Epidemiology of Filariasis Epidemiology of Filariasis Magnitude of






- Slides: 39
Epidemiology of Filariasis
Epidemiology of Filariasis ØMagnitude of the problem ØLife cycle: Agent & Vector ØClinical features ØDiagnosis ØTreatment
introduction Ø Caused by the nematode worm either Wuchereria bancrofti or Brugia malayi Ø Transmission: Culex quinquefasciatus & Mansonia annulifera/uniformis Ø Lymphatic system is affected Ø The disease manifests often in bizarre swelling of legs and hydrocele Ø A great deal of social stigma
introduction • A major public health problem in India • Recorded in “Susruta Samhita” • Clarke called elephantoid legs in Cochin as Malabar legs
filariasis Ø Lymphatic filariasis ü Wuchereria bancrofti, ü Brugia malayi ü Brugia timori Ø Lymphatic filariasis ü O. Volvulus ü M. Ozzardi etc
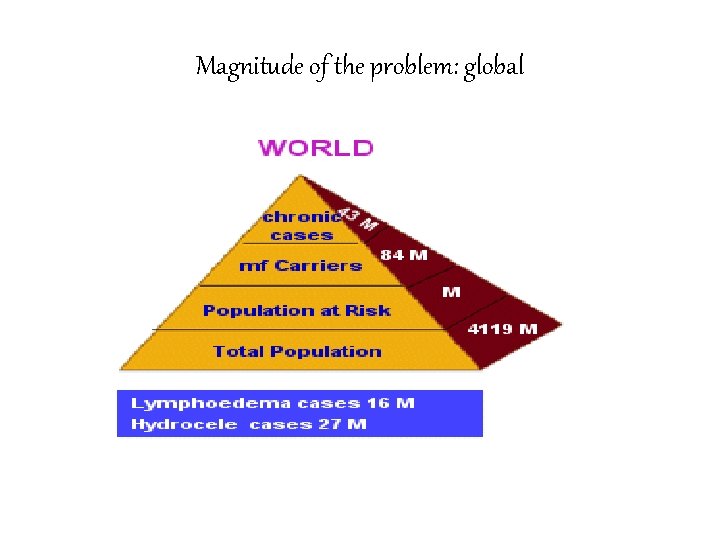
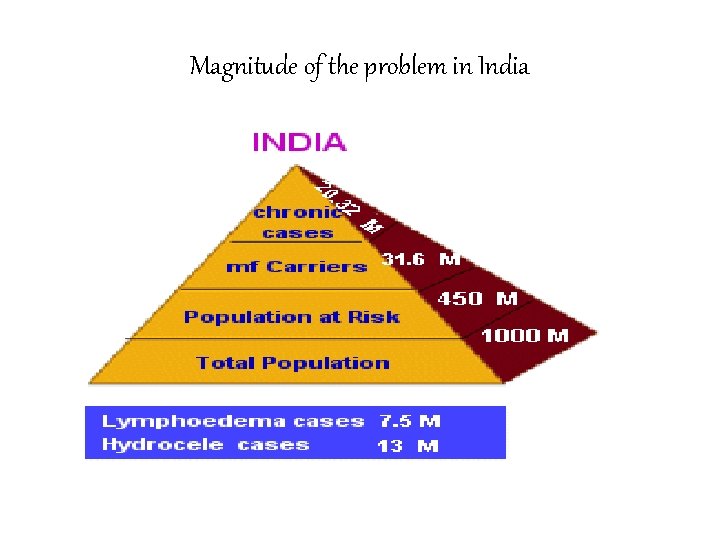
Magnitude of the problem: global Ø A major cause of clinical suffering, disability and handicap Ø Approximately 18% of the world's population — live in areas at risk of infection with lymphatic filarial parasites Ø Approximately one third of those at risk live in India, one third in Africa
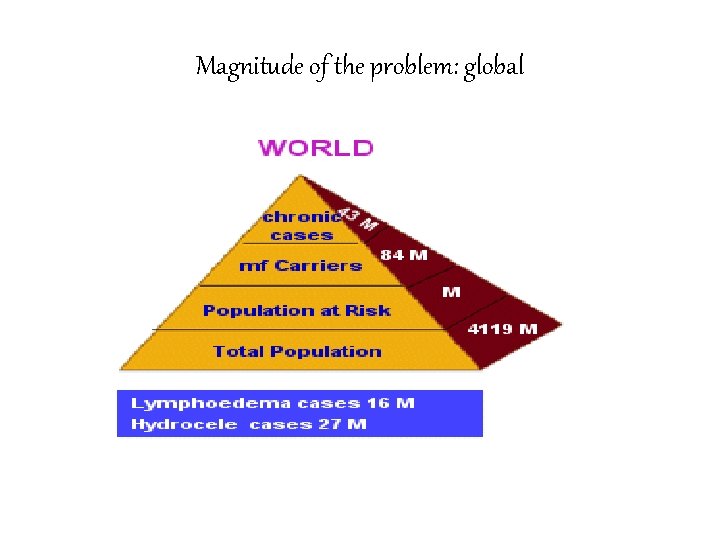
Magnitude of the problem: global
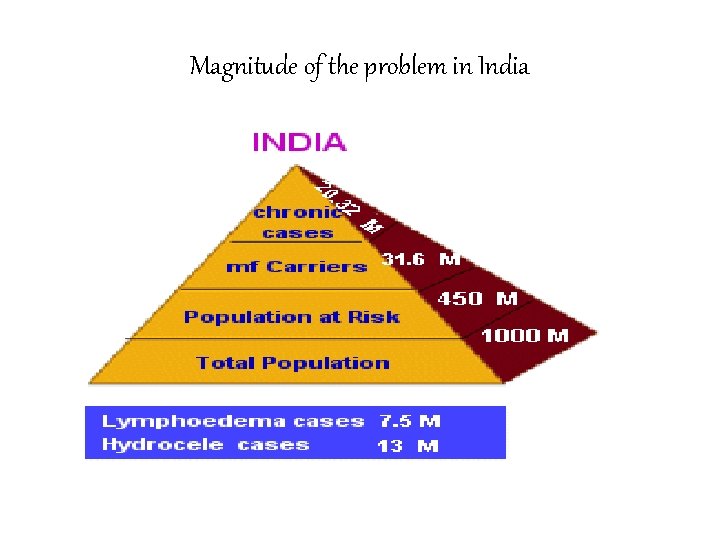
Magnitude of the problem in India


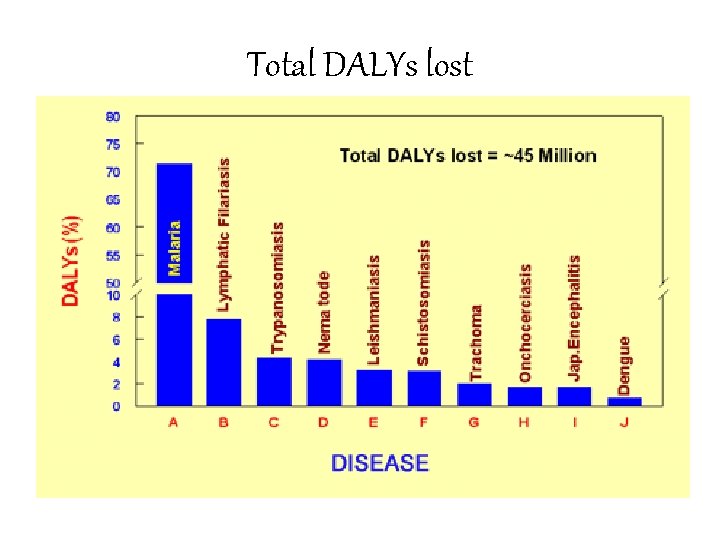
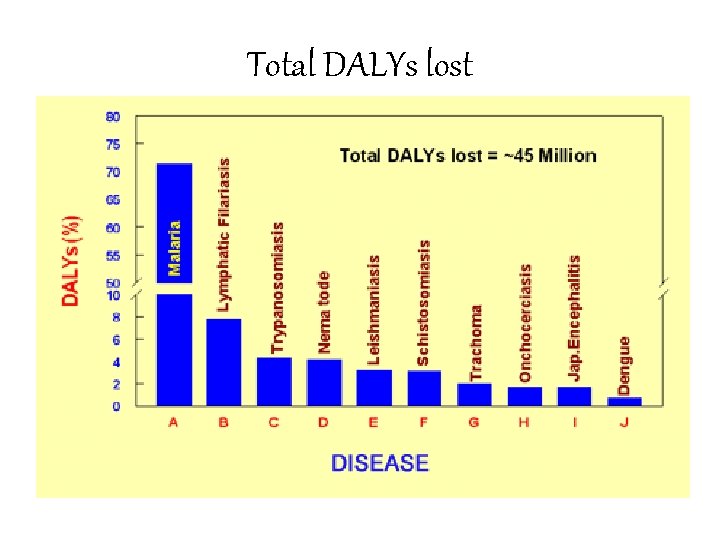
Total DALYs lost
Socio - economic burden Ø Second leading cause of disability in the world. Ø Causes stigma, isolation, psychological stress and family discord among the affected individuals Ø Impairs educational and employment opportunities Ø Impedes domestic and occupational activities
Socio-economic burden Ø A male chronic patient on average losses as many as 69 working days/annum Ø The treatment costs incurred by patients range from RS 1 to 1000 per episode an Ø India loses also 1. 2 billion man days due to LF
Epidemiology of Filariasis ØMagnitude of the problem ØLife cycle: Agent & Vector ØClinical features ØDiagnosis ØTreatment

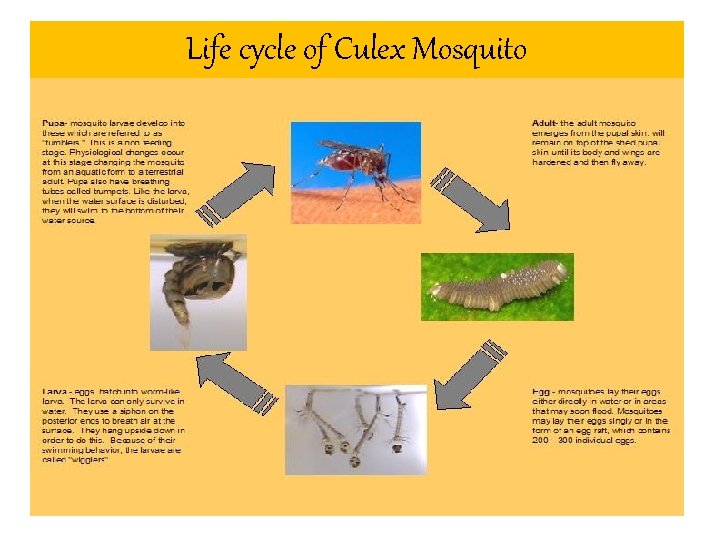
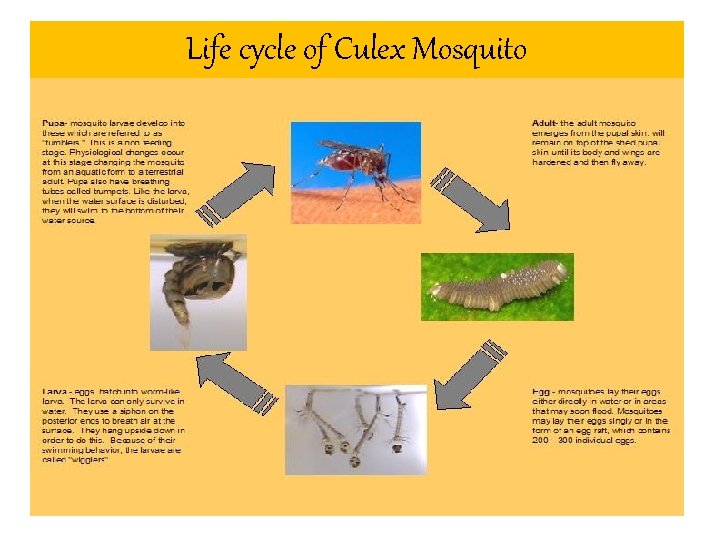
Life cycle of Culex Mosquito
About the vectors • W. bancrofti : Culex mosquitoes in most urban and semi-urban areas • Anopheles in the more rural areas of Africa and • Aedes species in many of the endemic Pacific islands.
The vector Ø Brugian parasites : Mansonia species serve as the major vector Ø Brugian parasites are confined to areas of east and south Asia, especially China, India, Indonesia, Malaysia and the Philippines.
Epidemiology of Filariasis ØMagnitude of the problem ØLife cycle: Agent & Vector ØClinical features ØDiagnosis ØTreatment
Clinical features Ø Asymptomatic microfilarimia Ø Acute manifestations Ø Chronic obstructive lesions Ø Occult filariasis: Tropical Pulmonary eosinophilia
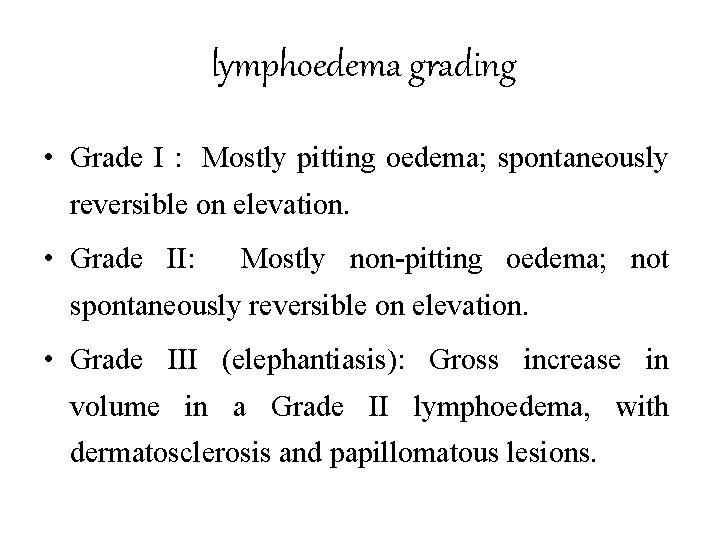
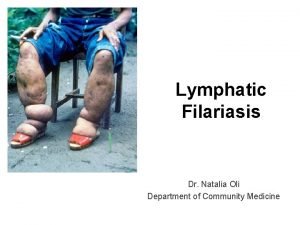
lymphoedema grading • Grade I : Mostly pitting oedema; spontaneously reversible on elevation. • Grade II: Mostly non-pitting oedema; not spontaneously reversible on elevation. • Grade III (elephantiasis): Gross increase in volume in a Grade II lymphoedema, with dermatosclerosis and papillomatous lesions.

elephantiasis

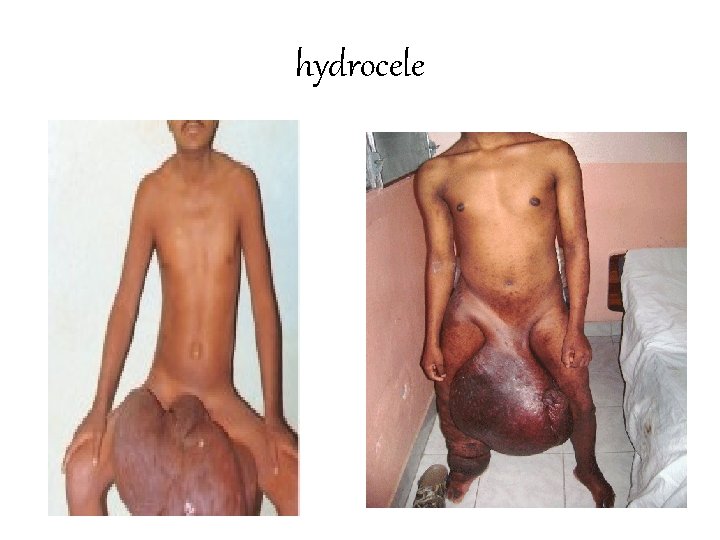
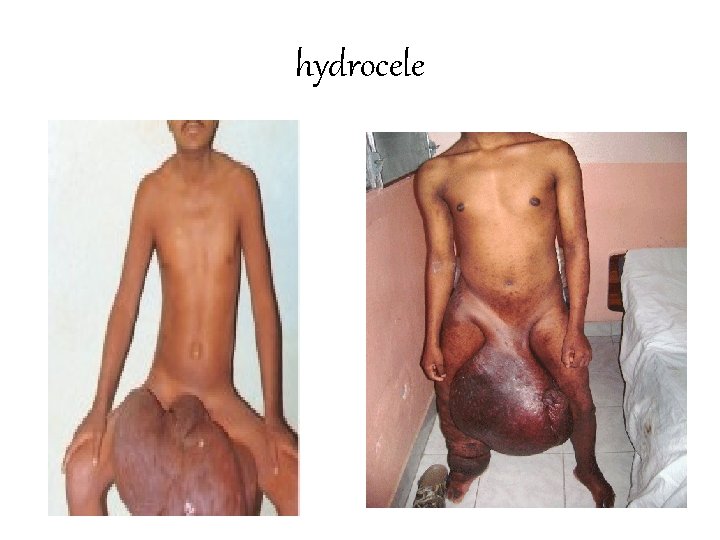
hydrocele
Bancroftian filariasis Ø Lymphatic vessels of the male genitalia are most commonly affected Ø Episodic funiculitis (inflammation of the spermatic cord) epididymitis and orchitis Ø Hydrocele is the most common sign of chronic bancroftian filariasis, followed by lymphoedema & elephantiasis
Brugian filariasis Ø Lymphadenitis: one inguinal lymph node at a time Ø Lymphangitis Ø The infected lymph node may become an abscess, ulcerate, and heal with fibrotic scarring Ø Characteristically, elephantiasis involves the leg below the knee but occasionally it affects the arm below the elbow
Epidemiology of Filariasis ØMagnitude of the problem ØLife cycle: Agent & Vector ØClinical features ØDiagnosis ØTreatment
Laboratory Diagnosis Ø Examining night blood collected by finger pricking Ø Og 4 C 3 ELISA Assay Ø ICT Card Test Ø Polycarbonate membrane filtration Test Ø Other tests Ø Serological techniques Indirect immuno fluorescent assay with mf and adult worm. Ø DNA based diagnostic tests
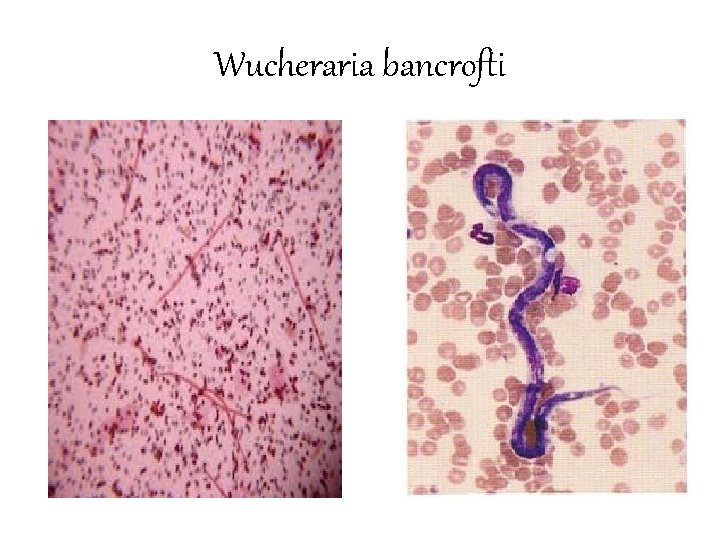
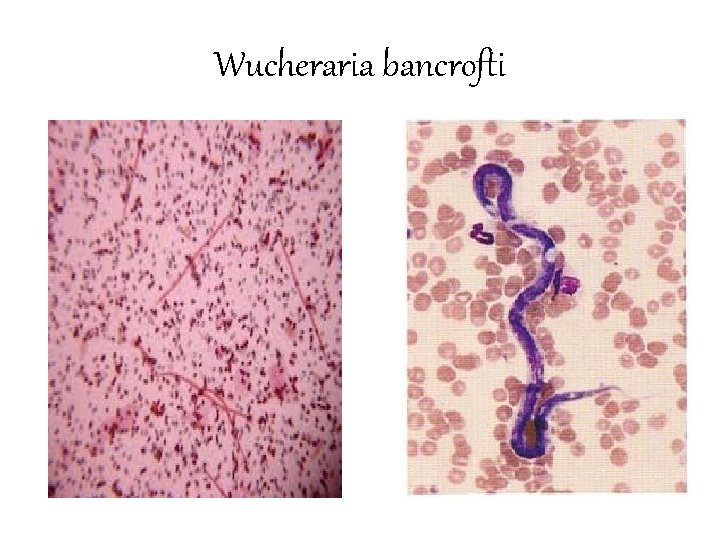
Wucheraria bancrofti
Epidemiology of Filariasis ØMagnitude of the problem ØLife cycle: Agent & Vector ØClinical features ØDiagnosis ØTreatment
Case treatment Ø Diethylcarbamazine (DEC): 6 mg/kg üFor 12 days over 2 weeks üToxic reactions Ø Ivermectin : 400 micro gm/kg single dose
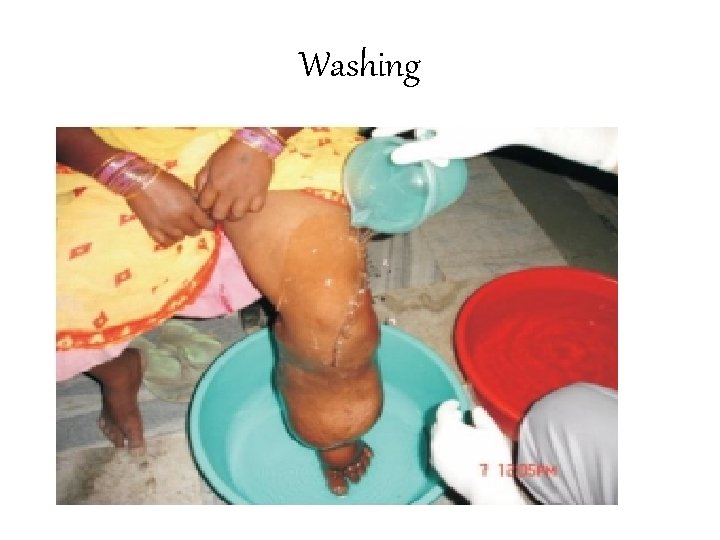
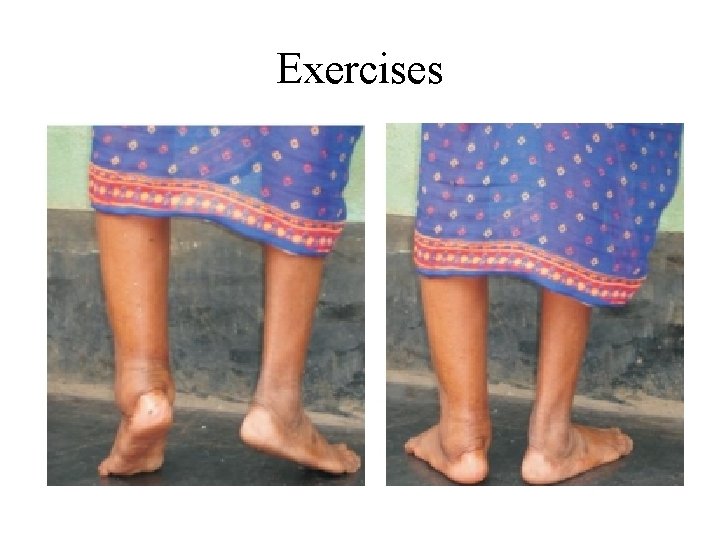
lymphoedema management Ø Washing Ø Prevention and cure of entry lesions Ø Elevation of the foot Ø Exercise Ø Wearing proper footwear Ø Hydrocelectomy
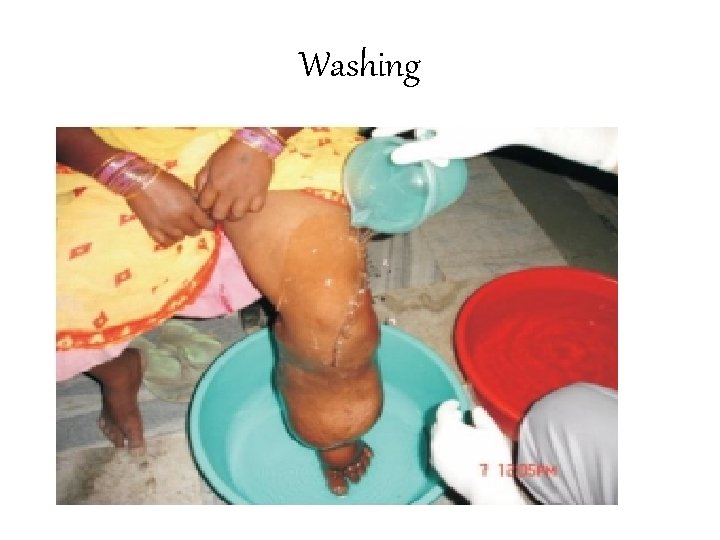
Washing

Prevention and cure of entry lesions
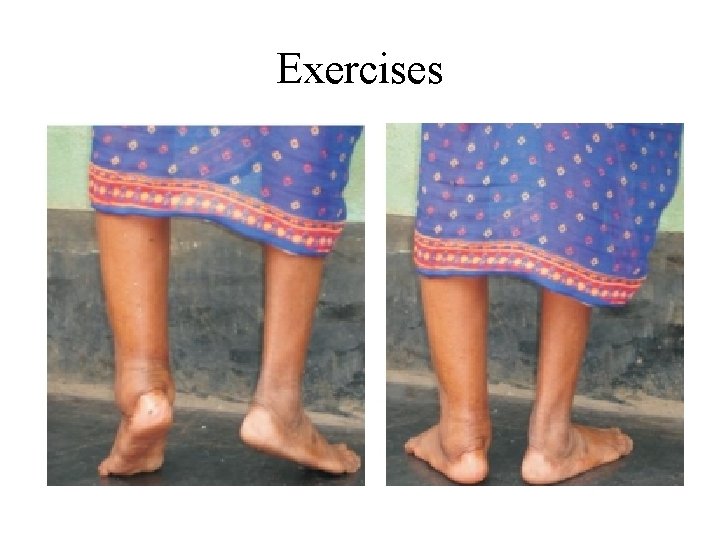
Exercises
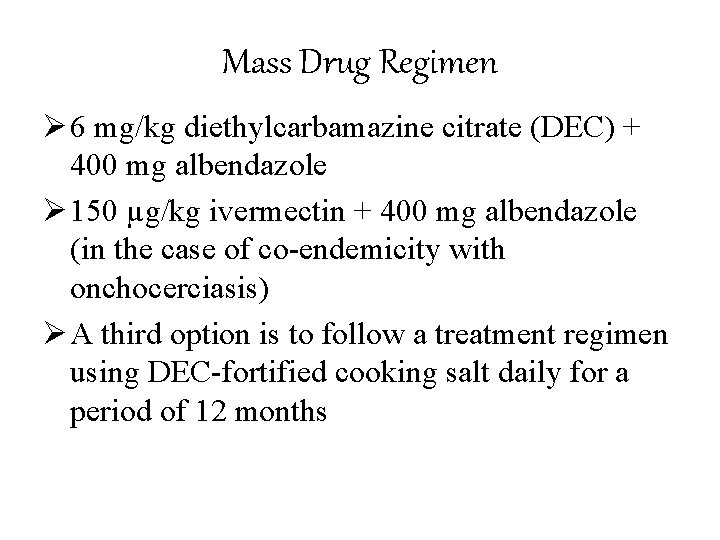
Mass Drug Regimen Ø 6 mg/kg diethylcarbamazine citrate (DEC) + 400 mg albendazole Ø 150 µg/kg ivermectin + 400 mg albendazole (in the case of co-endemicity with onchocerciasis) Ø A third option is to follow a treatment regimen using DEC-fortified cooking salt daily for a period of 12 months
questions Ø Clinical Spectrum of Filariasis Ø Treatment of Lymphatic Filariasis and Mass treatment regimen.
Next class ØFilaria survey ØPrevention & control strategies
Thank you!
 Parallax formula
Parallax formula Filariasis
Filariasis Filariasis infective stage
Filariasis infective stage Wuchereria
Wuchereria Esquistosomiasis
Esquistosomiasis Filariasis
Filariasis Filariasis cronica
Filariasis cronica Attack rate
Attack rate Seven uses of epidemiology
Seven uses of epidemiology Distribution in epidemiology
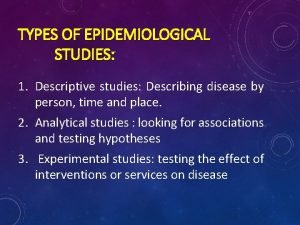
Distribution in epidemiology What is descriptive study in epidemiology
What is descriptive study in epidemiology Temporal relationship epidemiology example
Temporal relationship epidemiology example Nutrition epidemiology definition
Nutrition epidemiology definition How dr. wafaa elsadr epidemiology professor
How dr. wafaa elsadr epidemiology professor Certification board of infection control and epidemiology
Certification board of infection control and epidemiology Diabetic ketoacidosis epidemiology
Diabetic ketoacidosis epidemiology فاطمة خليفة
فاطمة خليفة Formula for attack rate
Formula for attack rate Descriptive vs analytical epidemiology
Descriptive vs analytical epidemiology How dr. wafaa elsadr epidemiology professor
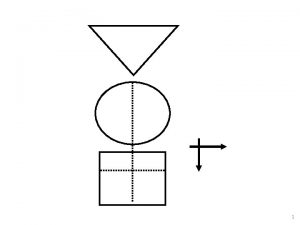
How dr. wafaa elsadr epidemiology professor Epidemiology triangle
Epidemiology triangle Gate frame epidemiology
Gate frame epidemiology Spurious association
Spurious association Attack rate epidemiology formula
Attack rate epidemiology formula Logistic regression epidemiology
Logistic regression epidemiology Nutritional epidemiology
Nutritional epidemiology Distribution in epidemiology
Distribution in epidemiology Defination of epidemiology
Defination of epidemiology Thesourceagents
Thesourceagents How to calculate incidence rate example
How to calculate incidence rate example Epidemiology definition
Epidemiology definition John snow epidemiology
John snow epidemiology Define epidemiology
Define epidemiology Field epidemiology ppt
Field epidemiology ppt Gordon epidemiology
Gordon epidemiology Gate frame epidemiology
Gate frame epidemiology Attack rate formula
Attack rate formula Ookinite
Ookinite Effect modification epidemiology
Effect modification epidemiology Concept of epidemiology
Concept of epidemiology