NEUROLOGY NEUROLOGY Phase 2 A Revision Session Amogh


- Slides: 67
NEUROLOGY
NEUROLOGY Phase 2 A Revision Session Amogh Patil and Azhar Merchant 31/03/17 The Peer Teaching Society is not liable for false or misleading information…
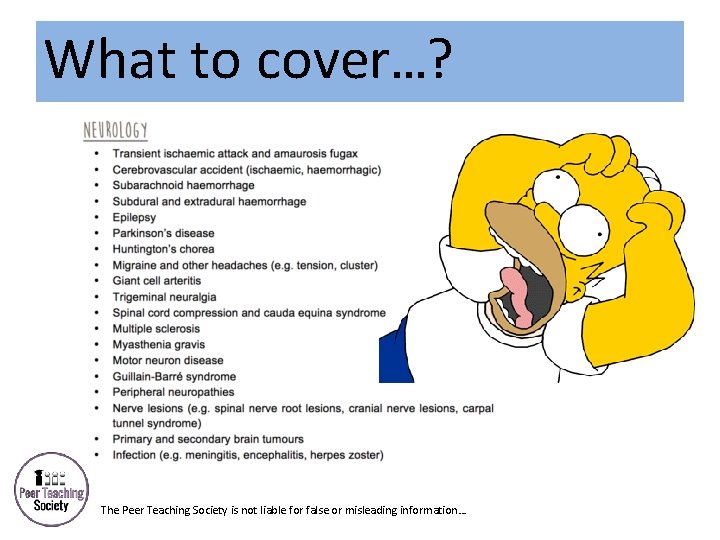
What to cover…? The Peer Teaching Society is not liable for false or misleading information…
TIA and stroke Aetiology • Thrombosis in situ • Embolism from heart (valve disease, mural thrombus – AF) or carotid (athero-thromboembolism) • CNS bleed – associated with HTN, aneurysm rupture, head injury • Young patient – vasculitis, thrombophilia, SAH Modifiable risk factors? x 4 • HTN, smoking, hyperlipidaemia, obesity Non-modifiable risk factors? x 4 • DM, male, vasculitis, hypotension The Peer Teaching Society is not liable for false or misleading information…
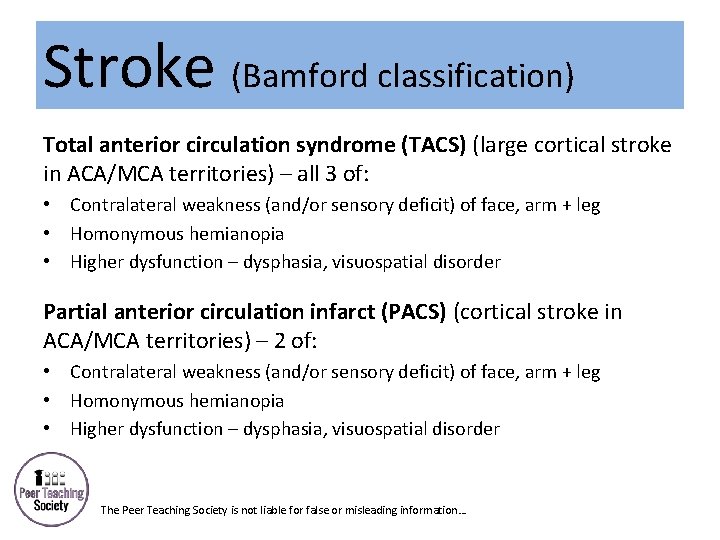
Stroke (Bamford classification) Total anterior circulation syndrome (TACS) (large cortical stroke in ACA/MCA territories) – all 3 of: • Contralateral weakness (and/or sensory deficit) of face, arm + leg • Homonymous hemianopia • Higher dysfunction – dysphasia, visuospatial disorder Partial anterior circulation infarct (PACS) (cortical stroke in ACA/MCA territories) – 2 of: • Contralateral weakness (and/or sensory deficit) of face, arm + leg • Homonymous hemianopia • Higher dysfunction – dysphasia, visuospatial disorder • The Peer Teaching Society is not liable for false or misleading information…
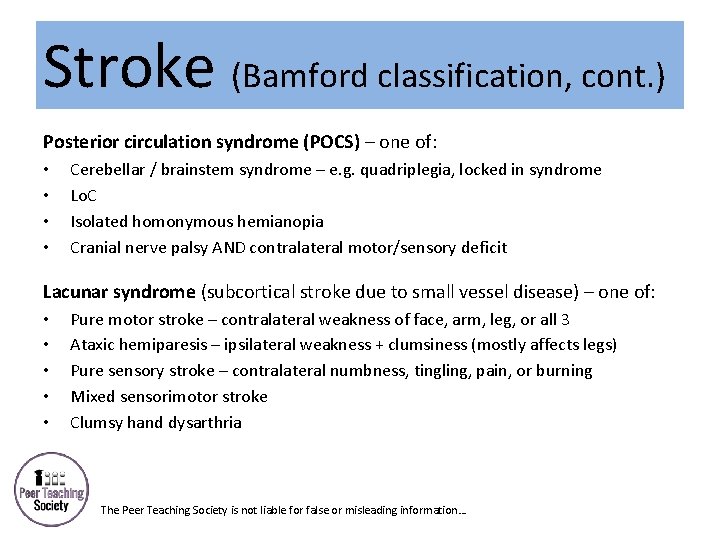
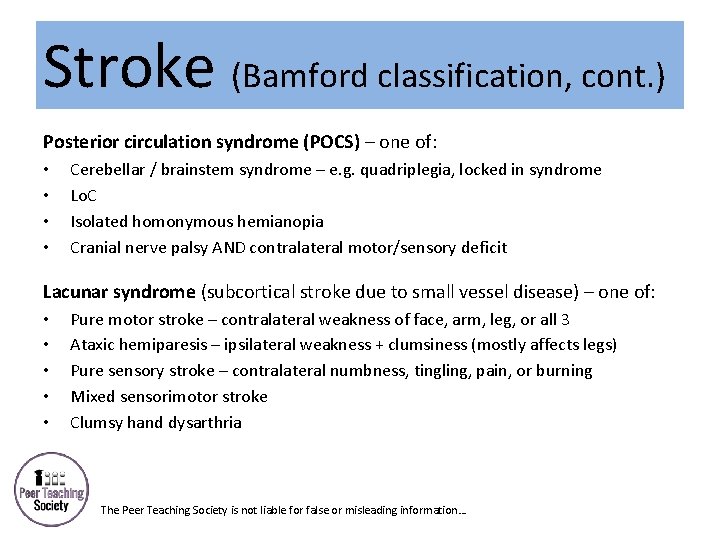
Stroke (Bamford classification, cont. ) Posterior circulation syndrome (POCS) – one of: • • Cerebellar / brainstem syndrome – e. g. quadriplegia, locked in syndrome Lo. C Isolated homonymous hemianopia Cranial nerve palsy AND contralateral motor/sensory deficit Lacunar syndrome (subcortical stroke due to small vessel disease) – one of: • • • Pure motor stroke – contralateral weakness of face, arm, leg, or all 3 Ataxic hemiparesis – ipsilateral weakness + clumsiness (mostly affects legs) Pure sensory stroke – contralateral numbness, tingling, pain, or burning Mixed sensorimotor stroke Clumsy hand dysarthria The Peer Teaching Society is not liable for false or misleading information…
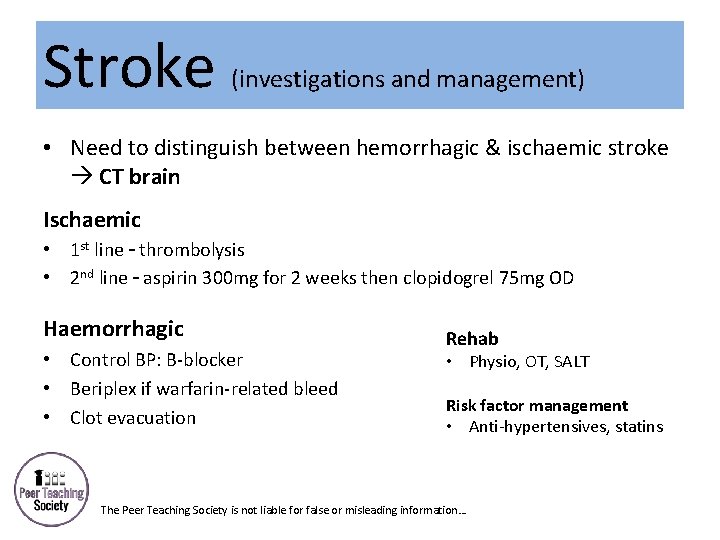
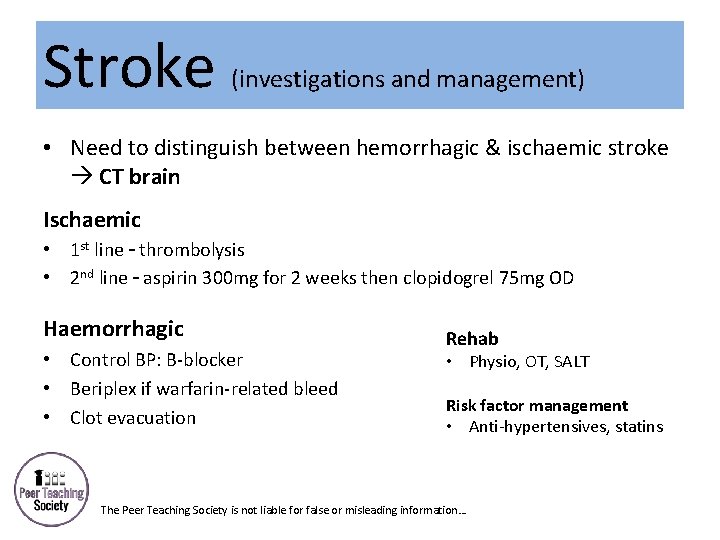
Stroke (investigations and management) • Need to distinguish between hemorrhagic & ischaemic stroke CT brain Ischaemic • 1 st line – thrombolysis • 2 nd line – aspirin 300 mg for 2 weeks then clopidogrel 75 mg OD Haemorrhagic • Control BP: B-blocker • Beriplex if warfarin-related bleed • Clot evacuation Rehab • Physio, OT, SALT Risk factor management • Anti-hypertensives, statins The Peer Teaching Society is not liable for false or misleading information…
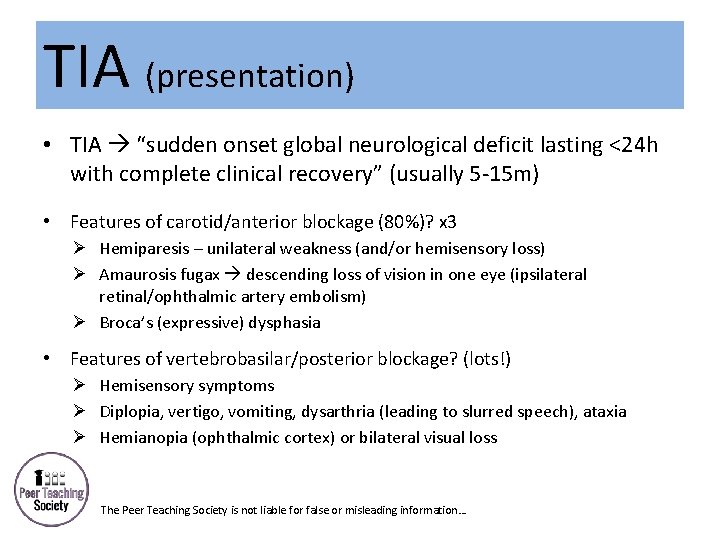
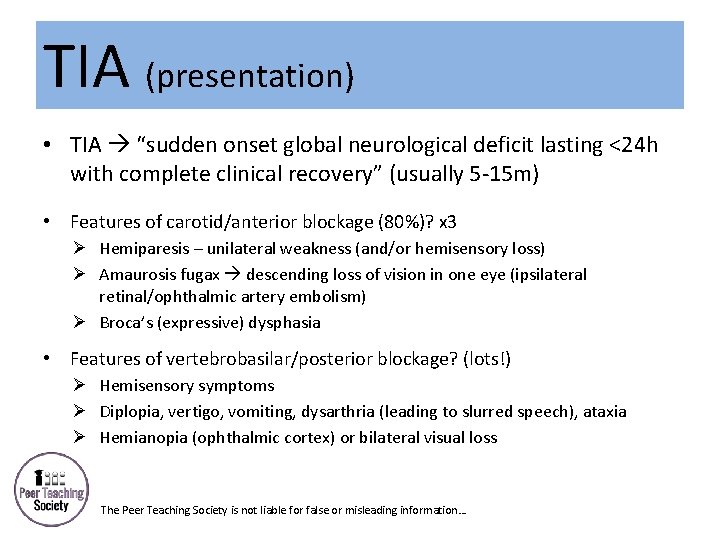
TIA (presentation) • TIA “sudden onset global neurological deficit lasting <24 h with complete clinical recovery” (usually 5 -15 m) • Features of carotid/anterior blockage (80%)? x 3 Ø Hemiparesis – unilateral weakness (and/or hemisensory loss) Ø Amaurosis fugax descending loss of vision in one eye (ipsilateral retinal/ophthalmic artery embolism) Ø Broca’s (expressive) dysphasia • Features of vertebrobasilar/posterior blockage? (lots!) Ø Hemisensory symptoms Ø Diplopia, vertigo, vomiting, dysarthria (leading to slurred speech), ataxia Ø Hemianopia (ophthalmic cortex) or bilateral visual loss The Peer Teaching Society is not liable for false or misleading information…
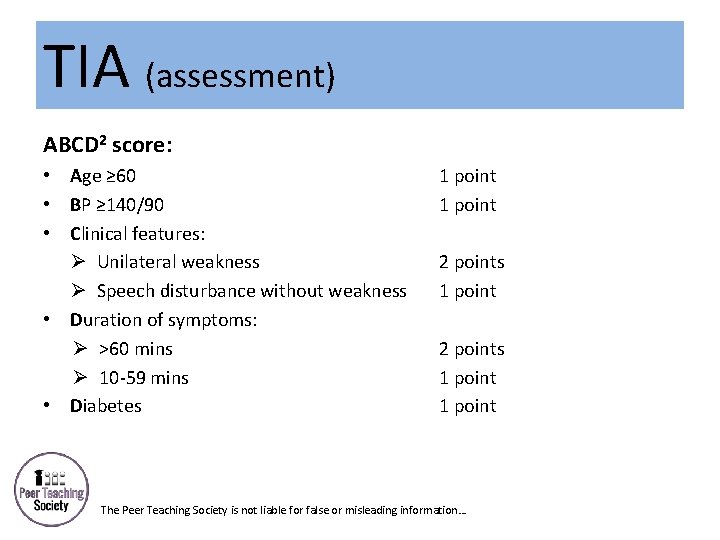
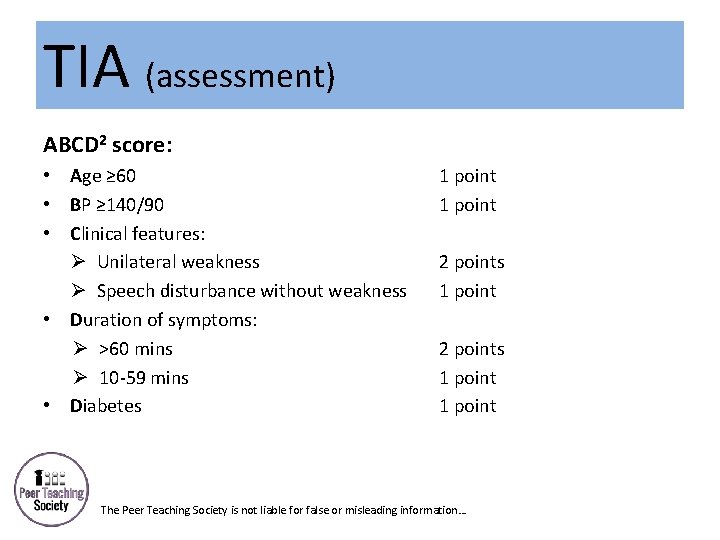
TIA (assessment) ABCD 2 score: • Age ≥ 60 • BP ≥ 140/90 • Clinical features: Ø Unilateral weakness Ø Speech disturbance without weakness • Duration of symptoms: Ø >60 mins Ø 10 -59 mins • Diabetes 1 point 2 points 1 point The Peer Teaching Society is not liable for false or misleading information…
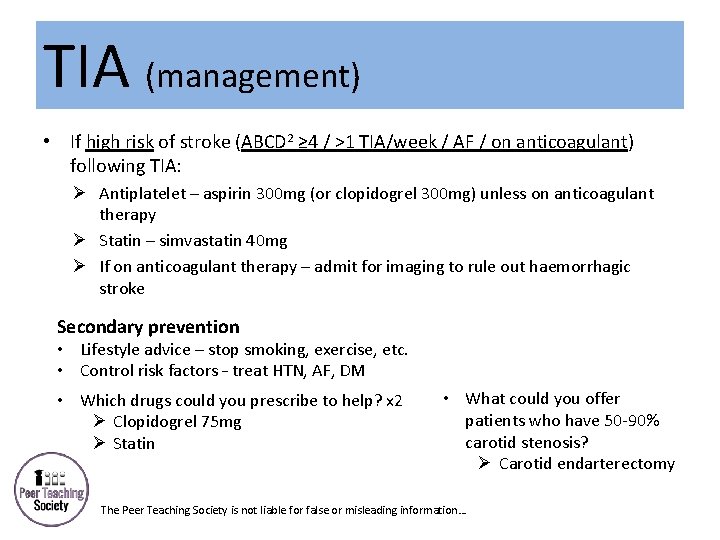
TIA (management) • If high risk of stroke (ABCD 2 ≥ 4 / >1 TIA/week / AF / on anticoagulant) following TIA: Ø Antiplatelet – aspirin 300 mg (or clopidogrel 300 mg) unless on anticoagulant therapy Ø Statin – simvastatin 40 mg Ø If on anticoagulant therapy – admit for imaging to rule out haemorrhagic stroke Secondary prevention • Lifestyle advice – stop smoking, exercise, etc. • Control risk factors – treat HTN, AF, DM • Which drugs could you prescribe to help? x 2 Ø Clopidogrel 75 mg Ø Statin • What could you offer patients who have 50 -90% carotid stenosis? Ø Carotid endarterectomy The Peer Teaching Society is not liable for false or misleading information…
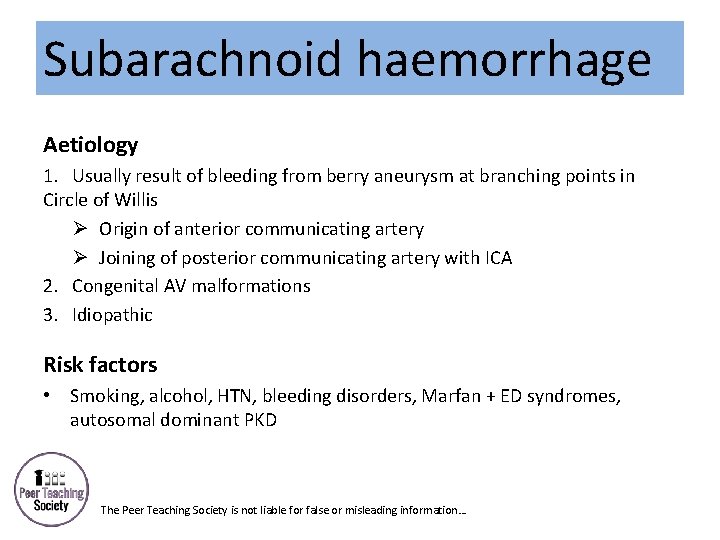
Subarachnoid haemorrhage Aetiology 1. Usually result of bleeding from berry aneurysm at branching points in Circle of Willis Ø Origin of anterior communicating artery Ø Joining of posterior communicating artery with ICA 2. Congenital AV malformations 3. Idiopathic Risk factors • Smoking, alcohol, HTN, bleeding disorders, Marfan + ED syndromes, autosomal dominant PKD The Peer Teaching Society is not liable for false or misleading information…
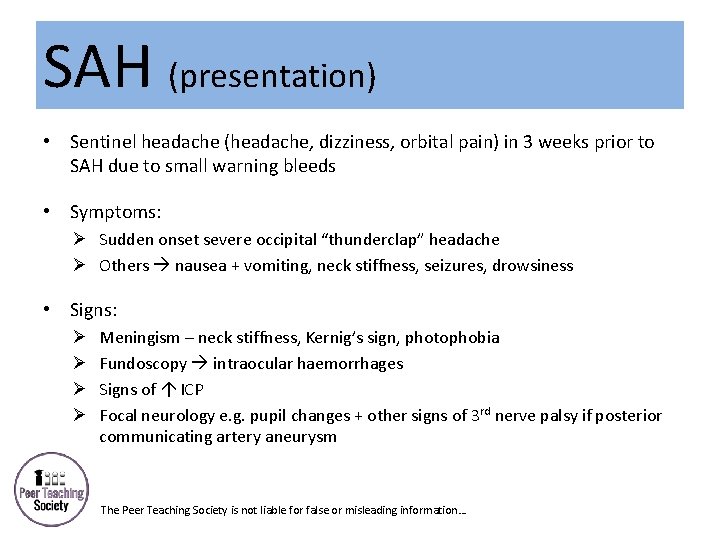
SAH (presentation) • Sentinel headache (headache, dizziness, orbital pain) in 3 weeks prior to SAH due to small warning bleeds • Symptoms: Ø Sudden onset severe occipital “thunderclap” headache Ø Others nausea + vomiting, neck stiffness, seizures, drowsiness • Signs: Ø Ø Meningism – neck stiffness, Kernig’s sign, photophobia Fundoscopy intraocular haemorrhages Signs of ICP Focal neurology e. g. pupil changes + other signs of 3 rd nerve palsy if posterior communicating artery aneurysm The Peer Teaching Society is not liable for false or misleading information…
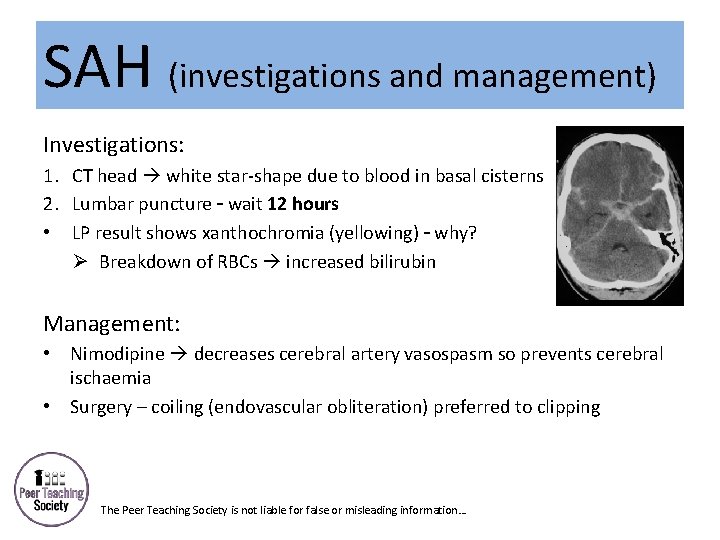
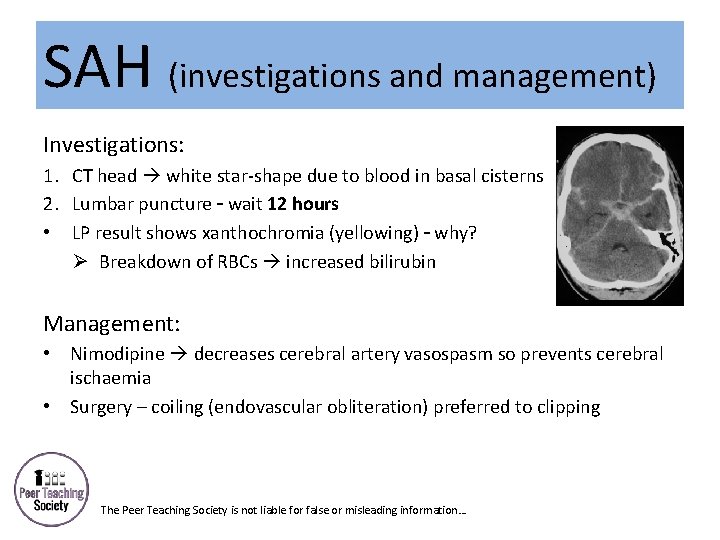
SAH (investigations and management) Investigations: 1. CT head white star-shape due to blood in basal cisterns 2. Lumbar puncture – wait 12 hours • LP result shows xanthochromia (yellowing) – why? Ø Breakdown of RBCs increased bilirubin Management: • Nimodipine decreases cerebral artery vasospasm so prevents cerebral ischaemia • Surgery – coiling (endovascular obliteration) preferred to clipping The Peer Teaching Society is not liable for false or misleading information…
Subdural and epidural haematoma Subdural haematoma • Which people are affected? Ø Elderly + alcoholics • Why are they affected? x 3 Ø Brain atrophy Ø Vein stretching Ø Increased likelihood to fall The Peer Teaching Society is not liable for false or misleading information…
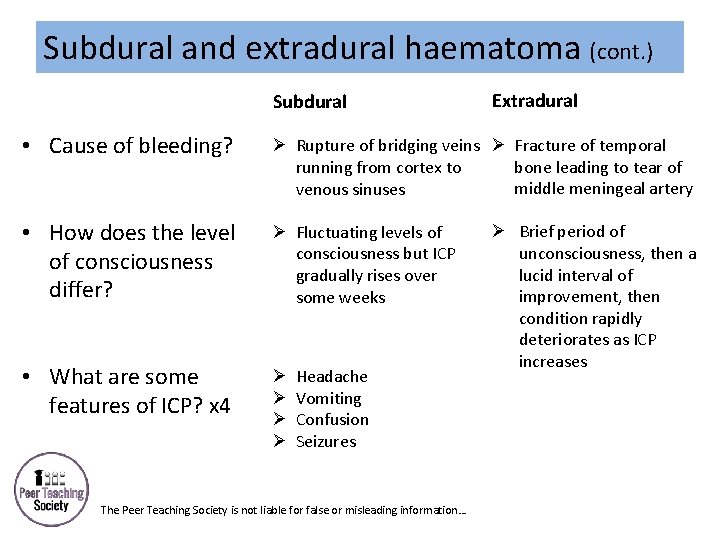
Subdural and extradural haematoma (cont. ) Subdural Extradural • Cause of bleeding? Ø Rupture of bridging veins Ø Fracture of temporal bone leading to tear of running from cortex to middle meningeal artery venous sinuses • How does the level of consciousness differ? Ø Fluctuating levels of consciousness but ICP gradually rises over some weeks • What are some features of ICP? x 4 Ø Ø Headache Vomiting Confusion Seizures The Peer Teaching Society is not liable for false or misleading information… Ø Brief period of unconsciousness, then a lucid interval of improvement, then condition rapidly deteriorates as ICP increases
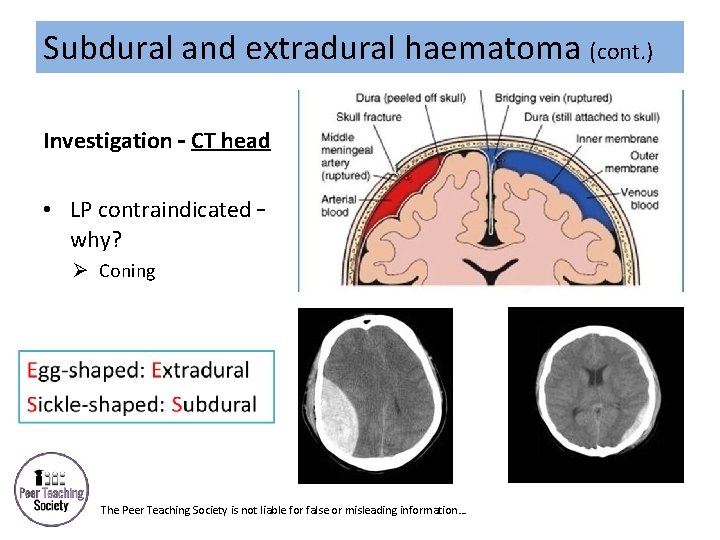
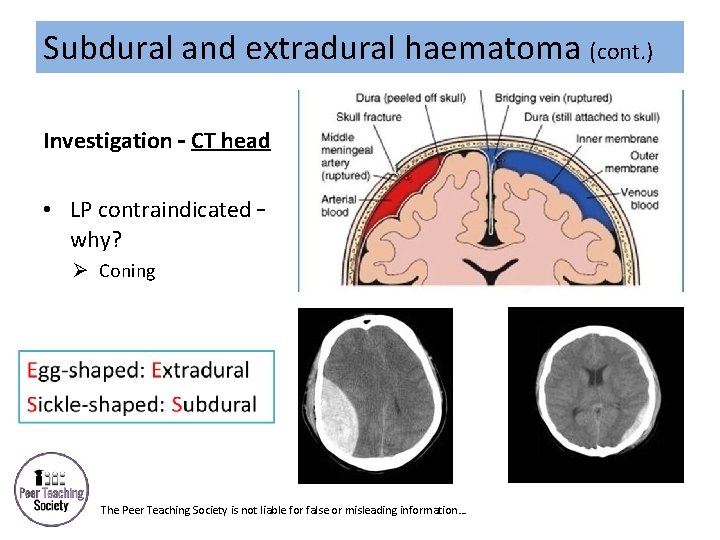
Subdural and extradural haematoma (cont. ) Investigation – CT head • LP contraindicated – why? Ø Coning The Peer Teaching Society is not liable for false or misleading information…
Subdural and extradural haematoma (cont. ) Management • First thing that should be done? Ø ABCDE • Next – how would you treat raised ICP? Ø Osmotic diuresis with mannitol • Surgery Ø SDH emergency evacuation via Burr hole craniotomy Ø EDH clot evacuation +/- ligation of bleeding vessel The Peer Teaching Society is not liable for false or misleading information…
Epilepsy (presentation) • “Recurrent tendency to have spontaneous, intermittent and abnormal electrical activity in a part of the brain, manifesting as seizures” • Prodrome aura ictal symptoms post-ictal symptoms Ø Prodrome = mood/behaviour change Ø Aura = part of seizure patient is aware of Ø Ictal symptoms = dependent on part of brain affected Ø Post-ictal symptoms = headache, confusion, amnesia, etc. The Peer Teaching Society is not liable for false or misleading information…
Epilepsy (classification) Partial (focal) seizures – limited to 1 hemisphere • Temporal (most common) Ø Smell/taste abnormalities, auditory phenomena Ø Automatisms lip smacking, walking without purpose Ø Memory phenomena déjà-vu/jamais-vu • Frontal Ø Motor phenomena (may lead to Jacksonian march (spreading clonic movement – Jacksonian march) • Occipital visual phenomena • Parietal sensory disturbances – tingling, numbness, etc. The Peer Teaching Society is not liable for false or misleading information…
Epilepsy (classification) Generalised seizures – simultaneous electrical discharge through cortex • Absence transient Lo. C <10 s, abrupt onset + termination • Myoclonic sudden, brief jerking of limb/face/trunk • Tonic increased tone • Tonic-clonic 1. Tonic phase (Lo. C + increased tone of limbs) 2. Clonic phase (rhythmical jerking of limbs) • Atonic no Lo. C, sudden loss of muscle tone e. g. drop of hand or fall The Peer Teaching Society is not liable for false or misleading information…
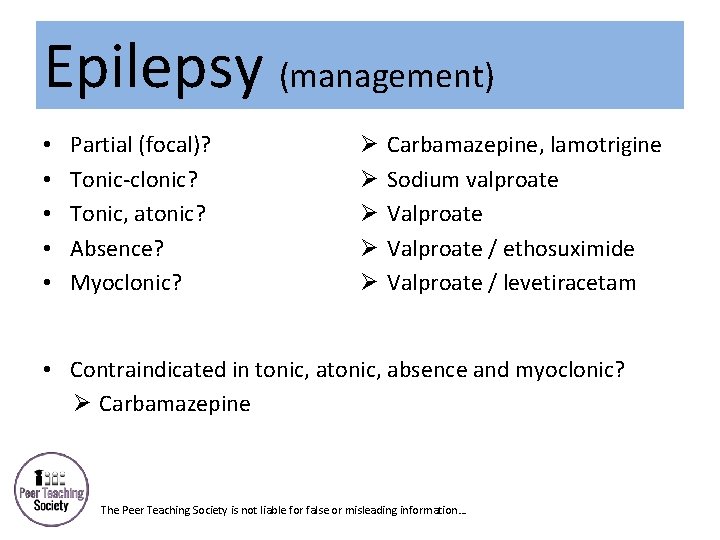
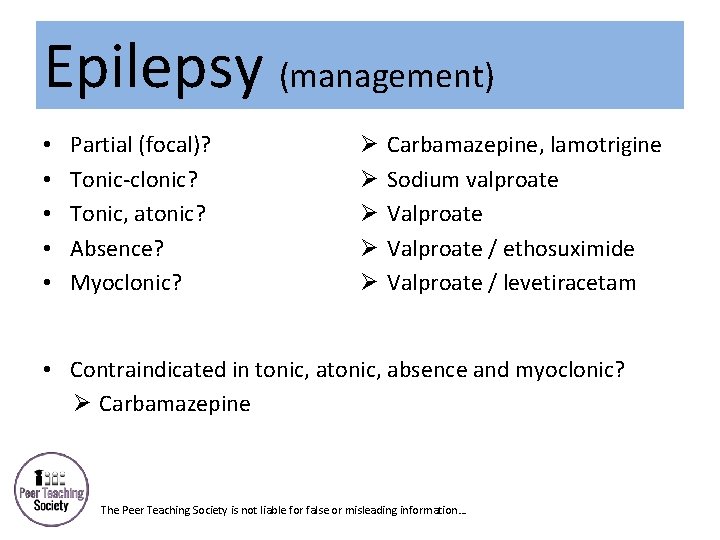
Epilepsy (management) • • • Partial (focal)? Tonic-clonic? Tonic, atonic? Absence? Myoclonic? Ø Ø Ø Carbamazepine, lamotrigine Sodium valproate Valproate / ethosuximide Valproate / levetiracetam • Contraindicated in tonic, absence and myoclonic? Ø Carbamazepine The Peer Teaching Society is not liable for false or misleading information…
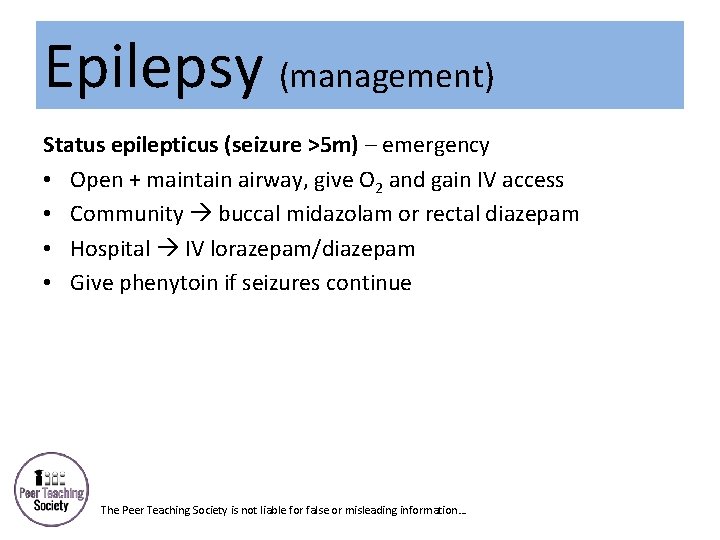
Epilepsy (management) Status epilepticus (seizure >5 m) – emergency • Open + maintain airway, give O 2 and gain IV access • Community buccal midazolam or rectal diazepam • Hospital IV lorazepam/diazepam • Give phenytoin if seizures continue The Peer Teaching Society is not liable for false or misleading information…
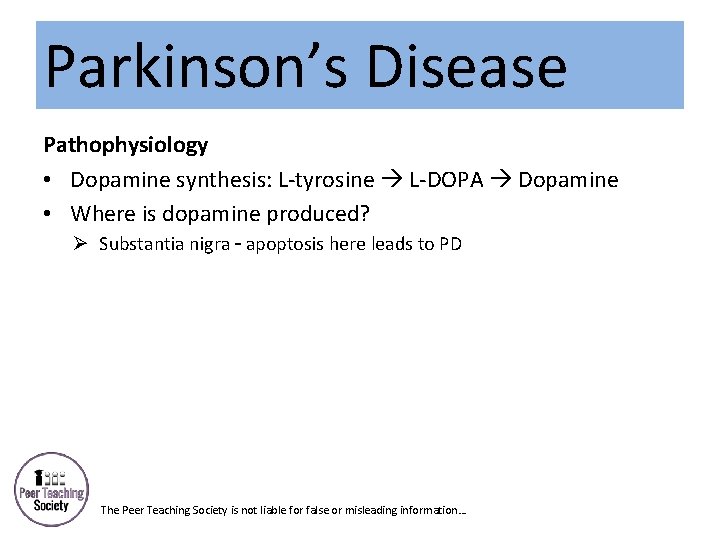
Parkinson’s Disease Pathophysiology • Dopamine synthesis: L-tyrosine L-DOPA Dopamine • Where is dopamine produced? Ø Substantia nigra – apoptosis here leads to PD The Peer Teaching Society is not liable for false or misleading information…
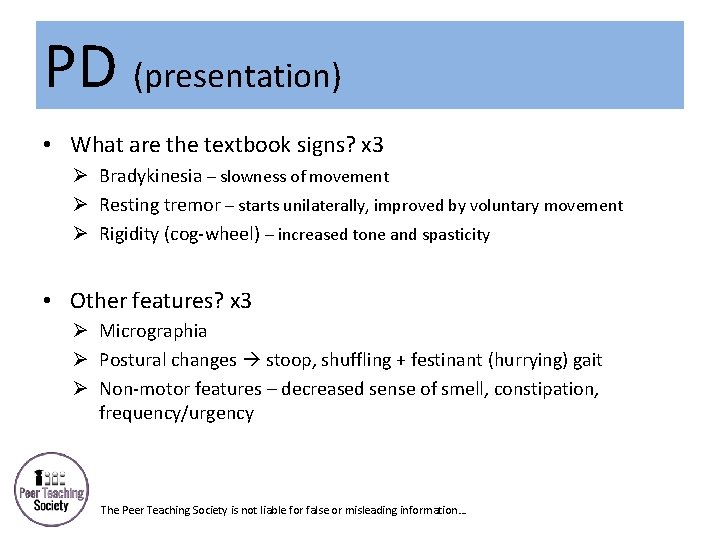
PD (presentation) • What are the textbook signs? x 3 Ø Bradykinesia – slowness of movement Ø Resting tremor – starts unilaterally, improved by voluntary movement Ø Rigidity (cog-wheel) – increased tone and spasticity • Other features? x 3 Ø Micrographia Ø Postural changes stoop, shuffling + festinant (hurrying) gait Ø Non-motor features – decreased sense of smell, constipation, frequency/urgency The Peer Teaching Society is not liable for false or misleading information…
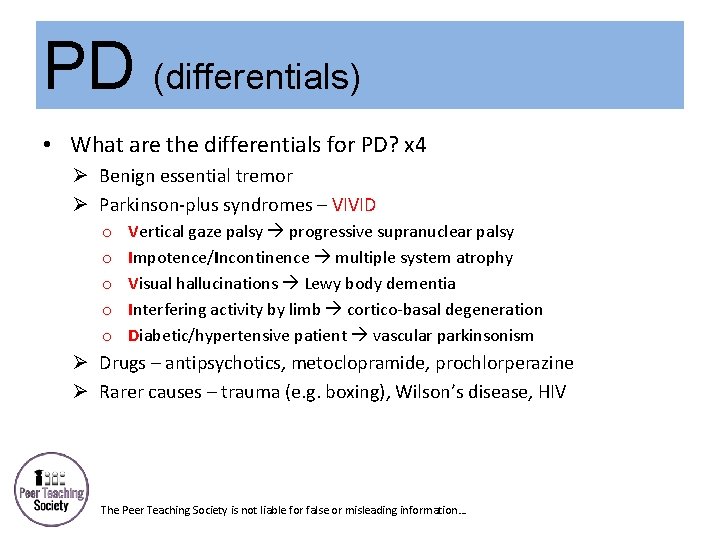
PD (differentials) • What are the differentials for PD? x 4 Ø Benign essential tremor Ø Parkinson-plus syndromes – VIVID o o o Vertical gaze palsy progressive supranuclear palsy Impotence/Incontinence multiple system atrophy Visual hallucinations Lewy body dementia Interfering activity by limb cortico-basal degeneration Diabetic/hypertensive patient vascular parkinsonism Ø Drugs – antipsychotics, metoclopramide, prochlorperazine Ø Rarer causes – trauma (e. g. boxing), Wilson’s disease, HIV The Peer Teaching Society is not liable for false or misleading information…
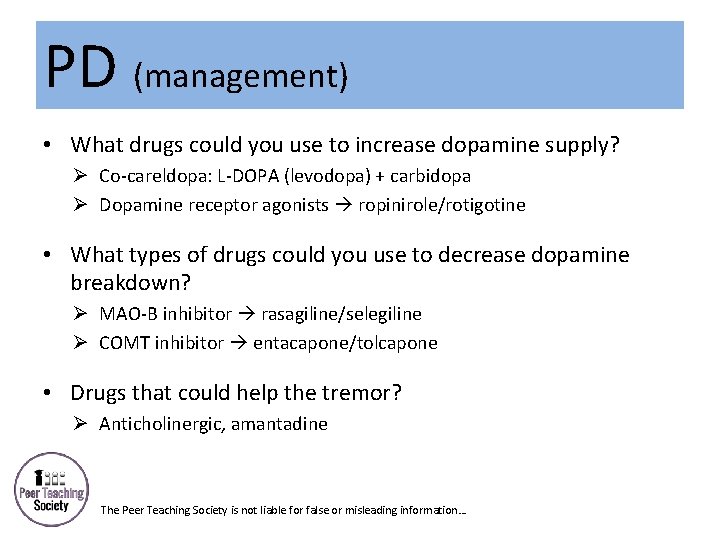
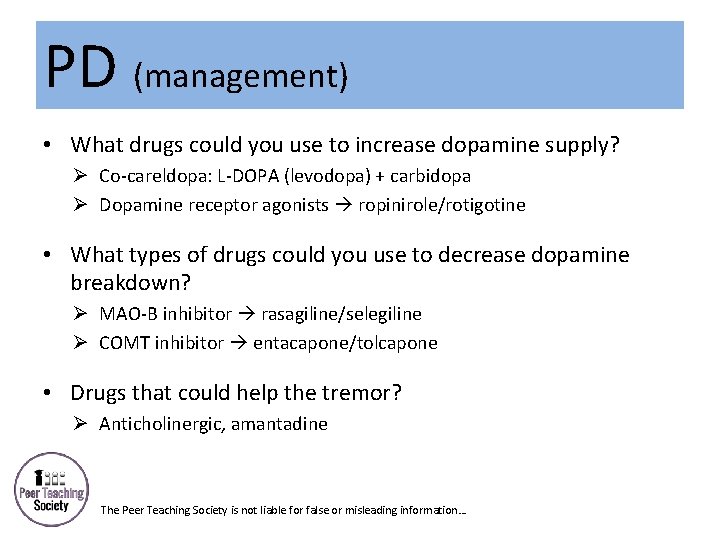
PD (management) • What drugs could you use to increase dopamine supply? Ø Co-careldopa: L-DOPA (levodopa) + carbidopa Ø Dopamine receptor agonists ropinirole/rotigotine • What types of drugs could you use to decrease dopamine breakdown? Ø MAO-B inhibitor rasagiline/selegiline Ø COMT inhibitor entacapone/tolcapone • Drugs that could help the tremor? Ø Anticholinergic, amantadine The Peer Teaching Society is not liable for false or misleading information…
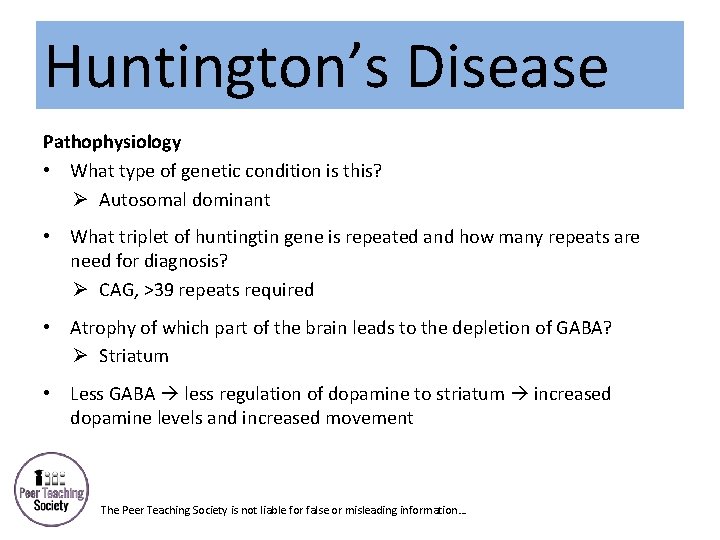
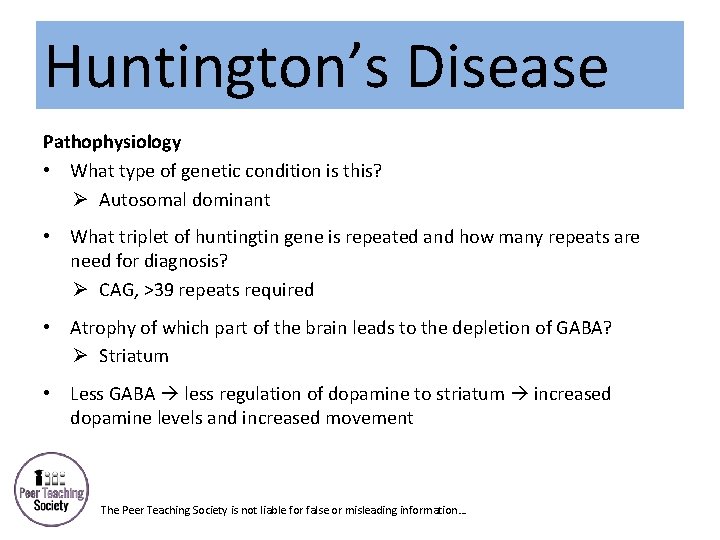
Huntington’s Disease Pathophysiology • What type of genetic condition is this? Ø Autosomal dominant • What triplet of huntingtin gene is repeated and how many repeats are need for diagnosis? Ø CAG, >39 repeats required • Atrophy of which part of the brain leads to the depletion of GABA? Ø Striatum • Less GABA less regulation of dopamine to striatum increased dopamine levels and increased movement The Peer Teaching Society is not liable for false or misleading information…
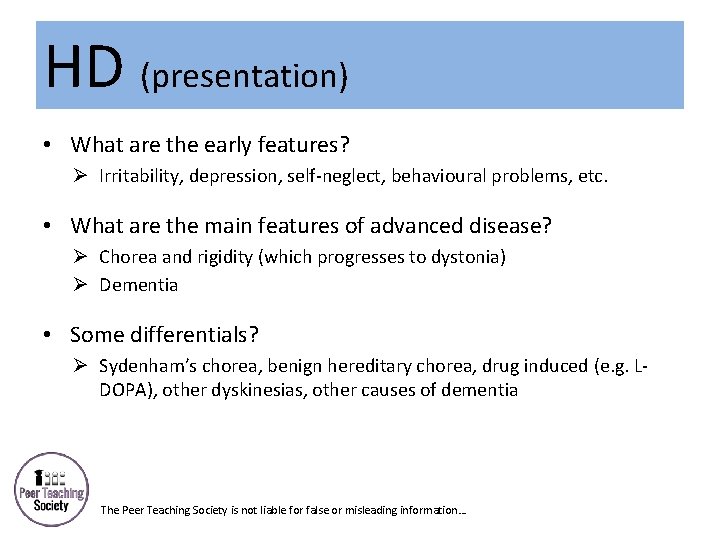
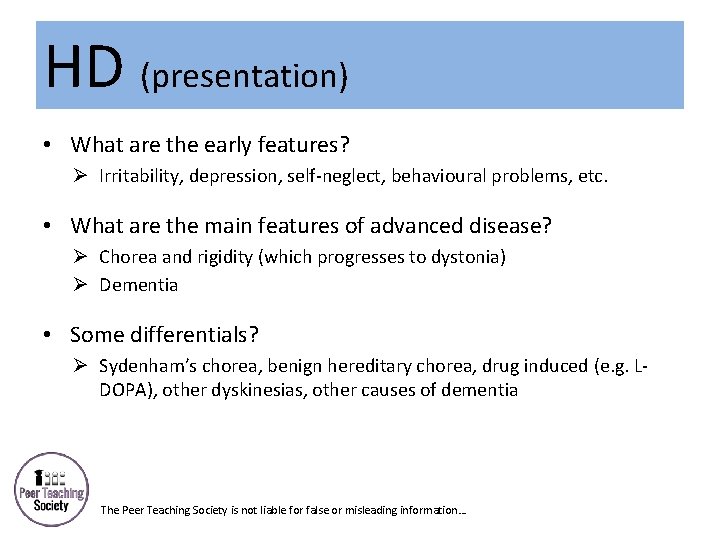
HD (presentation) • What are the early features? Ø Irritability, depression, self-neglect, behavioural problems, etc. • What are the main features of advanced disease? Ø Chorea and rigidity (which progresses to dystonia) Ø Dementia • Some differentials? Ø Sydenham’s chorea, benign hereditary chorea, drug induced (e. g. LDOPA), other dyskinesias, other causes of dementia The Peer Teaching Society is not liable for false or misleading information…
Headaches Classification • Primary – tension, cluster, migraine • Secondary – meningitis, encephalitis, GCA, medication overuse, venous thrombosis, tumour, SAH • Other – trigeminal neuralgia The Peer Teaching Society is not liable for false or misleading information…
Tension headache Classification • Episodic TH – <15 d per month • Chronic TH – >15 d per month, can be medication induced, also associated with depression Cause • Neurovascular irritation which refers to scalp muscles and soft tissues The Peer Teaching Society is not liable for false or misleading information…
Tension headache (cont. ) Presentation • What type of pain and where is it felt? Ø Generalised mild-moderate pressing/tightening pain bilaterally • Range of time it can last for? Ø 30 minutes to 7 days Treatment (as well as reassurance, stress relief, etc. ) • Types of drugs used for simple cases and chronic cases? Ø Simple ibuprofen, aspirin, etc. Ø Chronic TCA e. g. amitriptyline The Peer Teaching Society is not liable for false or misleading information…
Cluster headache Presentation • What type of onset where is the pain? Ø Rapid onset severe unilateral, orbital, supraorbital or temporal pain • Range of time it can last for? Ø 15 -180 minutes • What time of day do patients say they get these headaches? Ø Middle of night or morning hours (occurs after REM sleep) • Other symptoms? x 4 Ø Ipsilateral eye lacrimation & redness, rhinorrea, miosis and/or ptosis The Peer Teaching Society is not liable for false or misleading information…
Cluster headache (cont. ) Treatment • Acute case (name of drug, route administered)? Ø Subcutaneous sumatriptan • What else…? Ø 100% oxygen through non-rebreathable mask for 15 minutes • What drugs can be used as prevention? x 3 Ø Verapamil, lithium carbonate, prednisolone The Peer Teaching Society is not liable for false or misleading information…
Migraine • Triggers – CHOCOLATE: Ø Ø Ø Ø Ø Chocolate Hangovers Orgasms Cheese Oral contraceptive pill Lie-ins Alcohol Tumult Exercise The Peer Teaching Society is not liable for false or misleading information…
Migraine (presentation) Migraine without aura – 4 diagnostic criteria: • ≥ 5 attacks • Lasting 4 -72 h • ≥ 2 of the following 4: Ø Ø Unilateral Pulsating Moderate/severe pain Aggravation by (or avoidance of) routine physical activity • ≥ 1 of the following: Ø Nausea and/or vomiting Ø Photophobia and phonophobia The Peer Teaching Society is not liable for false or misleading information…
Migraine (presentation) Migraine with aura – 2 diagnostic criteria: • ≥ 1 reversible aura symptom Ø Ø Visual – zigzags, spots Unilateral sensory – tingling, numbness Speech – aphasia Motor weakness (known as “hemiplegic migraine” so rule out stroke & TIA) • ≥ 2 of the following 4: Ø ≥ 1 aura symptom spreads gradually over ≥ 5 m and/or ≥ 2 aura symptoms occurring in succession Ø Each aura symptom lasts 5 -60 m Ø ≥ 1 aura symptom is unilateral Ø Aura accompanied/followed within 60 m by headache The Peer Teaching Society is not liable for false or misleading information…
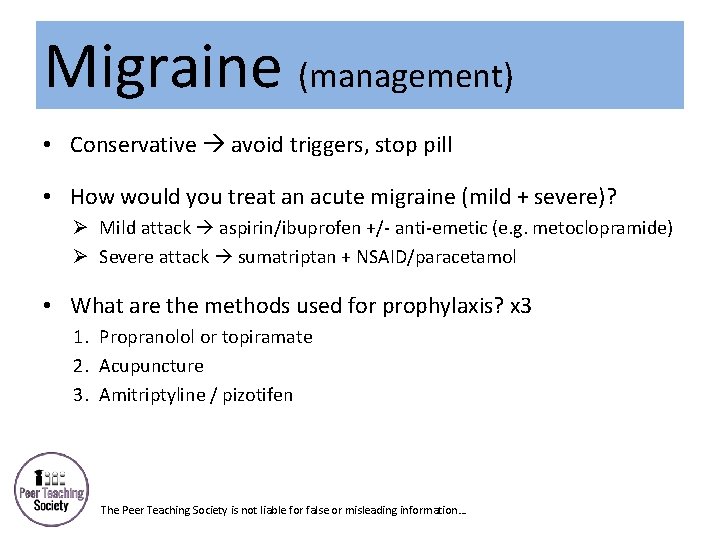
Migraine (management) • Conservative avoid triggers, stop pill • How would you treat an acute migraine (mild + severe)? Ø Mild attack aspirin/ibuprofen +/- anti-emetic (e. g. metoclopramide) Ø Severe attack sumatriptan + NSAID/paracetamol • What are the methods used for prophylaxis? x 3 1. Propranolol or topiramate 2. Acupuncture 3. Amitriptyline / pizotifen The Peer Teaching Society is not liable for false or misleading information…
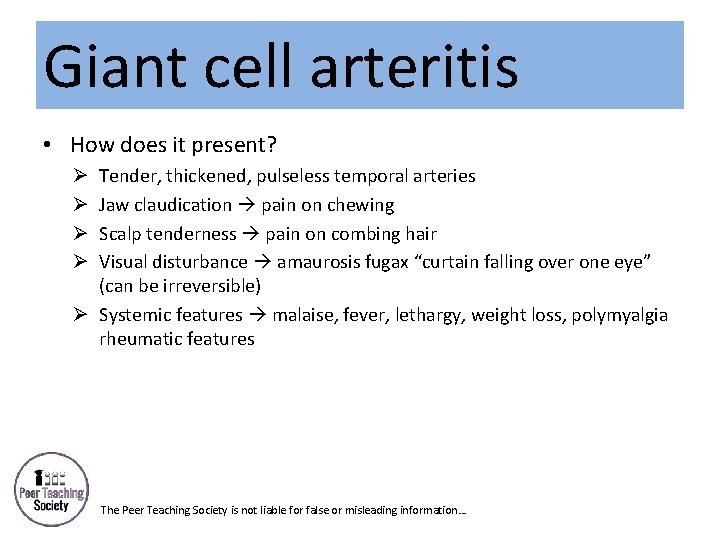
Giant cell arteritis • How does it present? Tender, thickened, pulseless temporal arteries Jaw claudication pain on chewing Scalp tenderness pain on combing hair Visual disturbance amaurosis fugax “curtain falling over one eye” (can be irreversible) Ø Systemic features malaise, fever, lethargy, weight loss, polymyalgia rheumatic features Ø Ø The Peer Teaching Society is not liable for false or misleading information…
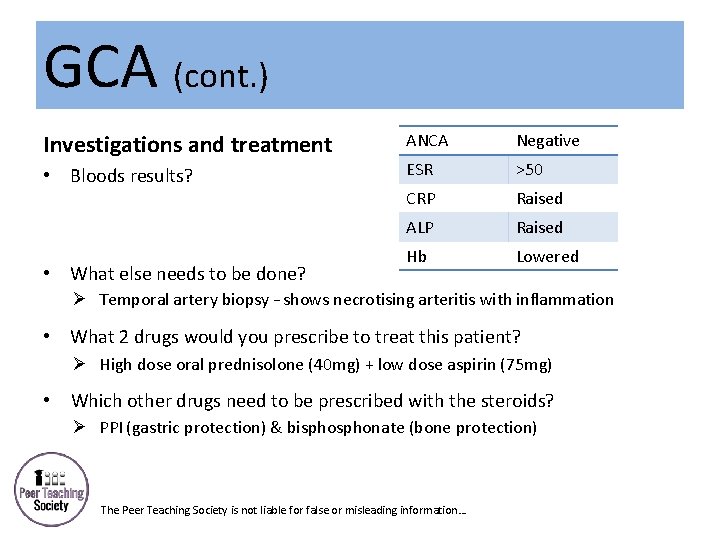
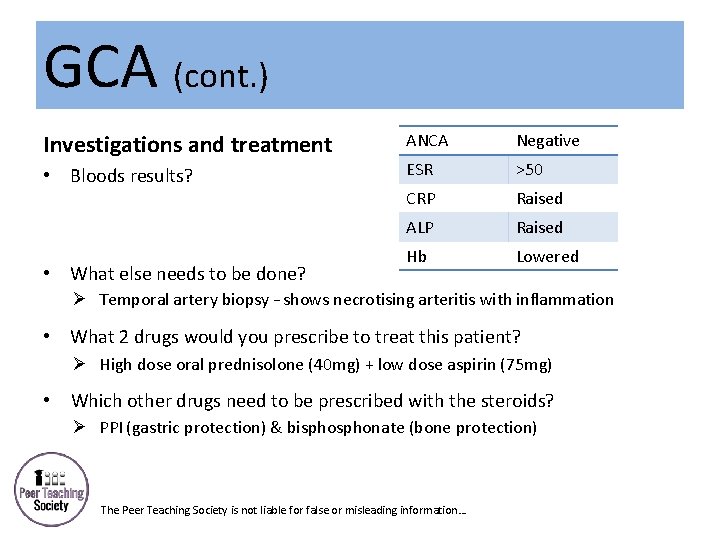
GCA (cont. ) Investigations and treatment • Bloods results? • What else needs to be done? ANCA Negative ESR >50 CRP Raised ALP Raised Hb Lowered Ø Temporal artery biopsy – shows necrotising arteritis with inflammation • What 2 drugs would you prescribe to treat this patient? Ø High dose oral prednisolone (40 mg) + low dose aspirin (75 mg) • Which other drugs need to be prescribed with the steroids? Ø PPI (gastric protection) & bisphonate (bone protection) • The Peer Teaching Society is not liable for false or misleading information…
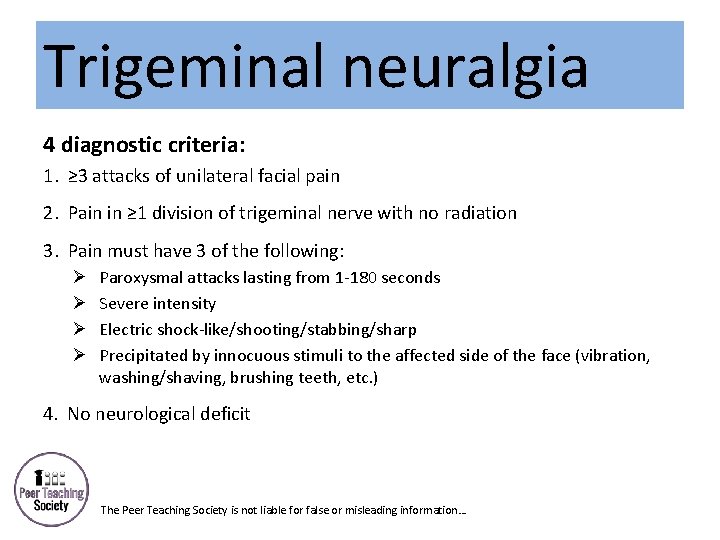
Trigeminal neuralgia 4 diagnostic criteria: 1. ≥ 3 attacks of unilateral facial pain 2. Pain in ≥ 1 division of trigeminal nerve with no radiation 3. Pain must have 3 of the following: Ø Ø Paroxysmal attacks lasting from 1 -180 seconds Severe intensity Electric shock-like/shooting/stabbing/sharp Precipitated by innocuous stimuli to the affected side of the face (vibration, washing/shaving, brushing teeth, etc. ) 4. No neurological deficit The Peer Teaching Society is not liable for false or misleading information…
Trigeminal neuralgia (cont. ) Treatment • 1 st line? Ø Carbamazepine 100 mg • 2 nd and 3 rd line? Ø Lamotrigine, phenytoin or gabapentin Ø Surgery rhizotomy (to deliberately damage nerve), stereotactic radiosurgery, etc. The Peer Teaching Society is not liable for false or misleading information…
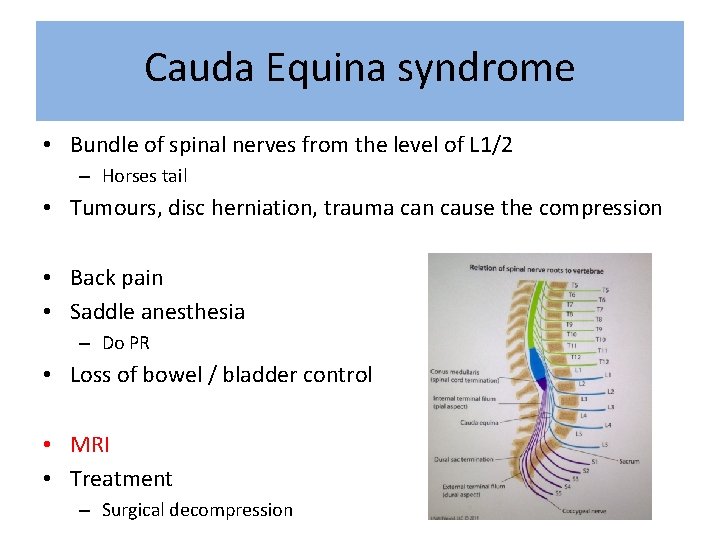
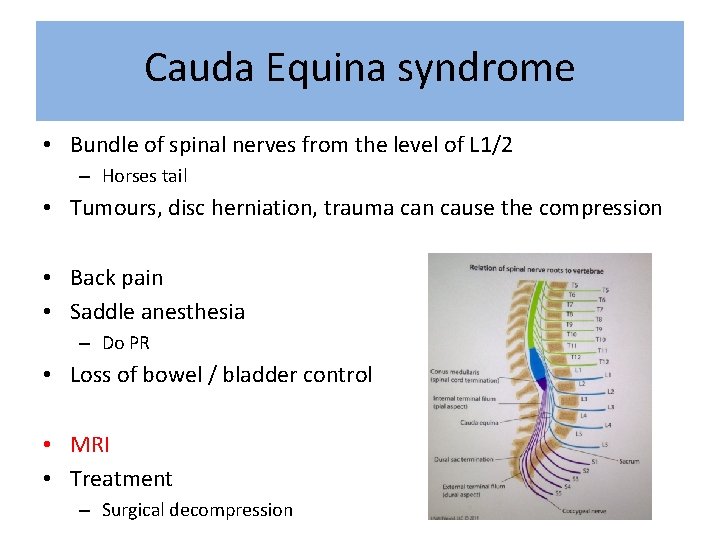
Cauda Equina syndrome • Bundle of spinal nerves from the level of L 1/2 – Horses tail • Tumours, disc herniation, trauma can cause the compression • Back pain • Saddle anesthesia – Do PR • Loss of bowel / bladder control • MRI • Treatment – Surgical decompression
Multiple Sclerosis • Etiology – Chronic autoimmune disorder of the CNS – Plaques of demyelination – Common sites are optic nerves, brainstem, cervical spinal cord • Types – Relapse and remitting – Primary progressive – Secondary progressive
Multiple Sclerosis • Typical patient – Young female – 2 distinct clinical episodes of CNS dysfunction – Remission in a few weeks • Ix – MRI brain and spine – Evoked potentials – LP shows oligoclonal Ig. G bands in CSF
Multiple Sclerosis • Management – Acute • Steroids = Methylprednisolone – Chronic • 1 st line = Beta Interferon, Glatiramer acetate • 2 nd line = Natalizumab – Symptom management • Tremor = BB, Spasticity = Baclofen – PT, OT, MDT
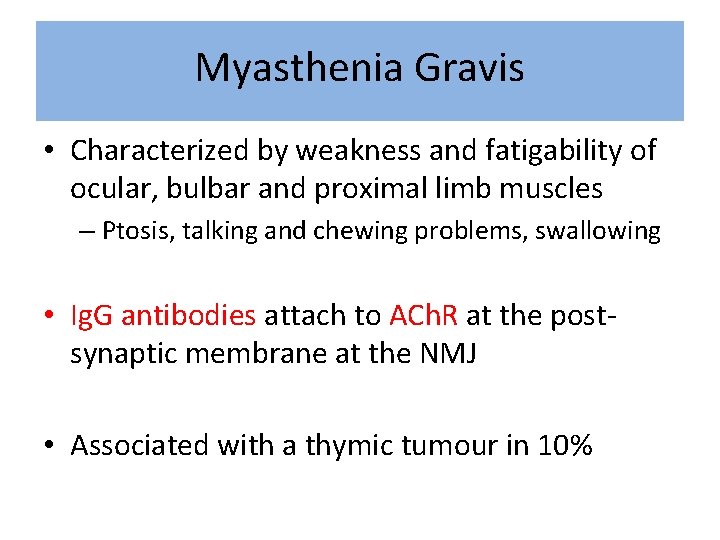
Myasthenia Gravis • Characterized by weakness and fatigability of ocular, bulbar and proximal limb muscles – Ptosis, talking and chewing problems, swallowing • Ig. G antibodies attach to ACh. R at the postsynaptic membrane at the NMJ • Associated with a thymic tumour in 10%
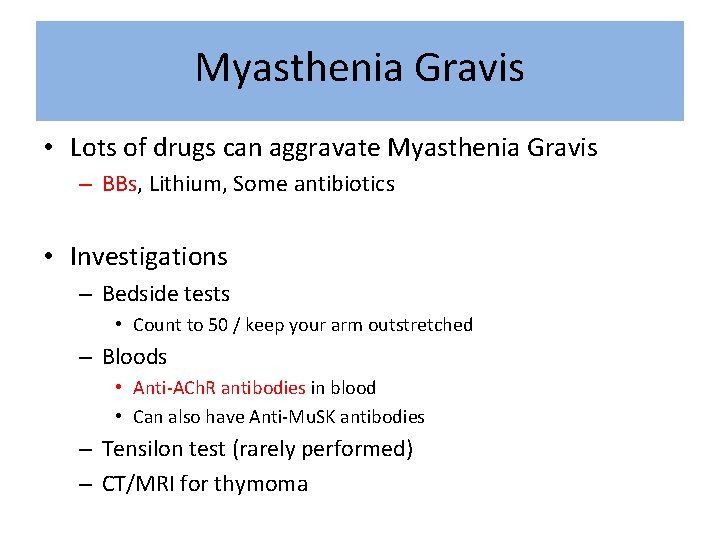
Myasthenia Gravis • Lots of drugs can aggravate Myasthenia Gravis – BBs, Lithium, Some antibiotics • Investigations – Bedside tests • Count to 50 / keep your arm outstretched – Bloods • Anti-ACh. R antibodies in blood • Can also have Anti-Mu. SK antibodies – Tensilon test (rarely performed) – CT/MRI for thymoma
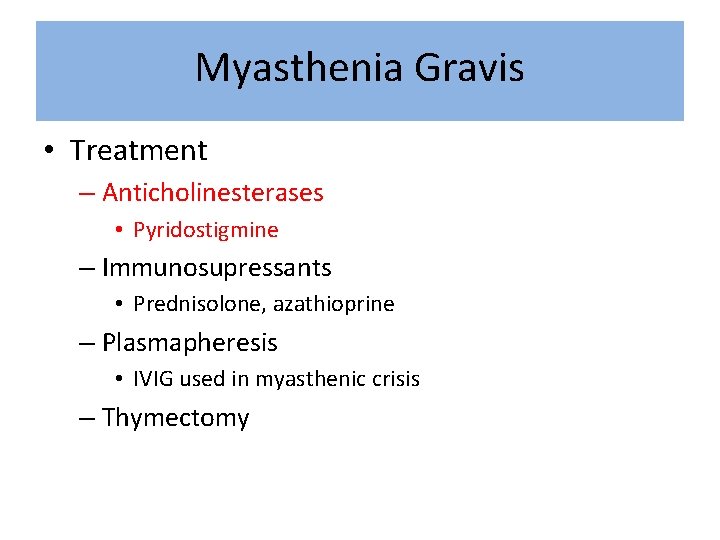
Myasthenia Gravis • Treatment – Anticholinesterases • Pyridostigmine – Immunosupressants • Prednisolone, azathioprine – Plasmapheresis • IVIG used in myasthenic crisis – Thymectomy
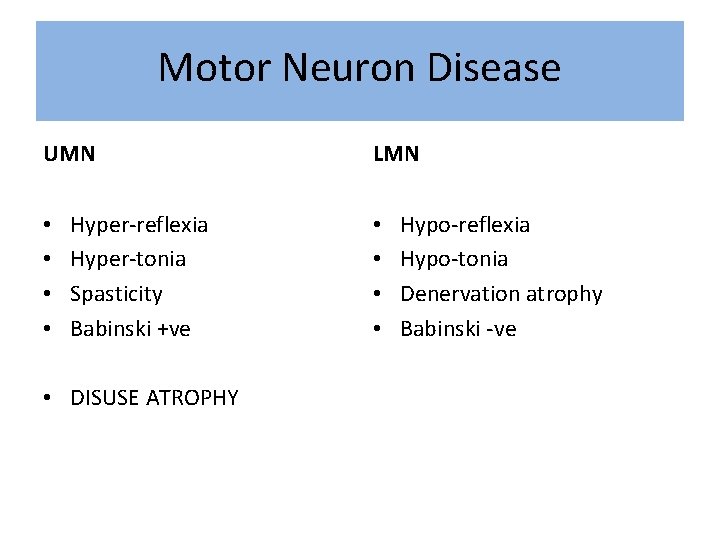
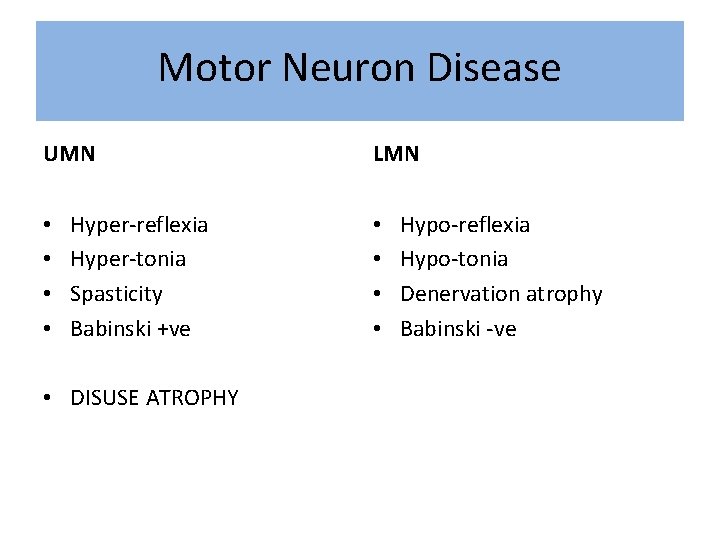
Motor Neuron Disease UMN • • Hyper-reflexia Hyper-tonia Spasticity Babinski +ve • DISUSE ATROPHY LMN • • Hypo-reflexia Hypo-tonia Denervation atrophy Babinski -ve
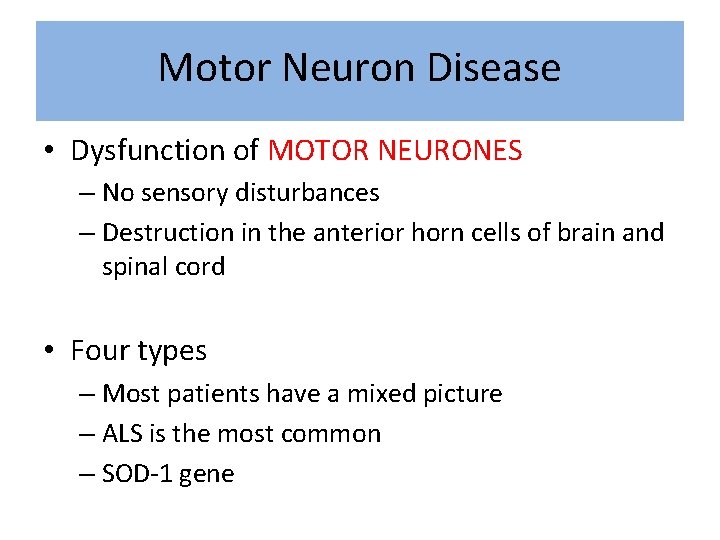
Motor Neuron Disease • Dysfunction of MOTOR NEURONES – No sensory disturbances – Destruction in the anterior horn cells of brain and spinal cord • Four types – Most patients have a mixed picture – ALS is the most common – SOD-1 gene
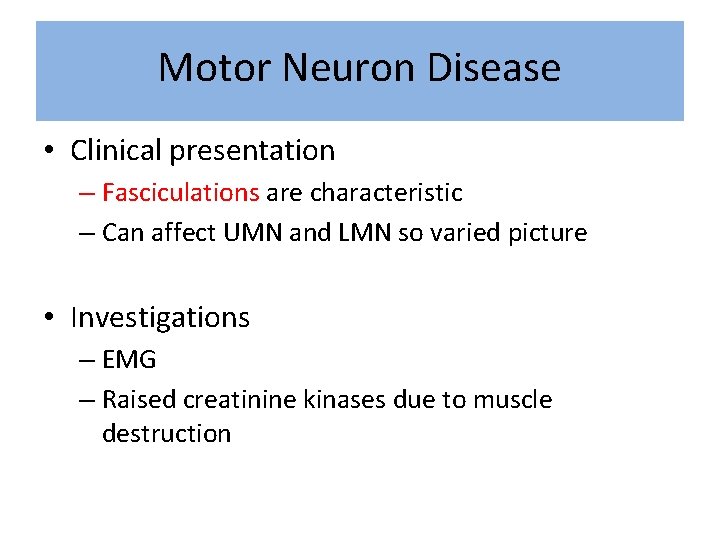
Motor Neuron Disease • Clinical presentation – Fasciculations are characteristic – Can affect UMN and LMN so varied picture • Investigations – EMG – Raised creatinine kinases due to muscle destruction
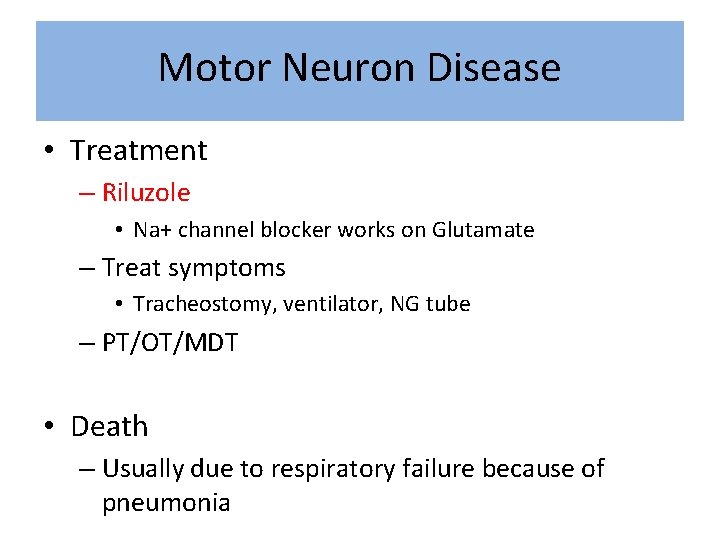
Motor Neuron Disease • Treatment – Riluzole • Na+ channel blocker works on Glutamate – Treat symptoms • Tracheostomy, ventilator, NG tube – PT/OT/MDT • Death – Usually due to respiratory failure because of pneumonia
Guillain Barre -syndrome • ACUTE neuropathy • Inflammatory and demyelinating • Triggered by infection – Campylobacter Jejuni, EBV, CMV
Guillain Barre -syndrome • Progressive onset of limb weakness after viral illness • Loss of reflexes • Often sensory and motor disturbances • Vary from mild to severe – Severe can cause respiratory depression – Vital capacity should be monitored if suspected
Guillain Barre -syndrome • Investigations – Mainly a clinical diagnosis – Nerve conduction studies – LP shows high protein in CSF • Treatment – IVIG – Ventilation is respiratory muscles involved
Peripheral neuropathies • Mononeuropathies = one nerve – Median, Radial, Sciatic, Common Peroneal • Polyneuropathies = multiple nerves – DAVID • • • Diabetes Alcohol Vitamin deficiency (B 12) Infective (GB) Drugs (isoniazid)
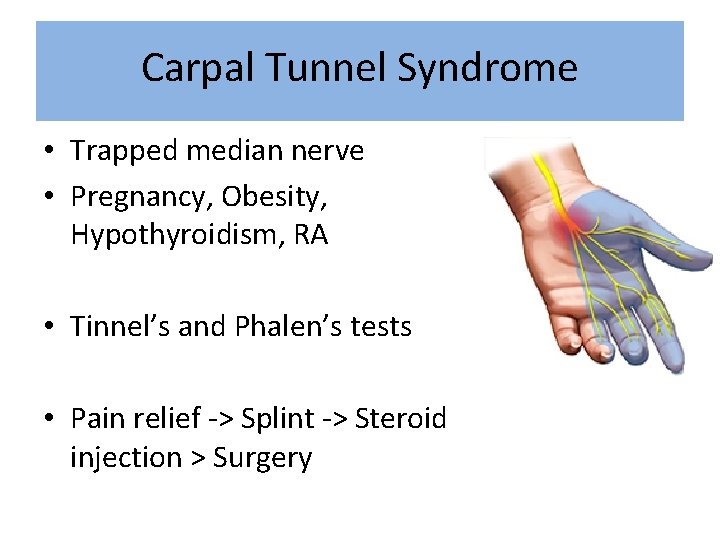
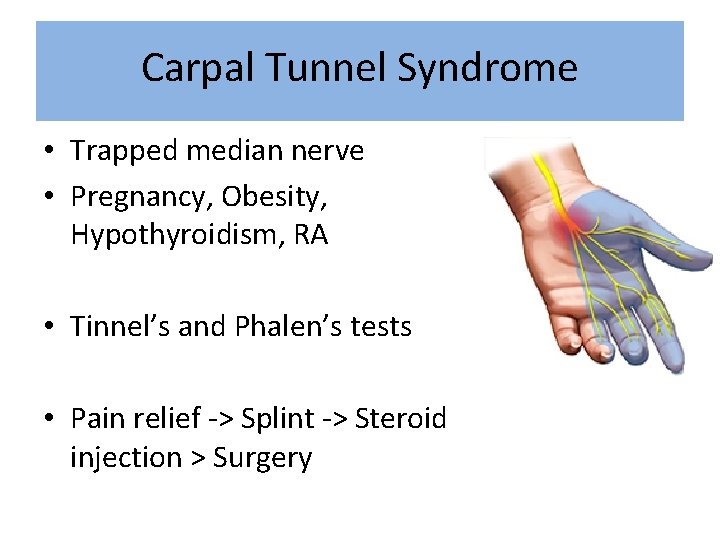
Carpal Tunnel Syndrome • Trapped median nerve • Pregnancy, Obesity, Hypothyroidism, RA • Tinnel’s and Phalen’s tests • Pain relief -> Splint -> Steroid injection > Surgery
Meningitis • Inflammation of the meninges – Neck stiffness, headache, photophobia • Can be viral or bacterial – Viral is often self-limiting • HSV, EBV, HIV, Mumps The Peer Teaching Society is not liable for false or misleading information…
Bacterial Meningitis • Bacterial is medical emergency – Neisseria meningitides – Streptococcus pneumonia – Listeria monocytogenes • Inflammation of the meninges – Neck stiffness, headache, photophobia • Fever , +ve kernig’s sign, • Non-blanching rash = meningococcal septicaemia The Peer Teaching Society is not liable for false or misleading information…
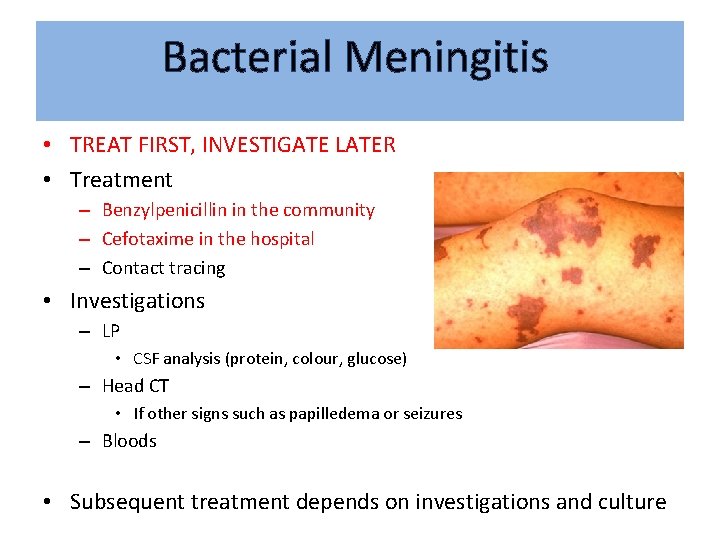
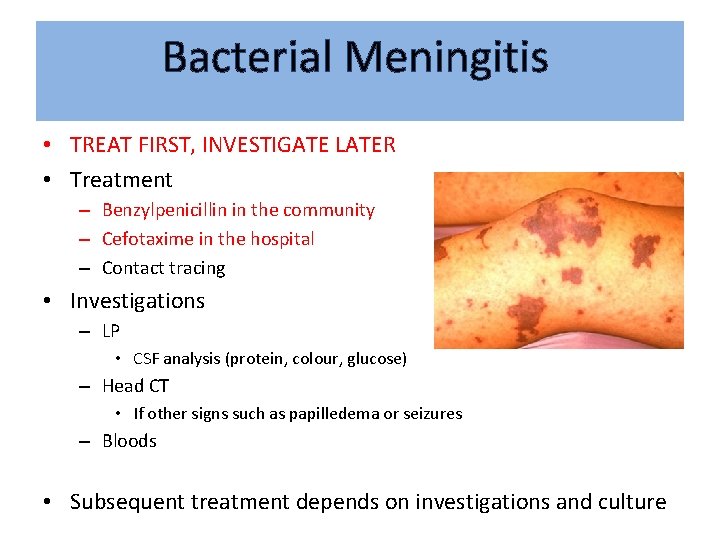
Bacterial Meningitis • TREAT FIRST, INVESTIGATE LATER • Treatment – Benzylpenicillin in the community – Cefotaxime in the hospital – Contact tracing • Investigations – LP • CSF analysis (protein, colour, glucose) – Head CT • If other signs such as papilledema or seizures – Bloods • Subsequent treatment depends on investigations and culture
Encephalitis • Infection of the actual brain parenchyma • Unlike meningitis, cerebral function is often altered – Can still get meningeal signs and symptoms though • Can be viral or bacterial – Herpes Simplex Virus is dangerous – Treat with high dose I. V acyclovir The Peer Teaching Society is not liable for false or misleading information…
Herpes Zoster • Initial infection of Herpes Zoster = chicken pox • Reactivation = shingles • Varicella lies dormant in the DRG • RFs for reactivation – Old age, poor immune system, chickenpox < 18 months age • Dermatomal distribution of rash and pain • Give oral acyclovir
Other things to go over… • • Spinal tracts Syphillis Brain Tumours Neuro-anatomy – Basal ganglia
Exam Qs 2016 SAQ: • Dense hemiparesis and aphasia (focus on psychosocial aspects) SBA: • Inhibitory neurotransmitter – GABA • Neurotransmitters of ANS – acetylcholine? • Microorganism causing meningitis • Nerves of the hand • Visual pathways • Initiation and control of ongoing voluntary movements The Peer Teaching Society is not liable for false or misleading information…
Top Tips • LECTURES • PAST PAPERS


 Amogh dhamdhere
Amogh dhamdhere Passive progressive
Passive progressive In a ∆-connected source feeding a y-connected load
In a ∆-connected source feeding a y-connected load Normal phase vs reverse phase chromatography
Normal phase vs reverse phase chromatography Normal phase vs reverse phase chromatography
Normal phase vs reverse phase chromatography Csce 441
Csce 441 Tswett pronunciation
Tswett pronunciation Phase to phase voltage
Phase to phase voltage Mobile phase and stationary phase
Mobile phase and stationary phase Which detector used in hplc
Which detector used in hplc Hplc definition
Hplc definition Nlff neurology
Nlff neurology Tufts anesthesia residency
Tufts anesthesia residency Dr raeburn
Dr raeburn Duplex ultrasound vs doppler
Duplex ultrasound vs doppler Vanderbilt neurology residents
Vanderbilt neurology residents Monomyth amplification
Monomyth amplification Nheent
Nheent Neurology
Neurology Nlff neurology
Nlff neurology Crude touch
Crude touch Qmc neurology
Qmc neurology Dr robert layzer
Dr robert layzer Mayzent fdo
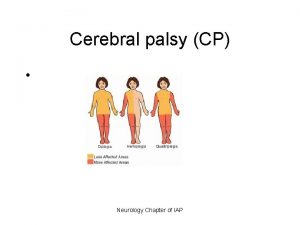
Mayzent fdo Cerebral palsy iap
Cerebral palsy iap Umass memorial pharmacy residency
Umass memorial pharmacy residency Oregon neurology associates
Oregon neurology associates Nex exam neurology
Nex exam neurology Uf neurology residents
Uf neurology residents The walton centre for neurology and neurosurgery
The walton centre for neurology and neurosurgery Joseph berger md neurology
Joseph berger md neurology Nbme shelf exam percentiles
Nbme shelf exam percentiles Neurology near loomis
Neurology near loomis Midwest neurology
Midwest neurology Mppd unhas
Mppd unhas Mary bridge pediatric neurology
Mary bridge pediatric neurology Motor strength scale
Motor strength scale Midwest neurology
Midwest neurology Contrallateral
Contrallateral Ece 310
Ece 310 Gate.aon/candidate
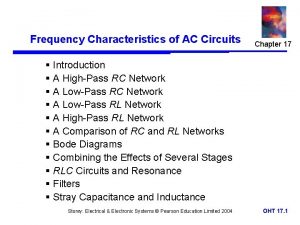
Gate.aon/candidate Solved: ph dincussion ac circuits session 12 q2. low-pass
Solved: ph dincussion ac circuits session 12 q2. low-pass Interactive session poster
Interactive session poster Speaker title
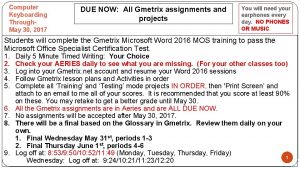
Speaker title Word 2016 session 2 post assessment
Word 2016 session 2 post assessment Types of social change
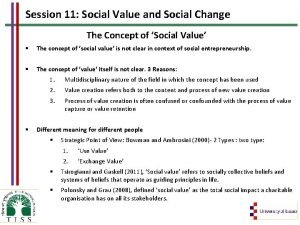
Types of social change Ergonomics session
Ergonomics session Rails session model
Rails session model Coaching session agenda
Coaching session agenda Wemba wharton
Wemba wharton Ece 313 uiuc
Ece 313 uiuc Welcome to new session 2020-21
Welcome to new session 2020-21 Horizontal line
Horizontal line Session will start soon
Session will start soon .net 5 session
.net 5 session Session tracking in servlet
Session tracking in servlet Balabit pricing
Balabit pricing Ucsd summer session
Ucsd summer session Alpha session 8
Alpha session 8 Explanation
Explanation Session jo
Session jo First cbt session structure
First cbt session structure Listening sessions for employees
Listening sessions for employees Personal trainers: session 2
Personal trainers: session 2 Alpha session 2
Alpha session 2 Jsf redirect page
Jsf redirect page Practical session meaning
Practical session meaning Pdp staff
Pdp staff