Emergency Neurology Connie Chen MD Neurology Consultants of











- Slides: 45
Emergency Neurology Connie Chen, MD Neurology Consultants of Dallas
Overview n Identification of emergency n Stabilizing and treatment of emergencies n Critical care neurology: continuing care.

Emergency Neurology n Coma n Seizure n Weakness “Do I need to act now? ” “Will it change pt outcome or management if I don’t? ”

Coma: Before You Act n Assess n Examine n Reevaluate assessment
Assess n All comatose states are not equal. Source? : “Is this neurologic, cardiac, chemical? ” Treat? : “Do I need to act now? ” Difference? : “Will it change pt outcome or management? ”
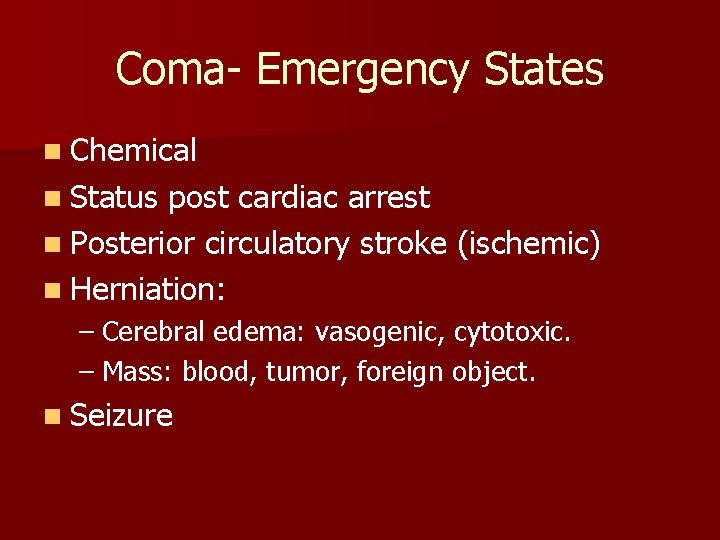
Coma- Emergency States n Chemical n Status post cardiac arrest n Posterior circulatory stroke (ischemic) n Herniation: – Cerebral edema: vasogenic, cytotoxic. – Mass: blood, tumor, foreign object. n Seizure

Coma- Scenarios n n n 81 yo woman, had c/o chest pain. Found down at home by EMS unresponsive. 62 yo man, family hears him vomit, fall, then found unresponsive. 50 yo woman, had c/o headache. Found down at work by co-workers, unresponsive. 78 yo man on warfarin collapses at home, found unresponsive. 55 yo man found convulsing in bed by wife, now unresponsive.
81 yo woman, had c/o chest pain. Found down at home by EMS unresponsive. n Source: cardiac (V. Fib arrest. ) Treat: hypothermia. Difference: yes.

Cardiac arrest- beyond the heart n Mild hypothermia (89 -93 F) decreases mortality, improves neurologic outcome. (level I) n Goal to reduced temperature: 4 hours from return of spontaneous circulation. n Duration of hypothermia: 12 -24 hours.
62 yo man, family hears him vomit, fall, then found unresponsive. n Source: posterior stroke n Treat: IV or IA t. PA n Difference: yes- and no.
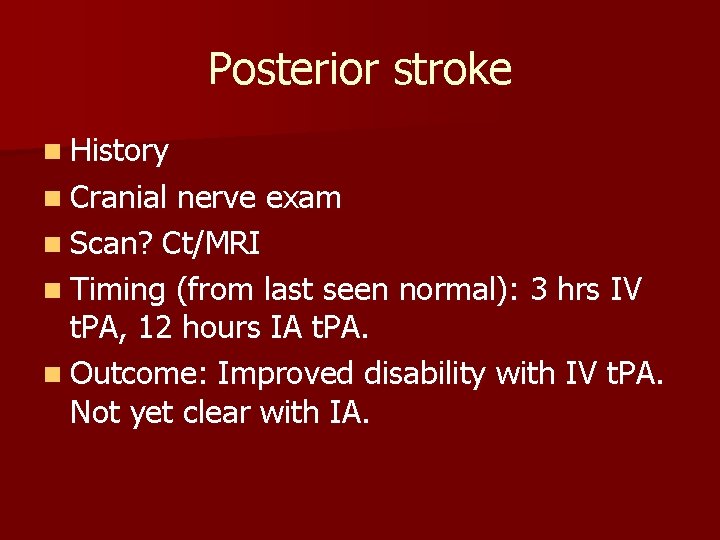
Posterior stroke n History n Cranial nerve exam n Scan? Ct/MRI n Timing (from last seen normal): 3 hrs IV t. PA, 12 hours IA t. PA. n Outcome: Improved disability with IV t. PA. Not yet clear with IA.
50 yo woman, had c/o headache. Found down at work by co-workers, unresponsive. n Source: Herniation from subarachnoid hemorrhage. n Treat: “brain rescue” n Difference: Yes! Treat within one hour of symptoms.
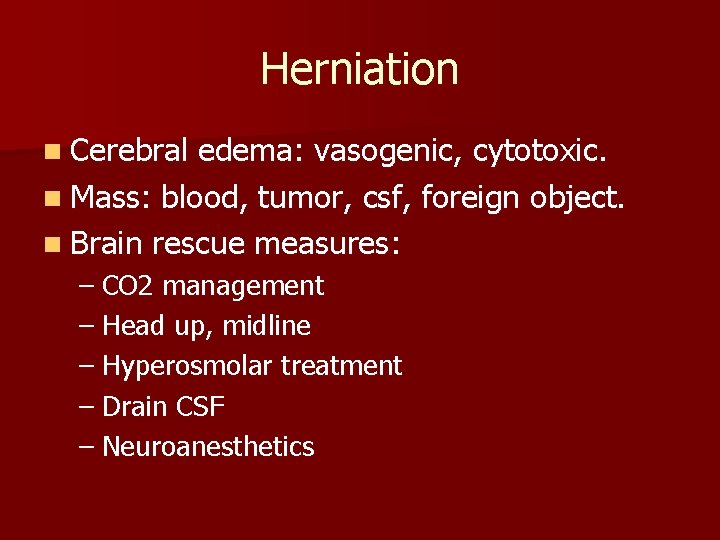
Herniation n Cerebral edema: vasogenic, cytotoxic. n Mass: blood, tumor, csf, foreign object. n Brain rescue measures: – CO 2 management – Head up, midline – Hyperosmolar treatment – Drain CSF – Neuroanesthetics

In Addition n Medical therapy of increased ICP is TEMPORARY- address the underlying condition.
78 yo man on warfarin collapses at home, found unresponsive. n Source: intracranial hemorrhage n Treat: immediate reversal of coagulopathy. BP control. n Difference: Yes! Most hematomas expand within first 24 hours.

Warfarin reversal n Vitamin K 10 mg IV now. If no IV, Vitamin K 10 mg PO now. n FFP 10 ml/kg over 90 minutes. (1 unit = 200 mls). Administer within 30 minutes of patient arrival. n Recheck INR q 2 -4 hrs. Redose Vitamin K and FFP as needed. n Never give initial FFP without vitamin K.

ICH Blood Pressure n Known hypertensive patient: MAP goal <130. n Not known hypertensive pt? SBP≤ 160. n Time to reach goal BP: one hour.
Sidetrack away from cases
Special Note n Brain death may be presented as coma. n Not strictly an emergency. n Good to know if pt is dead.
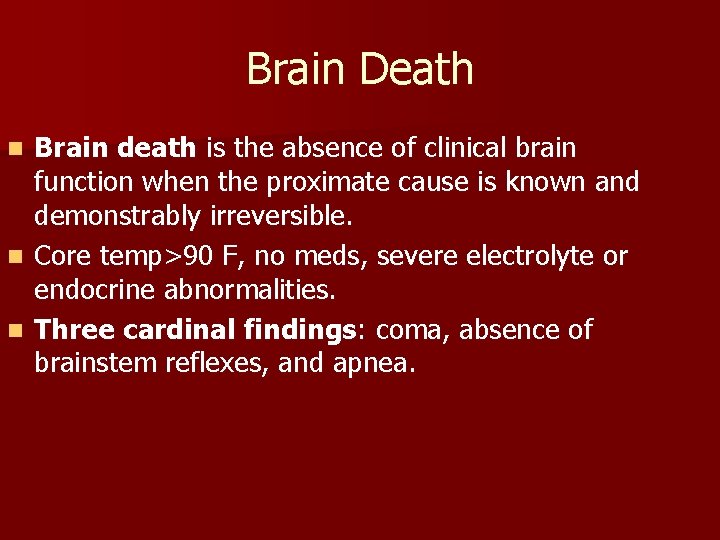
Brain Death Brain death is the absence of clinical brain function when the proximate cause is known and demonstrably irreversible. n Core temp>90 F, no meds, severe electrolyte or endocrine abnormalities. n Three cardinal findings: coma, absence of brainstem reflexes, and apnea. n
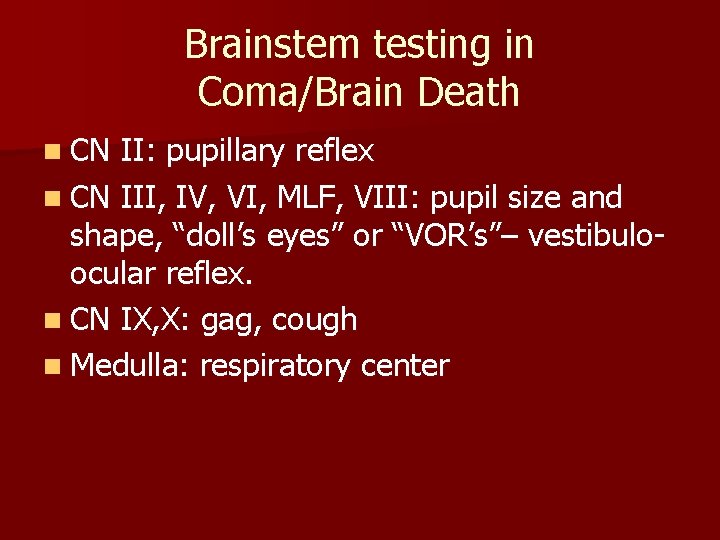
Brainstem testing in Coma/Brain Death n CN II: pupillary reflex n CN III, IV, VI, MLF, VIII: pupil size and shape, “doll’s eyes” or “VOR’s”– vestibuloocular reflex. n CN IX, X: gag, cough n Medulla: respiratory center
Back to Cases
55 yo man found convulsing in bed by wife, now unresponsive. n Source: status epilepticus n Treat: status epilepticus protocol n Difference: yes.
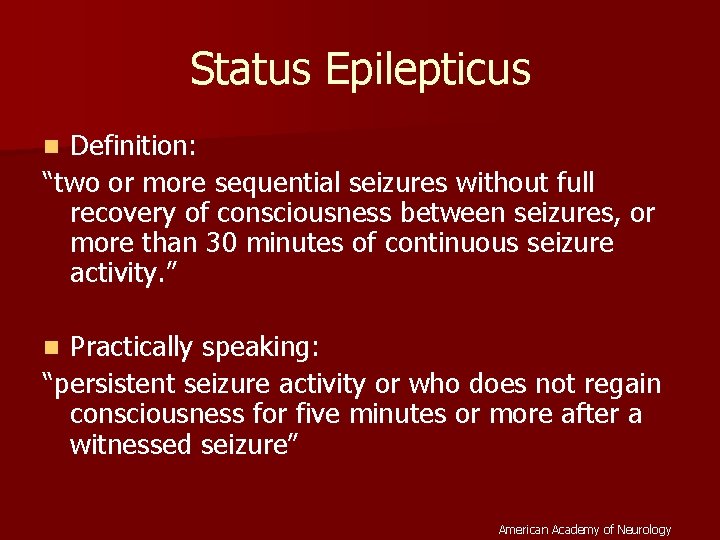
Status Epilepticus Definition: “two or more sequential seizures without full recovery of consciousness between seizures, or more than 30 minutes of continuous seizure activity. ” n Practically speaking: “persistent seizure activity or who does not regain consciousness for five minutes or more after a witnessed seizure” n American Academy of Neurology
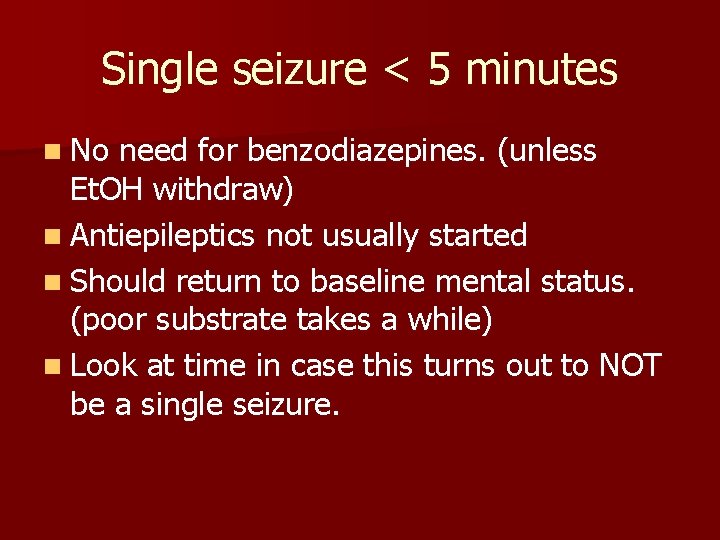
Single seizure < 5 minutes n No need for benzodiazepines. (unless Et. OH withdraw) n Antiepileptics not usually started n Should return to baseline mental status. (poor substrate takes a while) n Look at time in case this turns out to NOT be a single seizure.
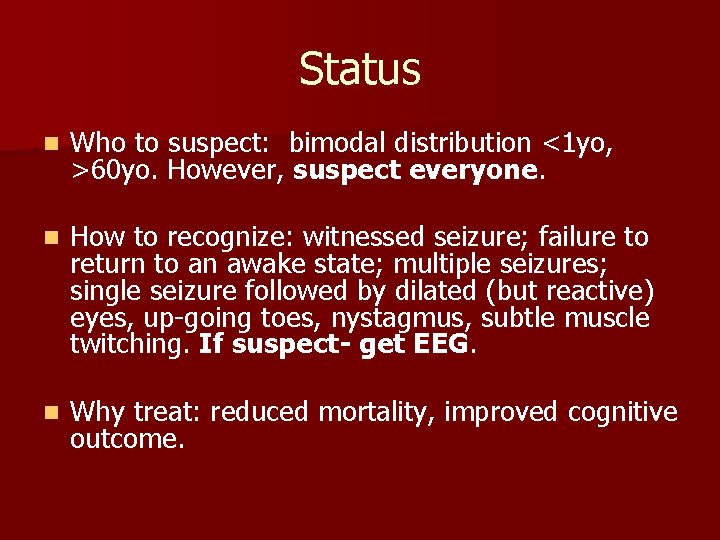
Status n Who to suspect: bimodal distribution <1 yo, >60 yo. However, suspect everyone. n How to recognize: witnessed seizure; failure to return to an awake state; multiple seizures; single seizure followed by dilated (but reactive) eyes, up-going toes, nystagmus, subtle muscle twitching. If suspect- get EEG. n Why treat: reduced mortality, improved cognitive outcome.
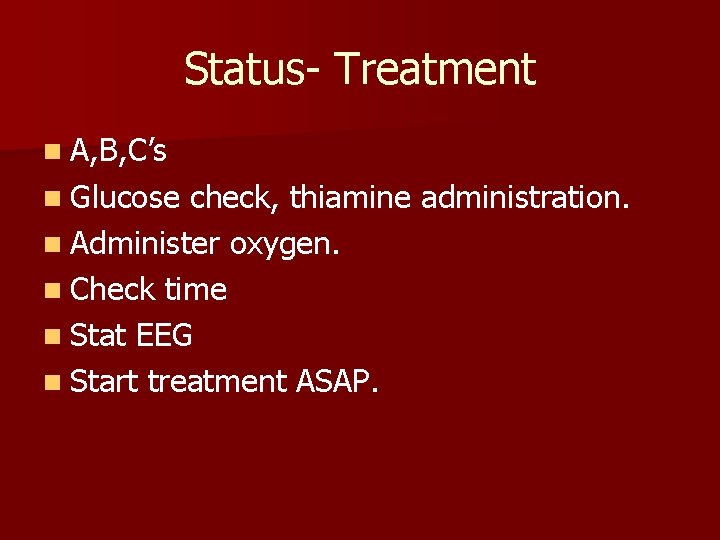
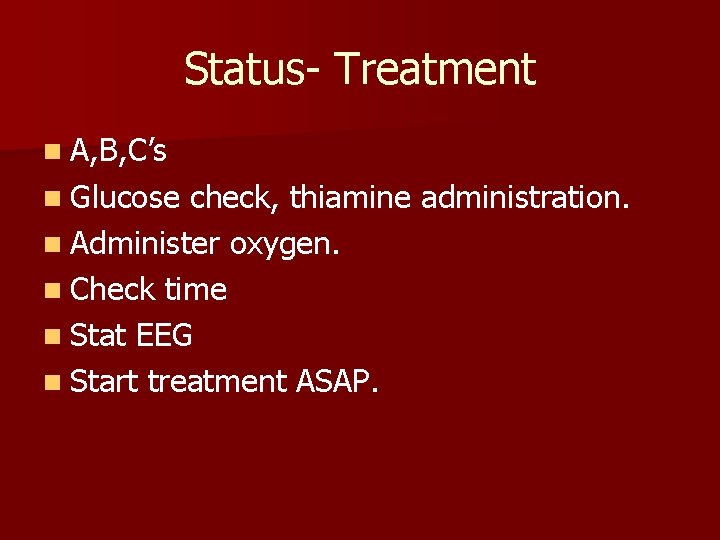
Status- Treatment n A, B, C’s n Glucose check, thiamine administration. n Administer oxygen. n Check time n Stat EEG n Start treatment ASAP.
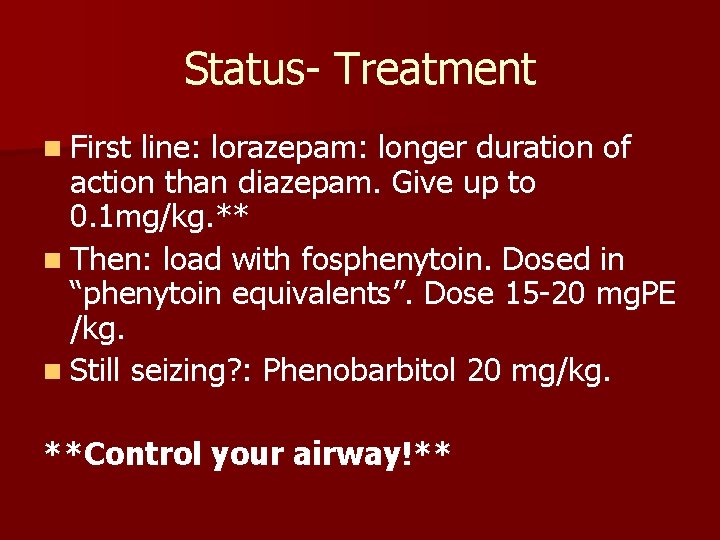
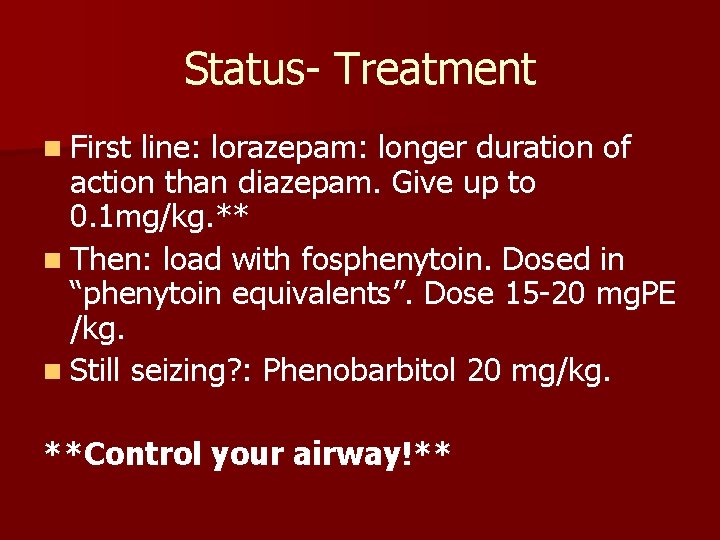
Status- Treatment n First line: lorazepam: longer duration of action than diazepam. Give up to 0. 1 mg/kg. ** n Then: load with fosphenytoin. Dosed in “phenytoin equivalents”. Dose 15 -20 mg. PE /kg. n Still seizing? : Phenobarbitol 20 mg/kg. **Control your airway!**

Am Fam Physician 2003; 68: 469 -76. Copyright© 2003 American Academy of Family Physicians. Antiepileptics in Status Drug Loading dose Maintenance dosage Adverse effects Diazepam (Valium) 10 to 20 mg None Respiratory depression, hypotension, sialorrhea Lorazepam (Ativan) 4 mg None Same as diazepam Phenytoin (Dilantin) 18 to 20 mg per kg at 50 mg per minute 5 mg per kg per day Cardiac depression, hypotension Fosphenytoin (Cerebyx) 18 to 20 mg per kg PE at 150 mg per minute None Cardiac depression, hypotension, paresthesias Phenobarbital 20 mg per kg 1 to 4 mg per kg per hour Respiratory suppression Pentobarbital 2 to 8 mg per kg 0. 5 to 5 mg per kg per hour Hypotension, respiratory suppression Midazolam (Versed) 0. 2 mg per kg 0. 75 to 10 mg per kg per minute Hypotension, respiratory suppression Propofol (Diprivan) 2 mg per kg 5 to 10 mg per kg per hour initially, then 1 to 3 mg per kg per hour Respiratory depression, hypotension, lipemia, acidosis PE = phenytoin equivalents.

Coma Cases Overview n Don’t assume etiology of coma unless you have proof. n It’s the second diagnosis that you will miss. n Delay of treatment often affects pt outcome. n “Multi-pronged” approach is better when time is an issue. n “Scan and wave. ”
Weakness
When is weakness an emergency? n Acute stroke (<3 hrs) n Spinal cord injury n Spinal cord compression
Acute Stroke n (for another day)

Spinal Cord Injury n Pattern of weakness: different grades– flaccid to “corticospinal tract” distribution of weakness. n Absent reflexes n Suspended sensory level, or sensory level ** Light touch is not appropriate for exam** n Weak rectal tone
Spinal cord injury n Within 8 hours of injury: start treatment n Solumedrol 30 mg/kg, then n Solumedrol 5. 4 mg/kg/hr for 23 hours. ** data is weak (level II-III)**
Spinal Cord Compression (tumor) n Dexamethasone 100 mg IV, then taper

Spinal Cord Injury/Compression n Medical therapy of spinal cord injury/compression is not well shown to improve outcome. n Emergent diagnosis and treatment (surgical) is needed to improve outcome. **longer you wait the worse (more permanent) the outcome**
Continuing Emergencies- Interface of Neurology and Critical Care
Neurocritical Care n Goals of Neurocritical Care – Recognition of neurologic decline in neurologically unstable pt’s. – Recognition of resultant complications on other organ systems. – Use of other organ systems to support/treat neurologic problem.
Neurocritical Care n Identification of “at risk” patients n Recognition of neurologic decline in neurologically unstable pt’s: – Herniation syndromes – Acute strokes – Development of hydrocephalus – Seizure – Extensions of neurologic injury – Spinal cord injury
Neurocritical Care n Recognition of resultant complications on other organ systems. – Neurogenic shock/ SIRS – Flash pulmonary edema – Cardiac dysfunction – Dysautonomia – Hypo or hypernatremia – Imminent loss of airway
Neurocritical Care n Use of other organ systems to treat neurologic problem: – Hyperventilation – BP augmentation – Hypothermia – Euglycemia n Assessing status. treatment’s effect on neurologic
Neurocritical Care: How is it Accomplished? n Patient care centers around neurologic exam. n Imaging studies are guided by exam. n Exam may be subtle in devastated pts. n Sedated patients all have lousy exams. n GCS is useless unless in head trauma. EXAM IS EVERYTHING!!
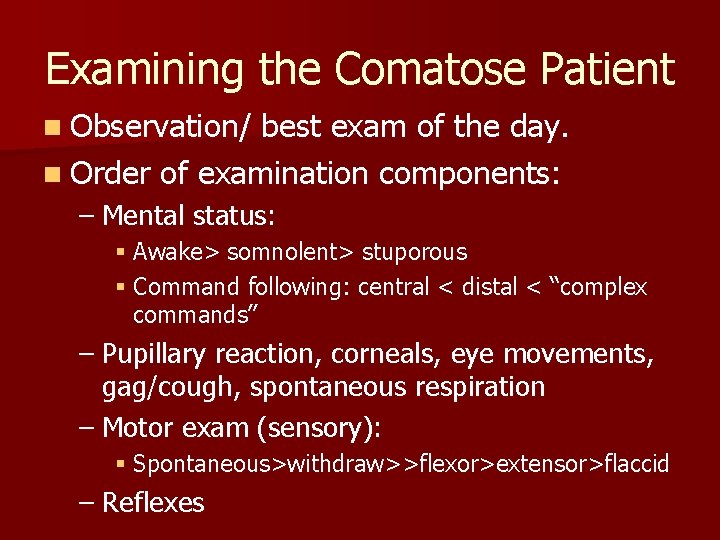
Examining the Comatose Patient n Observation/ best exam of the day. n Order of examination components: – Mental status: § Awake> somnolent> stuporous § Command following: central < distal < “complex commands” – Pupillary reaction, corneals, eye movements, gag/cough, spontaneous respiration – Motor exam (sensory): § Spontaneous>withdraw>>flexor>extensor>flaccid – Reflexes
Then what? Some Last Thoughts n Use exam to guide treatment. n Remember neurologic events happen in non-neurologic patients. n Neurologic recovery can be rapid- don’t give up too soon. – Inaction results in lack of prompt care – Worse outcome – Self-fulfilling prophecy
 Connie chen md
Connie chen md Neurology consultants northern ireland
Neurology consultants northern ireland Chen chen berlin
Chen chen berlin Connie sargent
Connie sargent Connie eldridge
Connie eldridge Consonant suffix
Consonant suffix John ritchie real estate
John ritchie real estate Connie holden
Connie holden Connie roozen
Connie roozen Barra connie
Barra connie Connie leonard cms
Connie leonard cms Connie lee md
Connie lee md Adxl-50
Adxl-50 Short poppy syndrome
Short poppy syndrome Connie white delaney
Connie white delaney Connie deckert
Connie deckert Pucne
Pucne Schopans
Schopans Dr connie feng
Dr connie feng Connie svabo
Connie svabo Connie abert
Connie abert Connie givens
Connie givens Connie ferris bailey
Connie ferris bailey Connie svabo
Connie svabo Connie white delaney
Connie white delaney Xtandi
Xtandi Connie lindsey
Connie lindsey Neurology
Neurology Nlff neurology
Nlff neurology Rrerl
Rrerl Nociceptive sensation
Nociceptive sensation Qmc neurology
Qmc neurology Williamson medical center pharmacy residency
Williamson medical center pharmacy residency Duplex vs doppler
Duplex vs doppler Cerebral palsy iap
Cerebral palsy iap Miqtu
Miqtu Umass surgery residents
Umass surgery residents Nlff neuro
Nlff neuro Uf neurology residents
Uf neurology residents Joseph berger md neurology
Joseph berger md neurology Robert layzer md
Robert layzer md Midwest neurology
Midwest neurology Neurology near loomis
Neurology near loomis Nex exam neurology
Nex exam neurology Alemutuzumab
Alemutuzumab Walton centre for neurology
Walton centre for neurology