Noon Report CC mouth ulcers Focus diagnostics and





- Slides: 32
Noon Report CC: mouth ulcers Focus: diagnostics and differential diagnosis Harrison Sapper Chief Facilitator: Shahana Baig-Lewis 4/22/2020
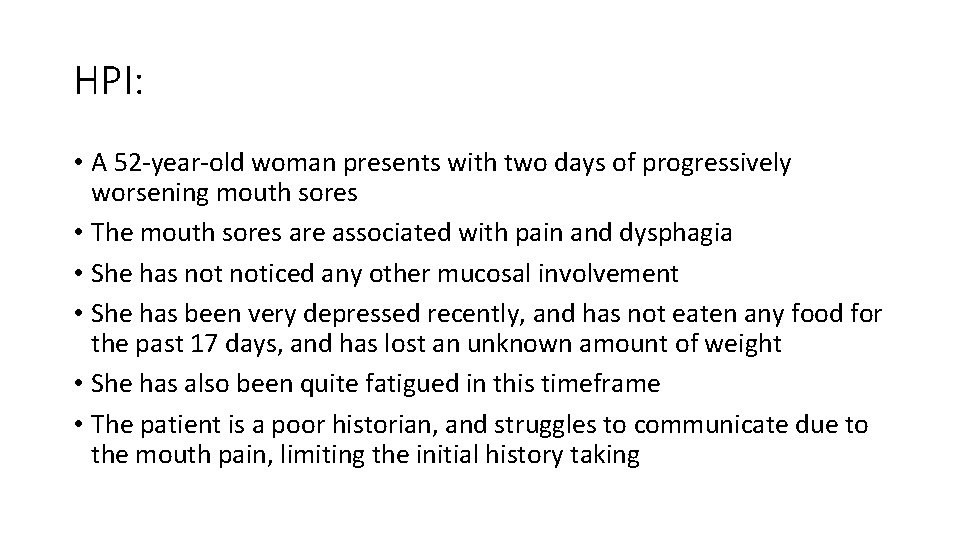
HPI: • A 52 -year-old woman presents with two days of progressively worsening mouth sores • The mouth sores are associated with pain and dysphagia • She has noticed any other mucosal involvement • She has been very depressed recently, and has not eaten any food for the past 17 days, and has lost an unknown amount of weight • She has also been quite fatigued in this timeframe • The patient is a poor historian, and struggles to communicate due to the mouth pain, limiting the initial history taking
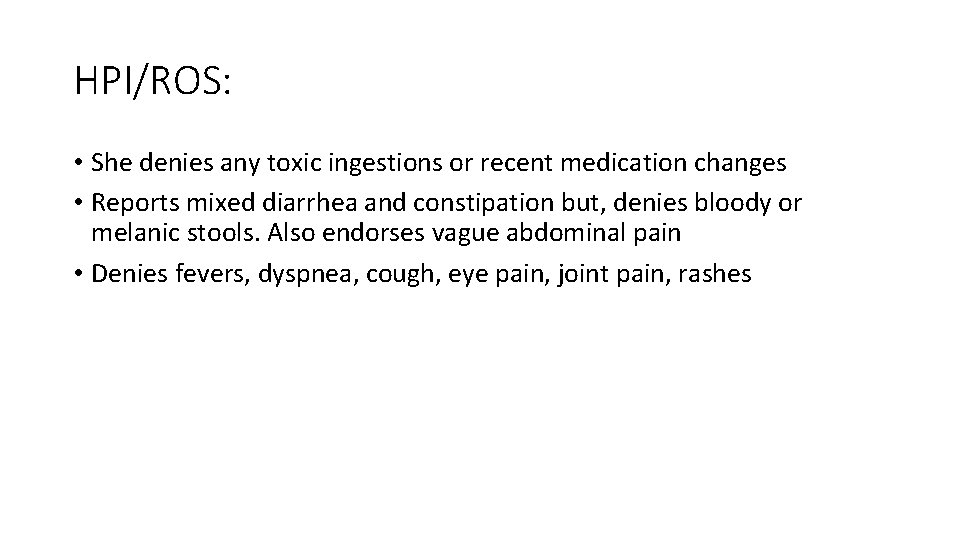
HPI/ROS: • She denies any toxic ingestions or recent medication changes • Reports mixed diarrhea and constipation but, denies bloody or melanic stools. Also endorses vague abdominal pain • Denies fevers, dyspnea, cough, eye pain, joint pain, rashes
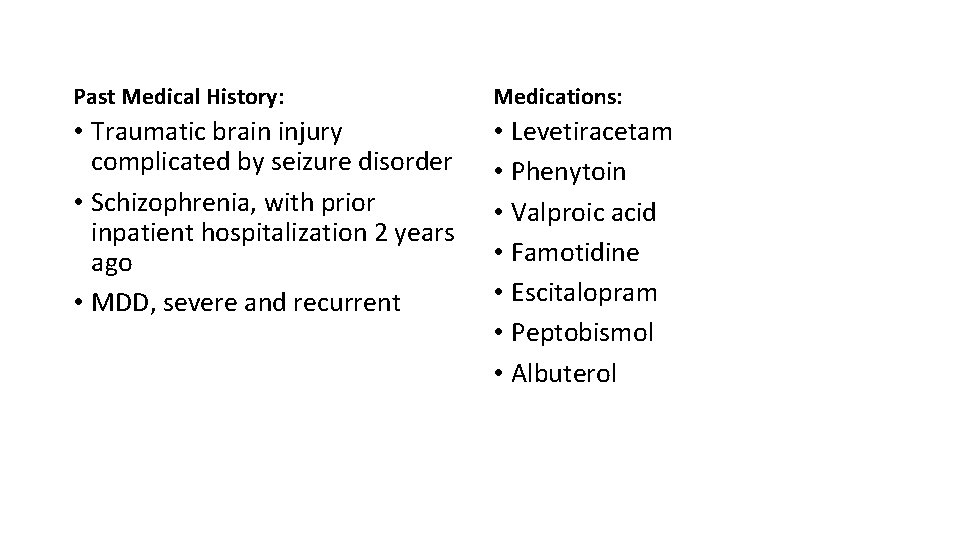
Past Medical History: Medications: • Traumatic brain injury complicated by seizure disorder • Schizophrenia, with prior inpatient hospitalization 2 years ago • MDD, severe and recurrent • Levetiracetam • Phenytoin • Valproic acid • Famotidine • Escitalopram • Peptobismol • Albuterol
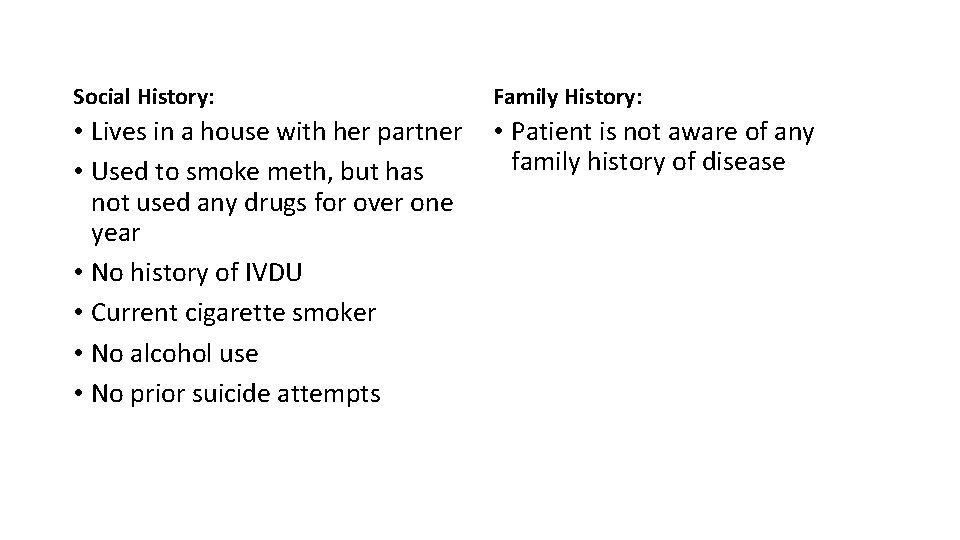
Social History: Family History: • Lives in a house with her partner • Used to smoke meth, but has not used any drugs for over one year • No history of IVDU • Current cigarette smoker • No alcohol use • No prior suicide attempts • Patient is not aware of any family history of disease
What is your differential diagnosis? What’s most likely? What can’t you miss?
Chief Pause! Let’s review the pertinent hx • Middle aged woman with • • TBI c/b seizure disorder on AEDs Schizophrenia MDD Prior meth use • Presents with • • acute onset oral ulcers with associated dysphagia, fatigue, and weight loss In the setting of depression and no PO intake ~ 2 weeks and the absence of medication changes
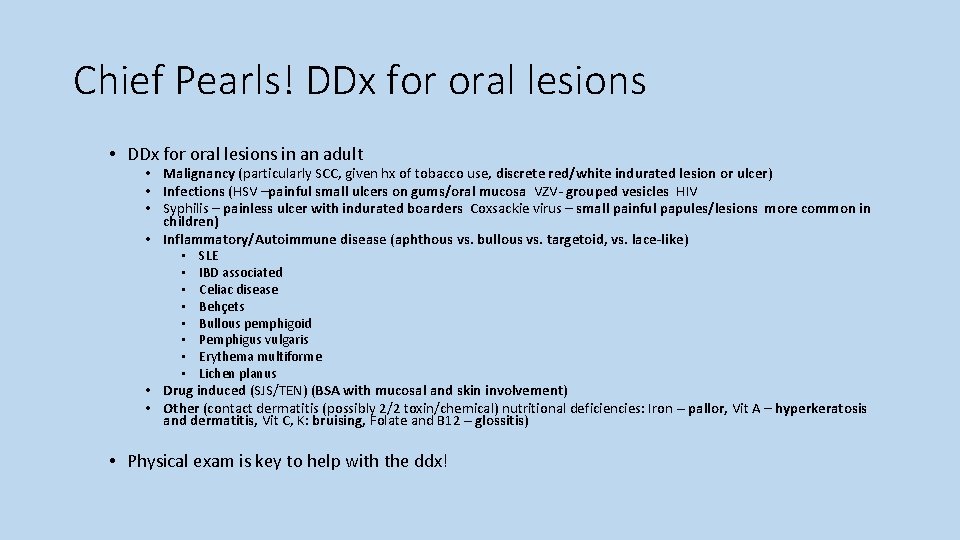
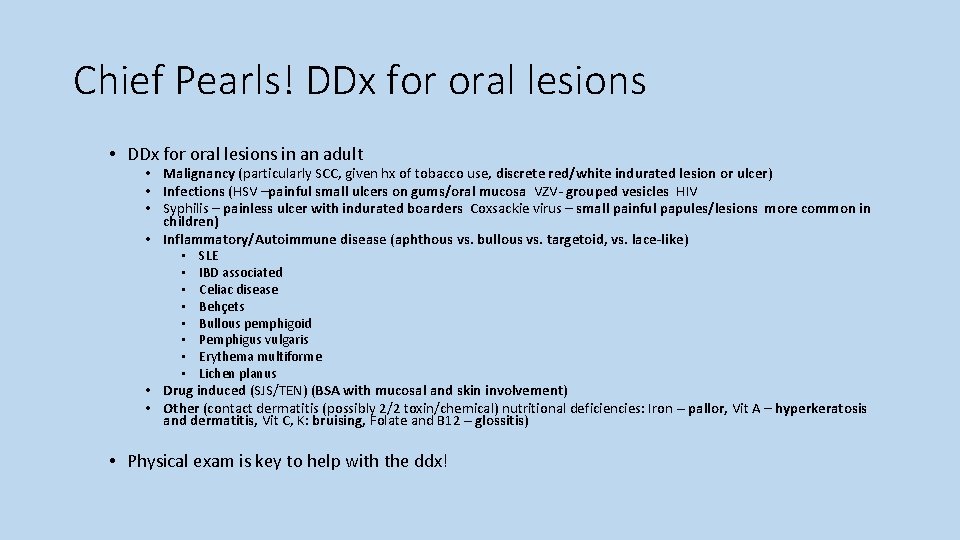
Chief Pearls! DDx for oral lesions • DDx for oral lesions in an adult • Malignancy (particularly SCC, given hx of tobacco use, discrete red/white indurated lesion or ulcer) • Infections (HSV –painful small ulcers on gums/oral mucosa VZV- grouped vesicles HIV • Syphilis – painless ulcer with indurated boarders Coxsackie virus – small painful papules/lesions more common in children) • Inflammatory/Autoimmune disease (aphthous vs. bullous vs. targetoid, vs. lace-like) • SLE • IBD associated • Celiac disease • Behçets • Bullous pemphigoid • Pemphigus vulgaris • Erythema multiforme • Lichen planus • Drug induced (SJS/TEN) (BSA with mucosal and skin involvement) • Other (contact dermatitis (possibly 2/2 toxin/chemical) nutritional deficiencies: Iron – pallor, Vit A – hyperkeratosis and dermatitis, Vit C, K: bruising, Folate and B 12 – glossitis) • Physical exam is key to help with the ddx!
Based on the HPI and history, what do you want to look for on exam? Why?
Chief Pearls! What to look for on Exam • Intraoral examination: • Visual and tactile inspection of the oral cavity with good light source • Extraoral examination • Eyes and nose (to assess for extraoral mucosal involvement) • LN (given concern for possible malignancy) • Abdomen, genitals, MSK, Skin (typically involved with AI conditions, drug reactions and nutritional deficiencies)
Exam: Vitals: afebrile, 120/70, HR 105, RR 20, on room air Gen: cachectic woman, appears older than age and chronically ill HEENT: poor dentition (pictures on next slide), eyes and nares appear normal CV: slightly tachycardic, regular rhythm, no murmurs Lungs: normal work of breathing, CTAB Abd: soft, non-tender, non-distended Ext: thin, warm, well perfused Skin: pale, no rashes Neuro: non-focal, slightly somnolent but easily arousable, will intermittently respond appropriately to basic questions


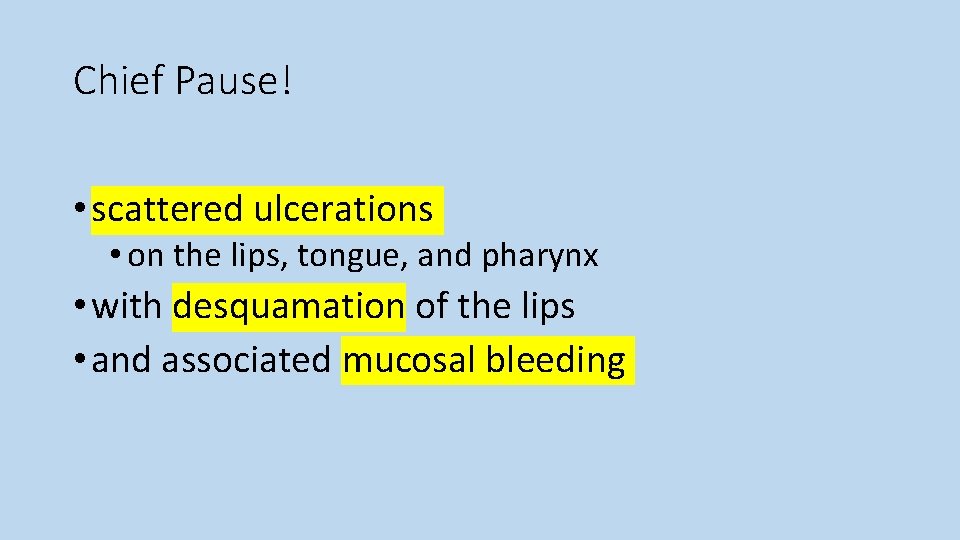
Chief Pause! • How would you describe the oral lesions?
Chief Pause! • scattered ulcerations • on the lips, tongue, and pharynx • with desquamation of the lips • and associated mucosal bleeding
How has your differential changed with the exam?
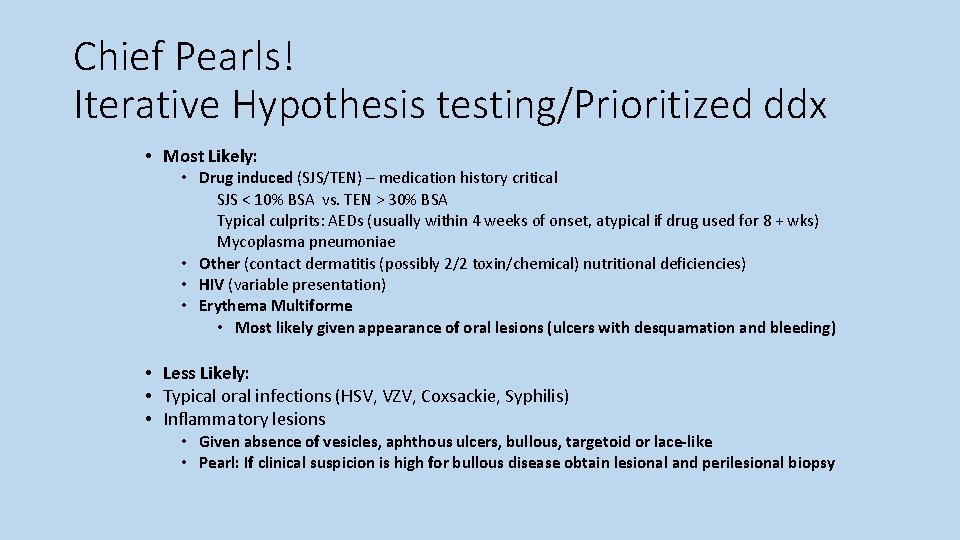
Chief Pearls! Iterative Hypothesis testing/Prioritized ddx • Most Likely: • Drug induced (SJS/TEN) – medication history critical SJS < 10% BSA vs. TEN > 30% BSA Typical culprits: AEDs (usually within 4 weeks of onset, atypical if drug used for 8 + wks) Mycoplasma pneumoniae • Other (contact dermatitis (possibly 2/2 toxin/chemical) nutritional deficiencies) • HIV (variable presentation) • Erythema Multiforme • Most likely given appearance of oral lesions (ulcers with desquamation and bleeding) • Less Likely: • Typical oral infections (HSV, VZV, Coxsackie, Syphilis) • Inflammatory lesions • Given absence of vesicles, aphthous ulcers, bullous, targetoid or lace-like • Pearl: If clinical suspicion is high for bullous disease obtain lesional and perilesional biopsy
Resident’s differential diagnoses: • SJS • Extra-intestinal manifestation of IBD • Erythema multiforme • Herpetic gingivostomatitis • Toxic ingestion / chemical injury • Aphthous ulcers • Autoimmune process • Malignancy
What’s your summary statement thus far?
Resident’s summary statement: • Middle-aged woman presents with two days progressively worsening mouth sores in the setting of not eating for 17 days due to severe depression
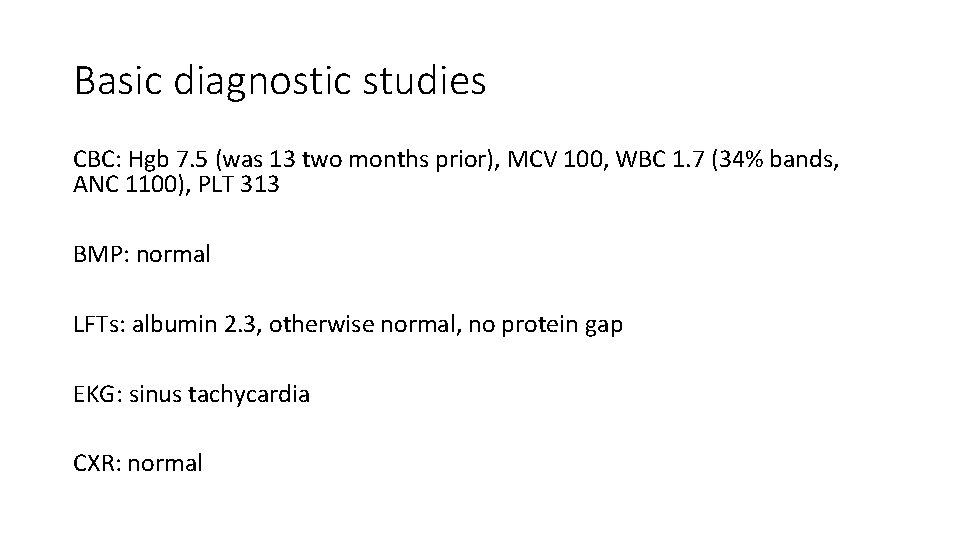
Basic diagnostic studies CBC: Hgb 7. 5 (was 13 two months prior), MCV 100, WBC 1. 7 (34% bands, ANC 1100), PLT 313 BMP: normal LFTs: albumin 2. 3, otherwise normal, no protein gap EKG: sinus tachycardia CXR: normal
Based on your differential, what other studies do you want? Why?
More laboratory studies -HIV: negative -Iron studies: normal, ferritin 286 -TSH: normal -B 12: normal -Rapid strep swab: negative -UDS, Tylenol, salicylates, alcohol level: all negative -Blood cultures: negative -Mouth ulcer swab cultures: normal oral flora -Valproate level: subtherapeutic, but detectable -Phenytoin level: undetectable -CRP: 20 -UA/micro: normal
Imaging studies CT neck, soft tissues, with IV contrast: extensive mucosal enhancement throughout oropharyngeal region, prominent pooling of secretions in posterior oropharynx
What is your leading diagnosis now? Can we streamline the summary statement more with this data?
Resident’s modified summary statement: • Middle-aged woman presents with two days progressively worsening mouth sores in the setting of not eating for 17 days due to severe depression, found to have diffuse mucosal enhancement, new anemia, and leukopenia

Hospital course: • The patient was initially unable to take anything by mouth and had significant secretions pooling in the posterior oropharynx • ENT evaluated the patient and patient was prescribed oral nystatin and chlorhexidine rinses, there was concern for bacterial superinfection • Dermatology evaluation raised concern for herpes infection or possible mycoplasma induced erythema multiforme • The patient was empirically treated with unasyn, acyclovir, and azithromycin for the above listed differential • However, even with those treatments the patient did not improve, and she remained unable to tolerate any PO intake for another 5 days
Take us home: Finally a test sent a few days previously returned her vitamin C level was undetectable The patient was started on high dose vitamin C, along with multivitamin supplements for presumed deficiencies Over the next two days the patient had complete resolution of her oral lesions and was able to eat food again normally Her anemia and leukopenia also gradually improved over the following few days and she was then discharged home


Resident Teaching Points: Scurvy! Scurvy is rare in the developed world, but is most frequently seen in patients with underlying psychiatric disorders who may have bizarre eating habits leading to nutritional deficiencies Patients often present with fatigue, oral bleeding, mouth pain, ulcerations and gum inflammation Scurvy can result in anemia and leukopenia Many vitamin deficiencies can manifest with oropharyngeal lesions such as angular cheilitis, glossitis, gingivitis, and ulcers
Resident Teaching Points Continued SJS is most likely to occur shortly after starting a culprit medication, and usually involves multiple different mucosal sites, so was unlikely in this case Erythema multiforme can present with similar lip desquamations as seen in this case, this can occur in cases of Mycoplasma pneumoniae In any malnourished patient with oropharyngeal lesions, nutritional deficiencies should be considered if there is any diagnostic uncertainty Patients with scurvy typically have rapid resolution of symptoms after receiving vitamin c
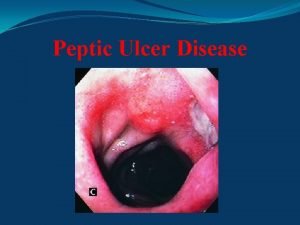
 Excessive acid production
Excessive acid production Gastritis x ray
Gastritis x ray Continuous bedside pressure mapping
Continuous bedside pressure mapping Peptic ulcer causes
Peptic ulcer causes Typhoid ulcer gross
Typhoid ulcer gross Stomach ulcer diet menu
Stomach ulcer diet menu Pratt's test for varicose veins
Pratt's test for varicose veins Johnson classification of ulcers
Johnson classification of ulcers Punched out edge ulcer
Punched out edge ulcer Integrated cost leadership/differentiation strategy
Integrated cost leadership/differentiation strategy Cost focus and differentiation focus
Cost focus and differentiation focus Focus on form vs focus on forms
Focus on form vs focus on forms Actor focus vs object focus
Actor focus vs object focus Da toolset
Da toolset Mitel system administration and diagnostics download
Mitel system administration and diagnostics download Idhaar tajweed
Idhaar tajweed Tanween
Tanween The rime of the ancient mariner analysis stanza by stanza
The rime of the ancient mariner analysis stanza by stanza Strategy based diagnostics
Strategy based diagnostics Duct diagnostics
Duct diagnostics Customer journey diagnostics
Customer journey diagnostics Win loader
Win loader Standard diagnostics korea
Standard diagnostics korea Laser beam diagnostic
Laser beam diagnostic Diagnostics infirmier
Diagnostics infirmier Viqt
Viqt Cole diagnostics jobs
Cole diagnostics jobs Casewise diagnostics
Casewise diagnostics Sensiring
Sensiring Sleep diagnostics butte mt
Sleep diagnostics butte mt Strongstep diagnostics
Strongstep diagnostics Prolight diagnostics forum
Prolight diagnostics forum Maximum number of diagnostics exceeded
Maximum number of diagnostics exceeded