Genital examination findings Its normal to be normal
Genital examination findings – “It’s normal to be normal” but what IS normal? Dr Jo Tully VFPMS Seminar 2017
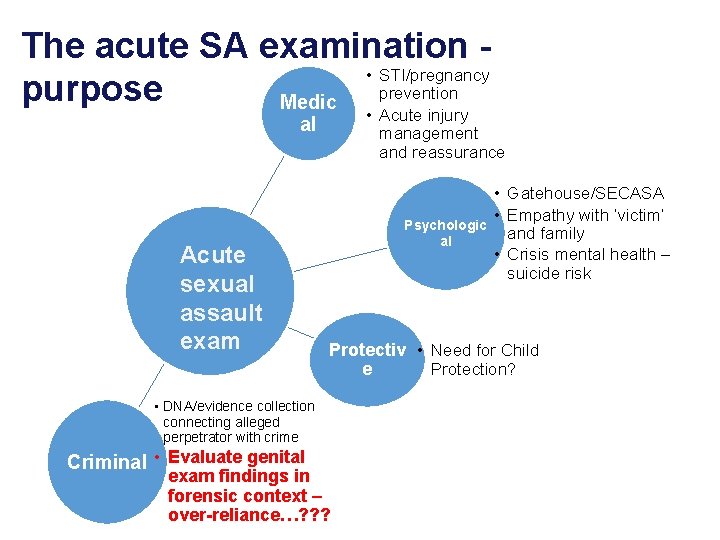
The acute SA examination • STI/pregnancy prevention purpose Medic • Acute injury management and reassurance al Acute sexual assault exam Psychologic al Protectiv • Need for Child Protection? e • DNA/evidence collection connecting alleged perpetrator with crime Criminal • Evaluate genital • Gatehouse/SECASA • Empathy with ‘victim’ and family • Crisis mental health – suicide risk exam findings in forensic context – over-reliance…? ? ?
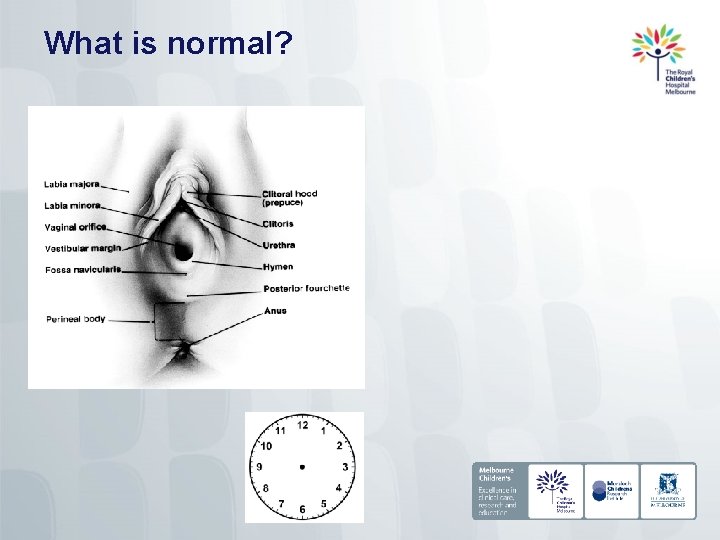
What is normal?
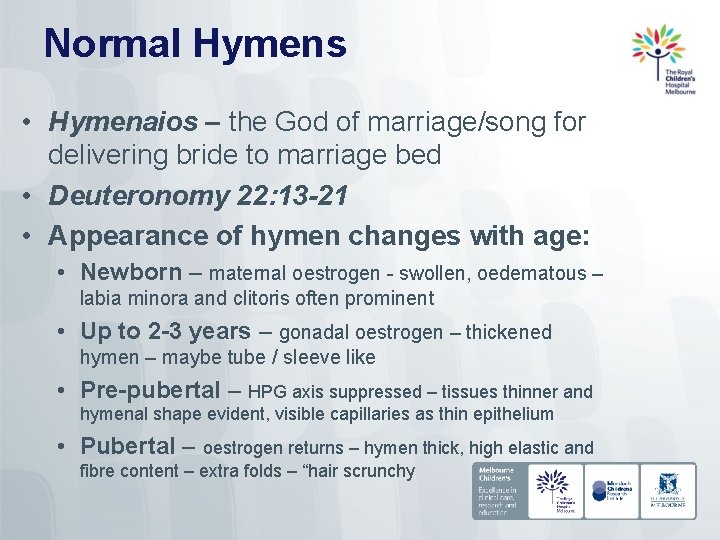
Normal Hymens • Hymenaios – the God of marriage/song for delivering bride to marriage bed • Deuteronomy 22: 13 -21 • Appearance of hymen changes with age: • Newborn – maternal oestrogen - swollen, oedematous – labia minora and clitoris often prominent • Up to 2 -3 years – gonadal oestrogen – thickened hymen – maybe tube / sleeve like • Pre-pubertal – HPG axis suppressed – tissues thinner and hymenal shape evident, visible capillaries as thin epithelium • Pubertal – oestrogen returns – hymen thick, high elastic and fibre content – extra folds – “hair scrunchy
Normal hymens
Normal prepubertal hymen
Normal post-pubertal hymen
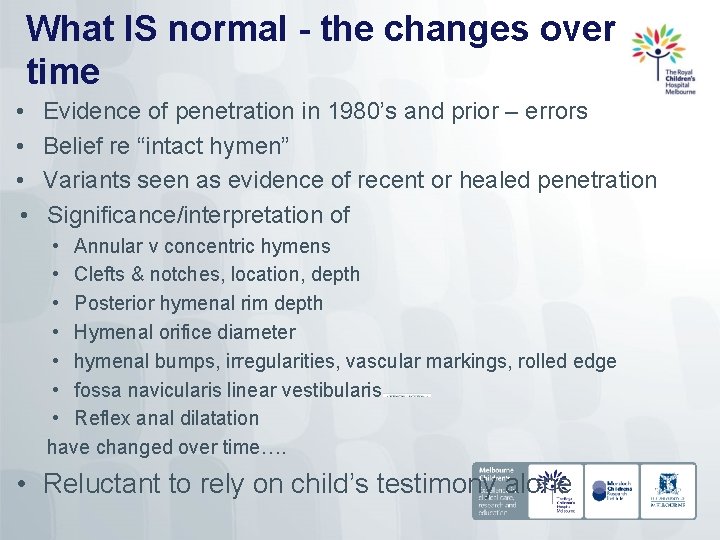
What IS normal - the changes over time • • Evidence of penetration in 1980’s and prior – errors Belief re “intact hymen” Variants seen as evidence of recent or healed penetration Significance/interpretation of • Annular v concentric hymens • Clefts & notches, location, depth • Posterior hymenal rim depth • Hymenal orifice diameter • hymenal bumps, irregularities, vascular markings, rolled edge • fossa navicularis linear vestibularis • Reflex anal dilatation have changed over time…. • Reluctant to rely on child’s testimony alone
Studies defining what is normal • Mc. Cann 1990 placed hymenal exam on scientific footing • Overturned findings previously cited as evidence of CSA • Non-abused pre-pubertal girls; unexpected genital findings are actually normal • Compare non-abused with abused – clarify the sensitivity and specificity • Longitudinal studies of acute injury healing to confirm link between certain acute findings and “healed” appearance • Problems with methodology – including only truly nonabused Appearance of the Hymen in Prepubertal Girls Berenson A, Pediatrics 1992: 89; 387 -394
Findings that remained of concern… • Posterior hymenal clefts/notches • Minimum posterior hymenal depth 1 mm • Hymen orifice diameter • Berenson differentiated deep from superficial clefts/notches • All authors commented on examination position/technique influencing findings
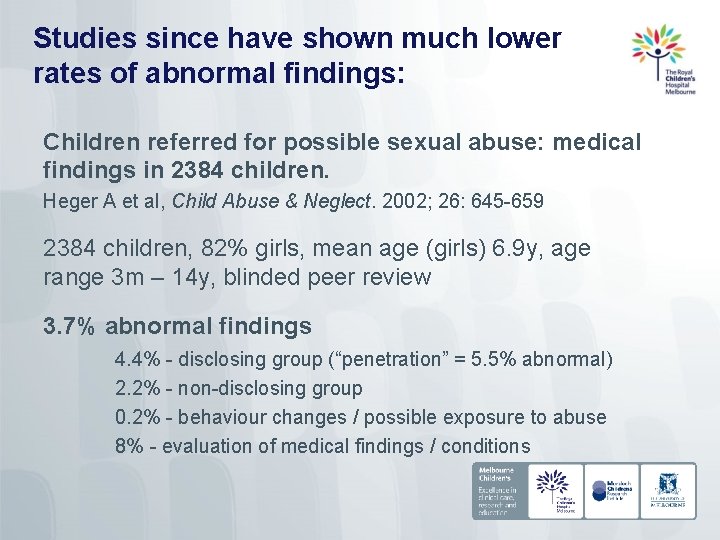
Studies since have shown much lower rates of abnormal findings: Children referred for possible sexual abuse: medical findings in 2384 children. Heger A et al, Child Abuse & Neglect. 2002; 26: 645 -659 2384 children, 82% girls, mean age (girls) 6. 9 y, age range 3 m – 14 y, blinded peer review 3. 7% abnormal findings 4. 4% - disclosing group (“penetration” = 5. 5% abnormal) 2. 2% - non-disclosing group 0. 2% - behaviour changes / possible exposure to abuse 8% - evaluation of medical findings / conditions
What happens when we get it “wrong”? • The Cleveland Enquiry 1989 – Butler-Sloss • Judicial enquiry into 121 children removed from parents care due to concerns re CSA based on RAD (over 2 cm) • Over 90 of the children later returned • Subsequent debate on significance of RAD (and other anal findings) • • Constipation Anaesthetic agents Neuromuscular disease Sexual abuse? Anal signs of child sexual abuse: a case–control study Christopher J Hobbs, Charlotte M Wright BMC Pediatrics 201414: 128

Where are we now? Published in J Paed Adolesc Gynecol 29 (2016)
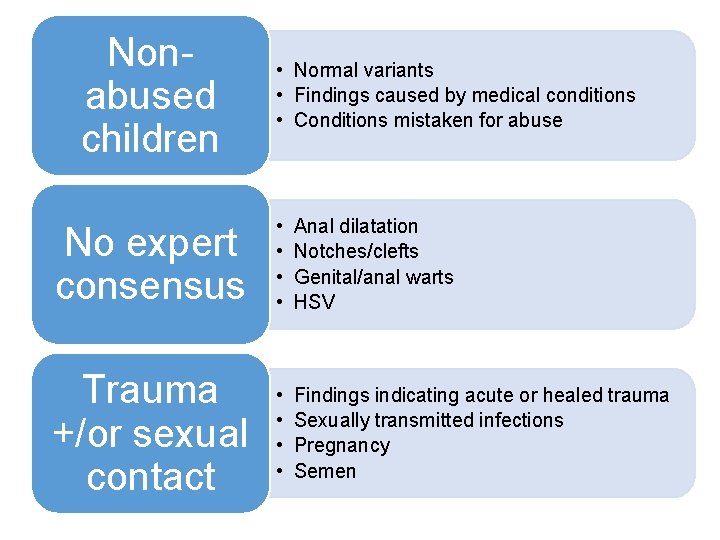
Nonabused children • Normal variants • Findings caused by medical conditions • Conditions mistaken for abuse No expert consensus • • Anal dilatation Notches/clefts Genital/anal warts HSV Trauma +/or sexual contact • • Findings indicating acute or healed trauma Sexually transmitted infections Pregnancy Semen
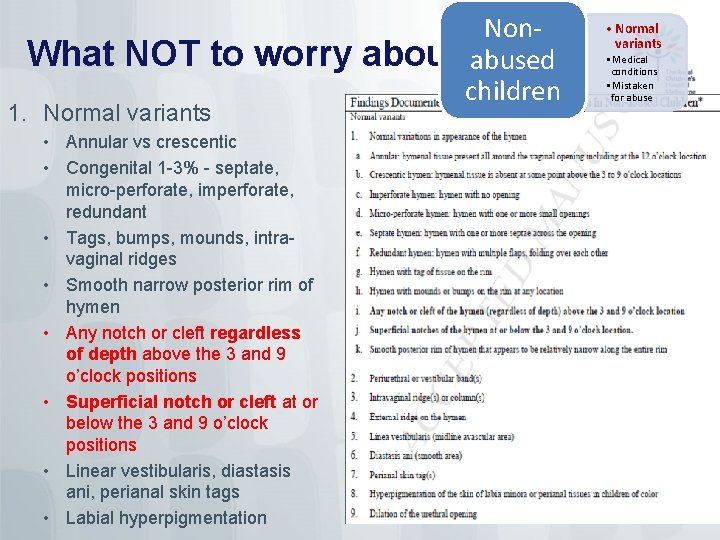
What NOT to worry 1. Normal variants • Annular vs crescentic • Congenital 1 -3% - septate, micro-perforate, imperforate, redundant • Tags, bumps, mounds, intravaginal ridges • Smooth narrow posterior rim of hymen • Any notch or cleft regardless of depth above the 3 and 9 o’clock positions • Superficial notch or cleft at or below the 3 and 9 o’clock positions • Linear vestibularis, diastasis ani, perianal skin tags • Labial hyperpigmentation Nonabout abused children • Normal variants • Medical conditions • Mistaken for abuse
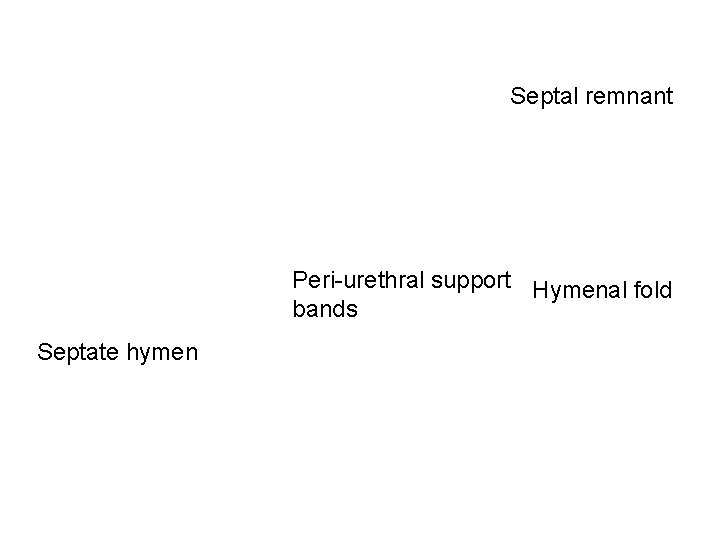
Septal remnant Peri-urethral support Hymenal fold bands Septate hymen
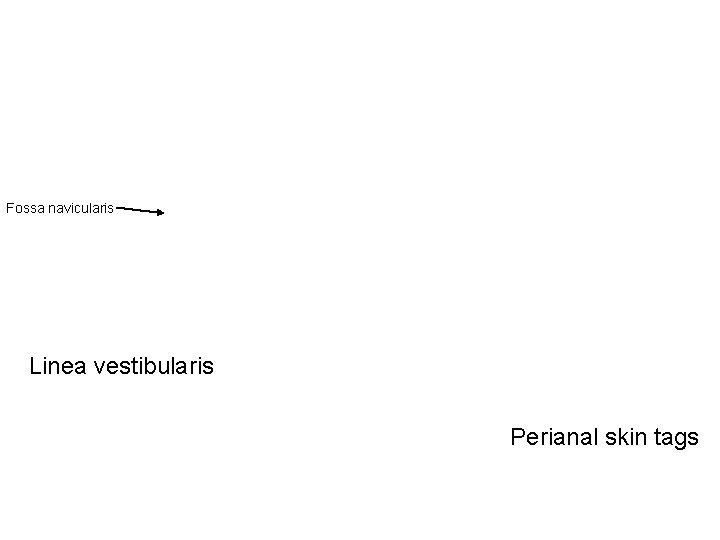
Fossa navicularis Linea vestibularis Perianal skin tags
Clefts, notches, bumps and mounds
Non-abused children 2. Findings commonly caused by conditions other than trauma or sexual contact • • Red vagina Labial adhesions Posterior fourchette friability Vaginal discharge Molluscum Anal ‘fissure’ /laceration Venous congestion perianal area Anal dilatation • • Constipation Sedation/anaesthesia Neuromuscular disease Post-mortem Nonabused children • Normal variants • Medical conditions • Mistaken for abuse
Non-abused children Non- • Normal variants abused • Medical conditions children • Mistaken for abuse 3. Conditions mistaken for abuse • Urethral/rectal prolapse • Lichen sclerosis • Ulcers • Infection (not STI) • Peri-anal creases • Post mortem changes

Conditions mistaken for abuse
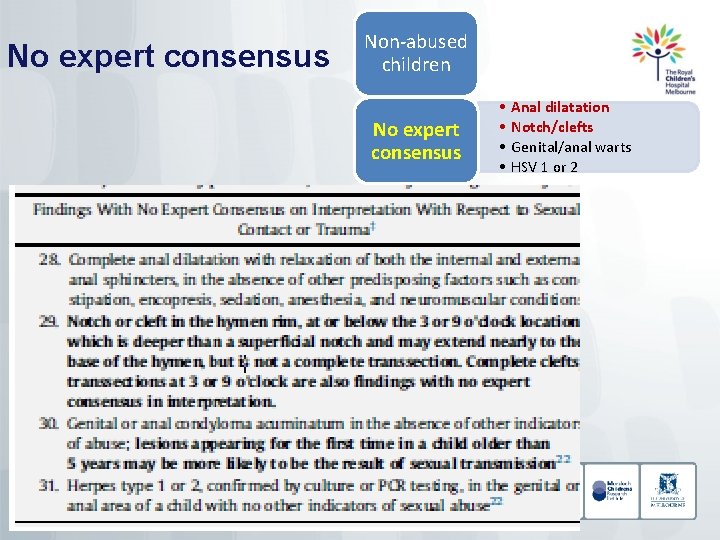
No expert consensus Non-abused children No expert consensus • • Anal dilatation Notch/clefts Genital/anal warts HSV 1 or 2
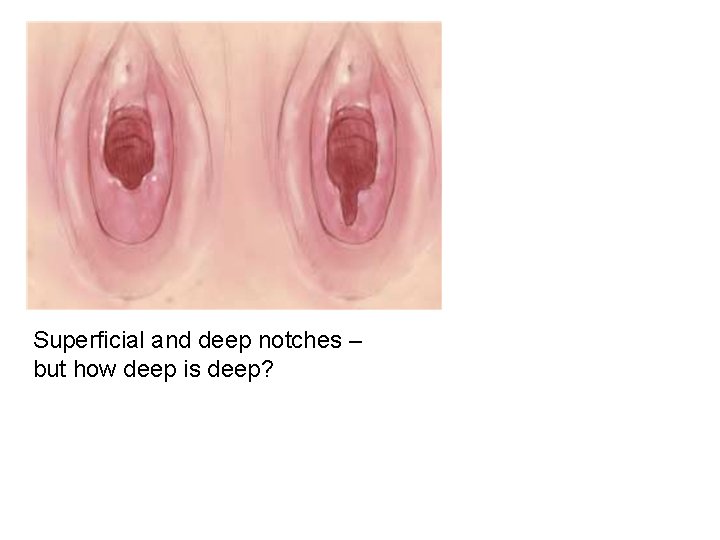
Superficial and deep notches – but how deep is deep?
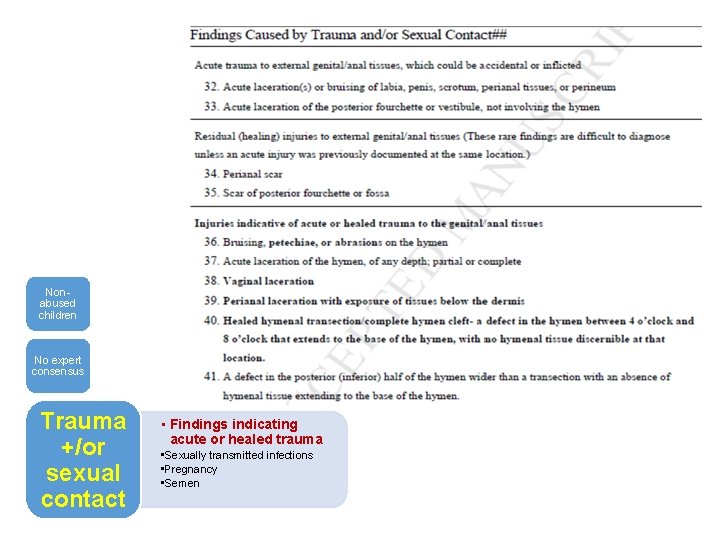
Nonabused children No expert consensus Trauma +/or sexual contact • Findings indicating acute or healed trauma • Sexually transmitted infections • Pregnancy • Semen
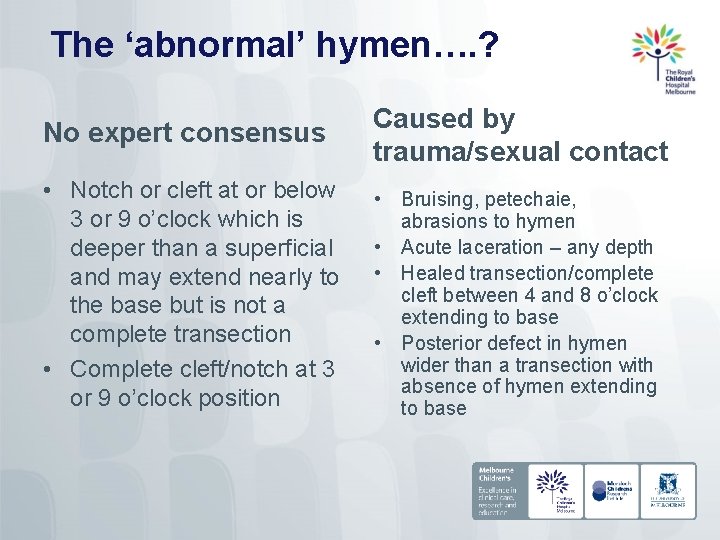
The ‘abnormal’ hymen…. ? No expert consensus Caused by trauma/sexual contact • Notch or cleft at or below 3 or 9 o’clock which is deeper than a superficial and may extend nearly to the base but is not a complete transection • Complete cleft/notch at 3 or 9 o’clock position • Bruising, petechaie, abrasions to hymen • Acute laceration – any depth • Healed transection/complete cleft between 4 and 8 o’clock extending to base • Posterior defect in hymen wider than a transection with absence of hymen extending to base

Genital injuries
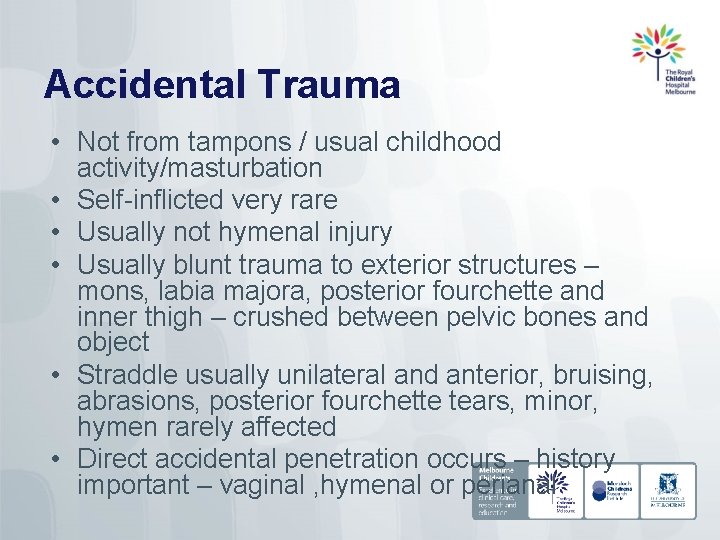
Accidental Trauma • Not from tampons / usual childhood activity/masturbation • Self-inflicted very rare • Usually not hymenal injury • Usually blunt trauma to exterior structures – mons, labia majora, posterior fourchette and inner thigh – crushed between pelvic bones and object • Straddle usually unilateral and anterior, bruising, abrasions, posterior fourchette tears, minor, hymen rarely affected • Direct accidental penetration occurs – history important – vaginal , hymenal or perianal
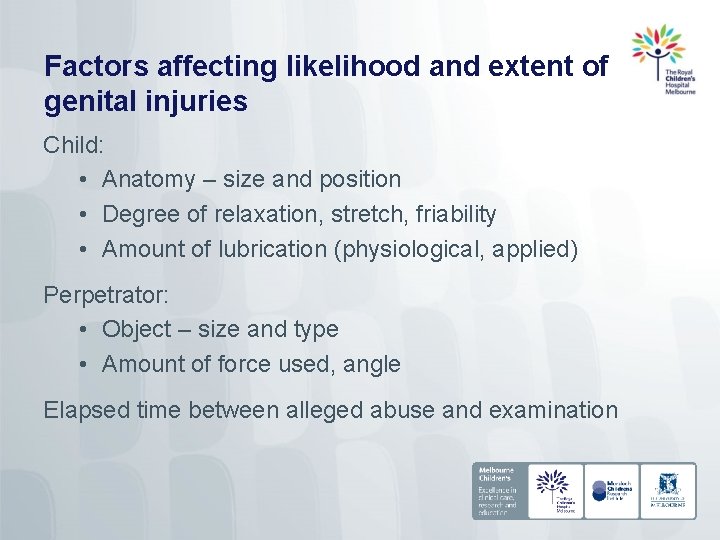
Factors affecting likelihood and extent of genital injuries Child: • Anatomy – size and position • Degree of relaxation, stretch, friability • Amount of lubrication (physiological, applied) Perpetrator: • Object – size and type • Amount of force used, angle Elapsed time between alleged abuse and examination
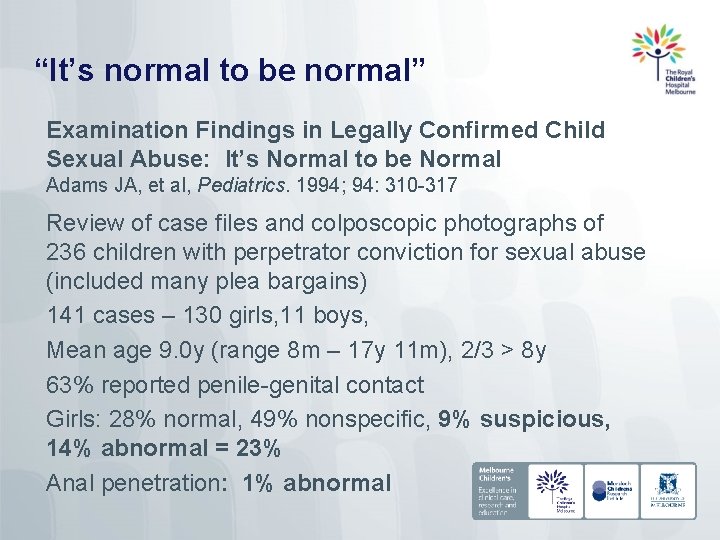
“It’s normal to be normal” Examination Findings in Legally Confirmed Child Sexual Abuse: It’s Normal to be Normal Adams JA, et al, Pediatrics. 1994; 94: 310 -317 Review of case files and colposcopic photographs of 236 children with perpetrator conviction for sexual abuse (included many plea bargains) 141 cases – 130 girls, 11 boys, Mean age 9. 0 y (range 8 m – 17 y 11 m), 2/3 > 8 y 63% reported penile-genital contact Girls: 28% normal, 49% nonspecific, 9% suspicious, 14% abnormal = 23% Anal penetration: 1% abnormal
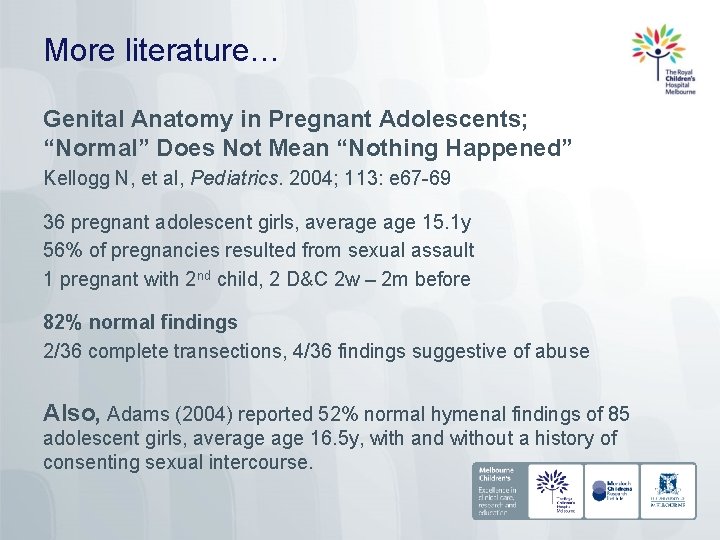
More literature… Genital Anatomy in Pregnant Adolescents; “Normal” Does Not Mean “Nothing Happened” Kellogg N, et al, Pediatrics. 2004; 113: e 67 -69 36 pregnant adolescent girls, average 15. 1 y 56% of pregnancies resulted from sexual assault 1 pregnant with 2 nd child, 2 D&C 2 w – 2 m before 82% normal findings 2/36 complete transections, 4/36 findings suggestive of abuse Also, Adams (2004) reported 52% normal hymenal findings of 85 adolescent girls, average 16. 5 y, with and without a history of consenting sexual intercourse.
So why are there so few abnormal findings? • • Nothing happened History not accurate Absence of injury (likely) Pubertal hymen able to stretch over objects without being injured Minor injury missed Genital mucosal injuries heal quickly Healed injury results in the same findings as the tissue preassault (regeneration vs. repair) Healed injury looks indistinguishable from average, but may be different compared to the tissue pre-assault
Summary of significant findings – take home message Acute hymenal trauma – abrasions, bruises, lacerations Healed hymenal transections extending to base STIs Positive forensic tests Pregnancy Photographic evidence of actual abuse Berkoff (2008) conducted a systematic review of the literature and concluded that, other than a hymenal transection, genital examination findings “cannot independently confirm or exclude non-acute sexual abuse as the cause of genital trauma in prepubertal girls”.

Summary History is the most important aspect Examine ASAP after alleged assault Examine in different positions – “multi-method”: • Supine / labial separation • Supine / labial traction • Prone-knee-chest / gluteal lift Photodocumentation, peer review Injuries unlikely – examination findings often normal Few residual abnormalities after injuries heal – examination findings indistinguishable from normal, except • Transection of posterior hymen clear indicator of past trauma • Jury out on deep clefts “It’s normal to be normal” (2015 AAP Sexual Assault Guidelines)
Conclusions “Medical professionals must take great care to interpret physical findings using research-derived knowledge concerning the variations of normal and the particular conditions that may be mistaken as abuse” “Since a majority of sexual abuse victims have normal genital examinations, a common theme in testimony is the explanation of the findings and that a physical examination alone does not prove or disprove that sexual abuse occurred. ” While interpreting medical findings is an important component of the assessment, “the importance of the child’s history in the diagnosis of sexual abuse cannot be overstated”

Thanks to: Dr Andrea Smith, Paediatrician, VFPMS
- Slides: 36