Liver Failure Mackay Memorial Hospital Department of Internal










- Slides: 32
Liver Failure Mackay Memorial Hospital Department of Internal Medicine Division of Gastroenterology R 4 陳泓達 97/6/22
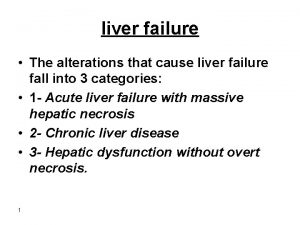
n Liver failure: Clinical syndrome: sudden loss of liver parenchymal and metabolic function Manifest as coagulopathy and encephalopathy
Acute liver failure : Defined as interval between onset of the illness and appearance of encephalopathy < 8 weeks n
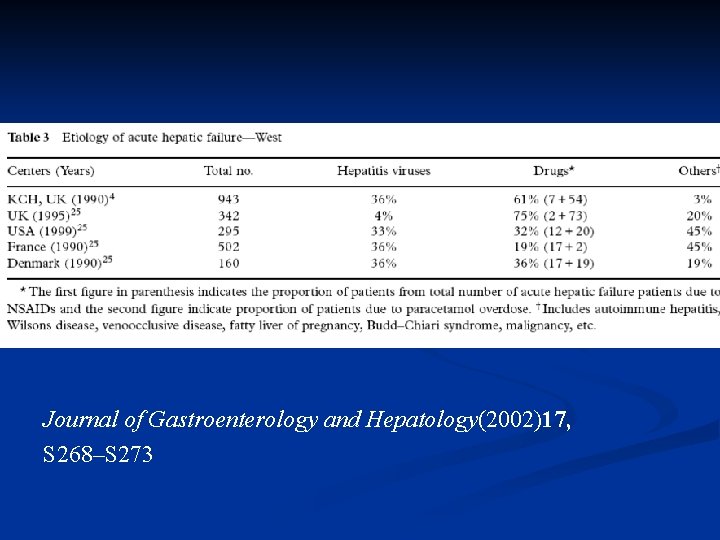
Etiology: Western countries: heterogenous, drugs (acetaminophen, NSAID), viruses Developing countries: viruses, regional Difference (endemic area ? ) n
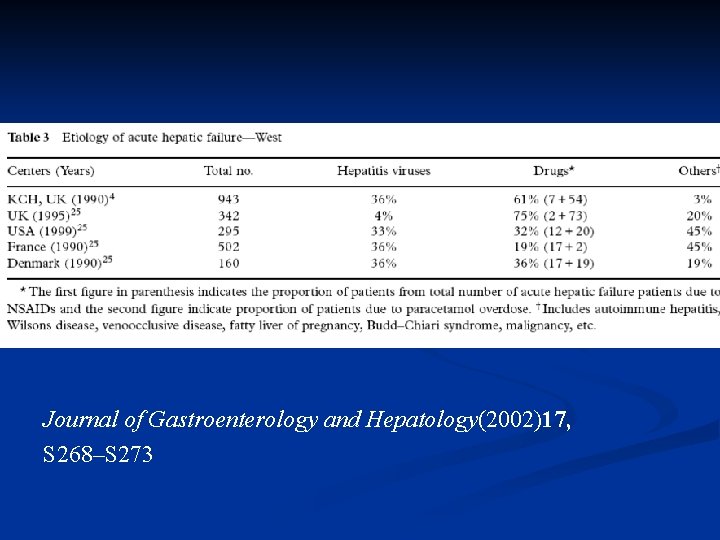
Journal of Gastroenterology and Hepatology(2002)17, S 268–S 273
Acetaminophen toxicity Idiosyncratic drug toxicity Hepatotropic viruses Miscellaneous causes Indeterminate acute liver failure (viruses can not be demonstrated ? )

Uncommon causes: Wilson’s disease, other infections (CMV, HSV, EBV), vascular abnormality, toxin, acute fatty liver of pregnancy, antoimmune hepatitis, ischemia, malignant infiltration n
Symptoms and signs: Jaundice, altered mental status, nausea/ vomiting, anorexia, fatigue, malaise, myalgia/arthralgia Most of them present hepatoencephalopathy and icteric appearance. n
Non-specific Management Hypoglycemia Encephalopathy Infections Hemorrhage Coagulopathy Hypotension(hypovolemia, vascular resistance ↓) Respiratory failure Renal failure Pancreatitis
Hypoglycemia: monitoring blood glucose, IV glucose supplement. n Infection: aseptic care, high index of suspicion, preemptive antibiotic. n Hemorrhage (i. e. GI): NG placement, H 2 blocker or PPI. n Hypotension: hemodynamic monitoring or central pressures, volume repletion n
Respiratory failure (ARDS): mechanical ventilation. n Renal failure (hypovolemia, hepatorenal syndrome, ATN): hemodynamic monitor, central pressure, volume repletion, avoid nephrotoxic agent n
Encephalopathy major complication n precise mechanism remains unclear n Hypothesis: Ammonia production n Treatment toward reducing ammonia production n Watch out airway, prevent aspiration n
Encephalopathy Stage 1: day-night reversal, mild confusion, somnolence n Stage 2: confusion, drowsiness n Stage 3: stupor n Stage 4: coma n

Encephalopathy Predisposing factor of hepatic encephalopathy: GI bleeding, increased protein intake, hypokalemic alkalosis, hyponatremia, infection, constipation, hypoxia, infection, sedatives and tranquilizers
Encephalopathy TX upon ammonia hypothesis n Correction of hypokalemia n Reduction in ammoniagenic substrates: cleansing enemas and dietary protein restriction. n Lactulose: improved encephalopathy, but not improved outcome. Dose 2 -3 soft stools per day
Encephalopathy Oral antibiotics: neomycin lack of evidence nephrotoxicity limited use. n

Cerebral Edema Cerebral edema develops in 75 - 80 % of patients with grade IV encephalopathy. n precise mechanism : not completely understood n Possible contributing factor: osmotic derangement in astrocytes changes in cellular metabolism alterations in cerebral blood flow n

Cerebral Edema Clinical manifestations: ↑intracranial pressure (ICP) and brainstem Herniation the most common causes of death in fulminant hepatic failure ischemic and hypoxic injury to the brain hypertension, bradycardia, and irregular respirations, ↑ muscle tone, hyperreflexia n

Cerebral Edema Monitoring of ICP: routinely used by more than one-half of liver transplantation programs in the United States n Tx: to maintain ICP below 20 mm. Hg and the CPP above 50 mm. Hg. n
Coagulopathy diminished capacity of the failing liver to synthesize coagulation factors. n The most common bleeding site: GI tract. n Prophylactic administration of FFP: not recommended. performed before transplant or invasive procedure n

Specific Treatment ACT intoxication: charcol followed by NAC n Drug induced hepatotoxicity: discontinue drugs supportive treatment n Viral hepatitis: HBV: anti-HBV treatment, lamivudine HSV/varicella zoster: acyclovir : others: supportive care n

Wilson’s disease: early diagnosis liver transplant n autoimmune hepatitis: confirm diagnosis (liver biopsy), corticosteroid liver transplant n acute fatty liver of pregnancy or the HELLP syndrome: obstetrical services, and expeditious delivery are recommended n

Acute ischemic injury (shock liver): cardiovascular support n Malignant infiltration: liver biopsy for : diagnosis treat underlying disease. n Indeterminate etiology: consider biopsy for diagnosis and further guide of treatment n
Liver transplant: remain backbone of treatment of fulminant hepatic failure reliable criteria to identify these patients who really need transplant. remain unresolved in fulminant hepatic failure. n
At King’s College hospital in London (not due to ACT) either PT>100 second or the presence of any three of the following variables: 1. age < 10 or > 40 years ; 2. an etiology of non-A, non-B hepatitis, halothane, drug induced liver failure; 3. duration of jaundice before onset of encephalopathy > 7 days, prothrombin time >50 s, and serum bilirubin > 300 mmol/L.

Encephalopathy Coagulopathy (PT)
Liver transplant Criteria: In chronic liver disease most commonly used prognostic model MELD score (Model for End-stage Liver Disease ) 3. 8[Ln serum bilirubin (mg/d. L)] + 11. 2[Ln INR] + 9. 6[Ln serum creatinine (mg/d. L)] + 6. 4 Ln: natural logarithm. n
Liver transplant n 1. 2. 3. CONTRAINDICATIONS: Cardiopulmonary disease can not be corrected, or preclude surgery. Malignancy outside of the liver within 5 years of evaluation, or can not be cured. Active alcohol and drug use

n Advanced age and HIV disease: relative contra -indication (site-specific management)
Liver support system Non-cell-based: plasmapheresis and charcoalbased hemoabsorption n Cell-based systems : known as bioartificial liver support systems n
Liver support system Non-cell-based: not improved survival. Available systems: molecular adsorbents recirculation system (MARS) n Cell-based systems: undergoing trial. n
 Hepatotropic viruses
Hepatotropic viruses Neonatal liver failure
Neonatal liver failure Hepatic encephalopathy staging
Hepatic encephalopathy staging Fhf
Fhf Acute liver failure criteria
Acute liver failure criteria Hepatic encephalopathy staging
Hepatic encephalopathy staging Failure to sense
Failure to sense Failure to sense
Failure to sense Ductile fracture surface
Ductile fracture surface Deepak memorial hospital
Deepak memorial hospital Quentin burdick memorial hospital
Quentin burdick memorial hospital Memorial christian hospital
Memorial christian hospital Chipping norton war memorial hospital
Chipping norton war memorial hospital Shaukat khanum pharmacy
Shaukat khanum pharmacy Torrance memorial transitional care unit
Torrance memorial transitional care unit Mckay elementary school
Mckay elementary school Dr veronica stanganelli
Dr veronica stanganelli Whyte and mackay swot analysis
Whyte and mackay swot analysis Patricia palacios mackay
Patricia palacios mackay George mackay brown hamnavoe
George mackay brown hamnavoe Katherine duer mackay
Katherine duer mackay Mst mackay
Mst mackay 2008 floods mackay
2008 floods mackay Minty pi
Minty pi Qms
Qms Environmental internal failure costs examples
Environmental internal failure costs examples Define hospital pharmacy
Define hospital pharmacy Hesf1
Hesf1 What is the organizational structure of a hospital
What is the organizational structure of a hospital Flagler hospital billing
Flagler hospital billing Swot analysis for internal audit
Swot analysis for internal audit Miami dade county internal services department
Miami dade county internal services department Elements of internal control system
Elements of internal control system