Noon Report CC Proteinuria Focus Diagnostic evaluation Cameron
- Slides: 32
Noon Report CC: Proteinuria Focus: Diagnostic evaluation Cameron Johnstone Chief facilitator: Kimberly Chesteen
BEFORE YOU GO! When you’re done, please take a moment to list ONE take away point from this case on the comments section for this blog post. It’s a small way for us to stay connected and hear each other’s thoughts with virtual reports. Thank you!
HPI: The setting is primary care clinic • 43 yo male healthy male here for an urgent care appointment after calling in earlier in the day about right flank pain • Acute onset, moderate intensity R flank pain 1 week prior • He also had a small episode of brown emesis and nausea at the time, this has since resolved • Describes the pain as “sore and achy”, about 6/10 now improved to 3/10 with massage treatments and rest • He cannot remember an inciting event or injury, but has been sitting uncomfortably in chair at work – perhaps aggravated a muscle
HPI/ROS: • He has not experienced any fevers or chills, dysuria or hematuria • He doesn’t have a history of kidney stones, chronic kidney disease, structural kidney abnormalities • He hasn’t performed any strenuous exercise recently and has been wellhydrated • He has also two episodes of headache and nausea and emesis in the last week. These have been occurring over 10 years with variable response to sumatriptan abortive treatment. • Otherwise he has been feeling well aside from issues with chronic anxiety and stress. • A comprehensive ROS is otherwise unremarkable
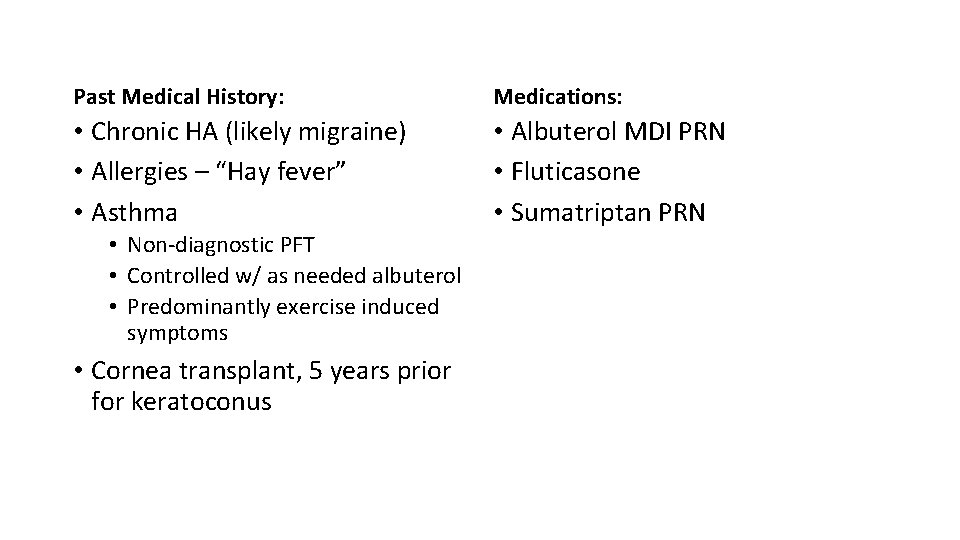
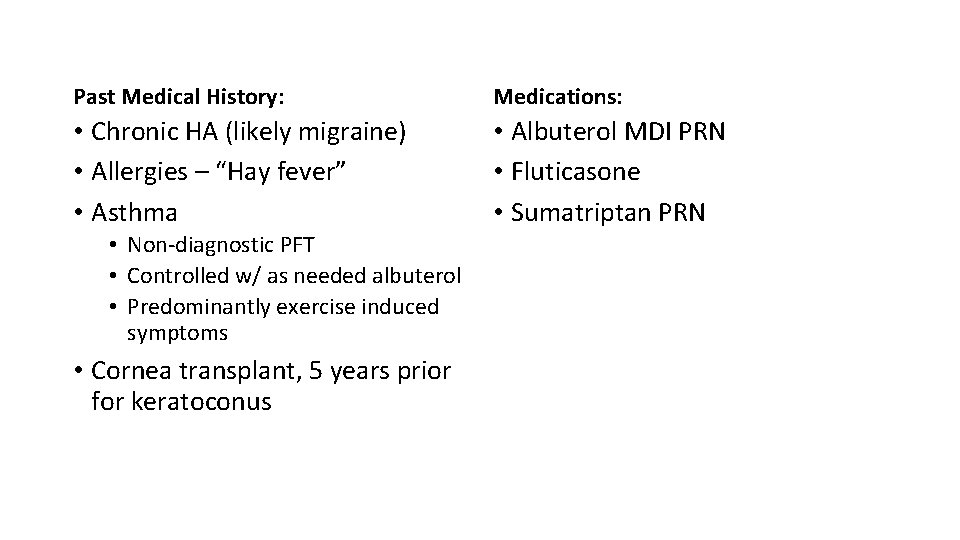
Past Medical History: Medications: • Chronic HA (likely migraine) • Allergies – “Hay fever” • Asthma • Albuterol MDI PRN • Fluticasone • Sumatriptan PRN • Non-diagnostic PFT • Controlled w/ as needed albuterol • Predominantly exercise induced symptoms • Cornea transplant, 5 years prior for keratoconus
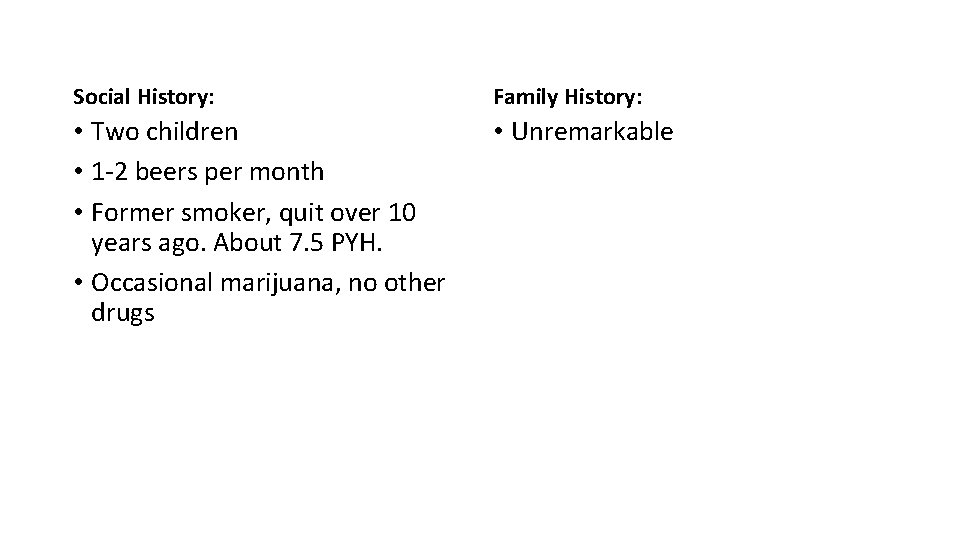
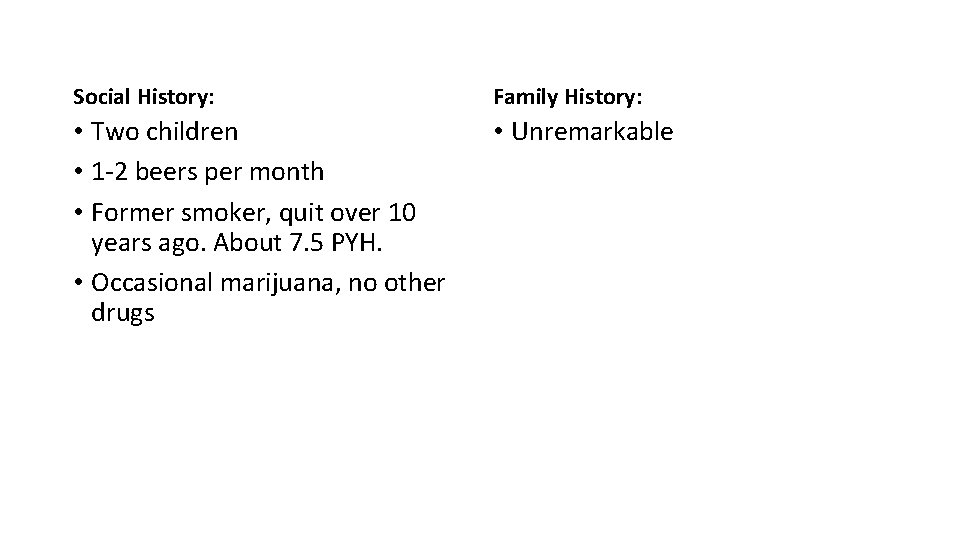
Social History: Family History: • Two children • 1 -2 beers per month • Former smoker, quit over 10 years ago. About 7. 5 PYH. • Occasional marijuana, no other drugs • Unremarkable
Based off of the history thus far, the chief complaint appears to be “flank pain. ” Associated symptoms include nausea and vomiting. Also with chronic headache symptoms.
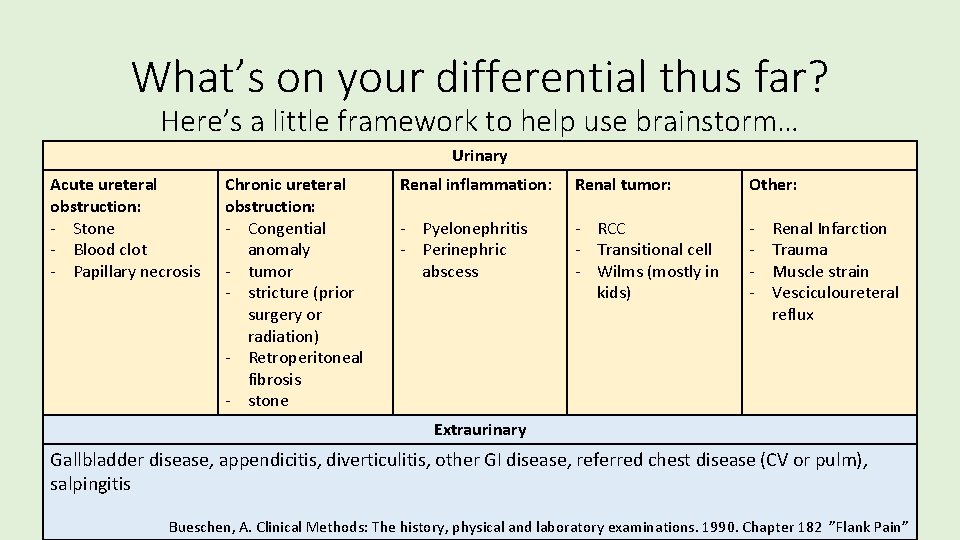
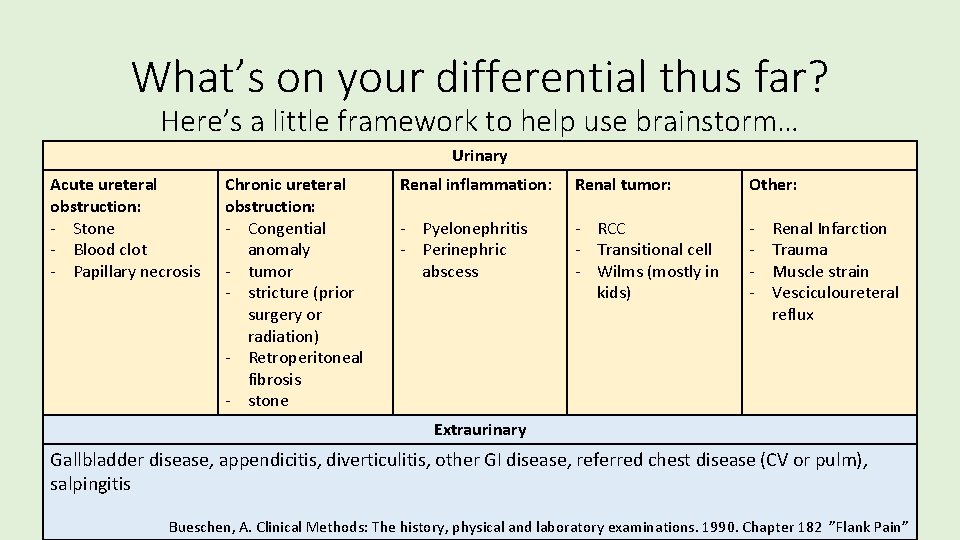
What’s on your differential thus far? Here’s a little framework to help use brainstorm… Urinary Acute ureteral obstruction: - Stone - Blood clot - Papillary necrosis Chronic ureteral obstruction: - Congential anomaly - tumor - stricture (prior surgery or radiation) - Retroperitoneal fibrosis - stone Renal inflammation: Renal tumor: Other: - Pyelonephritis - Perinephric abscess - RCC - Transitional cell - Wilms (mostly in kids) - Renal Infarction Trauma Muscle strain Vesciculoureteral reflux Extraurinary Gallbladder disease, appendicitis, diverticulitis, other GI disease, referred chest disease (CV or pulm), salpingitis Bueschen, A. Clinical Methods: The history, physical and laboratory examinations. 1990. Chapter 182 ”Flank Pain”
Based on the this presentation and history and our current differential, what do you want to look for on exam? Why?
Exam: Vitals: Temp 97, HR 68, BP 155/81, RR 18 Gen: middle age man resting comfortably, NAD Neck: no JVP elevation noted CV: Regular rate and rhythm, no murmurs rubs or gallops Lungs: Clear to auscultation bilaterally Abd: soft, not tender or distended Back: no tenderness to palpation or percussion of the right flank MSK: tenderness to palpation at the R paraspinal muscle/R oblique, pain w/ core active ROM Ext: Trace edema to ankles b/l Skin: No visible rashes, abrasions or jaundice Neuro: AOX 4, normal gait
Labs • Based the history and exam, the evaluating physician was concerned primarily for musculoskeletal pain and prescribed supportive therapy • However, to evaluate for possible nephrolithiasis or urinary tract infection, an outpatient urinalysis was also obtained • A few days later the following results appeared in inbox for evaluation
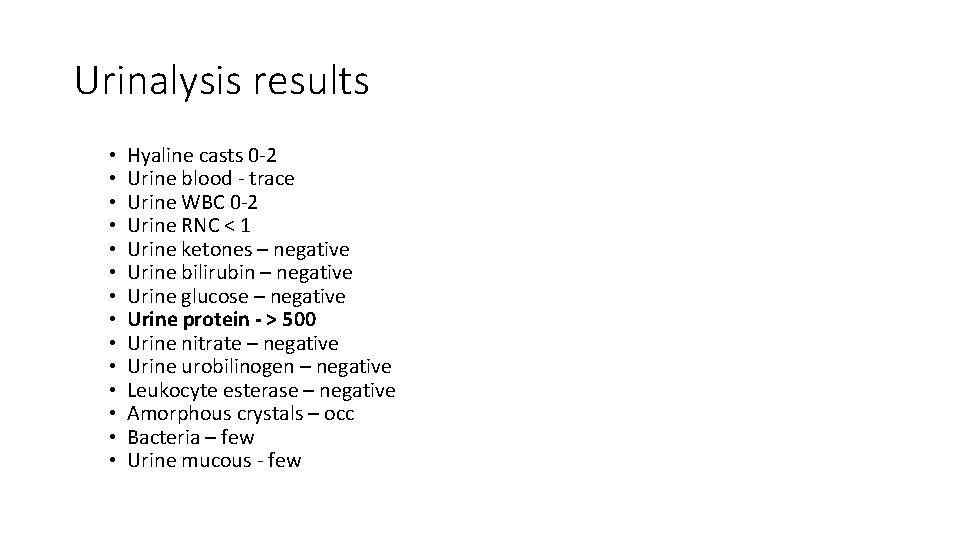
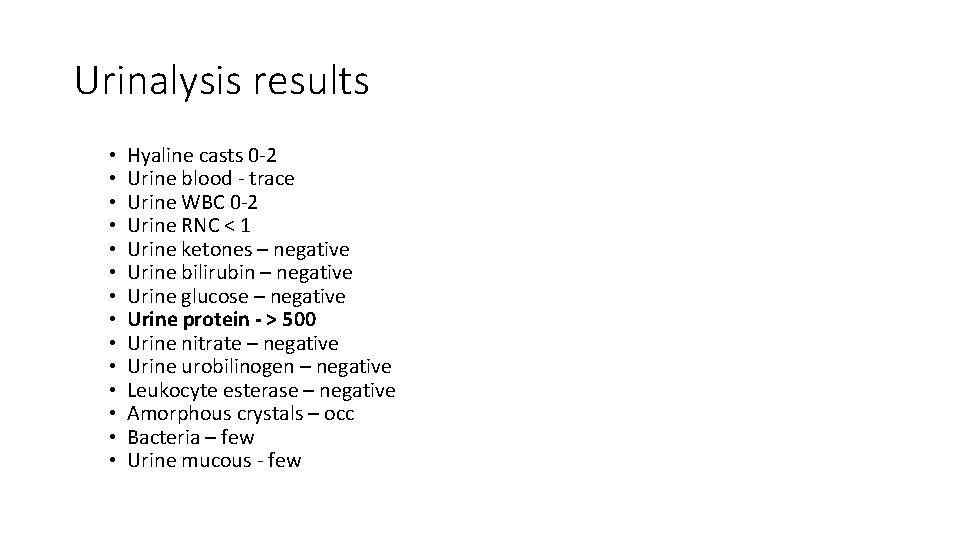
Urinalysis results • • • • Hyaline casts 0 -2 Urine blood - trace Urine WBC 0 -2 Urine RNC < 1 Urine ketones – negative Urine bilirubin – negative Urine glucose – negative Urine protein - > 500 Urine nitrate – negative Urine urobilinogen – negative Leukocyte esterase – negative Amorphous crystals – occ Bacteria – few Urine mucous - few
How would you describe the UA results? Are you surprised by the results? Does this explain his flank pain? Chief thought: For stones would expect blood on UA, and for pyelonephritis would expect WBCs, LE, nitrites. Proteinuria does not usually cause flank pain (and was not in our original differential)
What disease processes come to mind? How would you reframe this problem and proceed with further evaluation?
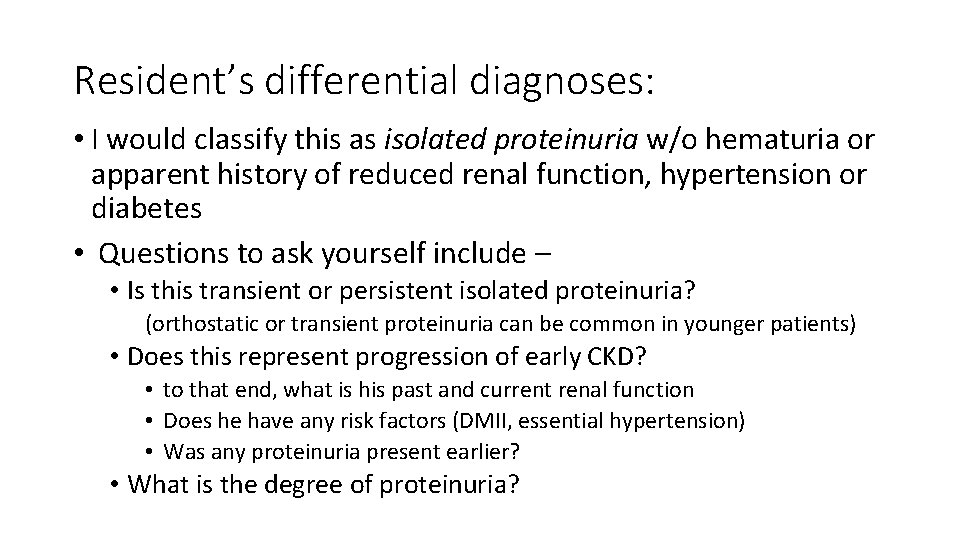
Resident’s differential diagnoses: • I would classify this as isolated proteinuria w/o hematuria or apparent history of reduced renal function, hypertension or diabetes • Questions to ask yourself include – • Is this transient or persistent isolated proteinuria? (orthostatic or transient proteinuria can be common in younger patients) • Does this represent progression of early CKD? • to that end, what is his past and current renal function • Does he have any risk factors (DMII, essential hypertension) • Was any proteinuria present earlier? • What is the degree of proteinuria?
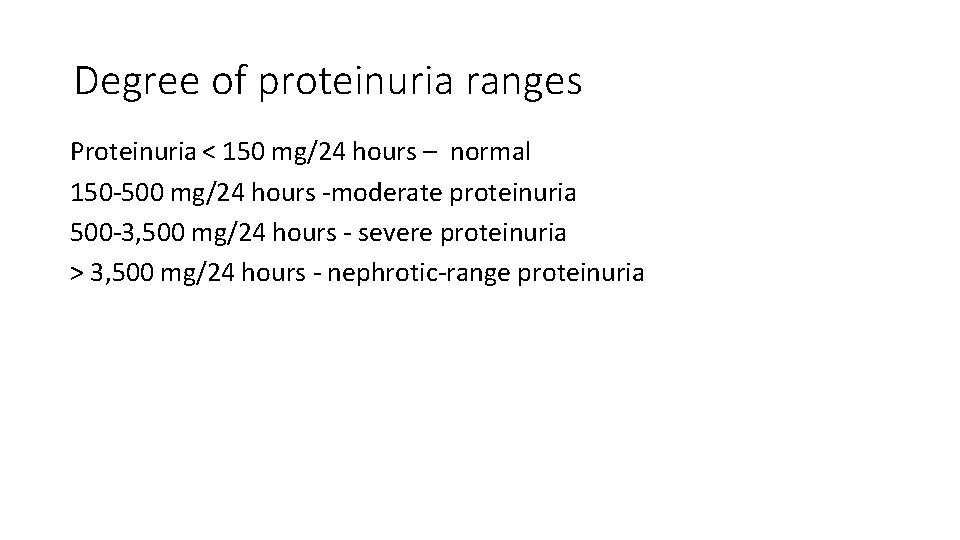
Degree of proteinuria ranges Proteinuria < 150 mg/24 hours – normal 150 -500 mg/24 hours -moderate proteinuria 500 -3, 500 mg/24 hours - severe proteinuria > 3, 500 mg/24 hours - nephrotic-range proteinuria
Further lab results Repeat UA – essentially the same (500+ protein, otherwise normal) BMP – Na 142, K 4. 0, Cl 106, CO 2 25, BUN 9, Cr 0. 9, Glucose 86, e. GFR 93 Total protein (urine) - +600, creatinine 144 This translates to a protein/creatinine ratio of > 4167 mg/g or estimated 24 urine protein excretion > 4. 2 g per day • On further review of records he has no evidence of diabetes or hypertension and normal renal function dating back over several years of records • However, he has had isolated proteinuria on UA over the last 3 years (previously 300+). • •
What’s your summary statement thus far? What is this patient’s primary problem?
Resident’s summary statement: 43 yo previously healthy man presenting with 1 week of moderate R flank pain found to have (? chronic) isolated nephrotic range proteinuria. Does this patient have nephrotic syndrome? What is the diagnostic criteria for nephrotic syndrome? Diagnostic criteria include: - nephrotic range proteinuria > 3, 500 mg/24 hours - clinical evidence of peripheral edema - serum albumin < 2. 5 g - hyperlipidemia (total cholesterol often > 300)
Further diagnostic studies CBC: WBC 10, Hg 16. 1, MCV 85, Plts 246 LFTs: Albumin 3. 1, otherwise normal Total cholesterol – 325 Urine sediment – no casts, dysmorphic RBC or WBC Renal US – “Unremarkable sonographic exam of the kidneys without evidence of nephrolithiasis or obstructive uropathy”
Nephrotic syndrome Based on these results, the patient appears to have nephrotic syndrome (nephrotic range proteinuria, peripheral edema, hypercholesteremia, and albumin which later dropped in range in the next several weeks). This raises the question of cause in an adult w/o other apparent symptoms. One useful framework is primary vs. secondary causes with history, physical and lab testing used to rule out secondary cause before obtaining kidney biopsy.
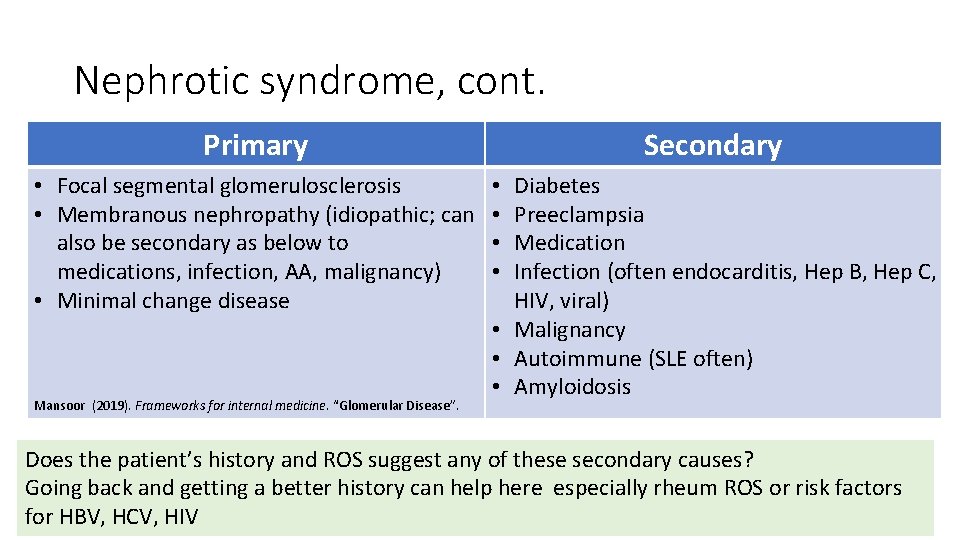
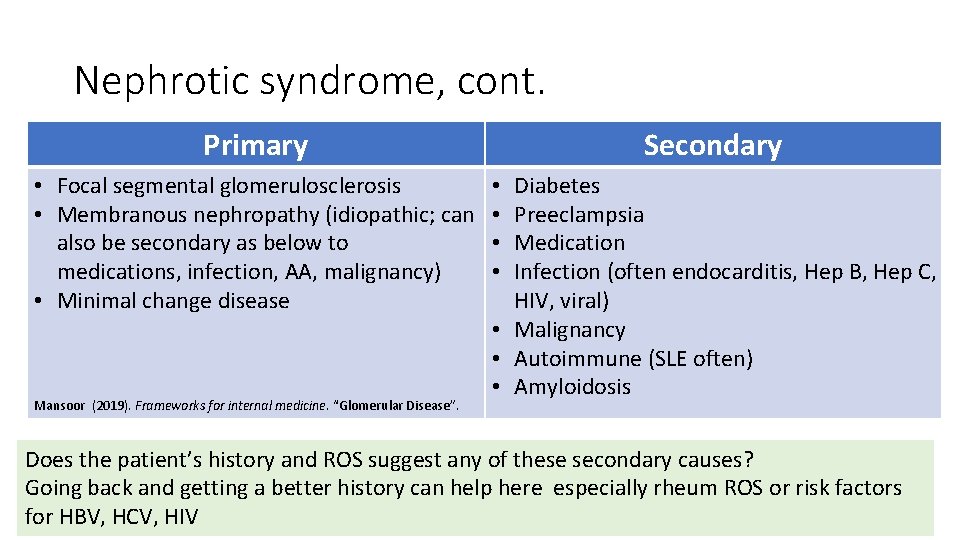
Nephrotic syndrome, cont. Primary • Focal segmental glomerulosclerosis • Membranous nephropathy (idiopathic; can also be secondary as below to medications, infection, AA, malignancy) • Minimal change disease Mansoor (2019). Frameworks for internal medicine. “Glomerular Disease”. Secondary Diabetes Preeclampsia Medication Infection (often endocarditis, Hep B, Hep C, HIV, viral) • Malignancy • Autoimmune (SLE often) • Amyloidosis • • Does the patient’s history and ROS suggest any of these secondary causes? Going back and getting a better history can help here especially rheum ROS or risk factors for HBV, HCV, HIV
What medications can cause nephrotic syndrome? NSAIDS Interferon Bisphonates Lithium Gold Penacillamine
Based on our framework for primary vs. secondary nephrotic syndrome, what studies would you get now? (click back to slide 20 if needed to build a diagnostic work up before proceeding forward)
Nephrotic syndrome, cont. The patient was referred to nephrology and completed an extensive evaluation including – HBV, HCV, HIV - negative SPEP w/o M-spike, UPEP normal as well ANA negative (<1: 80), C 3/C 4 normal No exposure to suspicious medications (NSAIDs, penicillamine) Kappa/lambda light chains both elevated in urine raised concern for amyloidosis however the ratio was normal suggesting polyclonal process. History of keratoconus prompted concern for possible Alport syndrome but no evidence on ophthalmological evaluation. Ultimately underwent renal biopsy with pathology consistent with primary membranous nephropathy with subepithelial immune deposits
Wait, remind me. What is Alport’s syndrome again? ? ? • AKA hereditary nephritis • associated with sensineural hearing loss and ocular abnormalities • It’s a basement membrane disease seen mostly in kids
Clinical pearl • Further supporting the diagnosis, patient was found to be phospholipase A 2 receptor antibody positive • In recent years, evaluating for anti-PLA 2 R antibodies has been found to correlate well with primary membranous nephropathy disease activity and can be used as a diagnostic test for primary glomerular nephropathy if biopsy is not possible. • M-type phospholipase A 2 receptor (PLA 2 R) is located on podocytes and in primary membranous nephropathy about 70% of patients have immune complexes vs. this receptor.
Take us home: - Based on biopsy results and phospholipase A 2 receptor antibody positivity, a diagnosis of primary membranous nephropathy was confirmed - He developed LE edema and hypertension; this improved with ACE-inhibitor therapy - Immunosuppression was considered but not started given improvement - Continued to have episodic recurrent flank pain. Cross-sectional revealed no mass concerning for associated malignancy and duplex US no renal arterial or venous thrombosis US (both at increased risk w/ nephrotic syndrome). - Ongoing pain is not thought to be related to membranous nephropathy
Resident Teaching Points About 20– 30% of cases of membranous glomerular nephropathy is found to be associated with secondary causes including - malignancy (primarily solid tumors) infection (hepatitis B, syphilis, malaria, schistosomiasis) rheumatologic disorders (SLE, RA, Ig. G 4 disease) drug exposure (NSAIDS, penicillamine, probenecid, others) with the remainder of adult cases primary or idiopathic
Resident Teaching Points Membranous nephropathy treatment 1 st line therapy for membranous nephropathy is: • ACE-inhibition • Treatment of dyslipidemia, edema and hypertension. • If the patient has refractory nephrotic range proteinuria, immunosuppression with a steroid course and cyclophosphamide or rituximab is considered. Nephrotic syndrome in general and particularly membranous nephropathy is associated with increased risk of arterial and venous thrombosis • thought to be due to loss of anticoagulant proteins antithrombin, protein C and S in the urine. • Renal arterial or venous thrombosis is most common complication • prophylactic AC considered for refractory cases but no great data. The risk of thrombi in nephrotic syndrome is a very important teaching point that is well highlighted on MKSAP questions. Deicsion for prophylactic anticoagulation is controversial because of the poor data.
• Thanks Cameron for a very cool case from clinic! • Please leave a comment in the blog on your team’s or your own learning points! The chiefs want to know!
References • Jameson, J. Larry, Anthony S. Fauci, et al. Harrison's Principles of Internal Medicine, 20 e. “Chapter 308: Glomerular Diseases”. New York: Mc. Graw-Hill, 2018. Access online through Access Medicine database. • Mansoor Andre M. (2019). Frameworks for internal medicine. “Chapter 34: Glomerular Disease”. Philadelphia: Wolters Kluwer. • Dyna. Med [Internet]. (MA): EBSCO Information Services. 1995 -. Record No. T 114446, Nephrotic Syndrome in Adults; [updated 2018 Nov 30, cited 2020, May 20]. Available from https: //www. dynamed. com/topics/dmp~AN~T 114446. Registration and login required. • KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Official Journal of the International Society of Nephrology. Volume 3, issue 1. January 2013. • Orth, Stephan and Eberhard Ritz. The nephrotic syndrome. N Engl J Med 1998; 338: 12021211. April 23, 1998.