MRI of Autoimmune Encephalitis an Interactive Tutorial e
- Slides: 50
MRI of Autoimmune Encephalitis: an Interactive Tutorial e. Ed. E-22 Control #: 1230 William B. Zucconi, DO Assistant Professor of Diagnostic Radiology Associate Residency Program Director, Diagnostic Radiology Vahe M. Zohrabian, MD Assistant Professor of Diagnostic Radiology Richard A. Bronen, MD Professor of Diagnostic Radiology & Neurosurgery Vice Chair of Academic Affairs
Disclosure: No conflict of interest • Dr. Zucconi: No disclosures • Dr. Zohrabian: No disclosures • Dr. Bronen: Consultant: Bristol-Myers Squibb
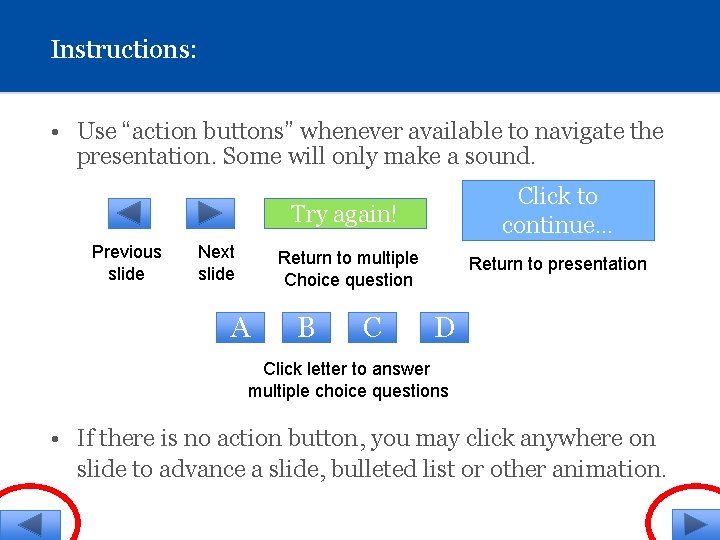
Instructions: • Use “action buttons” whenever available to navigate the presentation. Some will only make a sound. Previous slide Next slide A Try again! Click to continue… Return to multiple Choice question Return to presentation B C D Click letter to answer multiple choice questions • If there is no action button, you may click anywhere on slide to advance a slide, bulleted list or other animation.
Purpose of this exercise: • To update and engage the learner in an interactive tutorial on autoimmune encephalitis (AIE). The activity is intended for those with a beginning or intermediate level of understanding of this topic.
Approach: • Novel memory aids and "clickable" items (questions, findings within MRI images, etc. ) are embedded within the presentation in an interactive format to provide immediate feedback. • Clinically proven cases of AIE are used for the exercise. • Cases of clinically proven alternative diagnoses with similar imaging features also are included. • A literature review was performed and salient points presented.
Autoimmune Encephalitis: Introduction • Advances in the understanding of the pathophysiology and incidence of AIE necessitate rapid dissemination to the radiology community. • Autoimmune encephalitis, formerly known as “Limbic encephalitis” may account for over 20% of encephalitis cases. • From a radiologist's perspective, it is useful to separate those causes involving the limbic system from those which typically do not. • Differentiation also is made between causes of AIE which are commonly paraneoplastic and those that are not associated with tumors.
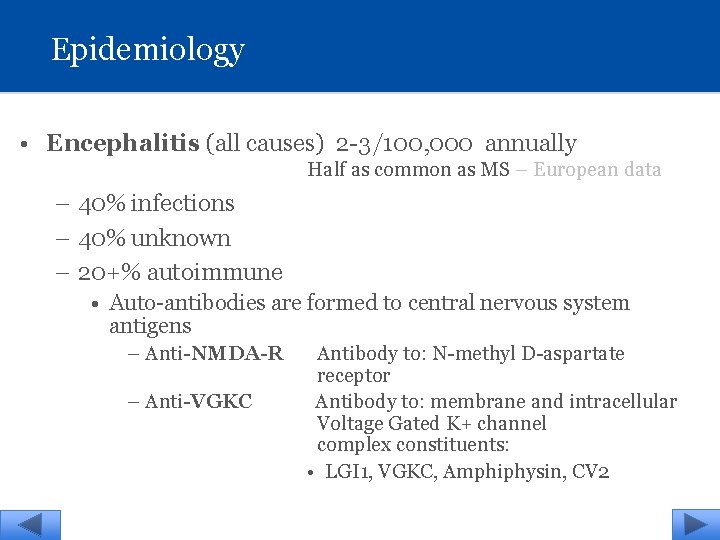
Epidemiology • Encephalitis (all causes) 2 -3/100, 000 annually Half as common as MS – European data – 40% infections – 40% unknown – 20+% autoimmune • Auto-antibodies are formed to central nervous system antigens – Anti-NMDA-R Antibody to: N-methyl D-aspartate receptor – Anti-VGKC Antibody to: membrane and intracellular Voltage Gated K+ channel complex constituents: • LGI 1, VGKC, Amphiphysin, CV 2
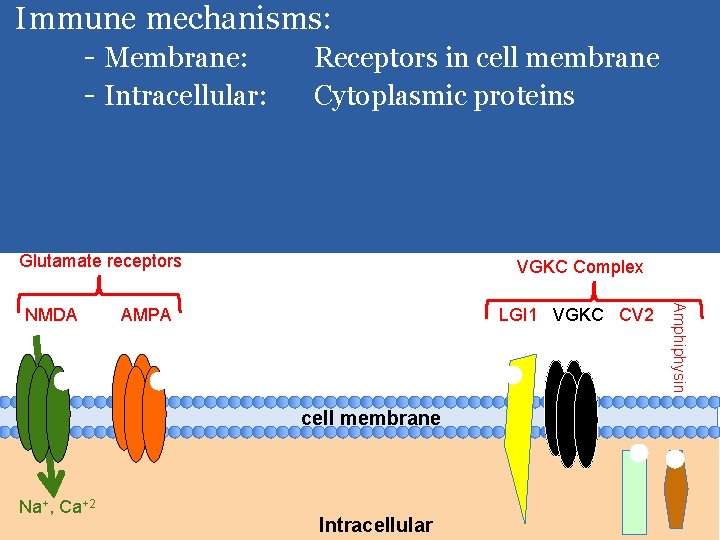
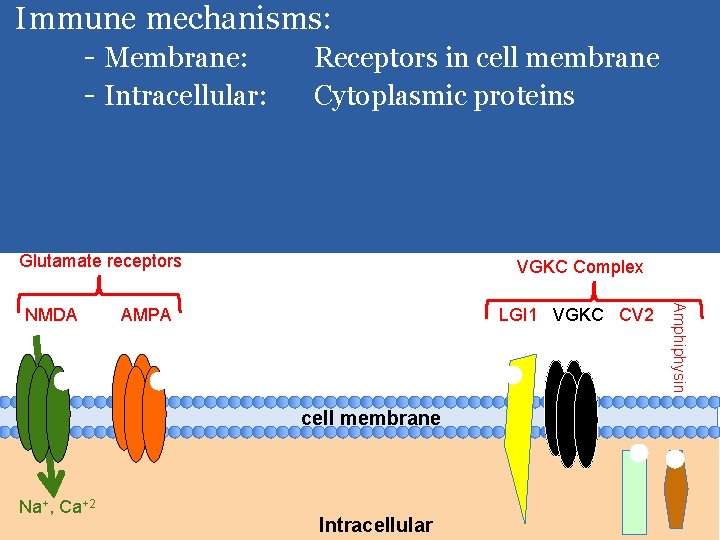
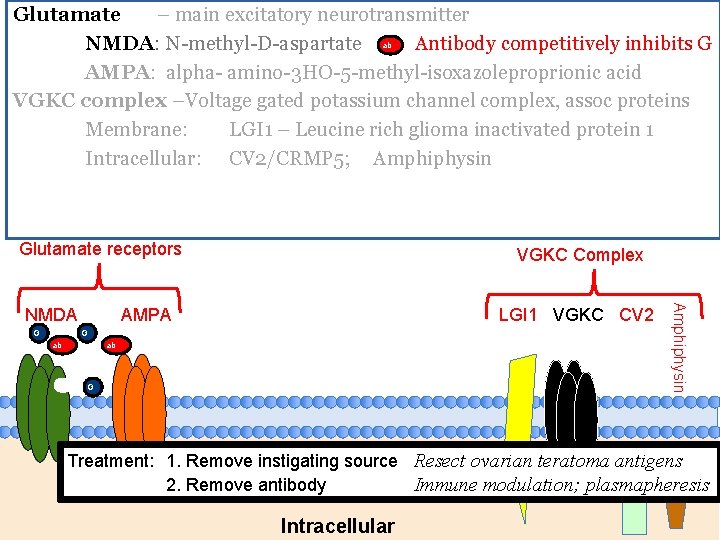
Membraneous: Glutamate –main excitatory neurotransmitter Immune mechanisms: NMDA: N-methyl-D-aspartate - Membrane: Receptors in cell membrane AMPA: alpha- amino-3 HO-5 -methyl-isoxazoleproprionic acid - Intracellular: Cytoplasmic proteins G G G VGKC complex –Voltage gated potassium channel complex, assoc proteins Membrane: LGI 1 – Leucine rich glioma inactivated protein 1 Intracellular: CV 2/CRMP 5; Amphiphysin Glutamate receptors AMPA LGI 1 VGKC CV 2 cell membrane Na+, Ca+2 Intracellular Amphiphysin NMDA VGKC Complex
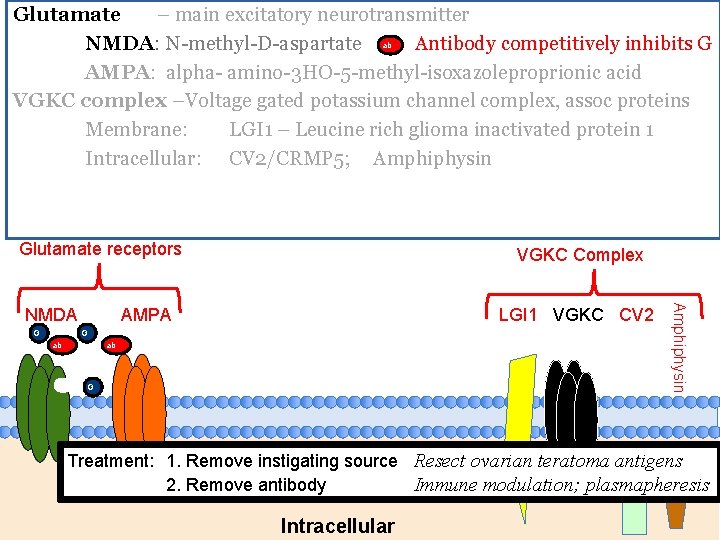
Glutamate – main excitatory neurotransmitter ab NMDA: N-methyl-D-aspartate Antibody competitively inhibits G AMPA: alpha- amino-3 HO-5 -methyl-isoxazoleproprionic acid VGKC complex –Voltage gated potassium channel complex, assoc proteins Membrane: LGI 1 – Leucine rich glioma inactivated protein 1 Intracellular: CV 2/CRMP 5; Amphiphysin Glutamate receptors G AMPA LGI 1 VGKC CV 2 G ab ab G Amphiphysin NMDA VGKC Complex Treatment: 1. Remove instigating source Resect ovarian teratoma antigens 2. Remove antibody Immune modulation; plasmapheresis Intracellular
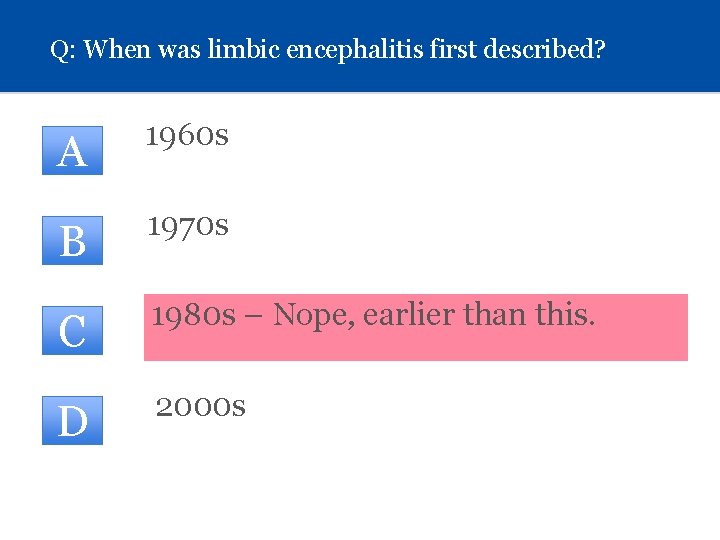
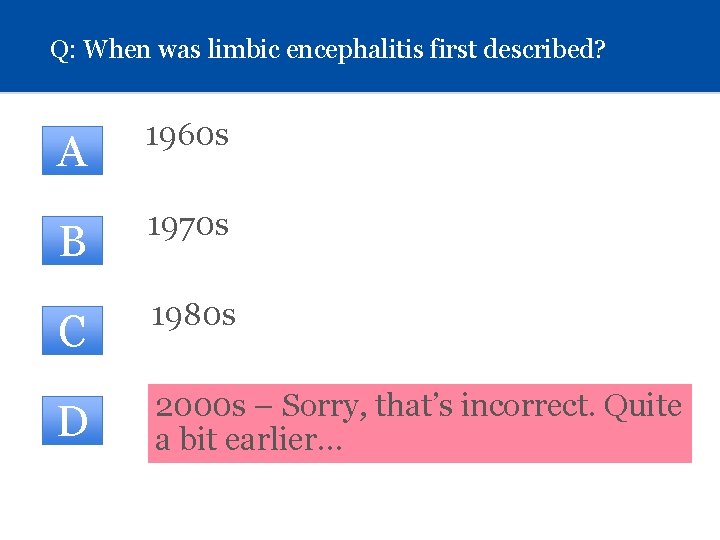
Q: When was limbic encephalitis first described? (Click on letter) A 1960 s B 1970 s C 1980 s D 2000 s
Q: When was limbic encephalitis first described? A CORRECT!! One of the first references is from 1966, by L. Brain et al, in Lancet describing a patient with Hashimoto’s Click to continue…
Q: When was limbic encephalitis first described? A 1960 s B 1970 s - No, sorry… even earlier ! C 1980 s D 2000 s
Q: When was limbic encephalitis first described? A 1960 s B 1970 s C 1980 s – Nope, earlier than this. D 2000 s
Q: When was limbic encephalitis first described? A 1960 s B 1970 s C 1980 s D 2000 s – Sorry, that’s incorrect. Quite a bit earlier…
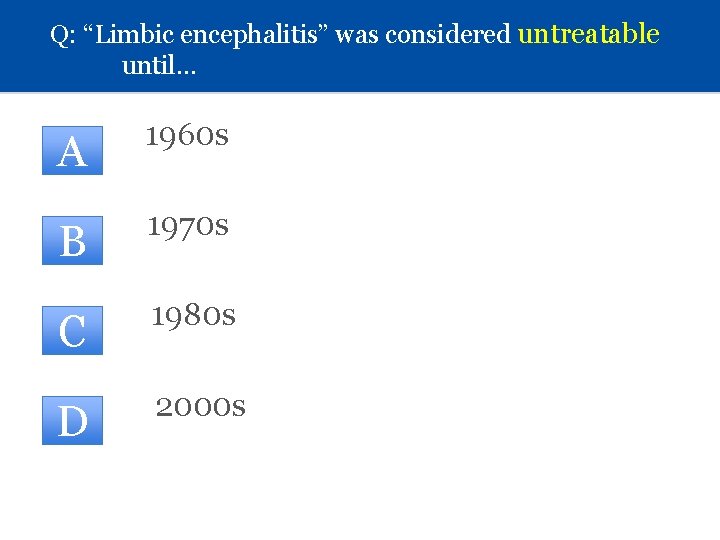
Q: “Limbic encephalitis” was considered untreatable until… A 1960 s B 1970 s C 1980 s D 2000 s
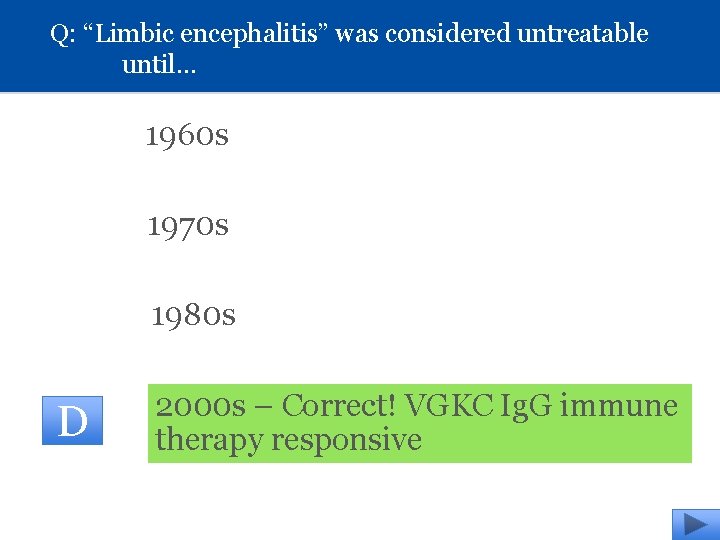
Q: “Limbic encephalitis” was considered untreatable until… 1960 s 1970 s 1980 s D 2000 s – Correct! VGKC Ig. G immune therapy responsive
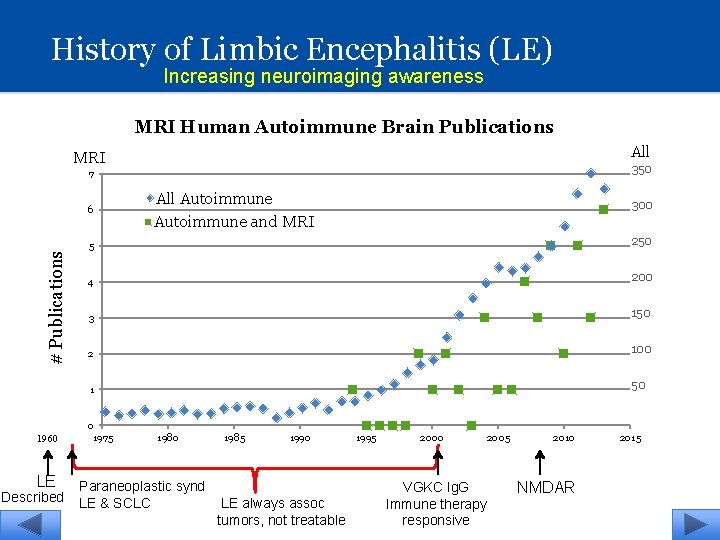
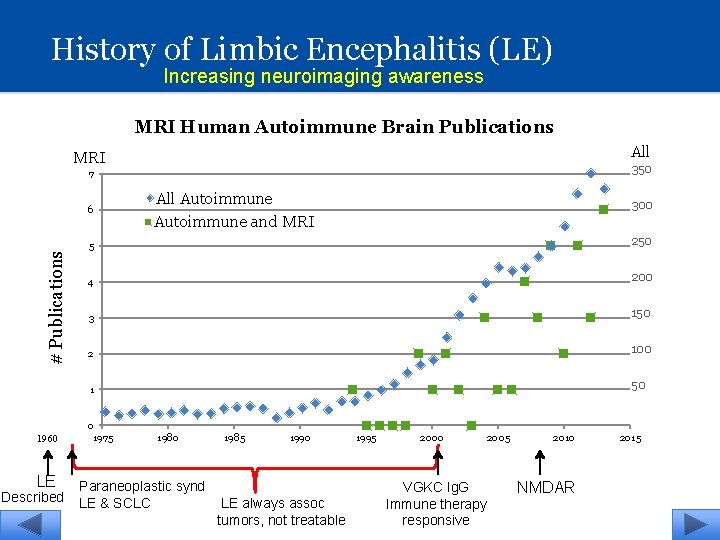
History of Limbic Encephalitis (LE) Increasing neuroimaging awareness MRI Human Autoimmune Brain Publications All MRI 350 7 # Publications 6 1960 LE Described All Autoimmune and MRI 300 5 250 4 200 3 150 2 100 1 50 0 1975 1980 Paraneoplastic synd LE & SCLC 1985 1990 LE always assoc tumors, not treatable 1995 2000 2005 VGKC Ig. G Immune therapy responsive 2010 NMDAR 2015
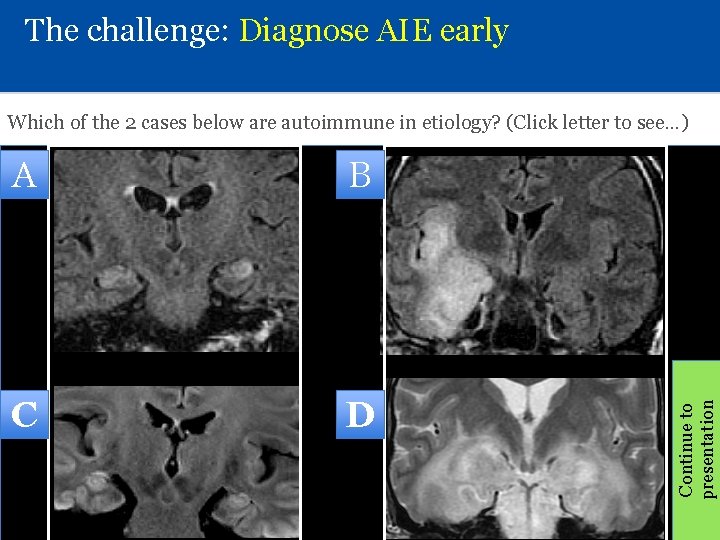
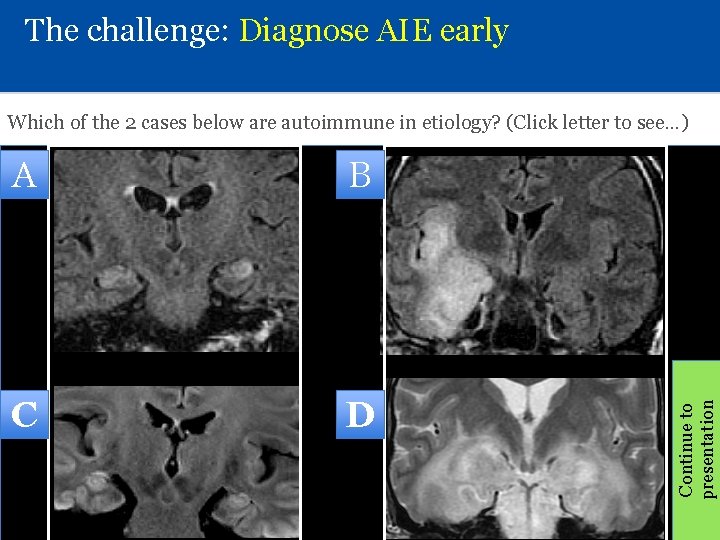
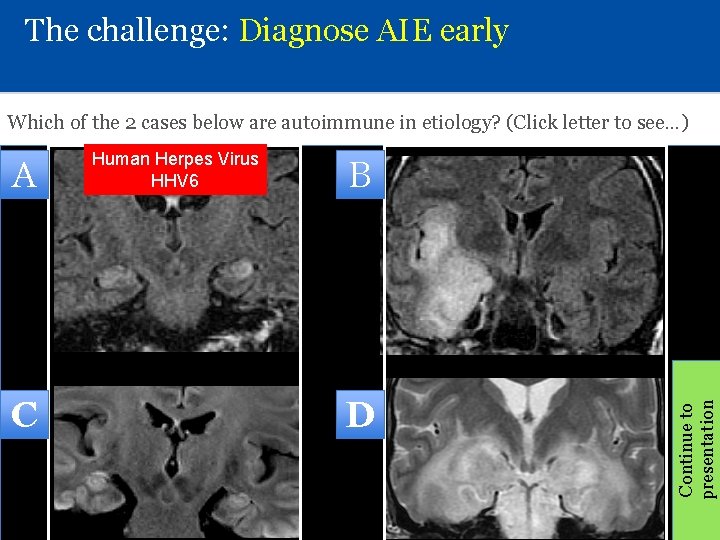
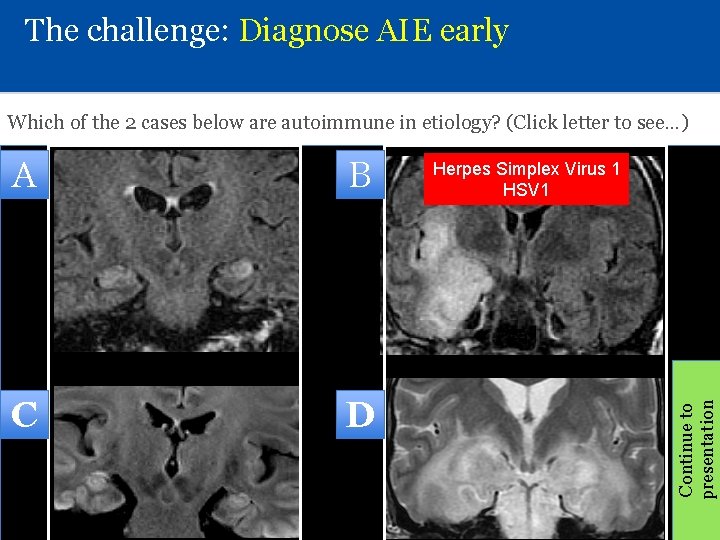
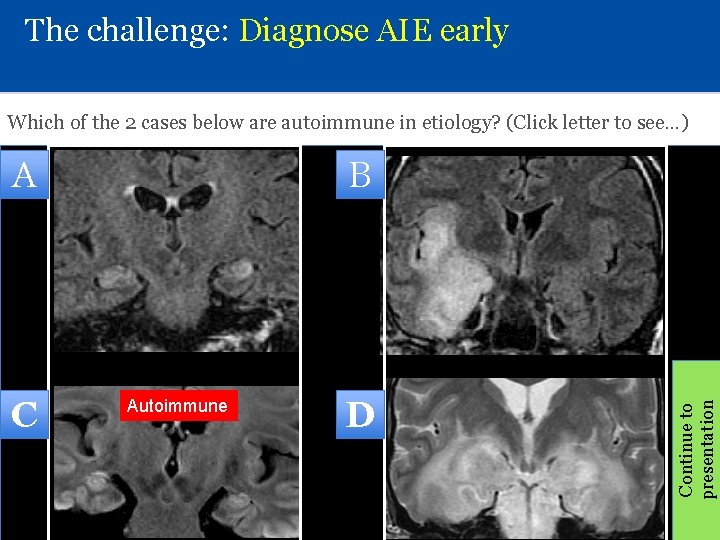
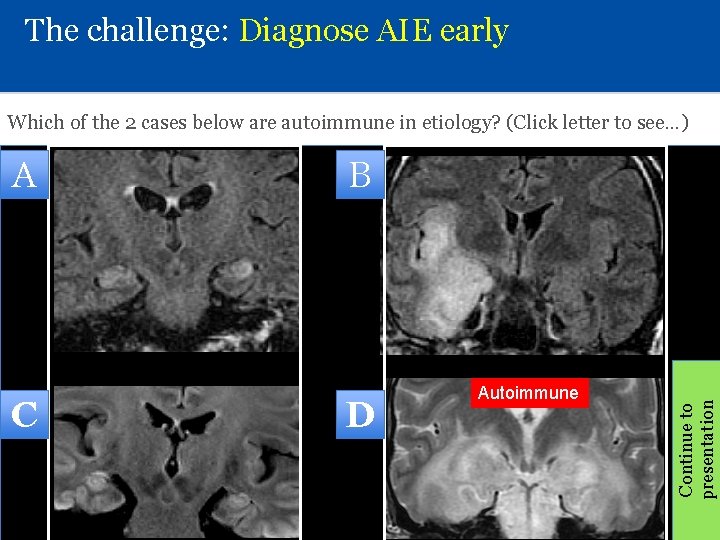
The challenge: Diagnose AIE early A B C D Continue to presentation Which of the 2 cases below are autoimmune in etiology? (Click letter to see…)
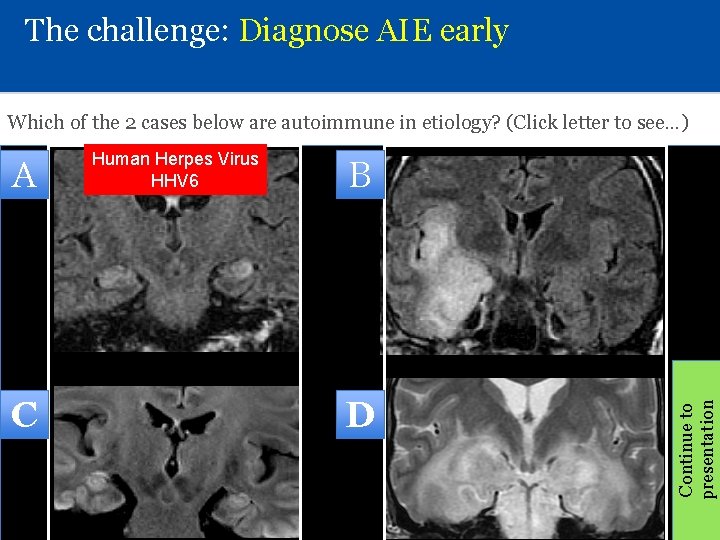
The challenge: Diagnose AIE early Which of the 2 cases below are autoimmune in etiology? (Click letter to see…) C B D Continue to presentation A Human Herpes Virus HHV 6
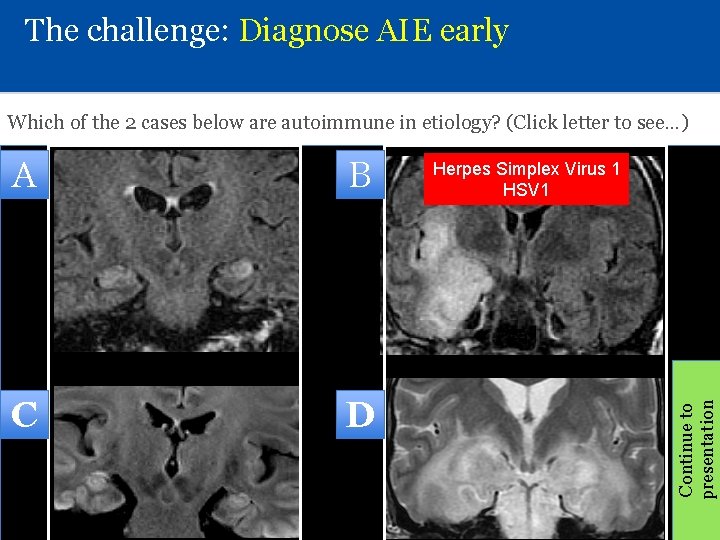
The challenge: Diagnose AIE early Which of the 2 cases below are autoimmune in etiology? (Click letter to see…) B C D Herpes Simplex Virus 1 HSV 1 Continue to presentation A
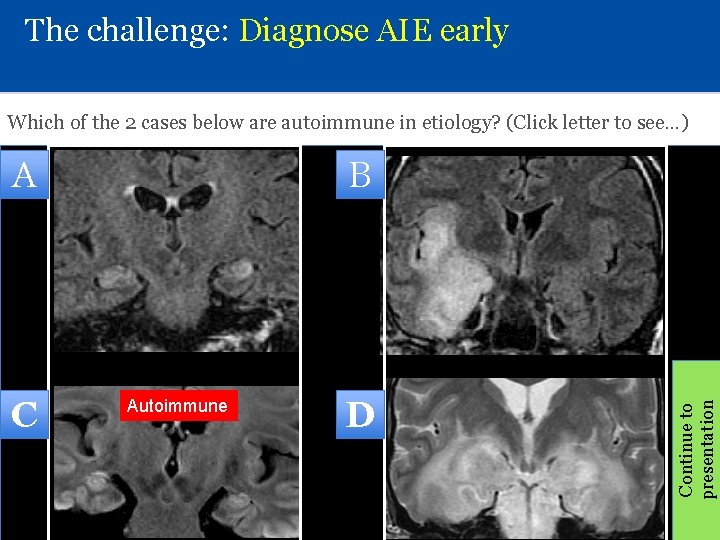
The challenge: Diagnose AIE early Which of the 2 cases below are autoimmune in etiology? (Click letter to see…) C B Autoimmune D Continue to presentation A
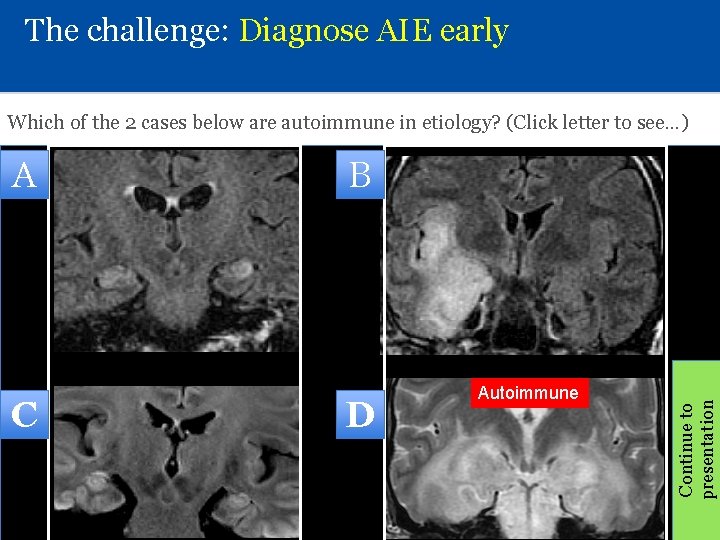
The challenge: Diagnose AIE early Which of the 2 cases below are autoimmune in etiology? (Click letter to see…) C B D Autoimmune Continue to presentation A
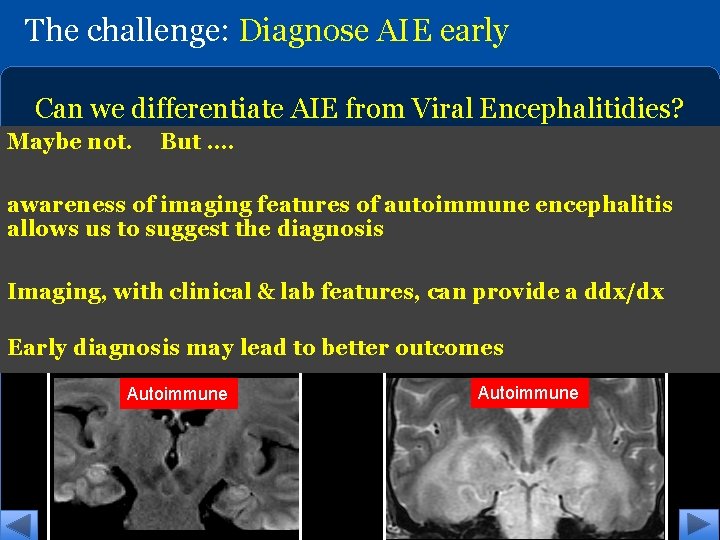
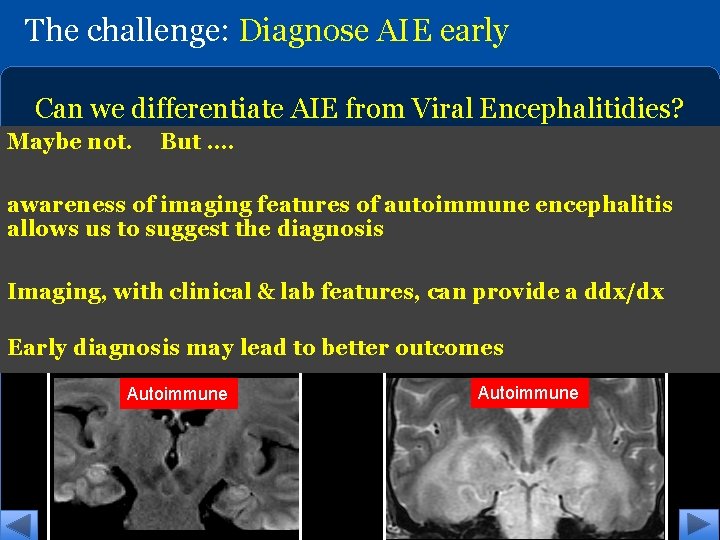
The challenge: Diagnose AIE early Can we differentiate AIE from Viral Encephalitidies? Which of the 2 cases below are autoimmune in etiology? Maybe not. But …. Human Herpes Virus HHV 6 Herpes Simplex Virus 1 HSV 1 awareness of imaging features of autoimmune encephalitis allows us to suggest the diagnosis Imaging, with clinical & lab features, can provide a ddx/dx Early diagnosis may lead to better outcomes Autoimmune
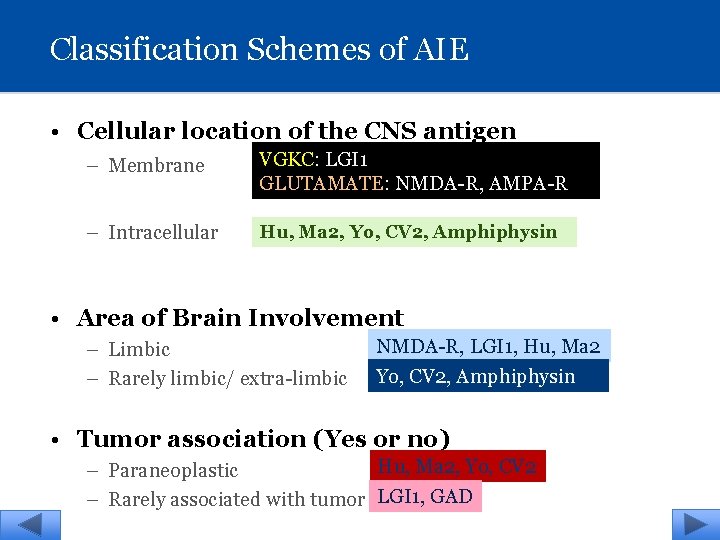
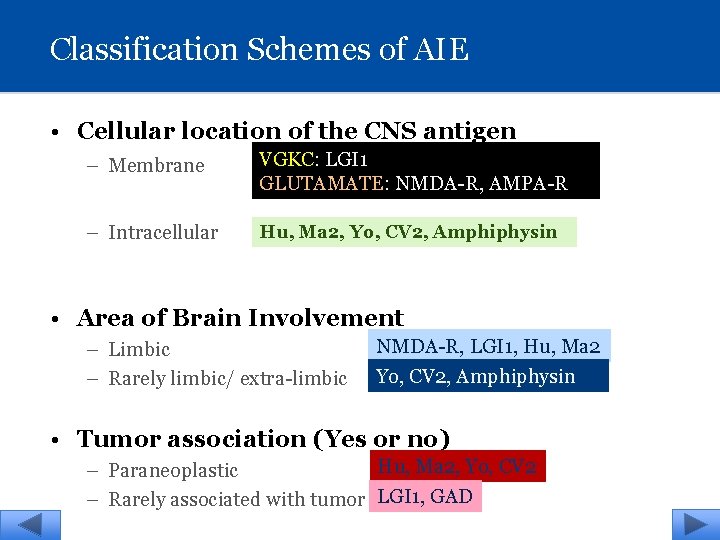
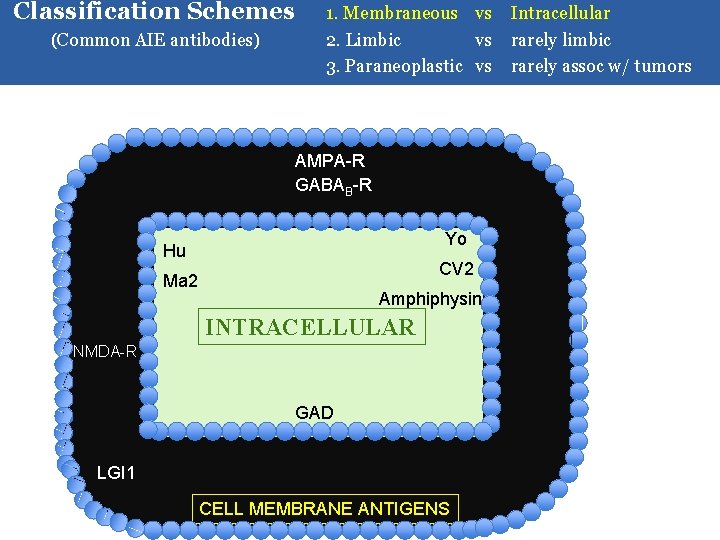
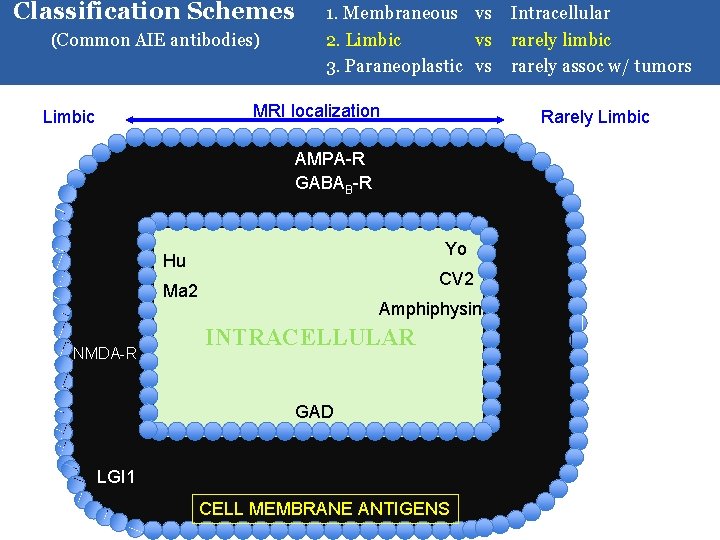
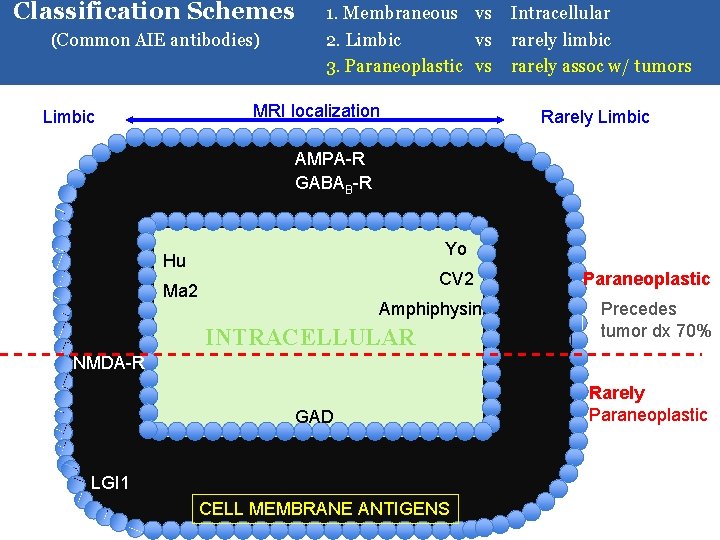
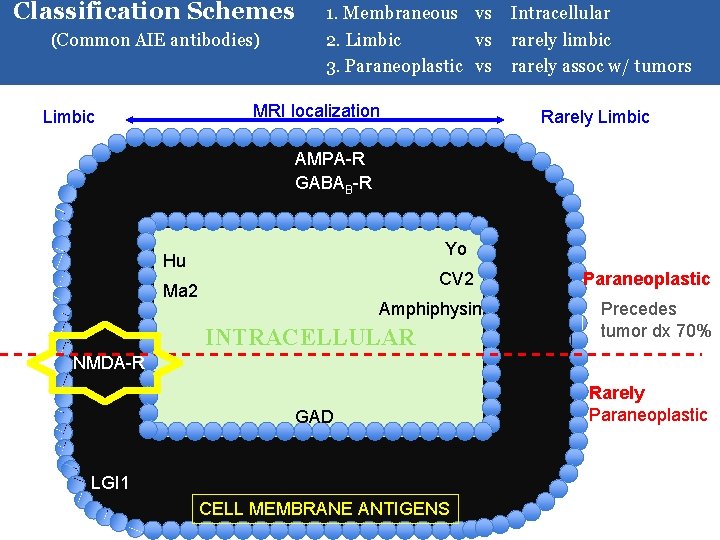
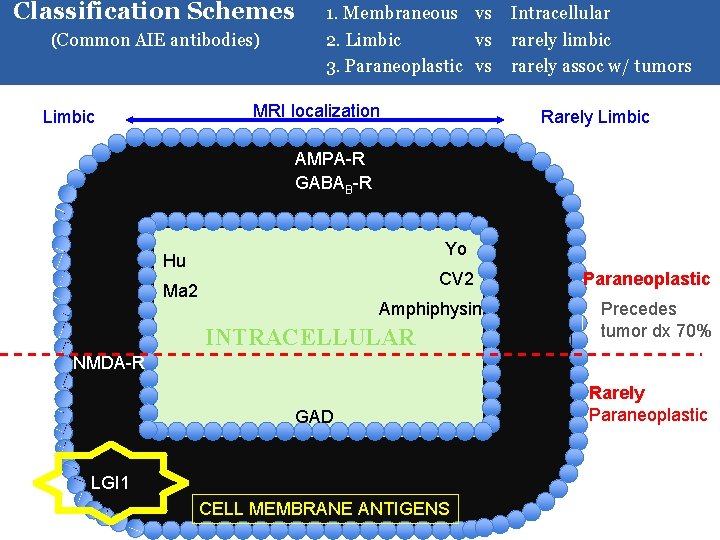
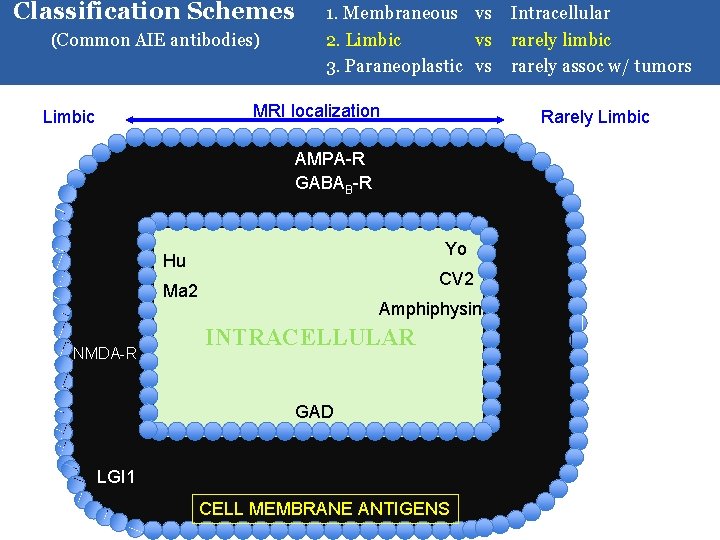
Classification Schemes of AIE • Cellular location of the CNS antigen – Membrane VGKC: LGI 1 GLUTAMATE: NMDA-R, AMPA-R – Intracellular Hu, Ma 2, Yo, CV 2, Amphiphysin • Area of Brain Involvement – Limbic – Rarely limbic/ extra-limbic NMDA-R, LGI 1, Hu, Ma 2 Yo, CV 2, Amphiphysin • Tumor association (Yes or no) Hu, Ma 2, Yo, CV 2 – Paraneoplastic – Rarely associated with tumor LGI 1, GAD
Classification Schemes (Common AIE antibodies) The antigens can be organized according to this scheme in the following cell pictograph:
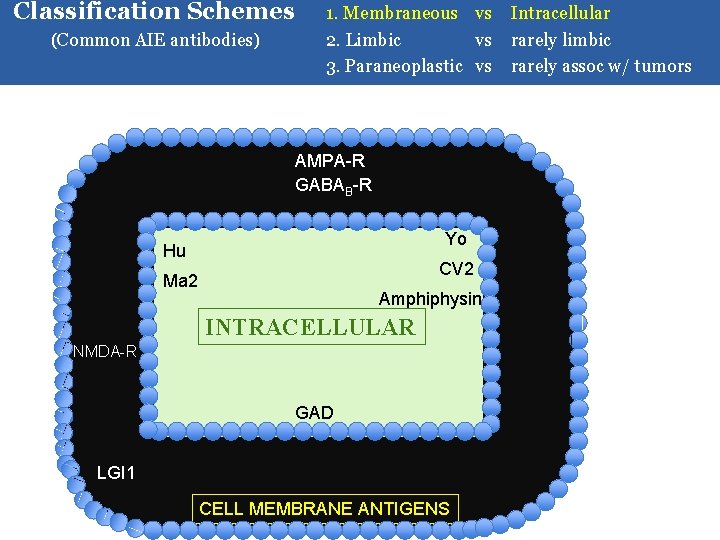
Classification Schemes (Common AIE antibodies) 1. Membraneous vs Intracellular 2. Limbic vs rarely limbic 3. Paraneoplastic vs rarely assoc w/ tumors AMPA-R GABAB-R Yo Hu CV 2 Ma 2 Amphiphysin INTRACELLULAR NMDA-R GAD LGI 1 CELL MEMBRANE ANTIGENS
Classification Schemes (Common AIE antibodies) 1. Membraneous vs Intracellular 2. Limbic vs rarely limbic 3. Paraneoplastic vs rarely assoc w/ tumors MRI localization Limbic Rarely Limbic AMPA-R GABAB-R Yo Hu CV 2 Ma 2 NMDA-R Amphiphysin INTRACELLULAR GAD LGI 1 CELL MEMBRANE ANTIGENS
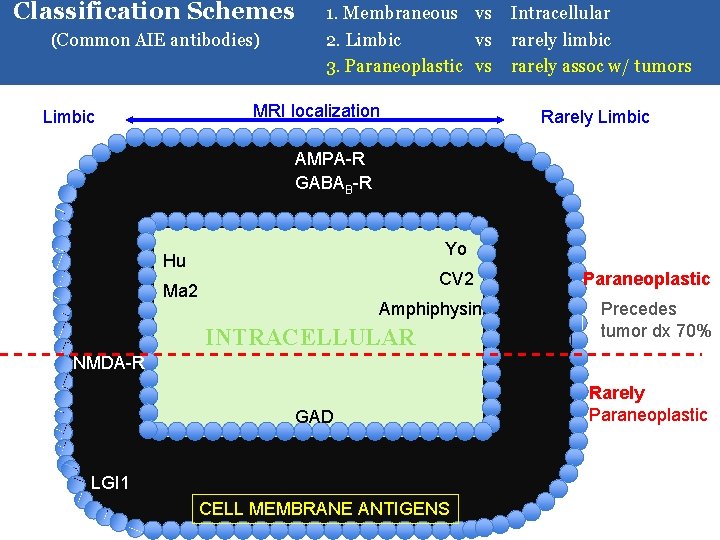
Classification Schemes (Common AIE antibodies) 1. Membraneous vs Intracellular 2. Limbic vs rarely limbic 3. Paraneoplastic vs rarely assoc w/ tumors MRI localization Limbic Rarely Limbic AMPA-R GABAB-R Yo Hu CV 2 Ma 2 Amphiphysin INTRACELLULAR Paraneoplastic Precedes tumor dx 70% NMDA-R GAD LGI 1 CELL MEMBRANE ANTIGENS Rarely Paraneoplastic
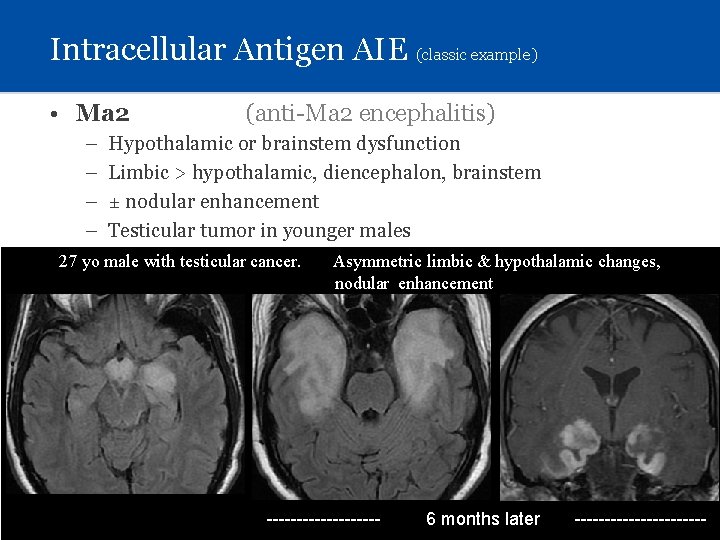
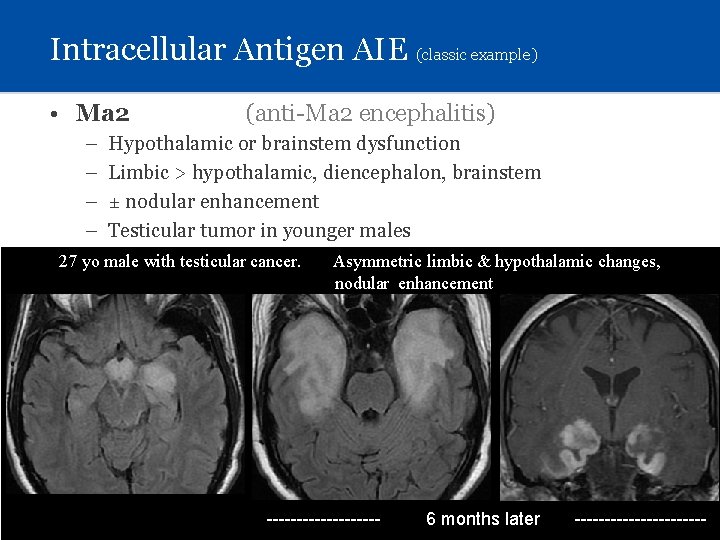
Intracellular Antigen AIE (classic example) • Ma 2 – – (anti-Ma 2 encephalitis) Hypothalamic or brainstem dysfunction Limbic > hypothalamic, diencephalon, brainstem ± nodular enhancement Testicular tumor in younger males 27 yo male with testicular cancer. Asymmetric limbic & hypothalamic changes, nodular enhancement ---------- 6 months later -----------
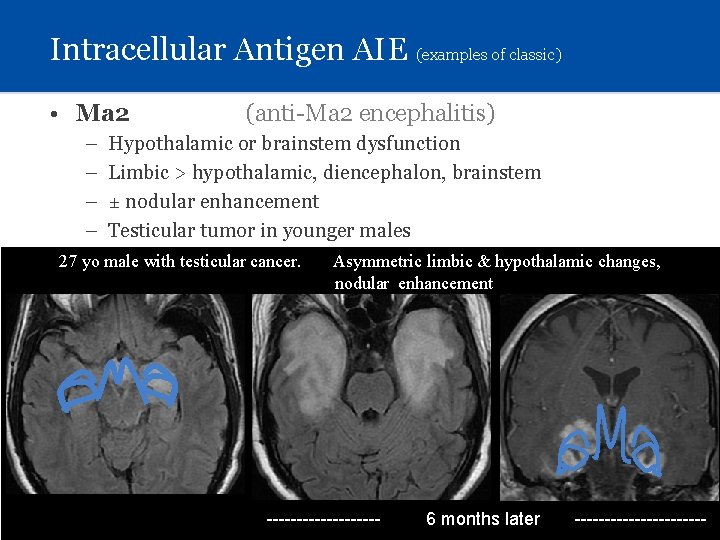
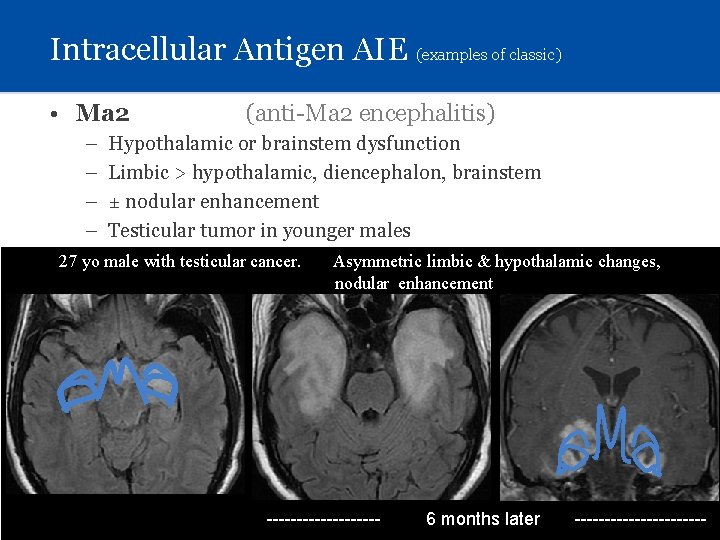
Intracellular Antigen AIE (examples of classic) • Ma 2 – – (anti-Ma 2 encephalitis) Hypothalamic or brainstem dysfunction Limbic > hypothalamic, diencephalon, brainstem ± nodular enhancement Testicular tumor in younger males 27 yo male with testicular cancer. • Yo – – Asymmetric limbic & hypothalamic changes, nodular enhancement (anti-Yo encephalitis) Most common paraneoplastic cerebellar AIE Cerebellar atrophy Intracellular antigens in Purkinje cells Ovarian & breast ca ---------- 6 months later -----------
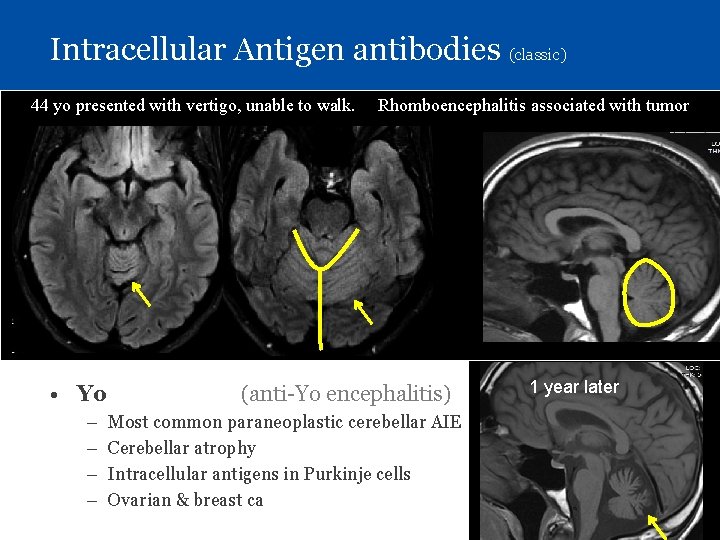
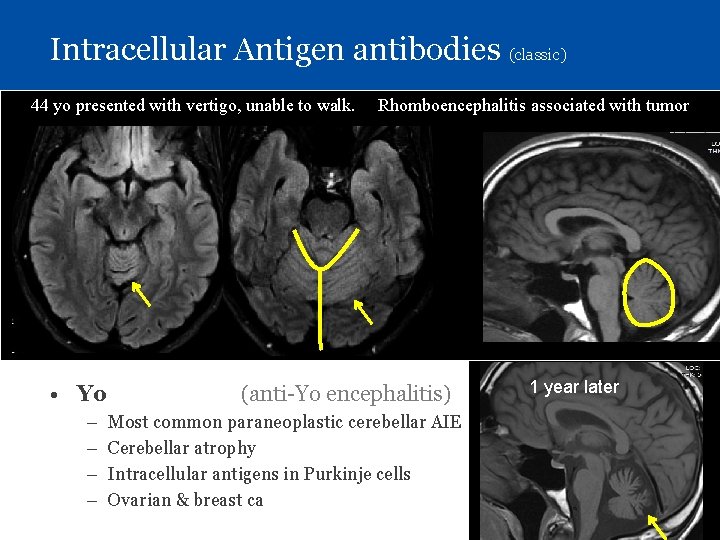
Intracellular Antigen antibodies (classic) 44 yo presented with vertigo, unable to walk. Rhomboencephalitis associated with tumor • Ma 2 – Hypothalamic or brainstem dysfunction – Limbic > diencephalon, brainstem – Testicular germinal cell tumor in younger males (Lung/breast ca) • Yo – – (anti-Yo encephalitis) Most common paraneoplastic cerebellar AIE Cerebellar atrophy Intracellular antigens in Purkinje cells Ovarian & breast ca 1 year later
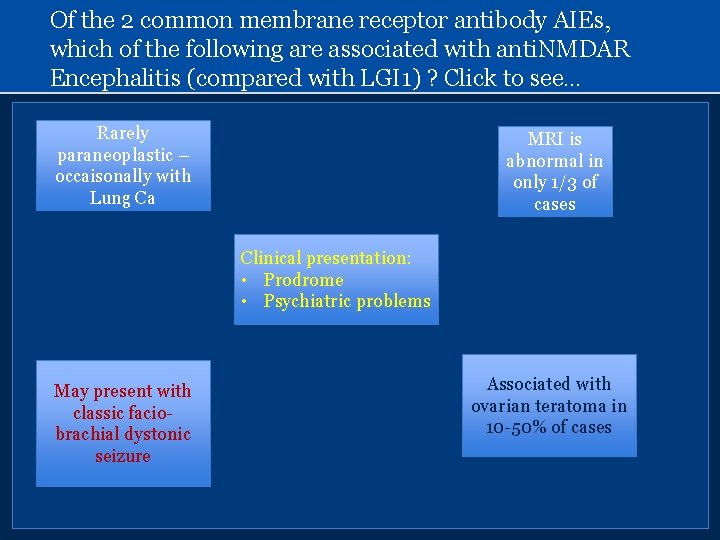
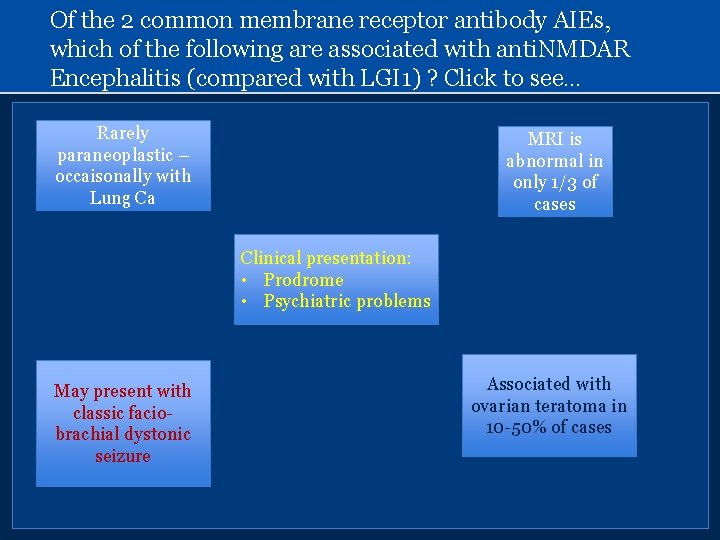
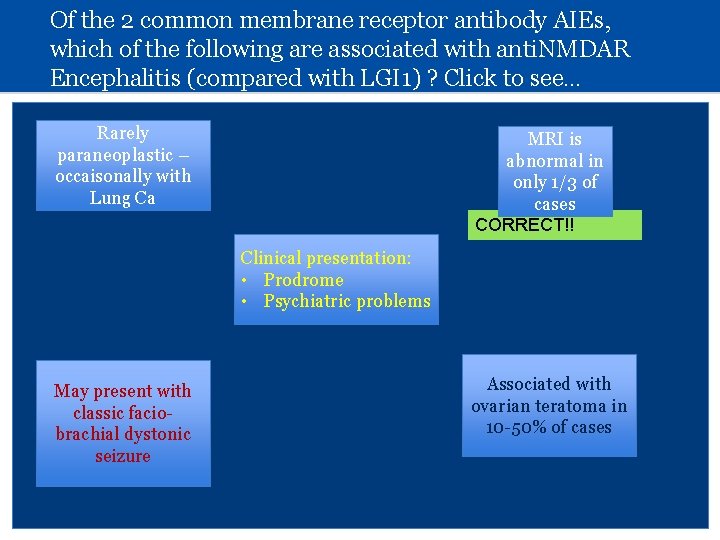
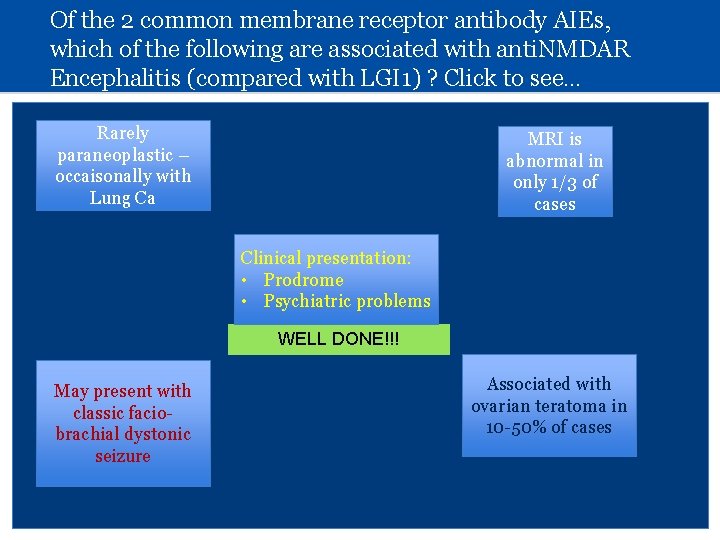
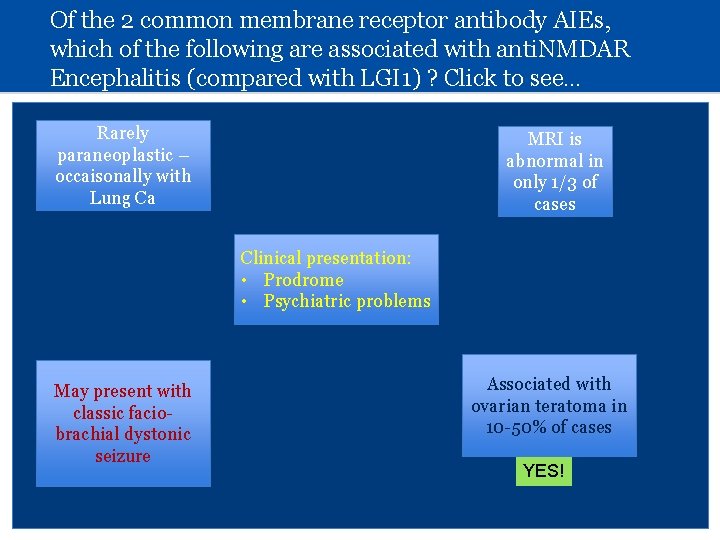
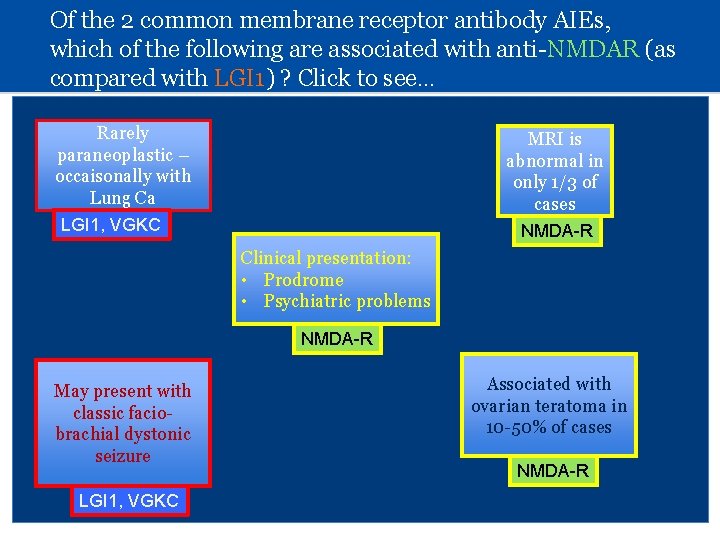
Of the 2 common membrane receptor antibody AIEs, which of the following are associated with anti. NMDAR Encephalitis (compared with LGI 1) ? Click to see… Rarely paraneoplastic – occaisonally with Lung Ca MRI is abnormal in only 1/3 of cases Clinical presentation: • Prodrome • Psychiatric problems May present with classic faciobrachial dystonic seizure Associated with ovarian teratoma in 10 -50% of cases
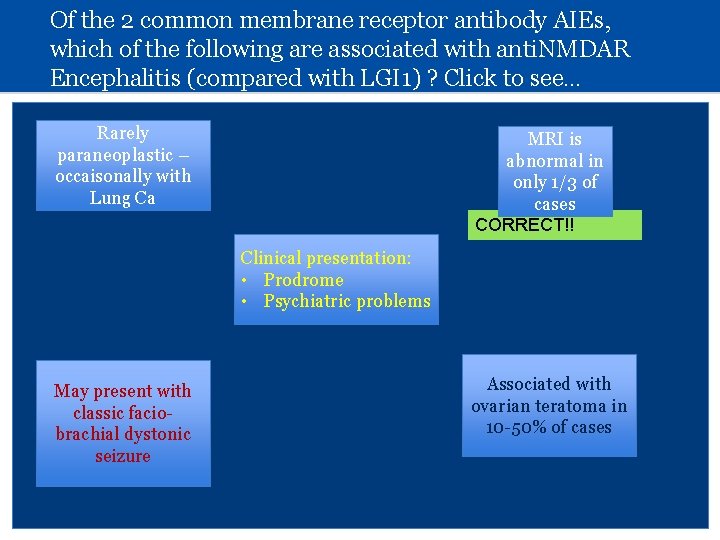
Of the 2 common membrane receptor antibody AIEs, which of the following are associated with anti. NMDAR Encephalitis (compared with LGI 1) ? Click to see… Rarely paraneoplastic – occaisonally with Lung Ca MRI is abnormal in only 1/3 of cases CORRECT!! Clinical presentation: • Prodrome • Psychiatric problems May present with classic faciobrachial dystonic seizure Associated with ovarian teratoma in 10 -50% of cases
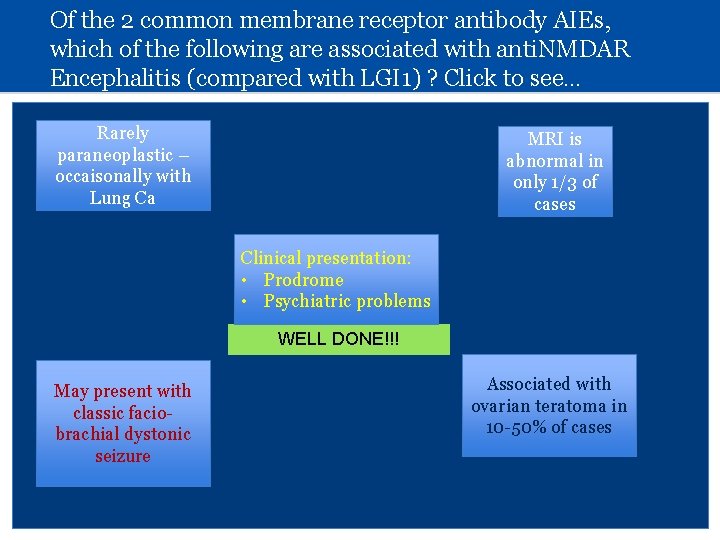
Of the 2 common membrane receptor antibody AIEs, which of the following are associated with anti. NMDAR Encephalitis (compared with LGI 1) ? Click to see… Rarely paraneoplastic – occaisonally with Lung Ca MRI is abnormal in only 1/3 of cases Clinical presentation: • Prodrome • Psychiatric problems WELL DONE!!! May present with classic faciobrachial dystonic seizure Associated with ovarian teratoma in 10 -50% of cases
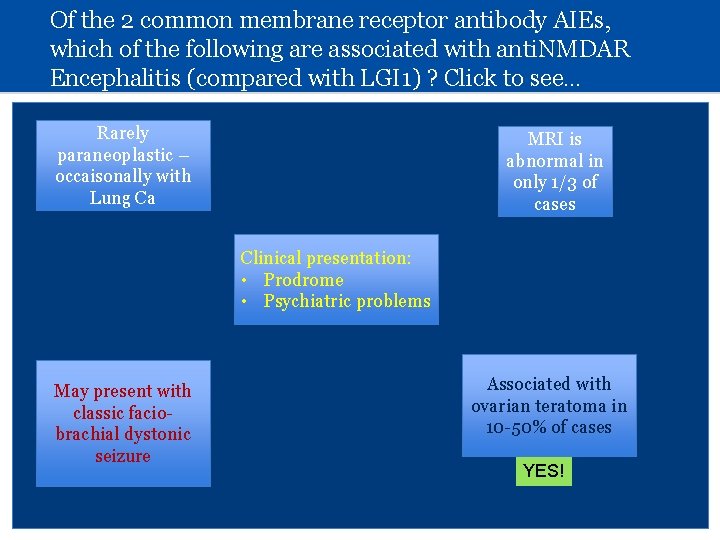
Of the 2 common membrane receptor antibody AIEs, which of the following are associated with anti. NMDAR Encephalitis (compared with LGI 1) ? Click to see… Rarely paraneoplastic – occaisonally with Lung Ca MRI is abnormal in only 1/3 of cases Clinical presentation: • Prodrome • Psychiatric problems May present with classic faciobrachial dystonic seizure Associated with ovarian teratoma in 10 -50% of cases YES!
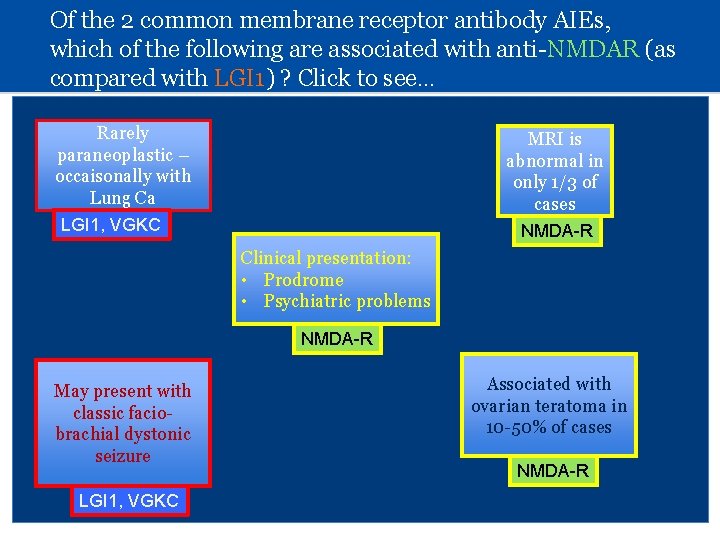
Of the 2 common membrane receptor antibody AIEs, which of the following are associated with anti-NMDAR (as compared with LGI 1) ? Click to see… Rarely paraneoplastic – occaisonally with Lung Ca MRI is abnormal in only 1/3 of cases LGI 1, VGKC NMDA-R Clinical presentation: • Prodrome • Psychiatric problems NMDA-R May present with classic faciobrachial dystonic seizure LGI 1, VGKC Associated with ovarian teratoma in 10 -50% of cases NMDA-R
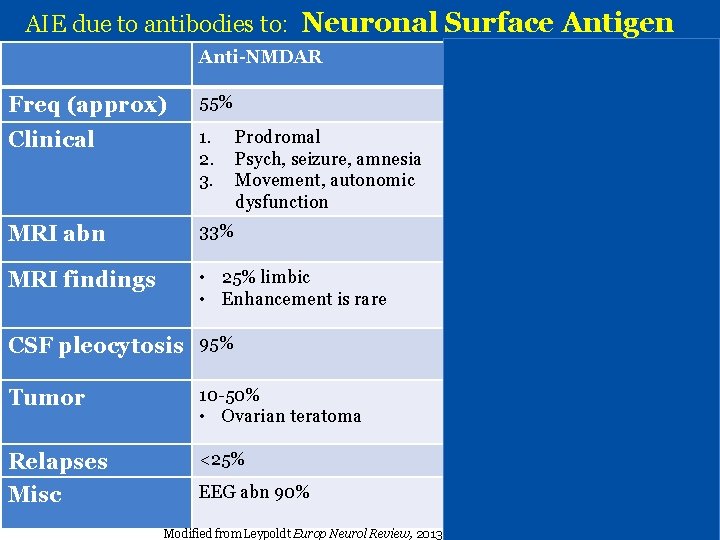
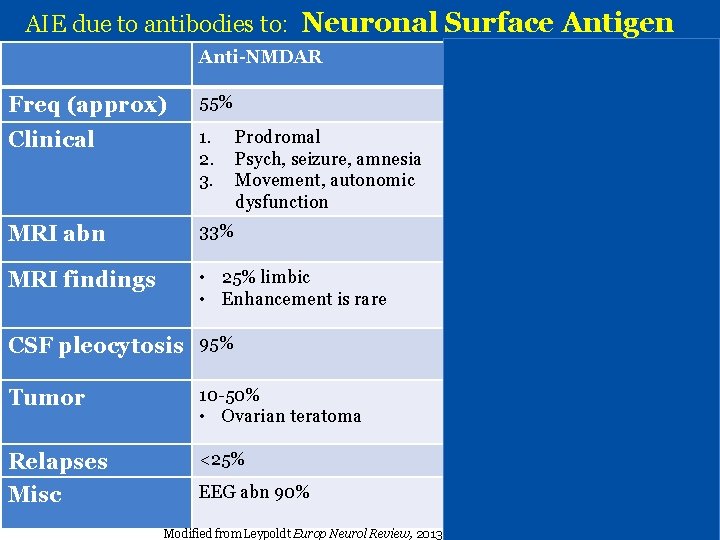
AIE due to antibodies to: Neuronal Surface Antigen Anti-NMDAR Anti-LGI 1 Freq (approx) 55% 30% Clinical 1. 2. 3. MRI abn 33% >80% MRI findings • 25% limbic • Enhancement is rare Limbic Prodromal Psych, seizure, amnesia Movement, autonomic dysfunction CSF pleocytosis 95% Limbic encephalitis, Facio-brachial dystonic seizure 40% Tumor 10 -50% • Ovarian teratoma <10% • Lung, thymoma Relapses <25% 15% Misc EEG abn 90% • Hyponatremia Modified from Leypoldt Europ Neurol Review, 2013
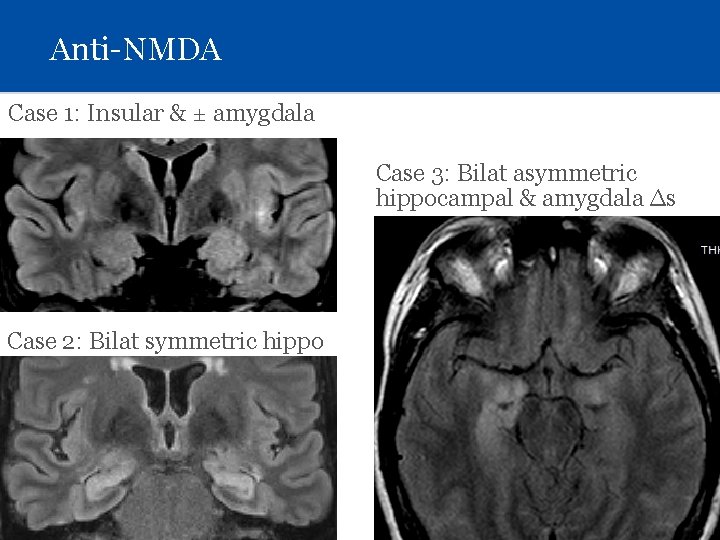
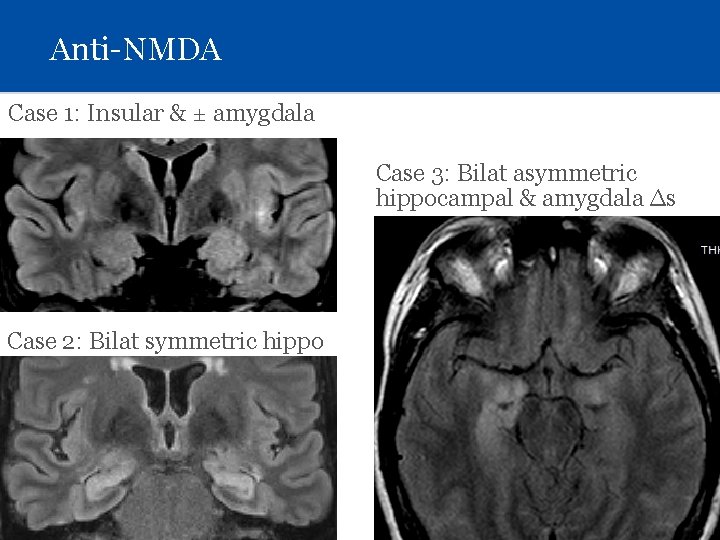
Anti-NMDA Case 1: Insular & ± amygdala Case 3: Bilat asymmetric hippocampal & amygdala ∆s Case 2: Bilat symmetric hippo
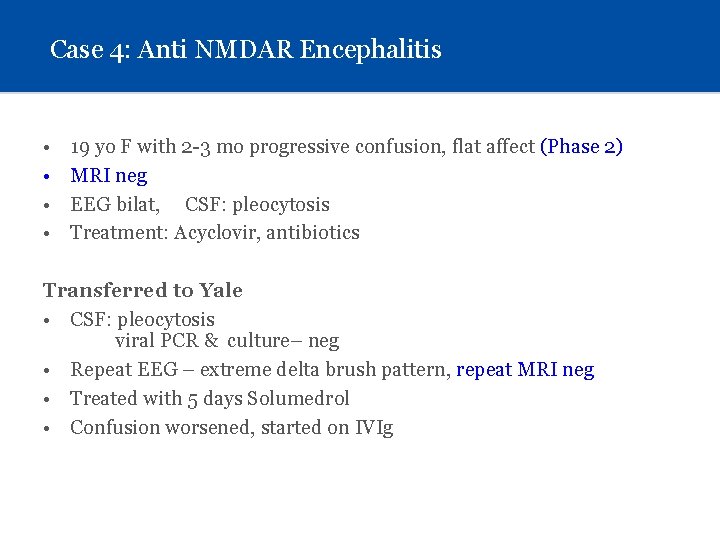
Case 4: Anti NMDAR Encephalitis • • 19 yo F with 2 -3 mo progressive confusion, flat affect (Phase 2) MRI neg EEG bilat, CSF: pleocytosis Treatment: Acyclovir, antibiotics Transferred to Yale • CSF: pleocytosis viral PCR & culture– neg • Repeat EEG – extreme delta brush pattern, repeat MRI neg • Treated with 5 days Solumedrol • Confusion worsened, started on IVIg
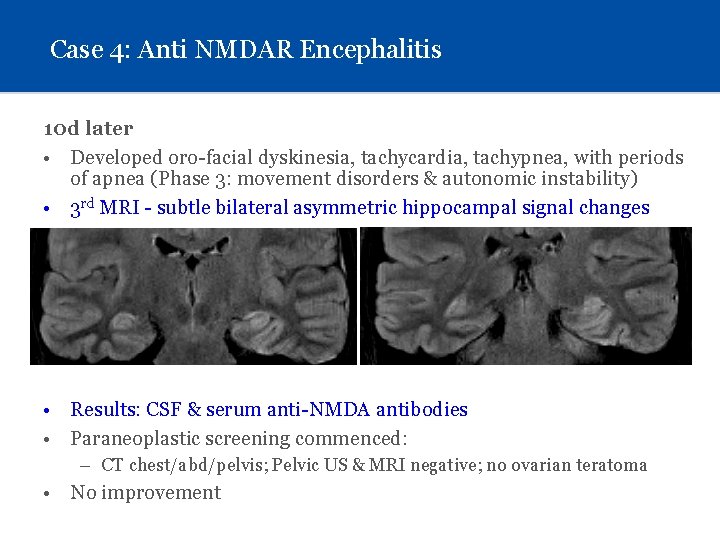
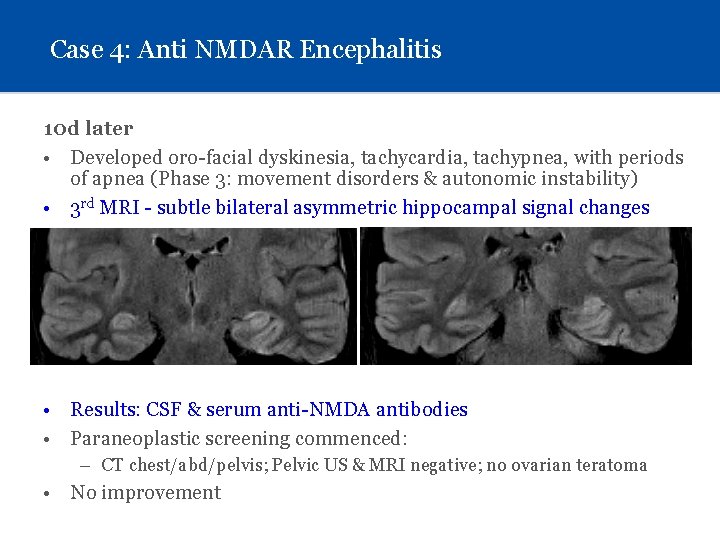
Case 4: Anti NMDAR Encephalitis 10 d later • Developed oro-facial dyskinesia, tachycardia, tachypnea, with periods of apnea (Phase 3: movement disorders & autonomic instability) • 3 rd MRI - subtle bilateral asymmetric hippocampal signal changes • Results: CSF & serum anti-NMDA antibodies • Paraneoplastic screening commenced: – CT chest/abd/pelvis; Pelvic US & MRI negative; no ovarian teratoma • No improvement
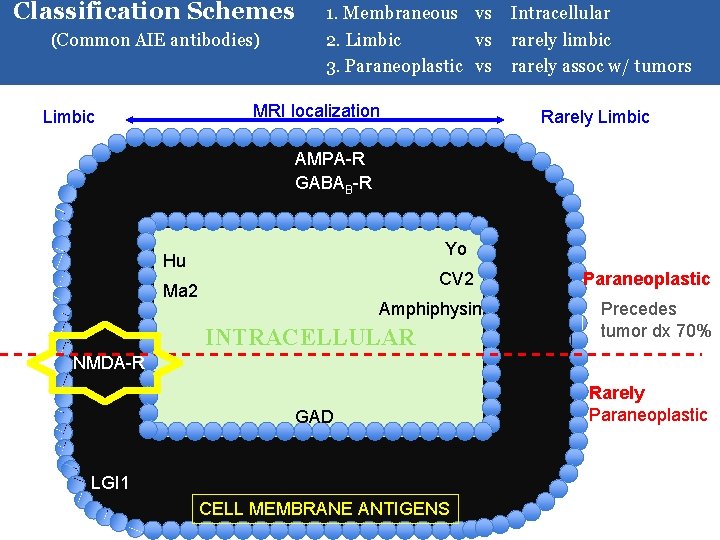
Classification Schemes (Common AIE antibodies) 1. Membraneous vs Intracellular 2. Limbic vs rarely limbic 3. Paraneoplastic vs rarely assoc w/ tumors MRI localization Limbic Rarely Limbic AMPA-R GABAB-R Yo Hu CV 2 Ma 2 Amphiphysin INTRACELLULAR Paraneoplastic Precedes tumor dx 70% NMDA-R GAD LGI 1 CELL MEMBRANE ANTIGENS Rarely Paraneoplastic
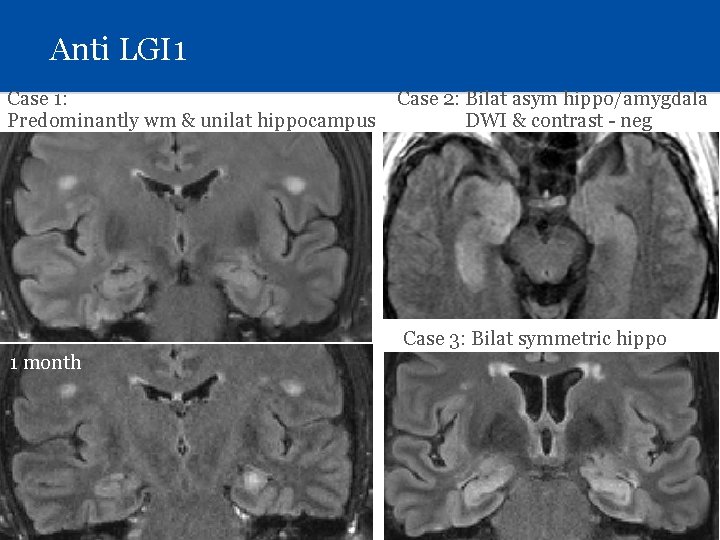
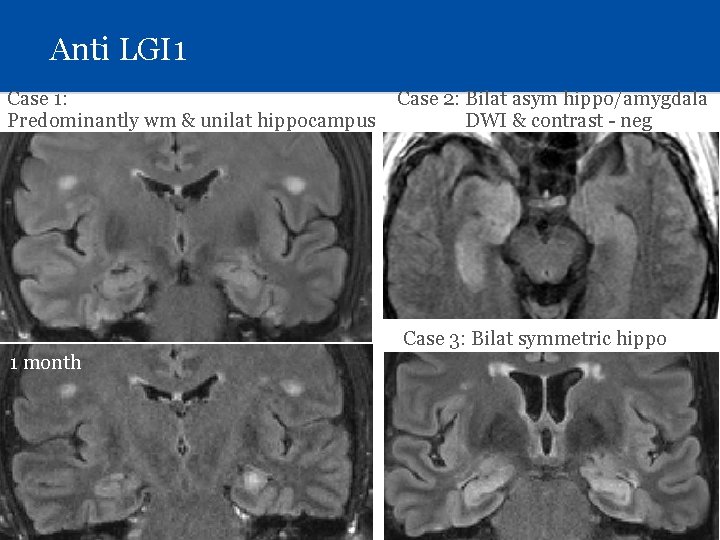
Anti LGI 1 Case 1: Predominantly wm & unilat hippocampus Case 2: Bilat asym hippo/amygdala DWI & contrast - neg Case 3: Bilat symmetric hippo 1 month
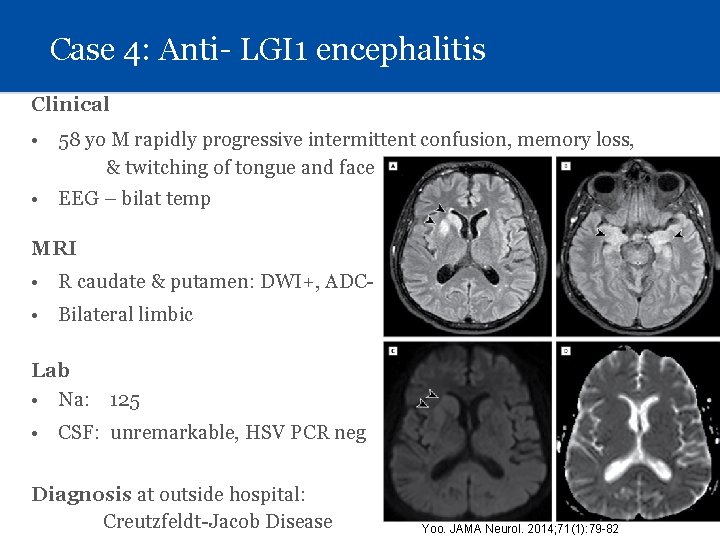
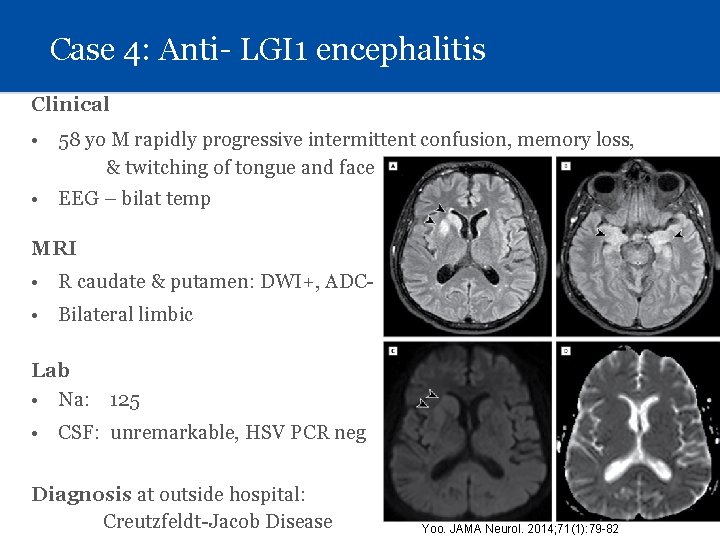
Case 4: Anti- LGI 1 encephalitis Clinical • 58 yo M rapidly progressive intermittent confusion, memory loss, & twitching of tongue and face • EEG – bilat temp MRI • R caudate & putamen: DWI+, ADC • Bilateral limbic Lab • Na: 125 • CSF: unremarkable, HSV PCR neg Diagnosis at outside hospital: Creutzfeldt-Jacob Disease Yoo. JAMA Neurol. 2014; 71(1): 79 -82
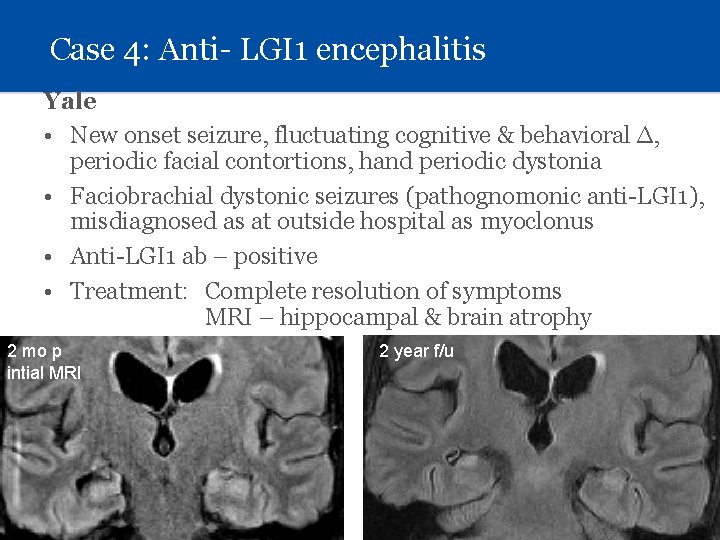
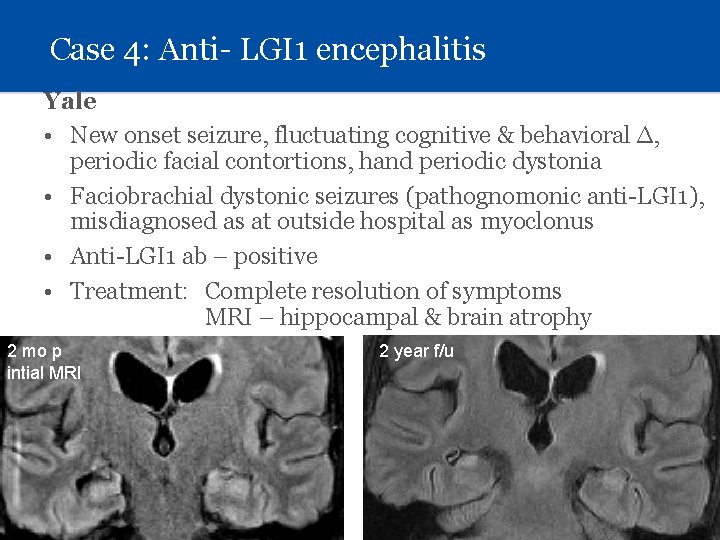
Case 4: Anti- LGI 1 encephalitis Yale • New onset seizure, fluctuating cognitive & behavioral ∆, periodic facial contortions, hand periodic dystonia • Faciobrachial dystonic seizures (pathognomonic anti-LGI 1), misdiagnosed as at outside hospital as myoclonus • Anti-LGI 1 ab – positive • Treatment: Complete resolution of symptoms MRI – hippocampal & brain atrophy 2 mo p intial MRI 2 year f/u
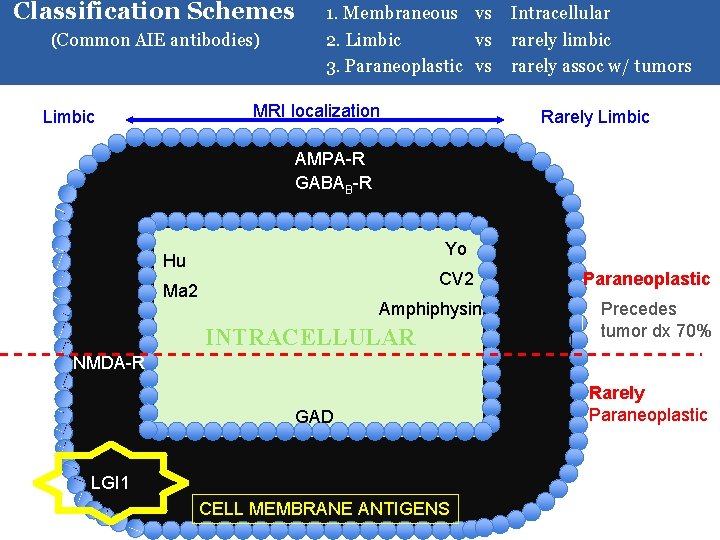
Classification Schemes (Common AIE antibodies) 1. Membraneous vs Intracellular 2. Limbic vs rarely limbic 3. Paraneoplastic vs rarely assoc w/ tumors MRI localization Limbic Rarely Limbic AMPA-R GABAB-R Yo Hu CV 2 Ma 2 Amphiphysin INTRACELLULAR Paraneoplastic Precedes tumor dx 70% NMDA-R GAD LGI 1 CELL MEMBRANE ANTIGENS Rarely Paraneoplastic
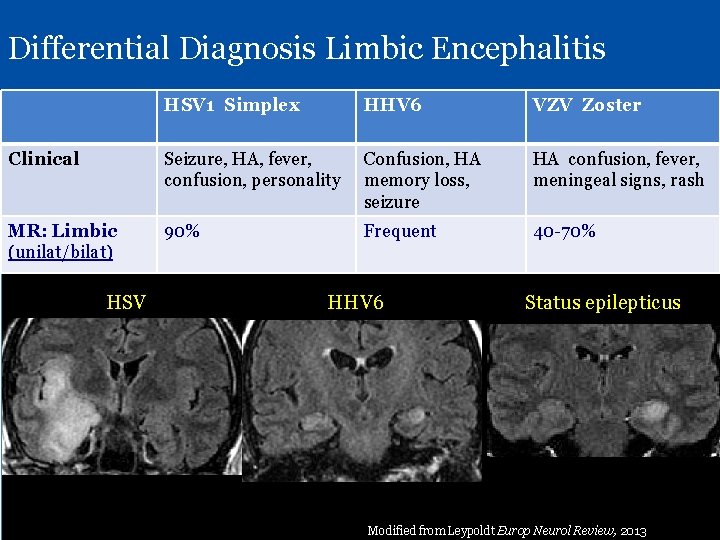
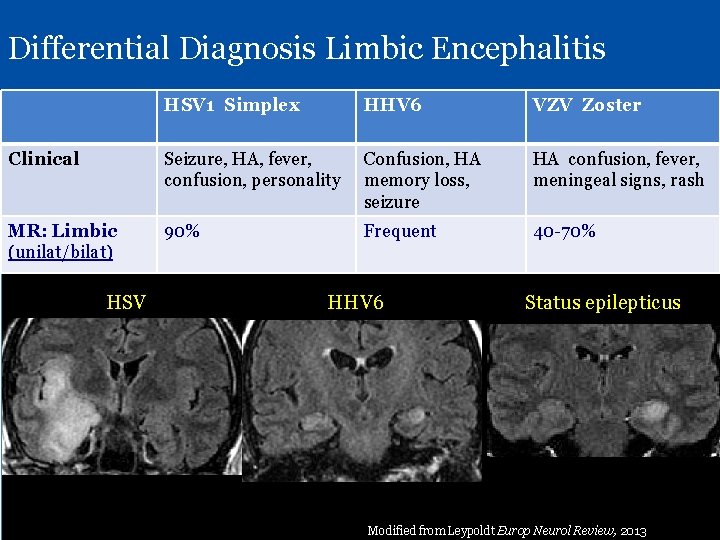
Differential Diagnosis Limbic Encephalitis HSV 1 Simplex HHV 6 VZV Zoster Clinical Seizure, HA, fever, confusion, personality Confusion, HA memory loss, seizure HA confusion, fever, meningeal signs, rash MR: Limbic (unilat/bilat) 90% Frequent 40 -70% HSV HHV 6 Status epilepticus Ddx LE includes SLE, Sjogrens, Primary angiitis CNS – MRI abnormalities very rare Modified from Leypoldt Europ Neurol Review, 2013
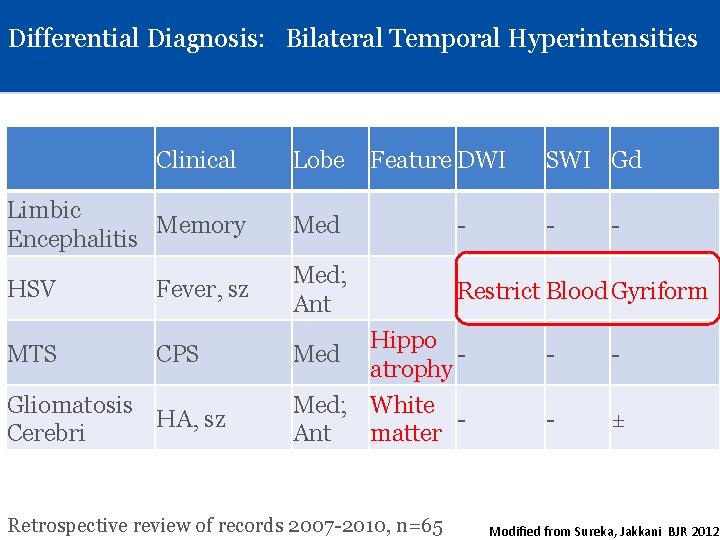
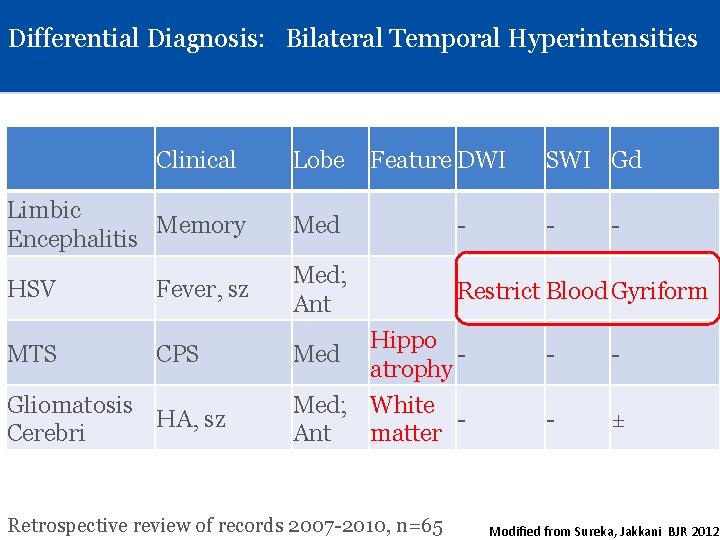
Differential Diagnosis: Bilateral Temporal Hyperintensities Clinical Lobe Feature DWI SWI Gd Limbic Memory Encephalitis Med - HSV Med; Ant Restrict Blood Gyriform MTS Fever, sz CPS Gliomatosis HA, sz Cerebri - - Hippo atrophy - - Med; White Ant matter - ± Med Retrospective review of records 2007 -2010, n=65 Modified from Sureka, Jakkani BJR 2012
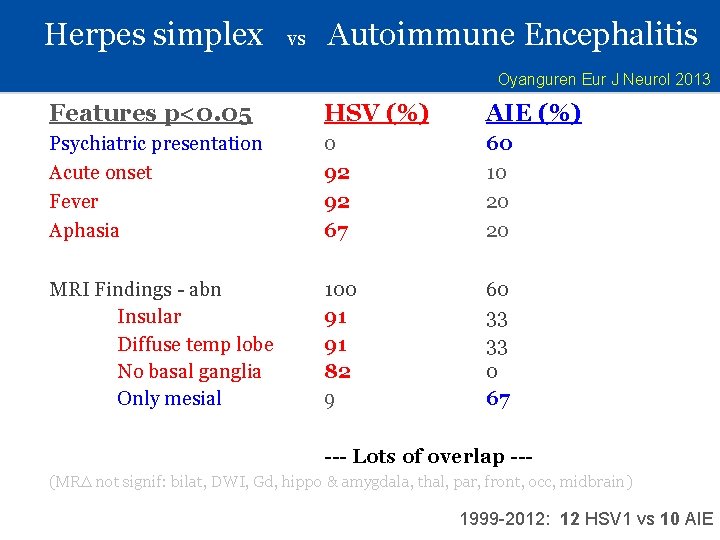
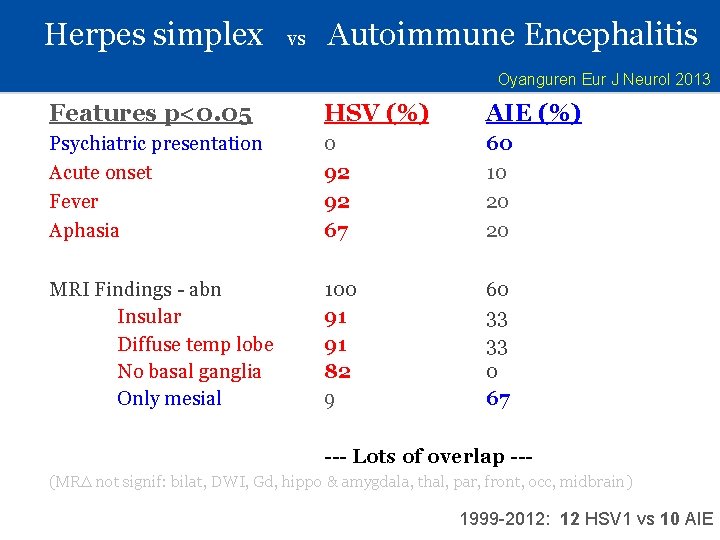
Herpes simplex vs Autoimmune Encephalitis Oyanguren Eur J Neurol 2013 Features p<0. 05 HSV (%) AIE (%) Psychiatric presentation Acute onset Fever Aphasia 0 92 92 67 60 10 20 20 MRI Findings - abn Insular Diffuse temp lobe No basal ganglia Only mesial 100 91 91 82 9 60 33 33 0 67 --- Lots of overlap --(MR∆ not signif: bilat, DWI, Gd, hippo & amygdala, thal, par, front, occ, midbrain) 1999 -2012: 12 HSV 1 vs 10 AIE
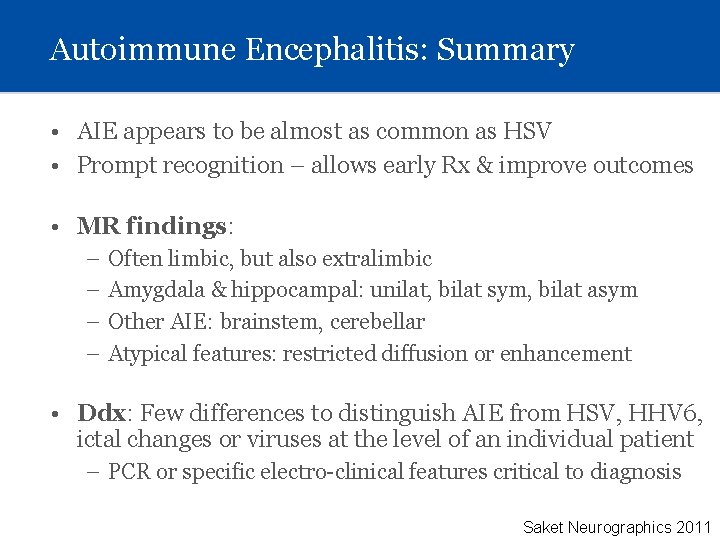
Autoimmune Encephalitis: Summary • AIE appears to be almost as common as HSV • Prompt recognition – allows early Rx & improve outcomes • MR findings: – – Often limbic, but also extralimbic Amygdala & hippocampal: unilat, bilat sym, bilat asym Other AIE: brainstem, cerebellar Atypical features: restricted diffusion or enhancement • Ddx: Few differences to distinguish AIE from HSV, HHV 6, ictal changes or viruses at the level of an individual patient – PCR or specific electro-clinical features critical to diagnosis Saket Neurographics 2011
Acknowledgements & References • Acknowledgements – cases & material – – Jiyeoun Yoo Pue Farooque Joachim Baehring Larry Hirsch • Key References – – – – – Leypoldt European Neurological Review, 2013; 8(1): 31 -7 Saket Neurographics 2011 Autoimmune Encephalitis EFNS Guidelines Eur J Neurol 2010 Sureka Jakkani BJR 2012 Oyanguren Eur J Neurol 2013 Varadkar Lancet Neurology 2014 Bien. European consensus statement Brain 2005 Bien Neurology 2002; Pradeep Acta Neurol Scand 2013 Bien Ann Neurology 2002 Ramussen Neurology 1958