NEUROLOGICAL EMERGENCIES STROKE WHAT IS A STROKE Neurological
- Slides: 31
NEUROLOGICAL EMERGENCIES: STROKE
WHAT IS A STROKE? “Neurological deficit of cerebrovascular cause that persists beyond 24 hours or is interrupted by death within 24 hours. ” - WHO Death or injury of brain tissue from oxygen deprivation.
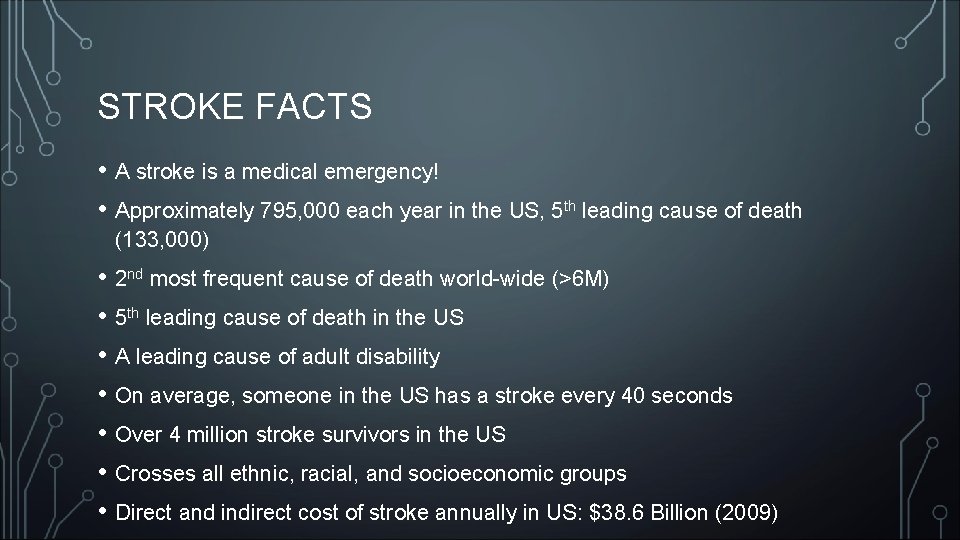
STROKE FACTS • A stroke is a medical emergency! • Approximately 795, 000 each year in the US, 5 th leading cause of death (133, 000) • 2 nd most frequent cause of death world-wide (>6 M) • 5 th leading cause of death in the US • A leading cause of adult disability • On average, someone in the US has a stroke every 40 seconds • Over 4 million stroke survivors in the US • Crosses all ethnic, racial, and socioeconomic groups • Direct and indirect cost of stroke annually in US: $38. 6 Billion (2009)
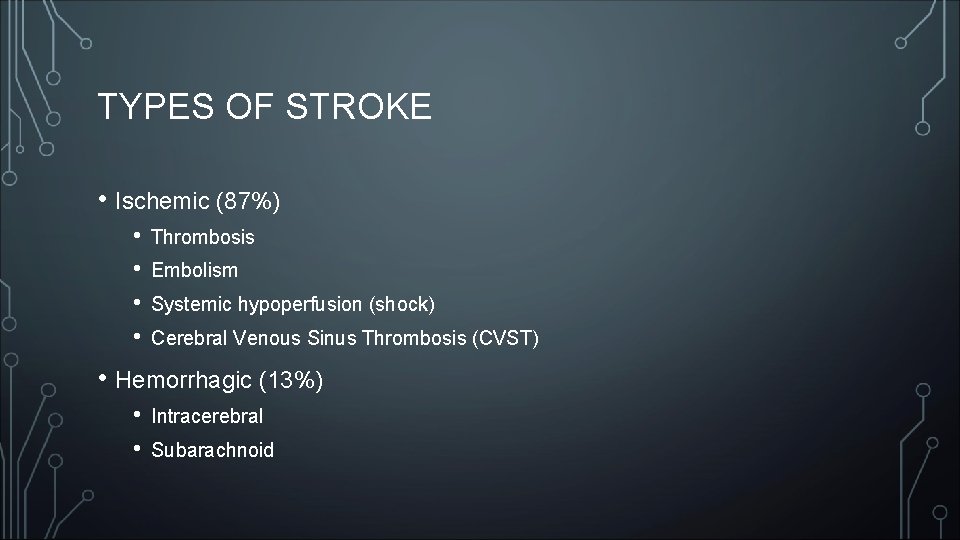
TYPES OF STROKE • Ischemic (87%) • • Thrombosis Embolism Systemic hypoperfusion (shock) Cerebral Venous Sinus Thrombosis (CVST) • Hemorrhagic (13%) • • Intracerebral Subarachnoid
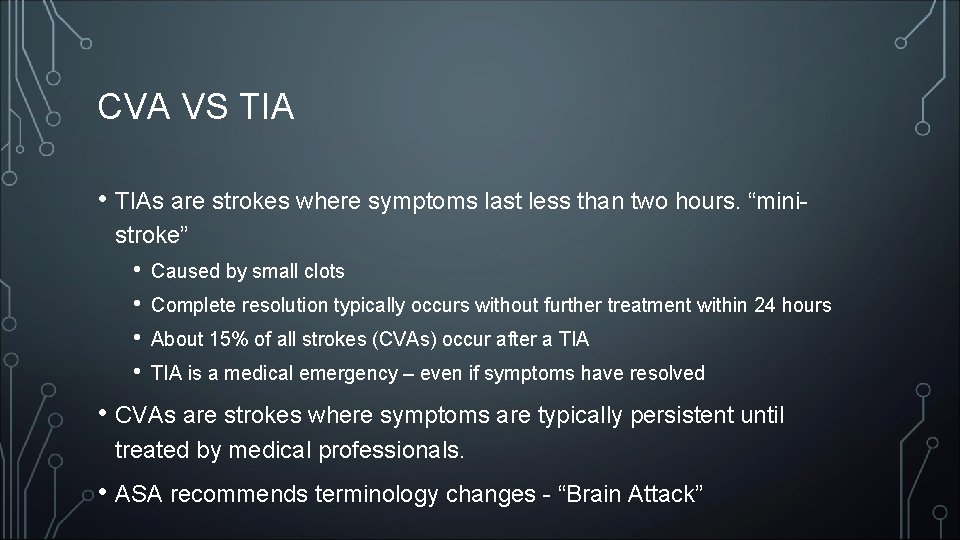
CVA VS TIA • TIAs are strokes where symptoms last less than two hours. “ministroke” • • Caused by small clots Complete resolution typically occurs without further treatment within 24 hours About 15% of all strokes (CVAs) occur after a TIA is a medical emergency – even if symptoms have resolved • CVAs are strokes where symptoms are typically persistent until treated by medical professionals. • ASA recommends terminology changes - “Brain Attack”
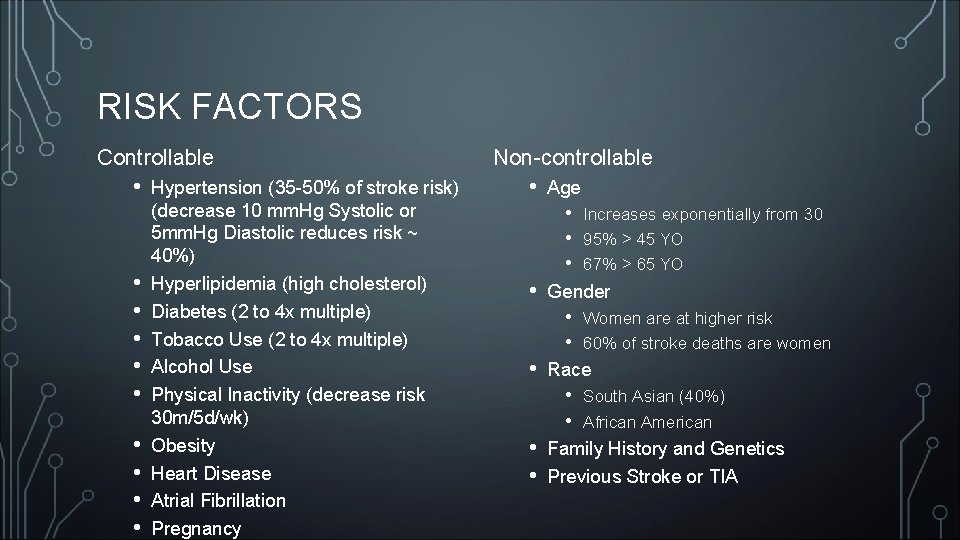
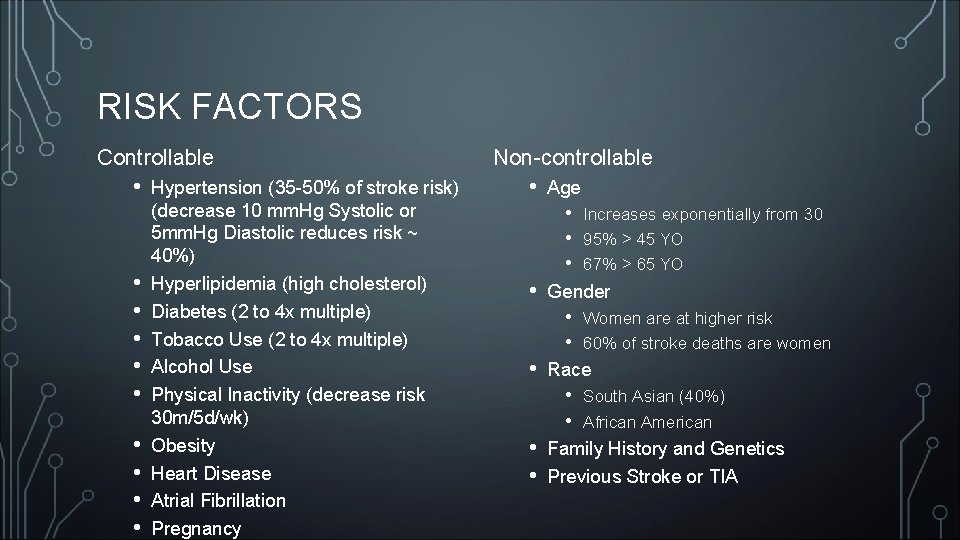
RISK FACTORS Controllable • • • Hypertension (35 -50% of stroke risk) (decrease 10 mm. Hg Systolic or 5 mm. Hg Diastolic reduces risk ~ 40%) Hyperlipidemia (high cholesterol) Diabetes (2 to 4 x multiple) Tobacco Use (2 to 4 x multiple) Alcohol Use Physical Inactivity (decrease risk 30 m/5 d/wk) Obesity Heart Disease Atrial Fibrillation Pregnancy Non-controllable • Age • • Gender • • • Women are at higher risk 60% of stroke deaths are women Race • • Increases exponentially from 30 95% > 45 YO 67% > 65 YO South Asian (40%) African American Family History and Genetics Previous Stroke or TIA
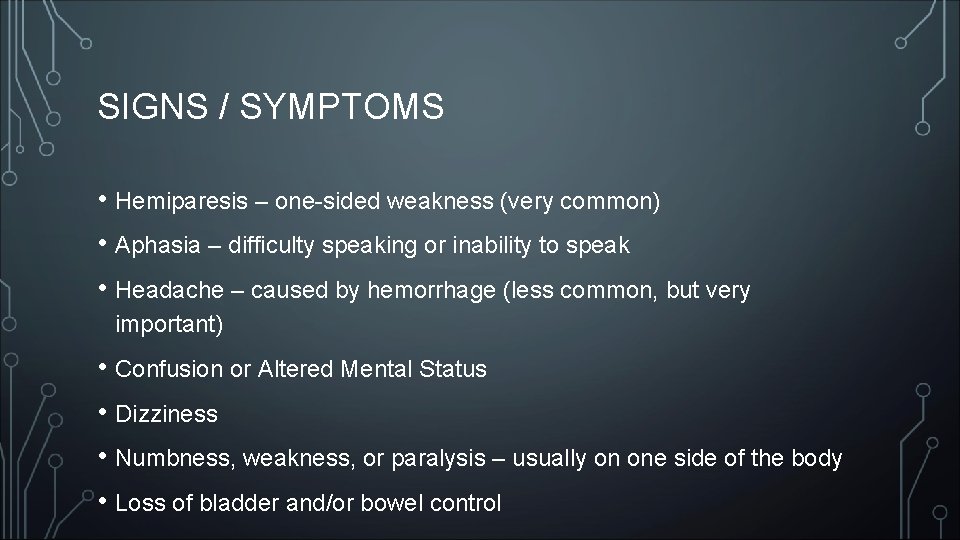
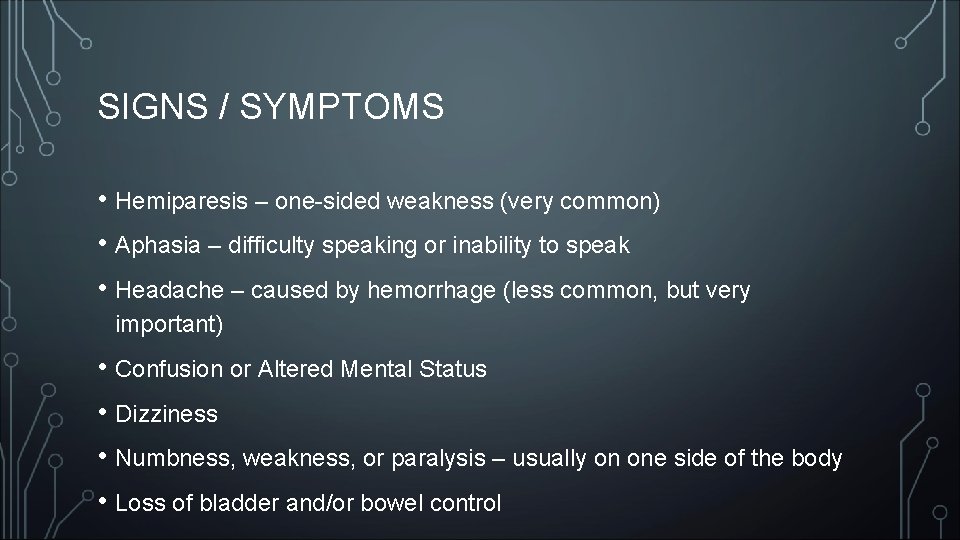
SIGNS / SYMPTOMS • Hemiparesis – one-sided weakness (very common) • Aphasia – difficulty speaking or inability to speak • Headache – caused by hemorrhage (less common, but very important) • Confusion or Altered Mental Status • Dizziness • Numbness, weakness, or paralysis – usually on one side of the body • Loss of bladder and/or bowel control
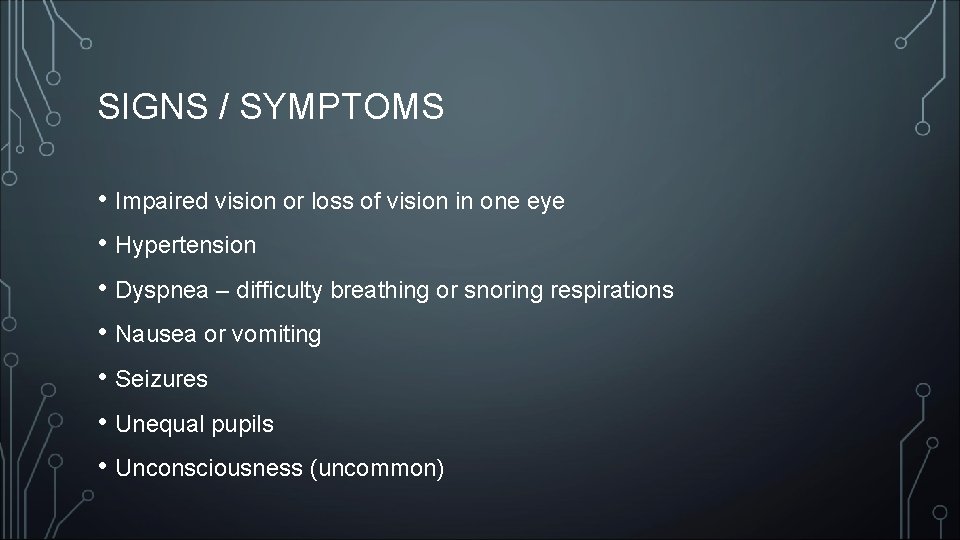
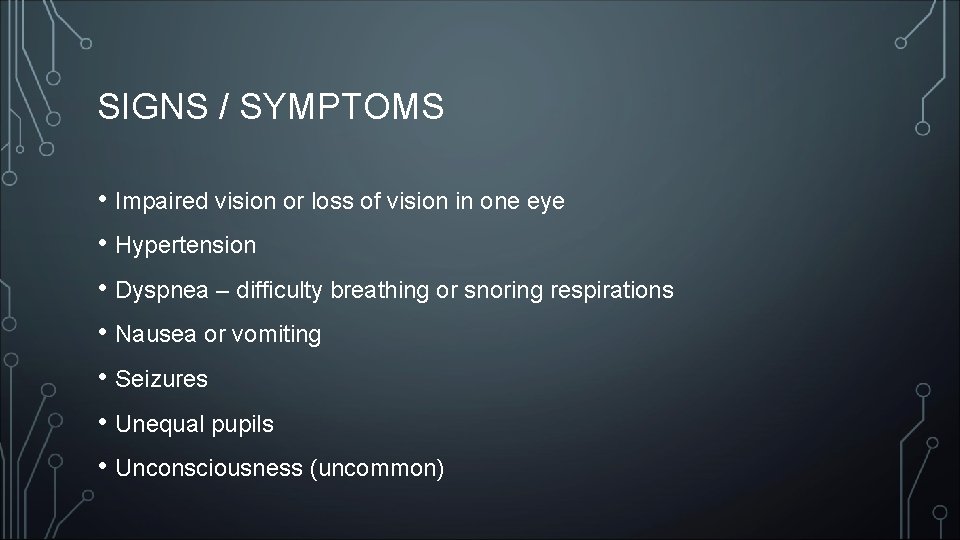
SIGNS / SYMPTOMS • Impaired vision or loss of vision in one eye • Hypertension • Dyspnea – difficulty breathing or snoring respirations • Nausea or vomiting • Seizures • Unequal pupils • Unconsciousness (uncommon)
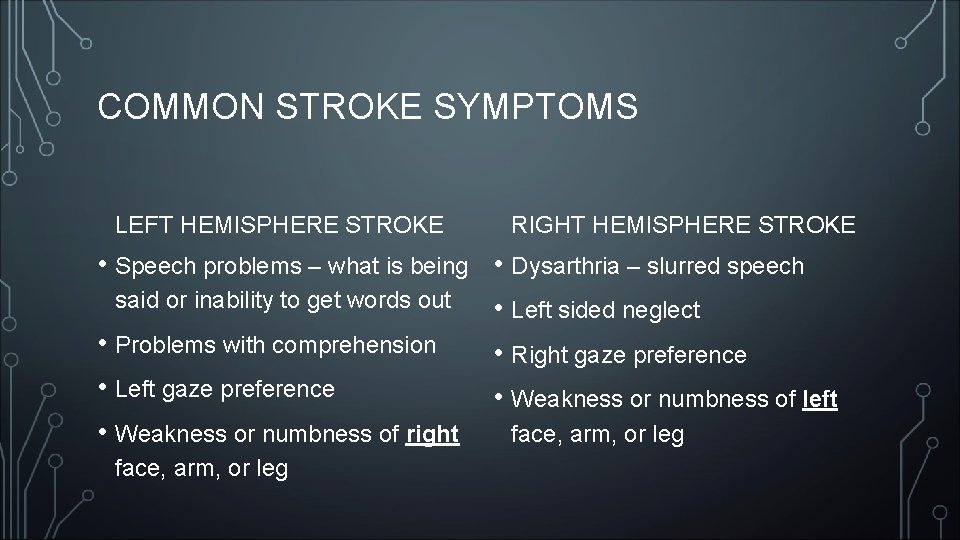
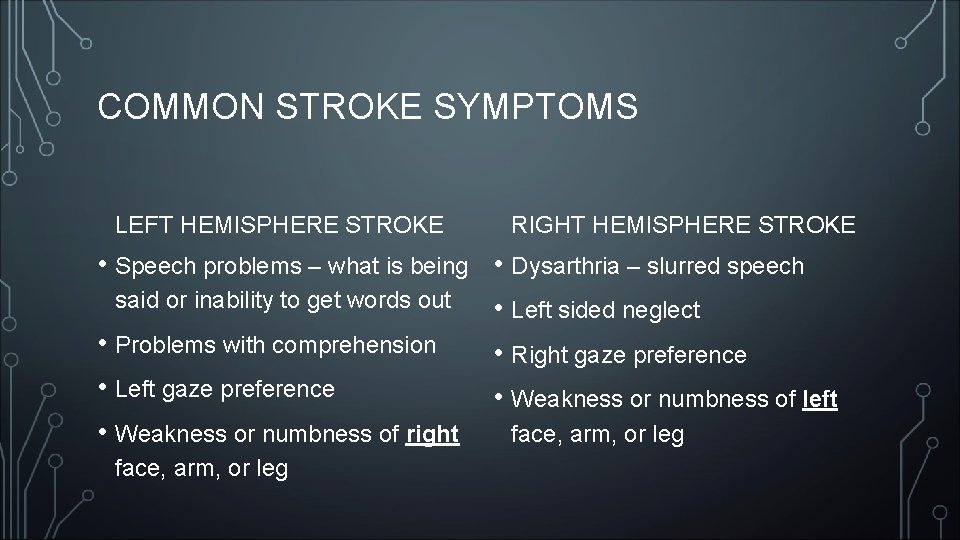
COMMON STROKE SYMPTOMS LEFT HEMISPHERE STROKE RIGHT HEMISPHERE STROKE • Speech problems – what is being • Dysarthria – slurred speech said or inability to get words out • Left sided neglect • Problems with comprehension • Right gaze preference • Left gaze preference • Weakness or numbness of left • Weakness or numbness of right face, arm, or leg
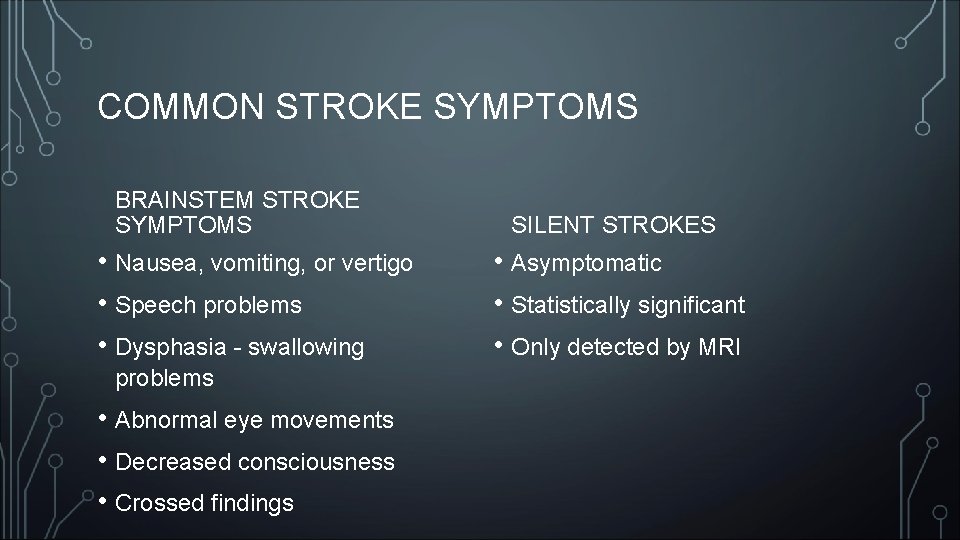
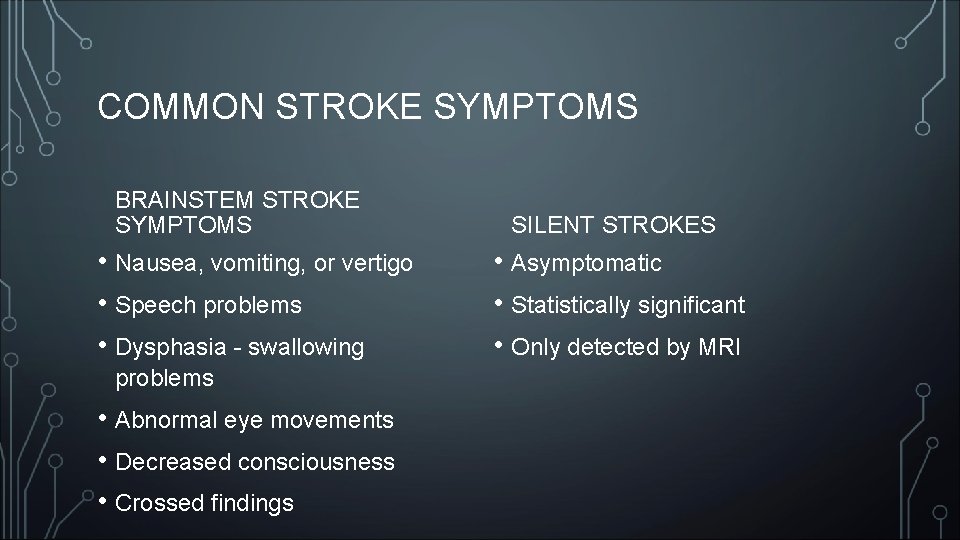
COMMON STROKE SYMPTOMS BRAINSTEM STROKE SYMPTOMS • Nausea, vomiting, or vertigo • Speech problems • Dysphasia - swallowing problems • Abnormal eye movements • Decreased consciousness • Crossed findings SILENT STROKES • Asymptomatic • Statistically significant • Only detected by MRI
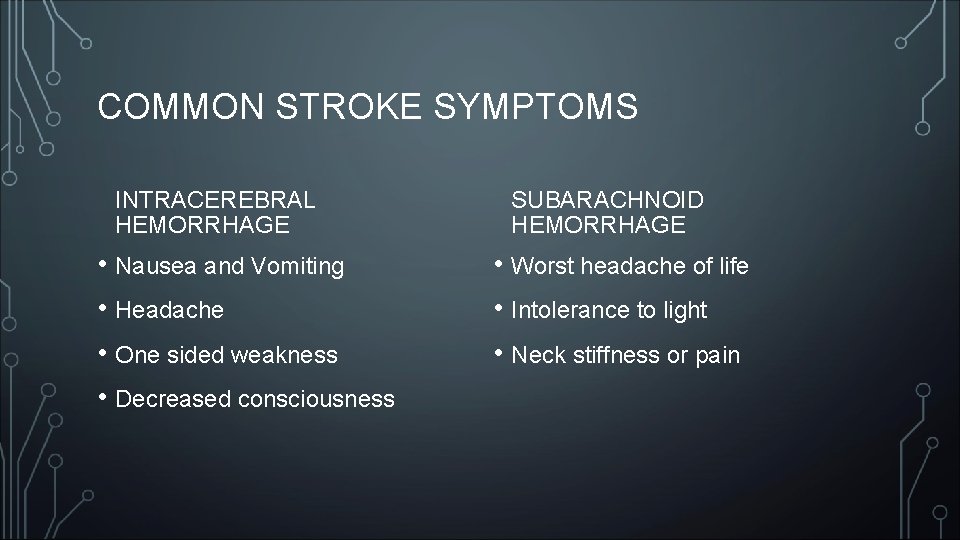
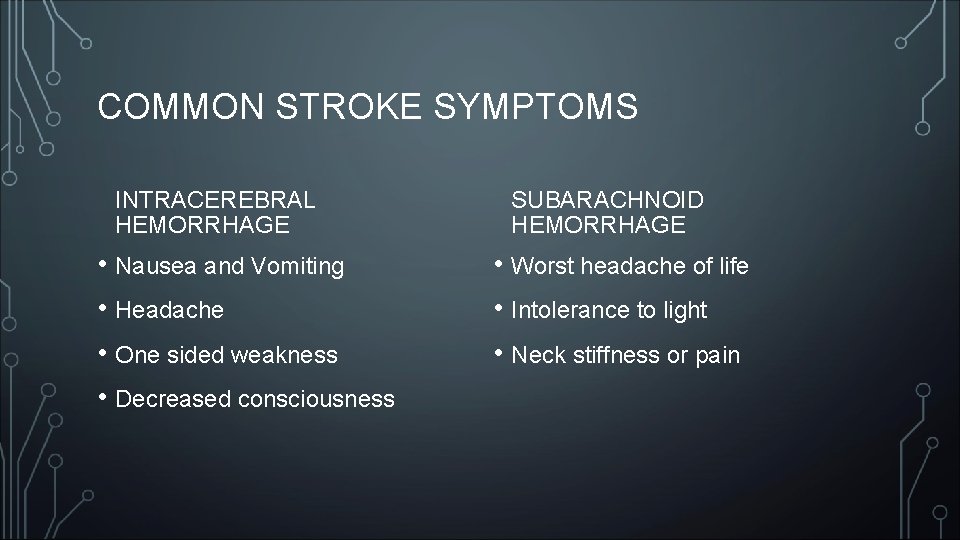
COMMON STROKE SYMPTOMS INTRACEREBRAL HEMORRHAGE • Nausea and Vomiting • Headache • One sided weakness • Decreased consciousness SUBARACHNOID HEMORRHAGE • Worst headache of life • Intolerance to light • Neck stiffness or pain
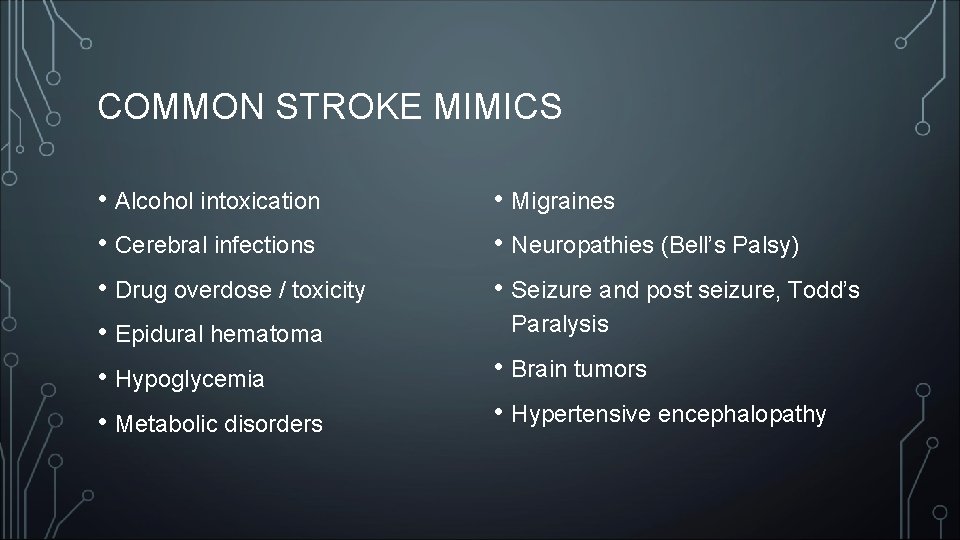
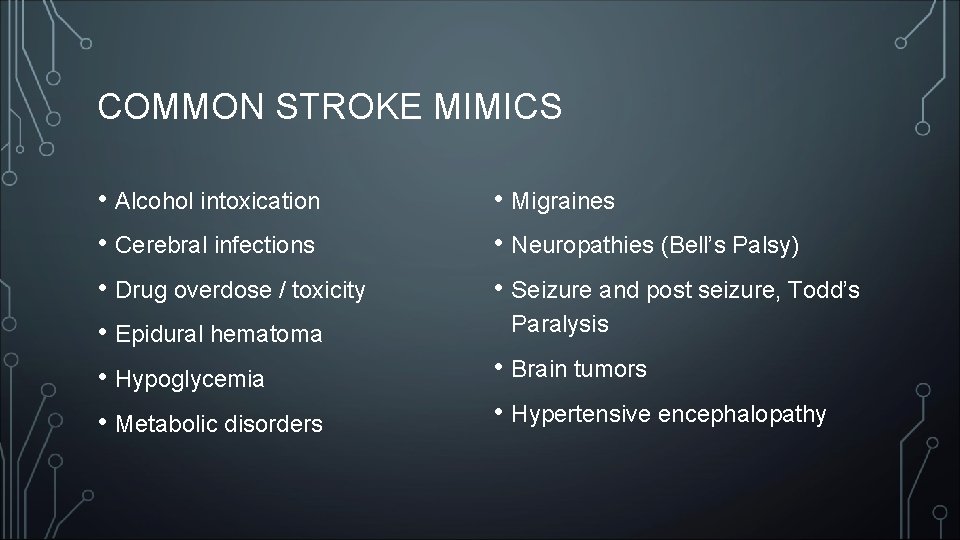
COMMON STROKE MIMICS • Alcohol intoxication • Cerebral infections • Drug overdose / toxicity • Epidural hematoma • Hypoglycemia • Metabolic disorders • Migraines • Neuropathies (Bell’s Palsy) • Seizure and post seizure, Todd’s Paralysis • Brain tumors • Hypertensive encephalopathy
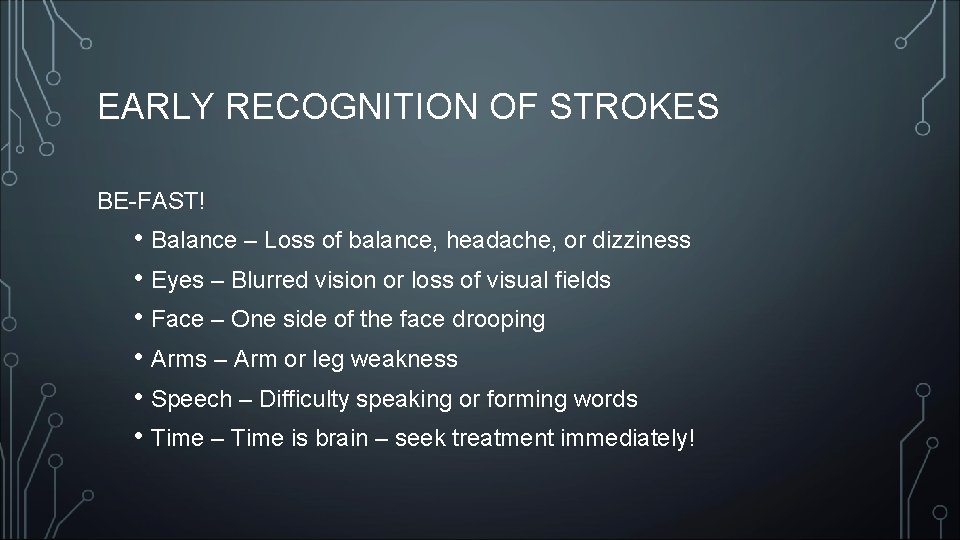
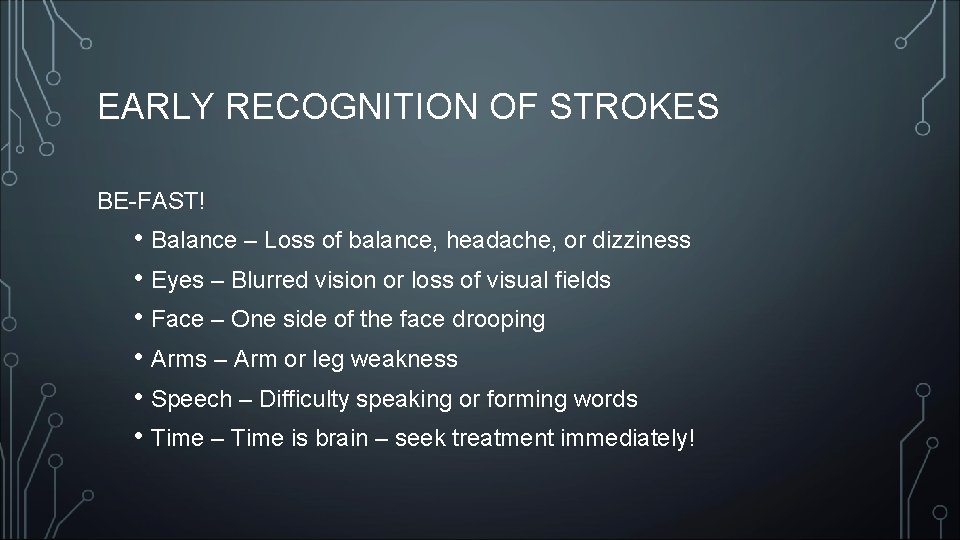
EARLY RECOGNITION OF STROKES BE-FAST! • Balance – Loss of balance, headache, or dizziness • Eyes – Blurred vision or loss of visual fields • Face – One side of the face drooping • Arms – Arm or leg weakness • Speech – Difficulty speaking or forming words • Time – Time is brain – seek treatment immediately!
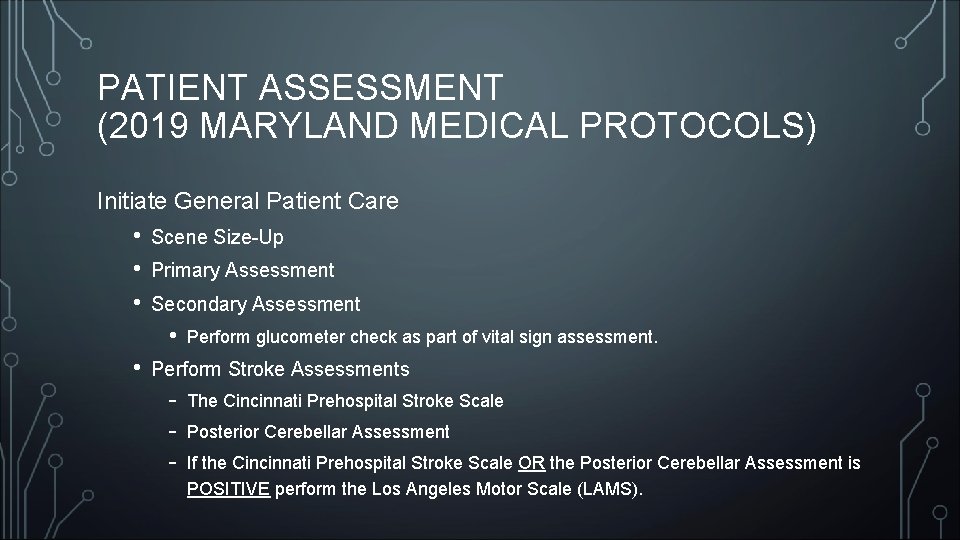
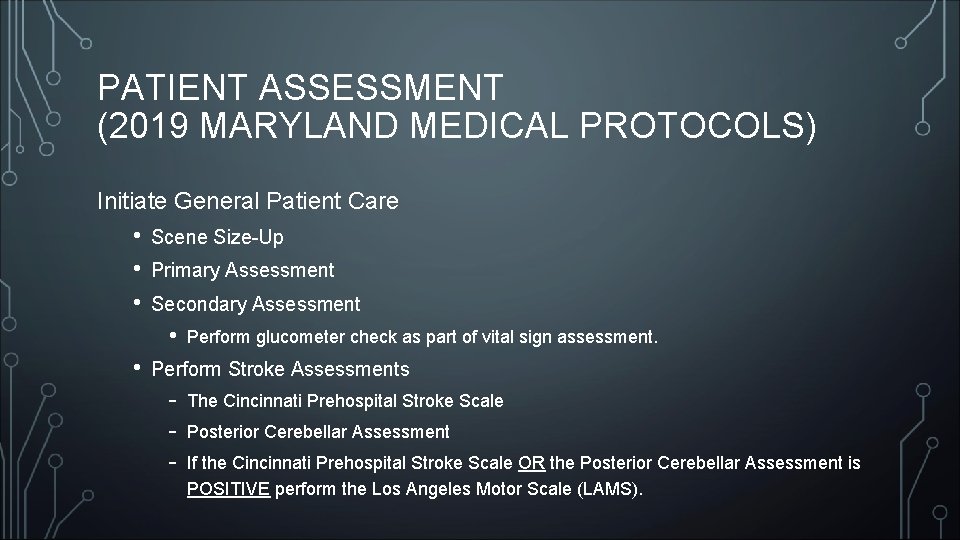
PATIENT ASSESSMENT (2019 MARYLAND MEDICAL PROTOCOLS) Initiate General Patient Care • • • Scene Size-Up Primary Assessment Secondary Assessment • • Perform glucometer check as part of vital sign assessment. Perform Stroke Assessments - The Cincinnati Prehospital Stroke Scale Posterior Cerebellar Assessment If the Cincinnati Prehospital Stroke Scale OR the Posterior Cerebellar Assessment is POSITIVE perform the Los Angeles Motor Scale (LAMS).
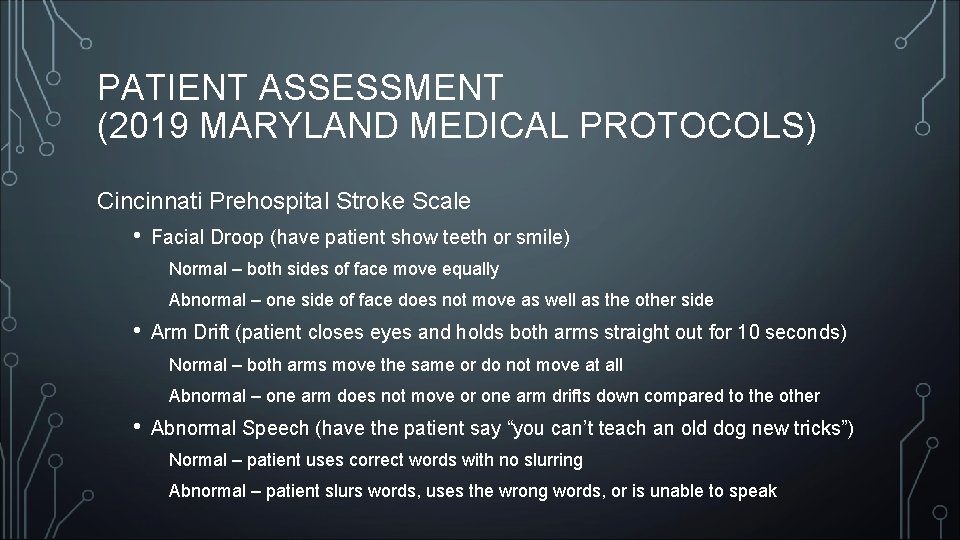
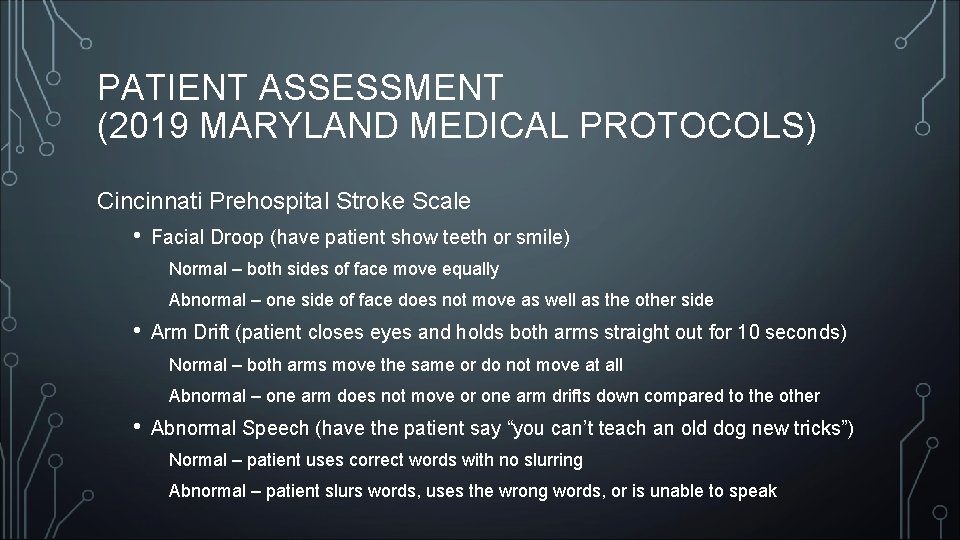
PATIENT ASSESSMENT (2019 MARYLAND MEDICAL PROTOCOLS) Cincinnati Prehospital Stroke Scale • Facial Droop (have patient show teeth or smile) Normal – both sides of face move equally Abnormal – one side of face does not move as well as the other side • Arm Drift (patient closes eyes and holds both arms straight out for 10 seconds) Normal – both arms move the same or do not move at all Abnormal – one arm does not move or one arm drifts down compared to the other • Abnormal Speech (have the patient say “you can’t teach an old dog new tricks”) Normal – patient uses correct words with no slurring Abnormal – patient slurs words, uses the wrong words, or is unable to speak
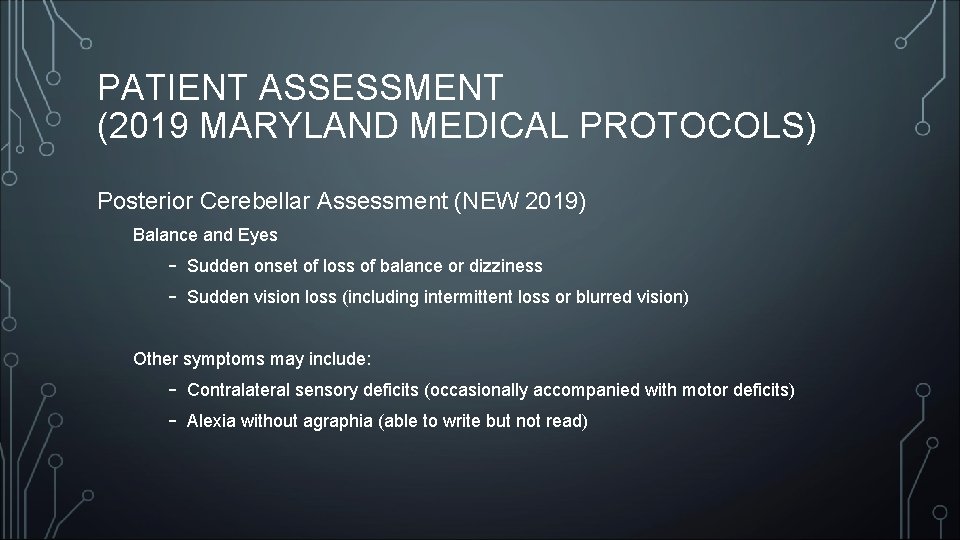
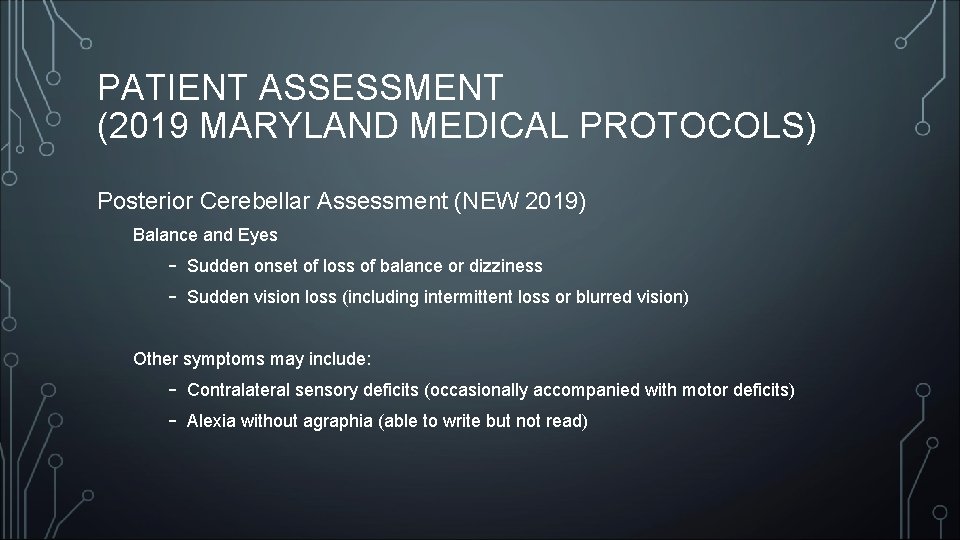
PATIENT ASSESSMENT (2019 MARYLAND MEDICAL PROTOCOLS) Posterior Cerebellar Assessment (NEW 2019) Balance and Eyes - Sudden onset of loss of balance or dizziness Sudden vision loss (including intermittent loss or blurred vision) Other symptoms may include: - Contralateral sensory deficits (occasionally accompanied with motor deficits) Alexia without agraphia (able to write but not read)
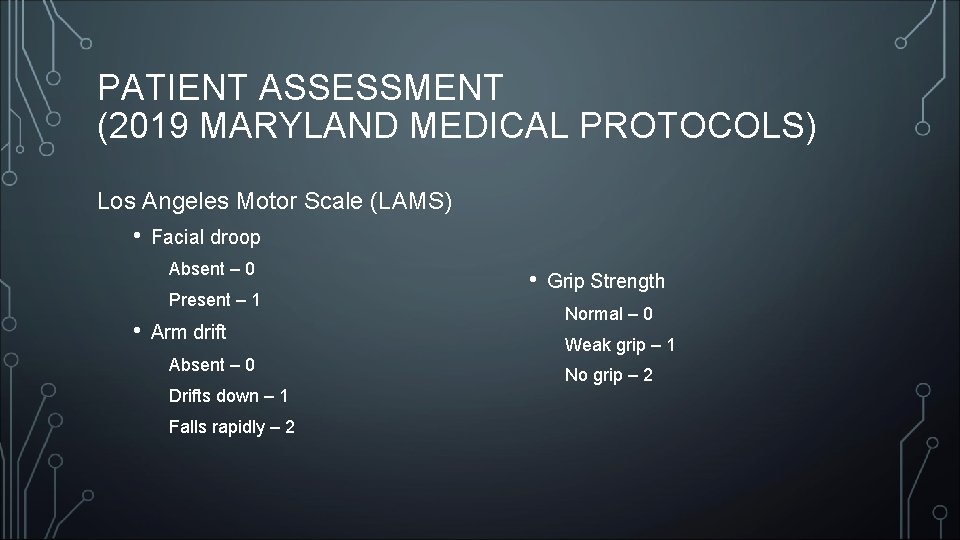
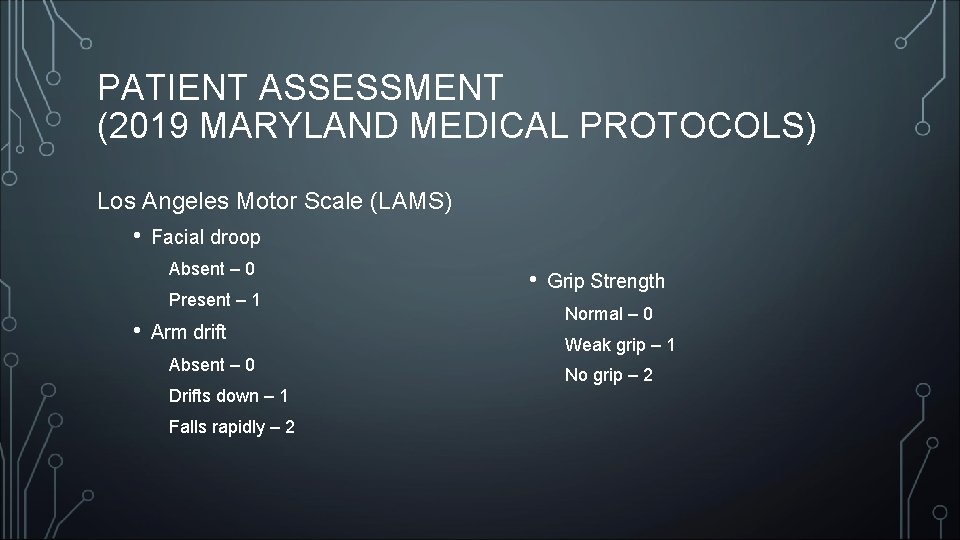
PATIENT ASSESSMENT (2019 MARYLAND MEDICAL PROTOCOLS) Los Angeles Motor Scale (LAMS) • Facial droop Absent – 0 Present – 1 • Arm drift Absent – 0 Drifts down – 1 Falls rapidly – 2 • Grip Strength Normal – 0 Weak grip – 1 No grip – 2
PATIENT ASSESSMENT (2019 MARYLAND MEDICAL PROTOCOLS) Strokes during pregnancy or shortly after giving birth are rare – but a significant increase recently. Fibrinolytic checklist is NO longer used for stroke patients (2017)
PATIENT TREATMENT (2019 MARYLAND MEDICAL PROTOCOLS) • Do not administer aspirin • Position patient with head elevated at 30 degrees • If patient has a positive Posterior Cerebellar Assessment OR Cincinnati Prehospital Stroke Scale AND can be delivered to the hospital within 20 hours of last known well time: • • • Patient is Priority 1 – notify receiving facility with “Stroke Alert with a last known well time of XX: XX” ASAP! Transport patient to closest Acute Stroke Ready, Primary, or Comprehensive Stroke Center If no stroke center with 30 minutes, go to the nearest hospital Consider aeromedical transport Obtain and document a contact telephone number for one or more individuals who have details about the patient’s medical history – this must be provided to the
PATIENT TREATMENT (2019 MARYLAND MEDICAL PROTOCOLS) • Administer oxygen at 2 -6 lpm via NC unless hypoxic or in respiratory distress • Use glucometer and treat accordingly if glucose is less than 70 mg/dl • ALS Interventions include: • Establish IV access with Lactated Ringers • • • Consult if patient is hypotensive Consider obtaining blood sample using closed system Do not treat hypertension in the field
PEDIATRIC PATIENTS (UNDER 18) (2019 MARYLAND MEDICAL PROTOCOLS) • Stroke is uncommon but does occur. Most often caused by: • • Congenital Heart Defects Infections (including Chicken Pox, Meningitis, or Encephalitis) Brain Injury Blood Disorders (such as Sickle Cell Disease) • Most often seen in infants, but can occur at any age • Consult with Pediatric Base Station, arrange transport to a Pediatric Trauma Center. • • Johns Hopkins Children’s Center, Baltimore Children’s National Medical Center, DC
ACUTE ISCHEMIC STROKE HOSPITAL TREATMENT OPTIONS • IV-t. PA – Tissue Plasminogen Activator “clot-buster” (alteplase) • Patient must be within the time window of 3. 5 hours (4. 5 hours for some patients) • Intra-arterial Thrombolysis • • • Doctor uses a catheter to administer t. PA directly into the clot Treatment can be administered up to 6 hours from symptom onset Patients must meet strict criteria • Mechanical Thrombectomy • • • Uses a device to retrieve the clot Treatment can be administered up to 8 hours from symptom onset If IV-t. PA fails or patient is ineligible, they may be eligible for mechanical
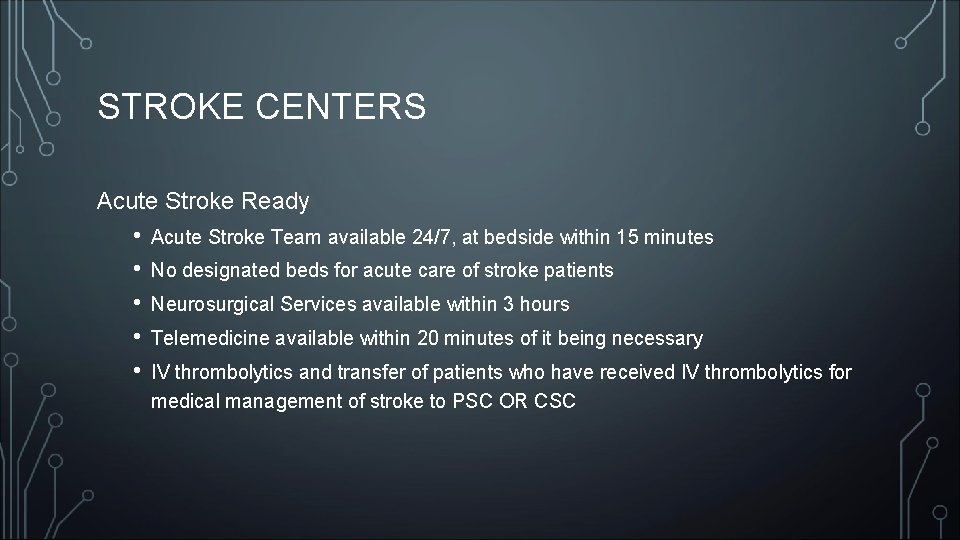
STROKE CENTERS Acute Stroke Ready • • • Acute Stroke Team available 24/7, at bedside within 15 minutes No designated beds for acute care of stroke patients Neurosurgical Services available within 3 hours Telemedicine available within 20 minutes of it being necessary IV thrombolytics and transfer of patients who have received IV thrombolytics for medical management of stroke to PSC OR CSC
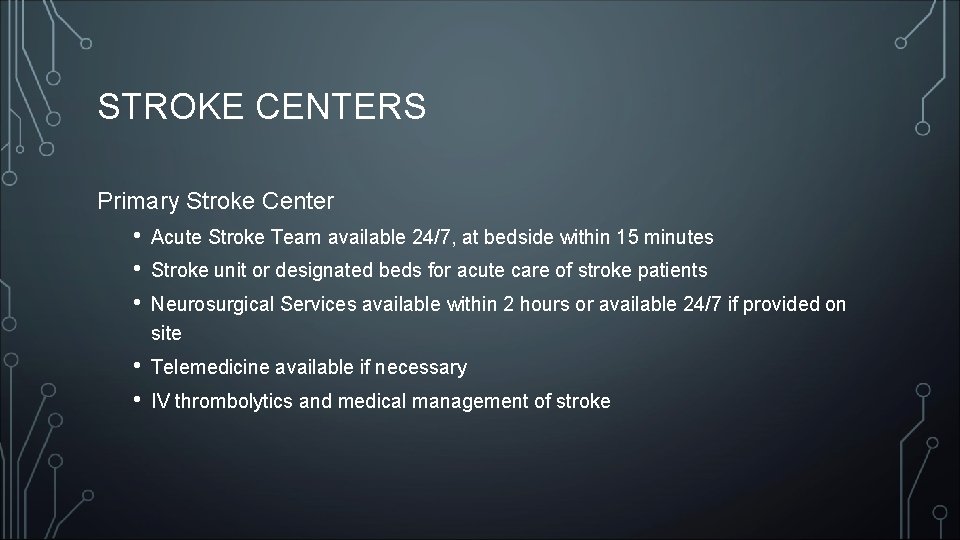
STROKE CENTERS Primary Stroke Center • • • Acute Stroke Team available 24/7, at bedside within 15 minutes • • Telemedicine available if necessary Stroke unit or designated beds for acute care of stroke patients Neurosurgical Services available within 2 hours or available 24/7 if provided on site IV thrombolytics and medical management of stroke
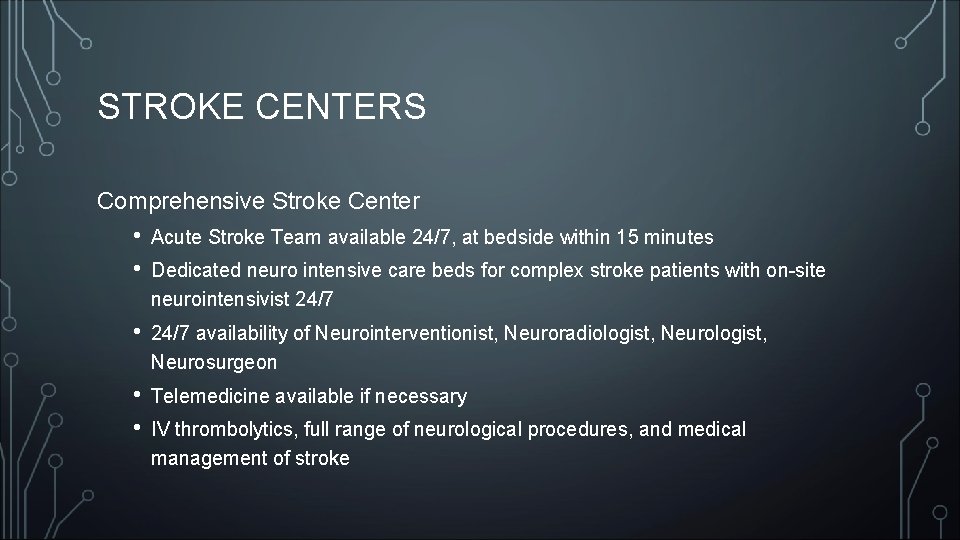
STROKE CENTERS Comprehensive Stroke Center • • Acute Stroke Team available 24/7, at bedside within 15 minutes • 24/7 availability of Neurointerventionist, Neuroradiologist, Neurosurgeon • • Telemedicine available if necessary Dedicated neuro intensive care beds for complex stroke patients with on-site neurointensivist 24/7 IV thrombolytics, full range of neurological procedures, and medical management of stroke
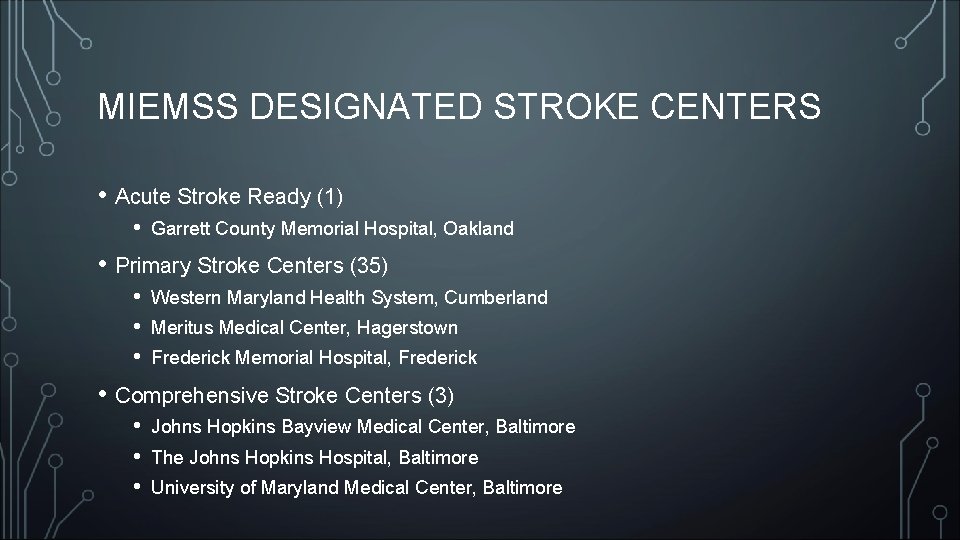
MIEMSS DESIGNATED STROKE CENTERS • Acute Stroke Ready (1) • Garrett County Memorial Hospital, Oakland • Primary Stroke Centers (35) • • • Western Maryland Health System, Cumberland Meritus Medical Center, Hagerstown Frederick Memorial Hospital, Frederick • Comprehensive Stroke Centers (3) • • • Johns Hopkins Bayview Medical Center, Baltimore The Johns Hopkins Hospital, Baltimore University of Maryland Medical Center, Baltimore
NATIONALLY RECOGNIZED STROKE CENTERS About 1600 recognized stroke facilities, including: • Acute Stroke Ready Hospital – approximately 70 • Primary Stroke Centers – approximately 1, 000 • Comprehensive Stroke Centers – approximately 175 • • • WVU, Morgantown WV UPMC, Pittsburgh PA UPMC Shadyside, Pittsburgh PA AHN, Pittsburgh PA UVA, Charlottesville VA
RECOVERY • Rehab can be inpatient, outpatient, or a combination • Various rehab programs depending on need, including: • • • Physical Therapy Occupational Therapy Speech-Language Therapy Patient / Family Education Support Groups
REDUCING RISK OF ADDITIONAL STROKES • Maintain a healthy blood pressure – ideally below 120/80 • Maintain healthy blood sugar and cholesterol levels • Address other health issues, especially atrial fibrillation and sleep apnea • Adopt healthy lifestyle habits, including diet and physical and mental exercise • Limit or eliminate alcohol, tobacco, and vaping • Maintenance medications may be required, such as aspirin, depending on stroke type
QUESTIONS ?
SOURCES • American Stroke Association (www. strokeassociation. org) • MIEMSS 2019 Maryland Medical Protocols (www. miemss. org) • Western Maryland Health System Stroke Center (www. wmhs. com) • The Joint Commission [formerly JCAHO] (www. jointcommission. org) • Wikipedia (www. wikipedia. org)
 Anterior stroke vs posterior stroke
Anterior stroke vs posterior stroke Muscle power neurological examination
Muscle power neurological examination What is focal neurological signs
What is focal neurological signs Neurological examination
Neurological examination Villa fridheim haapsalu
Villa fridheim haapsalu Glasgow coma scale video
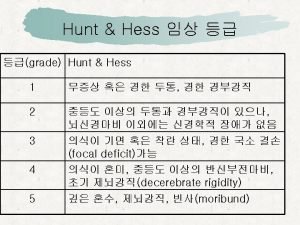
Glasgow coma scale video Wfns grade
Wfns grade Neurological exam
Neurological exam Neurological assessment chart
Neurological assessment chart Neurological disease
Neurological disease Neurological based behavior
Neurological based behavior Neurological assessment
Neurological assessment Psychomotor considerations language acquisition
Psychomotor considerations language acquisition Is adhd a neurological disorder
Is adhd a neurological disorder Amy lee plastic surgery
Amy lee plastic surgery Neurological examination
Neurological examination Motor function neurological assessment
Motor function neurological assessment Solent msk physiotherapy
Solent msk physiotherapy Biochemical theory criminology
Biochemical theory criminology Muscle power grading scale
Muscle power grading scale Normal pressure hydrocephalus triad
Normal pressure hydrocephalus triad Qut security emergency extension number
Qut security emergency extension number Lsu hematology oncology
Lsu hematology oncology Major nutritional deficiency diseases in emergencies
Major nutritional deficiency diseases in emergencies Chapter 32 environmental emergencies
Chapter 32 environmental emergencies A behavioral crisis is most accurately defined as
A behavioral crisis is most accurately defined as Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies Immunologic emergencies
Immunologic emergencies Chapter 35 geriatric emergencies
Chapter 35 geriatric emergencies Lesson 6: cardiac emergencies and using an aed
Lesson 6: cardiac emergencies and using an aed Chapter 16 cardiovascular emergencies
Chapter 16 cardiovascular emergencies Chapter 19 endocrine and hematologic emergencies
Chapter 19 endocrine and hematologic emergencies