VII Common pathway clotting factors Factor X Factor V Factor II Prothrombin Factor I Fibrinogen Factor IX Factor XI
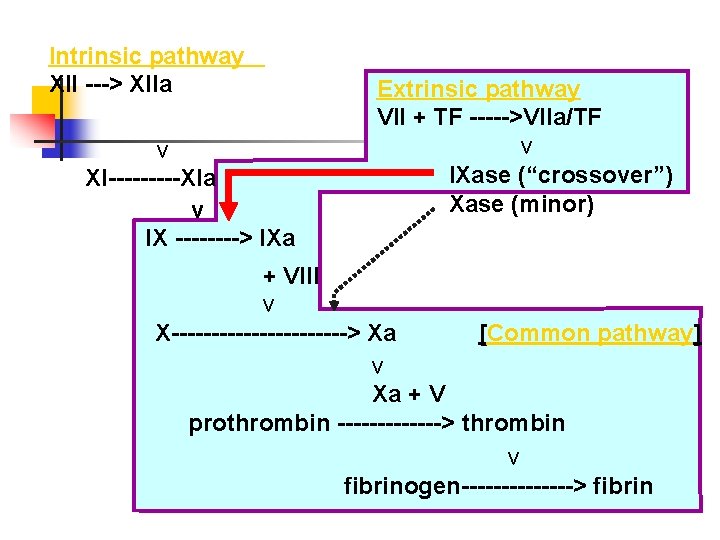
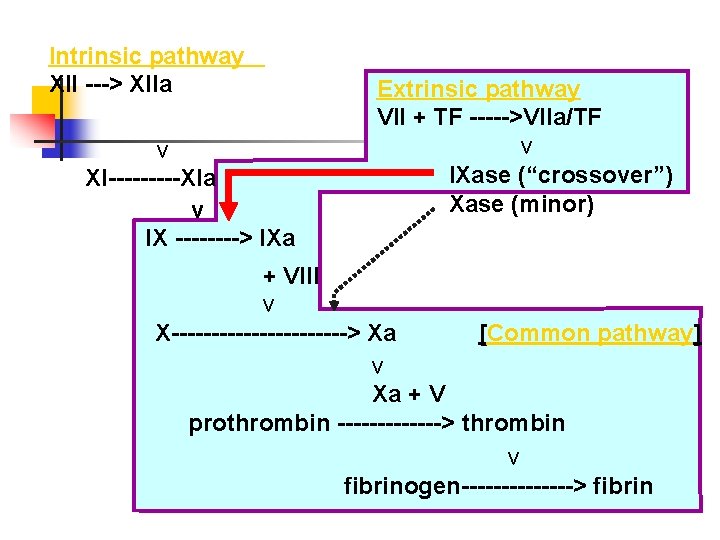
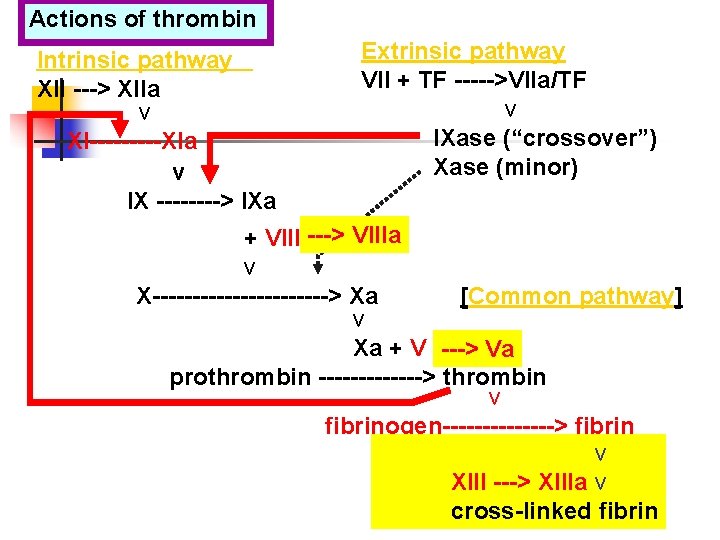
Intrinsic pathway XII ---> XIIa v XI-----XIa v IX ----> IXa Extrinsic pathway VII + TF ----->VIIa/TF v IXase (“crossover”) Xase (minor) + VIII v X-----------> Xa [Common pathway] v Xa + V prothrombin -------> thrombin v fibrinogen-------> fibrin
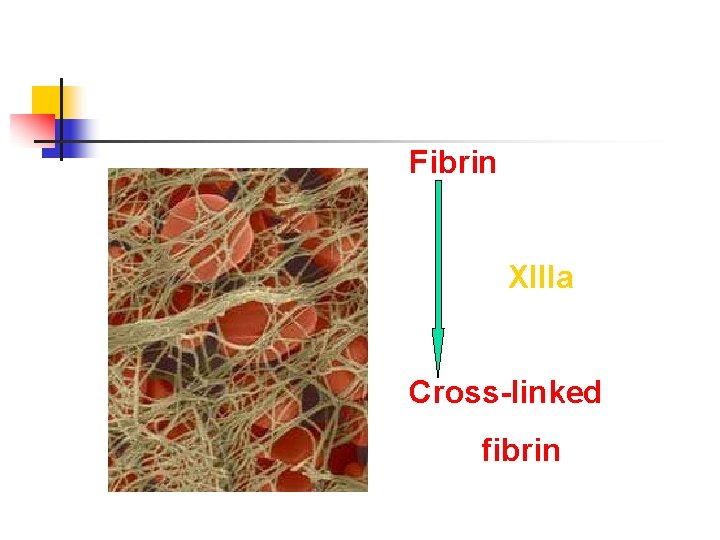
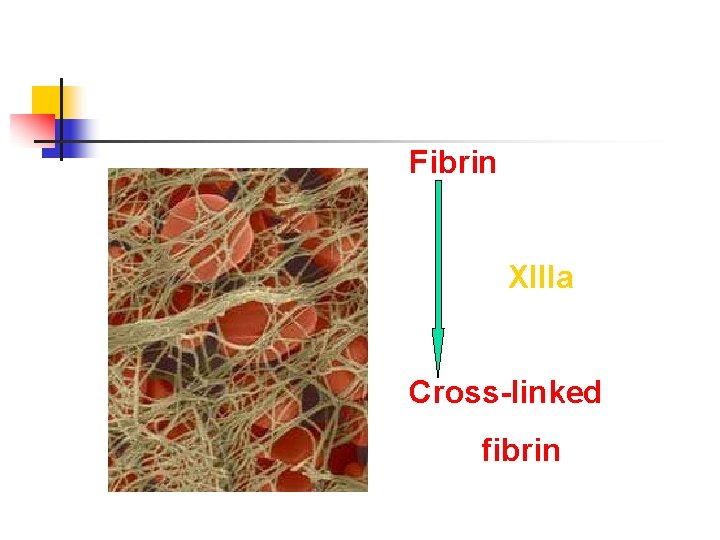
Fibrin XIIIa Cross-linked fibrin
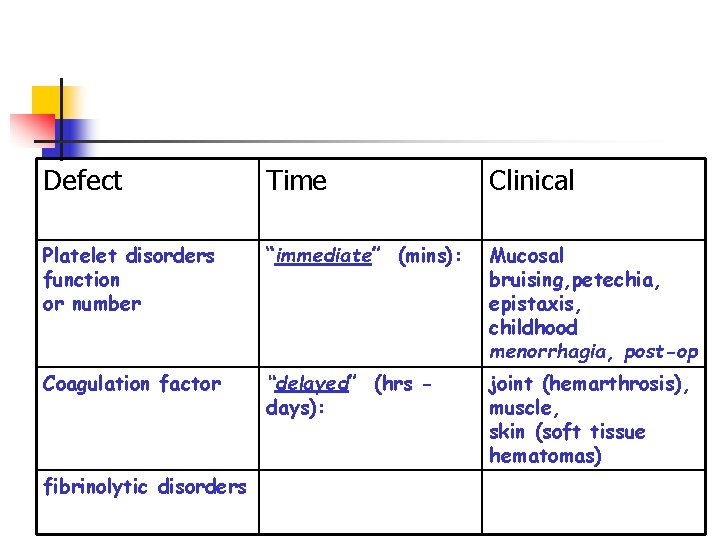
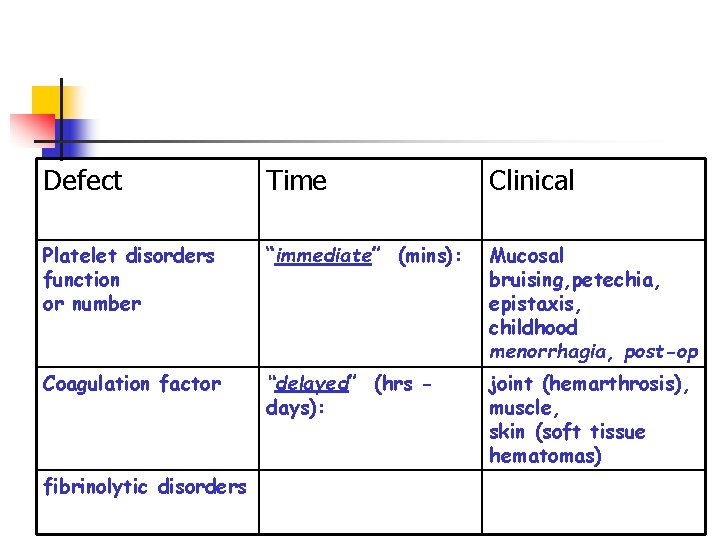
Defect Time Clinical Platelet disorders function or number “immediate” (mins): Mucosal bruising, petechia, epistaxis, childhood menorrhagia, post-op Coagulation factor “delayed” (hrs days): joint (hemarthrosis), muscle, skin (soft tissue hematomas) fibrinolytic disorders
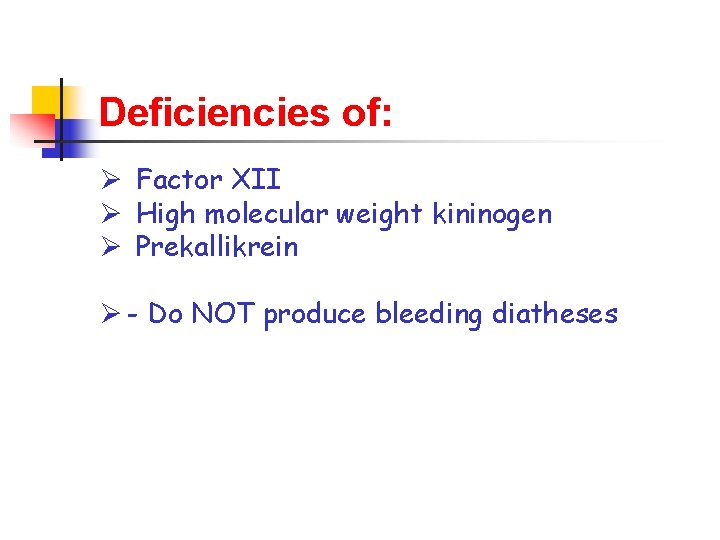
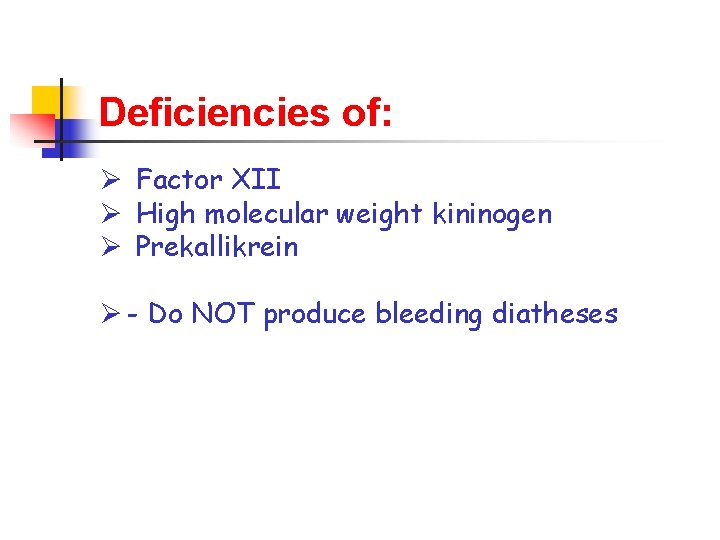
Deficiencies of: Ø Factor XII Ø High molecular weight kininogen Ø Prekallikrein Ø - Do NOT produce bleeding diatheses
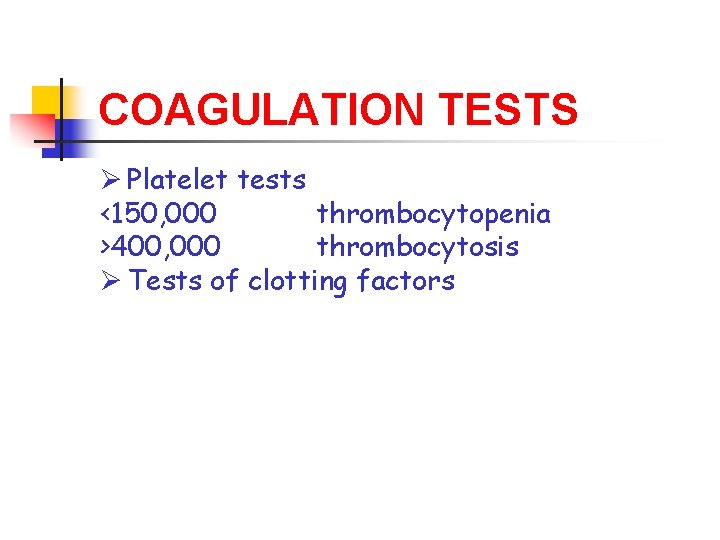
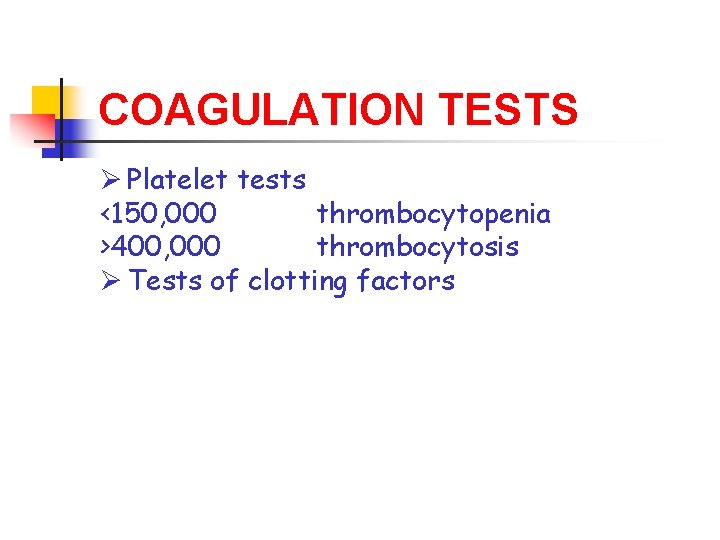
COAGULATION TESTS Ø Platelet tests <150, 000 thrombocytopenia >400, 000 thrombocytosis Ø Tests of clotting factors
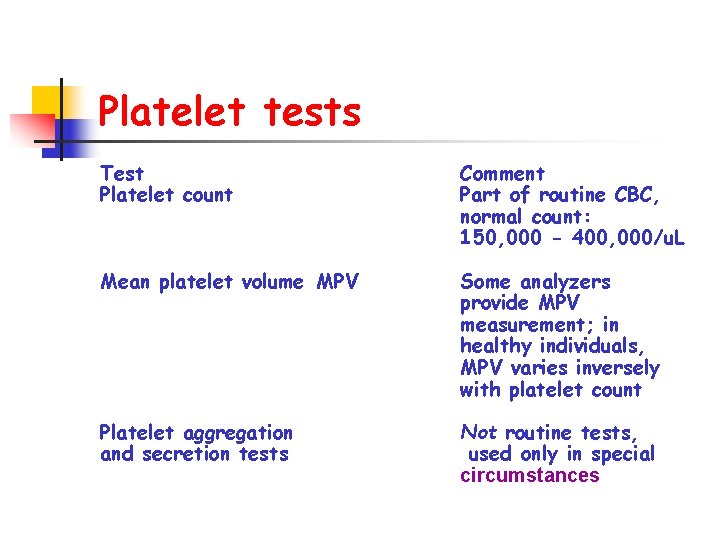
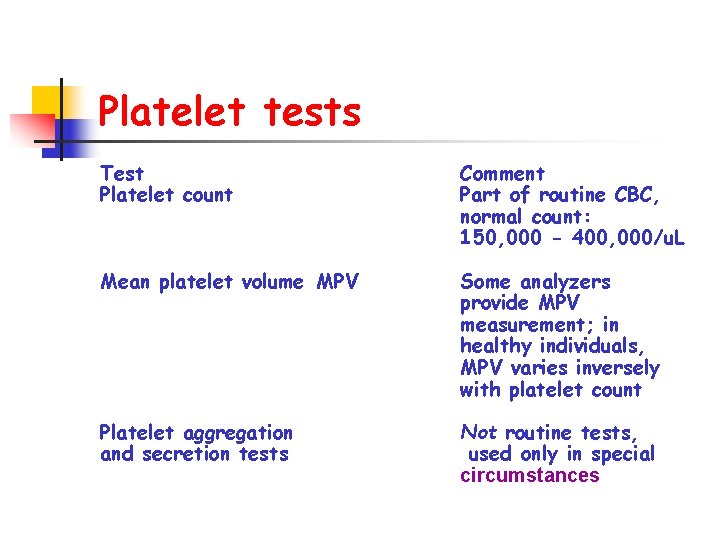
Platelet tests Test Platelet count Comment Part of routine CBC, normal count: 150, 000 - 400, 000/u. L Mean platelet volume MPV Some analyzers provide MPV measurement; in healthy individuals, MPV varies inversely with platelet count Platelet aggregation and secretion tests Not routine tests, used only in special circumstances

Tests of clotting factors Test Abbreviation Comment Prothrombin time PT extrinsic & common pathways Functional test VII X, V, II, I Partial thromboplastin PTT intrinsic & common pathways Functional test prekallikrein, HMWK XII, XI, IX, VIII X, V, II, I Thrombin time TT Fibrinogen concentration Quantitative test
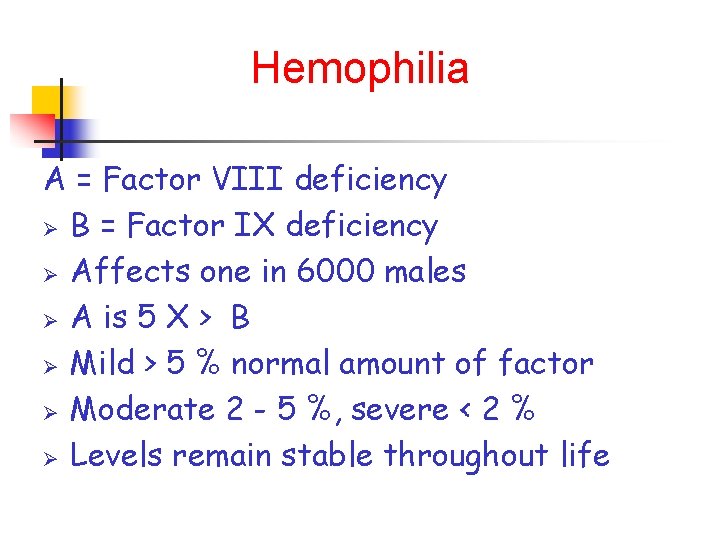
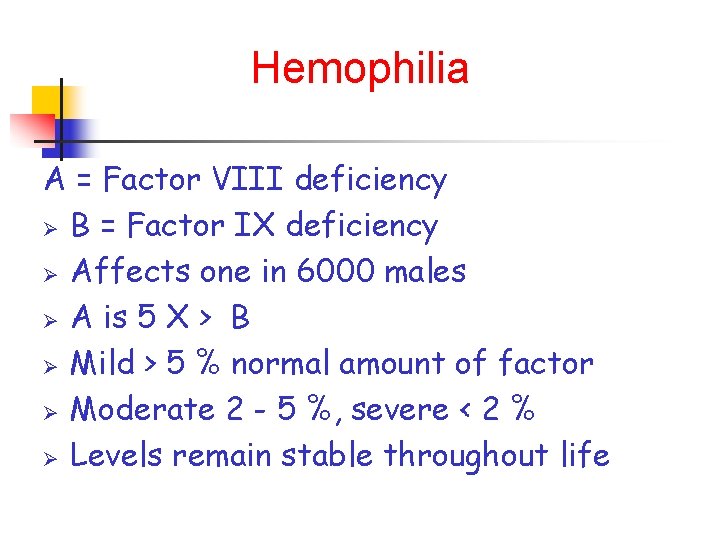
Hemophilia A = Factor VIII deficiency Ø B = Factor IX deficiency Ø Affects one in 6000 males Ø A is 5 X > B Ø Mild > 5 % normal amount of factor Ø Moderate 2 - 5 %, severe < 2 % Ø Levels remain stable throughout life
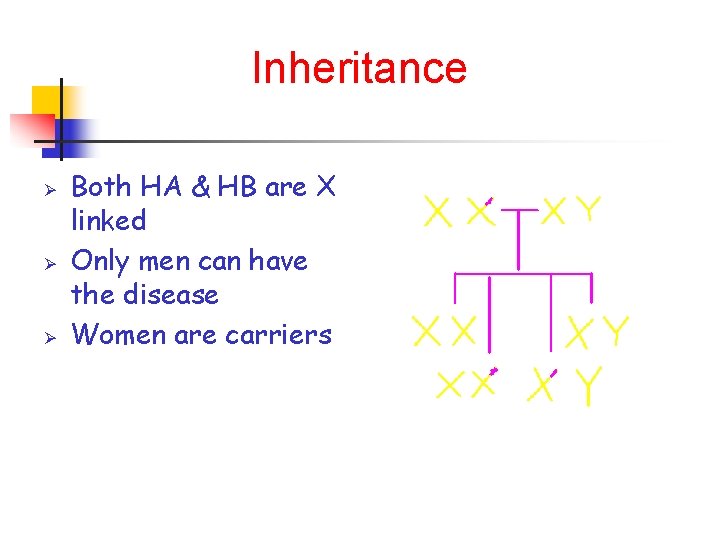
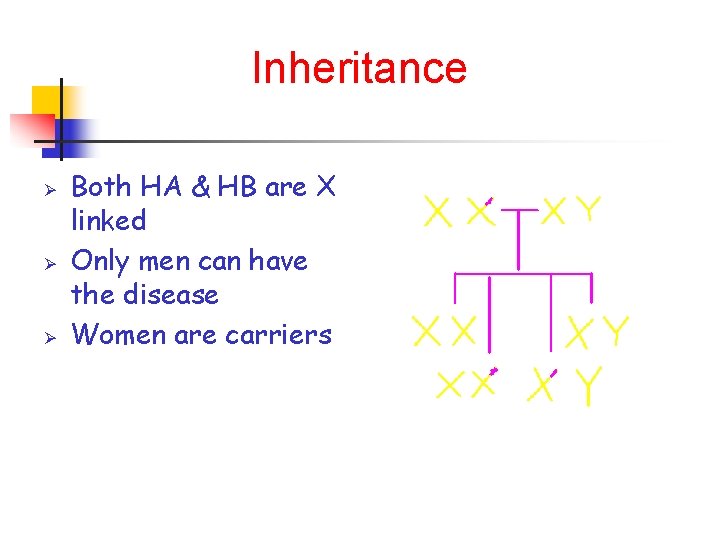
Inheritance Ø Ø Ø Both HA & HB are X linked Only men can have the disease Women are carriers
Clinical presentation Ø < 2 years: joint bleeds Rare Only bruising or mouth bleeds are seen Head injuries are a major concern Ø > 2 years joint and muscle bleeds become more common
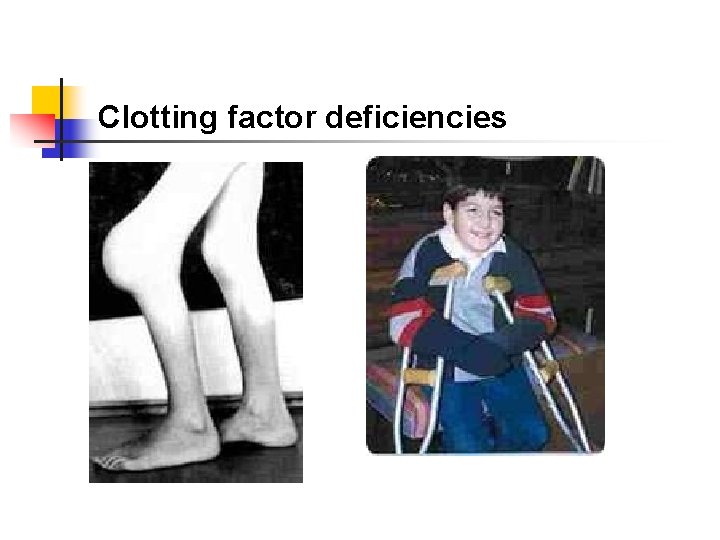
Clotting factor deficiencies
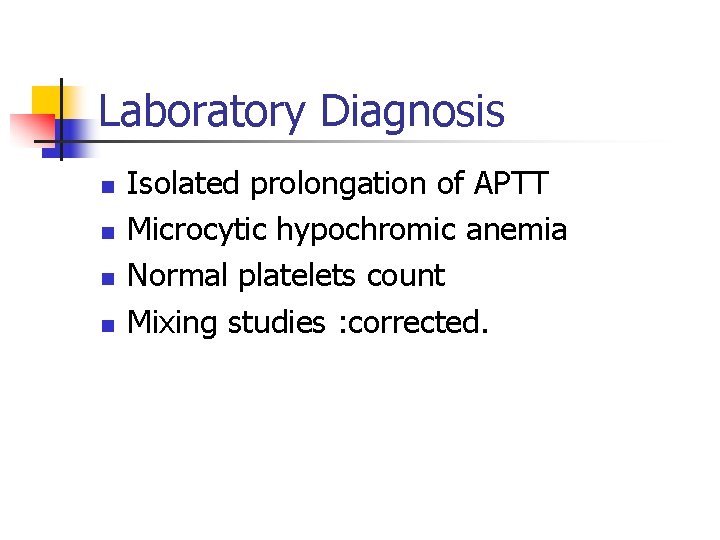
Laboratory Diagnosis n n Isolated prolongation of APTT Microcytic hypochromic anemia Normal platelets count Mixing studies : corrected.

When to treat Ø Ø All joint bleeds: Pain, swelling , warmth or loss of movement. Muscle bleeds that cause severe pain or are in a dangerous location Bruises usually don’t need treatment When in doubt.
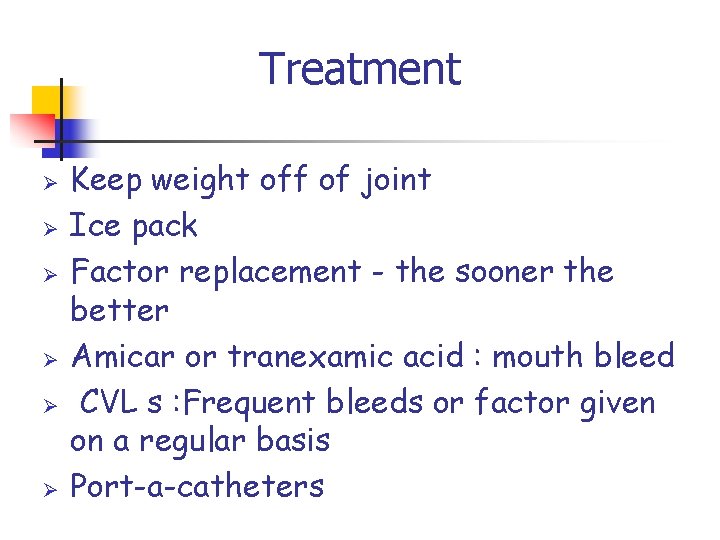
Treatment Ø Ø Ø Keep weight off of joint Ice pack Factor replacement - the sooner the better Amicar or tranexamic acid : mouth bleed CVL s : Frequent bleeds or factor given on a regular basis Port-a-catheters
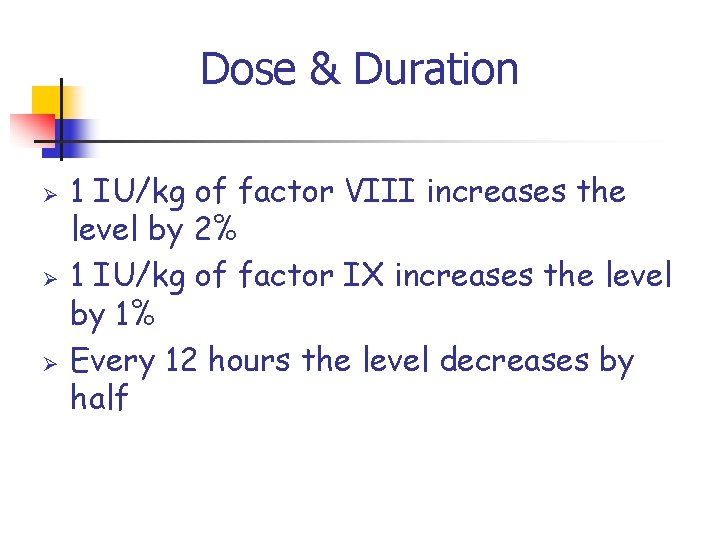
Dose & Duration Ø Ø Ø 1 IU/kg of factor VIII increases the level by 2% 1 IU/kg of factor IX increases the level by 1% Every 12 hours the level decreases by half
Prophylaxis Ø Ø Ø To prevent bleeds Started after developing a target joint Usually it is administered 3/week Stepwise approach: Initially 1/week, increasing to 2 -3/week if needed Goal is to prevent long-term joint damage
Team Approach Ø We all work together Child and parents Doctor and nurses Physiotherapy Social work Ø Ø Everyone has an essential role The aim is to get life to be as normal as possible
Factor VIII Replacement Ø Ø Mechanism of action : activate FX Mode of administration : IV Monitoring : no predict the effectiveness of treatment Indications : HA & HB Ø Ø Severe surgical bleeding Factor VII deficiency
Factor VIII Ø Ø Ø Derived from pooled human plasma Derived from pig (porcine) plasma Recombinate products

Porcine factor VIII Ø Ø Ø Hyate: C Apparently no pig viruses present Can replace human Factor VIII in clotting cascade Minimal cross reactivity with AHF antibodies Minimal von Willebrand factor present

von Willebrand Factor (V W F) Ø VWF bridges platelets to collagen exposure from blood vessel injury Ø VWF contributes to primary hemostasis Ø Factor VIII circulates bound to VWF. Ø VWD: clinically similar to platelet disorders Ø Most common inherited bleeding disorder
VWD Ø Ø Ø Ø Inherited as a dominant or recessive. Most common congenital bleeding disorder Affecting 1 -3% of the population. Personal and family bleeding history. Highly heterogeneous Ranging from asymptomatic to a life threatening bleeding. The most common bleeding symptoms ever were epistaxis, bruising Menorrhagia is one of the most important and frequent complications in women

Platelet disorders

DIAGNOSIS Ø Ø The condition is caused by a quantitative or qualitative deficiency of v. WF. Prolonged bleeding time (BT) & activated partial thromboplastin time (APTT) iron deficiency anemia. type 1 v. WD
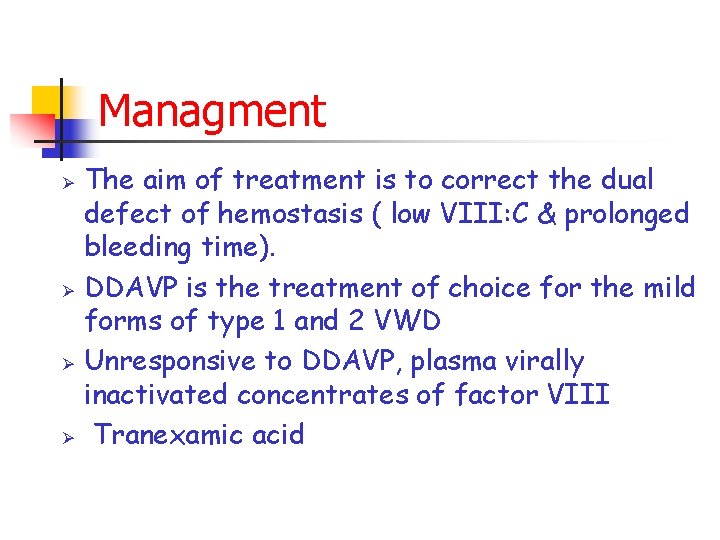
Managment Ø Ø The aim of treatment is to correct the dual defect of hemostasis ( low VIII: C & prolonged bleeding time). DDAVP is the treatment of choice for the mild forms of type 1 and 2 VWD Unresponsive to DDAVP, plasma virally inactivated concentrates of factor VIII Tranexamic acid
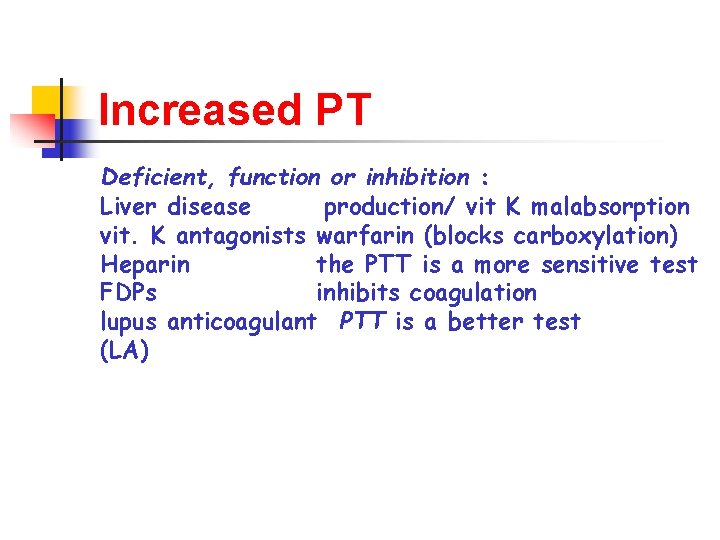
Increased PT Deficient, function or inhibition : Liver disease production/ vit K malabsorption vit. K antagonists warfarin (blocks carboxylation) Heparin the PTT is a more sensitive test FDPs inhibits coagulation lupus anticoagulant PTT is a better test (LA)
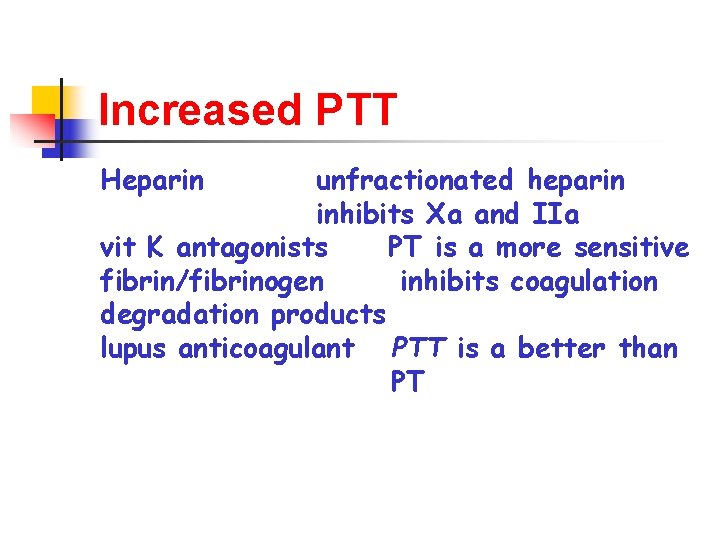
Increased PTT Heparin unfractionated heparin inhibits Xa and IIa vit K antagonists PT is a more sensitive fibrin/fibrinogen inhibits coagulation degradation products lupus anticoagulant PTT is a better than PT
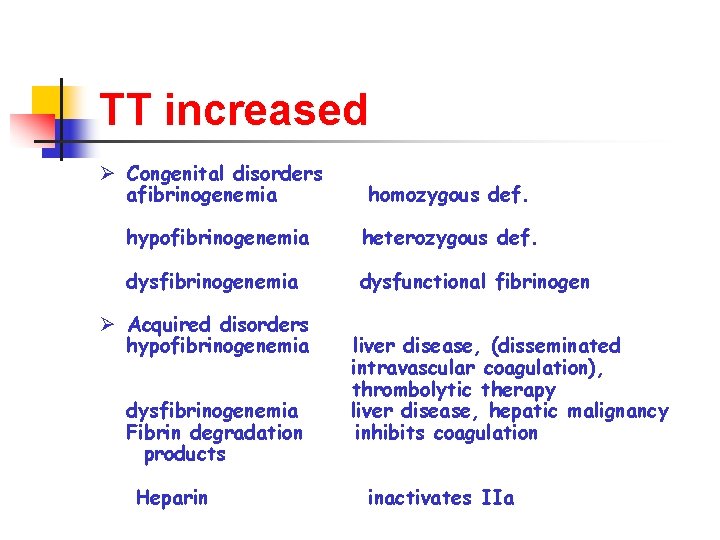
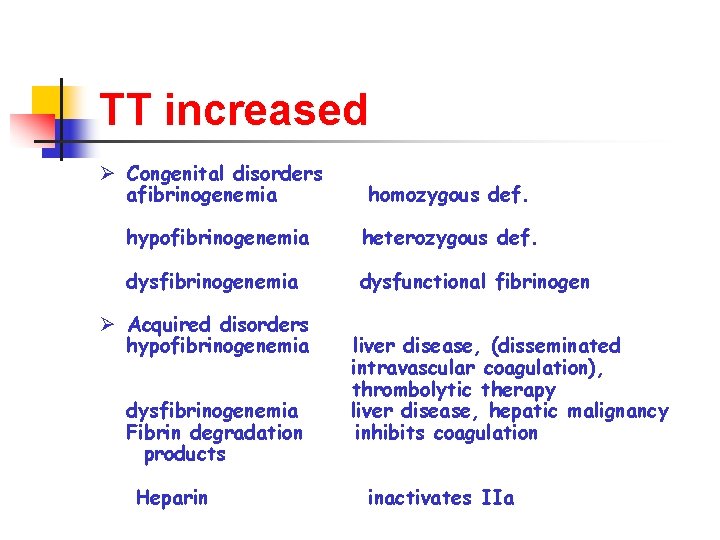
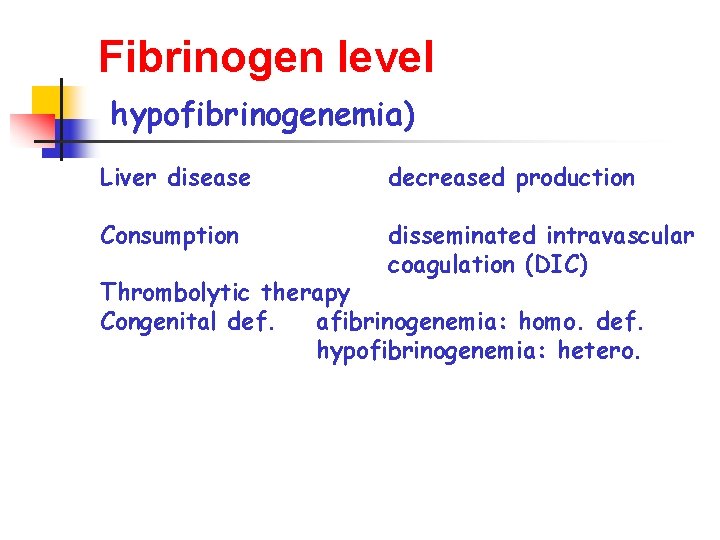
TT increased Ø Congenital disorders afibrinogenemia homozygous def. hypofibrinogenemia heterozygous def. dysfibrinogenemia dysfunctional fibrinogen Ø Acquired disorders hypofibrinogenemia dysfibrinogenemia Fibrin degradation products Heparin liver disease, (disseminated intravascular coagulation), thrombolytic therapy liver disease, hepatic malignancy inhibits coagulation inactivates IIa
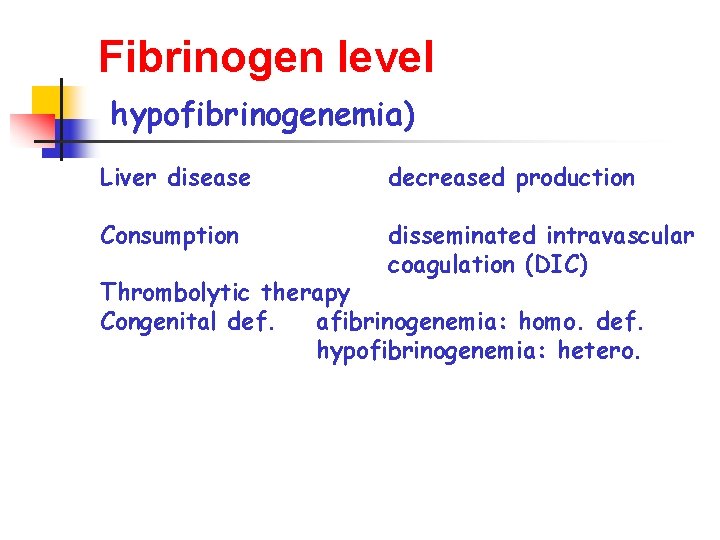
Fibrinogen level hypofibrinogenemia) Liver disease decreased production Consumption disseminated intravascular coagulation (DIC) Thrombolytic therapy Congenital def. afibrinogenemia: homo. def. hypofibrinogenemia: hetero.

Fibrinogen assay quantitative immunoassay: Functional “immunologic” or “antigenic” fibrinogen Increased: Estrogen Pregnancy Acute phase response decreased hypofibrinogenemia) also - dysfunctional fibrinogen (dysfibrinogenemia
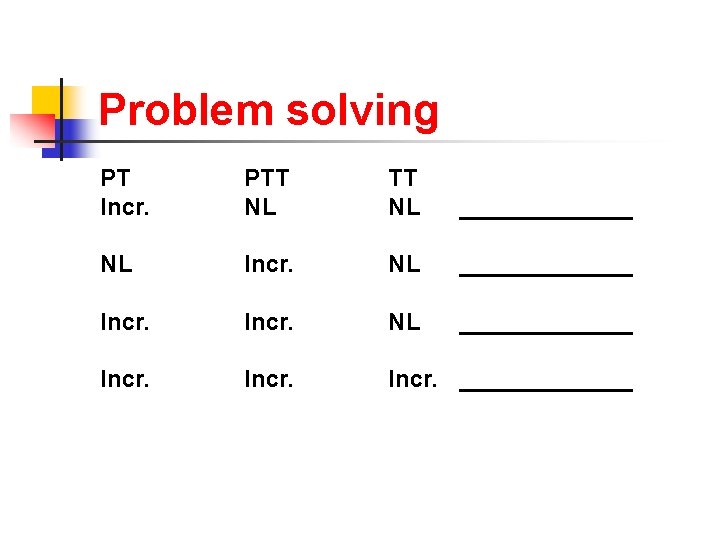
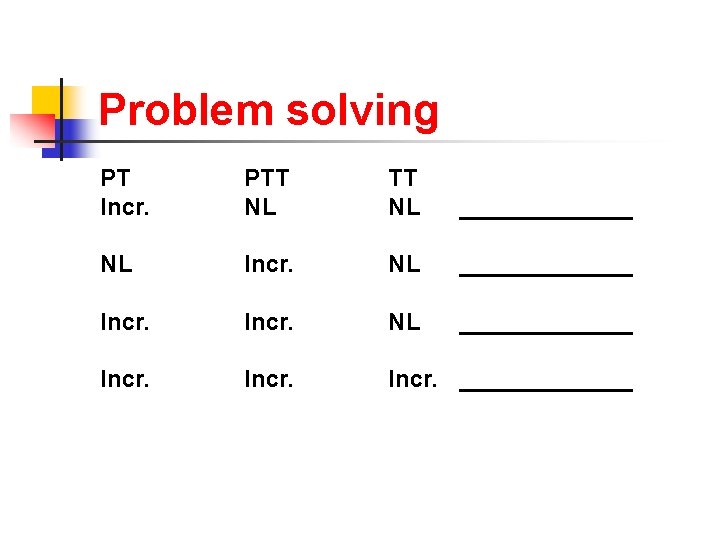
Problem solving PT Incr. PTT NL _______ NL Incr. NL _____________ Incr. _______
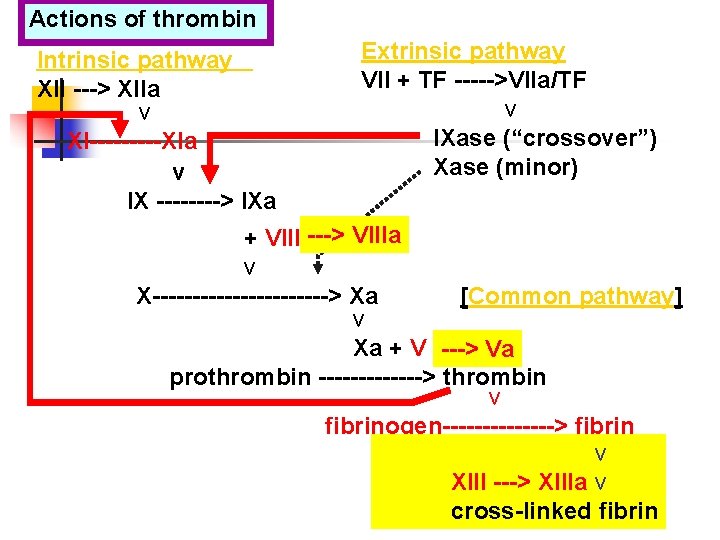
Actions of thrombin Intrinsic pathway XII ---> XIIa v XI-----XIa v IX ----> IXa Extrinsic pathway VII + TF ----->VIIa/TF v IXase (“crossover”) Xase (minor) + VIII ---> VIIIa v X-----------> Xa [Common pathway] v Xa + V ---> Va prothrombin -------> thrombin v fibrinogen-------> fibrin v XIII ---> XIIIa v cross-linked fibrin
 Coagulation disorders
Coagulation disorders Hematologist delta dental
Hematologist delta dental Hematologist delta dental
Hematologist delta dental Tarık zaher
Tarık zaher Tarık zaher
Tarık zaher Tarık zaher
Tarık zaher Ibrahim zaher
Ibrahim zaher Leishmaniasis
Leishmaniasis Hemostasis
Hemostasis Dvt workbook
Dvt workbook Clotting factors names
Clotting factors names Blood clotting mechanism
Blood clotting mechanism Coagulation pathway made easy
Coagulation pathway made easy Plasma and serum
Plasma and serum Surgical diathermy block diagram
Surgical diathermy block diagram Denaturation simple definition
Denaturation simple definition Examples of dextrinisation
Examples of dextrinisation Disseminated intravascular coagulation
Disseminated intravascular coagulation Coagulation profile test
Coagulation profile test Hemodynamic disorders pathology
Hemodynamic disorders pathology Disseminated intravascular coagulation pathophysiology
Disseminated intravascular coagulation pathophysiology Coagulation cascade
Coagulation cascade Composition of eggs
Composition of eggs Nécrose de coagulation anapath
Nécrose de coagulation anapath D'alessio
D'alessio Capillary method clotting time
Capillary method clotting time Describe the mechanism of coagulation of blood
Describe the mechanism of coagulation of blood Coagulation profile test
Coagulation profile test After looking up his friend's phone number alex
After looking up his friend's phone number alex Inherited traits are brainpop
Inherited traits are brainpop Similarities and differences between parents and offspring
Similarities and differences between parents and offspring Inherited traits and learned behaviors
Inherited traits and learned behaviors Learned traits examples
Learned traits examples Inherited trait
Inherited trait Blood type genetics
Blood type genetics An organism's inherited combination of alleles
An organism's inherited combination of alleles Are fingerprints genetically inherited
Are fingerprints genetically inherited Acquired traits in animals
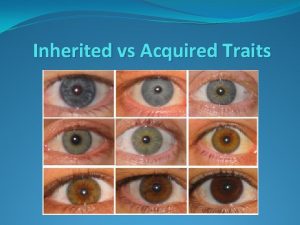
Acquired traits in animals Acquired trait
Acquired trait Ien toul
Ien toul An unchanging, biologically inherited behavior pattern.
An unchanging, biologically inherited behavior pattern. Inherited vs acquired traits
Inherited vs acquired traits