Disseminated Intravascular Coagulation Galila Zaher MRCPath 2005 Definition




- Slides: 50

Disseminated Intravascular Coagulation Galila Zaher MRCPath 2005
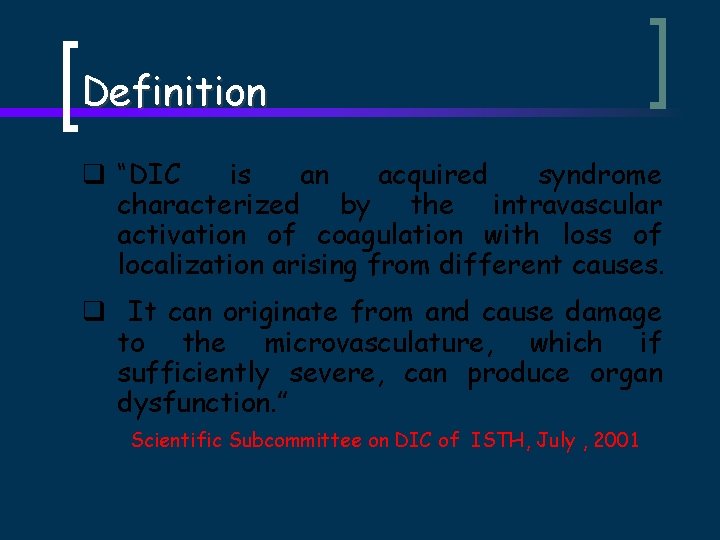
Definition q “DIC is an acquired syndrome characterized by the intravascular activation of coagulation with loss of localization arising from different causes. q It can originate from and cause damage to the microvasculature, which if sufficiently severe, can produce organ dysfunction. ” Scientific Subcommittee on DIC of ISTH, July , 2001
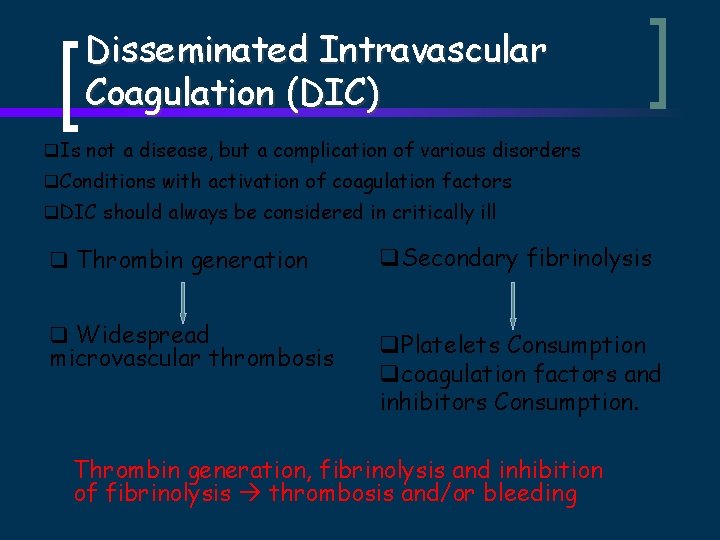
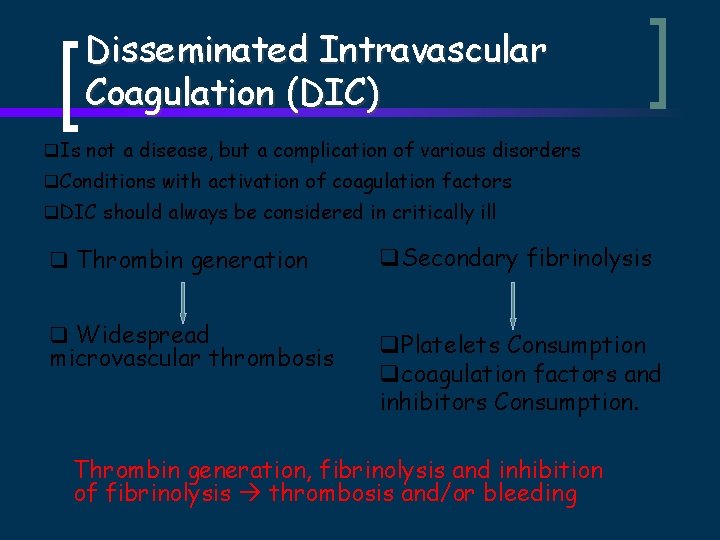
Disseminated Intravascular Coagulation (DIC) q. Is not a disease, but a complication of various disorders q. Conditions with activation of coagulation factors q. DIC should always be considered in critically ill q Thrombin generation q. Secondary fibrinolysis q Widespread q. Platelets Consumption qcoagulation factors and inhibitors Consumption. microvascular thrombosis Thrombin generation, fibrinolysis and inhibition of fibrinolysis thrombosis and/or bleeding
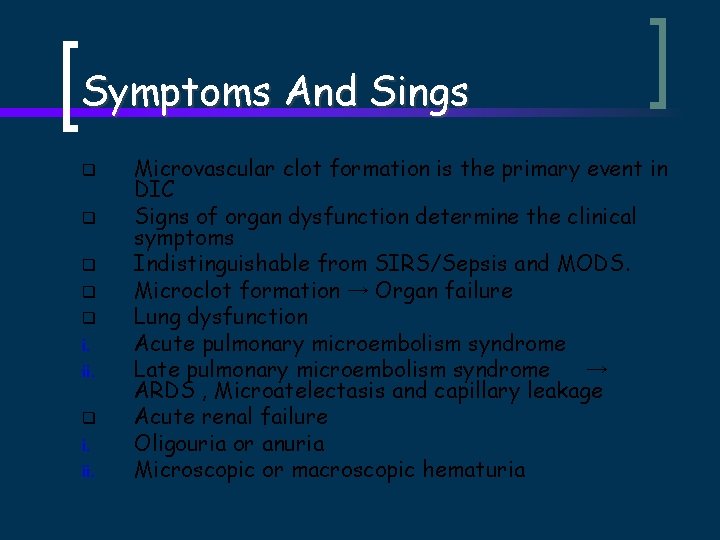
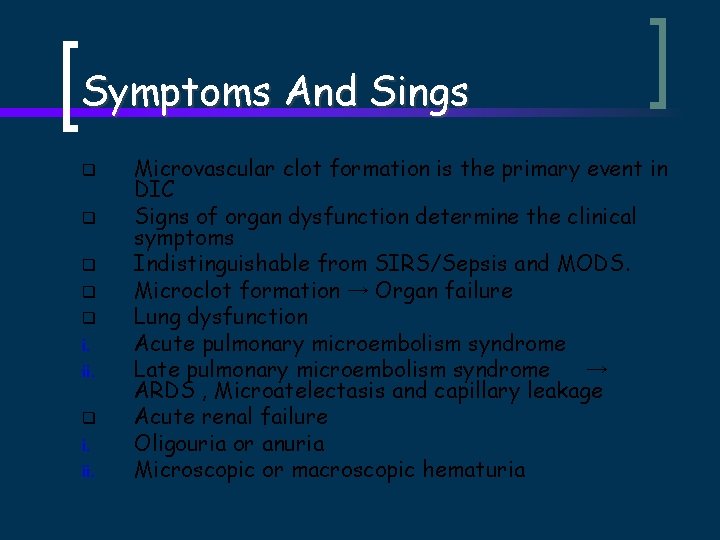
Symptoms And Sings q q q i. ii. Microvascular clot formation is the primary event in DIC Signs of organ dysfunction determine the clinical symptoms Indistinguishable from SIRS/Sepsis and MODS. Microclot formation → Organ failure Lung dysfunction Acute pulmonary microembolism syndrome Late pulmonary microembolism syndrome → ARDS , Microatelectasis and capillary leakage Acute renal failure Oligouria or anuria Microscopic or macroscopic hematuria
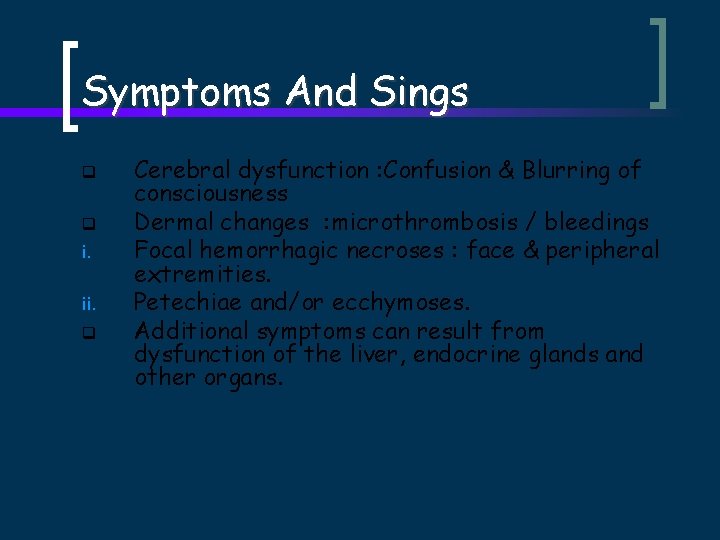
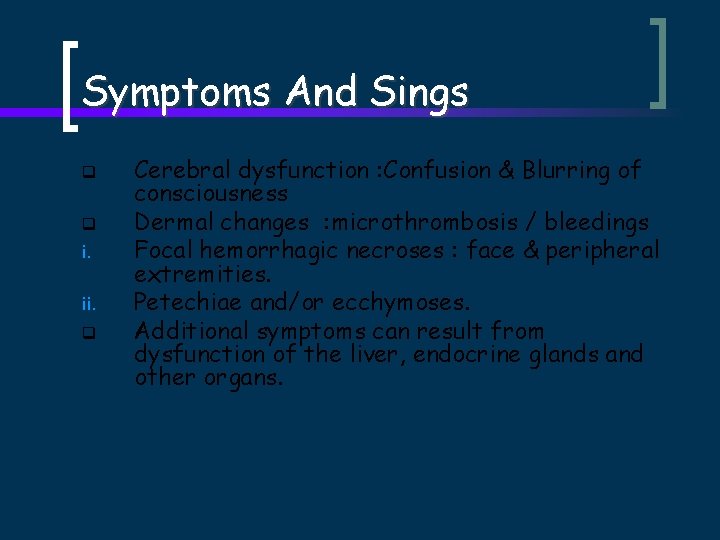
Symptoms And Sings q q i. ii. q Cerebral dysfunction : Confusion & Blurring of consciousness Dermal changes : microthrombosis / bleedings Focal hemorrhagic necroses : face & peripheral extremities. Petechiae and/or ecchymoses. Additional symptoms can result from dysfunction of the liver, endocrine glands and other organs.
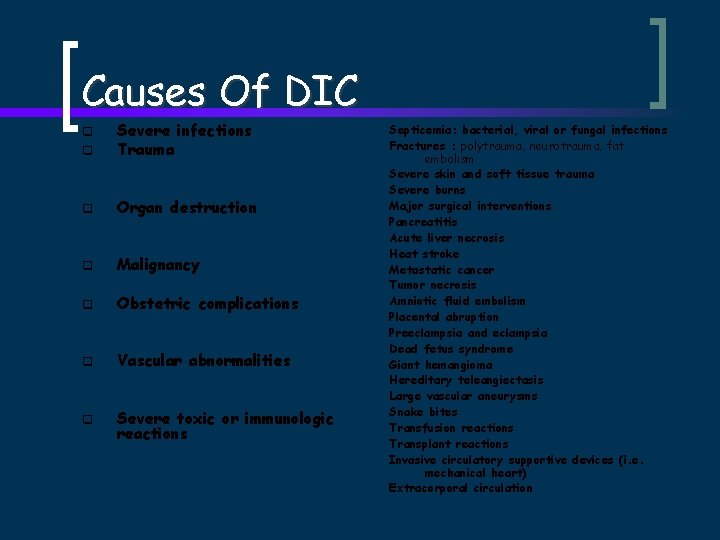
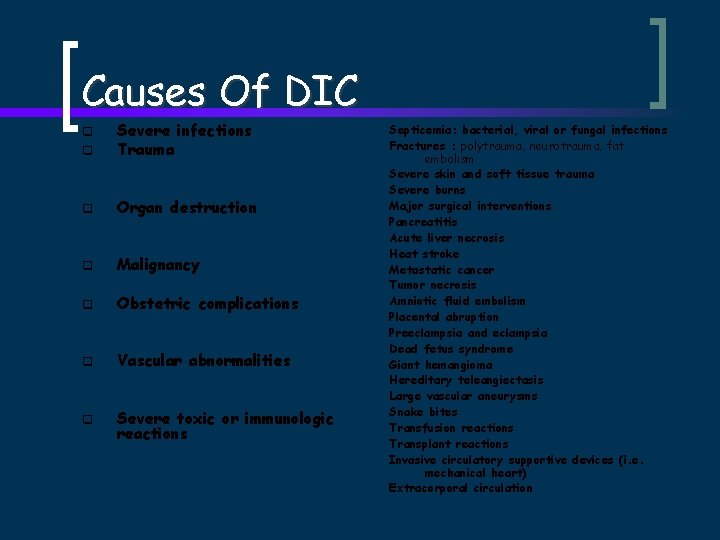
Causes Of DIC q Severe infections Trauma q Organ destruction q Malignancy q Obstetric complications q Vascular abnormalities q Severe toxic or immunologic reactions q Septicemia: bacterial, viral or fungal infections Fractures : polytrauma, neurotrauma, fat embolism Severe skin and soft tissue trauma Severe burns Major surgical interventions Pancreatitis Acute liver necrosis Heat stroke Metastatic cancer Tumor necrosis Amniotic fluid embolism Placental abruption Preeclampsia and eclampsia Dead fetus syndrome Giant hemangioma Hereditary teleangiectasis Large vascular aneurysms Snake bites Transfusion reactions Transplant reactions Invasive circulatory supportive devices (i. e. mechanical heart) Extracorporal circulation
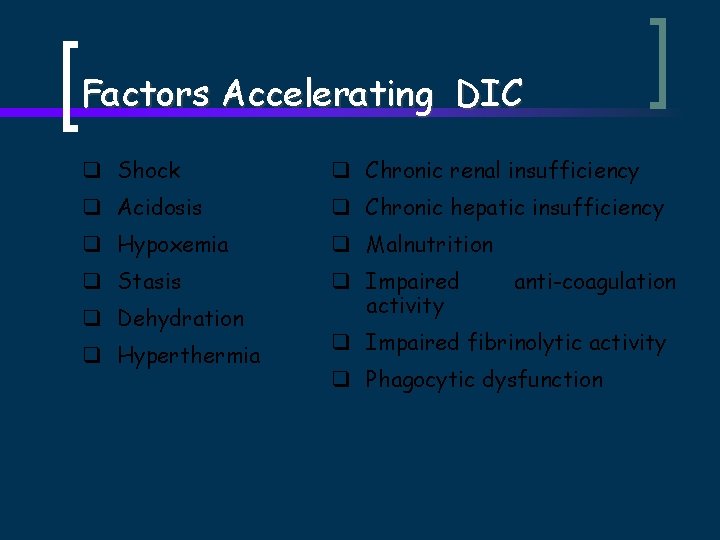
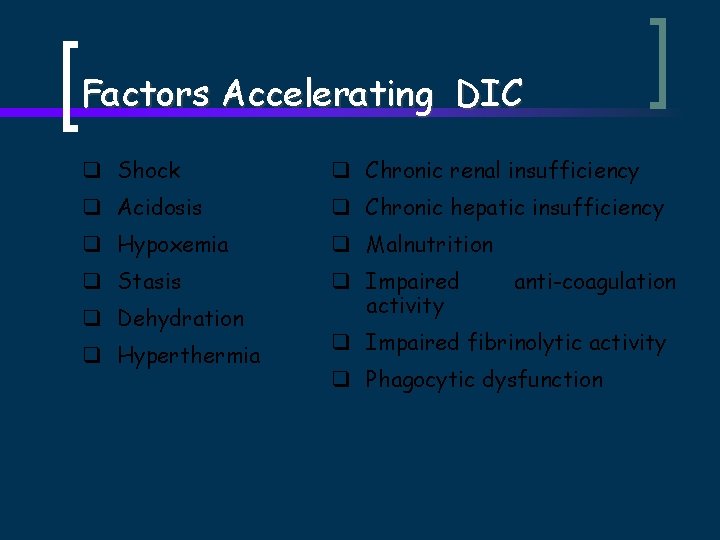
Factors Accelerating DIC q Shock q Chronic renal insufficiency q Acidosis q Chronic hepatic insufficiency q Hypoxemia q Malnutrition q Stasis q Impaired activity q Dehydration q Hyperthermia anti-coagulation q Impaired fibrinolytic activity q Phagocytic dysfunction
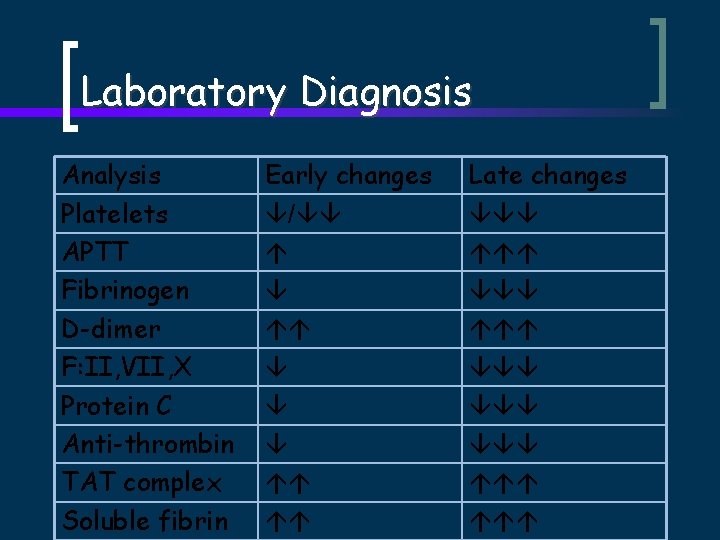
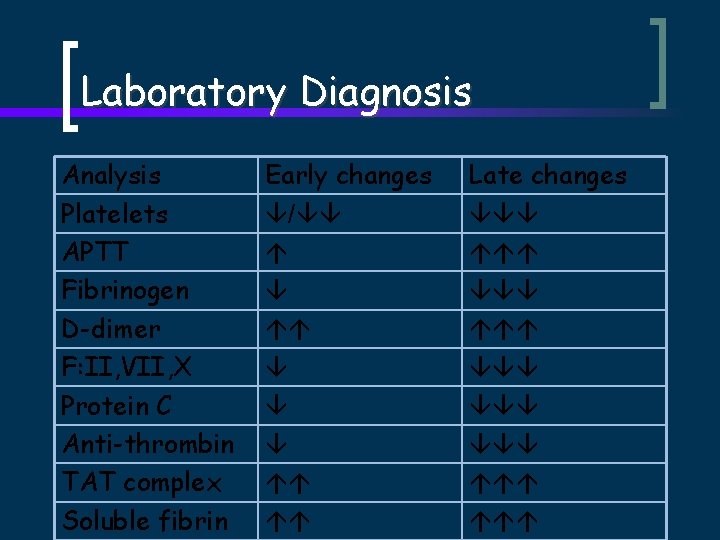
Laboratory Diagnosis Analysis Platelets APTT Fibrinogen D-dimer F: II, VII, X Protein C Anti-thrombin TAT complex Soluble fibrin Early changes / Late changes
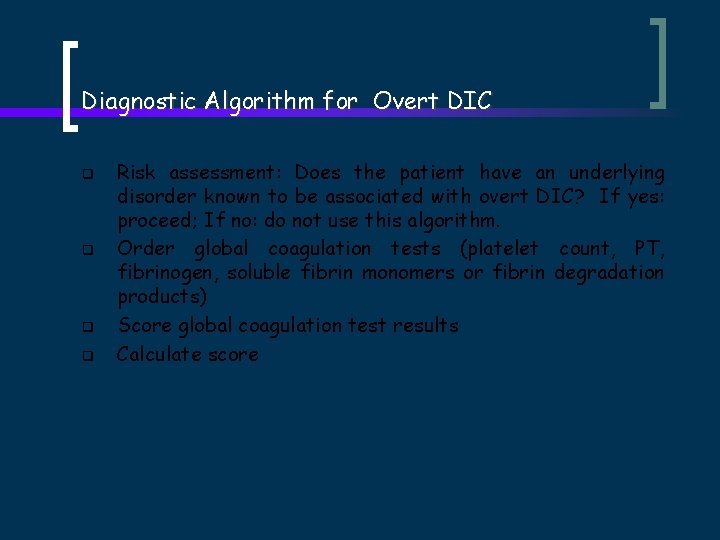
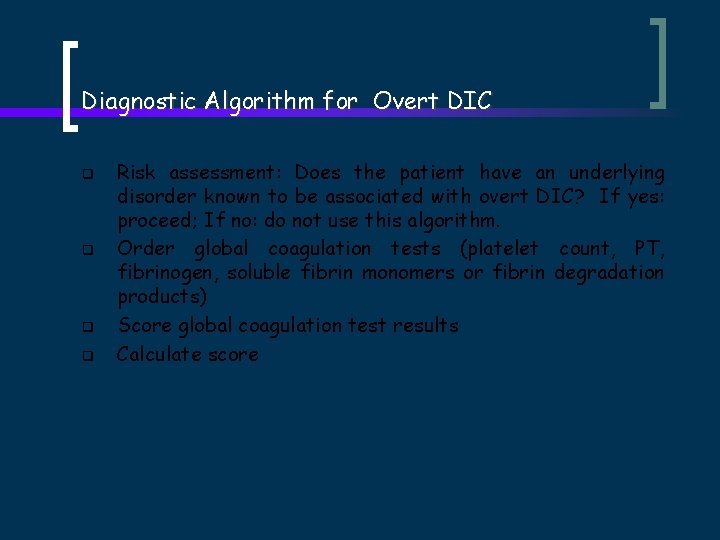
Diagnostic Algorithm for Overt DIC q q Risk assessment: Does the patient have an underlying disorder known to be associated with overt DIC? If yes: proceed; If no: do not use this algorithm. Order global coagulation tests (platelet count, PT, fibrinogen, soluble fibrin monomers or fibrin degradation products) Score global coagulation test results Calculate score
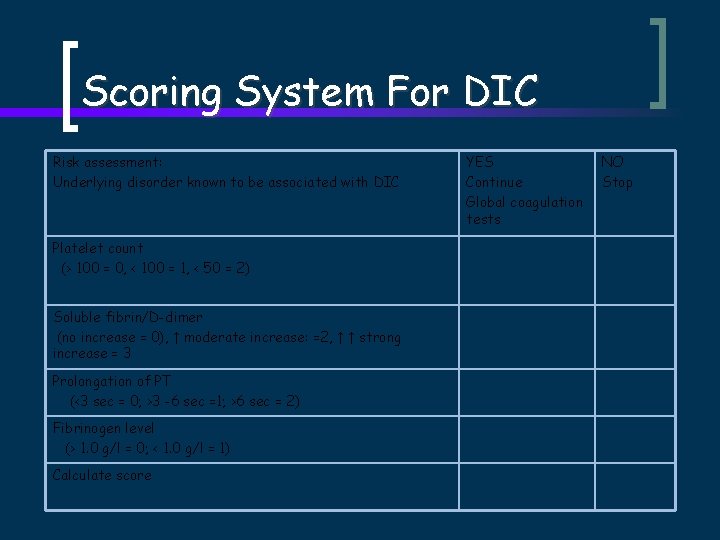
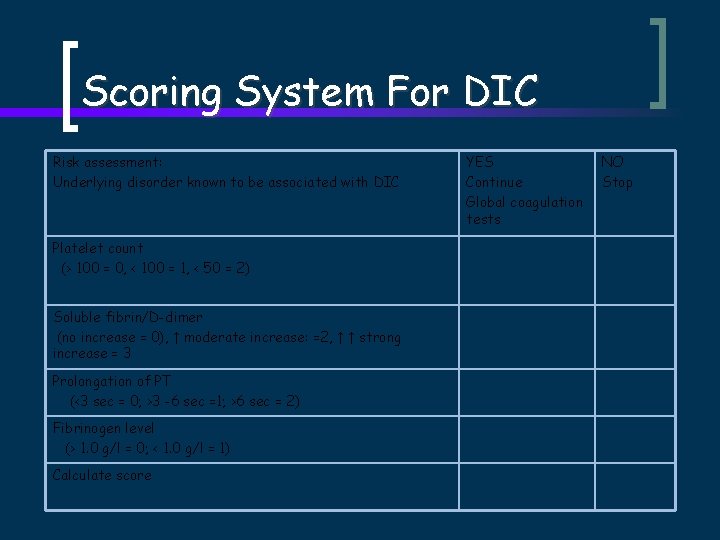
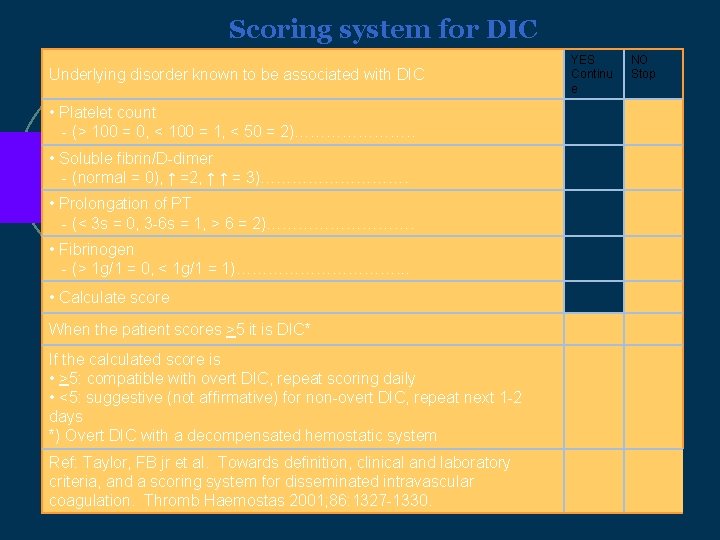
Scoring System For DIC Risk assessment: Underlying disorder known to be associated with DIC Platelet count (> 100 = 0, < 100 = 1, < 50 = 2) Soluble fibrin/D-dimer (no increase = 0), ↑ moderate increase: =2, ↑ ↑ strong increase = 3 Prolongation of PT (<3 sec = 0; >3 -6 sec =1; >6 sec = 2) Fibrinogen level (> 1. 0 g/l = 0; < 1. 0 g/l = 1) Calculate score YES Continue Global coagulation tests NO Stop
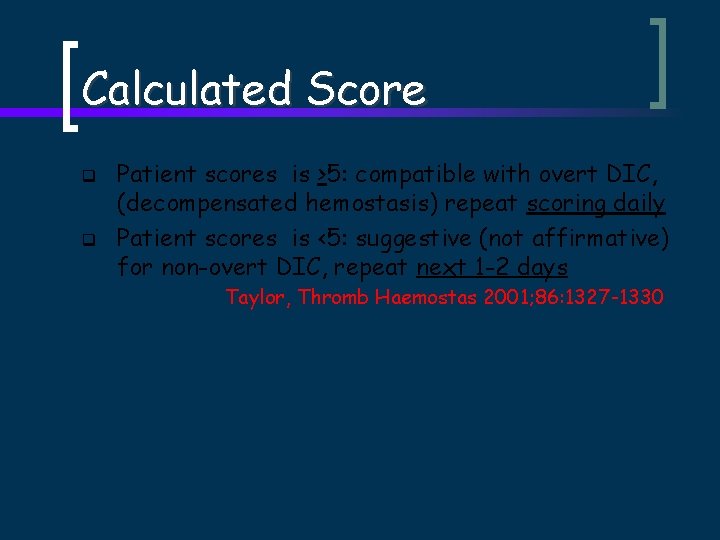
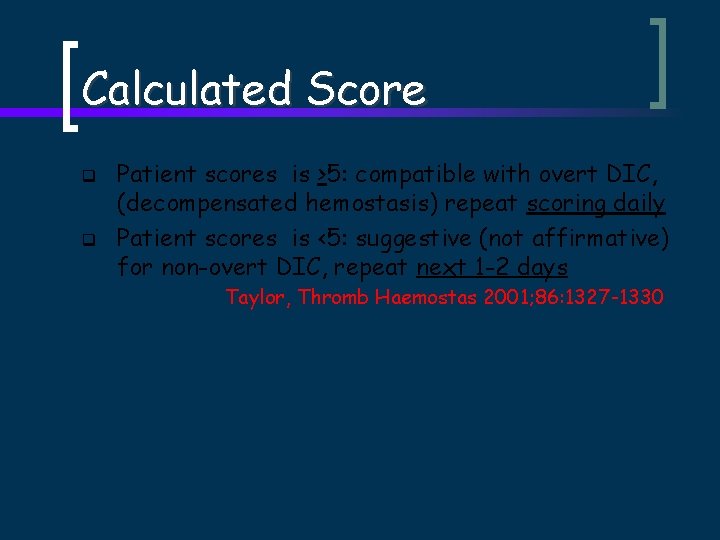
Calculated Score q q Patient scores is >5: compatible with overt DIC, (decompensated hemostasis) repeat scoring daily Patient scores is <5: suggestive (not affirmative) for non-overt DIC, repeat next 1 -2 days Taylor, Thromb Haemostas 2001; 86: 1327 -1330
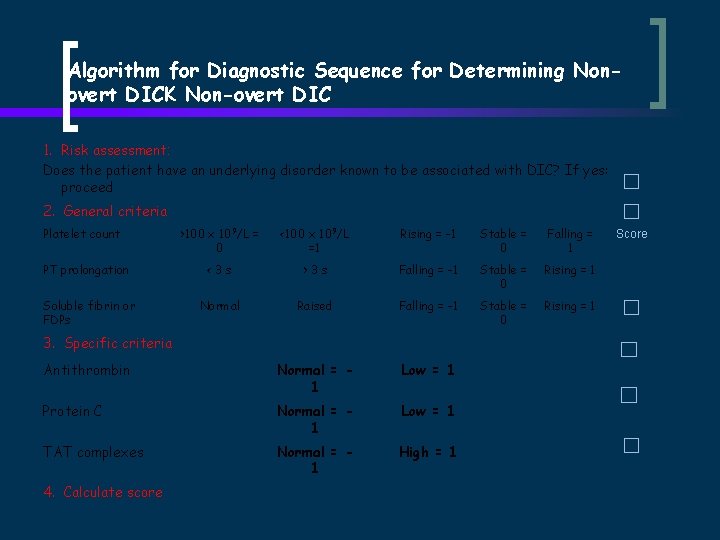
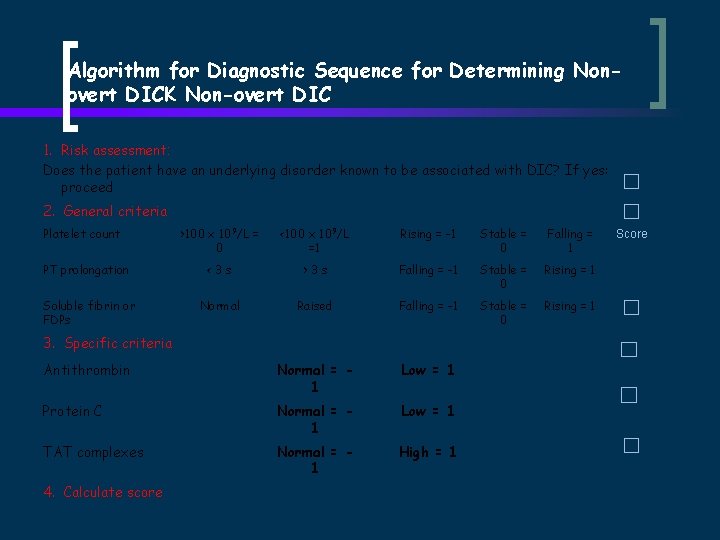
Algorithm for Diagnostic Sequence for Determining Nonovert DICK Non-overt DIC 1. Risk assessment: Does the patient have an underlying disorder known to be associated with DIC? If yes: proceed 2. General criteria Platelet count >100 x 109/L = 0 <100 x 109/L =1 Rising = -1 Stable = 0 Falling = 1 PT prolongation <3 s >3 s Falling = -1 Stable = 0 Rising = 1 Soluble fibrin or FDPs Normal Raised Falling = -1 Stable = 0 Rising = 1 Antithrombin Normal = 1 Low = 1 Protein C Normal = 1 Low = 1 TAT complexes Normal = 1 High = 1 3. Specific criteria 4. Calculate score Score
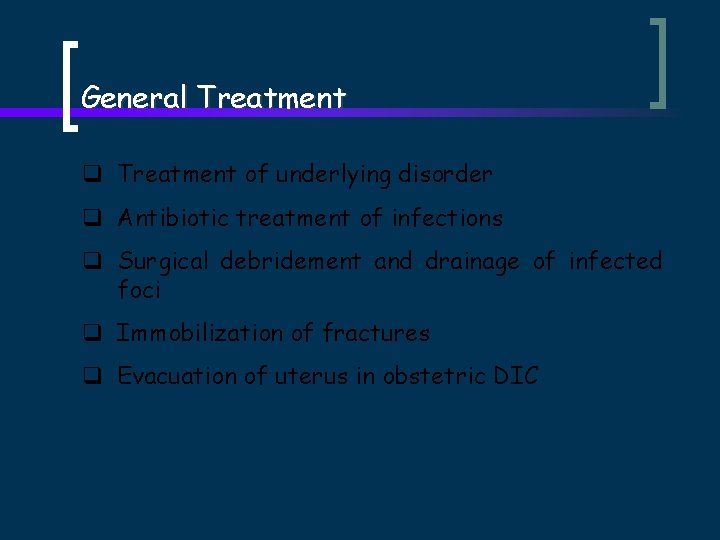
General Treatment q Treatment of underlying disorder q Antibiotic treatment of infections q Surgical debridement and drainage of infected foci q Immobilization of fractures q Evacuation of uterus in obstetric DIC
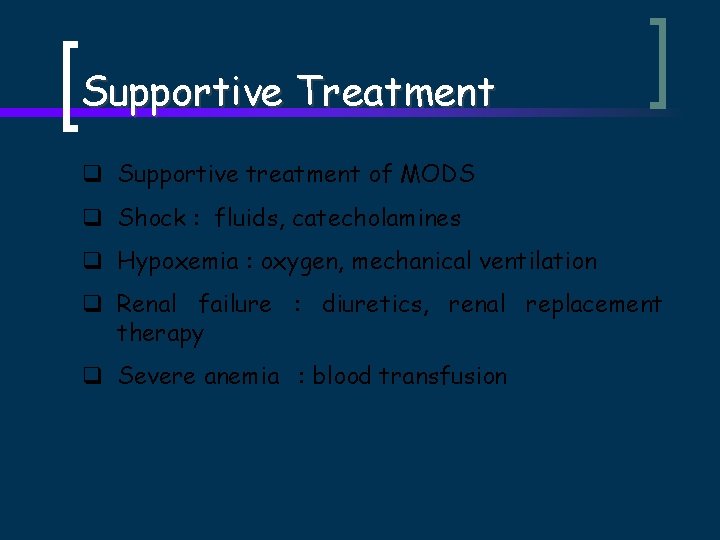
Supportive Treatment q Supportive treatment of MODS q Shock : fluids, catecholamines q Hypoxemia : oxygen, mechanical ventilation q Renal failure : diuretics, renal replacement therapy q Severe anemia : blood transfusion
Hemostatic Therapy q Antithrombotic treatment q AT concentrate. q q Concurrent treatment with heparin should be avoided, heparinworsens thrombocytopenia
ATenative q q q A quality antithrombin (AT)concentrate Loading dose for adult (70 kg) patient 2 x 1500 IU vials Follow up treatment based on measured AT levels Free from denatured AT (Hellstern et al, 1995) Two specific viral inactivation steps (SD + pasteurization) When treating DIC with AT , heparin should be avoided due to high risk of bleeding comlications Hoffmann et al, 2002
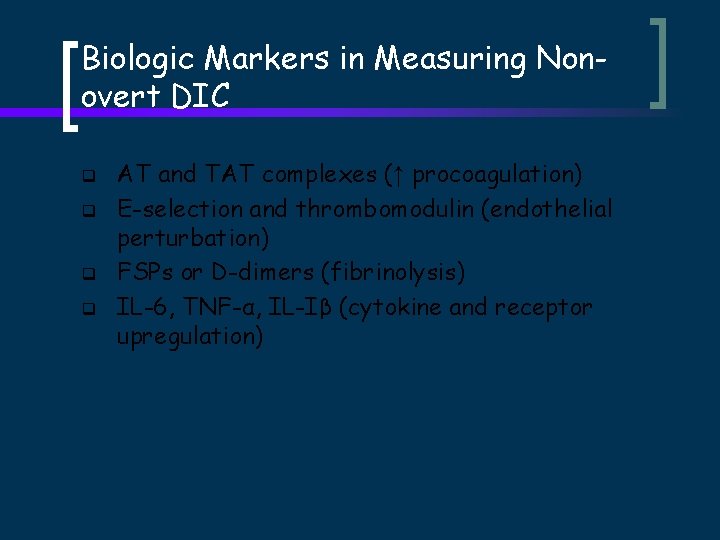
Biologic Markers in Measuring Nonovert DIC q q AT and TAT complexes (↑ procoagulation) E-selection and thrombomodulin (endothelial perturbation) FSPs or D-dimers (fibrinolysis) IL-6, TNF-α, IL-Iβ (cytokine and receptor upregulation)
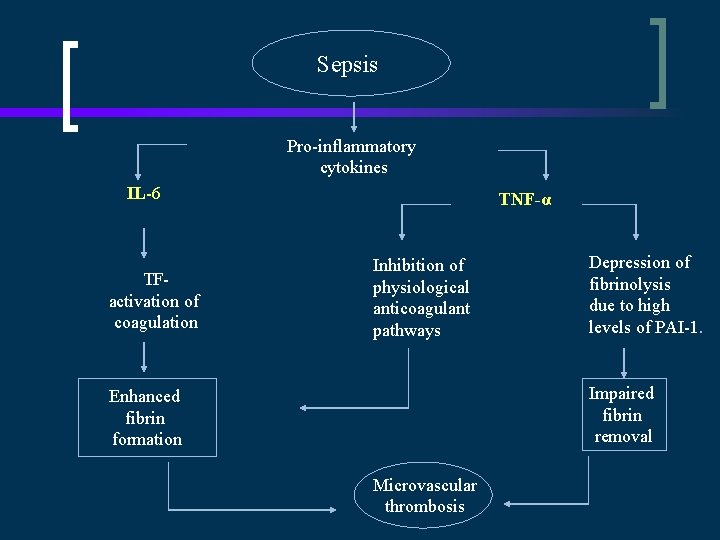
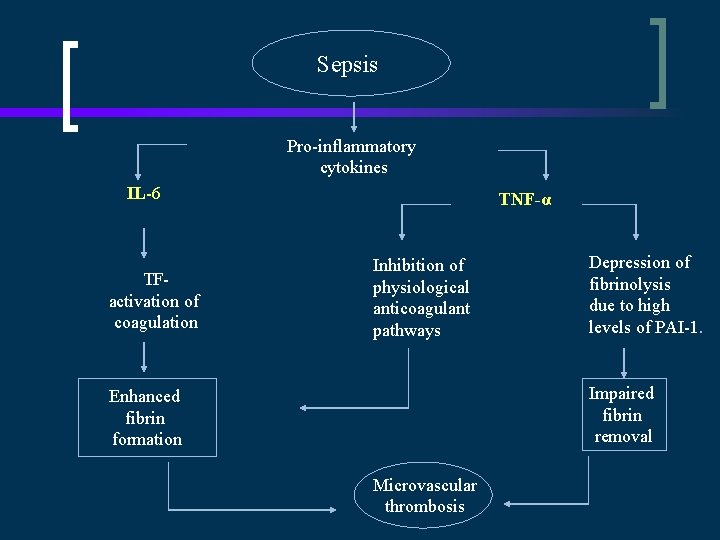
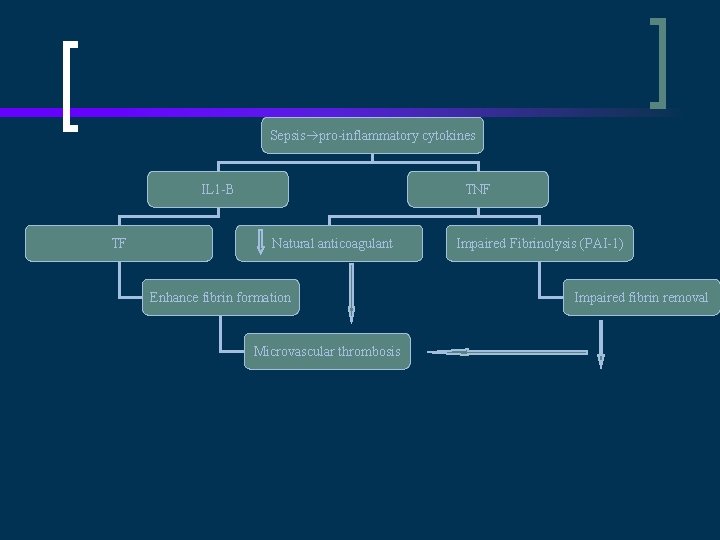
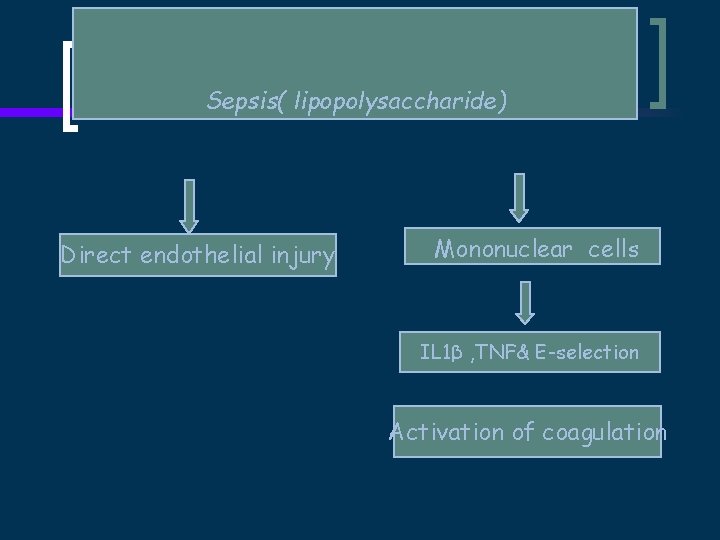
Sepsis Pro-inflammatory cytokines IL-6 TFactivation of coagulation TNF-α Inhibition of physiological anticoagulant pathways Depression of fibrinolysis due to high levels of PAI-1. Impaired fibrin removal Enhanced fibrin formation Microvascular thrombosis
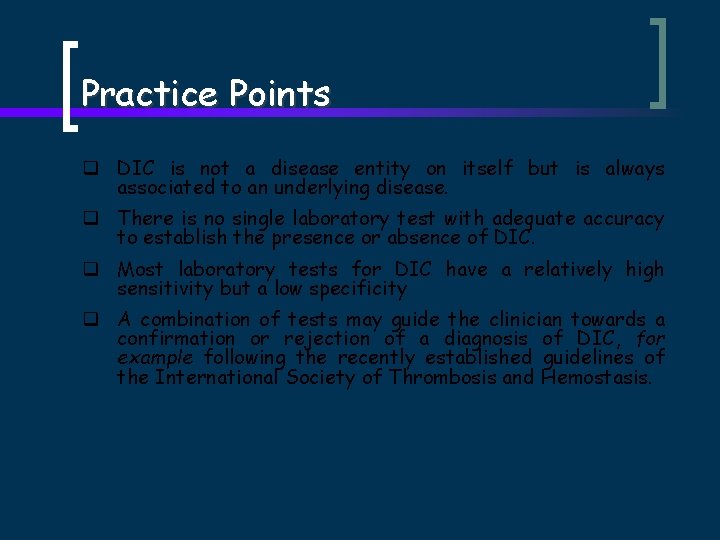
Practice Points q DIC is not a disease entity on itself but is always associated to an underlying disease. q There is no single laboratory test with adequate accuracy to establish the presence or absence of DIC. q Most laboratory tests for DIC have a relatively high sensitivity but a low specificity q A combination of tests may guide the clinician towards a confirmation or rejection of a diagnosis of DIC, for example following the recently established guidelines of the International Society of Thrombosis and Hemostasis.
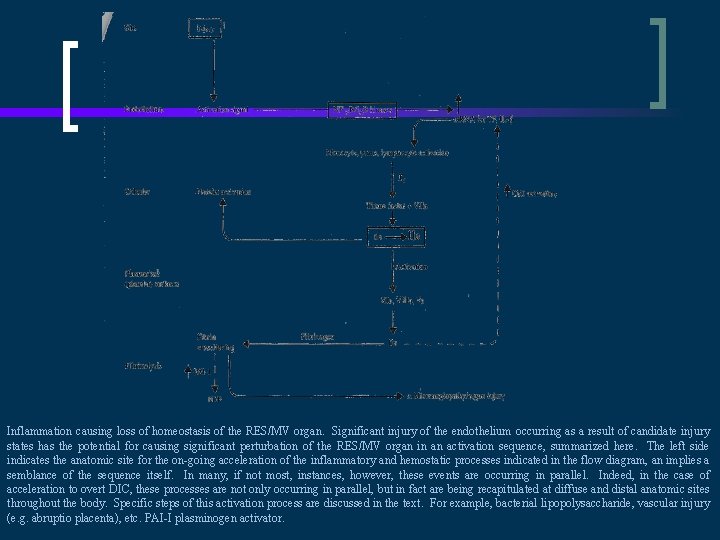
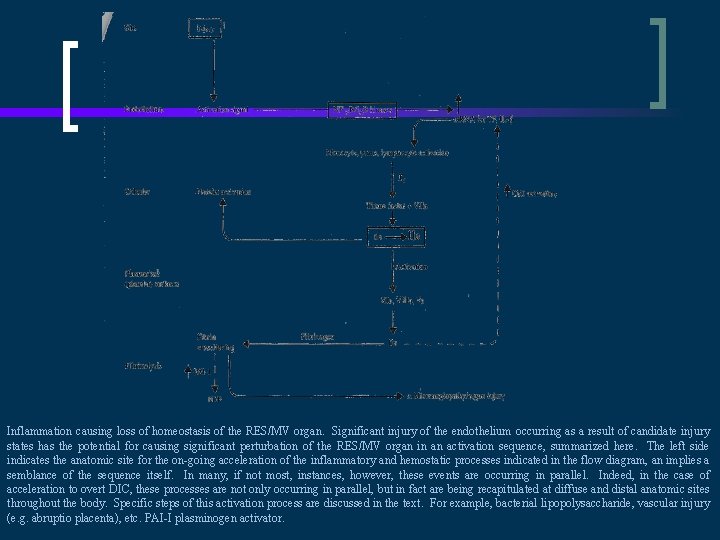
Inflammation causing loss of homeostasis of the RES/MV organ. Significant injury of the endothelium occurring as a result of candidate injury states has the potential for causing significant perturbation of the RES/MV organ in an activation sequence, summarized here. The left side indicates the anatomic site for the on-going acceleration of the inflammatory and hemostatic processes indicated in the flow diagram, an implies a semblance of the sequence itself. In many, if not most, instances, however, these events are occurring in parallel. Indeed, in the case of acceleration to overt DIC, these processes are not only occurring in parallel, but in fact are being recapitulated at diffuse and distal anatomic sites throughout the body. Specific steps of this activation process are discussed in the text. For example, bacterial lipopolysaccharide, vascular injury (e. g. abruptio placenta), etc. PAI-I plasminogen activator.
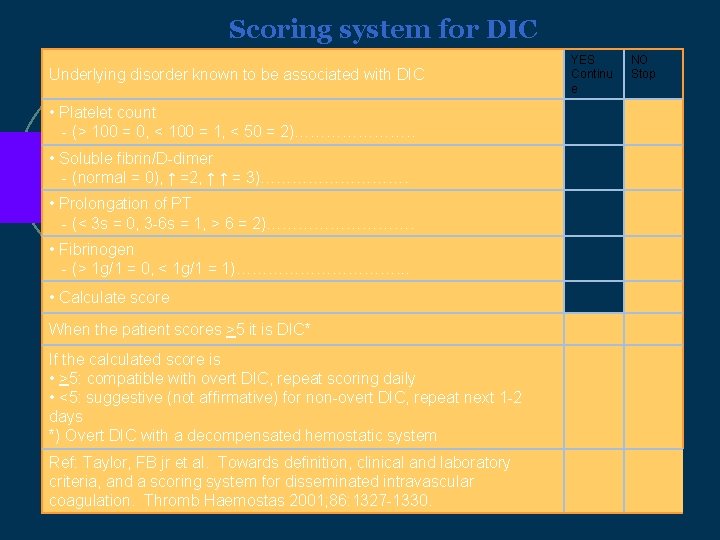
Scoring system for DIC Underlying disorder known to be associated with DIC • Platelet count - (> 100 = 0, < 100 = 1, < 50 = 2)…………………. . • Soluble fibrin/D-dimer - (normal = 0), ↑ =2, ↑ ↑ = 3)……………. • Prolongation of PT - (< 3 s = 0, 3 -6 s = 1, > 6 = 2)……………. • Fibrinogen - (> 1 g/1 = 0, < 1 g/1 = 1)……………. . . • Calculate score When the patient scores >5 it is DIC* If the calculated score is • >5: compatible with overt DIC, repeat scoring daily • <5: suggestive (not affirmative) for non-overt DIC, repeat next 1 -2 days *) Overt DIC with a decompensated hemostatic system Ref: Taylor, FB jr et al. Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemostas 2001; 86: 1327 -1330. YES Continu e NO Stop
DIC Subcommittee of the ISTH Dr Galila Zaher Consultant Haematologist MRCPath
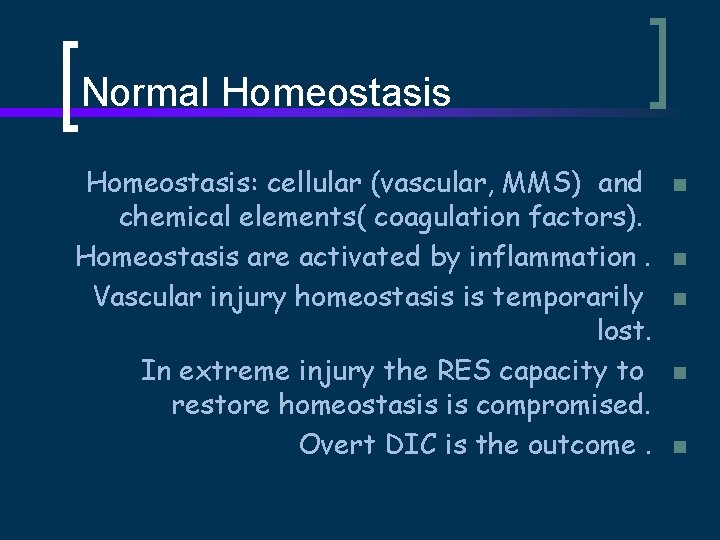
Normal Homeostasis: cellular (vascular, MMS) and chemical elements( coagulation factors). Homeostasis are activated by inflammation. Vascular injury homeostasis is temporarily lost. In extreme injury the RES capacity to restore homeostasis is compromised. Overt DIC is the outcome. n n n
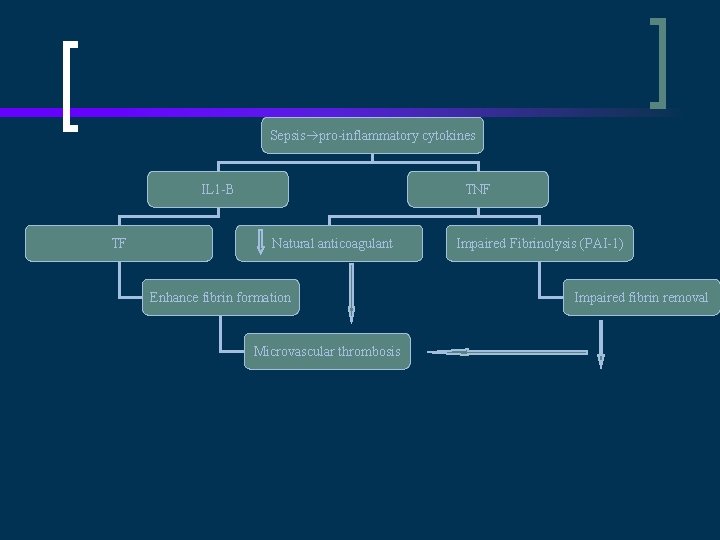
Sepsis pro-inflammatory cytokines IL 1 -B TF TNF Natural anticoagulant Enhance fibrin formation Microvascular thrombosis Impaired Fibrinolysis (PAI-1) Impaired fibrin removal
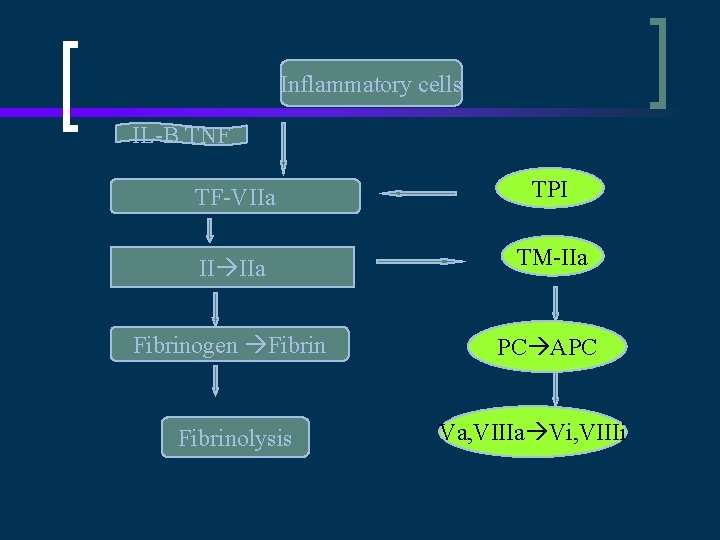
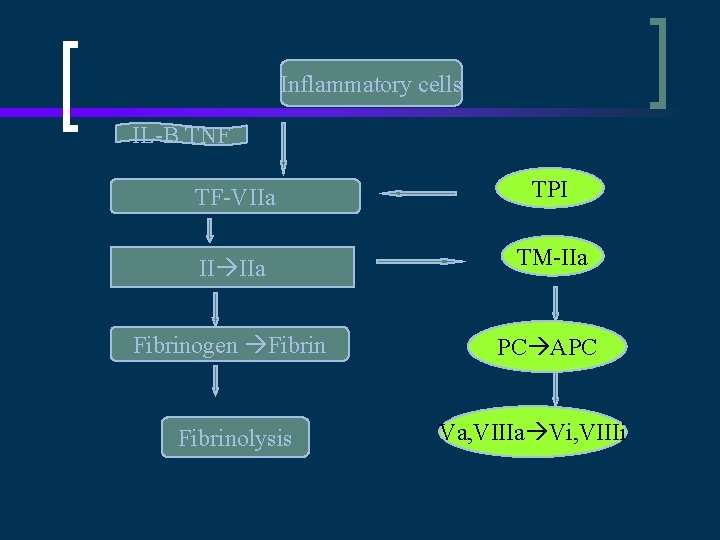
Inflammatory cells IL-B TNF TF-VIIa TPI II IIa TM-IIa Fibrinogen Fibrin PC APC Fibrinolysis Va, VIIIa Vi, VIIIi
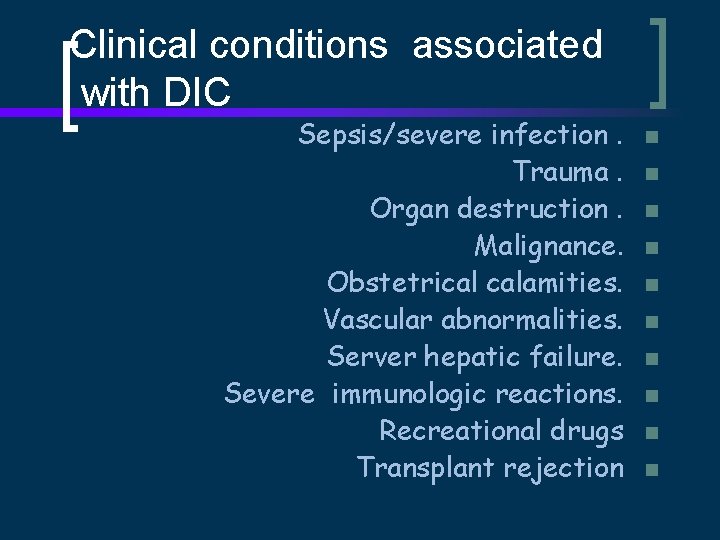
Clinical conditions associated with DIC Sepsis/severe infection. Trauma. Organ destruction. Malignance. Obstetrical calamities. Vascular abnormalities. Server hepatic failure. Severe immunologic reactions. Recreational drugs Transplant rejection n n
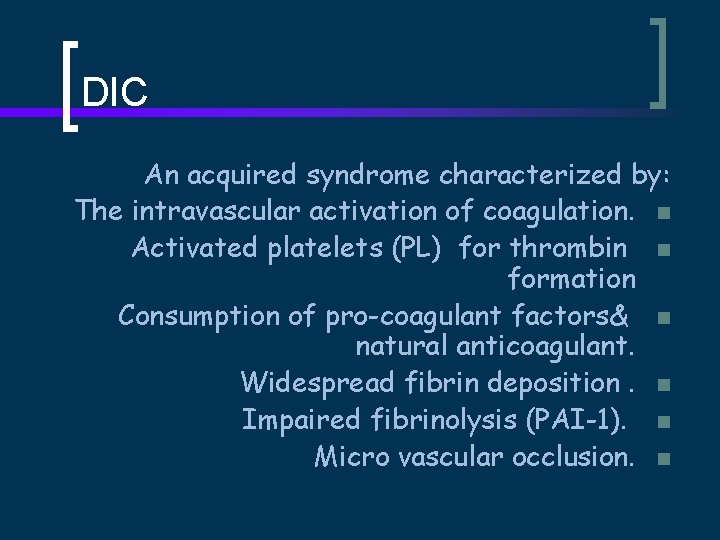
DIC An acquired syndrome characterized by: The intravascular activation of coagulation. n Activated platelets (PL) for thrombin n formation Consumption of pro-coagulant factors& n natural anticoagulant. Widespread fibrin deposition. n Impaired fibrinolysis (PAI-1). n Micro vascular occlusion. n
DIC Pro-inflammatory & pro-hemostatic. n Non-overt DIC. n Overt DIC. n Multiple organ dysfunction. n Decreased survival potential n ISTH SSC
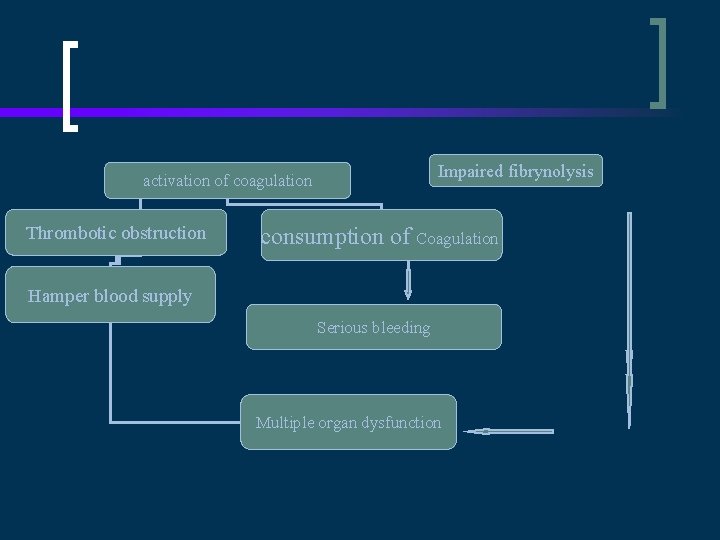
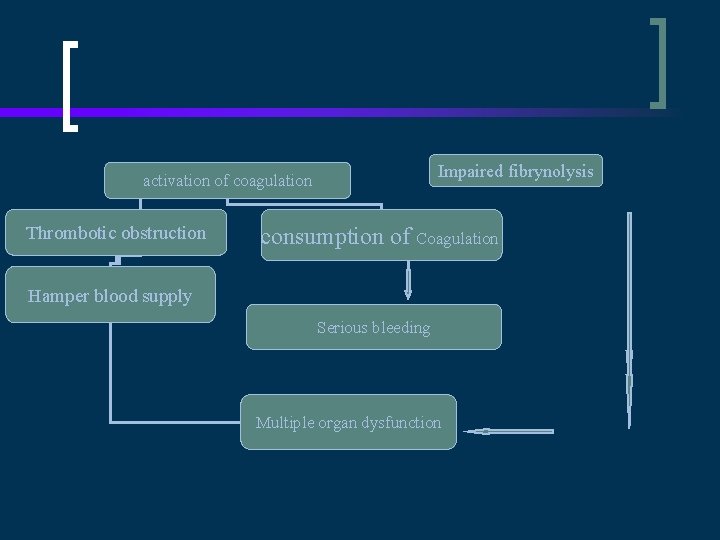
Impaired fibrynolysis activation of coagulation Thrombotic obstruction consumption of Coagulation Hamper blood supply Serious bleeding Multiple organ dysfunction
Non-overt DIC The injury not localized but selflimited no exhaustion of compensatory mechanisms. Cellular, hormonal and enzymatic responses to the injury are operating sufficiently. Haemostatic system is stressed but compensated. n n n

Reasons for such a distinction: Earlier diagnosis. Earlier management. Assess natural history. Management triggering (antibiotics , APC ) Assess treatment response (APC). n n n
DIAGNOSIS OF DIC No single test with accuracy to establish the +/- of DIC. Most lab tests high sens but low sp. Battery of tests. Serial testing. Inevitable delay. n n n
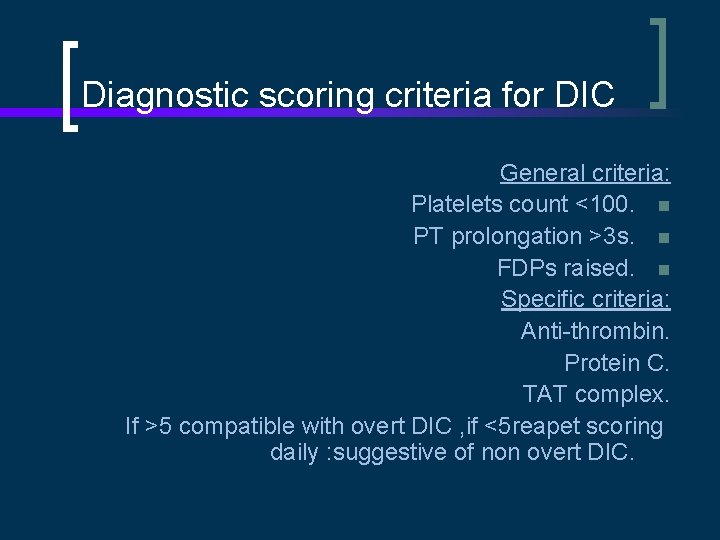
Diagnostic scoring criteria for DIC General criteria: Platelets count <100. n PT prolongation >3 s. n FDPs raised. n Specific criteria: Anti-thrombin. Protein C. TAT complex. If >5 compatible with overt DIC , if <5 reapet scoring daily : suggestive of non overt DIC.
BIOLOGIC MARKERS TO MEASURE NON -OVERT DIC Platelet activation. Endothelial cell perturbation, E-selectin &TM Pro-coagulant activation/inhibition AT & TAT Initiation of fibrinolysis FDPs & D-dimers. Cytokine and receptor: IL-I IL-6, TNF. APC (T-TM). n n n

The gold standard Single. Sensitive. Specific. Simple. Rapid for non-overt DIC. . i. iii. iv. v
Transmittance Waveform (TW) Charting optical changes in light transmittance over the duration of clot formation. The waveform shows an abrupt and rapid decrease in light transmission after the initiation of Ca 2+. The normal TW is a sigmoid shaped. Classify and quantify specific factor deficiencies, presence of heparin. n n ( Downey et al).
Transmittance Waveform in DIC Atypical TW APTT; biphasic waveform (BPW) Gradual decrease in light transmission after the addition of Ca 2+. Early, before conventional biochemical markers. Serially determined of the BPW predict outcome. Downey concluded that the BTW provides, a simple, rapid and robust measurement, appropriate clinical interventions. n n n
APTT BPW Not influenced by analytical variables: Time from venepuncture n Freeze-thawing. n Platelet count. n APTT reagent. n Not associated with medication or n plasma expanders.
BPW & DIC Diagnosis. The BTW preceded other laboratory tests (18 h). Monitor progression from non-overt to overt DIC. Monitoring the early response to therapy. n n
Transmittance Waveform in Non-overt DIC Assessing prognosis: MR 44% Vs 26%. . Sensitivity 97. 6% Specificity 98%. Only detected in DIC. PPV 74%. Direct relationship between the steepness & severity of haemostatic dysfunction, and clinical progression. n n n
The BTW Gradual decrease in light transmission after the addition of Ca 2+. BTW is due to the rapid formation of a precipitate and change in turbidity in re-calcified plasma. The precipitate contained (VLDL) plus (CRP). The Ca 2+-dependent formation of a complex between CRP and VLDL accounts for the BTW. n n
New Modalities In DIC APC concentrate. Heparin. Anti-thrombin concentrates. TFPI. r. NAPc 2. r. IL-10. n n n

APC concentrate Endotoxemia(T-TM). Depression of PC system. Enhance the pro-coagulant state. In sepsis reduce MR. 24 g/kg/h for 96 h. The first intervention shown to be effective in reducing mortality in sepsis. n n n
Anti-thrombin concentrates AT markedly reduced in sepsis. Consumption, degradation , and impaired synthesis. Low levels in sepsis increased mortality. II/III clinical studies. Doses supra-physiological plasma levels No significant reduction in MR in sepsis. • • •
r. NAPc 2: Inhibitor of the ternary complex (TF - VIIa and activated factor X). Derived from nematode anticoagulant proteins. r. IL-10 : abrogate the endotoxininduced affects on coagulation Ø • Ø
Heparin: Experimental studies : partly inhibit the activation of coagulation in sepsis and other causes of DIC. Outcome events never been demonstrated in controlled clinical trials. r. TFPI : Block endotoxin-induced thrombin generation with promising results. Sepsis : modestly reduced, or even increased, concentrations of TFPI. Ø n n Ø • •
Concluding remarks No single test with accuracy to establish the +/- of DIC. Diagnostic scoring criteria for. Downey concluded that the BTW provides, a simple, rapid and robust measurement, appropriate clinical interventions. Not influenced by analytical variables: APC conc The first intervention shown to be effective in reducing mortality in sepsis. n n n
Thanks
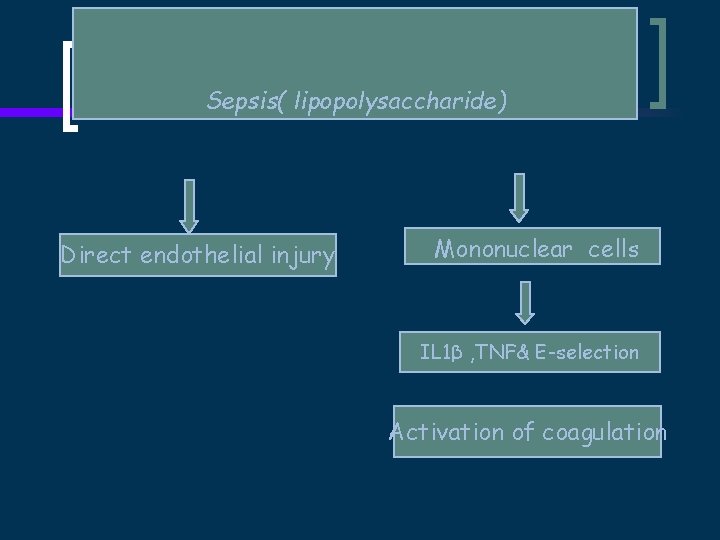
Sepsis( lipopolysaccharide) Direct endothelial injury Mononuclear cells IL 1β , TNF& E-selection Activation of coagulation
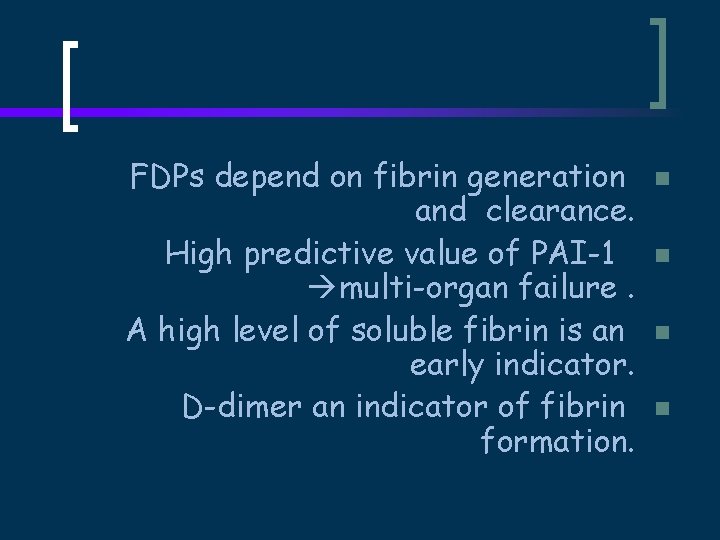
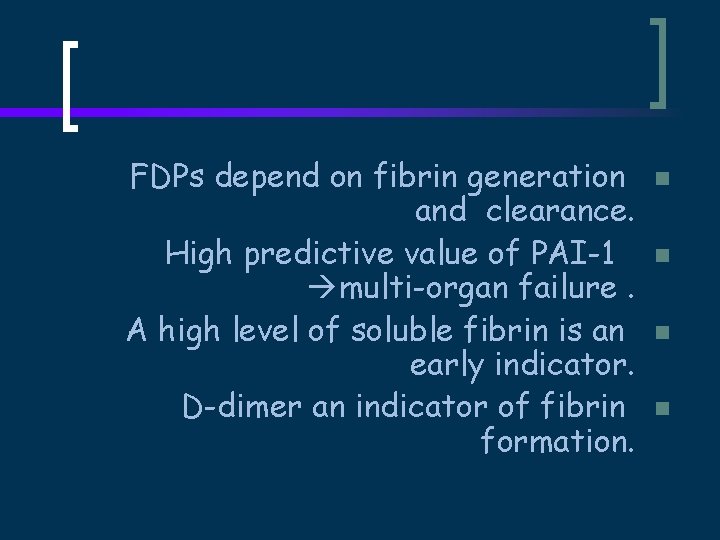
FDPs depend on fibrin generation and clearance. High predictive value of PAI-1 multi-organ failure. A high level of soluble fibrin is an early indicator. D-dimer an indicator of fibrin formation. n n
 Disseminated intravascular coagulation pathophysiology
Disseminated intravascular coagulation pathophysiology Disseminated intravascular coagulation
Disseminated intravascular coagulation Mrcpath
Mrcpath Mrcpath
Mrcpath After a node has prepared an lsp it must be disseminated to
After a node has prepared an lsp it must be disseminated to Tarık zaher
Tarık zaher Planet entegre yatak mobilya a.ş
Planet entegre yatak mobilya a.ş Tarık zaher
Tarık zaher Ibrahim zaher
Ibrahim zaher Chemoprophylaxis
Chemoprophylaxis Farmacodin
Farmacodin Intravascular hemolytic anemia
Intravascular hemolytic anemia Intravascular ultrasound
Intravascular ultrasound Intravascular ultrasound
Intravascular ultrasound Liquido intravascular
Liquido intravascular Espaço intravascular
Espaço intravascular Liquido intravascular
Liquido intravascular Hipernatremia clasificacion
Hipernatremia clasificacion Esquema de liquidos corporales
Esquema de liquidos corporales Protein denaturation definition
Protein denaturation definition Block diagram of diathermy machine
Block diagram of diathermy machine Coagulation time
Coagulation time Coagulation made easy
Coagulation made easy Coagulation profile test
Coagulation profile test Nécrose de coagulation anapath
Nécrose de coagulation anapath Fibronogen
Fibronogen Coagulation factors
Coagulation factors Fat
Fat Composition of eggs
Composition of eggs Coagulation profile test
Coagulation profile test Separation of serum
Separation of serum Zahn line
Zahn line Loading or coagulation
Loading or coagulation Coagulation modifier drugs
Coagulation modifier drugs Bernard soulier syndrome
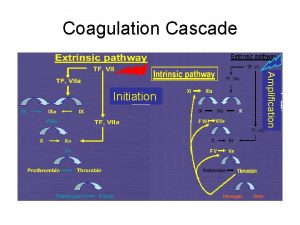
Bernard soulier syndrome Coagulation cascade
Coagulation cascade Hegman factor
Hegman factor Coagulation of blood flow chart
Coagulation of blood flow chart Dnet davidson
Dnet davidson Iso/iec 27001:2005 certification definition
Iso/iec 27001:2005 certification definition Wbtr 2005
Wbtr 2005 Child rights act 2005 images
Child rights act 2005 images Mental capacity act 2005 summary
Mental capacity act 2005 summary 1 de agosto de 2005
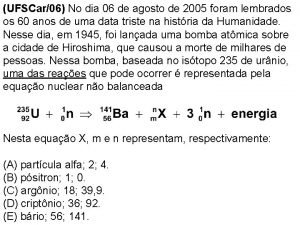
1 de agosto de 2005 Sfs-en 1838
Sfs-en 1838 Idf metabolic syndrome
Idf metabolic syndrome 13 october 2005
13 october 2005 Supplytime 2005
Supplytime 2005 6 stages of counseling process
6 stages of counseling process How to monitor log shipping in sql server 2005
How to monitor log shipping in sql server 2005 Sql server 2005 performance tuning
Sql server 2005 performance tuning