SPECTRUM OF AUTOIMMUNE ENCEPHALITIS IN CHILDREN AN UPDATE


- Slides: 27
SPECTRUM OF AUTOIMMUNE ENCEPHALITIS IN CHILDREN: AN UPDATE Dr. Tamoghna Biswas MBBS, MD (Pediatrics) Kolkata, WB
AUTOIMMUNE ENCEPHALITIS Expanding group of disorders Associated with antibodies against neuronal cell surface proteins or against synaptic receptors. Phenotype dependent on the type of causative antibodies and target antigens. Can affect any age group (infants to adults) More common in younger adults and children.
DIAGNOSTIC AND THERAPEUTIC CHALLENGE Broad spectrum of symptoms � Behavioral alterations and Psychosis � catatonia � Sleep cycle abnormalities � memory deficits � Seizures � Dyskinesia � Autonomic dysregulation Can be confused with a lot of other differentials presenting similarly. Mostly severe and potentially fatal, but patients frequently respond to immunotherapy with good outcomes.
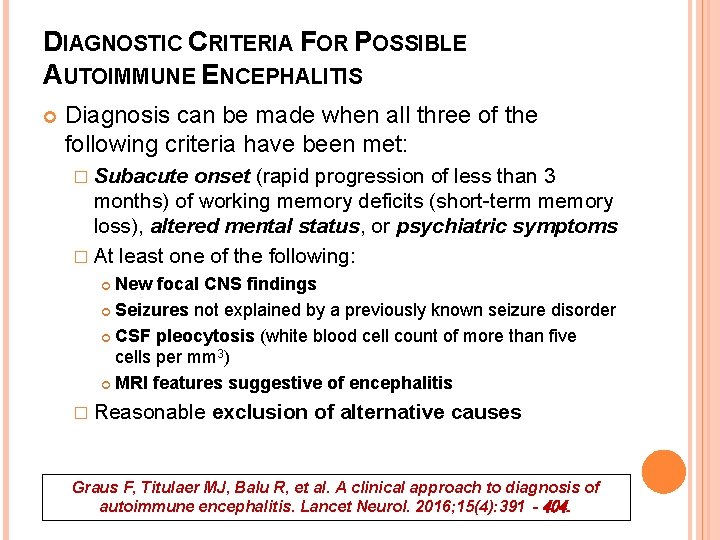
DIAGNOSTIC CRITERIA FOR POSSIBLE AUTOIMMUNE ENCEPHALITIS Diagnosis can be made when all three of the following criteria have been met: � Subacute onset (rapid progression of less than 3 months) of working memory deficits (short-term memory loss), altered mental status, or psychiatric symptoms � At least one of the following: New focal CNS findings Seizures not explained by a previously known seizure disorder CSF pleocytosis (white blood cell count of more than five cells per mm 3) MRI features suggestive of encephalitis � Reasonable exclusion of alternative causes Graus F, Titulaer MJ, Balu R, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 2016; 15(4): 391‐ 404.
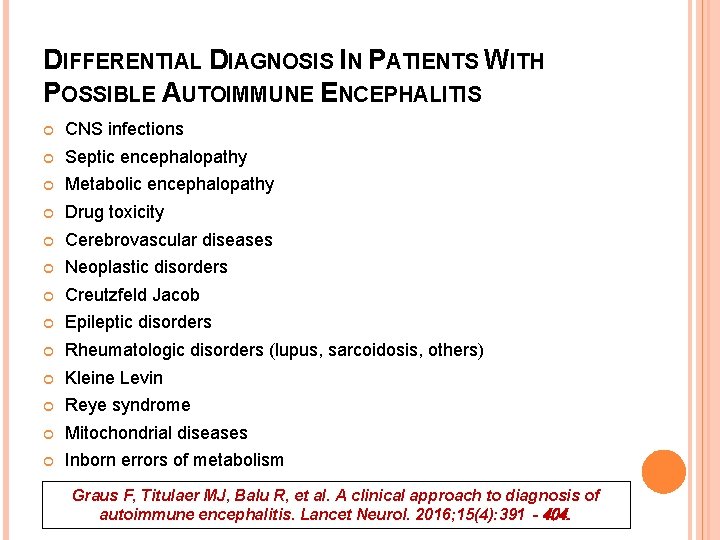
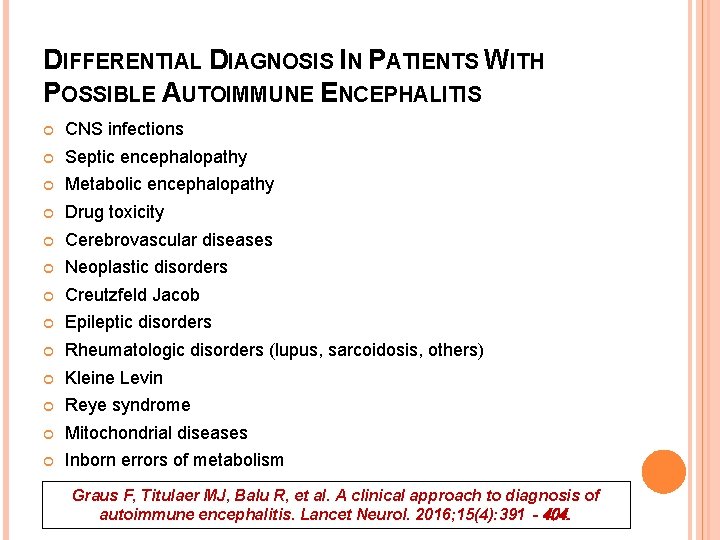
DIFFERENTIAL DIAGNOSIS IN PATIENTS WITH POSSIBLE AUTOIMMUNE ENCEPHALITIS CNS infections Septic encephalopathy Metabolic encephalopathy Drug toxicity Cerebrovascular diseases Neoplastic disorders Creutzfeld Jacob Epileptic disorders Rheumatologic disorders (lupus, sarcoidosis, others) Kleine Levin Reye syndrome Mitochondrial diseases Inborn errors of metabolism Graus F, Titulaer MJ, Balu R, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 2016; 15(4): 391‐ 404.
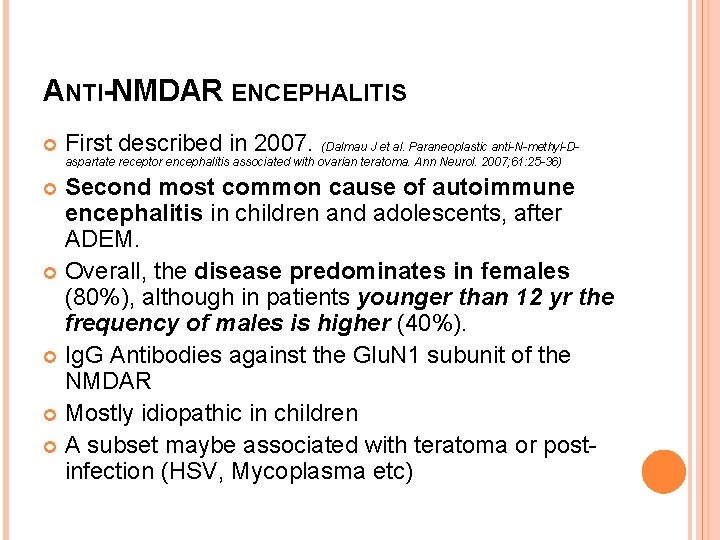
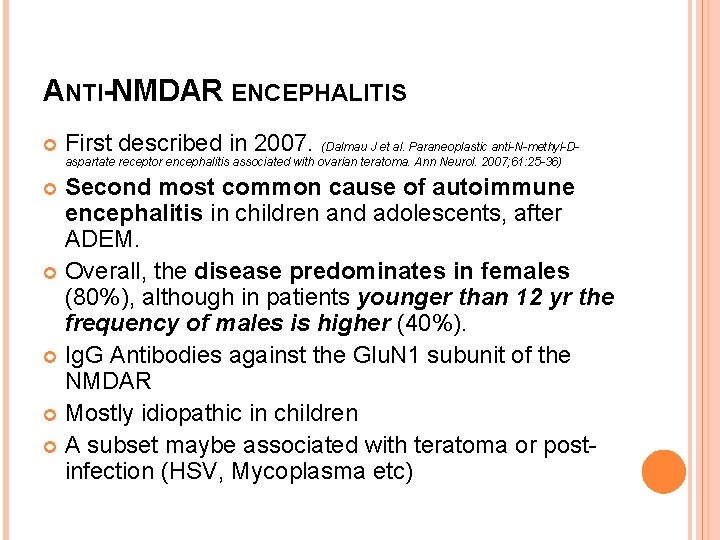
ANTI-NMDAR ENCEPHALITIS First described in 2007. (Dalmau J et al. Paraneoplastic anti-N-methyl-Daspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007; 61: 25 -36) Second most common cause of autoimmune encephalitis in children and adolescents, after ADEM. Overall, the disease predominates in females (80%), although in patients younger than 12 yr the frequency of males is higher (40%). Ig. G Antibodies against the Glu. N 1 subunit of the NMDAR Mostly idiopathic in children A subset maybe associated with teratoma or postinfection (HSV, Mycoplasma etc)
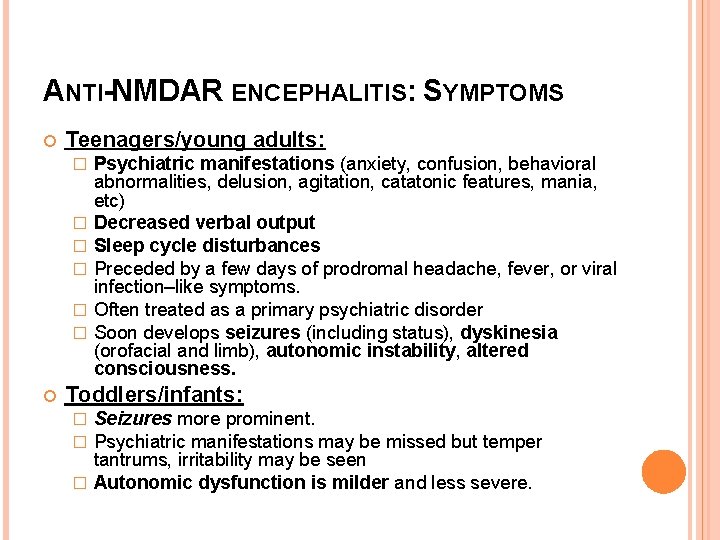
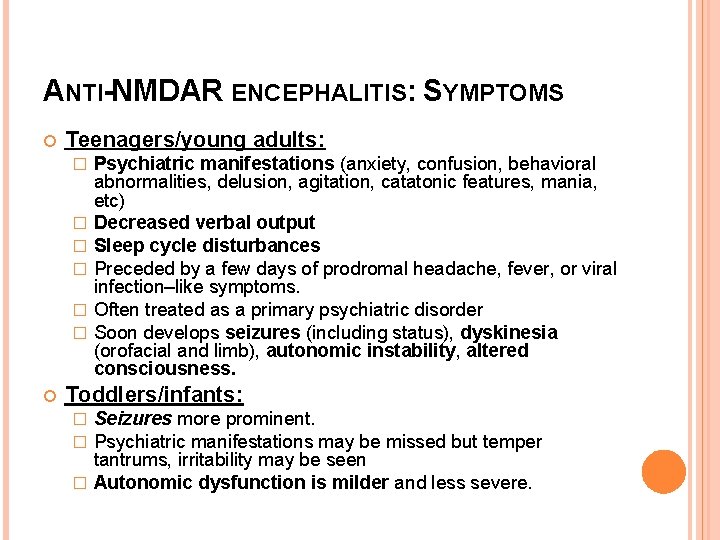
ANTI-NMDAR ENCEPHALITIS: SYMPTOMS Teenagers/young adults: � � � Psychiatric manifestations (anxiety, confusion, behavioral abnormalities, delusion, agitation, catatonic features, mania, etc) Decreased verbal output Sleep cycle disturbances Preceded by a few days of prodromal headache, fever, or viral infection–like symptoms. Often treated as a primary psychiatric disorder Soon develops seizures (including status), dyskinesia (orofacial and limb), autonomic instability, altered consciousness. Toddlers/infants: Seizures more prominent. Psychiatric manifestations may be missed but temper tantrums, irritability may be seen � Autonomic dysfunction is milder and less severe. � �
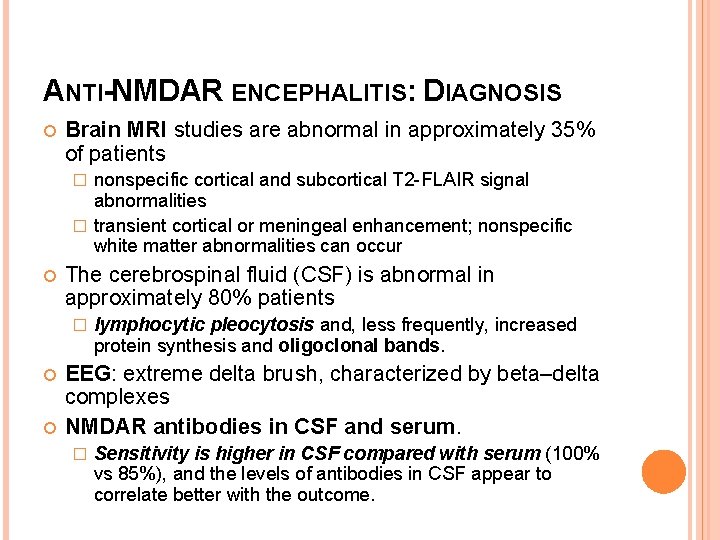
ANTI-NMDAR ENCEPHALITIS: DIAGNOSIS Brain MRI studies are abnormal in approximately 35% of patients nonspecific cortical and subcortical T 2 -FLAIR signal abnormalities � transient cortical or meningeal enhancement; nonspecific white matter abnormalities can occur � The cerebrospinal fluid (CSF) is abnormal in approximately 80% patients � lymphocytic pleocytosis and, less frequently, increased protein synthesis and oligoclonal bands. EEG: extreme delta brush, characterized by beta–delta complexes NMDAR antibodies in CSF and serum. � Sensitivity is higher in CSF compared with serum (100% vs 85%), and the levels of antibodies in CSF appear to correlate better with the outcome.
ANTI-NMDAR ENCEPHALITIS: TREATMENT First-line immunotherapies, including � Corticosteroids � IVIG � plasma exchange Can fail in upto 50% Reports of success with rituximab, cyclophosphamide Tumor removal suggested in tumor associated cases. Almost 80% cases recover, partially or fully. Recovery is slow, may take more than 2 y. Mortality is around 7%.
DEMYELINATION DISORDERS: ADEM Acute disseminated encephalomyelitis (ADEM) is the most frequent autoimmune encephalitis in children. Polyfocal neurologic deficits Acute onset Prodromal symptoms like lethargy, fever, headache, vomiting Meningeal signs, and seizures Encephalopathy is the hallmark of ADEM
DEMYELINATION DISORDERS: NMOSD presents with ON, TM, or an area postrema syndrome such as intractable vomiting or hiccups. 2015 INPD criteria places huge importance on AQP 4 -Ab for diagnosis. MOG-Ab has recently been identified in many of the AQP 4 -Ab-negative presentations, with no reports of both AQP 4 -Ab and MOG-Ab being present simultaneously. AQP 4 -Ab–positive NMOSD presents usually in the older adult, with MOG-Ab NMOSD much more common in children and young people. AQP 4 -Ab NMOSD is more common in females while MOG-Ab–associated disorders have only a slight female preponderance.
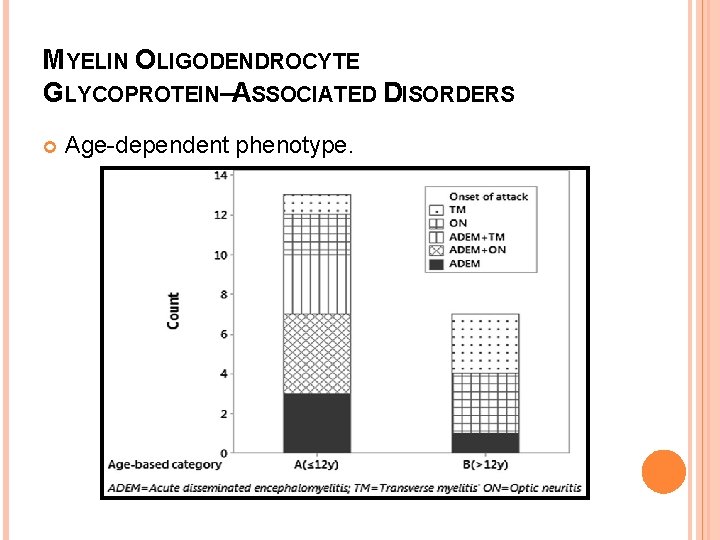
MYELIN OLIGODENDROCYTE GLYCOPROTEIN–ASSOCIATED DISORDERS Clinical phenotype overlaps with patients with ADEM and NMOSD. MOG-Ab is present in more than 30% of children presenting with an initial episode of demyelination. Up to 50% of cases of ADEM have been found to be associated with MOG-Ab positivity in the serum Almost all cases of MDEM are MOG-Ab positive.

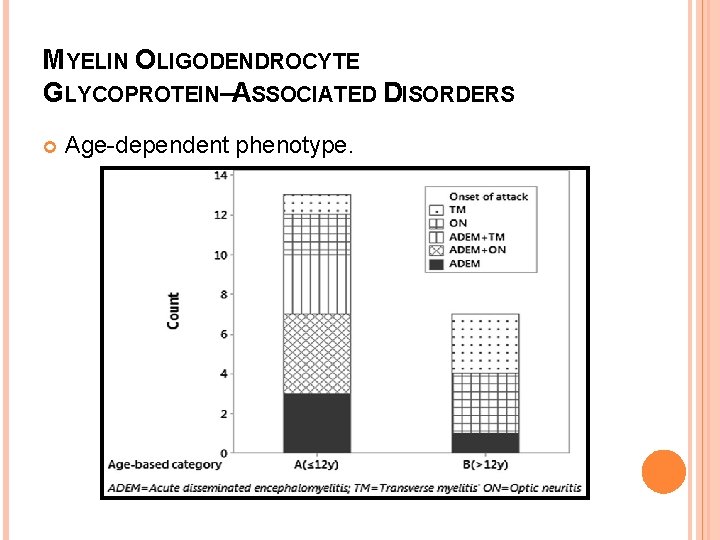
MYELIN OLIGODENDROCYTE GLYCOPROTEIN–ASSOCIATED DISORDERS Age-dependent phenotype.
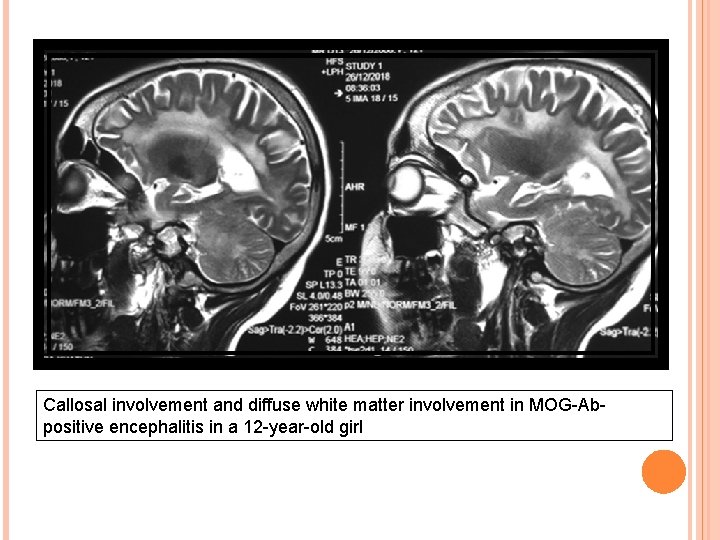
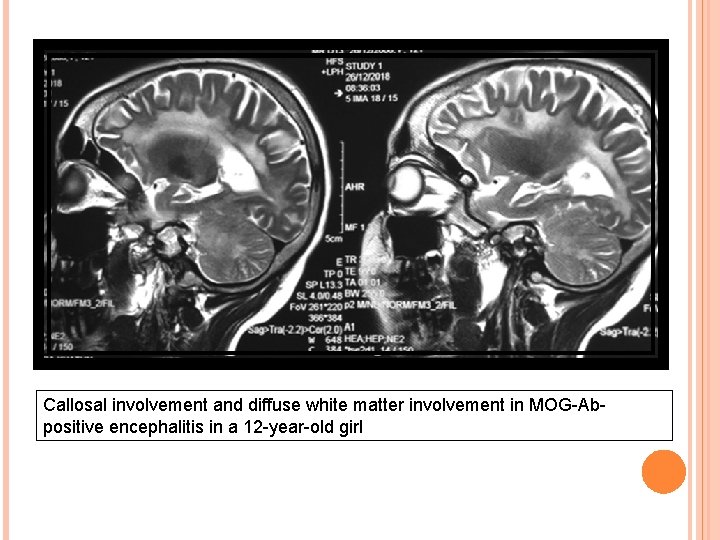
Callosal involvement and diffuse white matter involvement in MOG-Abpositive encephalitis in a 12 -year-old girl
ENCEPHALITIS ASSOCIATED WITH GABAA R ANTIBODIES Antibodies against α 1, β 3, or γ 2 subunits of the GABAa receptor. Almost 40% cases below 18 years of age. Association with thymoma in adults (40%), not reported in children. Refractory seizures and epilepsia partialis continua are the hallmark. Limb/orofacial dyskinesia may be seen.
ENCEPHALITIS ASSOCIATED WITH GABAA R ANTIBODIES EEG: � Almost always abnormal, epileptic activity. MRI: � Multifocal corticosubcortical FLAIR/T 2 hyperintensities in 77% of patients CSF: � Pleocytosis and/increased proteins Treatment: � Immunotherapy. � Good response in almost 80% cases.
AUTOIMMUNE LIMBIC ENCEPHALITIS Inflammatory process involving limbic system � Medial temporal lobe � Cingulate gyrus � Amygdala ‘Limbic encephalitis’ has been inappropriately used as a characteristic vague terminology encompassing any encephalitis with seizures/memory disturbances!
AUTOIMMUNE LIMBIC ENCEPHALITIS: IN ADULTS Antibodies against proteins earlier thought to be voltage-gated potassium channels (VGKC). Currently, two proteins are considered vital: � leucine-rich glioma-inactivated 1 (LGI 1) hyponatremia dystonic or myoclonic-like movements, described as faciobrachial dystonic seizures � Caspr 2 Morvan syndrome (encephalopathy, seizures, a sleep disorder, autonomic dysfunction, neuromyotonia) In patients without LGI 1 or Caspr 2, detection of VGKC has little to no clinical significance.
AUTOIMMUNE LIMBIC ENCEPHALITIS: IN CHILDREN In children, the identification of LGI 1 or Caspr 2 antibodies is unusual. A positive test for VGKC-complex antibodies does not necessarily indicate autoimmune encephalitis in children. Any disorder with seizures, altered sensorium or memory disturbance is NOT limbic encephalitis.
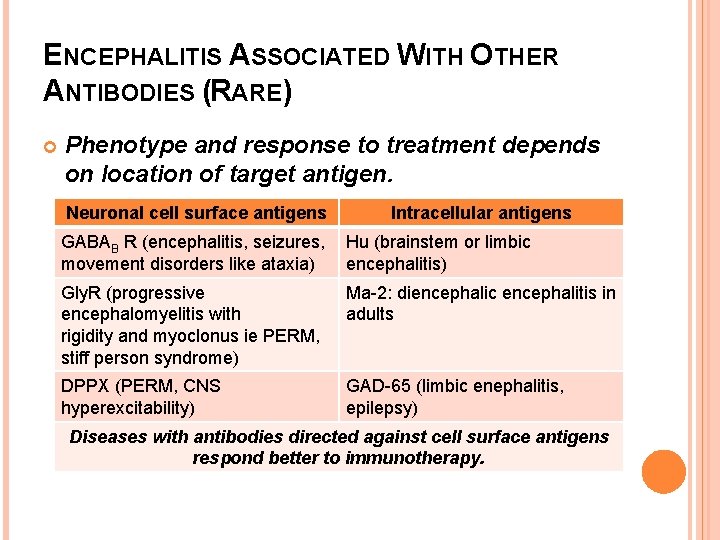
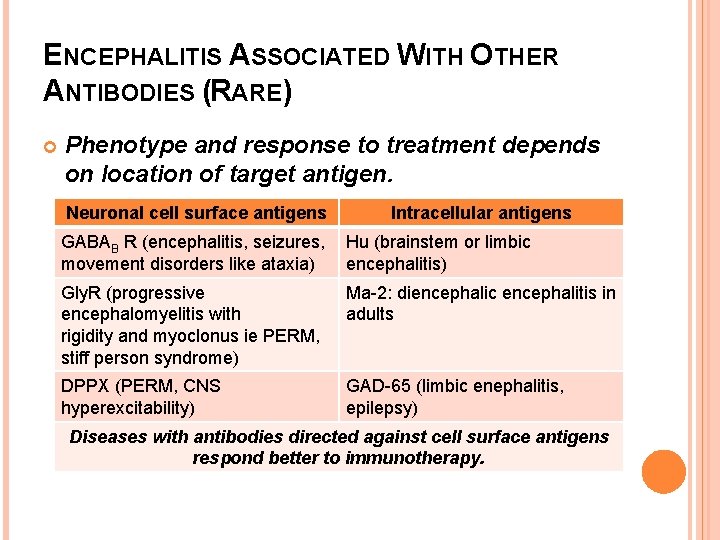
ENCEPHALITIS ASSOCIATED WITH OTHER ANTIBODIES (RARE) Phenotype and response to treatment depends on location of target antigen. Neuronal cell surface antigens Intracellular antigens GABAB R (encephalitis, seizures, movement disorders like ataxia) Hu (brainstem or limbic encephalitis) Gly. R (progressive encephalomyelitis with rigidity and myoclonus ie PERM, stiff person syndrome) Ma-2: diencephalic encephalitis in adults DPPX (PERM, CNS hyperexcitability) GAD-65 (limbic enephalitis, epilepsy) Diseases with antibodies directed against cell surface antigens respond better to immunotherapy.
OPSOCLONUS–MYOCLONUS AND OTHER CEREBELLAR–BRAINSTEM ENCEPHALITIS Irritability, ataxia, myocolonus, opsoclonus. Associated with neuroblastoma in >50% children aged less than 2 y. Associated with teratoma in young adults. MRI: Frequently normal, may show cerebellar atrophy. EEG: Normal. CSF: Usually normal, or may show some B-cell activation Most patients do NOT have detectable autoantibodies, some have Hu antibodies. Treatment: ACTH, immunotherapy (IVIg, steroids), rituximab, tumor removal if tumor-associated
BICKERSTAFF ENCEPHALITIS Symptoms: � Opthalmoplegia � Ataxia � Decreased consciousness, � Hypersomnolence � Hyperreflexia (Hyporeflexia may be seen in Miller-Fisher overlap) GQ-1 b autoantibodies in 65% Abnormal MRI in 30% cases. Abnormal NCV (predominant axonal injury) in 45% patients. Good response to immunotherapy.
HASHIMOTO ENCEPHALOPATHY Steroid-responsive encephalopathy with autoimmune thyroiditis (SREAT) Anti-TPO antibodies. Non specific clinical features which includes strokelike episodes, seizures, hallucinations, behavior changes, sleep cycle alterations, ataxia etc. CSF: Elevated protein level, rarely pleocytosis EEG: Generalized slowing MRI: may be normal. Excellent response to steroids.
RASMUSSEN ENCEPHALITIS Unclear etiology, parainfectious-autoimmune mechanism suggested. Presents in children aged 6 -8 years. Progressive refractory partial seizures (may be unilateral), cognitive decline, hemiplegia, and brain hemiatrophy. MRI: Unilateral hemispheric atrophy. Treatment: � � � high-dose steroids, plasma exchange, or IVIG (in early stages of the disease) Rituximab Intraventicular γ-interferon Tacrolimus Adalimumab Functional hemispherectomy (most effective treatment)
OTHER SUSPECTED TYPES OF AUTOIMMUNE ENCEPHALITIS Rapid-onset obesity with hypothalamic dysfunction, hypoventilation, and autonomic dysregulation (ROHHAD) Basal ganglia encephalitis Pseudomigraine syndrome with CSF pleocytosis (PMP) or headache with neurologic deficits and CSF lymphocytosis (Ha. NDL)

Thank You
 Backup and recovery techniques
Backup and recovery techniques Equine encephalitis
Equine encephalitis Health education for meningitis slideshare
Health education for meningitis slideshare Sleeping princesses
Sleeping princesses Hsv encephalitis
Hsv encephalitis Rasmussen syndrome
Rasmussen syndrome Japanese encephalitis virus
Japanese encephalitis virus Virus herpes simplex de type 2
Virus herpes simplex de type 2 Ueno pronunciation
Ueno pronunciation Equine encephalitis
Equine encephalitis Nursing diagnosis of retinal detachment slideshare
Nursing diagnosis of retinal detachment slideshare Autoimmune diet
Autoimmune diet Is crohns autoimmune
Is crohns autoimmune Beau's lines autoimmune disease
Beau's lines autoimmune disease Hijama for hyperthyroidism
Hijama for hyperthyroidism Absortpion
Absortpion Explain electronic configuration of cu and cr
Explain electronic configuration of cu and cr Microsoft security essential tidak bisa update
Microsoft security essential tidak bisa update Flash player update
Flash player update Tomato flames
Tomato flames Update data sisdmk
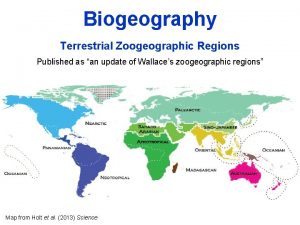
Update data sisdmk An update of wallace’s zoogeographic regions of the world
An update of wallace’s zoogeographic regions of the world Nepal research and education network
Nepal research and education network Replace
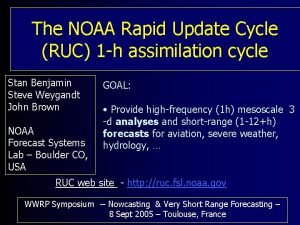
Replace Recovery techniques based on immediate update
Recovery techniques based on immediate update Language windows 10
Language windows 10 Microsoft update
Microsoft update Excel ismétlődések törlése
Excel ismétlődések törlése