Masqueraders of Asthma Differential Diagnosis of Asthma in


- Slides: 31
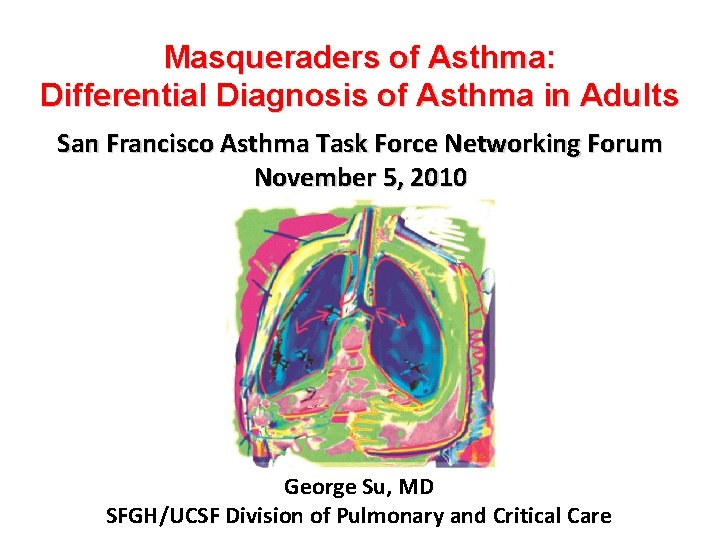
Masqueraders of Asthma: Differential Diagnosis of Asthma in Adults San Francisco Asthma Task Force Networking Forum November 5, 2010 George Su, MD SFGH/UCSF Division of Pulmonary and Critical Care
asqma “asthma” aazein “aazein”
Wheeze • A continuous, coarse, whistling sound produced in the respiratory tract during breathing • Some part of the respiratory tract must be narrowed or obstructed, or airflow velocity increased

Case 1 • 58 yo male, presents with worsening shortness of breath over the past 7 months. • +Wheeze, is noted nearly daily, and is elicited reproducibly by cold weather and exposure to fumes and cats. • +Moderately productive cough daily. Up to 2 packs of cigarettes a day over the past 40 years, current smoker. • PMH: DM, HTN • Works as a custodian at the local university.
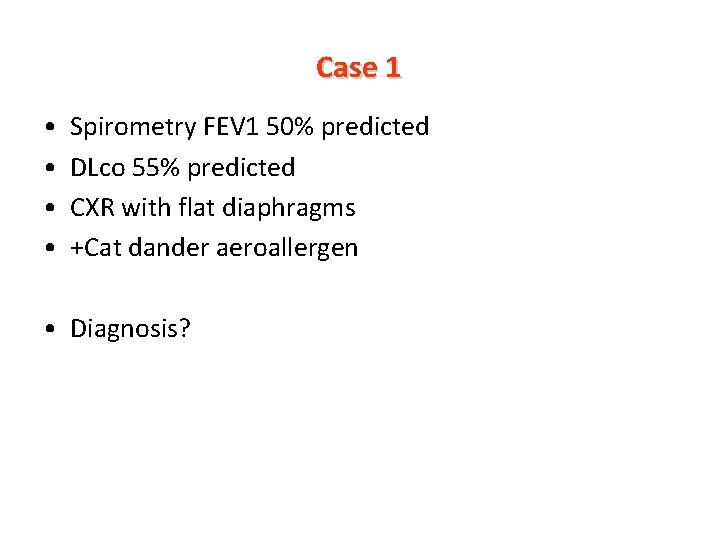
Case 1 • • Spirometry FEV 1 50% predicted DLco 55% predicted CXR with flat diaphragms +Cat dander aeroallergen • Diagnosis?
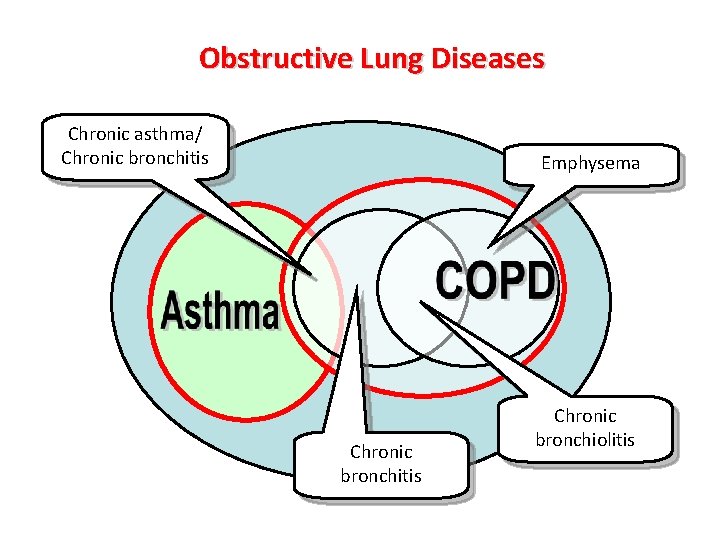
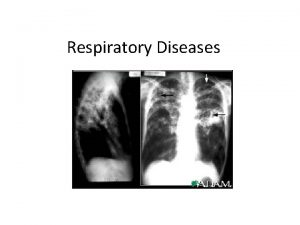
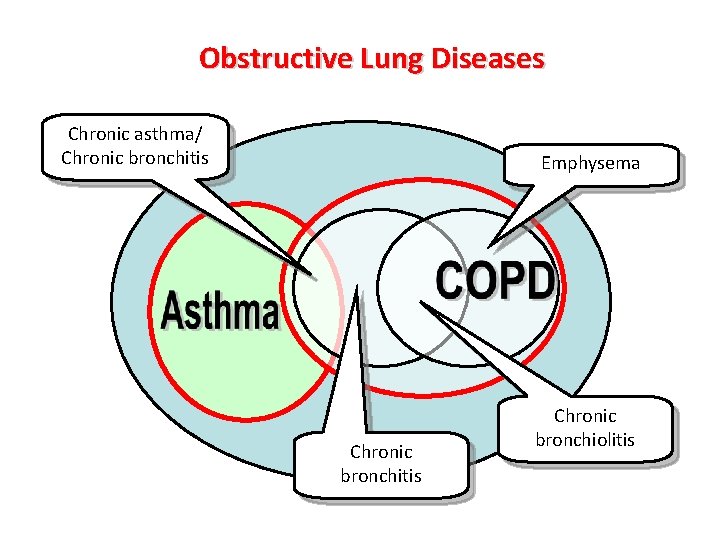
Obstructive Lung Diseases Chronic asthma/ Chronic bronchitis Emphysema Chronic bronchitis Chronic bronchiolitis
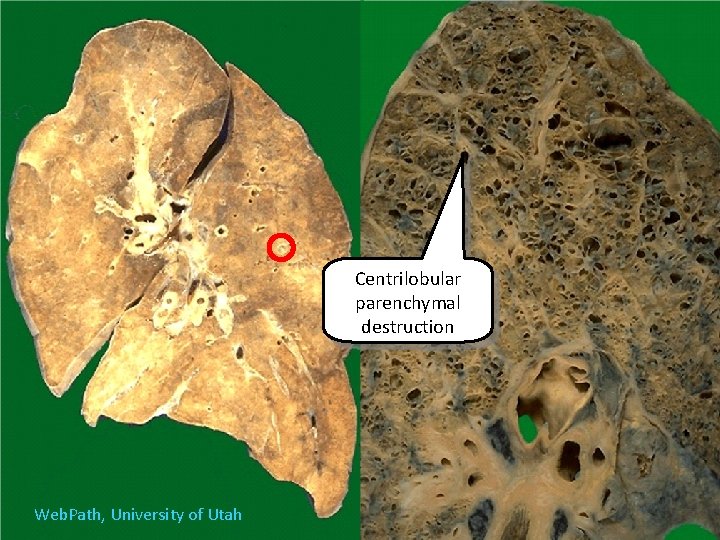
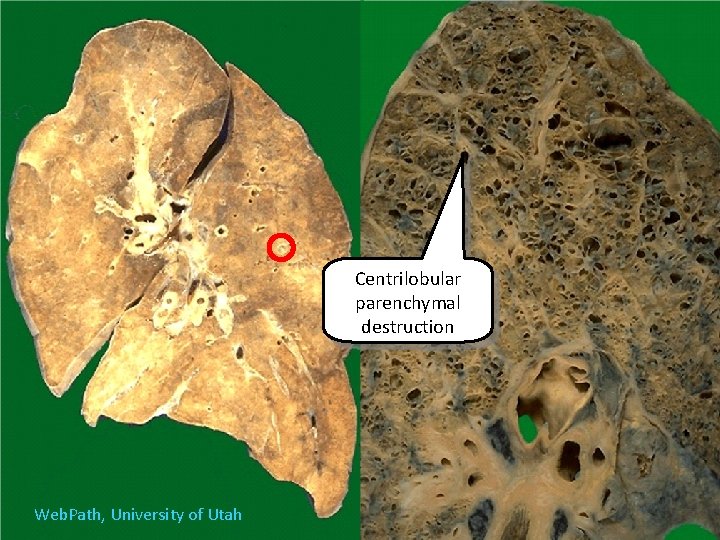
Centrilobular parenchymal destruction Web. Path, University of Utah
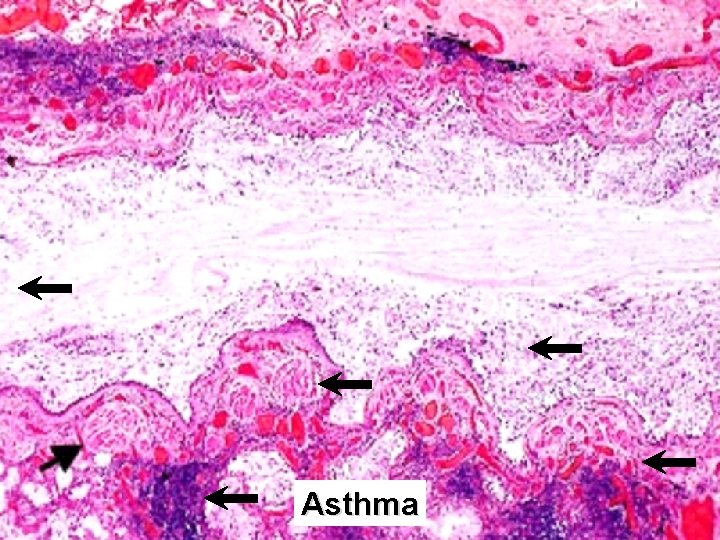
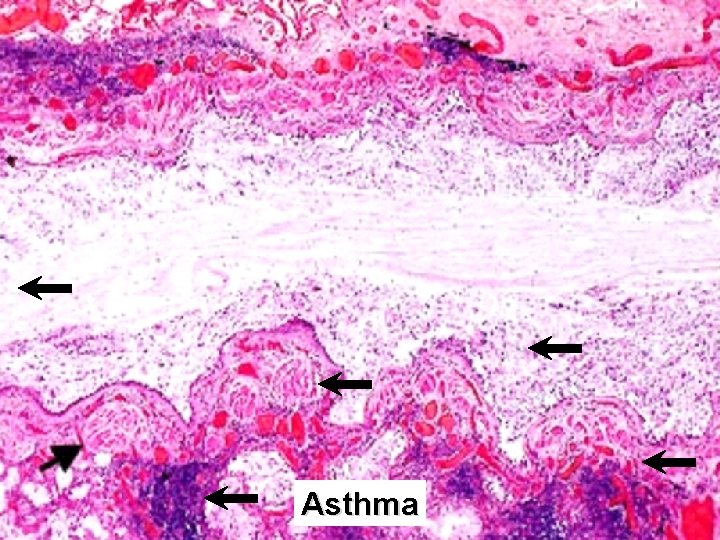
Asthma
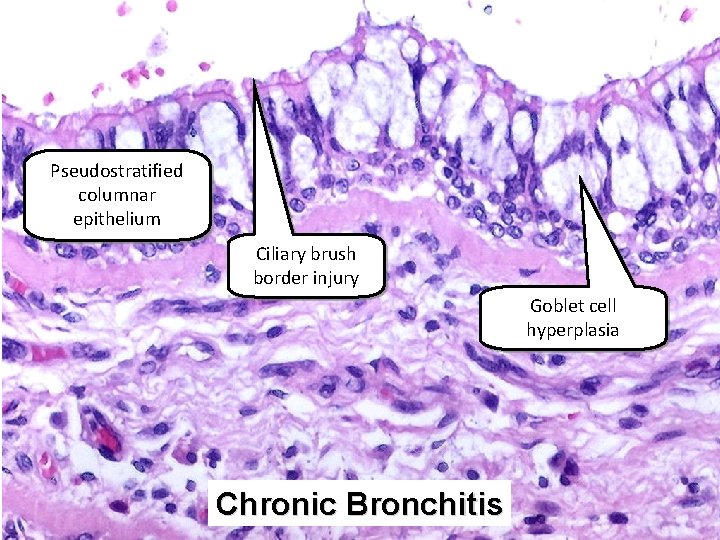
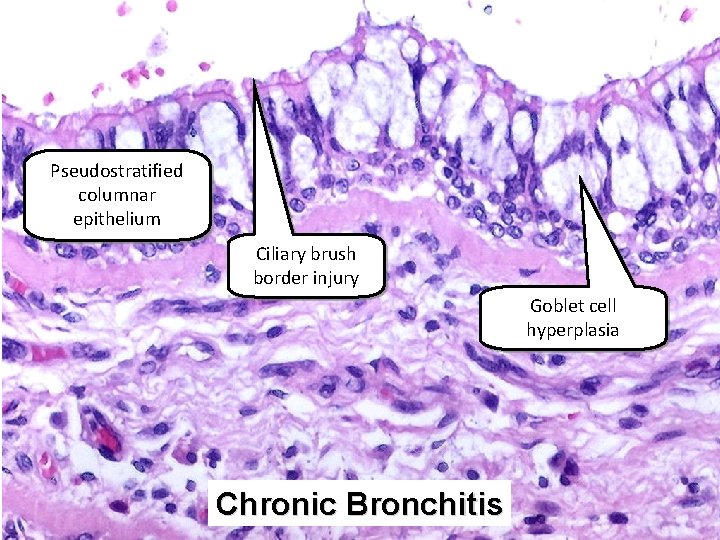
Pseudostratified columnar epithelium Ciliary brush border injury Goblet cell hyperplasia Chronic Bronchitis
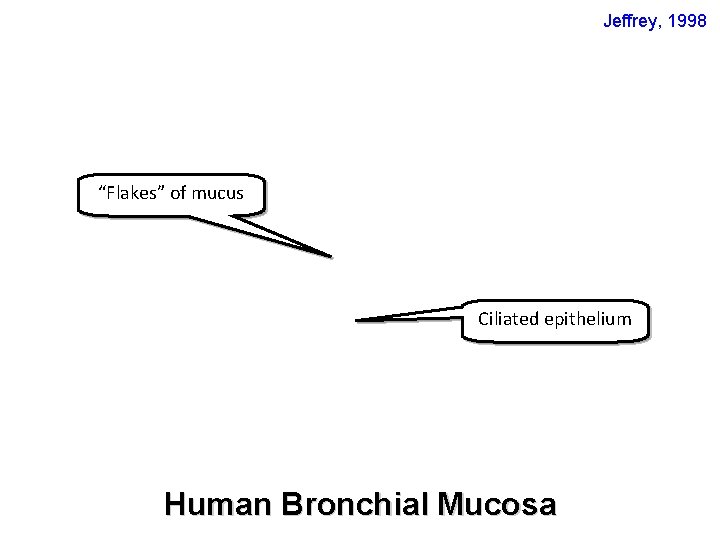
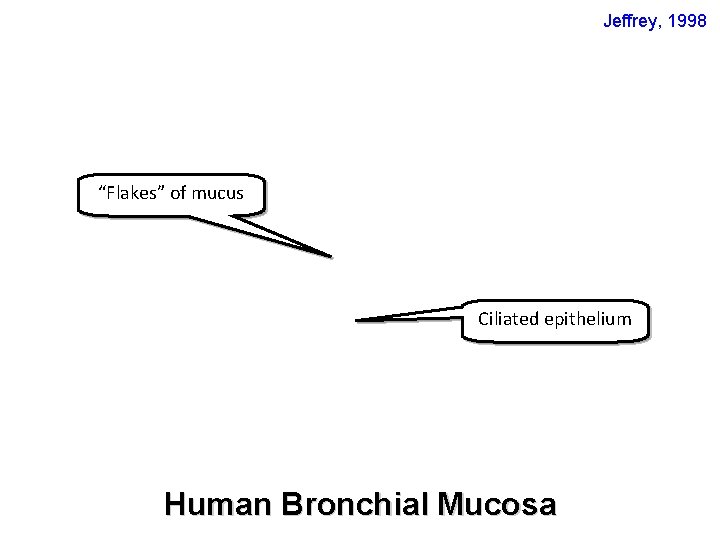
Jeffrey, 1998 “Flakes” of mucus Ciliated epithelium Human Bronchial Mucosa
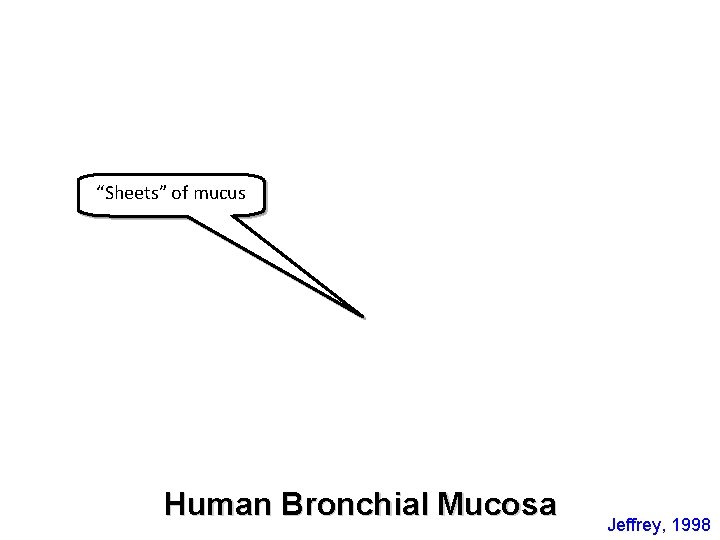
“Sheets” of mucus Human Bronchial Mucosa Jeffrey, 1998
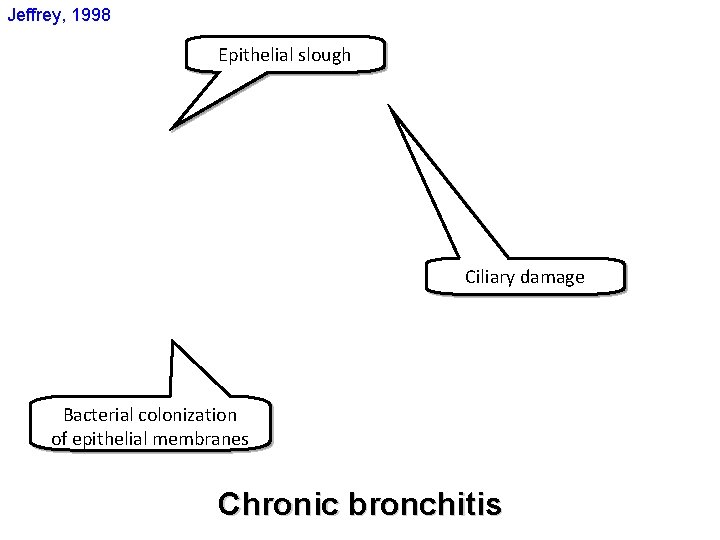
Jeffrey, 1998 Epithelial slough Ciliary damage Bacterial colonization of epithelial membranes Chronic bronchitis
Normal alveoli
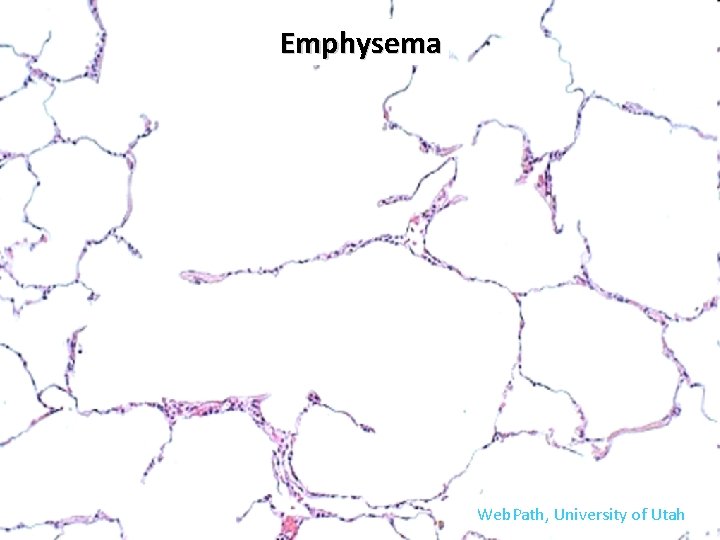
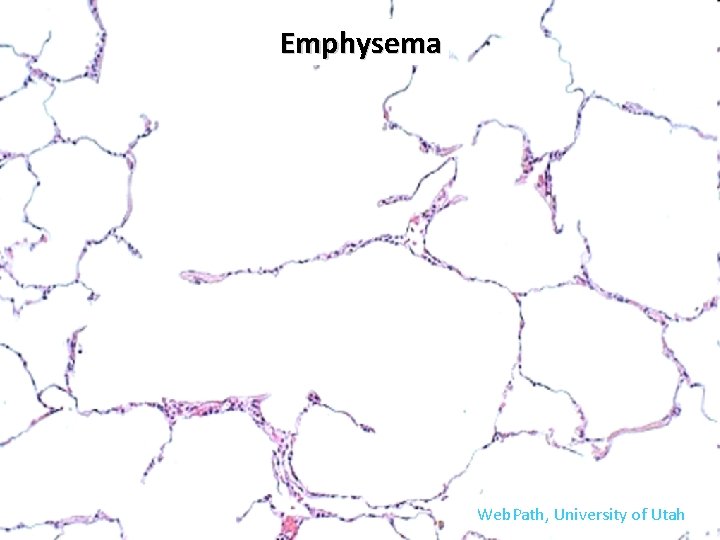
Emphysema Web. Path, University of Utah
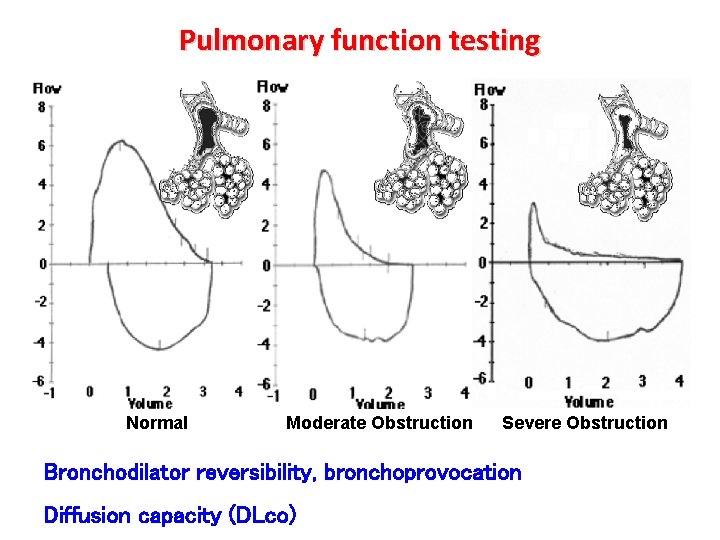
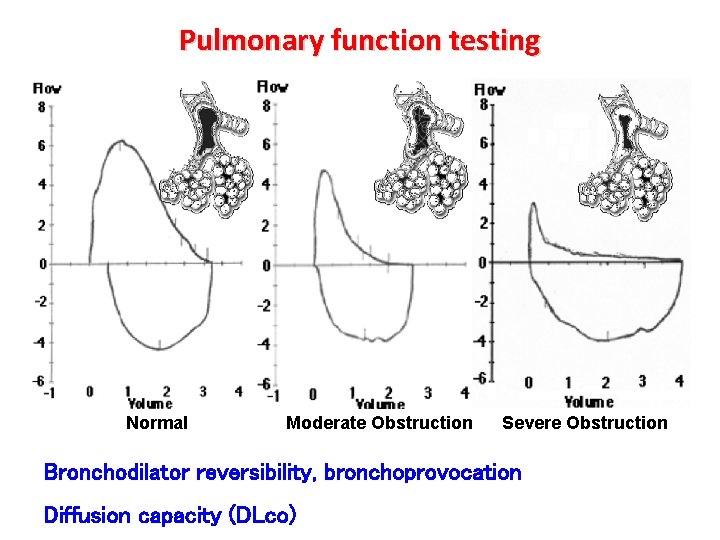
Pulmonary function testing Normal Moderate Obstruction Severe Obstruction Bronchodilator reversibility, bronchoprovocation Diffusion capacity (DLco)
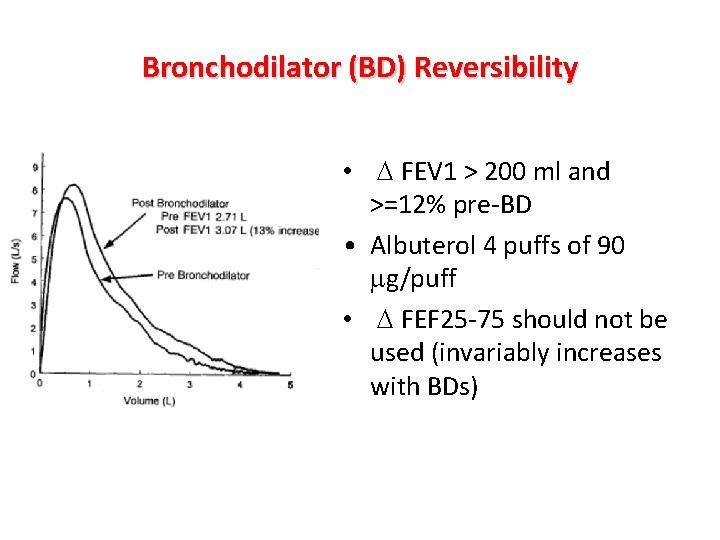
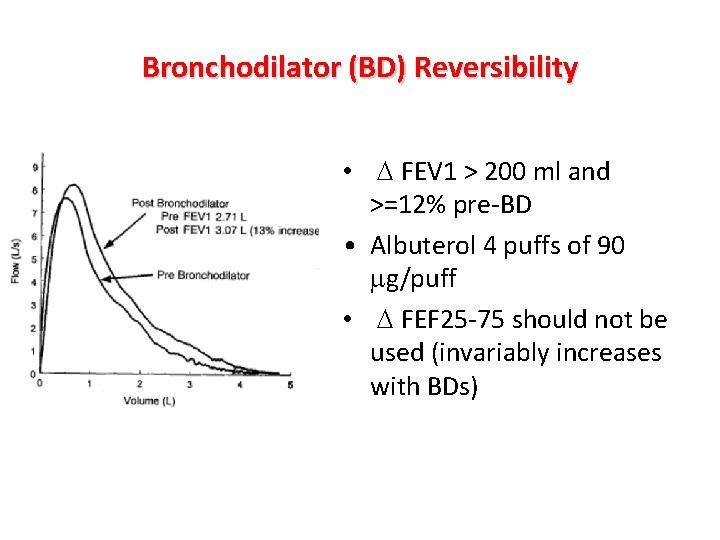
Bronchodilator (BD) Reversibility • D FEV 1 > 200 ml and >=12% pre-BD • Albuterol 4 puffs of 90 mg/puff • D FEF 25 -75 should not be used (invariably increases with BDs)
Bronchoprovocation • Methacholine • Sxs consistent with asthma, but normal spirometry and no BD response • Atypical sxs of bronchospasm (chest tightness, insomnia, cough-variant, etc. ) • Optimal diagnostic value when pretest probability 30 -70% • More useful in excluding diagnosis (negative predictive power is very good)
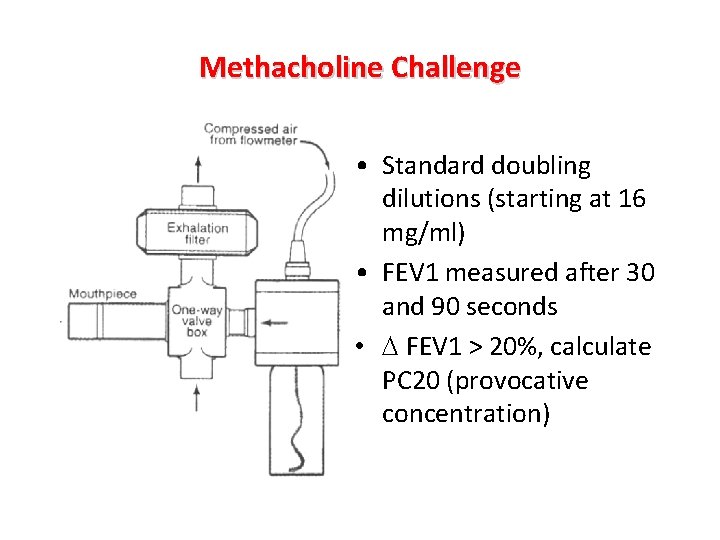
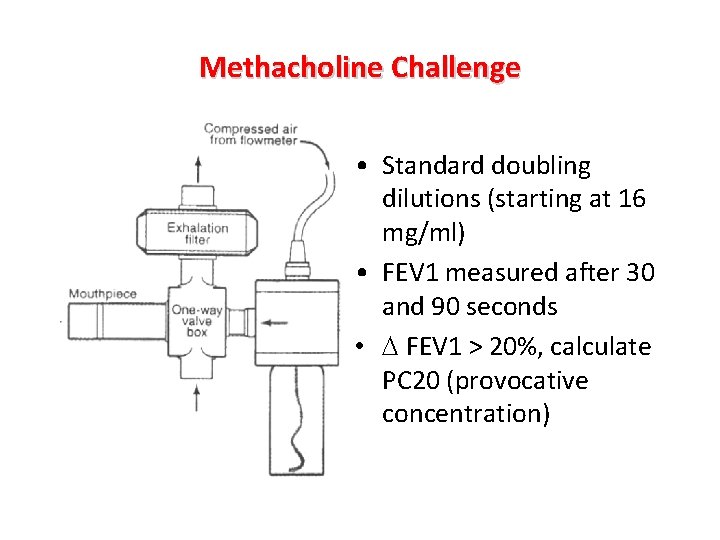
Methacholine Challenge • Standard doubling dilutions (starting at 16 mg/ml) • FEV 1 measured after 30 and 90 seconds • D FEV 1 > 20%, calculate PC 20 (provocative concentration)
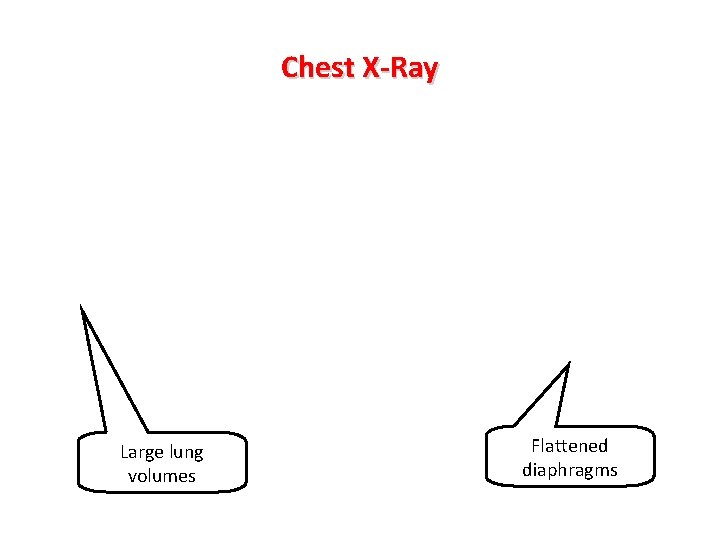
Chest X-Ray Large lung volumes Flattened diaphragms
Emphysema
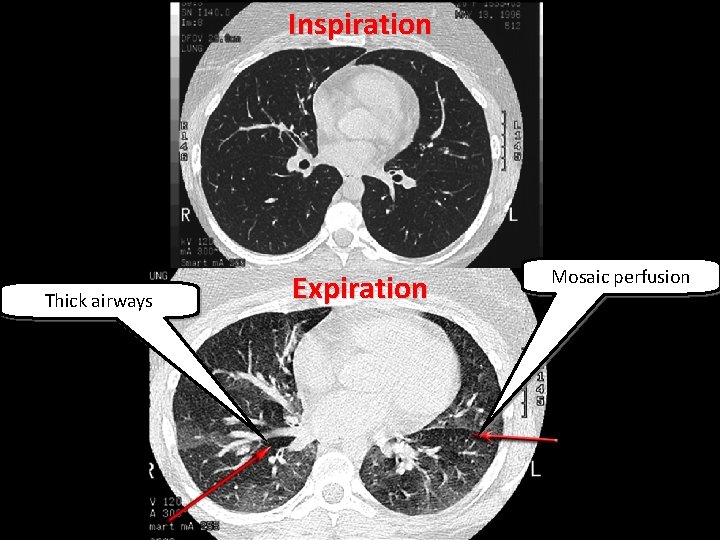
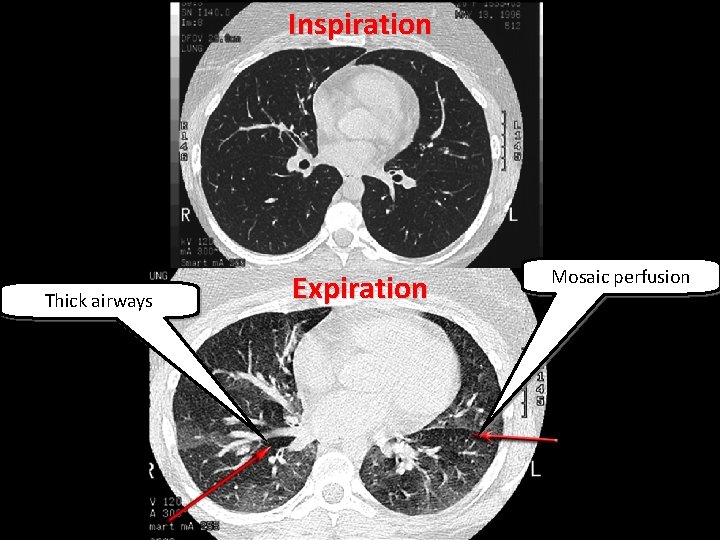
Inspiration Thick airways Expiration Mosaic perfusion
Eosinophils Neutrophils

Clinical Presentation Younger patients Non-smokers Reversible obstruction Triggers for airways hyperresponsiveness Atopy Chronic bronchitis: Cough/secretions Most days 3 mo/year ³ 2 successive years Older patients >40 yo Smokers Irreversible obstruction Progressive Occupational exposures
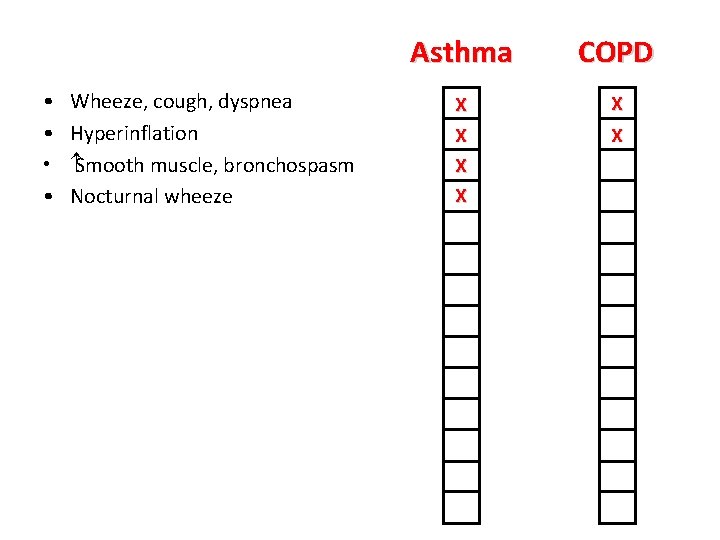
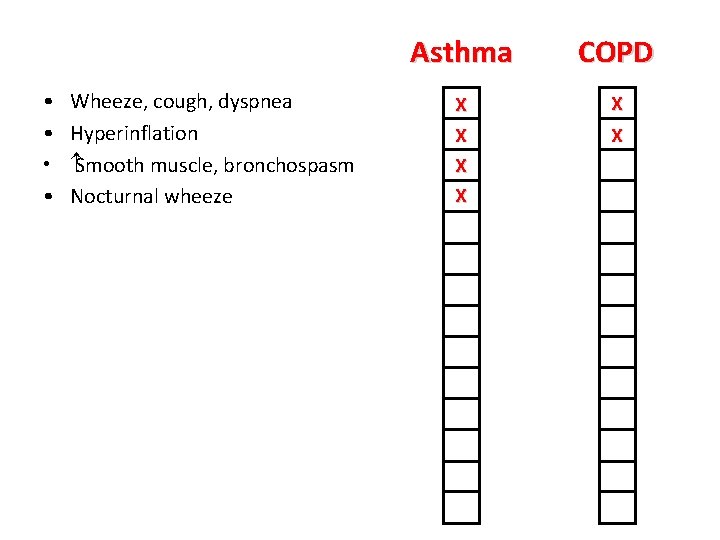
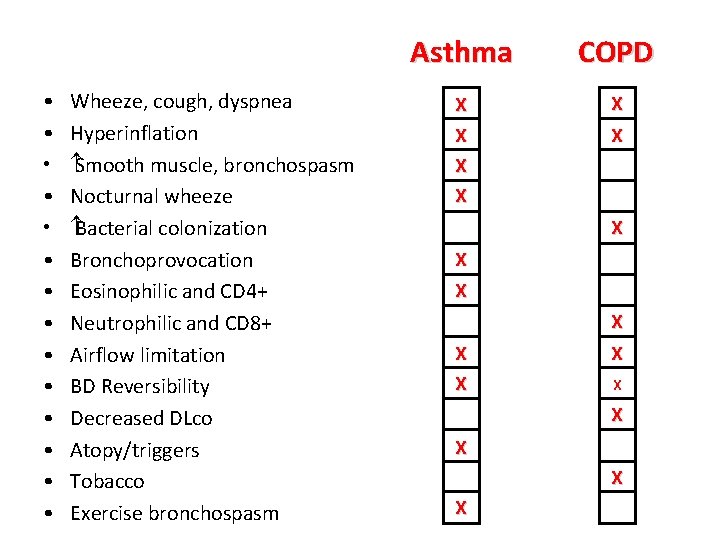
• • Wheeze, cough, dyspnea Hyperinflation Smooth muscle, bronchospasm Nocturnal wheeze Asthma COPD X X X
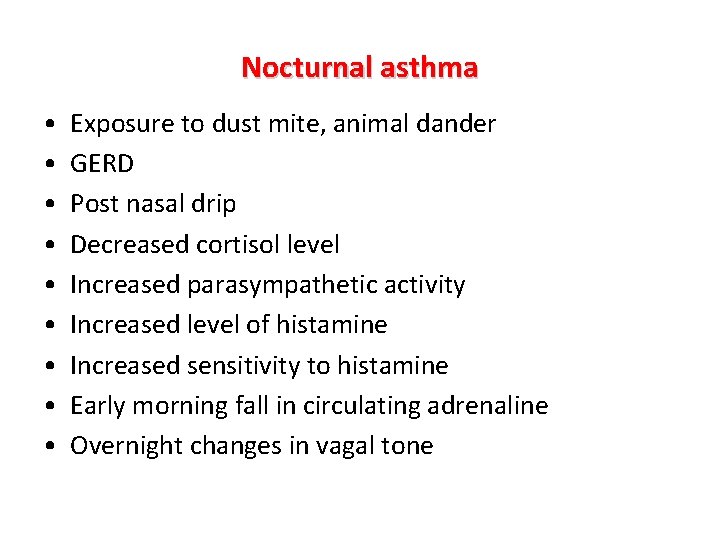
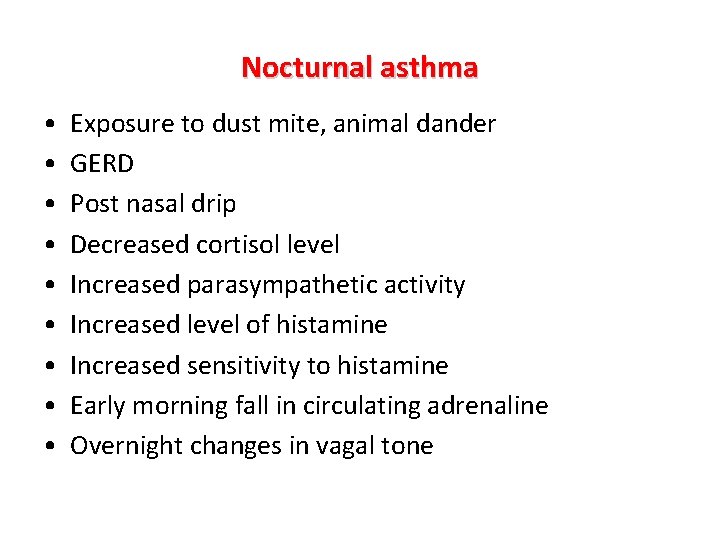
Nocturnal asthma • • • Exposure to dust mite, animal dander GERD Post nasal drip Decreased cortisol level Increased parasympathetic activity Increased level of histamine Increased sensitivity to histamine Early morning fall in circulating adrenaline Overnight changes in vagal tone
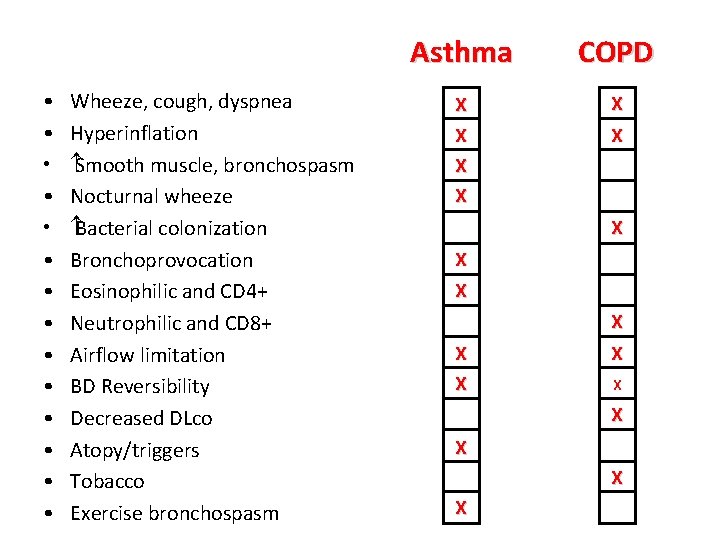
• • • • Wheeze, cough, dyspnea Hyperinflation Smooth muscle, bronchospasm Nocturnal wheeze Bacterial colonization Bronchoprovocation Eosinophilic and CD 4+ Neutrophilic and CD 8+ Airflow limitation BD Reversibility Decreased DLco Atopy/triggers Tobacco Exercise bronchospasm Asthma COPD X X X X X
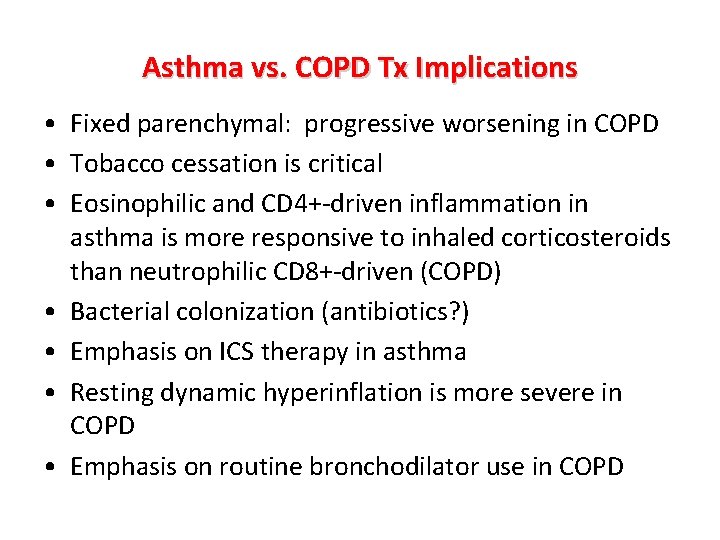
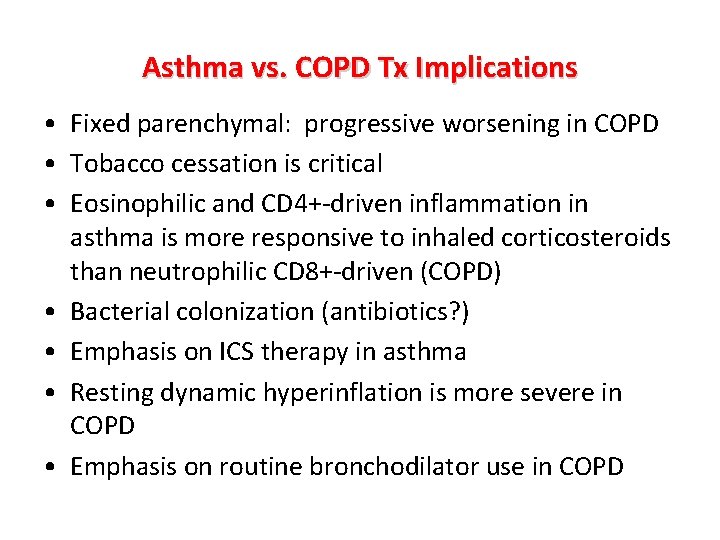
Asthma vs. COPD Tx Implications • Fixed parenchymal: progressive worsening in COPD • Tobacco cessation is critical • Eosinophilic and CD 4+-driven inflammation in asthma is more responsive to inhaled corticosteroids than neutrophilic CD 8+-driven (COPD) • Bacterial colonization (antibiotics? ) • Emphasis on ICS therapy in asthma • Resting dynamic hyperinflation is more severe in COPD • Emphasis on routine bronchodilator use in COPD
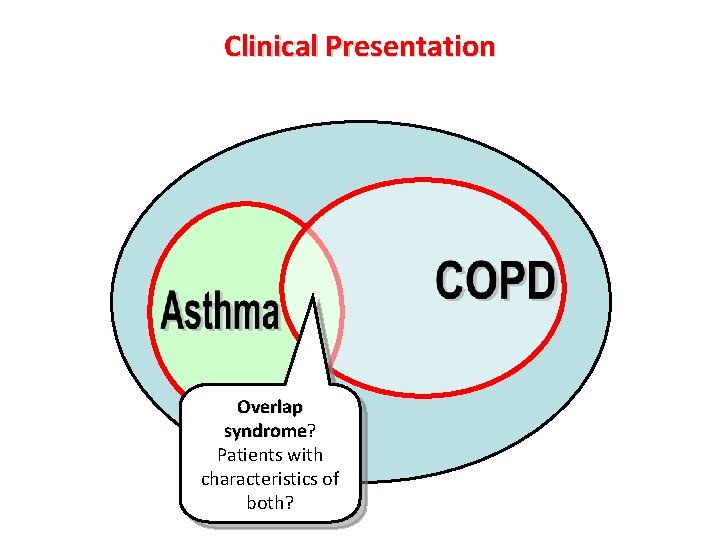
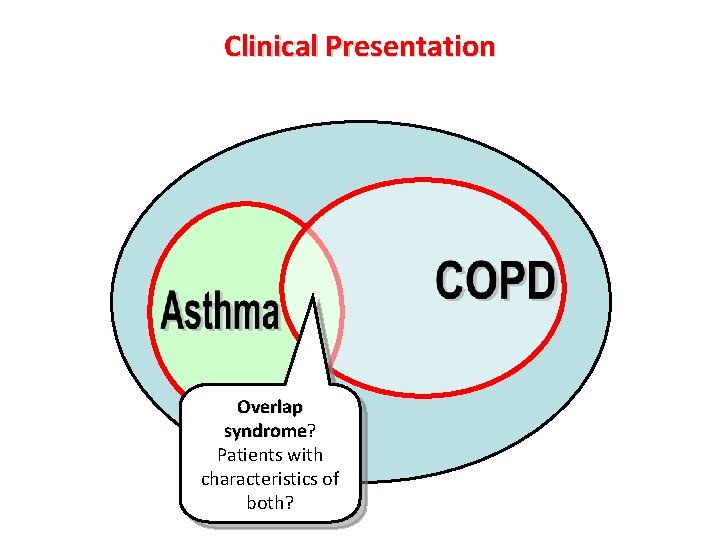
Clinical Presentation Overlap syndrome? syndrome Patients with characteristics of both?
Asthma/COPD “Overlap syndrome” • Exhibits features of both conditions • Incompletely reversible airflow obstruction • +Increased variability of airflow (BD response, increased airways hyperresponsiveness) • Dlco deficit • Worse prognosis 1, higher utilization of resources • These patients are excluded from clinical trials, so results are not generalizable to them • 30% asthmatics are smokers 1. Shaya et al. , 2008
Case 2 • 43 yo F with long standing history of “asthma” • Wheeze and shortness of breath with exercise and stress • Treated with maximum dose ICS • Has received multiple prednisone courses • Presents to you, Cushingoid • Inspiratory wheeze
 Pathology of asthma
Pathology of asthma Asthma diagnosis criteria
Asthma diagnosis criteria Second phase of nursing process
Second phase of nursing process Objectives of nursing process
Objectives of nursing process What are the nursing process
What are the nursing process Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Neonatal jaundice physical examination
Neonatal jaundice physical examination Patellar dislocation
Patellar dislocation Differential diagnosis of molar pregnancy
Differential diagnosis of molar pregnancy Implantation spotting
Implantation spotting Bakers cyst differential diagnosis
Bakers cyst differential diagnosis Diakarbi
Diakarbi Corte axial
Corte axial Kavram çeşitleri
Kavram çeşitleri Differential diagnosis of stroke
Differential diagnosis of stroke Types of gastric ulcer
Types of gastric ulcer Differentials for hydrocephalus
Differentials for hydrocephalus Carpal tunnel syndrome differential diagnosis
Carpal tunnel syndrome differential diagnosis Saw tooth appearance in lichen planus
Saw tooth appearance in lichen planus Myelopathy vs radiculopathy
Myelopathy vs radiculopathy Broadbent sign in constrictive pericarditis
Broadbent sign in constrictive pericarditis What does black tarry stool look like
What does black tarry stool look like Papulovesicular rash differential diagnosis
Papulovesicular rash differential diagnosis Vitamin c differential diagnosis mnemonic
Vitamin c differential diagnosis mnemonic Conjunctivitis differential diagnosis
Conjunctivitis differential diagnosis Fairy skin
Fairy skin Leukocoria differential diagnosis
Leukocoria differential diagnosis Differential diagnosis of articular syndrome
Differential diagnosis of articular syndrome Erythroderma differential diagnosis
Erythroderma differential diagnosis Differential diagnosis of stroke
Differential diagnosis of stroke Differential diagnosis of otitis externa
Differential diagnosis of otitis externa