Pediatric Seizures Jeffrey Frank Child Neurology Oregon Neurology




- Slides: 32
Pediatric Seizures Jeffrey Frank Child Neurology Oregon Neurology Associates
Disclosure • I do not have a financial interest, arrangement or affiliation with any organizations that could be perceived as a real or apparent conflict of interest in the context of the subject of this presentation.
Seizures Historically • Ancient Babylonia – Miqtu – “the falling disease” – If a person loses consciousness and foams at the mouth, it is Miqtu – ‘to possess’ • Ghosts and demons
Seizures Historically • Hippocrates – Not a sacred disease – First to describe epilepsy as a brain disorder • The Falling Sickness • Shakespeare – Epilepsy – Othello 1603 – Epilepsia • to seize • to be taken hold of
Seizure • Old French ‘seisir’ – to take possession by force • Popular – sudden and severe event • Medically – transient occurrence of signs and/or symptoms due to abnormal, excessive or synchronous neuronal activity in the brain – Epileptic Seizure
Epilepsy • Historical - Two or more unprovoked seizures • ILAE 2005 - disorder of the brain characterized by an enduring predisposition to generate epileptic seizures and by the neurobiologic, cognitive, psychological, and social consequences of this condition. The definition of epilepsy requires the occurrence of at least one epileptic seizure
Epilepsy • At least two unprovoked (or reflex) seizures occurring greater than 24 hours apart. • One unprovoked (or reflex) seizure and a probability of further seizures similar to the general recurrence risk (at least 60%) after two unprovoked seizures, occurring over the next 10 years. • Diagnosis of an epilepsy syndrome – Epilepsy is considered to be resolved for individuals who had an age-dependent epilepsy syndrome but are now past the applicable age or those who have remained seizure-free for the last 10 years, with no seizure medicines for the last 5 years.
Seizure? • Popular – sudden and severe event • Medical – Epileptic seizure • Synchronous neuronal activity – Nonepileptic seizure
Nonepileptic Seizures • Psychogenic – Psychologically induced – Behavioral episode • Nonpsychogenic – “Organic” but not of epileptic origin
Nonpsychogenic • • “Organic” Typically not responsive to anticonvulsants May still be stereotyped Any age
Nonepileptic Childhood Events
Breath Holding Spells • Typically 6 mos to 2 yrs – Can extend to 5 -6 years • • • Provoked Gasp Apnea Pallor/cyanosis Altered sensorium, stupor or syncope Twitches or jerking movements Breathing returns after syncope Child typically recovers quickly

Benign Sleep Myoclonus • • Sudden, quick, jerk-like movement In sleep Not rhythmical Patient can be woken
Stereotypies • • Rigidly, repetitive and invariable Inappropriate in nature Head Banging Hand Flapping Body Rocking Toe Walking Echolalia
Benign Paroxysmal Vertigo • Sudden onset dizziness or ataxia – Can be provoked by vestibular stimulation • Typically lasts minutes – Can last up to 2 days • May act very scared • Often hold on to people/objects • May be accompanied by headache
Non Epileptic All Ages
Migraine Variants • • Hemiplegia Loss of vision Aphasia / slurred speech Confusion Fluctuating consciousness Visual auras Vertigo
Syncope • Often preceded by symptoms – Dizziness, darkening vision, weakness • • • Loss of tone / Limp Pallor / Cyanosis Eyes closed May have convulsive mvmts Lucid on wakening
Tics • Stereotyped • Multiple versions – Motor or Vocal • Suppressible • Can be complex
“Normal” Behavior • Daydreaming • Sleep • Confusional Arousal
Epileptic Seizures • Stereotyped complex movements – May be focal or generalized – Though student may have multiple types – Evolution • Paroxysmal – Clear beginning and end • Involuntary / Uncontrollable • Not distractible / interruptible • Post-ictal phase

Generalized Seizure Types • Generalized Tonic Clonic – ‘Grand Mal’ • Tonic Seizure – Stiffening • Myoclonic Seizure – Jerk-like movements • Atonic – Sudden loss of postural tone • Absence – ‘Petit mal’

Focal Seizure Types • Focal Motor seizure – Sustained, rhythmical movements – May progress, migrate or generalize • Clonic – Jerking movements • Complex Partial – Alteration of awareness – Staring • Autonomic
Psychogenic Nonepileptic • “Pseudoseizure” • Psychological / Psychiatric / Behavioral – Subconscious/unconscious symptoms • Somatization Disorder • Conversion – Conscious • Factitious • Malingering – Anxiety
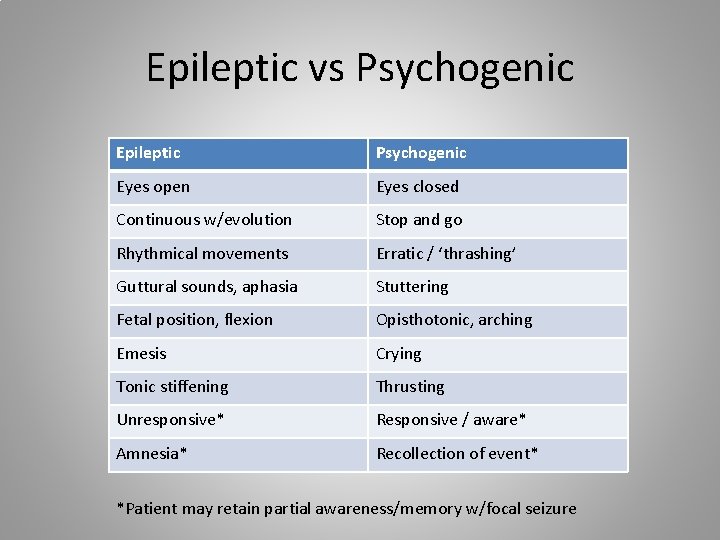
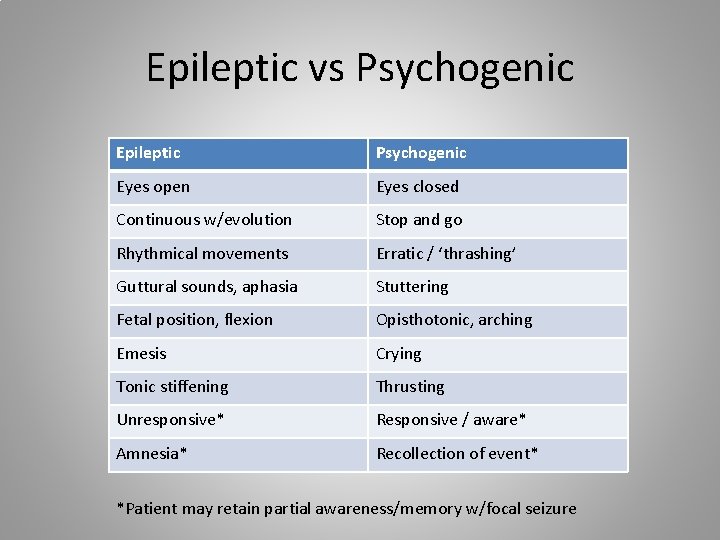
Epileptic vs Psychogenic Epileptic Psychogenic Eyes open Eyes closed Continuous w/evolution Stop and go Rhythmical movements Erratic / ‘thrashing’ Guttural sounds, aphasia Stuttering Fetal position, flexion Opisthotonic, arching Emesis Crying Tonic stiffening Thrusting Unresponsive* Responsive / aware* Amnesia* Recollection of event* *Patient may retain partial awareness/memory w/focal seizure
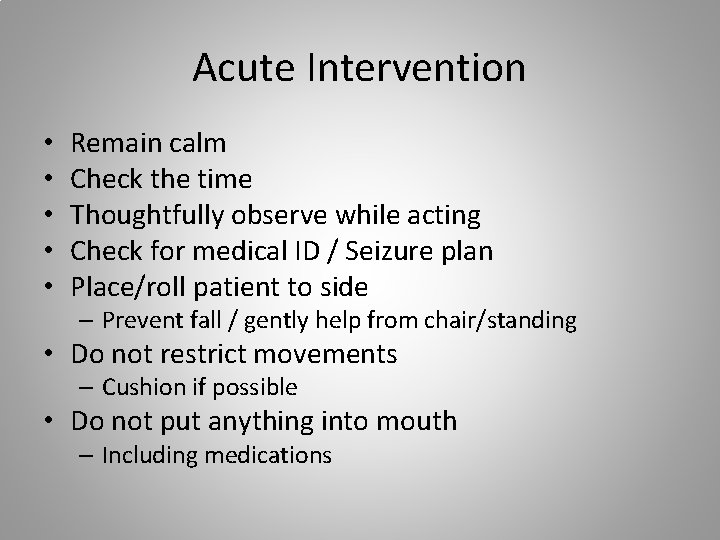
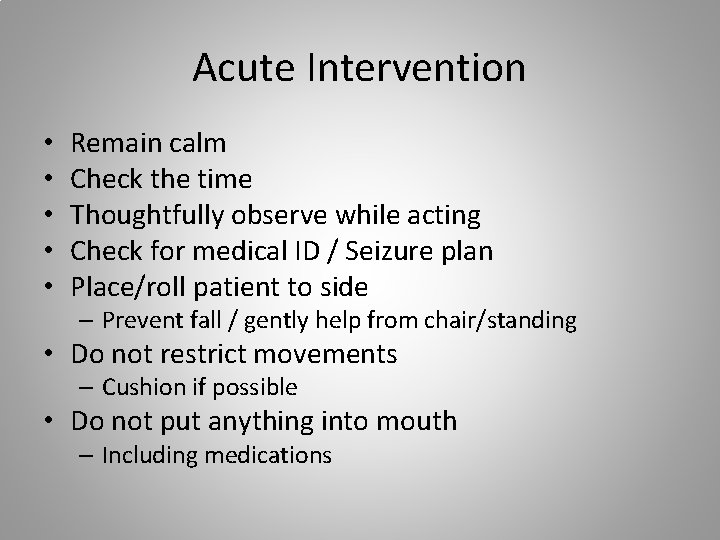
Acute Intervention • • • Remain calm Check the time Thoughtfully observe while acting Check for medical ID / Seizure plan Place/roll patient to side – Prevent fall / gently help from chair/standing • Do not restrict movements – Cushion if possible • Do not put anything into mouth – Including medications
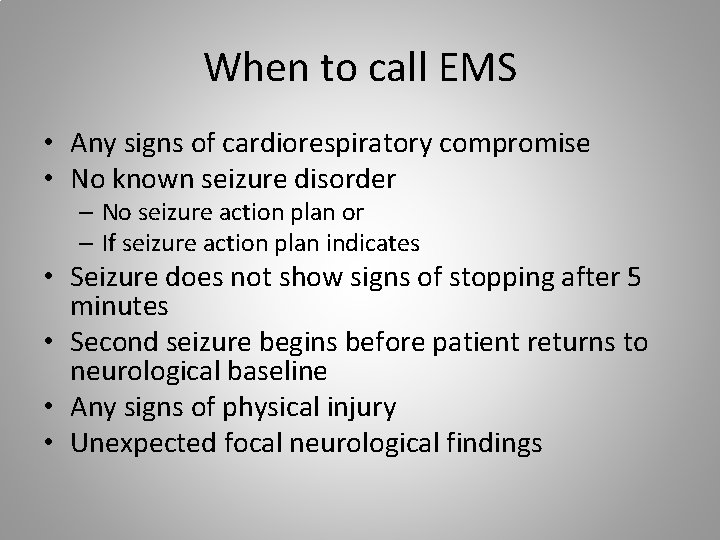
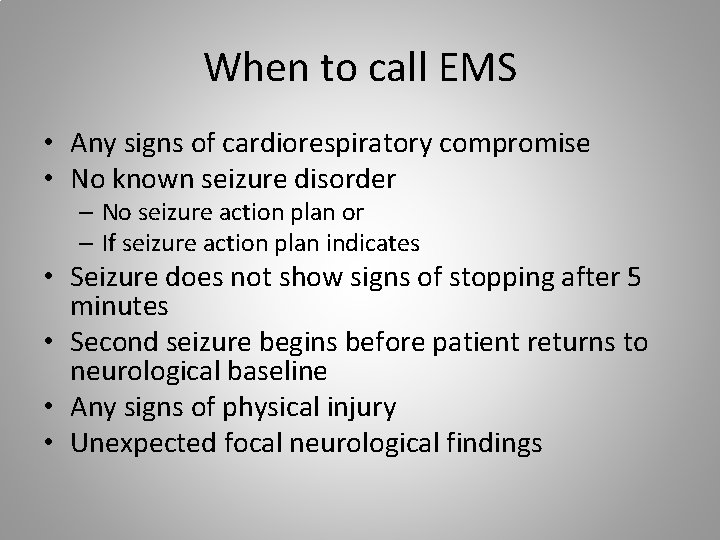
When to call EMS • Any signs of cardiorespiratory compromise • No known seizure disorder – No seizure action plan or – If seizure action plan indicates • Seizure does not show signs of stopping after 5 minutes • Second seizure begins before patient returns to neurological baseline • Any signs of physical injury • Unexpected focal neurological findings

After the Seizure • Document details of seizure – Time of onset – Length – Description of movements, evolution – Triggers? – Post-ictal phase? – Awareness/responsiveness?
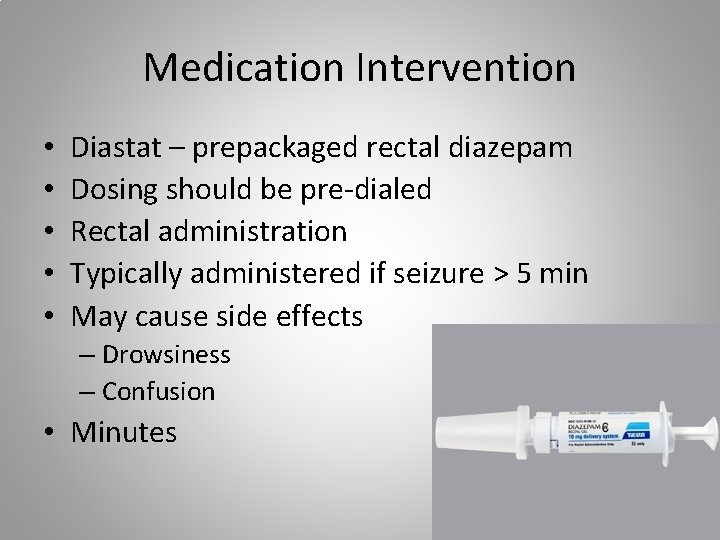
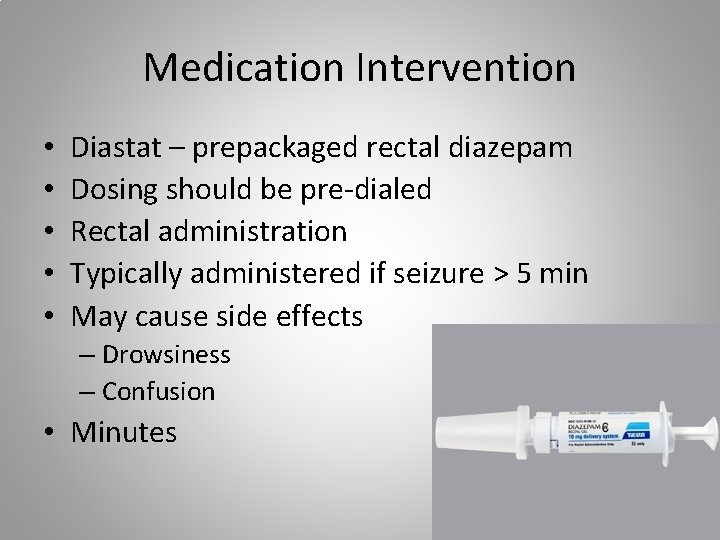
Medication Intervention • • • Diastat – prepackaged rectal diazepam Dosing should be pre-dialed Rectal administration Typically administered if seizure > 5 min May cause side effects – Drowsiness – Confusion • Minutes
Intranasal Midazolam • • May need to be drawn up ½ total dose in each nostril Typically for seizure > 5 min May cause side effects – Drowsiness – Confusion • Minutes
Oral Medications • Rarely used • Not to be given during seizure effective consciousness / swallowing ability • May have role for cluster of events
Home? • No EMS criteria • Rapidly / progressively recovering • No known triggers – Missed doses – Intercurrent illness / fever – Sleep deprived • No history of clusters
 Pediatric seizures
Pediatric seizures Mary bridge neurology
Mary bridge neurology Miqtu
Miqtu Definition of sick child ppt
Definition of sick child ppt Psychomotor seizures
Psychomotor seizures Seizures
Seizures Seizure meaning
Seizure meaning Ptsd seizures
Ptsd seizures Psychomotor seizures
Psychomotor seizures Tonic-clonic seizures
Tonic-clonic seizures Types of febrile seizures
Types of febrile seizures Seizures and tremors
Seizures and tremors Abdominal ultrasound scan glasgow
Abdominal ultrasound scan glasgow Tonic vs clonic
Tonic vs clonic Simple partial seizures vs complex
Simple partial seizures vs complex Basic mechanisms underlying seizures and epilepsy
Basic mechanisms underlying seizures and epilepsy Nursing management of encephalitis
Nursing management of encephalitis Non epileptic seizures
Non epileptic seizures What is a seizure
What is a seizure Frank william abagnale jr wife
Frank william abagnale jr wife 전위 순회
전위 순회 Neurology
Neurology Nlff neurology
Nlff neurology Dr raeburn forbes
Dr raeburn forbes Neurology strength scale
Neurology strength scale Uf neurology residents
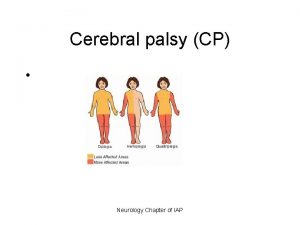
Uf neurology residents Cerebral palsy iap
Cerebral palsy iap Nheent
Nheent West coast neurology
West coast neurology Neurology near loomis
Neurology near loomis Nin bajaj
Nin bajaj Williamson medical center pharmacy residency
Williamson medical center pharmacy residency Midwest neurology
Midwest neurology