Infections of Nervous System Encephalitis Meningitis Encephalitis Severe



- Slides: 34
Infections of Nervous System Encephalitis Meningitis
Encephalitis • Severe inflammation of the brain • Usually caused by a mosquito-borne or a tic -borne virus • Can also be caused by: – Ingestion of infected goat’s milk – Accidental injection or inhalation of the virus
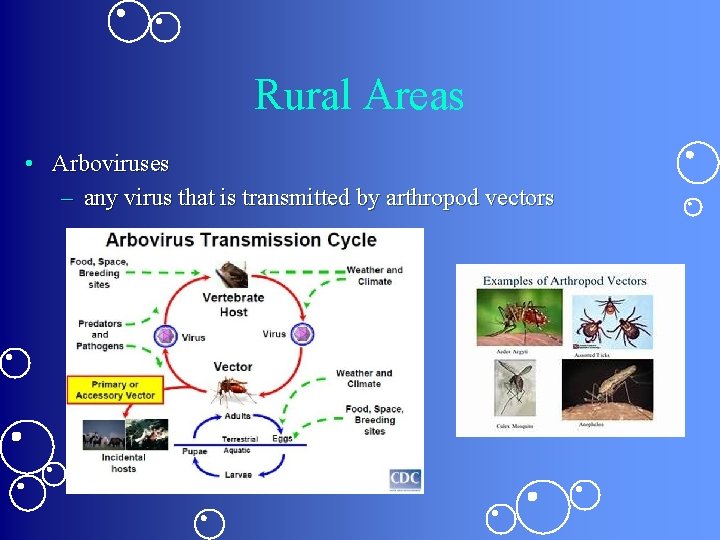
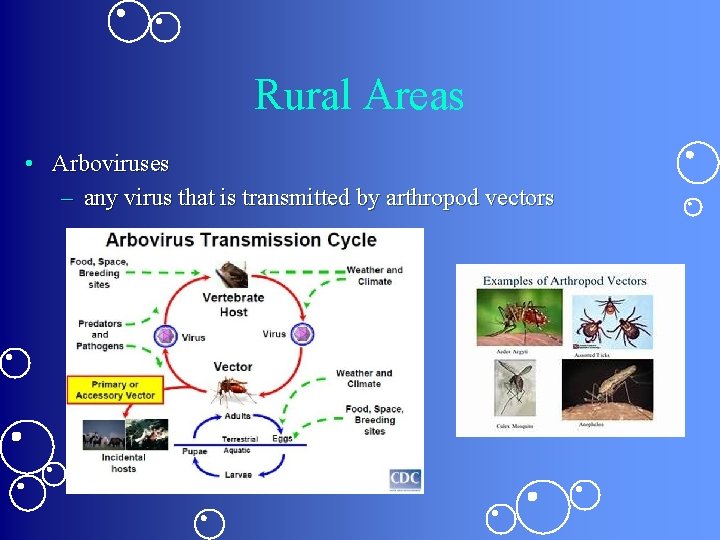
Rural Areas • Arboviruses – any virus that is transmitted by arthropod vectors
Urban Areas • Usually caused by enteroviruses – named by their transmission-route through the intestine – often found in the respiratory secretions and stool of an infected person – Types • Coxsackievirus • Echovirus • Poliovirus – Historically, poliomyelitis was the most significant disease caused by an enterovirus
Other viruses implicated • • • Herpesvirus Mumps HIV Adenoviruses Demyelinating diseases following: – Measles – Varicella – Rubella – Vaccination
Pathophysiology • Intense lymphocytic infiltration of brain tissues and leptomeninges – arachnoid and pia mater – the two innermost layers of tissue that cover the brain and spinal cord • Leads to: – Cerebral edema, degeneration of the brain’s ganglion cells, & diffuse nerve cell destruction
Signs & Symptoms • Fever of 102 -105 (38. 8 -40. 6) • Headache • Vomiting
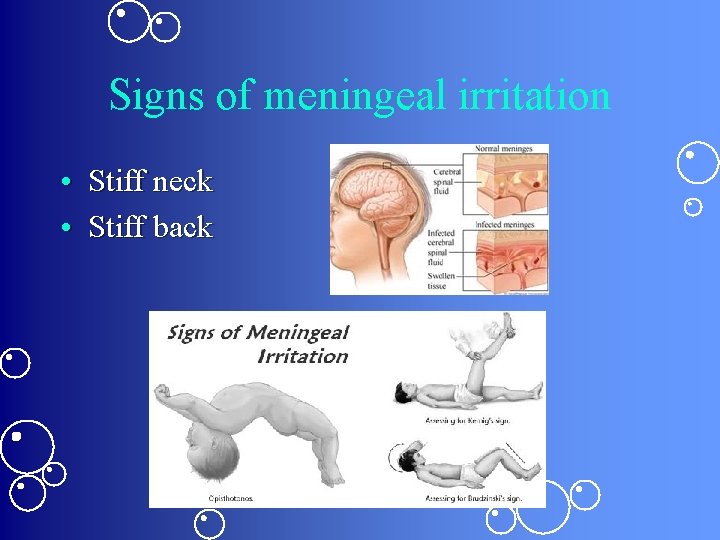
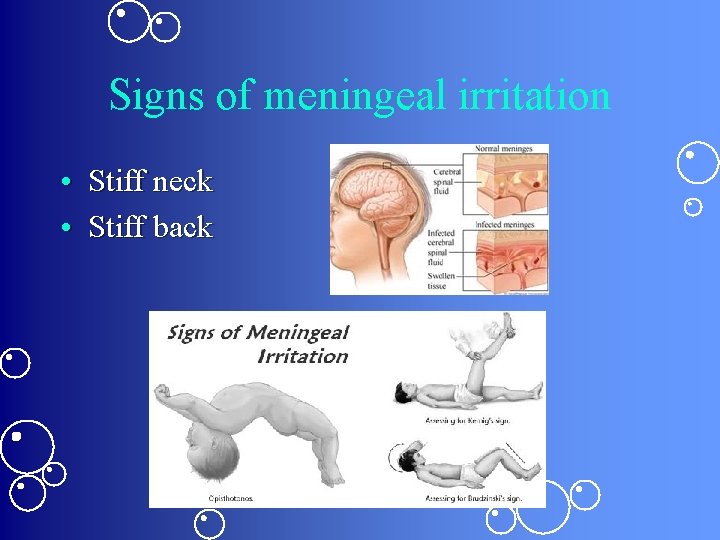
Signs of meningeal irritation • Stiff neck • Stiff back
Signs of neuron damage • • • Drowsiness Coma Paralysis Seizures Ataxia Organic psychoses
Diagnostics • CSF or blood analysis to identify the causative virus • Technetium-99 scan may show localized abnormalities • CT scan may disclose localized abnormalities
Treatment • Antiviral agents such as acyclovir • Anticonvulsants to prevent or control seizures • Furosemide or Mannitol to reduce cerebral swelling • Sedative to alleviate restlessness • ASA or Tylenol to relieve headache and reduce fever • Fluids & lytes to prevent dehydration and electrolyte imbalance • Antibiotics for secondary infections
Nursing Actions • • Frequent neuro assessments Monitor I & O Position changes to avoid joint stiffness & neck pain ROM to prevent contractures Darkened room & decreased stimulation Maintain adequate nutrition Reassure patient & family that behavior changes caused by the condition usually disappear Frequent reorientation
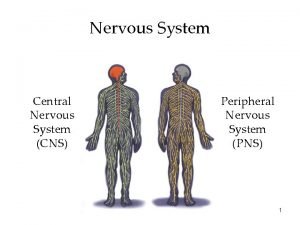
Meningitis • Brain & spinal cord become inflamed – Usually d/t bacterial infection • May involve all 3 layers of meninges – Dura mater – Arachnid mater – Pia mater

Promptness improves prognosis • If treated early, decreased risk of complications: – Increased ICP – Hydrocephalus – Cerebral infarction – Cranial nerve deficits • Optic neuritis • Deafness – Brain abscess – Seizures or coma
Etiology • Bacteremia – Pneumonia – Empyema – Osteomyelitis – Endocarditis • Aseptic – Virus or other organism • Sometimes no causative organism can be found
Other Infections Associated with Meningitis • • • Sinusitis Otitis media Encephalitis Myelitis Brain abscess – H flu – Strep Pneumonia – E Coli
Any Opening • May follow trauma or invasive procedures – Skull fx – Penetrating head wound – Lumbar puncture – Ventricular shunting
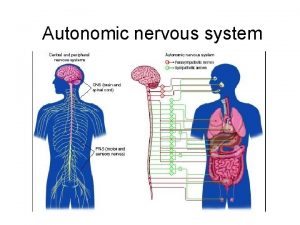
Routes of Entry 1. The blood • Most common 2. A direct opening between the CSF & the environment as a result of trauma 3. Along the cranial and peripheral nerves 4. Through the mouth or nose
Pathophysiology • Invading organism triggers an inflammatory response in the meninges • Neutrophils gather in the area & produce an exudate in the subarachnoid space – Causes the CSF to thicken • CSF flows less readily around the brain & spinal cord – Can block the arachnoid villi & further obstruct CSF flow leading to hydrocephalus

Exudate can also • Exacerbate the inflammatory response – Increases the pressure in the brain • Extend to the cranial and peripheral nerves – Triggering additional inflammation • Irritate the meninges – Disrupting their cell membranes – Causing edema
Consequences of Meningitis • • • Elevated ICP Engorged blood vessels Disrupted cerebral blood supply Possible thrombosis or rupture Cerebral infarction if ICP can’t be reduced Possible encephalitis – Secondary infection of the brain tissue
Aseptic Meningitis • Lymphocytes infiltrate the pia-arachnoid layers but usually not as severely as in bacterial meningitis – No exudate is formed • Makes this type of meningitis, self-limiting
Signs & Symptoms • Fever, chills, & malaise – d/t infection & inflammation • Headache & vomiting • Sometimes papilledema – Inflammation & edema of the optic nerve – Results from increased ICP
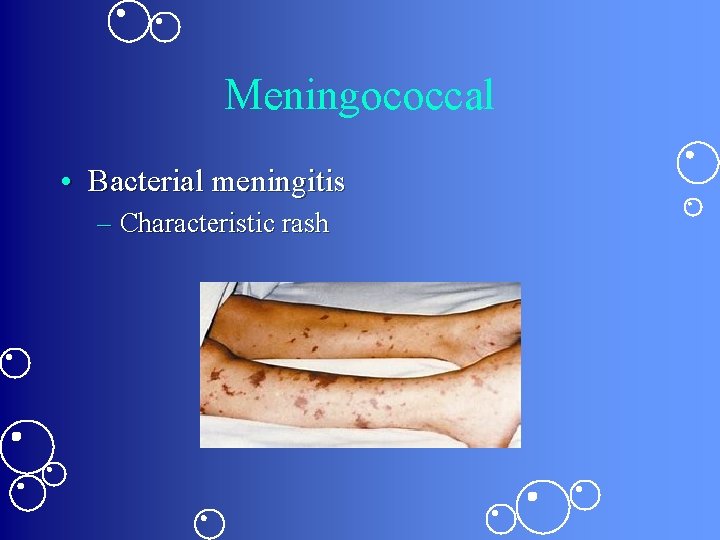
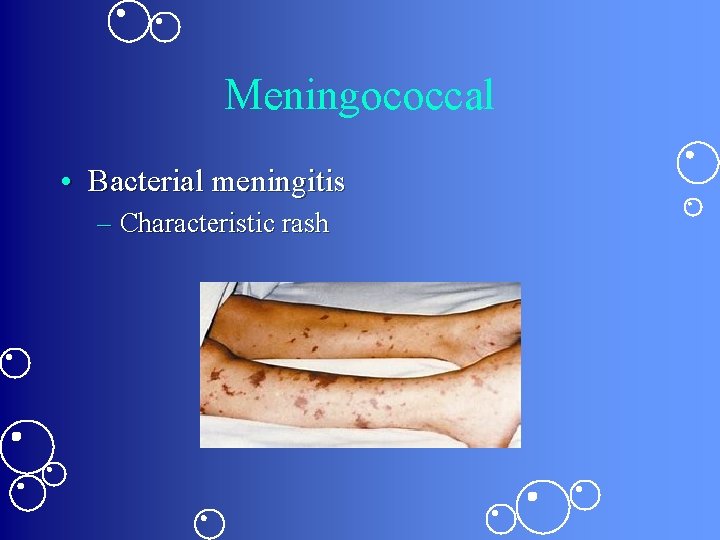
Meningococcal • Bacterial meningitis – Characteristic rash
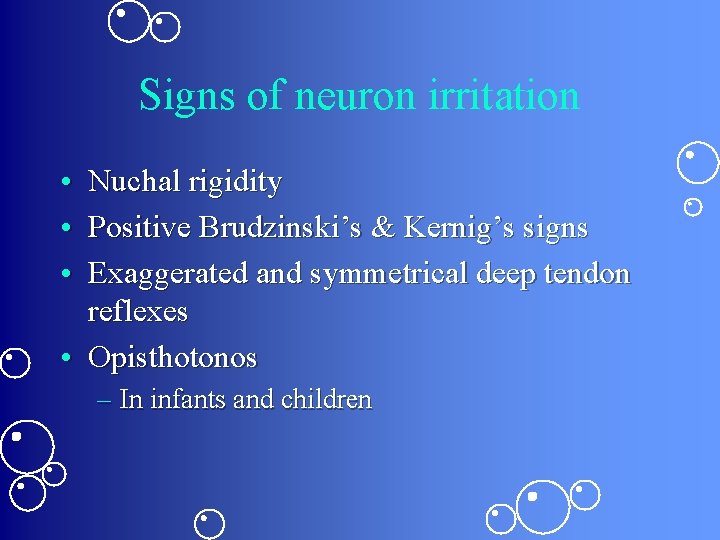
Signs of neuron irritation • Nuchal rigidity • Positive Brudzinski’s & Kernig’s signs • Exaggerated and symmetrical deep tendon reflexes • Opisthotonos – In infants and children
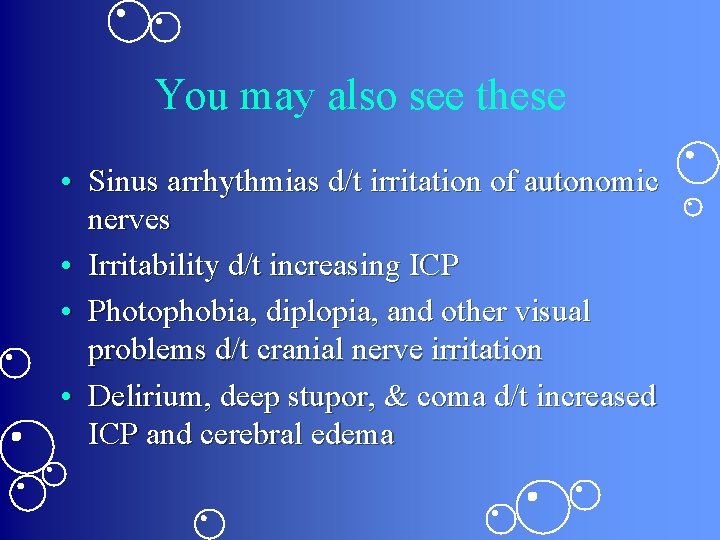
You may also see these • Sinus arrhythmias d/t irritation of autonomic nerves • Irritability d/t increasing ICP • Photophobia, diplopia, and other visual problems d/t cranial nerve irritation • Delirium, deep stupor, & coma d/t increased ICP and cerebral edema
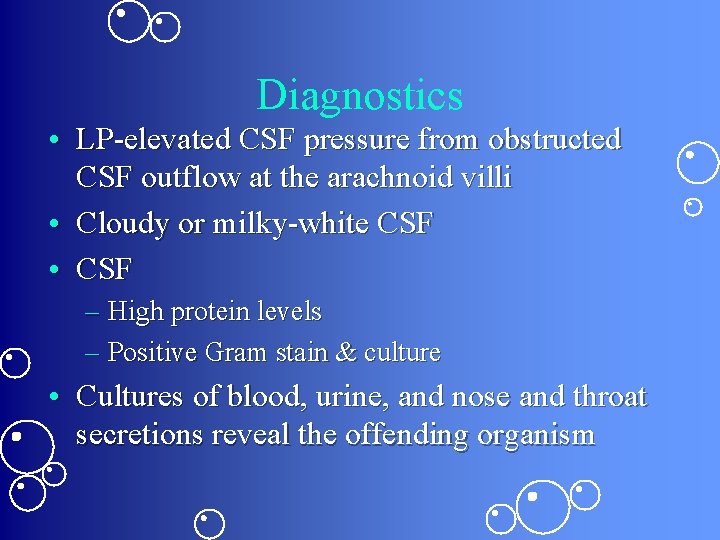
Diagnostics • LP-elevated CSF pressure from obstructed CSF outflow at the arachnoid villi • Cloudy or milky-white CSF • CSF – High protein levels – Positive Gram stain & culture • Cultures of blood, urine, and nose and throat secretions reveal the offending organism
Diagnostics, cont’d • CXR may reveal pneumonitis or lung abscess • Sinus and skull X-rays may identify paranasal sinusitis as the underlying infection or a skull fx as the mechanism for entrance of microorganisms • WBC count reveals leukocytosis
Treatment • • • Antibiotic therapy, usually for 2 weeks Digoxin to control arrhythmia Mannitol to decrease cerebral edema Anticonvulsant to prevent seizures Sedative to reduce restlessness Acetaminophen to relieve headache and fever
Supportive Measures • Bed rest • Fever reduction – Cooling blanket • Isolation if indicated – Family education
Nursing Actions • Frequent neuro assessments • Monitor for deterioration – Temperature increase, decreasing LOC, onset of seizures, altered respirations • Monitor fluid balance • Positioning • Maintain adequate nutrition & elimination • Maintain a quiet environment • Sterile technique for any dressing changes • Administer meds as indicated

Think of appropriate nursing diagnoses for patients with these infections
 Label the different types of neuronal pools in the figure.
Label the different types of neuronal pools in the figure. Sensory input and motor output
Sensory input and motor output Processes of neurons
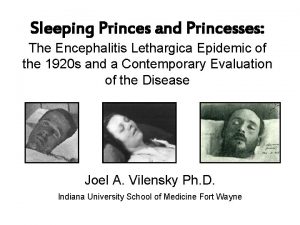
Processes of neurons Sleeping princesses
Sleeping princesses Culex mosquito
Culex mosquito Equine encephalitis
Equine encephalitis Equine encephalitis
Equine encephalitis Hsv encephalitis
Hsv encephalitis Virus herpes simplex de type 2
Virus herpes simplex de type 2 Nursing diagnosis of meningitis slideshare
Nursing diagnosis of meningitis slideshare Nursing care plan for headache slideshare
Nursing care plan for headache slideshare Fever and headache
Fever and headache Sfumato pronunciation
Sfumato pronunciation Nervous system and digestive system
Nervous system and digestive system Endocrine system vs nervous system
Endocrine system vs nervous system General mechanism of hormone action
General mechanism of hormone action Endocrine system
Endocrine system Opportunistic infections
Opportunistic infections Can methotrexate cause yeast infections
Can methotrexate cause yeast infections Opportunistic infections
Opportunistic infections Chapter 25 sexually transmitted infections and hiv/aids
Chapter 25 sexually transmitted infections and hiv/aids Understanding the mirai botnet
Understanding the mirai botnet Storch infections
Storch infections Storch infections
Storch infections Bone and joint infections
Bone and joint infections Neurosiphyllis
Neurosiphyllis Bacterial vaginosis
Bacterial vaginosis Postpartum infections
Postpartum infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Genital infections
Genital infections Amber blumling
Amber blumling Ciliary escalator
Ciliary escalator Classification of acute gingival infections
Classification of acute gingival infections Nursing management of increased intracranial pressure
Nursing management of increased intracranial pressure Meningitis belt africa
Meningitis belt africa