Neurological emergencies Mackay Memorial Hospital Department of Neurology





- Slides: 37
Neurological emergencies Mackay Memorial Hospital Department of Neurology Ju-Fen Yeh 1
l l 2 Coma Hyperacute stroke (<3 hrs) and thrombolytic therapy, post-thrombolytic care Brain edema , herniation and increased intracranial pressure (IICP) Status epilepticus
COMA 3
l l l 4 Stabilize (ABC) Obtain a history Physical examination / neurological examination Laboratory test (including toxin or drug screen) Find out possible causes (most common causes are toxic and metabolic derangements, which are potentially treatable and reversible) Neuroimages (CT or MRI)
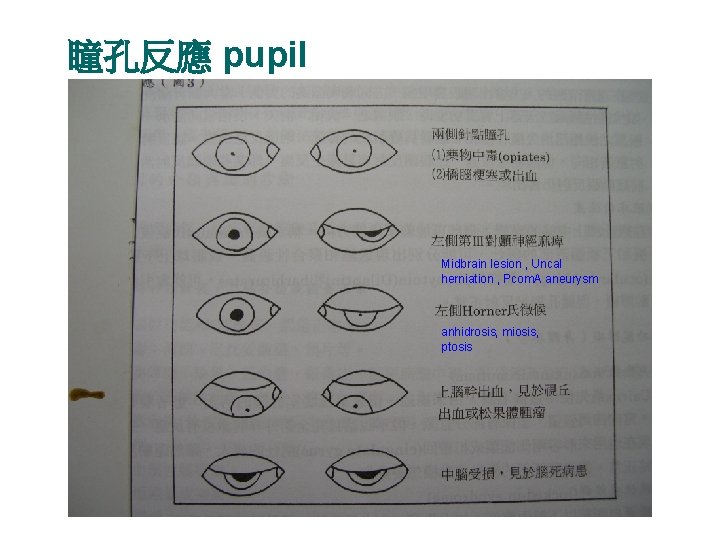
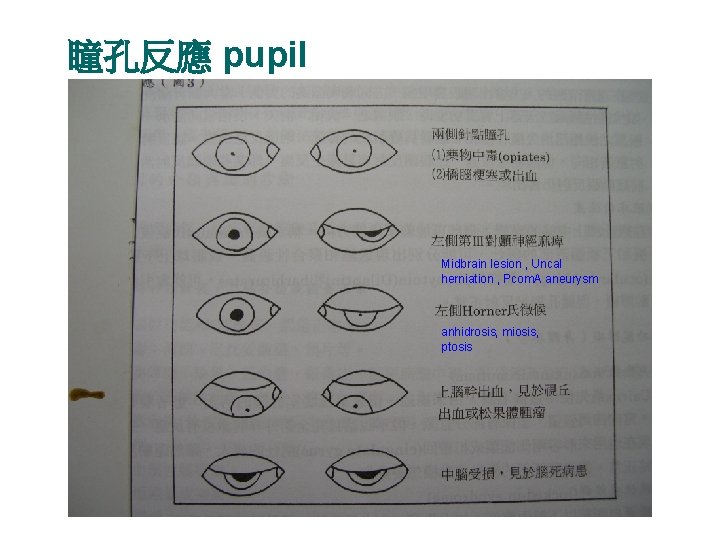
瞳孔反應 pupil Midbrain lesion , Uncal herniation , Pcom. A aneurysm anhidrosis, miosis, ptosis 5

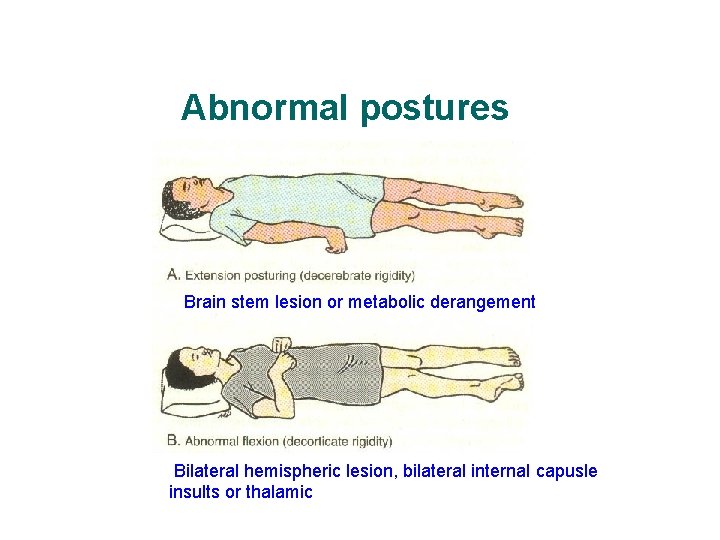
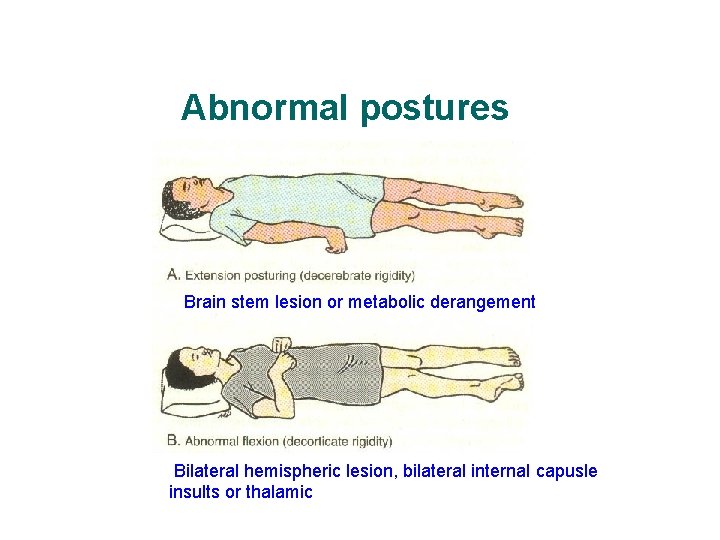
Abnormal postures Brain stem lesion or metabolic derangement 7 Bilateral hemispheric lesion, bilateral internal capusle insults or thalamic
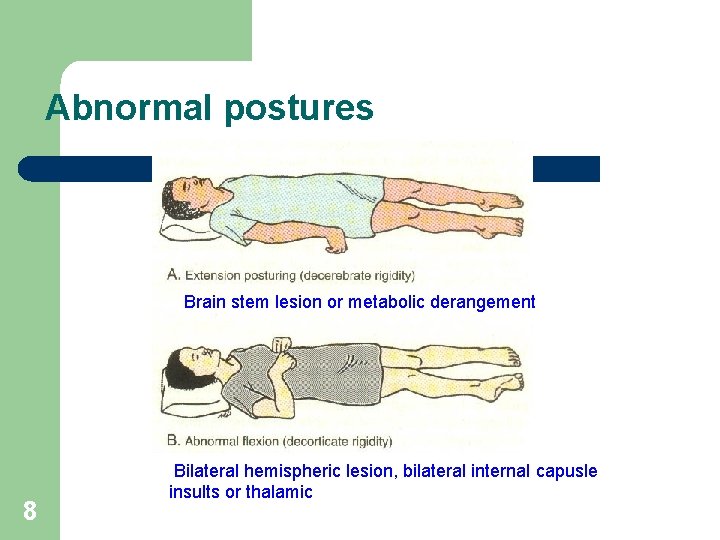
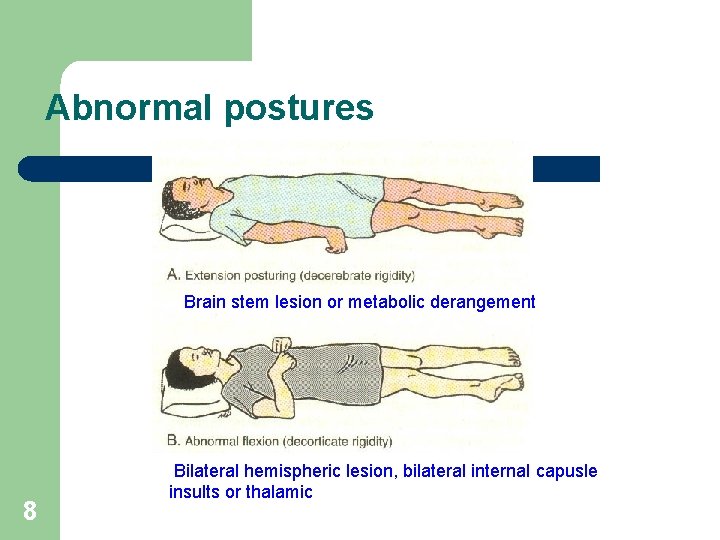
Abnormal postures Brain stem lesion or metabolic derangement 8 Bilateral hemispheric lesion, bilateral internal capusle insults or thalamic


Hyperacute stroke Thrombolytic therapy Post thrombolytic R’x care 11


13
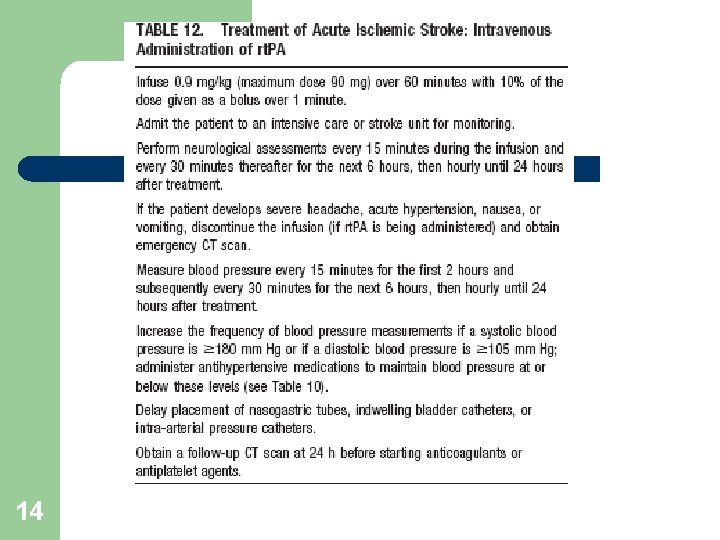
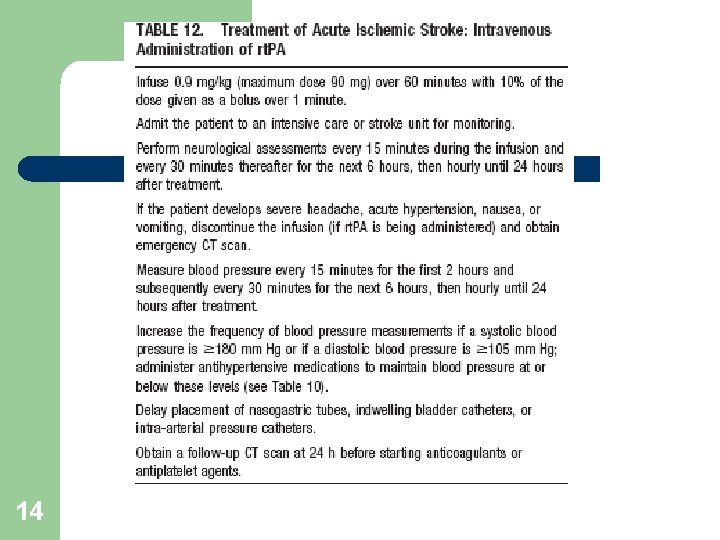
14
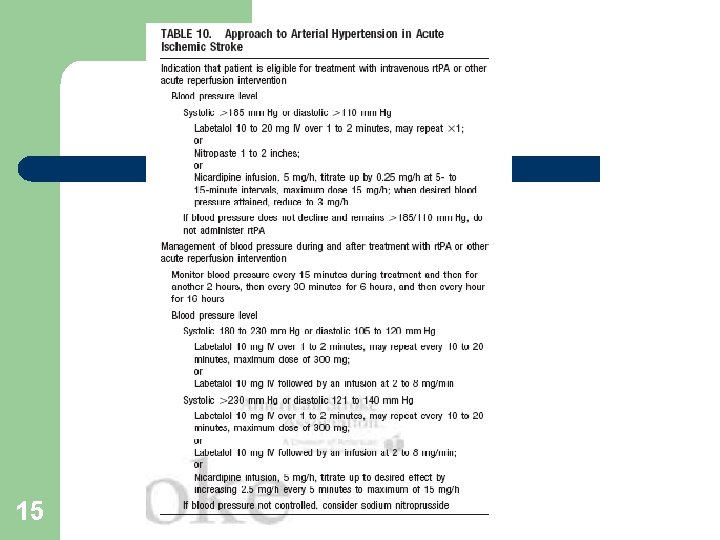
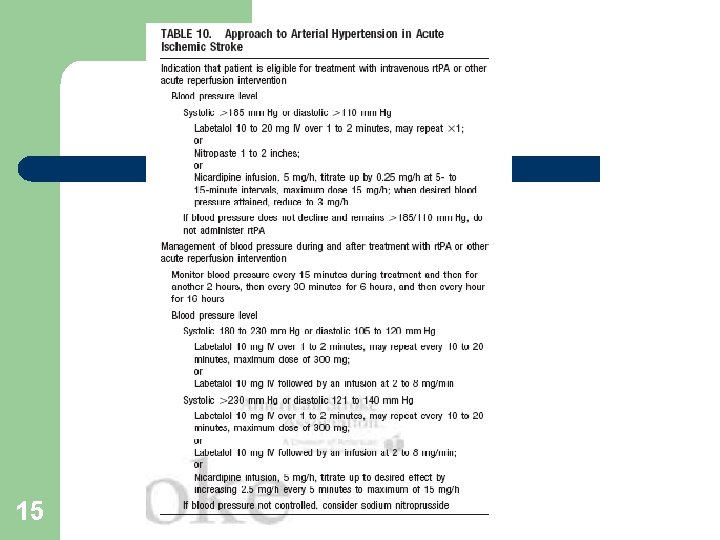
15
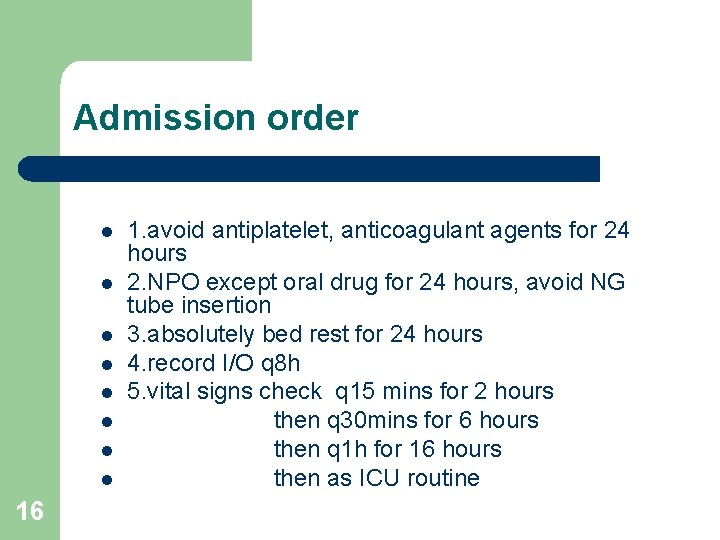
Admission order l l l l 16 1. avoid antiplatelet, anticoagulant agents for 24 hours 2. NPO except oral drug for 24 hours, avoid NG tube insertion 3. absolutely bed rest for 24 hours 4. record I/O q 8 h 5. vital signs check q 15 mins for 2 hours then q 30 mins for 6 hours then q 1 h for 16 hours then as ICU routine
l l l 17 6. GCS, Light reflex, pupil size Q 1 h for 24 hours then as ICU routine 7. call on duty resident for NIHSS and NE examination at __ (2 nd hour) and __ (24 th hour) 8. mark ecchymosis site and observation qid 9. urine observation, call resident if hematuira 10. avoid Foley tube insertion in initial 30 mins. if no urine output or bladder distension in 6 hours then consider Foley tube insertion
l l 18 12. Emergent management of BP : *1. If SBP >=180 -230 or DBP 105 -120 mm. Hg for >= 2 readings 5 -10 mins apart : (1) intravenous Trandate 10 mg over 1 -2 mins. the dose may be repeated or doubled every 1020 mins up to a total dose of 150 mg (2) monitor BP q 15 mins during Trandate treatment and observe for development of hypotension
l *2. If SBP >230 or DBP 121 -140 mm. Hg for >= 2 readings 5 -10 mins apart : (1)(2)同上(1)(2) (3) If no satisfactory response , infuse sodium nitroprusside (0. 5 -10 ug/kg/min) (4) continue monitoring BP 19
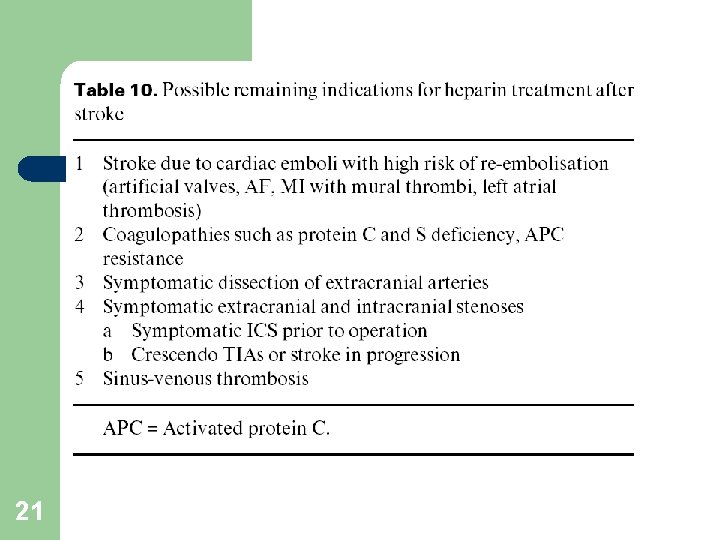
Anticoagulation l l 20 Heparin : not a standard therapy for all stroke subtypes Contraindication: large infarcts uncontrollable arterial hypertension advanced microvascular change in the brain
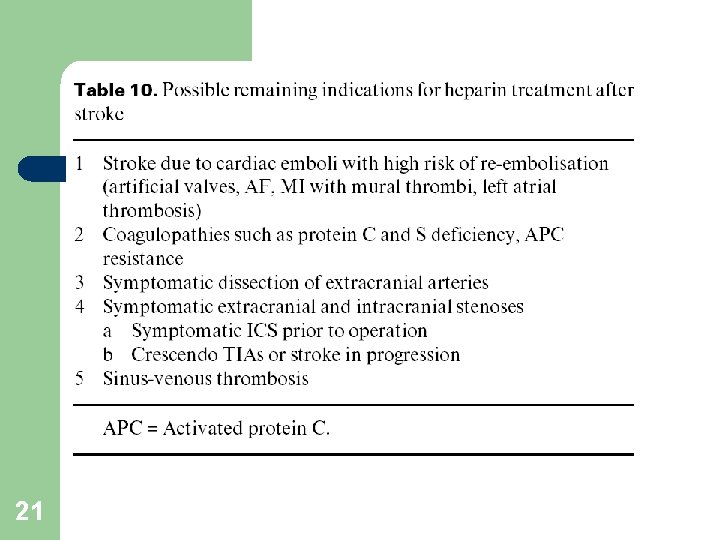
21
Brain edema, herniation Increased intracranial pressure (IICP) 1. 2. 3. 22 Brain edema IICP Risks of herniation
Brain edema , herniation increased intracranial pressure (IICP) l l l 23 Brain edema is defined as an increase in brain sodium and water content It occurs in many neurological conditions , such as stroke, trauma, tumors, infections, encephalopathies, and hydrocephalus ICP related to : brain tissue, blood , CSF. Normal ICP 7 -15 cm Hg. CPP=MAP-ICP, CPP should be kept > 70 mm. Hg.
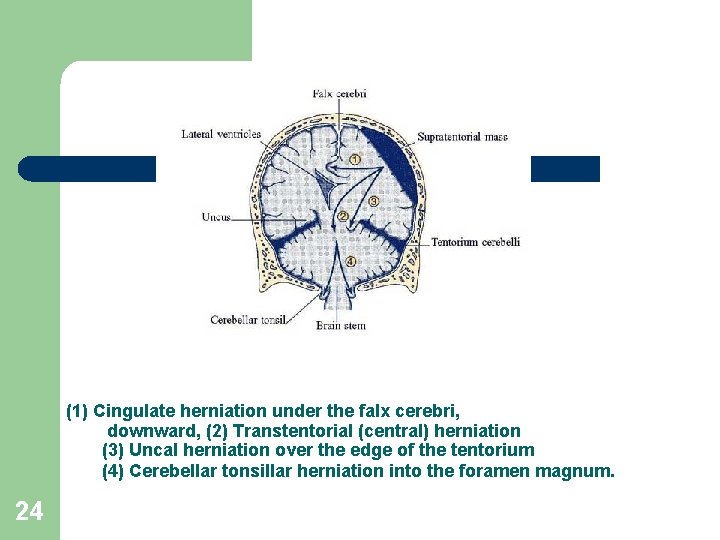
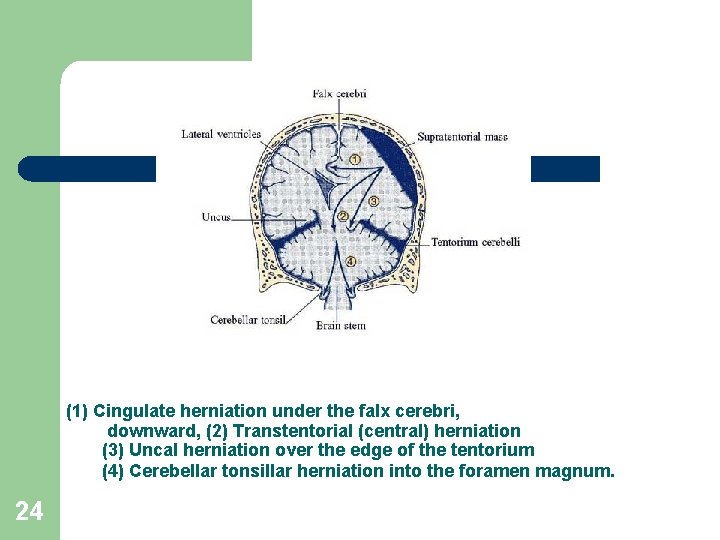
(1) Cingulate herniation under the falx cerebri, downward, (2) Transtentorial (central) herniation (3) Uncal herniation over the edge of the tentorium (4) Cerebellar tonsillar herniation into the foramen magnum. 24
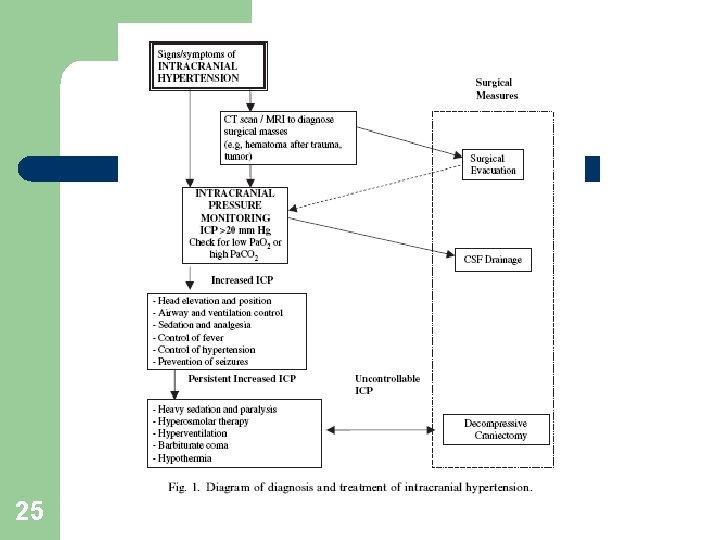
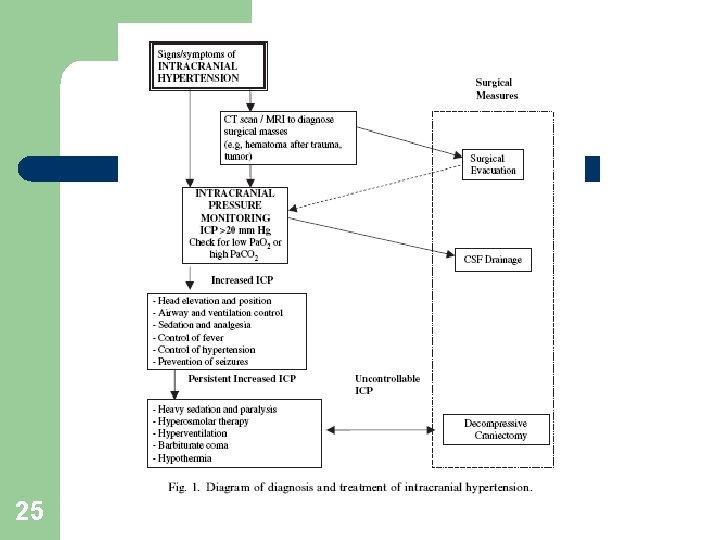
25
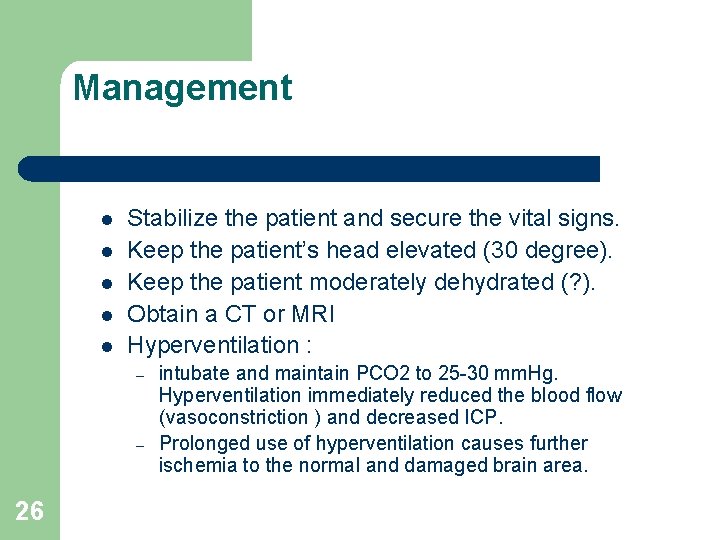
Management l l l Stabilize the patient and secure the vital signs. Keep the patient’s head elevated (30 degree). Keep the patient moderately dehydrated (? ). Obtain a CT or MRI Hyperventilation : – – 26 intubate and maintain PCO 2 to 25 -30 mm. Hg. Hyperventilation immediately reduced the blood flow (vasoconstriction ) and decreased ICP. Prolonged use of hyperventilation causes further ischemia to the normal and damaged brain area.
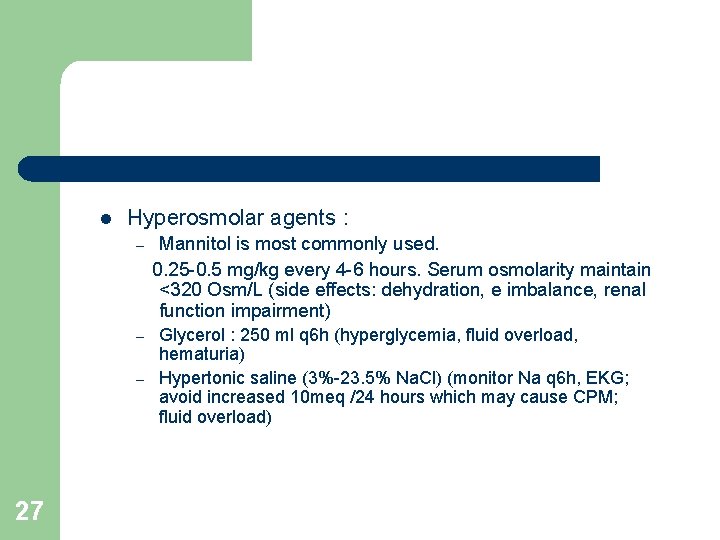
l Hyperosmolar agents : – – – 27 Mannitol is most commonly used. 0. 25 -0. 5 mg/kg every 4 -6 hours. Serum osmolarity maintain <320 Osm/L (side effects: dehydration, e imbalance, renal function impairment) Glycerol : 250 ml q 6 h (hyperglycemia, fluid overload, hematuria) Hypertonic saline (3%-23. 5% Na. Cl) (monitor Na q 6 h, EKG; avoid increased 10 meq /24 hours which may cause CPM; fluid overload)
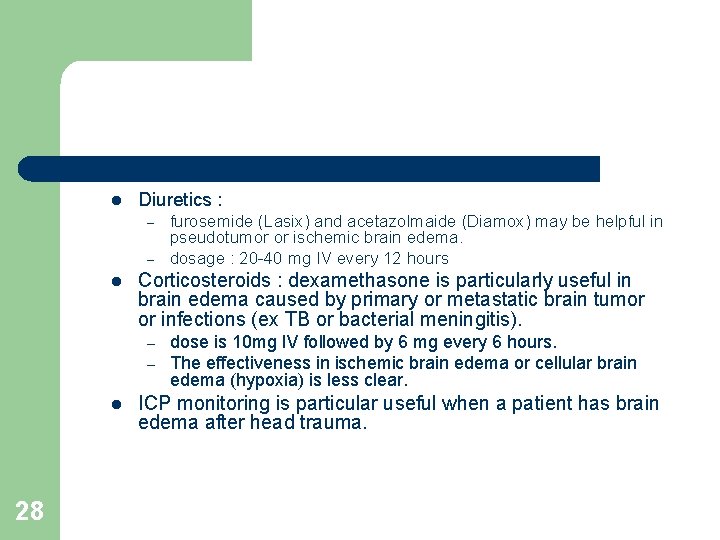
l Diuretics : – – l Corticosteroids : dexamethasone is particularly useful in brain edema caused by primary or metastatic brain tumor or infections (ex TB or bacterial meningitis). – – l 28 furosemide (Lasix) and acetazolmaide (Diamox) may be helpful in pseudotumor or ischemic brain edema. dosage : 20 -40 mg IV every 12 hours dose is 10 mg IV followed by 6 mg every 6 hours. The effectiveness in ischemic brain edema or cellular brain edema (hypoxia) is less clear. ICP monitoring is particular useful when a patient has brain edema after head trauma.
Status Epilepticus 1. 2. 3. 29 Definition Causes treatment
Status epilepticus – definition l l l 30 Seizures last longer than 10 minutes or if two or more seizures occur in close succession without recovery of consciousness Consider any seizure with duration greater than 5 minutes , not 30 minutes as historically defined Convulsive or non-convulsive , focal (epilepsy partialis continua ) or generalized
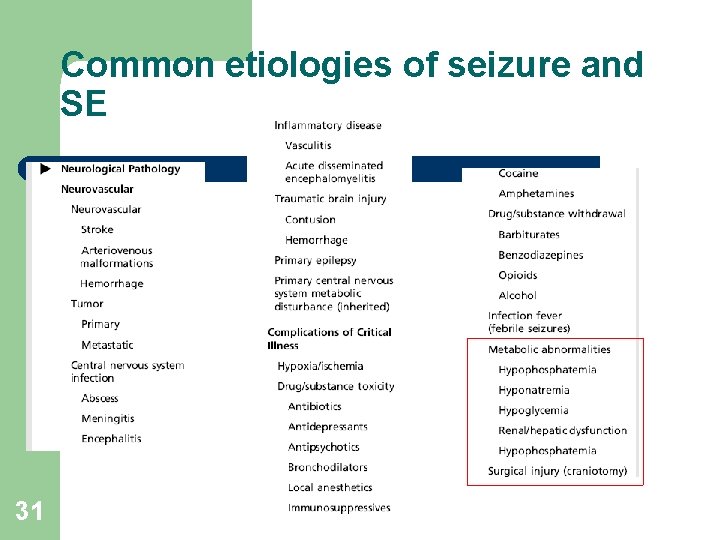
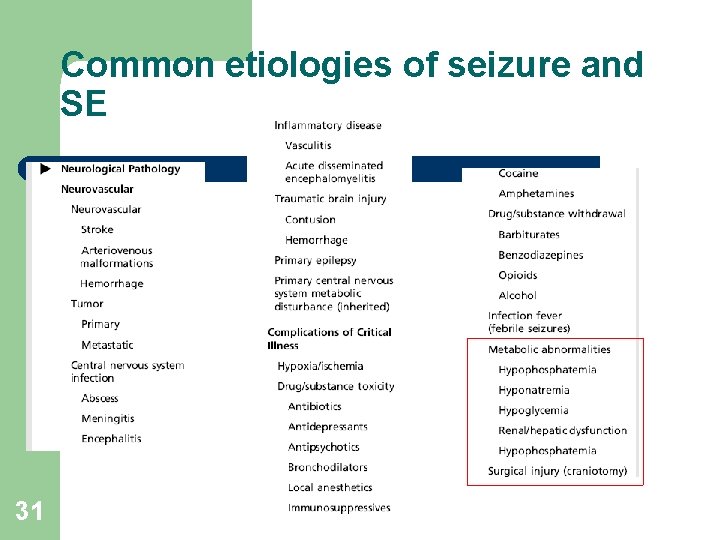
Common etiologies of seizure and SE 31
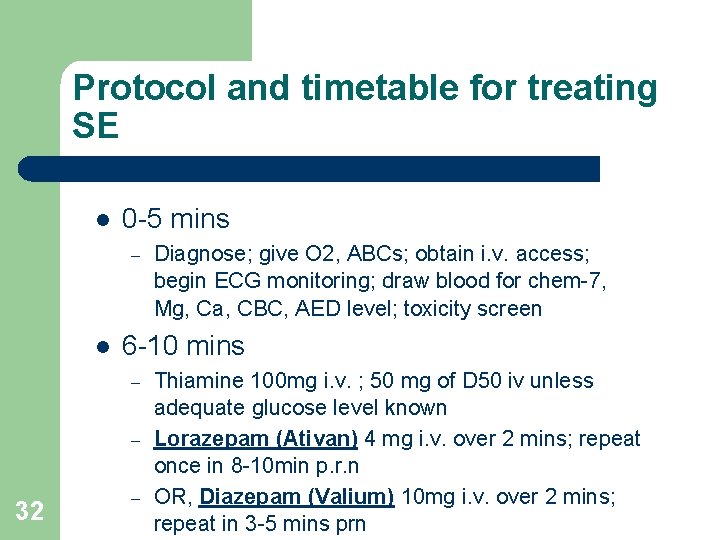
Protocol and timetable for treating SE l 0 -5 mins – l 6 -10 mins – – 32 Diagnose; give O 2, ABCs; obtain i. v. access; begin ECG monitoring; draw blood for chem-7, Mg, Ca, CBC, AED level; toxicity screen – Thiamine 100 mg i. v. ; 50 mg of D 50 iv unless adequate glucose level known Lorazepam (Ativan) 4 mg i. v. over 2 mins; repeat once in 8 -10 min p. r. n OR, Diazepam (Valium) 10 mg i. v. over 2 mins; repeat in 3 -5 mins prn
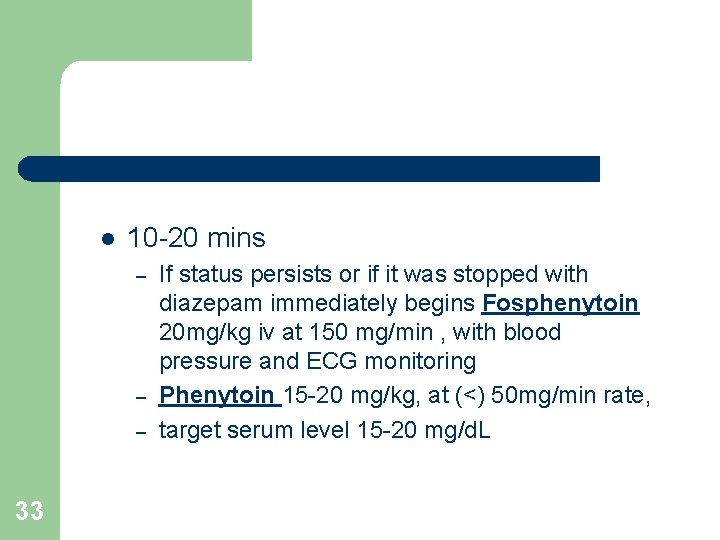
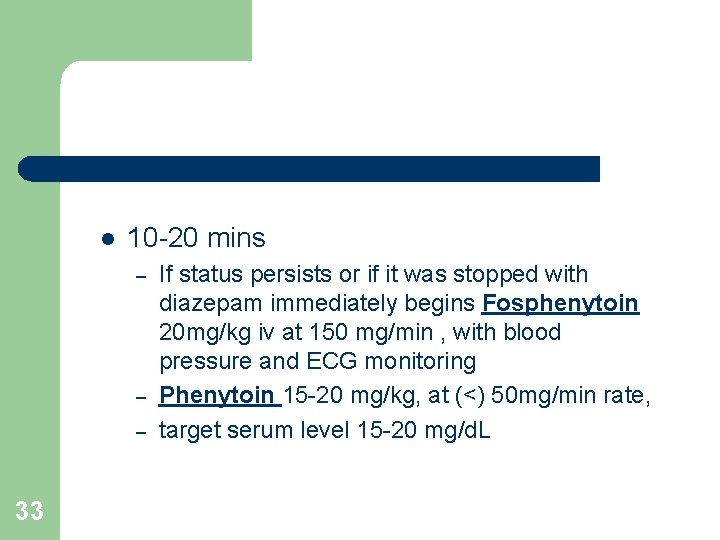
l 10 -20 mins – – – 33 If status persists or if it was stopped with diazepam immediately begins Fosphenytoin 20 mg/kg iv at 150 mg/min , with blood pressure and ECG monitoring Phenytoin 15 -20 mg/kg, at (<) 50 mg/min rate, target serum level 15 -20 mg/d. L
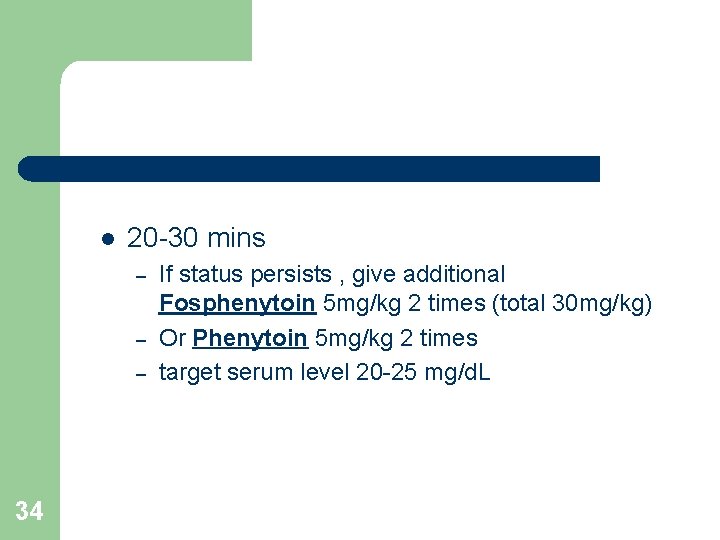
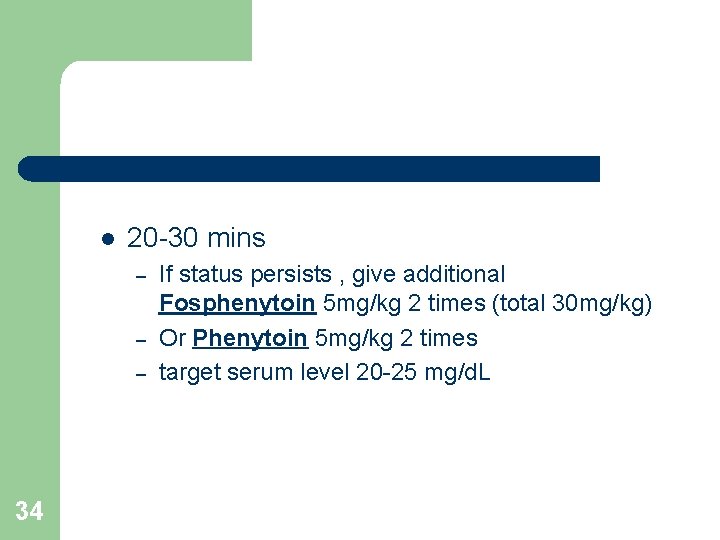
l 20 -30 mins – – – 34 If status persists , give additional Fosphenytoin 5 mg/kg 2 times (total 30 mg/kg) Or Phenytoin 5 mg/kg 2 times target serum level 20 -25 mg/d. L
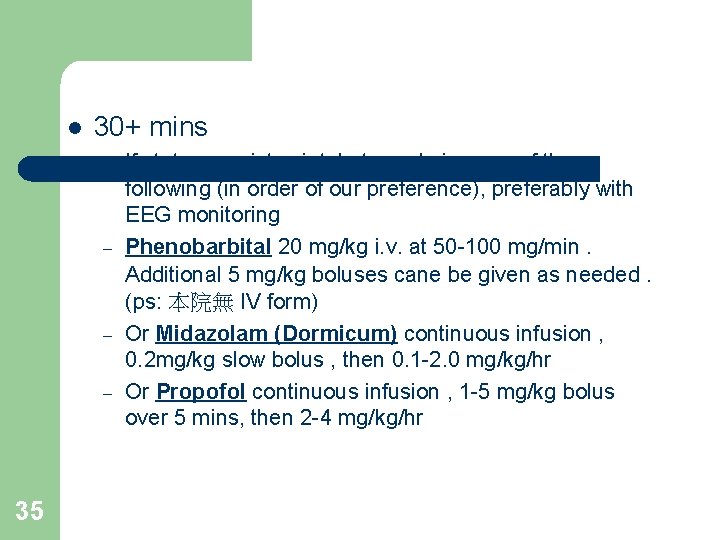
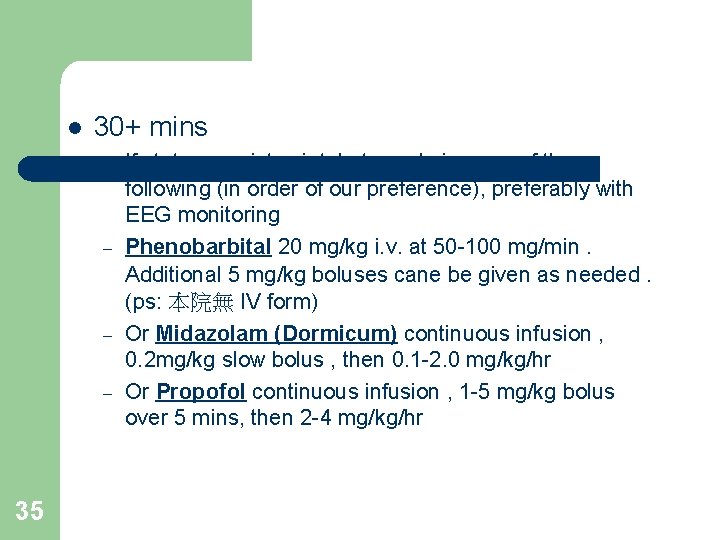
l 30+ mins – – 35 If status persists , intubate and give one of the following (in order of our preference), preferably with EEG monitoring Phenobarbital 20 mg/kg i. v. at 50 -100 mg/min. Additional 5 mg/kg boluses cane be given as needed. (ps: 本院無 IV form) Or Midazolam (Dormicum) continuous infusion , 0. 2 mg/kg slow bolus , then 0. 1 -2. 0 mg/kg/hr Or Propofol continuous infusion , 1 -5 mg/kg bolus over 5 mins, then 2 -4 mg/kg/hr
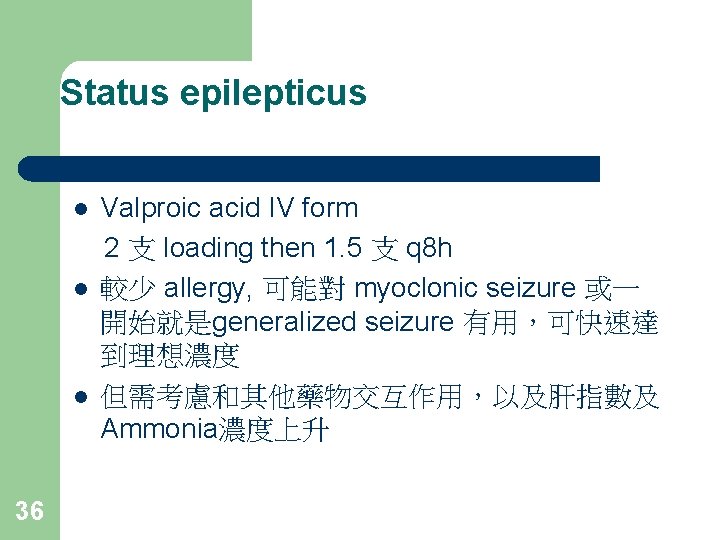
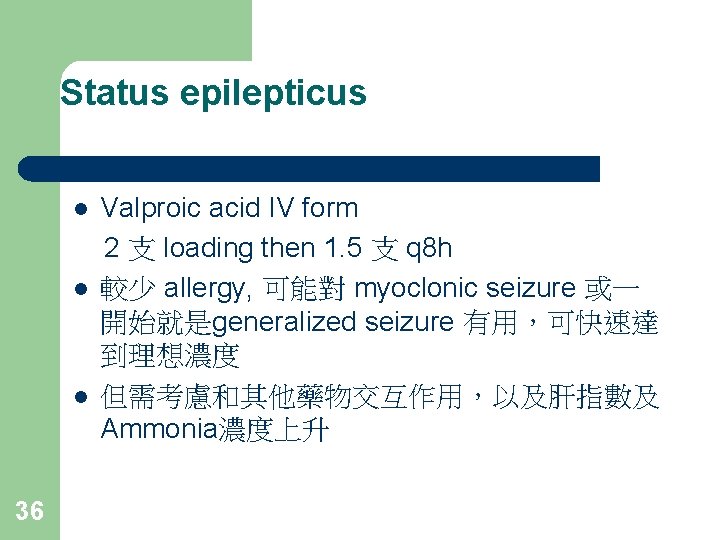
Status epilepticus l l l 36 Valproic acid IV form 2 支 loading then 1. 5 支 q 8 h 較少 allergy, 可能對 myoclonic seizure 或一 開始就是generalized seizure 有用,可快速達 到理想濃度 但需考慮和其他藥物交互作用,以及肝指數及 Ammonia濃度上升
Status epilepticus l l 37 Phenobarbital : 20 mg/kg i. v. , 5 mg/kg bolus (本院無 IV form) Gabapentin (Neurontin) Topiramate (Topamax) Rivotril
 Hepatotropic viruses
Hepatotropic viruses Raeburn forbes
Raeburn forbes Mppd unhas
Mppd unhas Torrance memorial tcu
Torrance memorial tcu Memorial christian hospital bangladesh
Memorial christian hospital bangladesh Chipping norton war memorial hospital
Chipping norton war memorial hospital Deepak memorial hospital
Deepak memorial hospital Shaukat khanum memorial cancer hospital and research centre
Shaukat khanum memorial cancer hospital and research centre Quentin burdick memorial hospital
Quentin burdick memorial hospital Patricia palacios mackay
Patricia palacios mackay Robbie mackay
Robbie mackay Mackay elementary school tenafly
Mackay elementary school tenafly George mackay brown hamnavoe
George mackay brown hamnavoe Dr veronica stanganelli
Dr veronica stanganelli Mst mackay
Mst mackay Katherine duer mackay
Katherine duer mackay Whyte and mackay swot analysis
Whyte and mackay swot analysis 2008 floods mackay
2008 floods mackay Glasgow coma scale video
Glasgow coma scale video Neurological examination
Neurological examination Neurological considerations in language acquisition
Neurological considerations in language acquisition Motor function neurological assessment
Motor function neurological assessment Neurological disease
Neurological disease Mrc sum score
Mrc sum score Muscle power neurological examination
Muscle power neurological examination The major premise of the genetic theory is that
The major premise of the genetic theory is that What is focal neurological signs
What is focal neurological signs Michael levitt uw
Michael levitt uw Villa fridheim haapsalu
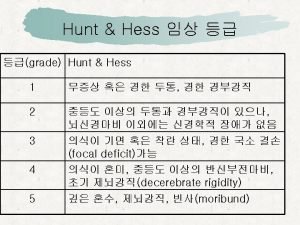
Villa fridheim haapsalu World federation of neurological surgeons scale
World federation of neurological surgeons scale Ao classification system
Ao classification system Stoneham centre physiotherapy
Stoneham centre physiotherapy Neurological assessment chart
Neurological assessment chart Ryan waters neurosurgeon
Ryan waters neurosurgeon Neurological based behavior
Neurological based behavior Pupil assessment
Pupil assessment Fudoscopy
Fudoscopy Is adhd a neurological disorder
Is adhd a neurological disorder