Noon Report CC Headache Focus differential and evaluation


- Slides: 33
Noon Report CC: Headache Focus: differential and evaluation Natalie Freitas 5/13/2020 Chief facilitator: Shahana Baig-Lewis
HPI: • 43 -year-old previously healthy female physician presenting with headache, nausea, fatigue and difficulty concentrating x 3 days
HPI/ROS: • Headache - describes as 8/10, dull, retro-orbital/frontal, progressive, a/w nausea, no other migrainous symptoms, no prior h/o headaches • Mild neck stiffness, no pain with flexion • Denies vision changes, vertigo, tinnitus, focal neuro deficits, syncope or confusion • Denies abdominal pain, vomiting, diarrhea, polyuria or polydipsia • Denies fever, chills, wt change, SOB, CP, LE swelling • Avid runner, averages 7 -8 mi/day, drinks ~4 L water/day
Past Medical History: Medications: • Remote ASD repair • Chronically irregular periods • H/o fertility treatment • None
Social History: Family History: • Runs daily • Works as MD in primary care • Never smoker • No etoh use • Ashkenazi heritage • Father w/ brain cancer • Maternal and paternal aunt w/ breast cancer
What is your differential diagnosis? What’s most likely? What can’t you miss?
Chief Pause! • Let’s summarize the relevant hx: • Middle age avid runner of Ashkenazi heritage with family hx significant for multiple malignancies • Presenting with • New subacute retro-orbital headache • With associated nausea, fatigue, and confusion • What illness script have we described? • What would you build your ddx on?
Chief Pearls! New onset headache with associated symptoms = secondary headache disorder Secondary headaches can be caused by intracranial or extracranial processes Intracranial causes of secondary headache for this patient would include: vascular, infections, and malignancies Extracranial causes of secondary headache for this patient would include: medications, sinusitis, TMJ disorder, disorders of serum tonicity
Chief Pearls! At this point, a secondary headache disorder is most likely The not miss etiologies would include vascular and malignancy (especially given family hx). Infectious and CSF disorders are less likely. Extracranial etiologies remain on the differential and medication review, exam, and basic laboratory work-up will help differentiate further.
Based on the HPI and history, what do you want to look for on exam? Why?
Chief Pearls! What to Look for on Exam • Review vitals, particularly blood pressure • Complete neuro exam • To assess for focal neuro deficits/signs of elevated intracranial pressure • Additionally would palpate temples, sinuses, assess for TMJ dysfunction, and evaluate for oral lesions

Exam: Vitals: afebrile, HR 70 s, BP 120/70 s, BMI 22 Gen: Well nourished, no distress HEENT: NCAT, MMM, no funduscopic exam performed Neck: supple, no meningismus, no JVD CV: normal RRR, no murmur appreciated Lungs: effort normal, breath sounds normal Abd: soft, NT/ND, normal bowel sounds Ext: WWP, no edema Skin: warm/dry, no rashes, no jaundice, no pallor Neuro: AOx 4, non-focal
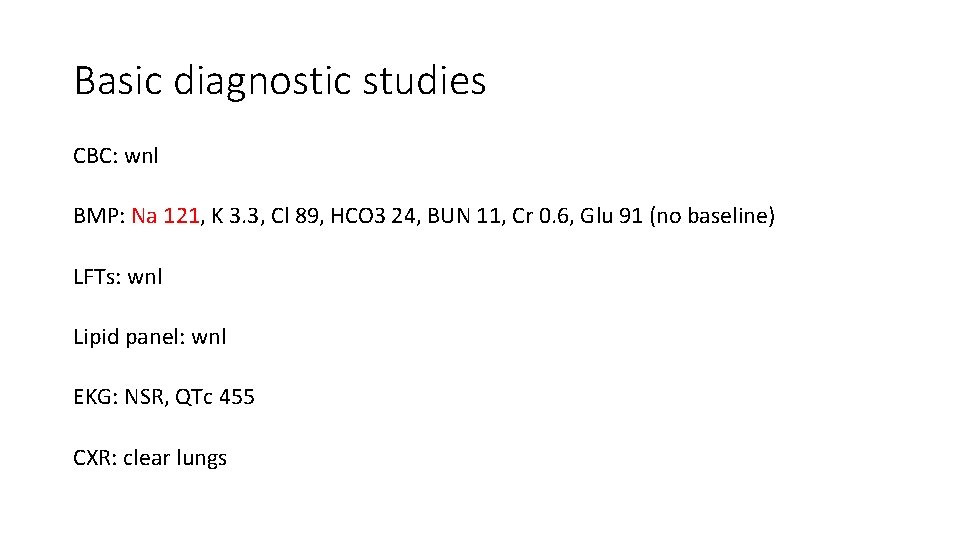
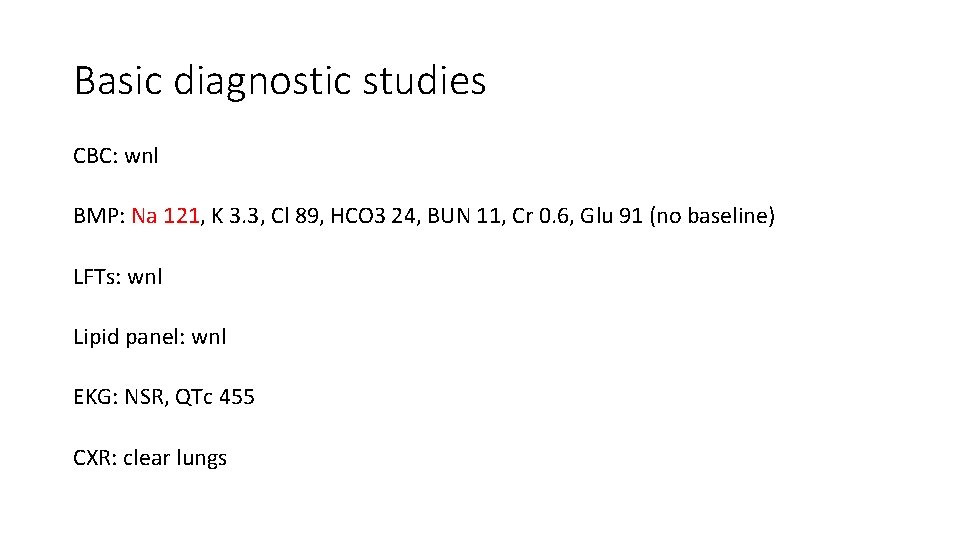
Basic diagnostic studies CBC: wnl BMP: Na 121, K 3. 3, Cl 89, HCO 3 24, BUN 11, Cr 0. 6, Glu 91 (no baseline) LFTs: wnl Lipid panel: wnl EKG: NSR, QTc 455 CXR: clear lungs
How has your differential changed?
Chief Pause! Based on hx, exam and basic laboratory work-up presentation most consistent with: • secondary headache due to extracranial etiology • Of which disorder of serum tonicity/hyponatremia most likely
What’s your summary statement thus far?
Resident’s summary statement: • 43 y previously healthy female presenting with new progressive frontal headache, nausea w/o emesis and lethargy for several days found to be afebrile, hemodynamically stable and euvolemic on exam with labs notable for Na 121 consistent with moderately symptomatic hyponatremia of unclear etiology and duration.
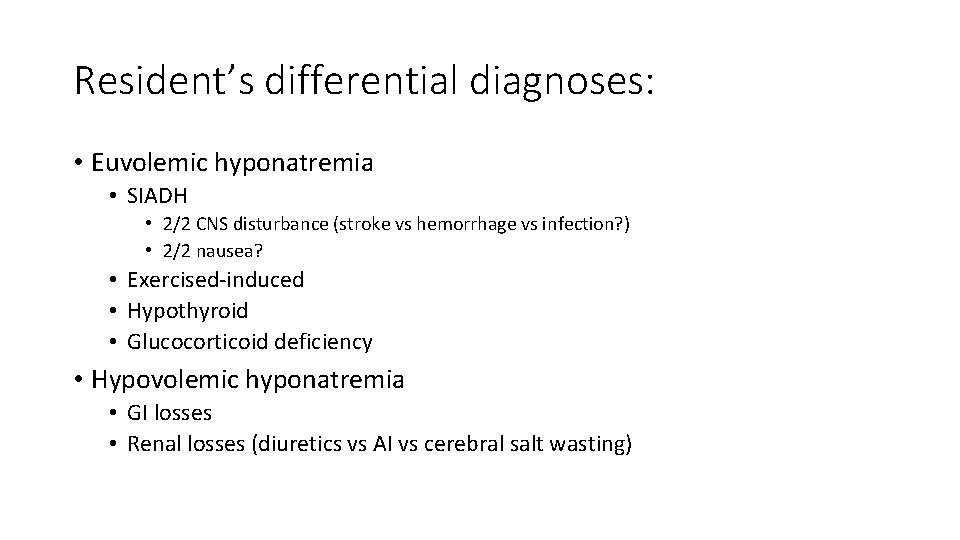
Resident’s differential diagnoses: • Euvolemic hyponatremia • SIADH • 2/2 CNS disturbance (stroke vs hemorrhage vs infection? ) • 2/2 nausea? • Exercised-induced • Hypothyroid • Glucocorticoid deficiency • Hypovolemic hyponatremia • GI losses • Renal losses (diuretics vs AI vs cerebral salt wasting)
Based on your differential, what other studies do you want? Why?
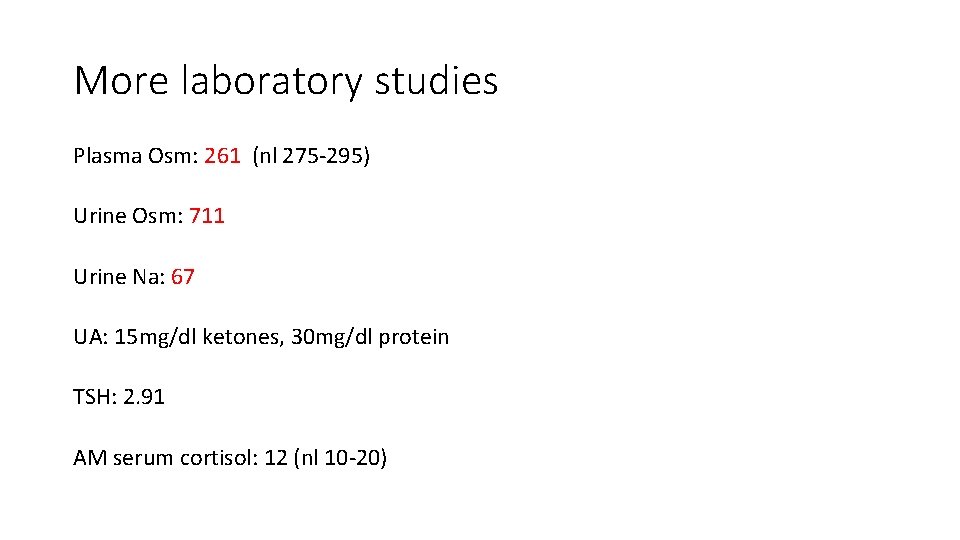
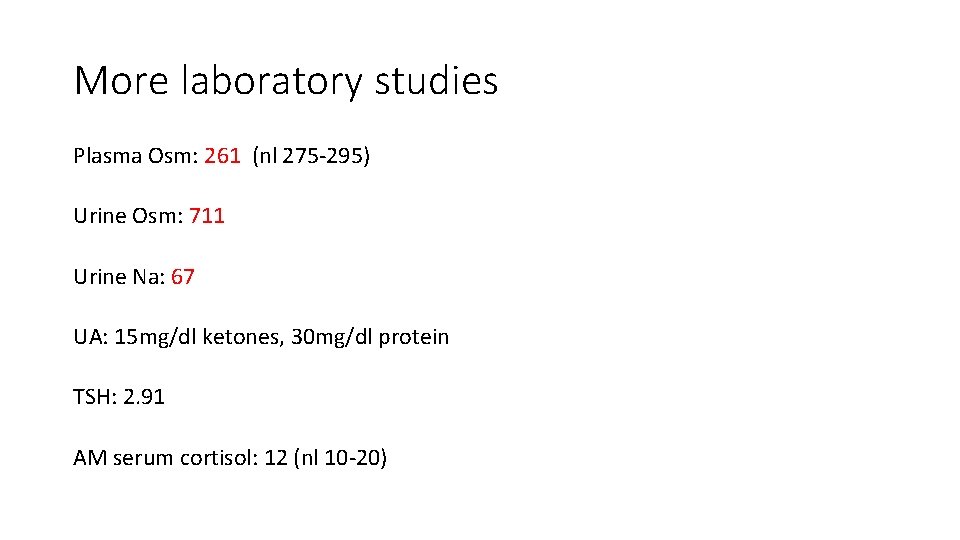
More laboratory studies Plasma Osm: 261 (nl 275 -295) Urine Osm: 711 Urine Na: 67 UA: 15 mg/dl ketones, 30 mg/dl protein TSH: 2. 91 AM serum cortisol: 12 (nl 10 -20)
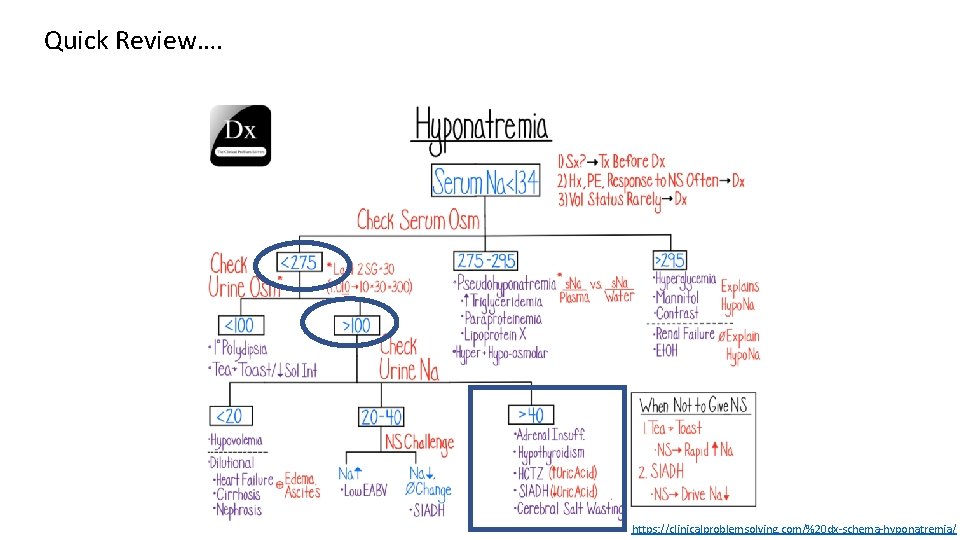
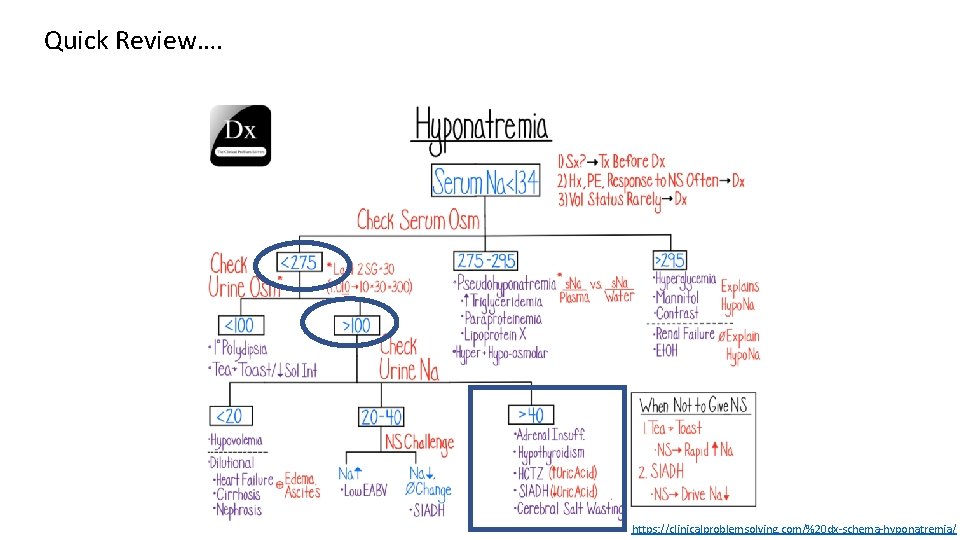
Quick Review…. https: //clinicalproblemsolving. com/%20 dx-schema-hyponatremia/
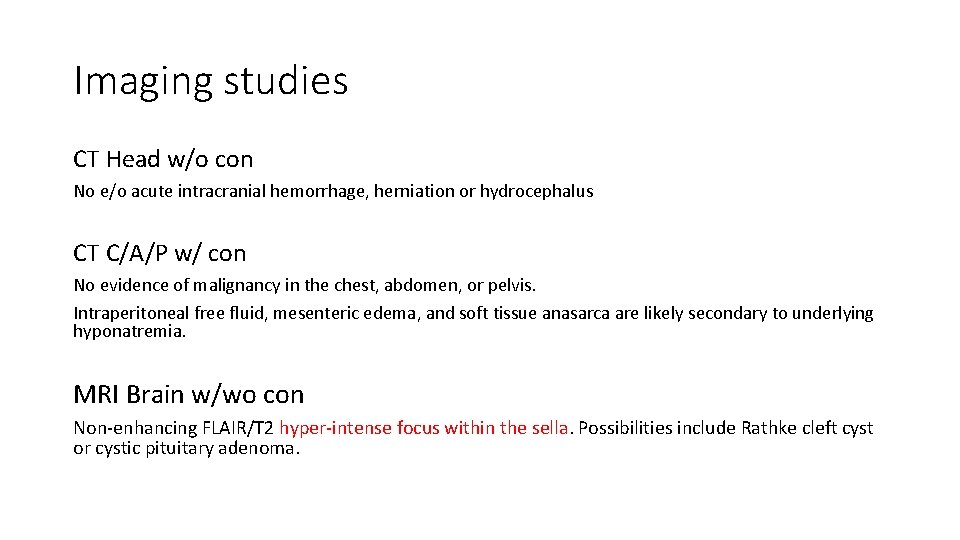
Imaging studies CT Head w/o con No e/o acute intracranial hemorrhage, herniation or hydrocephalus CT C/A/P w/ con No evidence of malignancy in the chest, abdomen, or pelvis. Intraperitoneal free fluid, mesenteric edema, and soft tissue anasarca are likely secondary to underlying hyponatremia. MRI Brain w/wo con Non-enhancing FLAIR/T 2 hyper-intense focus within the sella. Possibilities include Rathke cleft cyst or cystic pituitary adenoma.
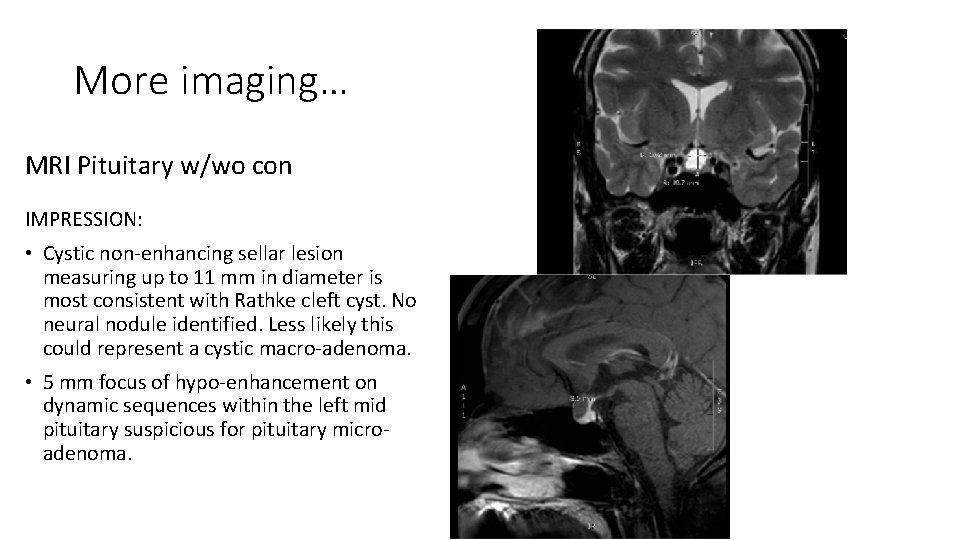
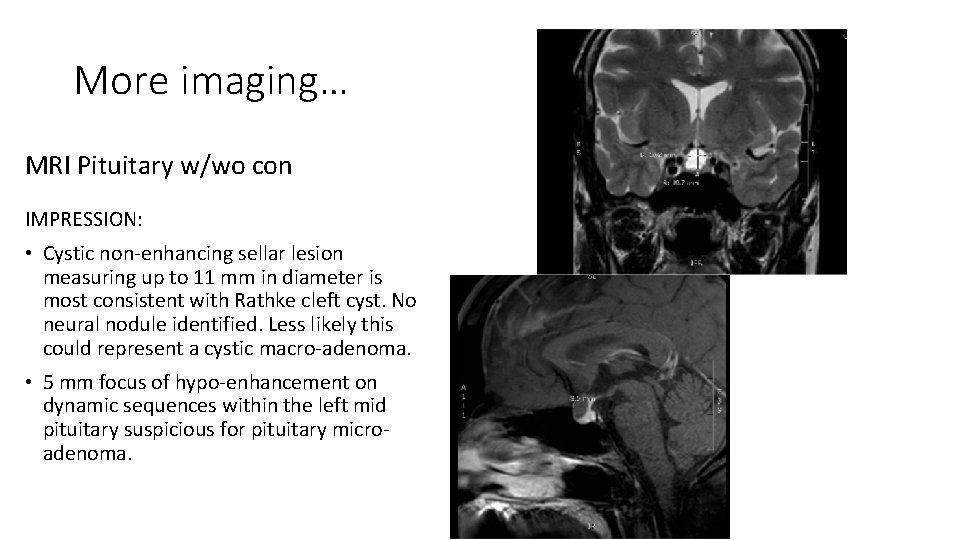
More imaging… MRI Pituitary w/wo con IMPRESSION: • Cystic non-enhancing sellar lesion measuring up to 11 mm in diameter is most consistent with Rathke cleft cyst. No neural nodule identified. Less likely this could represent a cystic macro-adenoma. • 5 mm focus of hypo-enhancement on dynamic sequences within the left mid pituitary suspicious for pituitary microadenoma.
What is your leading diagnosis now? Can we streamline the summary statement more with this data?
Resident’s modified summary statement: • 43 yo previously healthy female presenting with symptomatic hypotonic euvolemic hyponatremia consistent with SIADH found to have pituitary lesion on brain MRI of unclear significance.
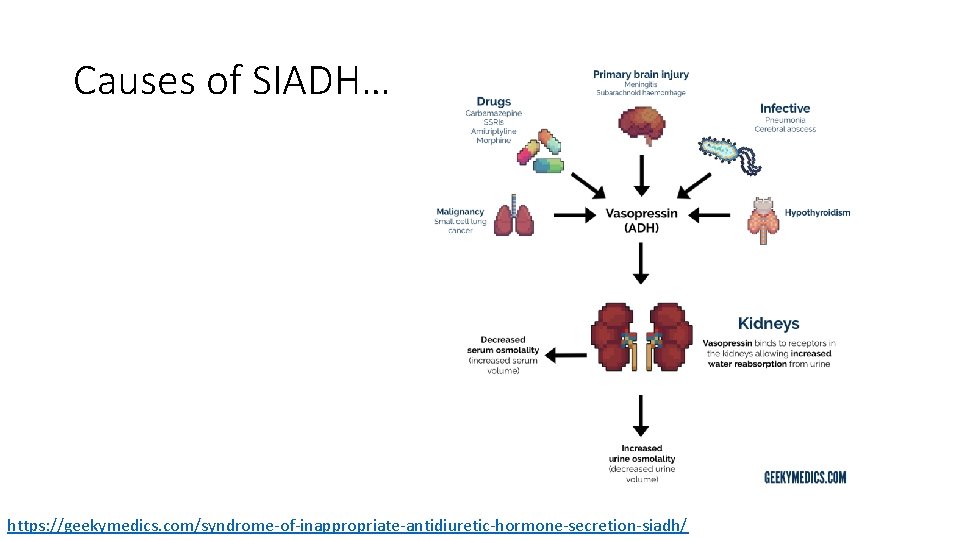
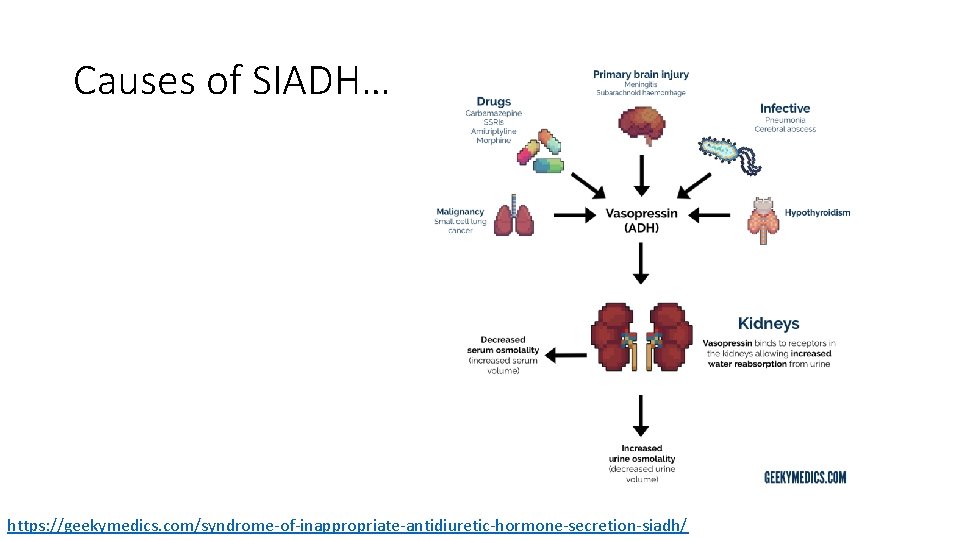
Causes of SIADH… https: //geekymedics. com/syndrome-of-inappropriate-antidiuretic-hormone-secretion-siadh/
Hospital course: • Initially treated in ICU with hypertonic saline, fluid restriction, salt tabs and urea without sustained improvement in Na • Eventually Tolvaptan used with improvement in Na and symptoms • Malignancy work up negative • Endocrine workup revealed normal pit function (Cosyntropin stim test, Prolactin, IGF-1, GH, FSH, LH, TSH) • Most likely etiology thought to be SIADH 2/2 reset osmostat in setting of regular intense exercise
Wait, what about the pituitary lesion? • Neurosurgery and neuroendocrine consulted -recommended against surgery at that time due to concerns could worsen hyponatremia • Ophthalmology consulted - no visual field defects noted
Follow up. . . • Outpatient repeat imaging showed stable lesion • However, pt later developed diabetes insipidus concerning for craniopharyngioma • Underwent endoscopic endonasal transphenoidal resection • However, path report showed normal pituitary tissue
Could the pituitary lesion have contributed to hyponatremia? • Hypopituitarism is known to cause hyponatremia mainly by vasopressindependent mechanisms related to hypothyroidism or secondary adrenal insufficiency; however, our pt had normal pit function • Few case reports of pituitary tumors causing SIADH with normal pit function where pituitary stalk compression leads to excessive or inappropriate secretion of ADH[1] • This local mechanical stress causing SIADH is less common and seems less likely in our pt whose Na stabilized prior to surgical intervention • More commonly mass effect of local tumors in pituitary region cause hormone deficiencies and decreased ADH as seen with craniopharyngiomas causing DI
Resident Teaching Points • Hyponatremia is common and a systematic approach is needed to identify underlying cause • Volume status, serum osm, urine osm and urine sodium are good places to start • SIADH should be suspected in hypotonic euvolemic hyponatremia with urine osm > 100 mosmol/kg and urine Na concentration is usually > 40 m. Eq/L • Common causes of SIADH include CNS disturbances, malignancy, pulmonary disease, drugs (AEDs, SSRIs) and hormone deficiencies (AI, hypothyroidism) • Pituitary adenomas may be less common cause of SIADH with few cases reported [2]

Resident Teaching Points (cont) • Reset osmostat is a subset of SIADH where ADH is secreted at a lower serum osomotic threshold • Etiology largely unknown although non-osmotic triggers for ADH secretion including intense exercise and non-specific stresses such as pain have been implicated • Resulting hyponatremia is usually chronic, mild to moderate and asymptomatic • Usually not amenable to fluid restriction, salt or urea supplementation or diuretics • Reset osmostat, excessive fluid intake, and sweat sodium loss are all thought to be cause of exercise-associated hyponatremia
References 1. Dilrukshi MDSA, Sandakumari GVN, Abeysundara PK, Chang T. Craniopharyngioma presenting with severe hyponatremia, hyponatremia-induced myopathy, and panhypopituitarism: a case report. Journal of Medical Case Reports. 2017; 11(1). doi: 10. 1186/s 13256 -017 -1210 -x. 2. Zogheri A, Mambro AD, Mannelli M, Serio M, Forti G, Peri A. Hyponatremia and pituitary adenoma: Think twice about the etiopathogenesis. Journal of Endocrinological Investigation. 2006; 29(8): 750 -753. doi: 10. 1007/bf 03344188. 3. Dx Schema – Hyponatremia. The Clinical Problem Solvers. https: //clinicalproblemsolving. com/ dx-schema-hyponatremia/. Published March 6, 2020. Accessed May 6, 2020. 4. Potter L, Black Z. SIADH. Geeky Medics. https: //geekymedics. com/syndrome-of-inappropriate-antidiuretic-hormone-secretionsiadh/. Published April 19, 2020. Accessed May 6, 2020. 5. Up. To. Date. https: //www. uptodate. com/contents/exercise-associated-hyponatremia? search=exercise associated hyponatremia emergency&source=search_result&selected. Title=1~19&usage_type=default&display_rank=1#H 9. Accessed May 6, 2020. 6. Up. To. Date. https: //www. uptodate. com/contents/pathophysiology-and-etiology-of-the-syndrome-of-inappropriate-antidiuretic -hormone-secretion-siadh? section. Name=Patterns of ADH secretion&search=reset osmostat&topic. Ref=2357&anchor=H 4&source=see_link#H 4. Accessed May 6, 2020. 7. Up. To. Date. https: //www. uptodate. com/contents/diagnostic-evaluation-of-adults-withhyponatremia? search=hyponatremia&source=search_result&selected. Title=2~150&usage_type=default&display_rank=2. Accessed May 6, 2020.