Neurology Neurology Phase 1 Revision Session Gemma Morgan

- Slides: 57
Neurology
Neurology Phase 1 Revision Session Gemma Morgan and Lucy Ryder 27/03/17 The Peer Teaching Society is not liable for false or misleading information…
Case 1 • 77 yr old male • Sudden onset weakness in left arm, slurred speech and L sided facial droop • Resolved in 5 mins • Smokes 20/day for 40 years Most likely diagnosis? The Peer Teaching Society is not liable for false or misleading information…
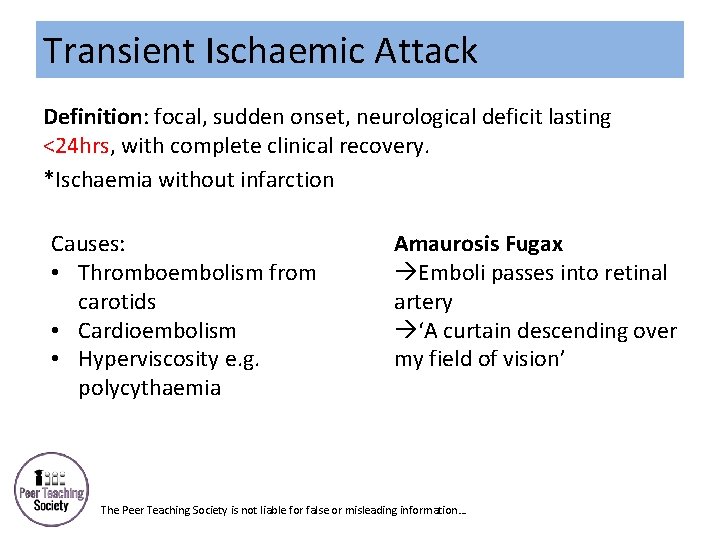
Transient Ischaemic Attack Definition: focal, sudden onset, neurological deficit lasting <24 hrs, with complete clinical recovery. *Ischaemia without infarction Causes: • Thromboembolism from carotids • Cardioembolism • Hyperviscosity e. g. polycythaemia Amaurosis Fugax Emboli passes into retinal artery ‘A curtain descending over my field of vision’ The Peer Teaching Society is not liable for false or misleading information…
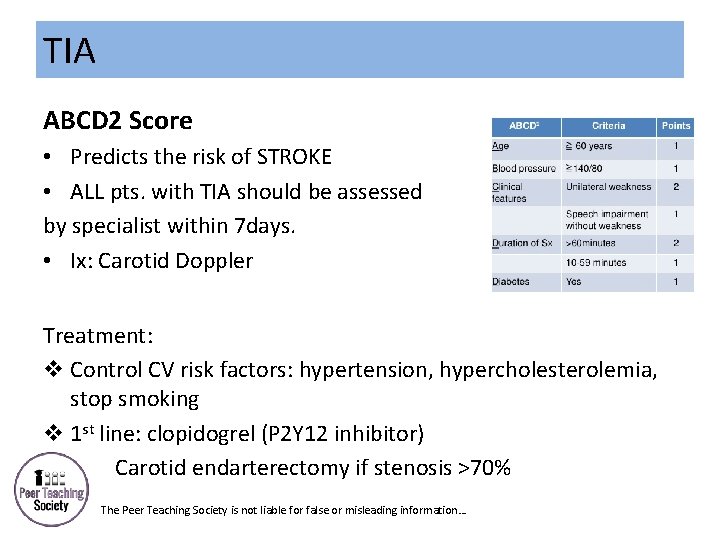
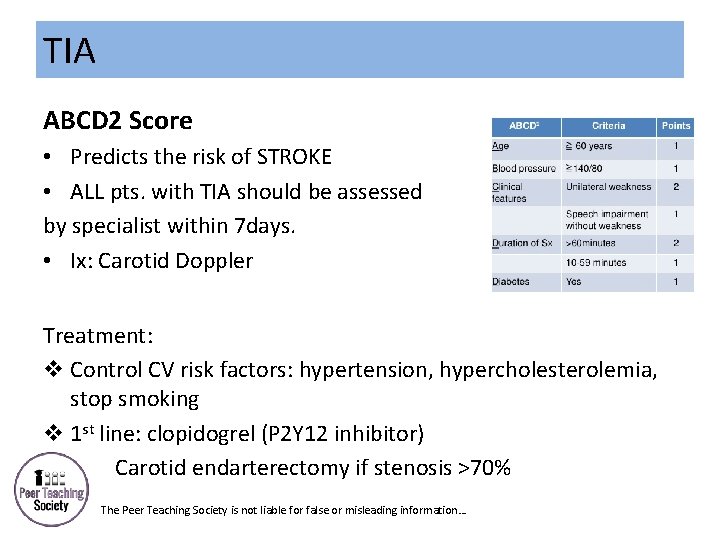
TIA ABCD 2 Score • Predicts the risk of STROKE • ALL pts. with TIA should be assessed by specialist within 7 days. • Ix: Carotid Doppler Treatment: v Control CV risk factors: hypertension, hypercholesterolemia, stop smoking v 1 st line: clopidogrel (P 2 Y 12 inhibitor) v Carotid endarterectomy if stenosis >70% The Peer Teaching Society is not liable for false or misleading information…
Case 2 • 80 yr old female • Sudden onset R arm weakness, sensory loss in R arm, difficulty speaking and swallowing • Present for >5 hrs with no improvement • PMH: AF, Hypertension, Diabetes Most likely diagnosis? On which side of the brain? Most likely occluded artery? The Peer Teaching Society is not liable for false or misleading information…
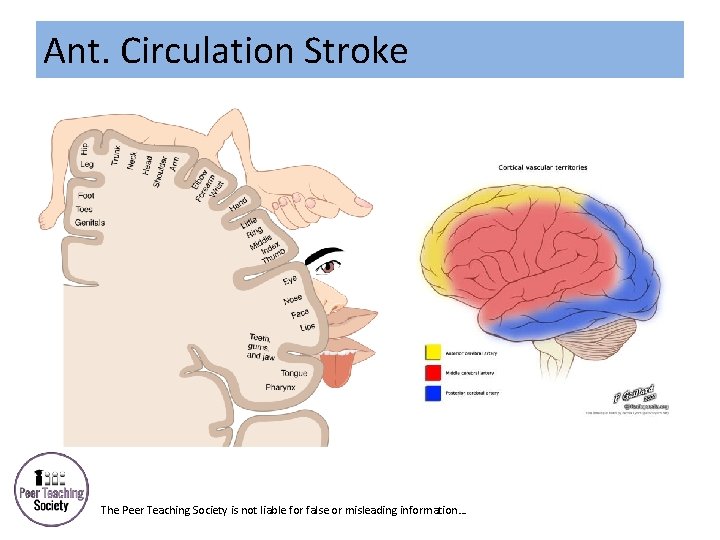
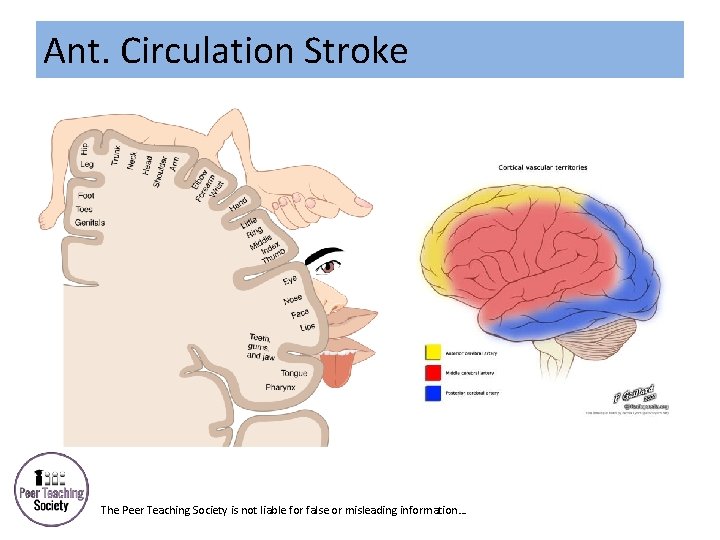
Ant. Circulation Stroke The Peer Teaching Society is not liable for false or misleading information…
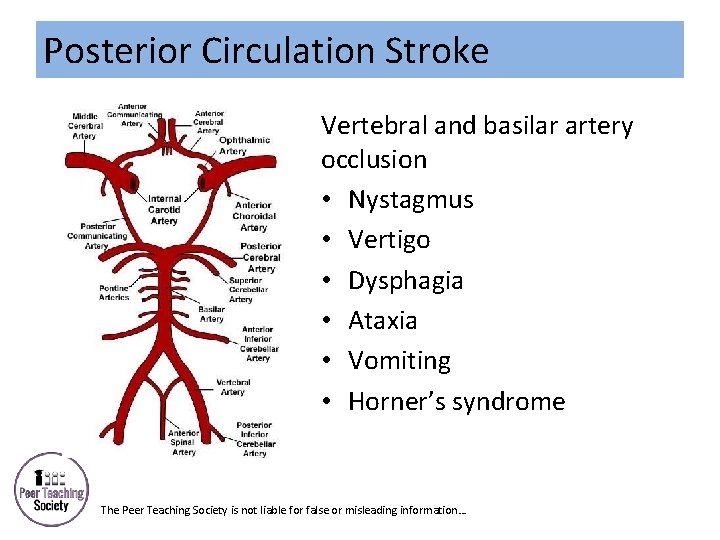
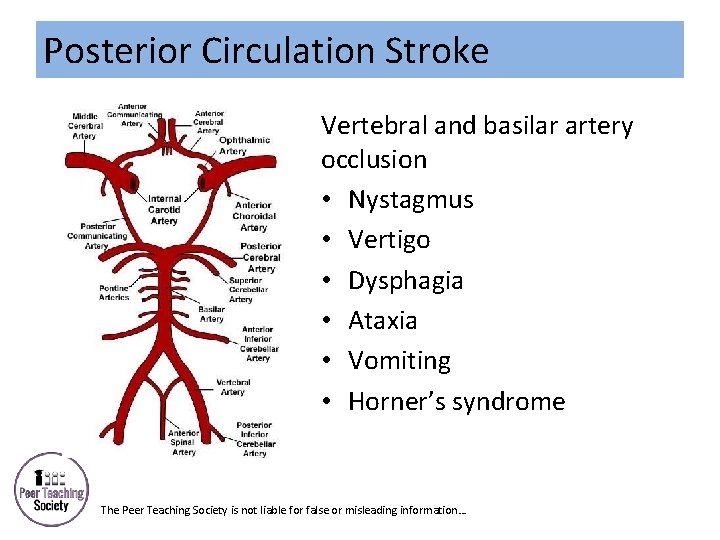
Posterior Circulation Stroke Vertebral and basilar artery occlusion • Nystagmus • Vertigo • Dysphagia • Ataxia • Vomiting • Horner’s syndrome The Peer Teaching Society is not liable for false or misleading information…
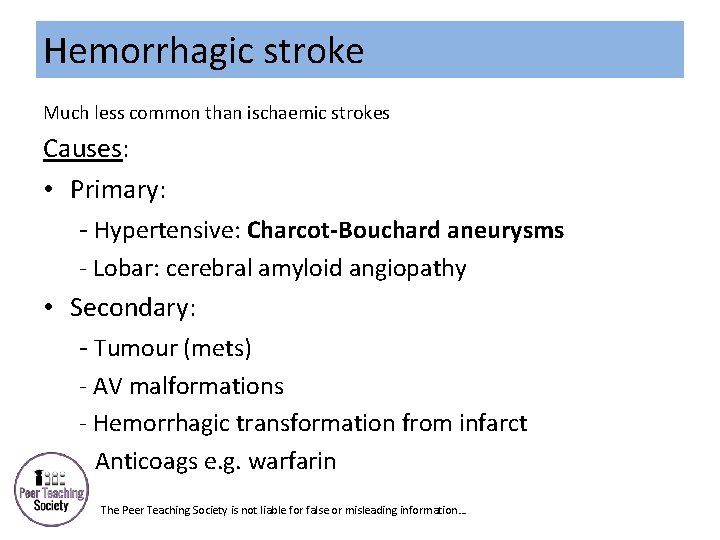
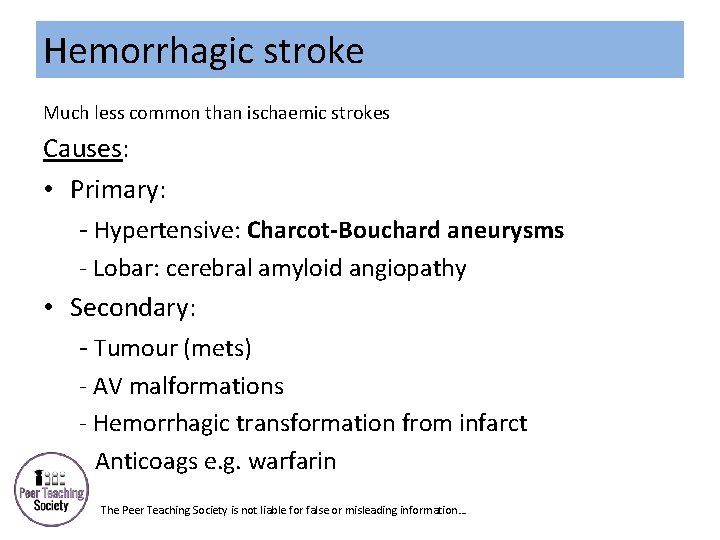
Hemorrhagic stroke Much less common than ischaemic strokes Causes: • Primary: - Hypertensive: Charcot-Bouchard aneurysms - Lobar: cerebral amyloid angiopathy • Secondary: - Tumour (mets) - AV malformations - Hemorrhagic transformation from infarct --Anticoags e. g. warfarin The Peer Teaching Society is not liable for false or misleading information…
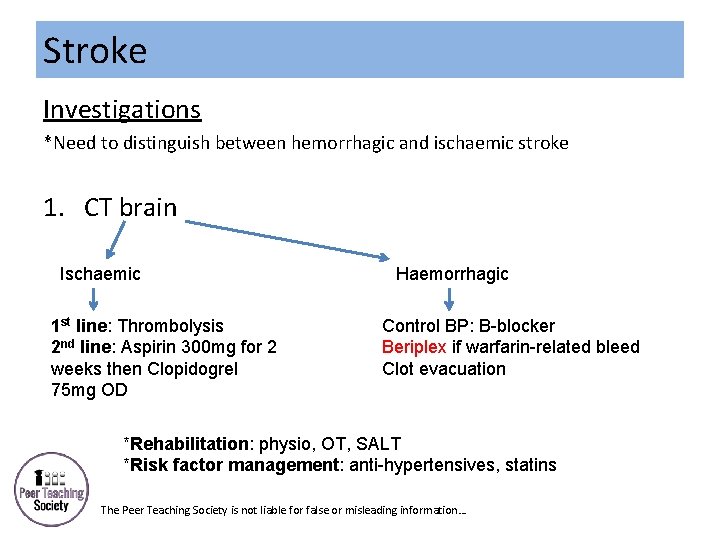
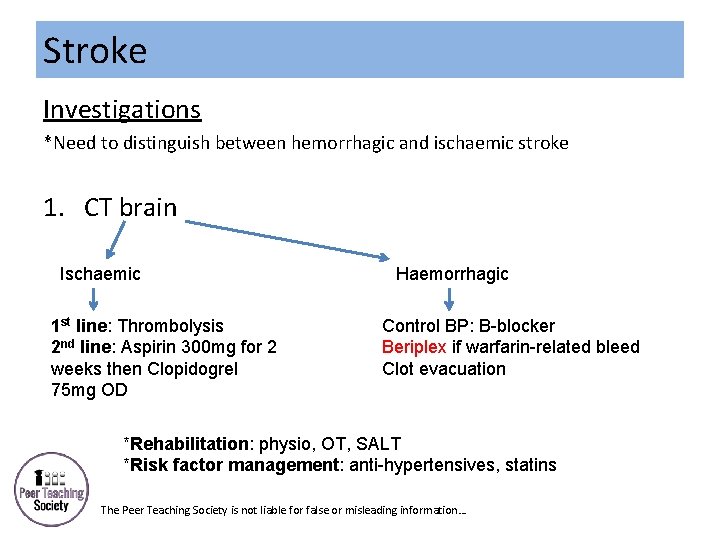
Stroke Investigations *Need to distinguish between hemorrhagic and ischaemic stroke 1. CT brain Ischaemic 1 st line: Thrombolysis 2 nd line: Aspirin 300 mg for 2 weeks then Clopidogrel 75 mg OD Haemorrhagic Control BP: B-blocker Beriplex if warfarin-related bleed Clot evacuation *Rehabilitation: physio, OT, SALT *Risk factor management: anti-hypertensives, statins The Peer Teaching Society is not liable for false or misleading information…
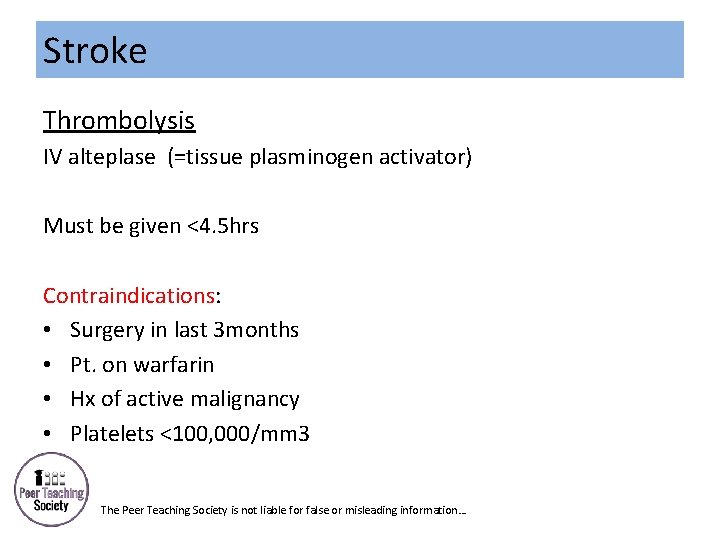
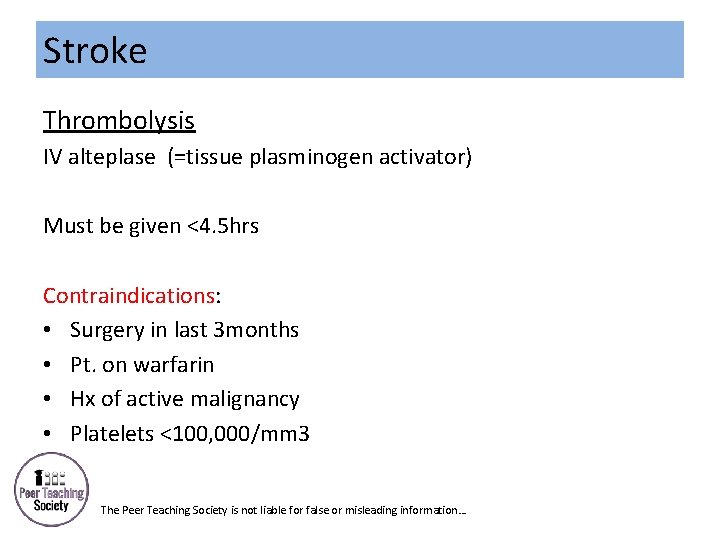
Stroke Thrombolysis IV alteplase (=tissue plasminogen activator) Must be given <4. 5 hrs Contraindications: • Surgery in last 3 months • Pt. on warfarin • Hx of active malignancy • Platelets <100, 000/mm 3 The Peer Teaching Society is not liable for false or misleading information…
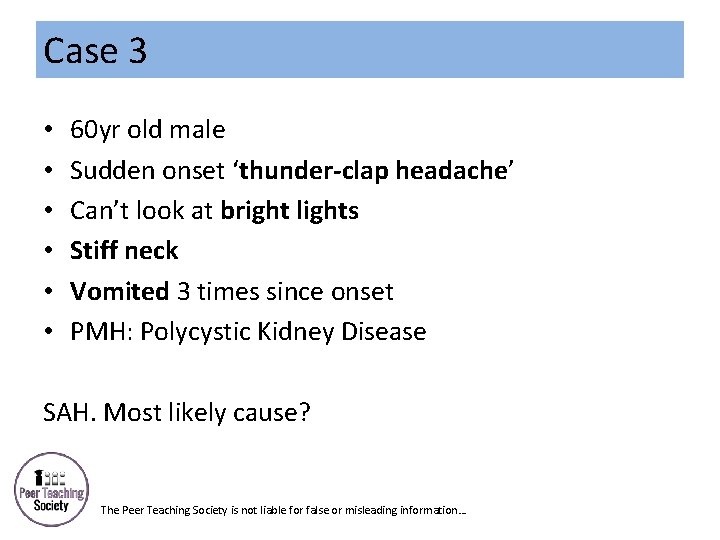
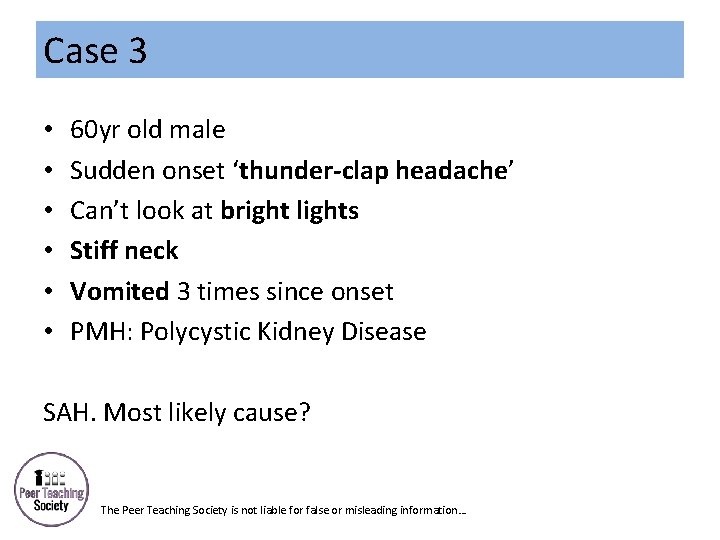
Case 3 • • • 60 yr old male Sudden onset ‘thunder-clap headache’ Can’t look at bright lights Stiff neck Vomited 3 times since onset PMH: Polycystic Kidney Disease SAH. Most likely cause? The Peer Teaching Society is not liable for false or misleading information…
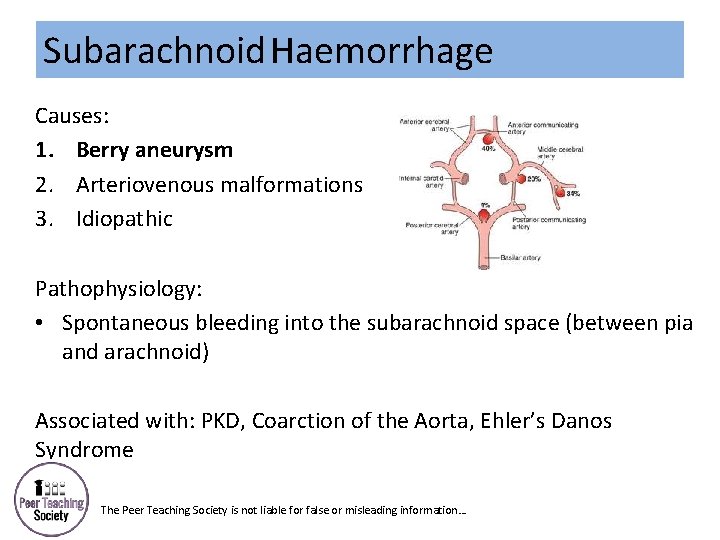
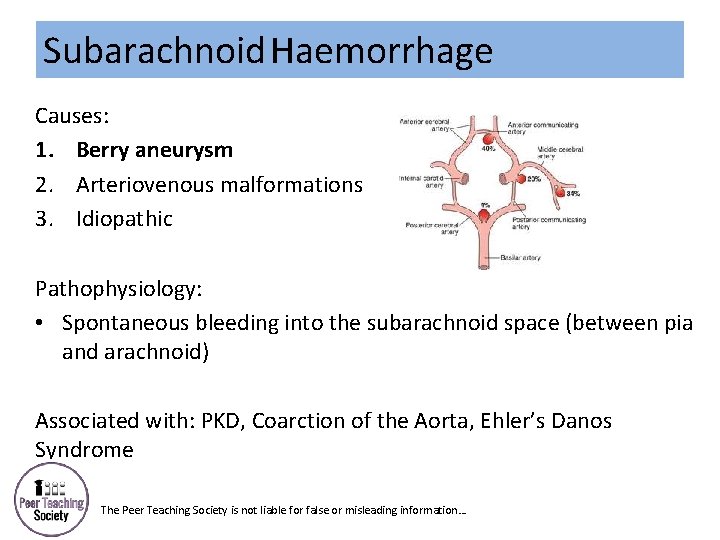
Subarachnoid Haemorrhage Causes: 1. Berry aneurysm 2. Arteriovenous malformations 3. Idiopathic Pathophysiology: • Spontaneous bleeding into the subarachnoid space (between pia and arachnoid) Associated with: PKD, Coarction of the Aorta, Ehler’s Danos Syndrome The Peer Teaching Society is not liable for false or misleading information…
Subarachnoid Haemorrhage Symptoms: • Sudden onset severe headache • Loss of consciousness • Photophobia • Seizures • Nausea + vomiting Sentinel headache: prodromal headache (small leak before rupture) Signs: +ve signs of meningism: Kernig’s sign, neck stiffness The Peer Teaching Society is not liable for false or misleading information…
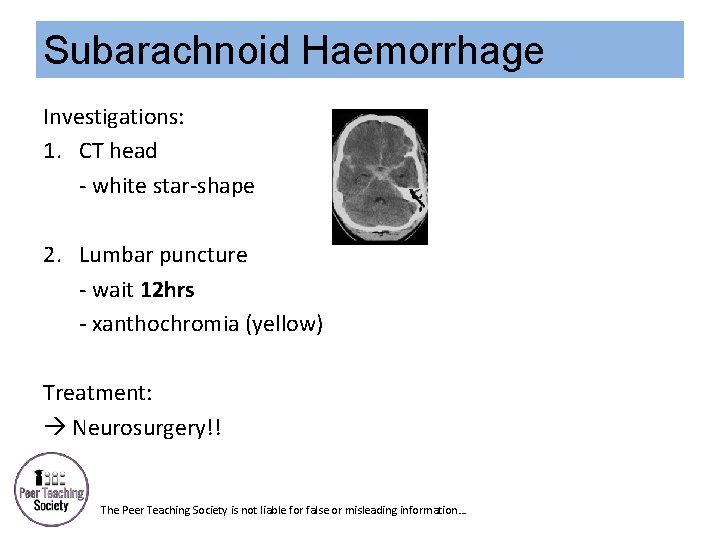
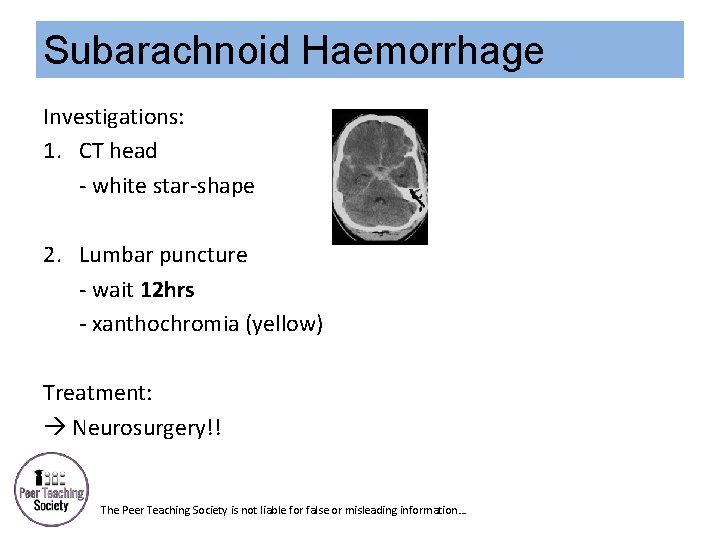
Subarachnoid Haemorrhage Investigations: 1. CT head - white star-shape 2. Lumbar puncture - wait 12 hrs - xanthochromia (yellow) Treatment: Neurosurgery!! The Peer Teaching Society is not liable for false or misleading information…
Case 4 • • • Elderly lady, many falls within the last month In the last week became very drowsy and unsteady Daughter says she is confused Seizure this morning Fluctuating levels of consciousness Most likely diagnosis? The Peer Teaching Society is not liable for false or misleading information…
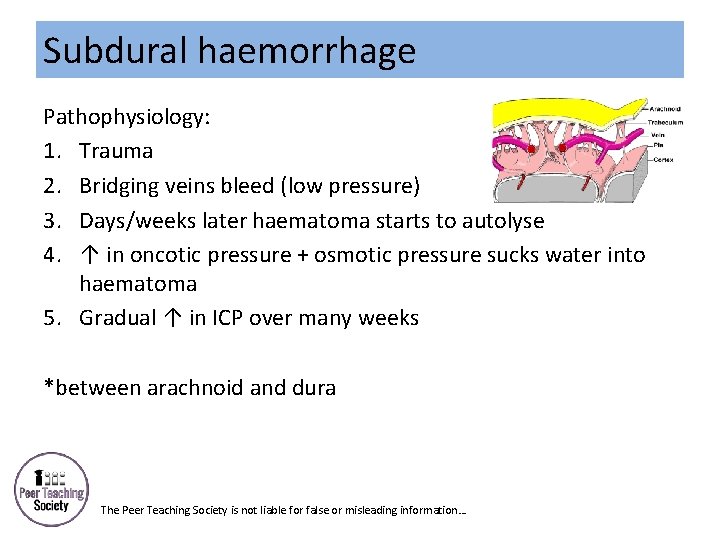
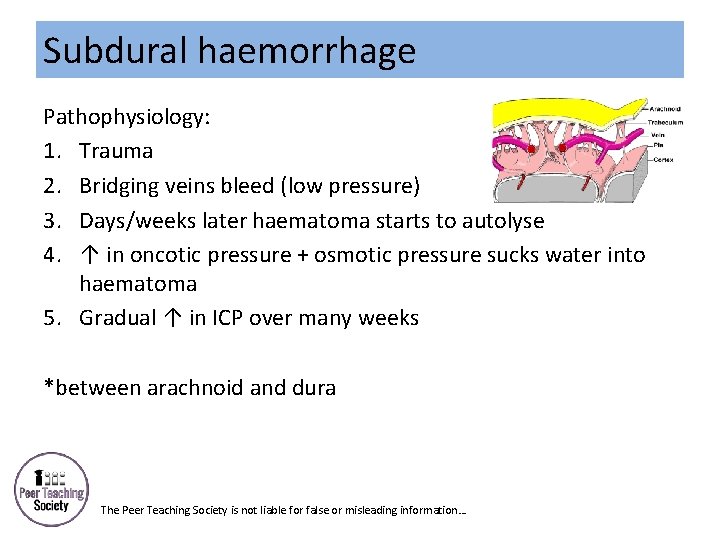
Subdural haemorrhage Pathophysiology: 1. Trauma 2. Bridging veins bleed (low pressure) 3. Days/weeks later haematoma starts to autolyse 4. ↑ in oncotic pressure + osmotic pressure sucks water into haematoma 5. Gradual ↑ in ICP over many weeks *between arachnoid and dura The Peer Teaching Society is not liable for false or misleading information…
Subdural haemorrhage Symptoms of ↑ Intracranial Pressure (ICP) v Headache v Seizures v Vomiting Investigations CT head: - Crescent-shaped mass - Midline shift Treatment: NEUROGURGERY 1 st line: clot evacuation, 2 nd line craniotomy The Peer Teaching Society is not liable for false or misleading information…
Case 5 • • 36 yr old male Traffic accident this morning Slight headache but otherwise felt fine Now (12 hrs later), drowsy Diagnosis? What is this phenomenon called? The Peer Teaching Society is not liable for false or misleading information…
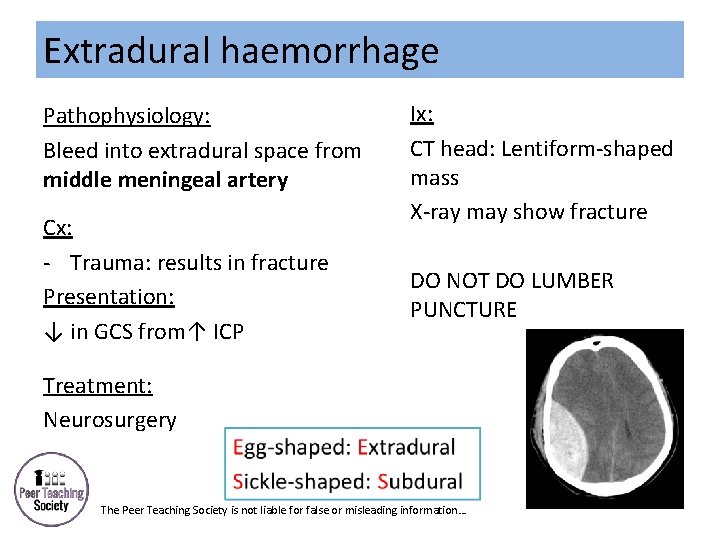
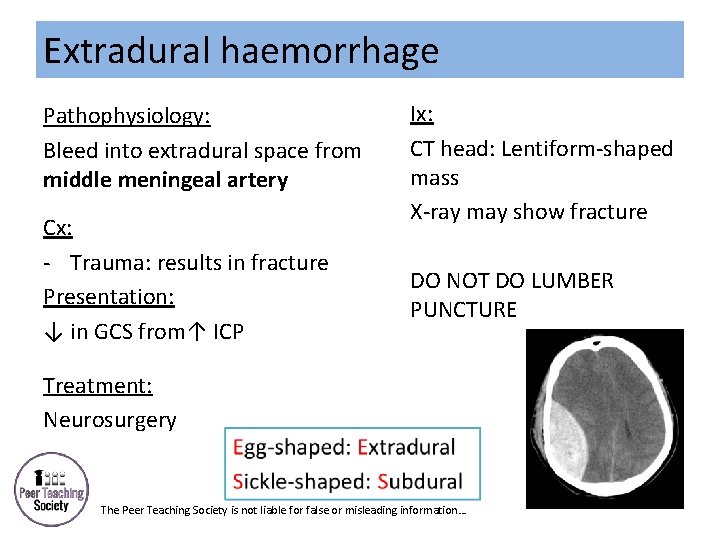
Extradural haemorrhage Pathophysiology: Bleed into extradural space from middle meningeal artery Cx: - Trauma: results in fracture Presentation: ↓ in GCS from↑ ICP Ix: CT head: Lentiform-shaped mass X-ray may show fracture DO NOT DO LUMBER PUNCTURE Treatment: Neurosurgery The Peer Teaching Society is not liable for false or misleading information…
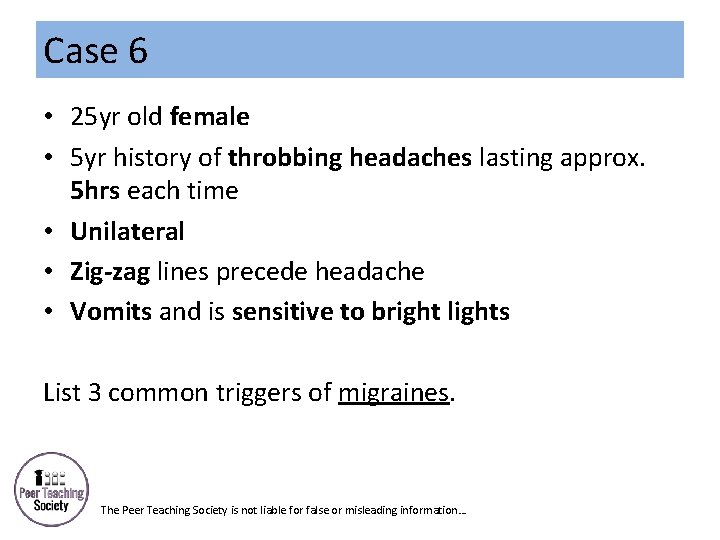
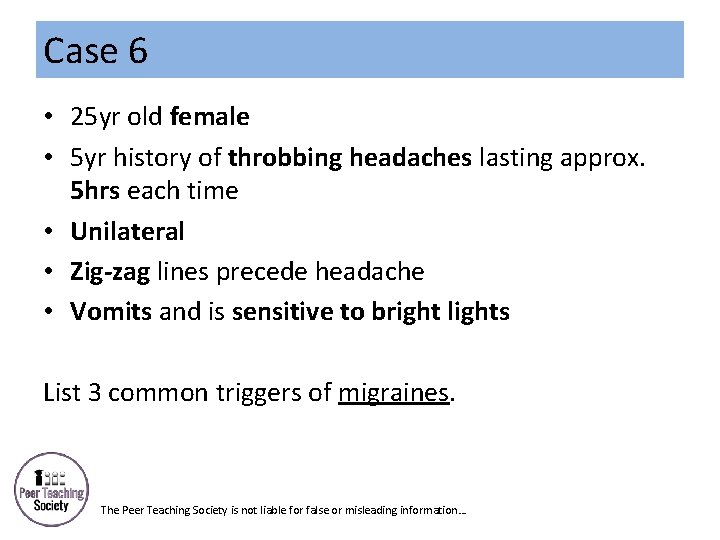
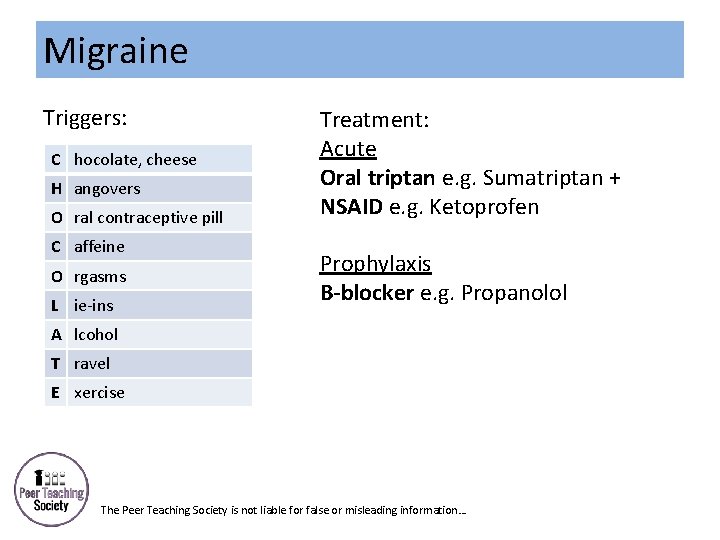
Case 6 • 25 yr old female • 5 yr history of throbbing headaches lasting approx. 5 hrs each time • Unilateral • Zig-zag lines precede headache • Vomits and is sensitive to bright lights List 3 common triggers of migraines. The Peer Teaching Society is not liable for false or misleading information…
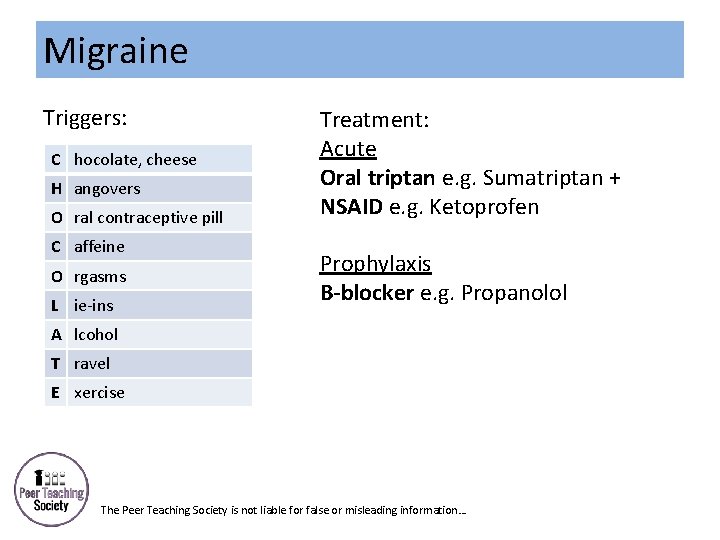
Migraine Triggers: C hocolate, cheese H angovers O ral contraceptive pill C affeine O rgasms L ie-ins Treatment: Acute Oral triptan e. g. Sumatriptan + NSAID e. g. Ketoprofen Prophylaxis B-blocker e. g. Propanolol A lcohol T ravel E xercise The Peer Teaching Society is not liable for false or misleading information…
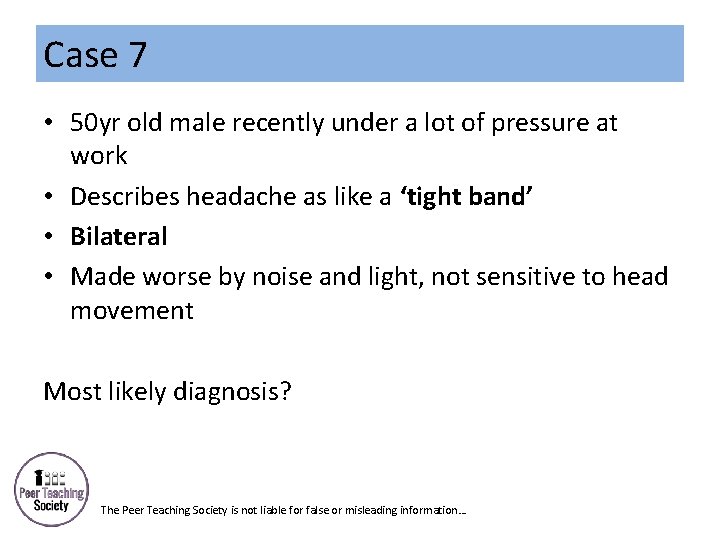
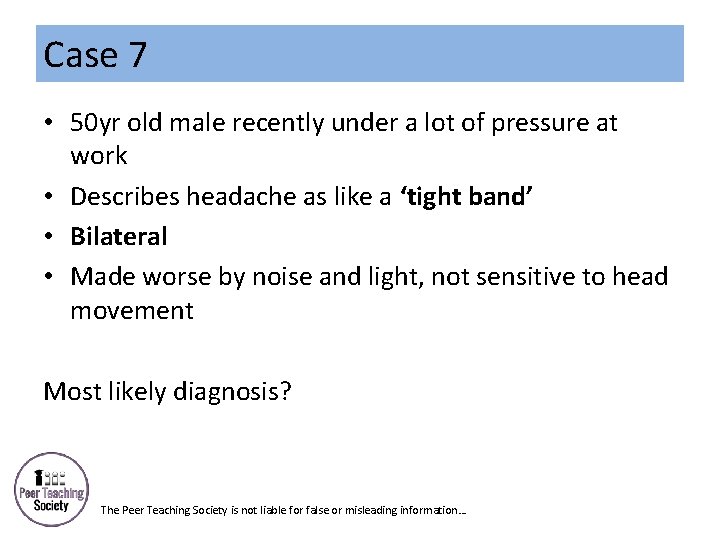
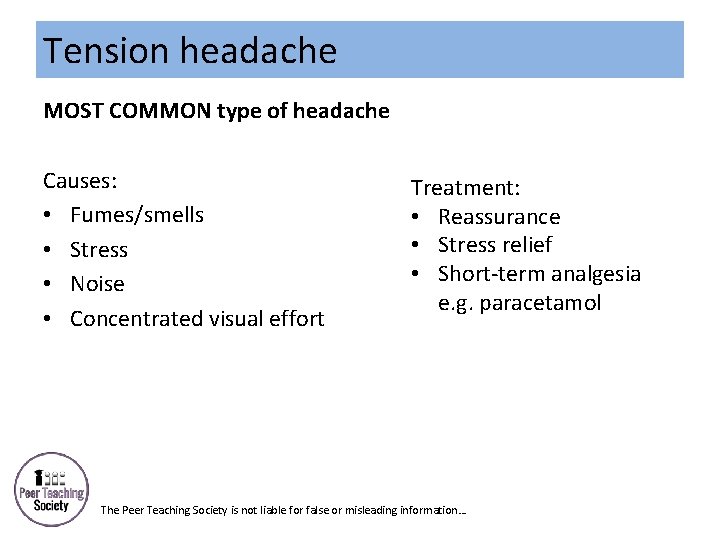
Case 7 • 50 yr old male recently under a lot of pressure at work • Describes headache as like a ‘tight band’ • Bilateral • Made worse by noise and light, not sensitive to head movement Most likely diagnosis? The Peer Teaching Society is not liable for false or misleading information…
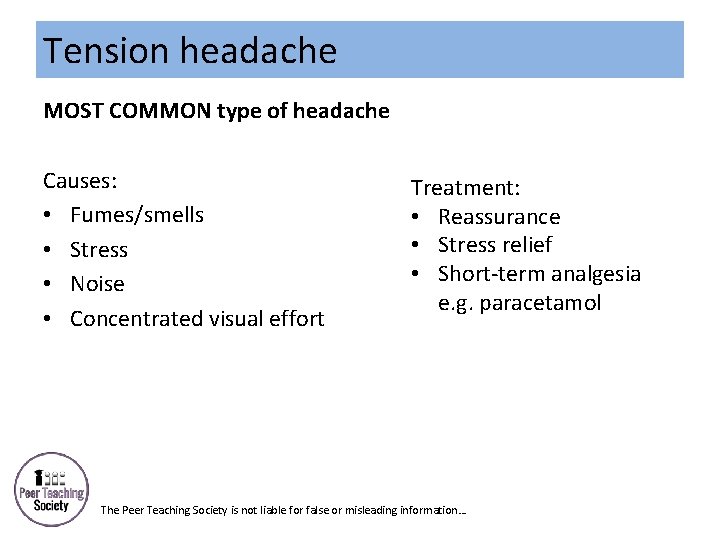
Tension headache MOST COMMON type of headache Causes: • Fumes/smells • Stress • Noise • Concentrated visual effort Treatment: • Reassurance • Stress relief • Short-term analgesia e. g. paracetamol The Peer Teaching Society is not liable for false or misleading information…
Case 8 • • • 40 yr old male smoker Sudden onset excruciating pain around 1 eye 5 episodes in the last week Similar pain 1 year ago Lasts 30 mins Usually wakes him up from sleep: ‘alarm-clock headache’ Cluster headache. What’s the treatment? The Peer Teaching Society is not liable for false or misleading information…
Cluster Headaches Treatment: • 100% O 2 • Sumatriptan at onset Prevention: • Verapamil The Peer Teaching Society is not liable for false or misleading information…
Case 9 • 60 yr old female • New onset headache, doesn’t go away with painkillers • Tenderness when brushing hair • Pain in jaw when eating • Loss of vision in 1 eye • Pain and stiffness in shoulders Most likely diagnosis? What’s the treatment? The Peer Teaching Society is not liable for false or misleading information…
Giant Cell Arteritis (temporal arteritis) = granulomatous inflammation of blood vessel walls (vasculitis) Causes: • Primary • Secondary: SLE. RA, HIV Investigations: • ↑ ESR • Temporal artery biopsy Treatment: High-dose steroids e. g. IV methylprednisolone The Peer Teaching Society is not liable for false or misleading information…
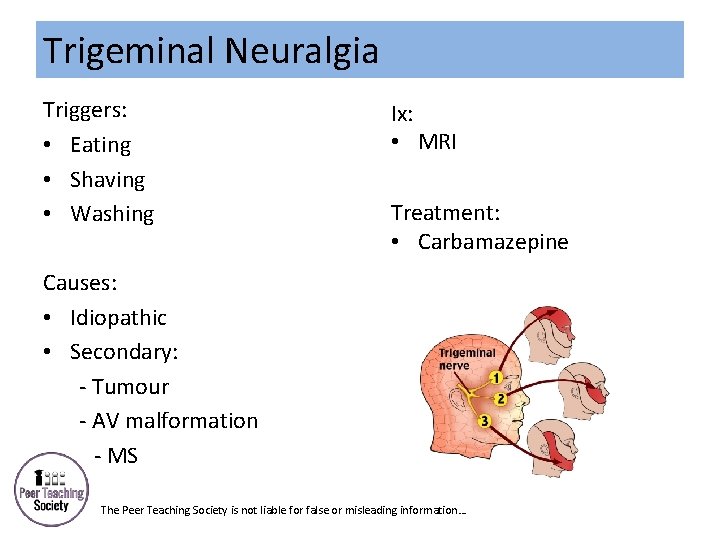
Case 10 • • 86 yr old female Severe electric shock sensation over jaw Occurs when brushing teeth Lasts only a few seconds Trigeminal neuralgia. Which branch of trigeminal nerve is most affected? The Peer Teaching Society is not liable for false or misleading information…
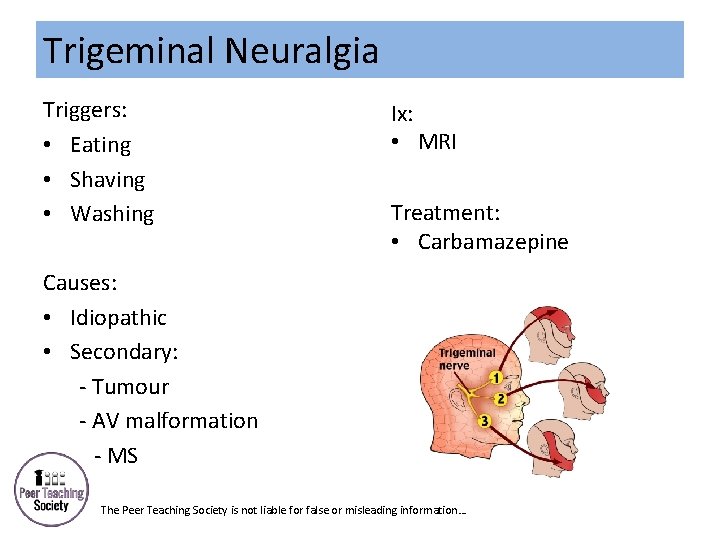
Trigeminal Neuralgia Triggers: • Eating • Shaving • Washing Ix: • MRI Treatment: • Carbamazepine Causes: • Idiopathic • Secondary: - Tumour - AV malformation --- MS The Peer Teaching Society is not liable for false or misleading information…
Case 11 • • • 65 yr old male Resting tremor in L hand for one month Hand writing is smaller Difficulty doing up buttons When questioned he has a 2 yr history of anosmia Parkinson’s Disease. What are the 4 Parkinsonism traits? The Peer Teaching Society is not liable for false or misleading information…
Idiopathic Parkinson’s Disease Aetiology: Genetic susceptibility and environmental factors Parkinsonism: 1. Tremor 2. Rigidity 3. Bradykinesia 4. Postural instability Gait: • Reduced arm swing on 1 side • Shuffling • Stooped posture • Difficulty starting *Cognitive impairment The Peer Teaching Society is not liable for false or misleading information…
Idiopathic Parkinson’s Disease Treatment: v Multi-disciplinary team v Postural exercise v Education Levodopa + dopa-decarboxylase inhibitor ‘on-off’ phenomenon The Peer Teaching Society is not liable for false or misleading information…
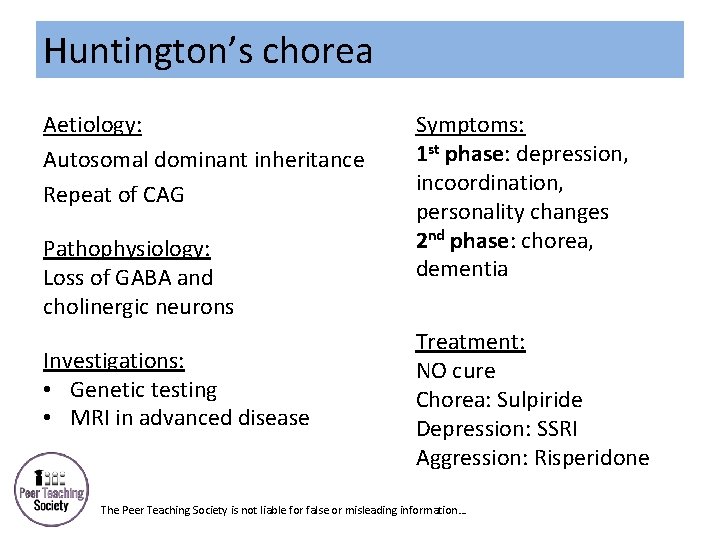
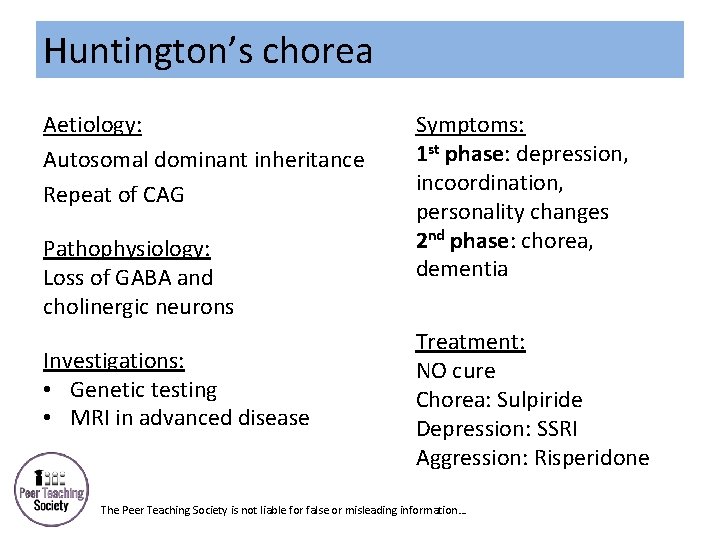
Huntington’s chorea Aetiology: Autosomal dominant inheritance Repeat of CAG Pathophysiology: Loss of GABA and cholinergic neurons Investigations: • Genetic testing • MRI in advanced disease Symptoms: 1 st phase: depression, incoordination, personality changes 2 nd phase: chorea, dementia Treatment: NO cure Chorea: Sulpiride Depression: SSRI Aggression: Risperidone The Peer Teaching Society is not liable for false or misleading information…
Case 12 • • • 12 yr old male Limbs stiffened Fell to the floor Limbs jerked, tongue biting and urinary incontinence Last 4 minutes Hx of 3 similar episodes Most likely diagnosis? The Peer Teaching Society is not liable for false or misleading information…
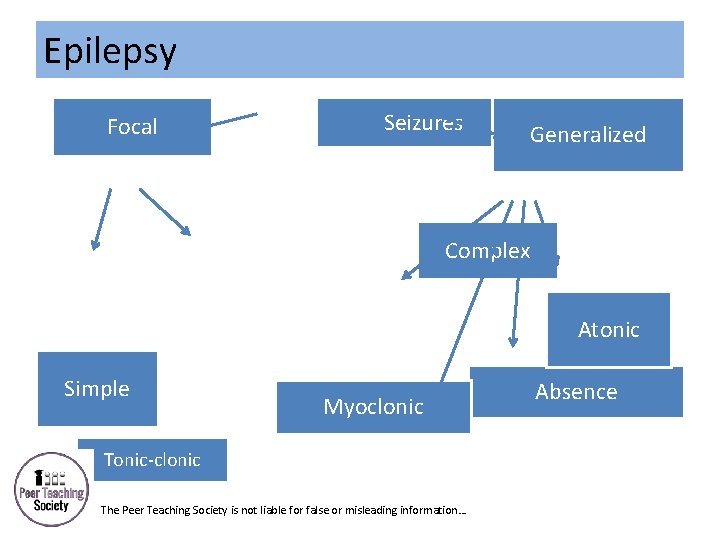
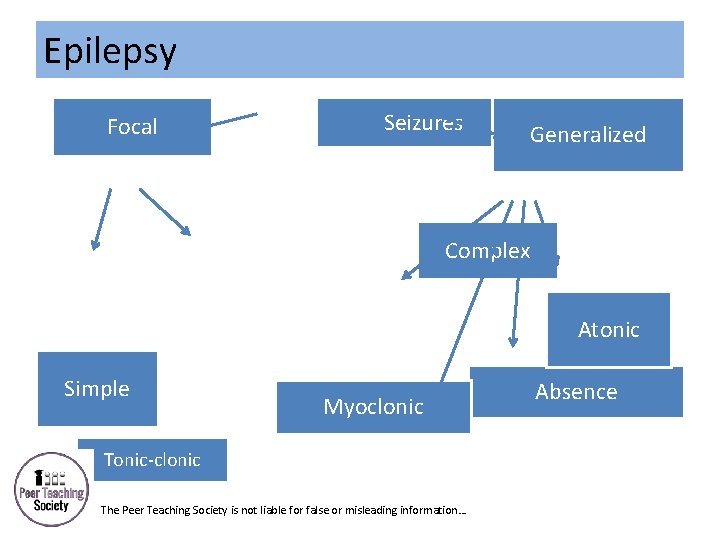
Epilepsy Focal Seizures Generalized Complex Atonic Simple Myoclonic Tonic-clonic The Peer Teaching Society is not liable for false or misleading information… Absence
Epilepsy Treatment: Focal • Carbemazepine: inhibits Na+ channels OR Lamotrigine: inhibits glutamate release Generalized • Sodium valproate OR Lamotrigine The Peer Teaching Society is not liable for false or misleading information…
Case • Women presents with 3 month history of back pain. The pair radiates down her right leg to her foot. No weakness of sensory disturbance. • What dose she have? • If she had sexual dysfunction/ incontinence? The Peer Teaching Society is not liable for false or misleading information…
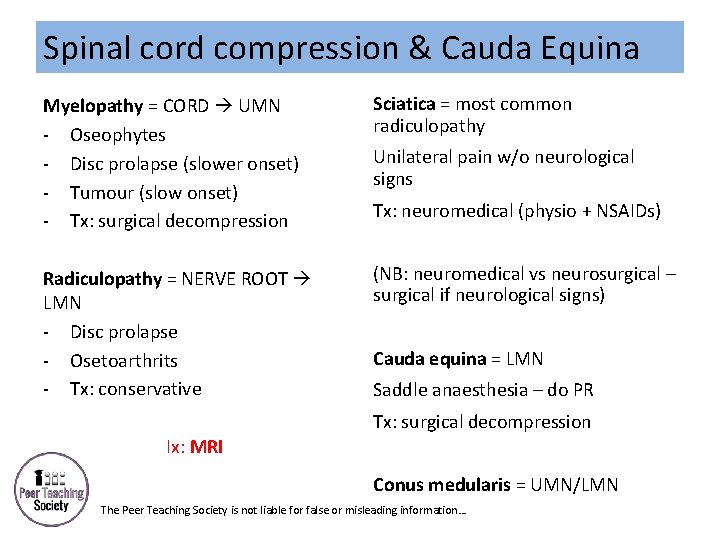
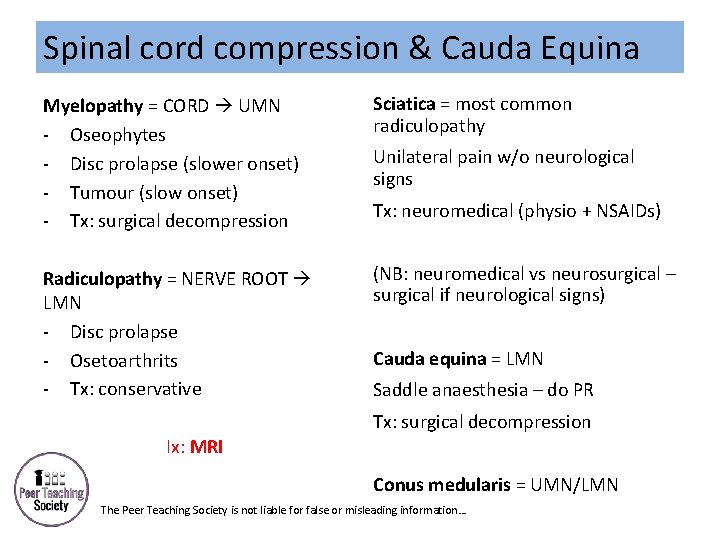
Spinal cord compression & Cauda Equina Myelopathy = CORD UMN - Oseophytes - Disc prolapse (slower onset) - Tumour (slow onset) - Tx: surgical decompression Sciatica = most common radiculopathy Radiculopathy = NERVE ROOT LMN - Disc prolapse - Osetoarthrits - Tx: conservative (NB: neuromedical vs neurosurgical – surgical if neurological signs) Unilateral pain w/o neurological signs Tx: neuromedical (physio + NSAIDs) Cauda equina = LMN Saddle anaesthesia – do PR Tx: surgical decompression Ix: MRI Conus medularis = UMN/LMN The Peer Teaching Society is not liable for false or misleading information…
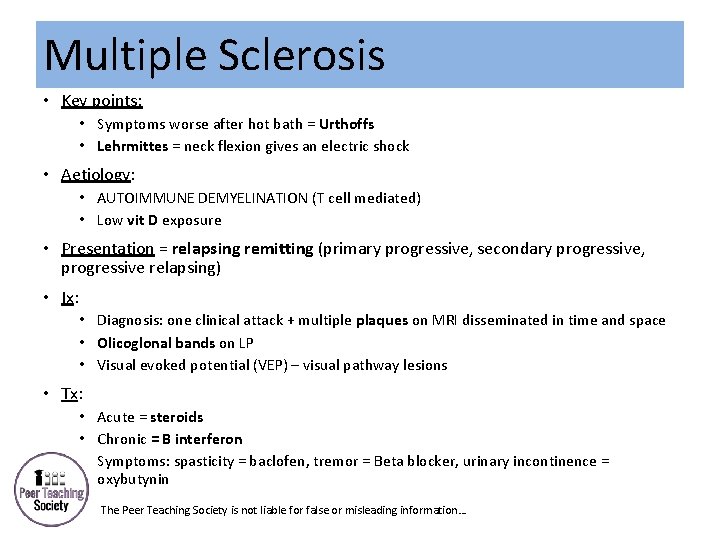
Case • A woman presents with a 2 month history of pain and tingling in both her legs. She also report weakness. When questioned she had a previous episode of eye pain 1 year ago. • What does she have? The Peer Teaching Society is not liable for false or misleading information…
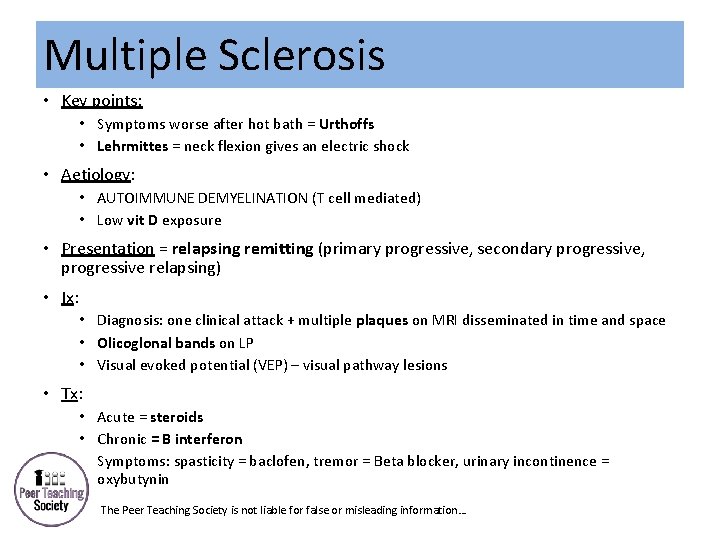
Multiple Sclerosis • Key points: • Symptoms worse after hot bath = Urthoffs • Lehrmittes = neck flexion gives an electric shock • Aetiology: • AUTOIMMUNE DEMYELINATION (T cell mediated) • Low vit D exposure • Presentation = relapsing remitting (primary progressive, secondary progressive, progressive relapsing) • Ix: • Diagnosis: one clinical attack + multiple plaques on MRI disseminated in time and space • Olicoglonal bands on LP • Visual evoked potential (VEP) – visual pathway lesions • Tx: • Acute = steroids • Chronic = B interferon • Symptoms: spasticity = baclofen, tremor = Beta blocker, urinary incontinence = oxybutynin The Peer Teaching Society is not liable for false or misleading information…
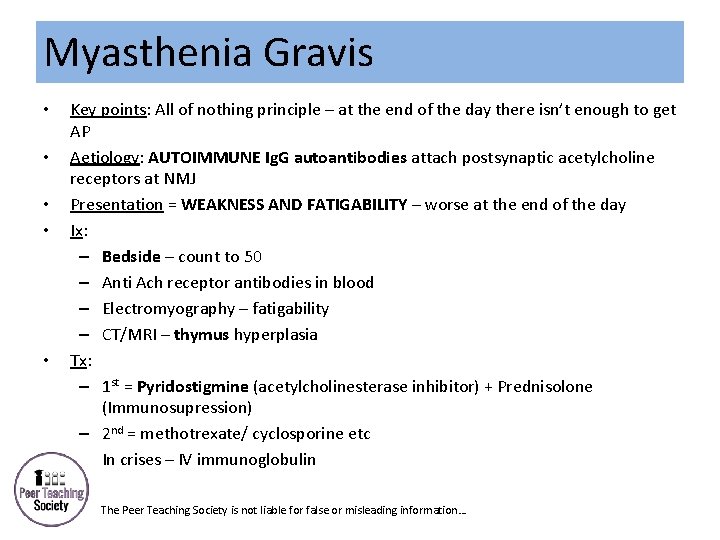
Case • Woman who is slurring her words, struggling to climb stairs. On examination she find it difficult to stand from sitting. Her symptoms are worse at night. She is not in pain. • What dose she have? The Peer Teaching Society is not liable for false or misleading information…
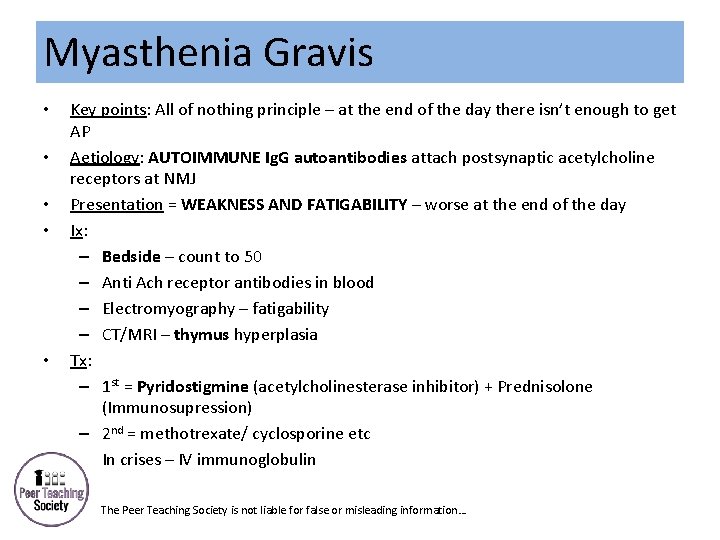
Myasthenia Gravis • • • Key points: All of nothing principle – at the end of the day there isn’t enough to get AP Aetiology: AUTOIMMUNE Ig. G autoantibodies attach postsynaptic acetylcholine receptors at NMJ Presentation = WEAKNESS AND FATIGABILITY – worse at the end of the day Ix: – Bedside – count to 50 – Anti Ach receptor antibodies in blood – Electromyography – fatigability – CT/MRI – thymus hyperplasia Tx: – 1 st = Pyridostigmine (acetylcholinesterase inhibitor) + Prednisolone (Immunosupression) – 2 nd = methotrexate/ cyclosporine etc – In crises – IV immunoglobulin The Peer Teaching Society is not liable for false or misleading information…
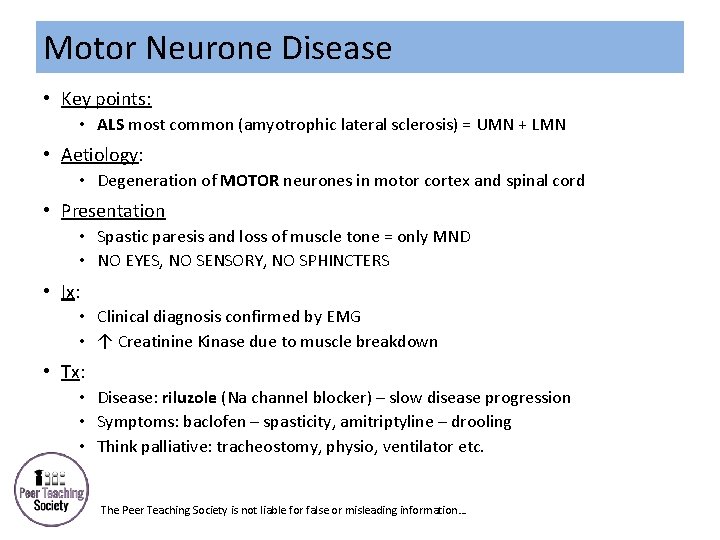
Case • A 50 year old man presents with difficult carrying out daily chores and his work as a builder. He cant lift heavy things, his arms and legs feel weak. He denies any loss of sensation. His symptoms are getting progressively worse. • What could he have? The Peer Teaching Society is not liable for false or misleading information…
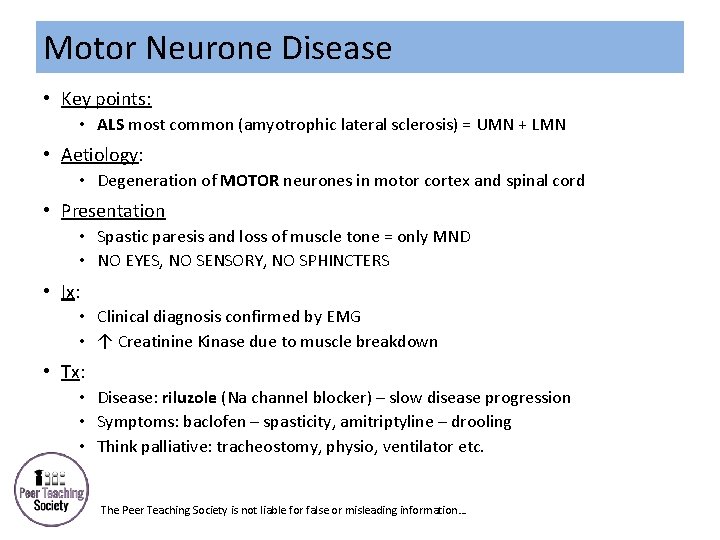
Motor Neurone Disease • Key points: • ALS most common (amyotrophic lateral sclerosis) = UMN + LMN • Aetiology: • Degeneration of MOTOR neurones in motor cortex and spinal cord • Presentation • Spastic paresis and loss of muscle tone = only MND • NO EYES, NO SENSORY, NO SPHINCTERS • Ix: • Clinical diagnosis confirmed by EMG • ↑ Creatinine Kinase due to muscle breakdown • Tx: • Disease: riluzole (Na channel blocker) – slow disease progression • Symptoms: baclofen – spasticity, amitriptyline – drooling • Think palliative: tracheostomy, physio, ventilator etc. The Peer Teaching Society is not liable for false or misleading information…
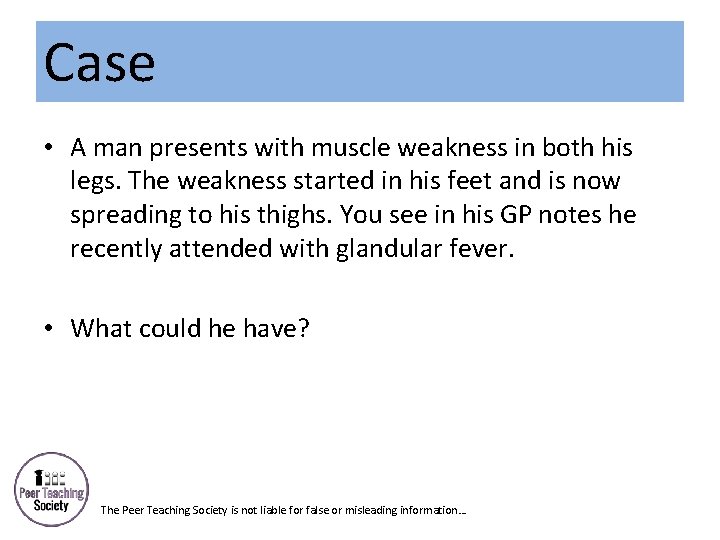
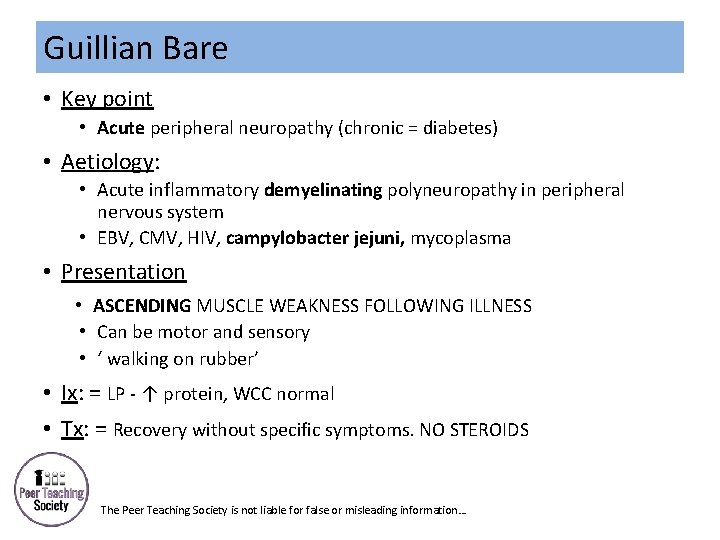
Case • A man presents with muscle weakness in both his legs. The weakness started in his feet and is now spreading to his thighs. You see in his GP notes he recently attended with glandular fever. • What could he have? The Peer Teaching Society is not liable for false or misleading information…
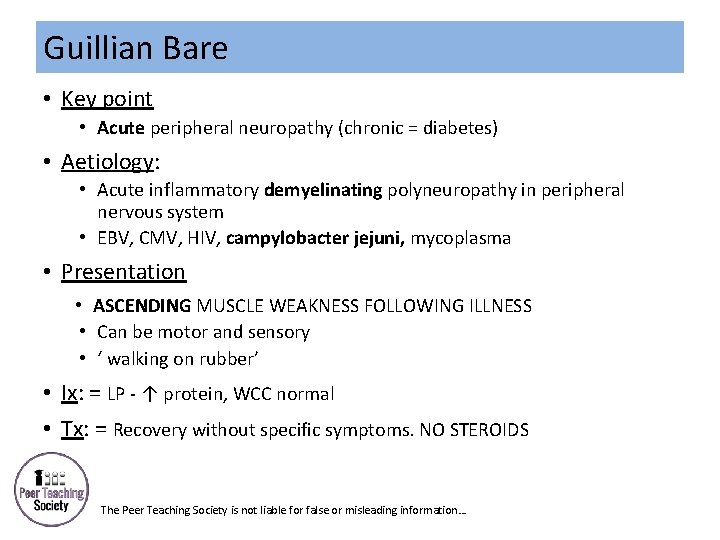
Guillian Bare • Key point • Acute peripheral neuropathy (chronic = diabetes) • Aetiology: • Acute inflammatory demyelinating polyneuropathy in peripheral nervous system • EBV, CMV, HIV, campylobacter jejuni, mycoplasma • Presentation • ASCENDING MUSCLE WEAKNESS FOLLOWING ILLNESS • Can be motor and sensory • ‘ walking on rubber’ • Ix: = LP - ↑ protein, WCC normal • Tx: = Recovery without specific symptoms. NO STEROIDS The Peer Teaching Society is not liable for false or misleading information…
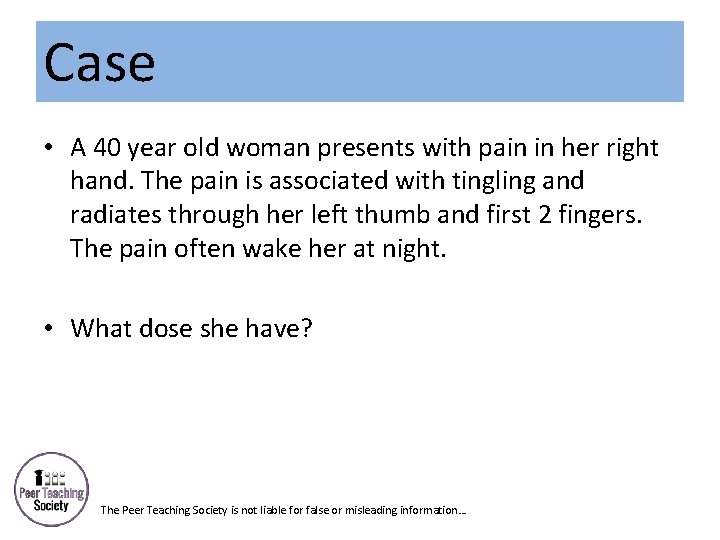
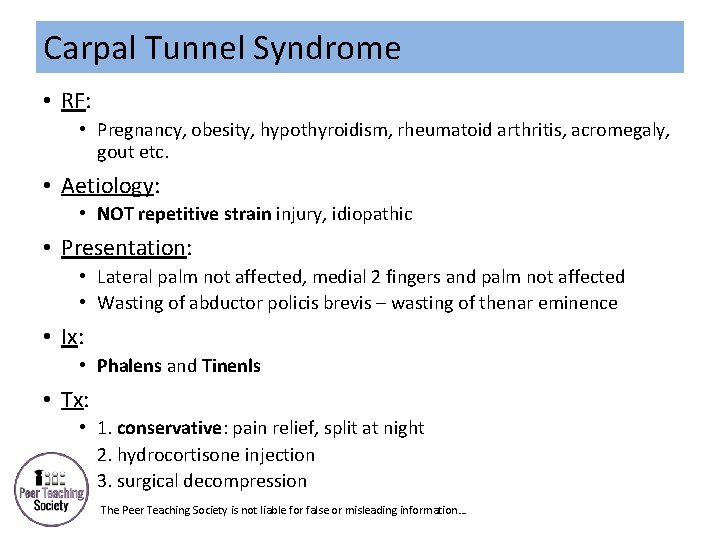
Case • A 40 year old woman presents with pain in her right hand. The pain is associated with tingling and radiates through her left thumb and first 2 fingers. The pain often wake her at night. • What dose she have? The Peer Teaching Society is not liable for false or misleading information…
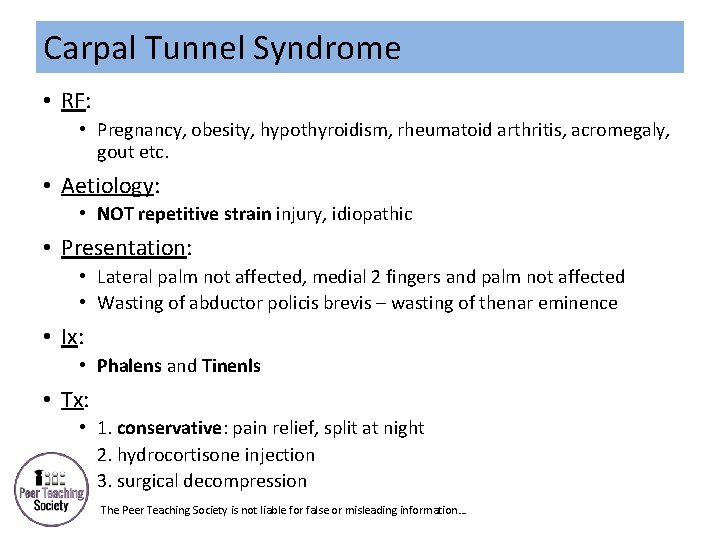
Carpal Tunnel Syndrome • RF: • Pregnancy, obesity, hypothyroidism, rheumatoid arthritis, acromegaly, gout etc. • Aetiology: • NOT repetitive strain injury, idiopathic • Presentation: • Lateral palm not affected, medial 2 fingers and palm not affected • Wasting of abductor policis brevis – wasting of thenar eminence • Ix: • Phalens and Tinenls • Tx: • 1. conservative: pain relief, split at night • 2. hydrocortisone injection • 3. surgical decompression The Peer Teaching Society is not liable for false or misleading information…
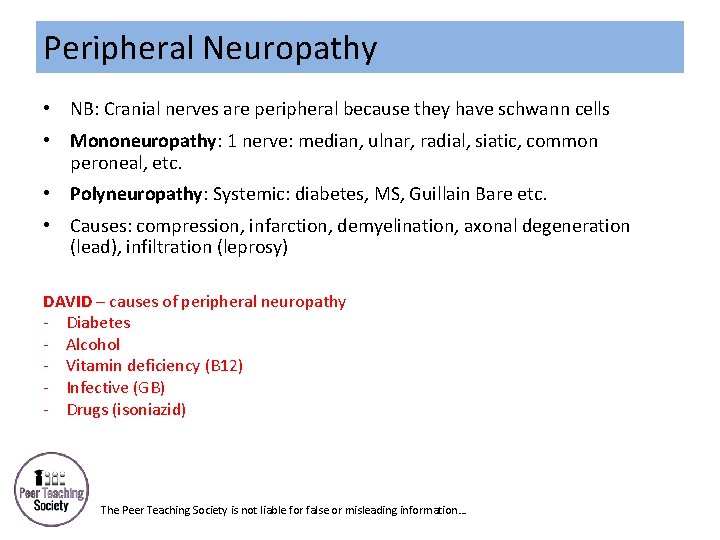
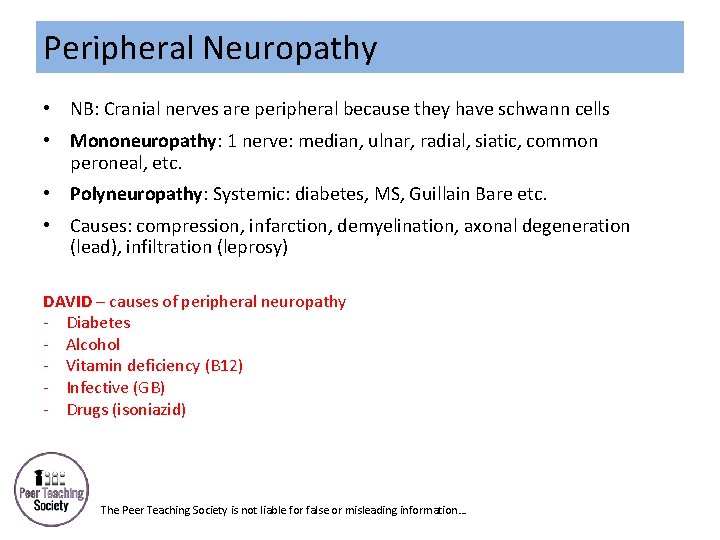
Peripheral Neuropathy • NB: Cranial nerves are peripheral because they have schwann cells • Mononeuropathy: 1 nerve: median, ulnar, radial, siatic, common peroneal, etc. • Polyneuropathy: Systemic: diabetes, MS, Guillain Bare etc. • Causes: compression, infarction, demyelination, axonal degeneration (lead), infiltration (leprosy) DAVID – causes of peripheral neuropathy - Diabetes - Alcohol - Vitamin deficiency (B 12) - Infective (GB) - Drugs (isoniazid) The Peer Teaching Society is not liable for false or misleading information…
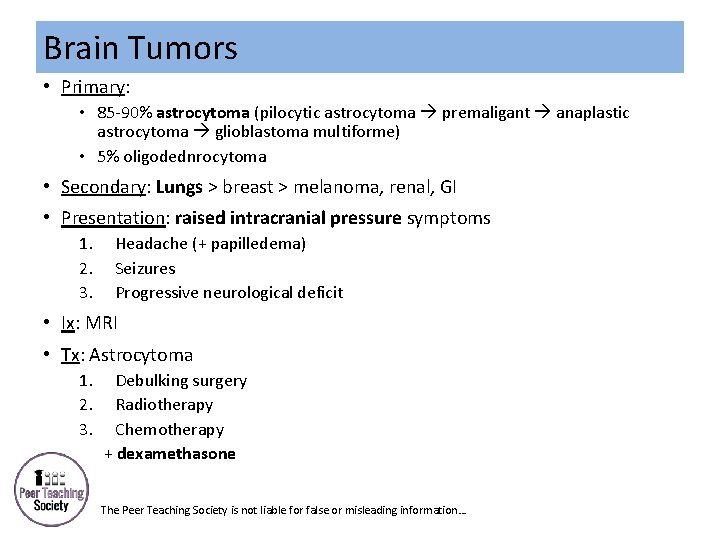
Case • A young man presents with a history of morning headaches. He has been vomiting every few days for a few weeks and last week suffered from his first seizure. • What are you worried about? The Peer Teaching Society is not liable for false or misleading information…
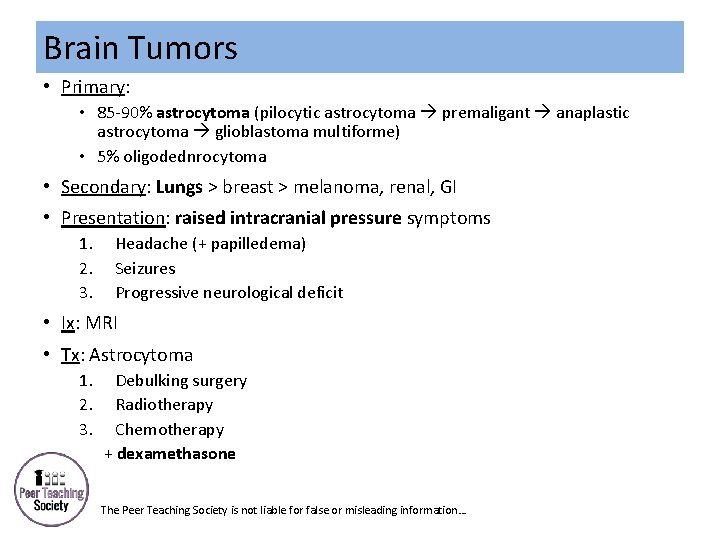
Brain Tumors • Primary: • 85 -90% astrocytoma (pilocytic astrocytoma premaligant anaplastic astrocytoma glioblastoma multiforme) • 5% oligodednrocytoma • Secondary: Lungs > breast > melanoma, renal, GI • Presentation: raised intracranial pressure symptoms 1. 2. 3. Headache (+ papilledema) Seizures Progressive neurological deficit • Ix: MRI • Tx: Astrocytoma 1. 2. 3. Debulking surgery Radiotherapy Chemotherapy + dexamethasone The Peer Teaching Society is not liable for false or misleading information…
Case • A teenage girl presents with a recent onset fever and headache. She has pain radiating down her neck and is complaining of bright lights. When you examine her she has a rash starting to form on her lower back. During the consultation she beings to become drowsy. • What are you worried about? The Peer Teaching Society is not liable for false or misleading information…
Meningitis • Aetiology: • Viral: • EBV, herpes simplex, echovirus, mumps • Bacterial: 1. 2. 3. Strep pneumoniae = most common Nesisseria meningitis = worse prognosis Listeria monocytogene • Presentation: • Meningitis: fever, headache, stiff neck, photophobia • Septicaemia: non-blanching rash • Ix: 2 nd = LP • Tx: 1 st • GP – IM benpen • Hospital – IV cefotaxime • Contacts: rifampicin, men C vaccine The Peer Teaching Society is not liable for false or misleading information…
Other infections: Encephalitis Herpes Zoster • Herpes simplex = worst • Inflammation of cortex/ white matter/ brainstem/ basal ganglia • Meningeal signs + seizures • Blood cultures, CT, LP, EEG • Tx: IV acyclovir • = shingles • Varicella zoster = chicken pox • Dormant in dorsal root ganglion • Reactivation = shingles • Pain in dermatomal distribution that doesn’t cross midline • Tx: • Acute = oral acyclovir • Post-herpetic neuralgia = amitriptyline etc. The Peer Teaching Society is not liable for false or misleading information…
Exam Qs 2016 SAQ: • Dense hemiparesis and aphasia (focus on psychosocial aspects) SBA: • Inhibitory neurotransmitter – GABA • Neurotransmitters of ANS – acetylcholine? • Microorganism causing meningitis • Nerves of the hand • Visual pathways • Initiation and control of ongoing voluntary movements The Peer Teaching Society is not liable for false or misleading information…

 Active revision vs passive revision
Active revision vs passive revision Gemma deulofeu
Gemma deulofeu Gemma del toro
Gemma del toro Angela ding
Angela ding Dr gemma moore
Dr gemma moore Diagrama rad
Diagrama rad Gemma architectuur
Gemma architectuur Gemma costa
Gemma costa Le gemma
Le gemma La riproduzione asessuata delle piante
La riproduzione asessuata delle piante Gemma
Gemma Gemma augustea analyse
Gemma augustea analyse Gemma tetlow
Gemma tetlow Taste perception
Taste perception Paolo gemma
Paolo gemma Grafcet de conduite
Grafcet de conduite Gemma bradshaw
Gemma bradshaw Gemma donati dante
Gemma donati dante Gemma downey
Gemma downey Gemma laming
Gemma laming Gemma grafcet word
Gemma grafcet word Difference between thematic and content analysis
Difference between thematic and content analysis Bagian tubuh lumut tanduk
Bagian tubuh lumut tanduk Gemma bedrijfsfuncties
Gemma bedrijfsfuncties Normal phase vs reverse phase chromatography
Normal phase vs reverse phase chromatography Phase to phase voltage
Phase to phase voltage Normal phase vs reverse phase chromatography
Normal phase vs reverse phase chromatography Hplc reverse phase vs normal phase
Hplc reverse phase vs normal phase Csce 441
Csce 441 Line current and phase current
Line current and phase current Mobile phase and stationary phase
Mobile phase and stationary phase Stationary and mobile phase
Stationary and mobile phase Hplc detector types
Hplc detector types Neurology strength scale
Neurology strength scale Tufts medical center anesthesiology residency
Tufts medical center anesthesiology residency Contrallateral
Contrallateral Difference between doppler and duplex
Difference between doppler and duplex Erlanger neurology
Erlanger neurology Neurology
Neurology Nlff neurology
Nlff neurology Neurologists northern ireland
Neurologists northern ireland Vanderbilt neurology residents
Vanderbilt neurology residents Pvnt neurology
Pvnt neurology Nheent
Nheent Robert layzer md
Robert layzer md Oregon neurology associates
Oregon neurology associates Dr bajaj neurologist
Dr bajaj neurologist Rachel ditrapani md
Rachel ditrapani md Pmg neurology
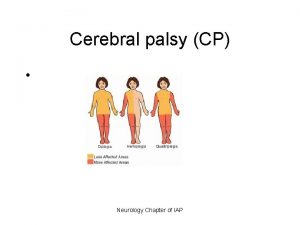
Pmg neurology Cerebral palsy iap
Cerebral palsy iap Uf neurology residency
Uf neurology residency Umass memorial pharmacy
Umass memorial pharmacy Psychiatry shelf exam percentiles
Psychiatry shelf exam percentiles The walton centre for neurology and neurosurgery
The walton centre for neurology and neurosurgery Neurology near loomis
Neurology near loomis Joseph berger md neurology
Joseph berger md neurology Department of neurology
Department of neurology Mary bridge neurology
Mary bridge neurology