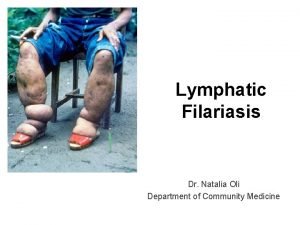
Lymphatic Filariasis Dr Natalia Oli Department of Community

- Slides: 33
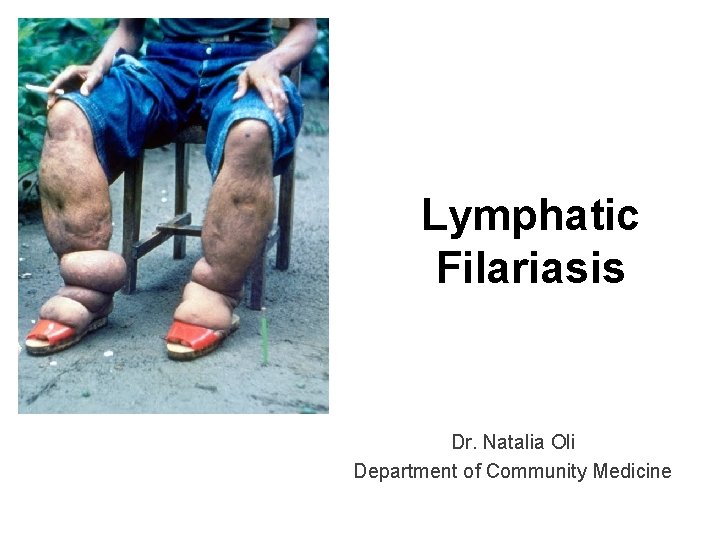
Lymphatic Filariasis Dr. Natalia Oli Department of Community Medicine
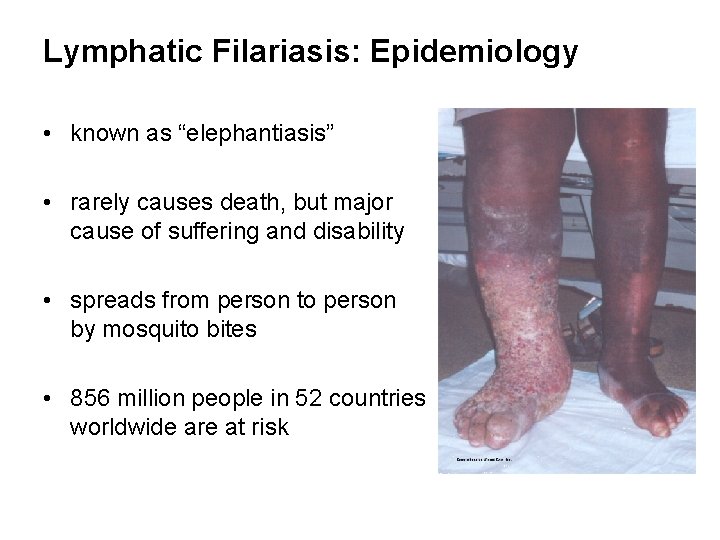
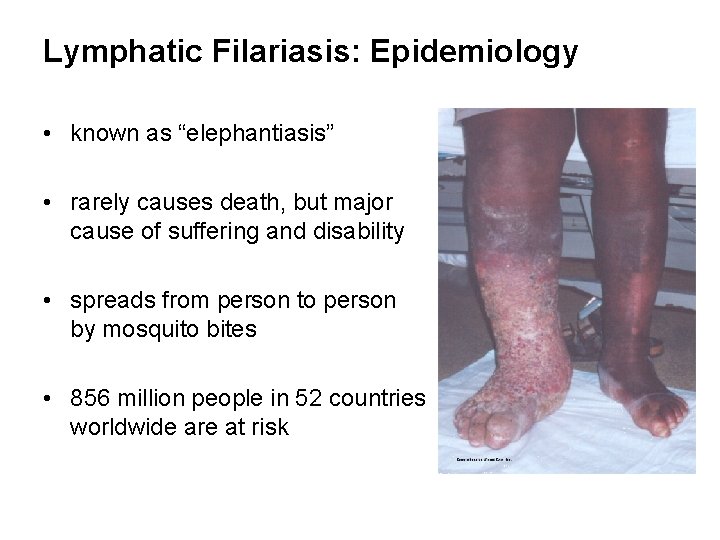
Lymphatic Filariasis: Epidemiology • known as “elephantiasis” • rarely causes death, but major cause of suffering and disability • spreads from person to person by mosquito bites • 856 million people in 52 countries worldwide are at risk
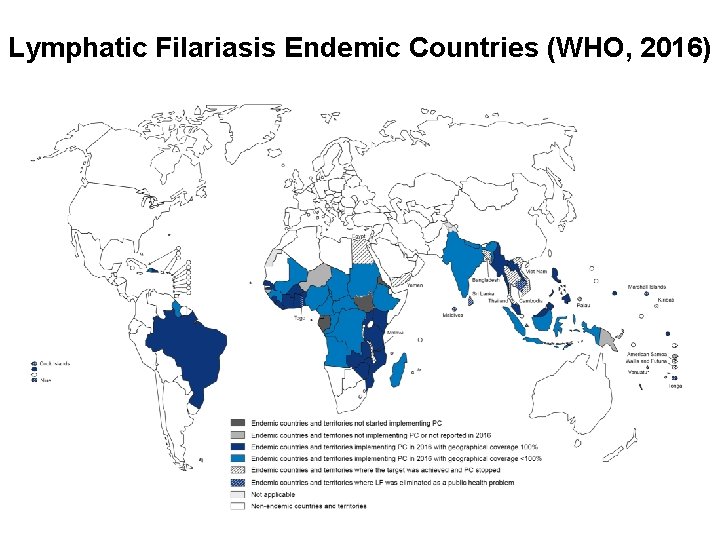
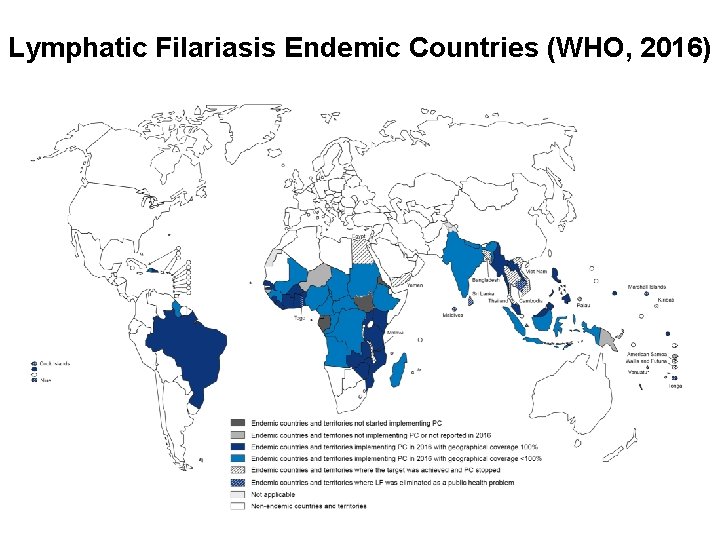
Lymphatic Filariasis Endemic Countries (WHO, 2016)
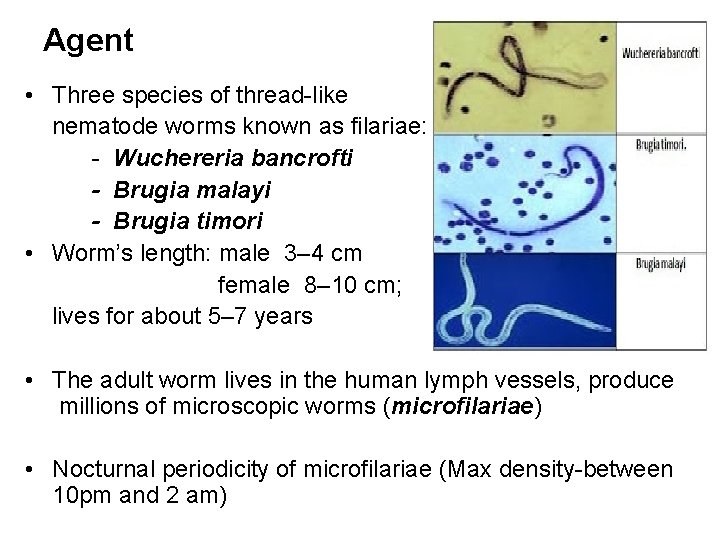
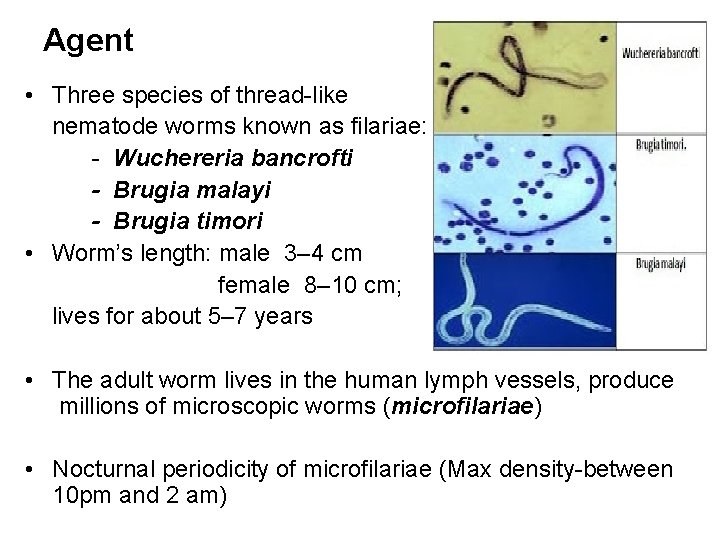
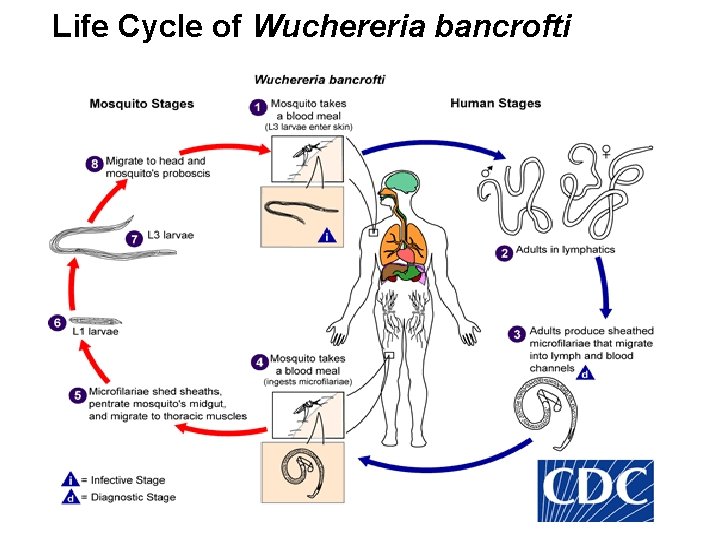
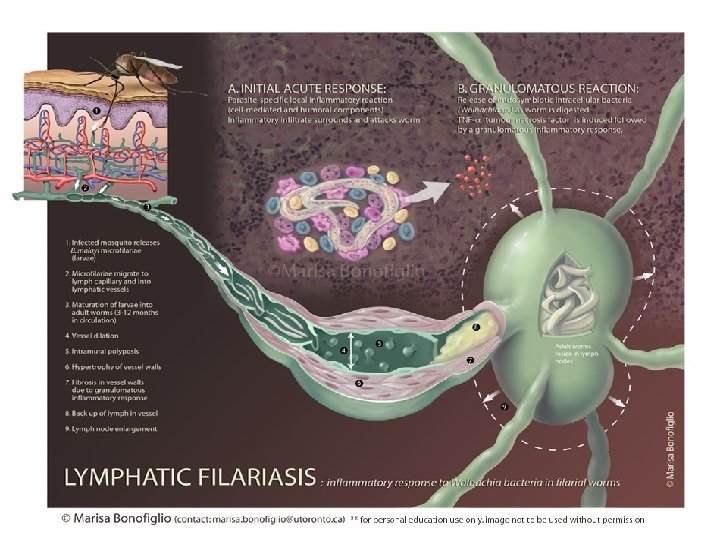
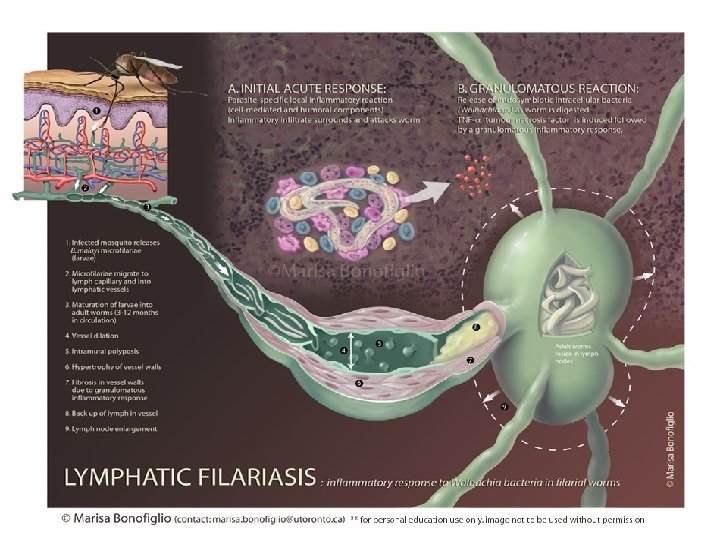
Agent • Three species of thread-like nematode worms known as filariae: - Wuchereria bancrofti - Brugia malayi - Brugia timori • Worm’s length: male 3– 4 cm female 8– 10 cm; lives for about 5– 7 years • The adult worm lives in the human lymph vessels, produce millions of microscopic worms (microfilariae) • Nocturnal periodicity of microfilariae (Max density-between 10 pm and 2 am)
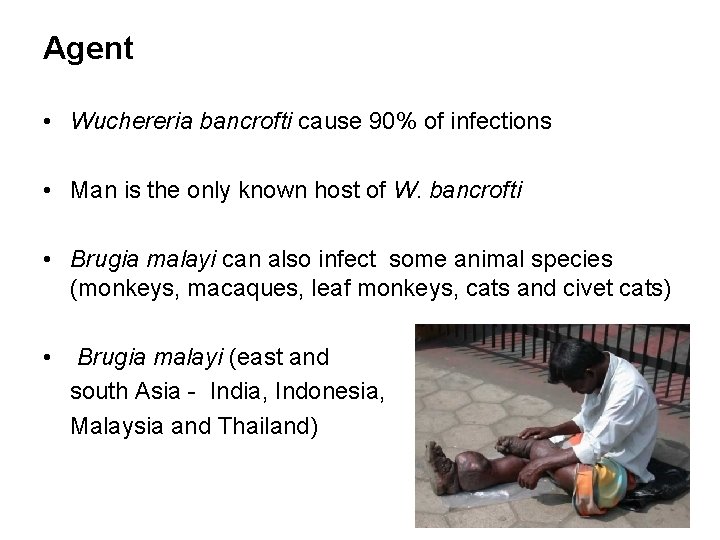
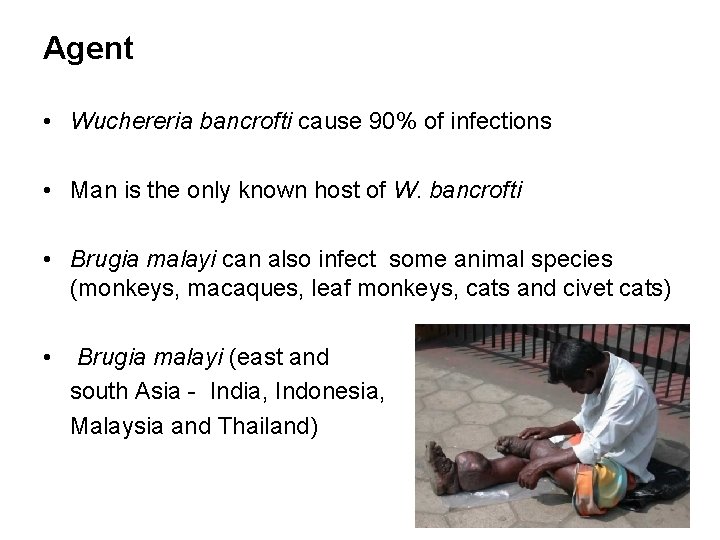
Agent • Wuchereria bancrofti cause 90% of infections • Man is the only known host of W. bancrofti • Brugia malayi can also infect some animal species (monkeys, macaques, leaf monkeys, cats and civet cats) • Brugia malayi (east and south Asia - India, Indonesia, Malaysia and Thailand)
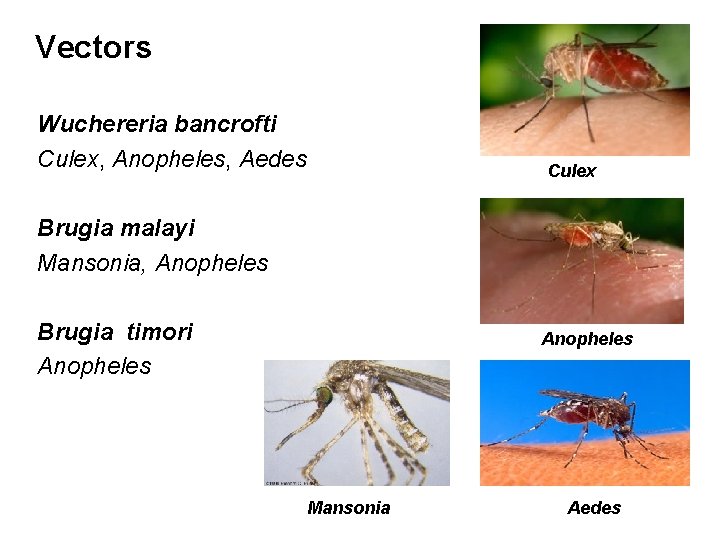
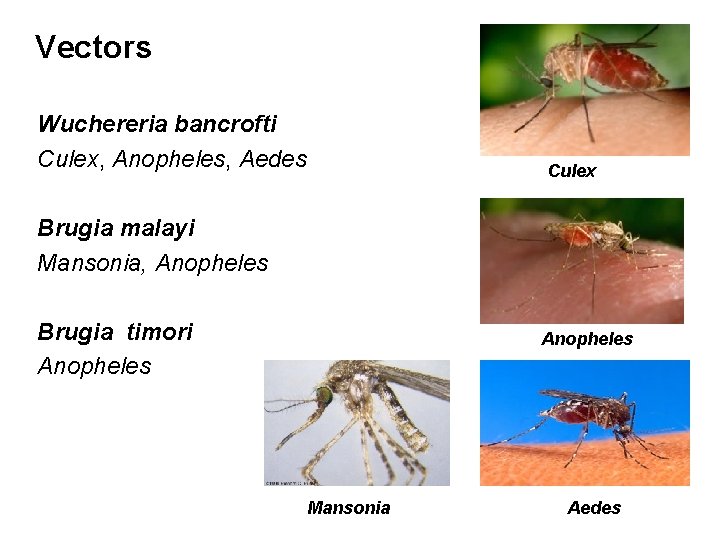
Vectors Wuchereria bancrofti Culex, Anopheles, Aedes Culex Brugia malayi Mansonia, Anopheles Brugia timori Anopheles Mansonia Aedes
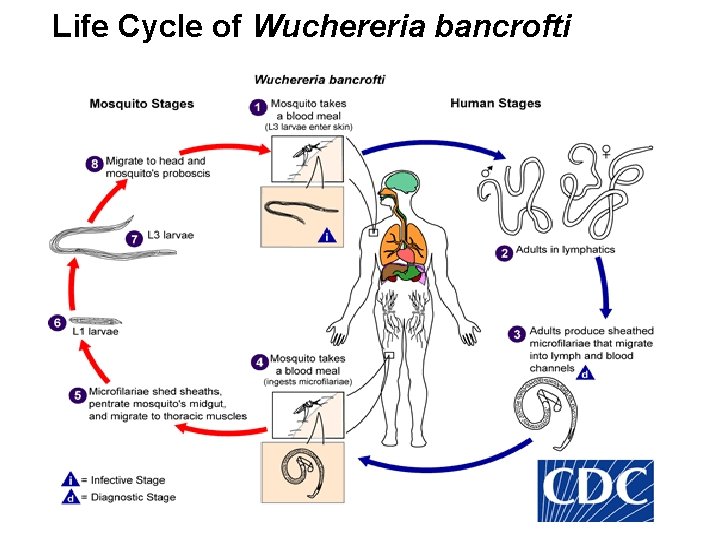
Life Cycle of Wuchereria bancrofti
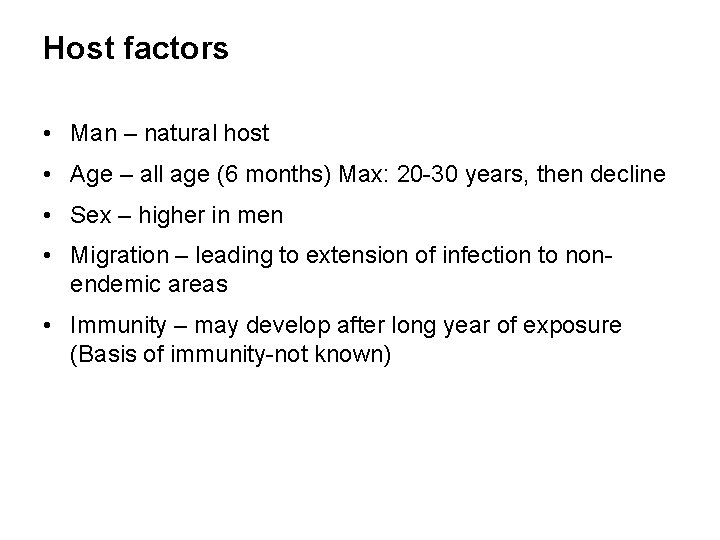
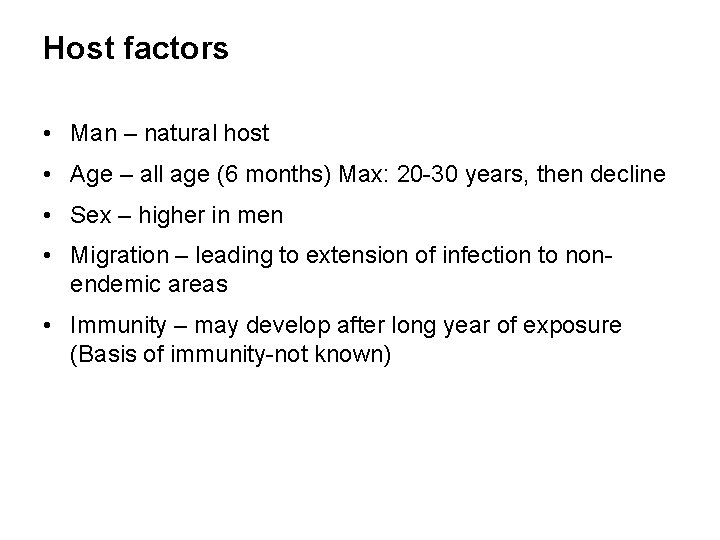
Host factors • Man – natural host • Age – all age (6 months) Max: 20 -30 years, then decline • Sex – higher in men • Migration – leading to extension of infection to nonendemic areas • Immunity – may develop after long year of exposure (Basis of immunity-not known)
Social and Environmental Factors • Climate is an important factor which influences: - The breeding of mosquitoes - Longevity (optimum temperature 20 -300 C and humidity 70%) - The development of parasite in the vector • Associated with urbanization, poverty, industrialization, illiteracy and poor sanitation • Sanitation, town planning, sewage and drainage
Transmission in a community is influenced by: • the number of infected persons (prevalence) • the density of microfilaria in the blood of infected persons • the density of vector mosquitoes • characteristics of the vector that affect development of infective larvae • frequency of human-vector contact
Clinical manifestations 1) Majority of infected people are asymptomatic - have circulating microfilariae - important source of infection - may have subclinical lymphatic damage and as many as 40% have kidney damage, with proteinuria and haematuria 2) Acute: attacks of ‘filarial fever’ - pain and inflammation of lymph nodes and ducts related to bacterial and fungal super infections of the tissue that are already compromised lymphatic function - fever, nausea
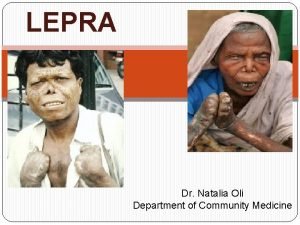
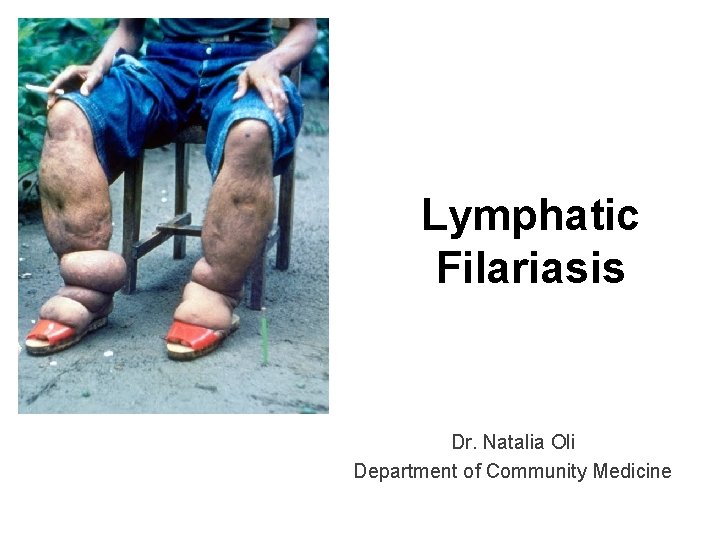
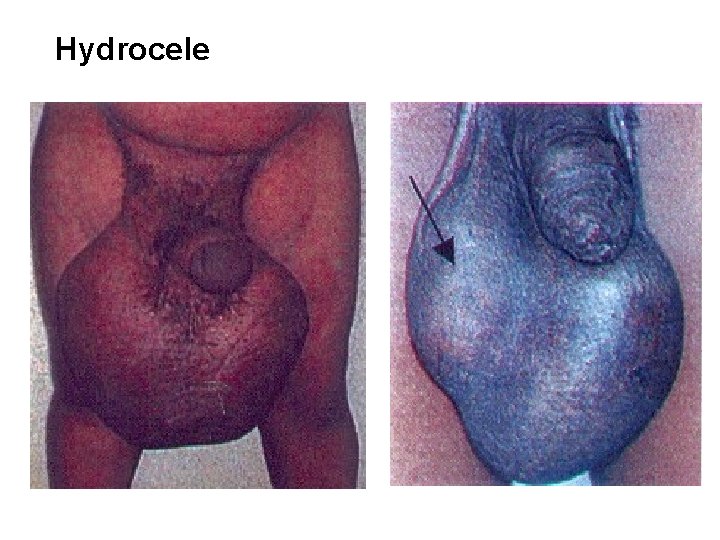
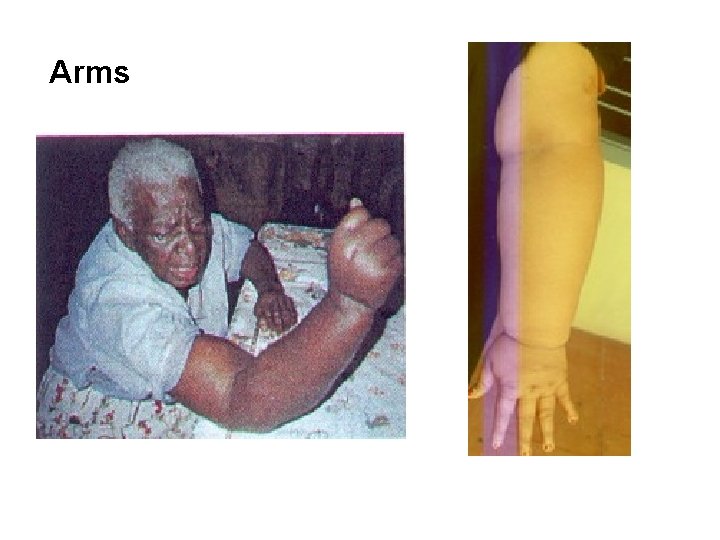
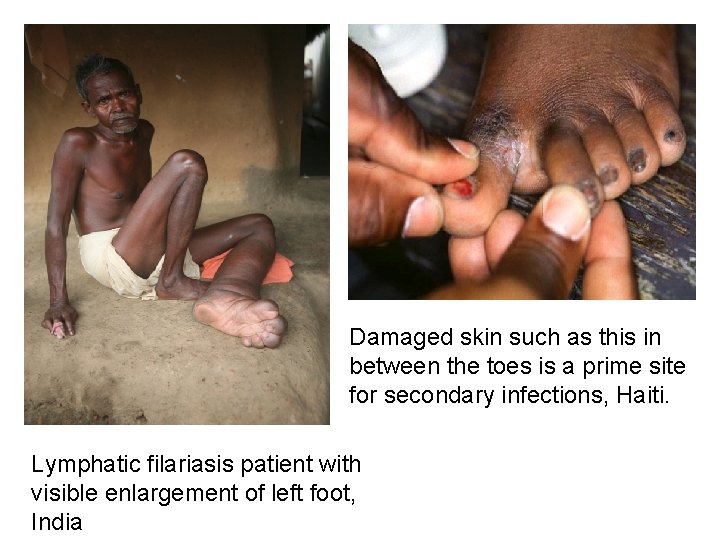
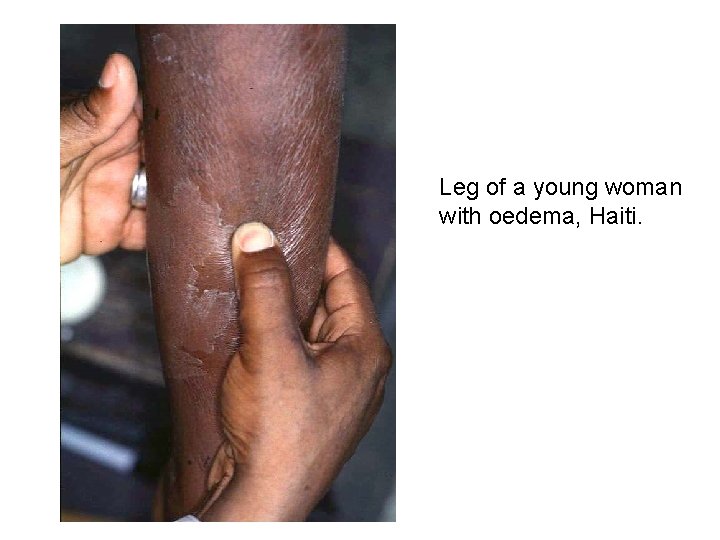
Clinical manifestations 3) Chronic Manifestation: Symptoms (30% of the patients) - lymphoedema of the limbs - hardening and thickening of the skin (elephantiasis) - genital disease (hydrocele, chylocele, and swelling of the scrotum and penis) • recurrent acute attacks, which are extremely painful and are accompanied by fever
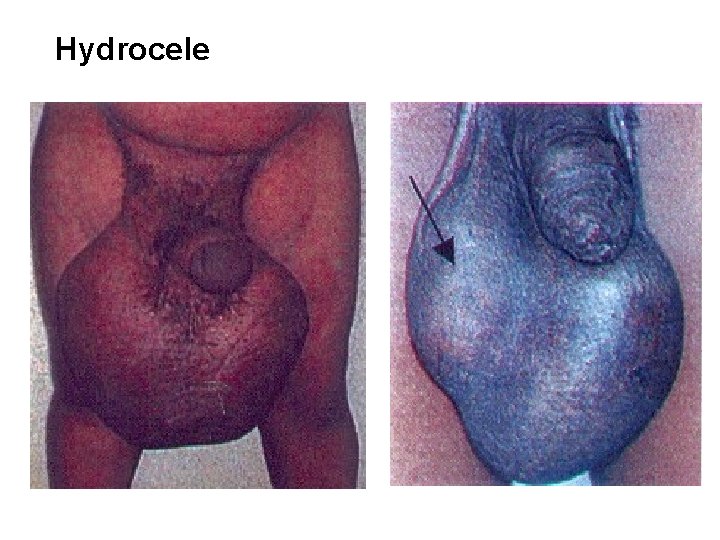
Hydrocele

Legs
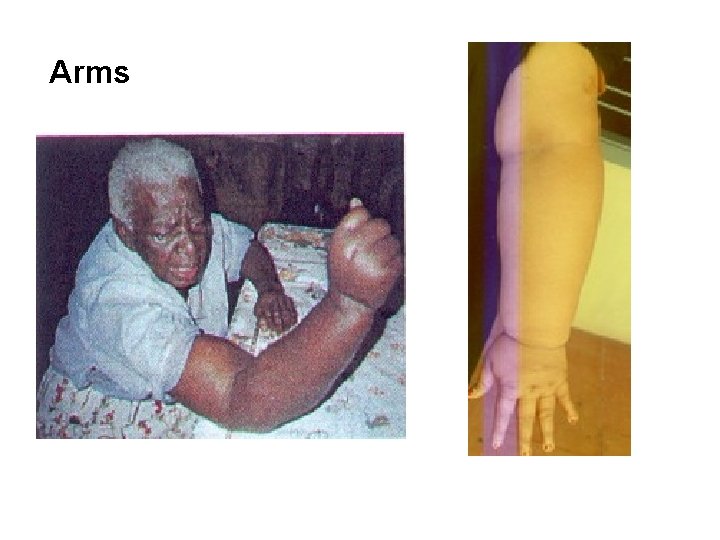
Arms
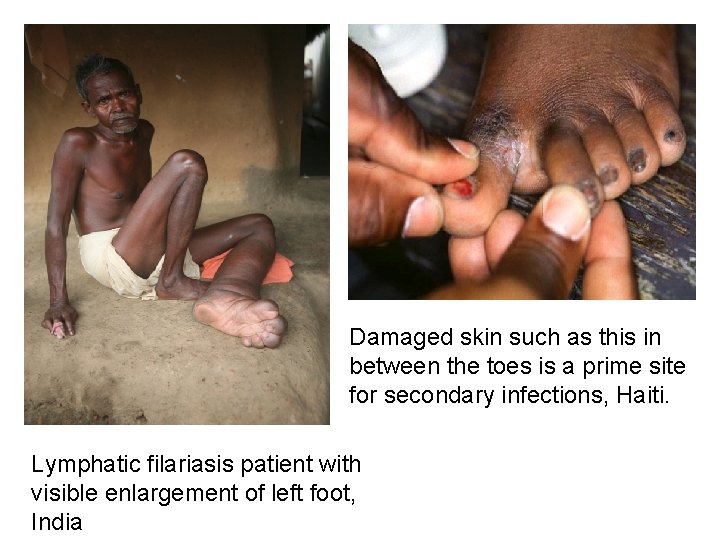
Damaged skin such as this in between the toes is a prime site for secondary infections, Haiti. Lymphatic filariasis patient with visible enlargement of left foot, India
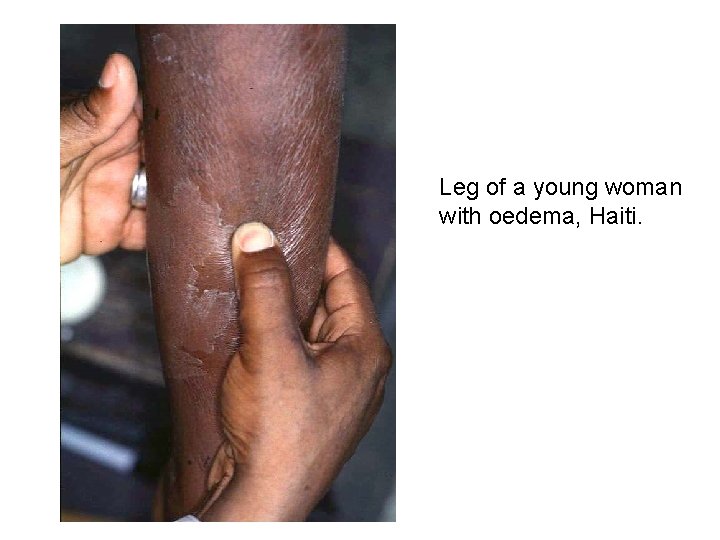
Leg of a young woman with oedema, Haiti.
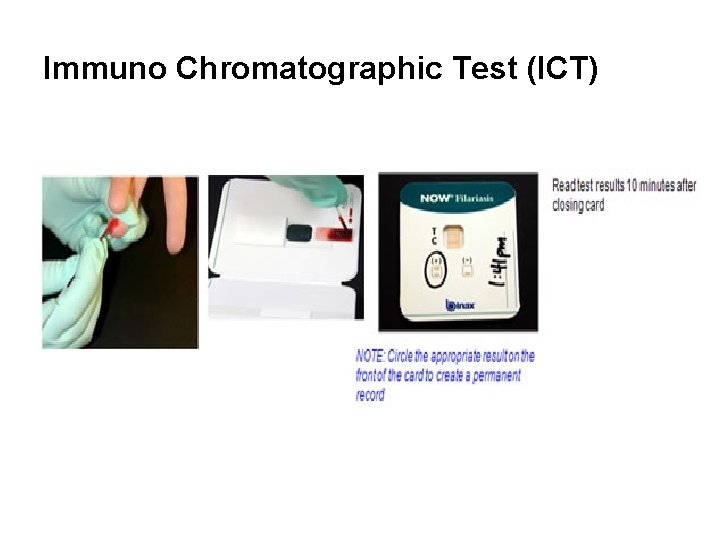
Diagnosis 1. Microscopic examination (microfilarae in the peripheral blood - Thick blood smear): - 2 -3 drops of free flowing blood by finger prick method - specific time, depending on the periodicity of the microfilariae (between 8: 30 pm- 12 mid night) 2. Immuno Chromatographic Test (ICT): Antigen detection by Card test and through ELISA - “Gold Standard” for diagnosing Wuchereria bancrofti infection (high sensitivity and specificity) - 100 μl of finger-prick blood drawn at any time, day or night
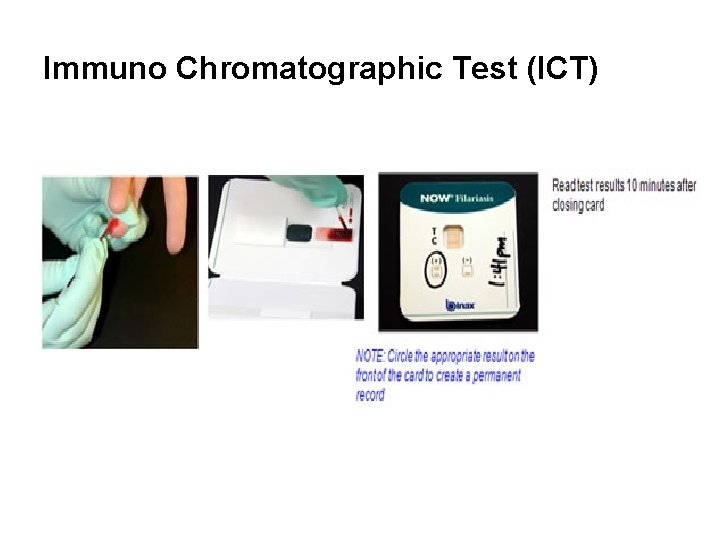
Immuno Chromatographic Test (ICT)
Lymphatic Filariasis Elimination Strategy • Global Programme to Eliminate Lymphatic Filariasis (GPELF) was launched in 2000 - interrupting the transmission cycle - control morbidity (relief of suffering)
Lymphatic Filariasis Elimination Strategy • Mass Drug Administration (MDA) – preventive chemotherapy: - combined dose of 2 medicines given annually to an entire at-risk population in the following way: Albendazole (400 mg) Diethylcarbamazine citrate (DEC) (6 mg/kg) - at least 5 rounds are recommended in the community to stop transmission
Lymphatic Filariasis Elimination Strategy • Vector Control - reducing the mosquito density and preventing humanmosquito contact : Indoor residual spraying long-lasting insecticidal nets environmental approach
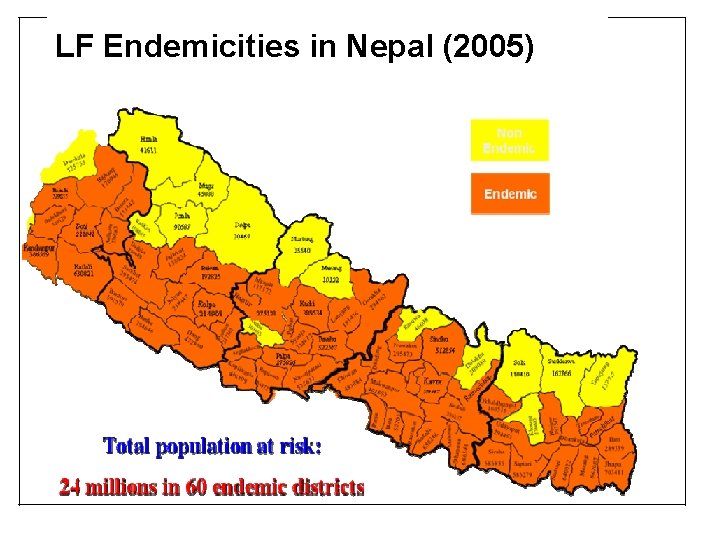
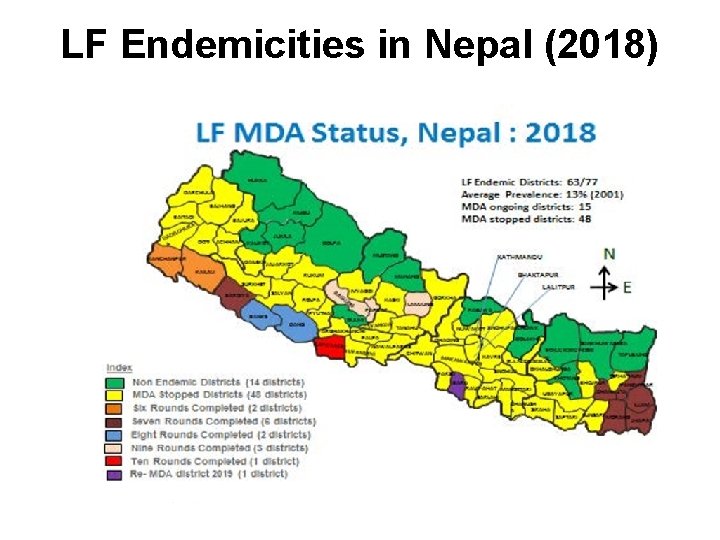
Situation in Nepal • Agent - Wuchereria bancrofti (only recorded parasite in Nepal) • Vector - The mosquito, Culex quinquefasciatus • 13% average prevalence of LF infection in the country, ranging from <1% to 39% • Nepal conducted LF mapping in 2001 and 2005 (Immunochromatography Test card), remapping - 2012 61 districts were mapped as endemic for LF • More LF cases are seen in the Terai than in the Hills
National Plan of Action (2003‐ 2020 AD) for the Elimination of Lymphatic Filariasis • Epidemiology and Disease Control Division under the Department of Health Services Goal: People of Nepal no longer suffer from LF Objectives: • To eliminate LF as a public health problem by 2020 • To interrupt the transmission of Lymphatic Filariasis • To reduce and prevent morbidity • To provide de‐worming benefit through use of Albendazole to endemic community especially to the children • To reduce mosquito vectors
National Plan of Action (2003‐ 2020 AD) for the Elimination of Lymphatic Filariasis Target: • To scale up MDA to all LF endemic districts by 2014 • To achieve <1% prevalence (microfilaraemia rate) in all endemic districts after 6 years of MDA by 2018
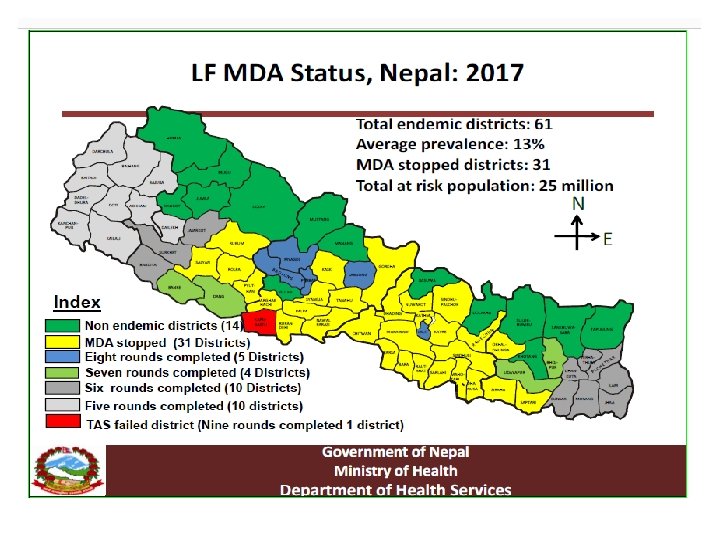
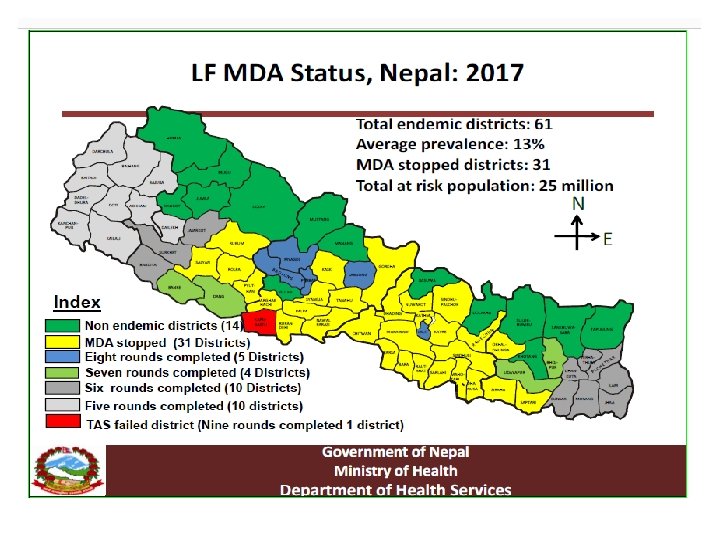
Lymphatic Filariasis: national major activities Mass Drug Administration (MDA) • Was started in Parsa district in 2003 • Gradually scaled up to all endemic districts achieving 100% geographical coverage by 2013 • MDA has been stopped (phased out) in 20 districts ( post MDA surveillance initiated in 5 districts) by 2015 year • All endemic districts completed the recommended six rounds of MDA by 2018.
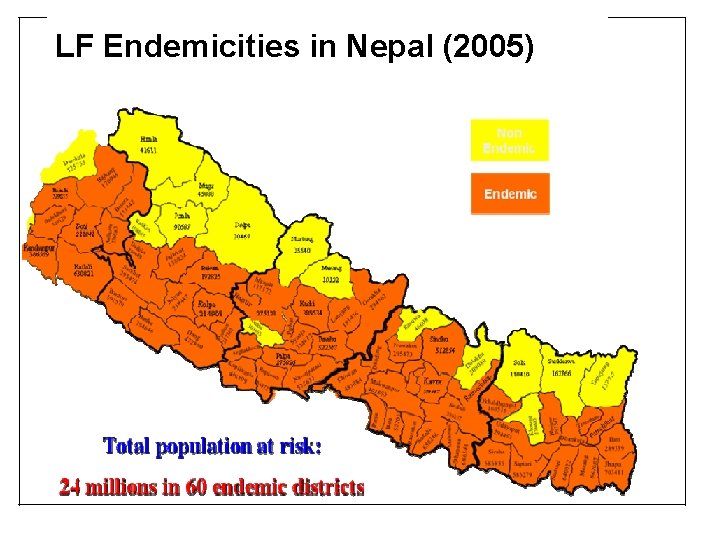
LF Endemicities in Nepal (2005)
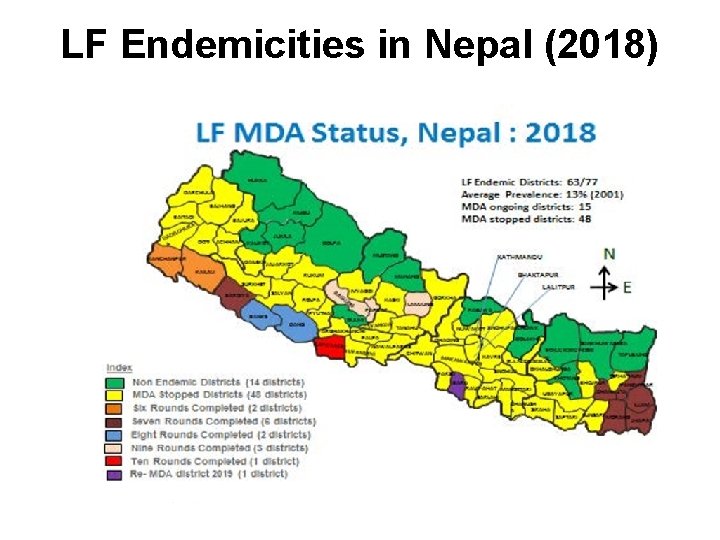
LF Endemicities in Nepal (2018)
Lymphatic Filariasis: national major activities Morbidity management and disability prevention • To reduce suffering in infected people living with chronic and morbid conditions including elephantiasis, lymphedema and hydrocele • Has been initiated in selected districts and high endemic areas • Includes home-based self-care by people living with lymphedema and elephantiasis, hospital based management and surgical corrections of hydroceles
Lymphatic Filariasis: national major activities Post MDA surveillance • is ongoing in MDA stopped (phased out) districts • The monitoring of microfilaria in human populations was by collecting night blood samples and performing smear examination for lymphatic filariasis microfilaria • No or low infections in MDA stopped districts
Challenges and ways forward The major challenges that remain: • To consolidate the achievements (ensuring quality MDA including achieving high coverage in urban areas and some specific communities) • Sustaining low prevalence in MDA phased out districts • Expanding morbidity management and disability prevention, and post MDA surveillance • The biggest challenge is the persistent high prevalence in some districts despite completing the recommended rounds of MDA.
 Filariasis
Filariasis Grading of oedema
Grading of oedema Fujita-hu.ac.jp
Fujita-hu.ac.jp Filariasis cronica
Filariasis cronica Filariasis
Filariasis Filariasis treatment
Filariasis treatment Suomen esihistoria
Suomen esihistoria Nk oli
Nk oli Oli paradigması
Oli paradigması Kolmivuoroviljely
Kolmivuoroviljely Butufu
Butufu Moral padam
Moral padam Padam oli
Padam oli Suma wieku ani i oli wynosi 22 lata
Suma wieku ani i oli wynosi 22 lata Examples of inverted commas
Examples of inverted commas Kekkonen poikkeuslaki
Kekkonen poikkeuslaki Paradigme oli
Paradigme oli Kehonkieli oli ympyrä suuri tai pieni
Kehonkieli oli ympyrä suuri tai pieni Oli systems, inc.
Oli systems, inc. Nyc youth and community development
Nyc youth and community development Georgia department of community health
Georgia department of community health Community action cycle for community mobilization
Community action cycle for community mobilization Contoh aitem
Contoh aitem The cyclist natalia goncharova
The cyclist natalia goncharova Natalia humphreys
Natalia humphreys Natalia konradus
Natalia konradus Natalia ada
Natalia ada św natalia atrybuty
św natalia atrybuty Natalia galindo xxx
Natalia galindo xxx Natália bánesová
Natália bánesová Natalia rimas
Natalia rimas Natalia castro
Natalia castro Natalia sierzputowska wiek
Natalia sierzputowska wiek Natalia laverde
Natalia laverde