Lec 07 8 Platelets and Hemostasis Assist Prof
- Slides: 35
Lec 07 & 8: Platelets and Hemostasis Assist. Prof. Dr. Mudhir S. Shekha 1
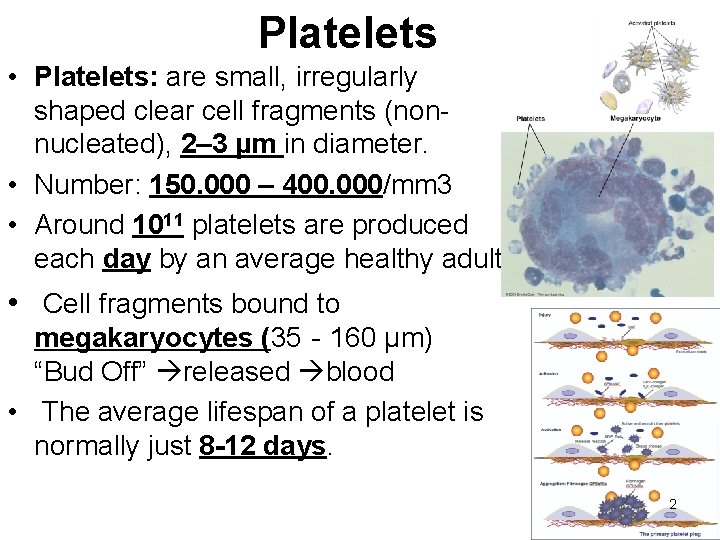
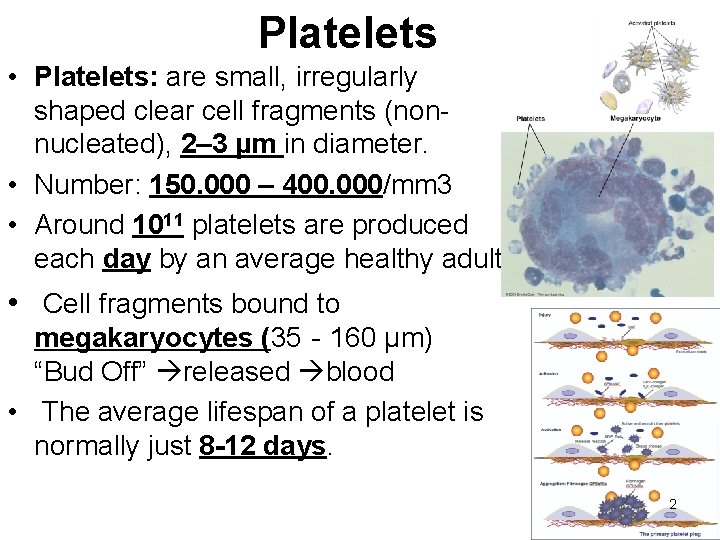
Platelets • Platelets: are small, irregularly shaped clear cell fragments (nonnucleated), 2– 3 µm in diameter. • Number: 150. 000 – 400. 000/mm 3 • Around 1011 platelets are produced each day by an average healthy adult. • Cell fragments bound to megakaryocytes (35‐ 160 μm) “Bud Off” released blood • The average lifespan of a platelet is normally just 8 -12 days. 2
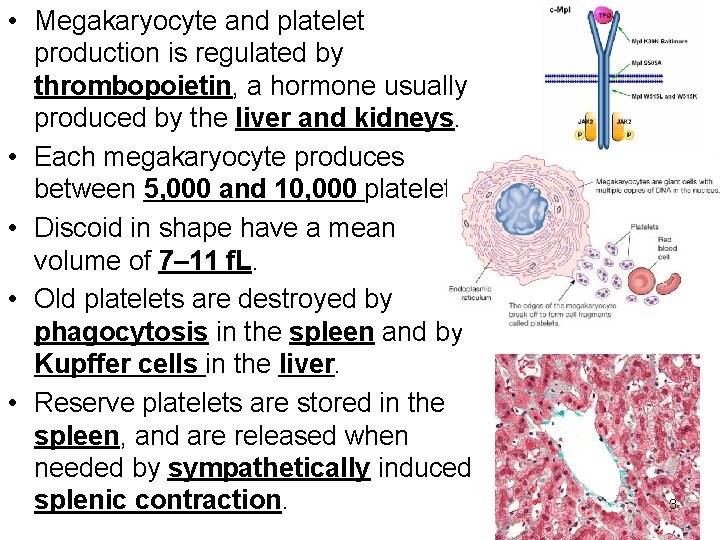
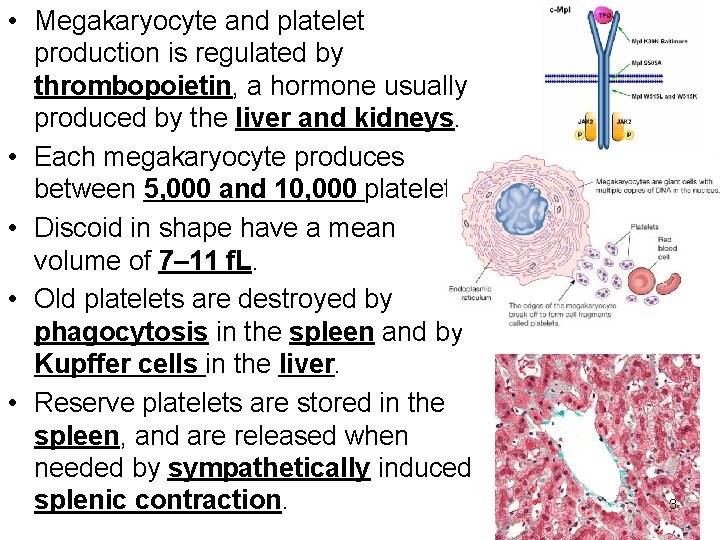
• Megakaryocyte and platelet production is regulated by thrombopoietin, a hormone usually produced by the liver and kidneys. • Each megakaryocyte produces between 5, 000 and 10, 000 platelets • Discoid in shape have a mean volume of 7– 11 f. L. • Old platelets are destroyed by phagocytosis in the spleen and by Kupffer cells in the liver. • Reserve platelets are stored in the spleen, and are released when needed by sympathetically induced splenic contraction. 3
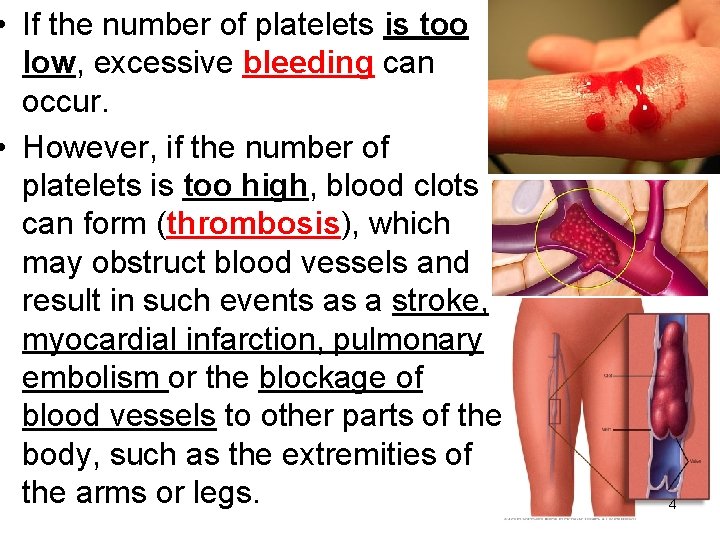
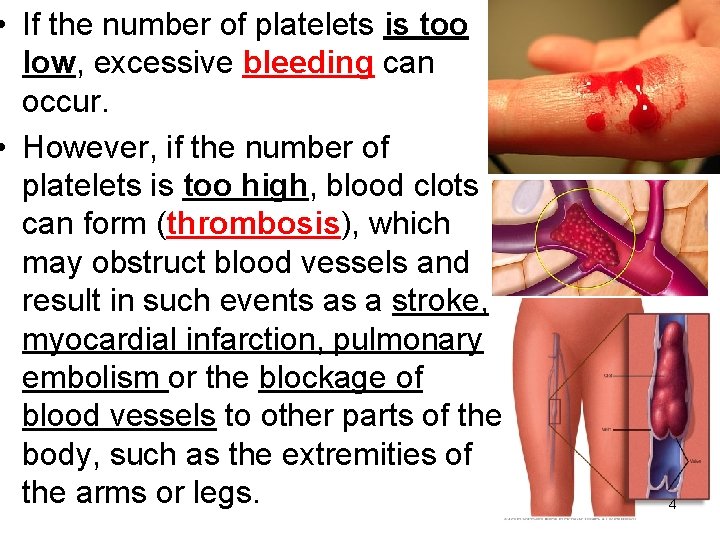
• If the number of platelets is too low, excessive bleeding can occur. • However, if the number of platelets is too high, blood clots can form (thrombosis), which may obstruct blood vessels and result in such events as a stroke, myocardial infarction, pulmonary embolism or the blockage of blood vessels to other parts of the body, such as the extremities of the arms or legs. 4
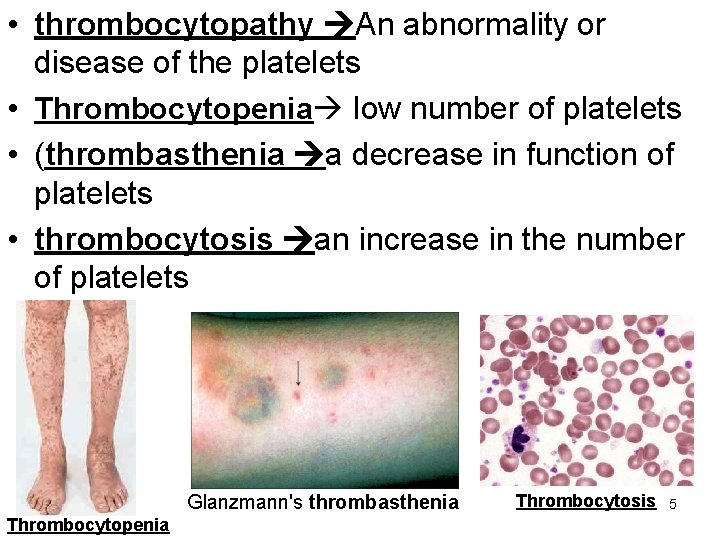
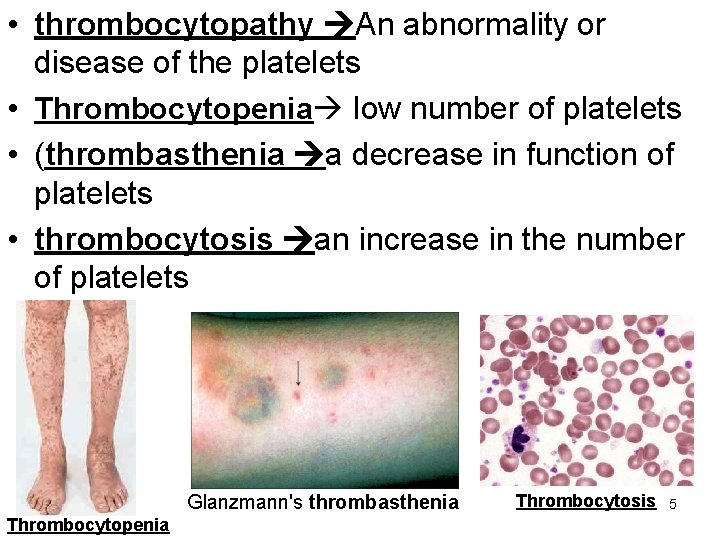
• thrombocytopathy An abnormality or disease of the platelets • Thrombocytopenia low number of platelets • (thrombasthenia a decrease in function of platelets • thrombocytosis an increase in the number of platelets Glanzmann's thrombasthenia Thrombocytopenia Thrombocytosis 5
Platelet structure 1 - Surface coat mucopolysaccharide • • • GPIb-IX-V: It is the major platelet receptor for VWF. GPIa and GPVI: receptors for collagen. GPIIb-IIIa: receptor for v. WF. Thromboxane A 2 (TXA 2) receptor. ADP receptors: P 2 Y 12 and P 2 Y 1. 2 - Plasma membrane: is formed of 3 layers and invaginates inside to form open membrane system and contain Lipids (phospholipids, cholesterol & glycolipids). Carbohydrates & Proteins (Glycoproteins). This membrane is the basis structure of platelet factor 3 (PF 3). Responsible for the release of fatty acid derivatives: PGs, 6 prostacyclins.
Platelet structure 7
Structural Zone • Organized network of protein filaments. • Maintain shape of resting platelet—discoid. • 3 principle types of filaments: a). Microtubules: - Located beneath the cell membrane of resting platelet. Maintain discoid shape. b). Microfilaments: - Mediate contractile events. c). Intermediate filaments. 8
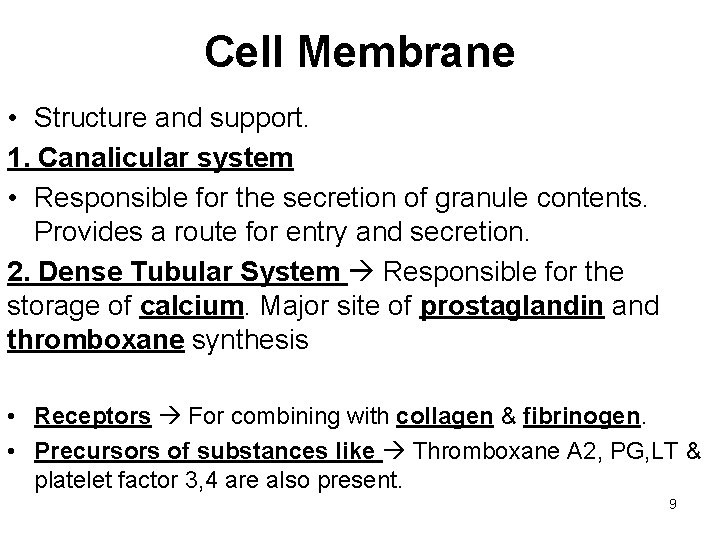
Cell Membrane • Structure and support. 1. Canalicular system • Responsible for the secretion of granule contents. Provides a route for entry and secretion. 2. Dense Tubular System Responsible for the storage of calcium. Major site of prostaglandin and thromboxane synthesis • Receptors For combining with collagen & fibrinogen. • Precursors of substances like Thromboxane A 2, PG, LT & platelet factor 3, 4 are also present. 9
Organelle Zone • - Secretion and storage. • Mitochondria. Power house of cell & Produce ATP & ADP. • Endoplasmic Reticulum – stores large amount of calcium. • Glycogen particles: support metabolic activities & Synthesizes various Enzymes. • lysosomes which contain hydrolytic enzymes • Actin & Myosin – same as those of contractile proteins of muscle. Responsible for platelet contraction & clot retraction. • Granules: dispersed within the cytoplasm, which serve as storage sites for proteins platelet function 10
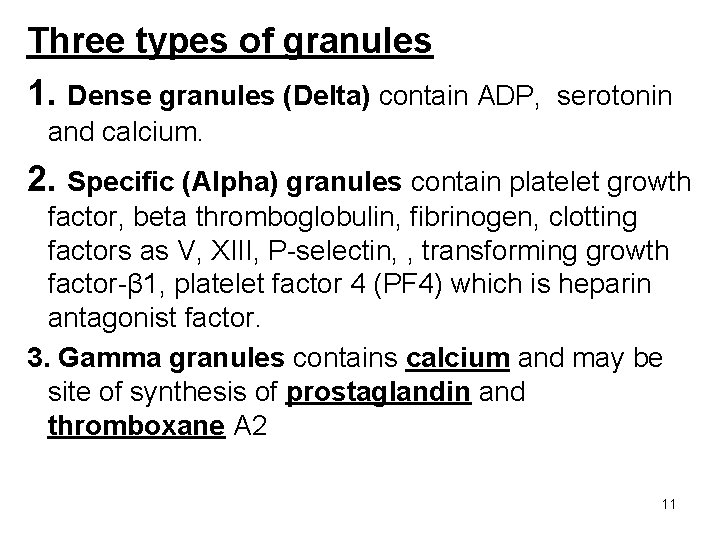
Three types of granules 1. Dense granules (Delta) contain ADP, serotonin and calcium. 2. Specific (Alpha) granules contain platelet growth factor, beta thromboglobulin, fibrinogen, clotting factors as V, XIII, P-selectin, , transforming growth factor-β 1, platelet factor 4 (PF 4) which is heparin antagonist factor. 3. Gamma granules contains calcium and may be site of synthesis of prostaglandin and thromboxane A 2 11
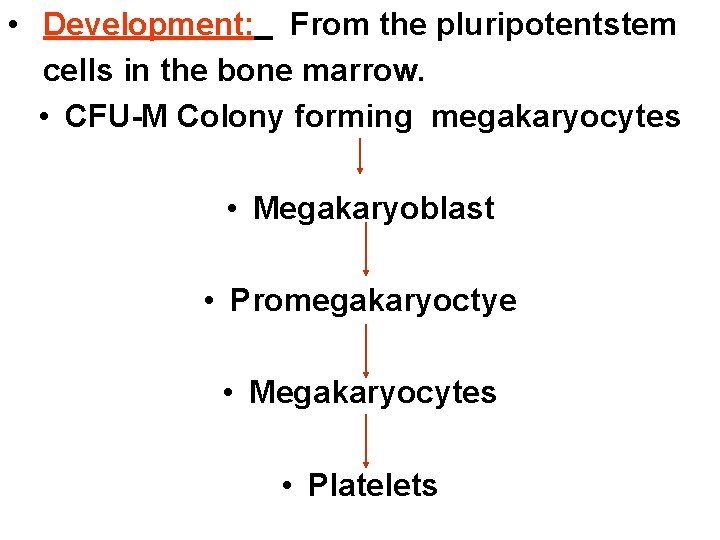
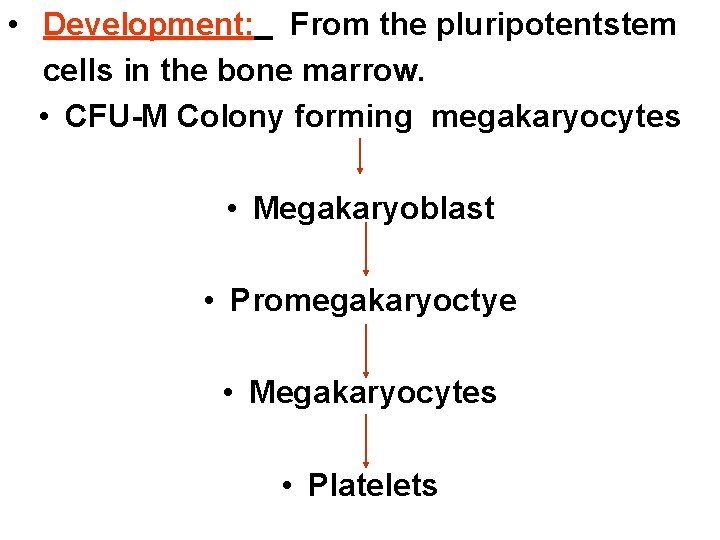
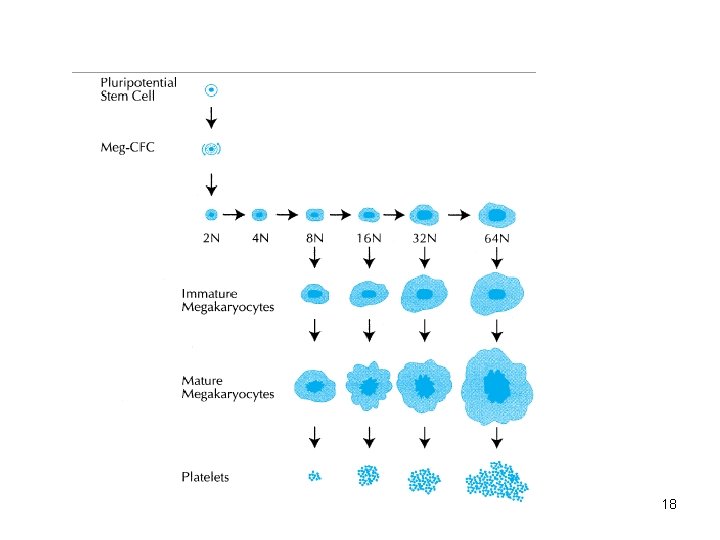
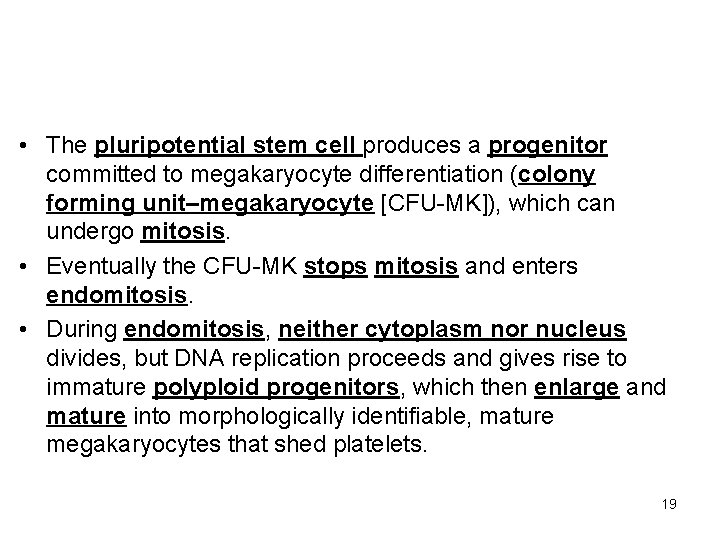
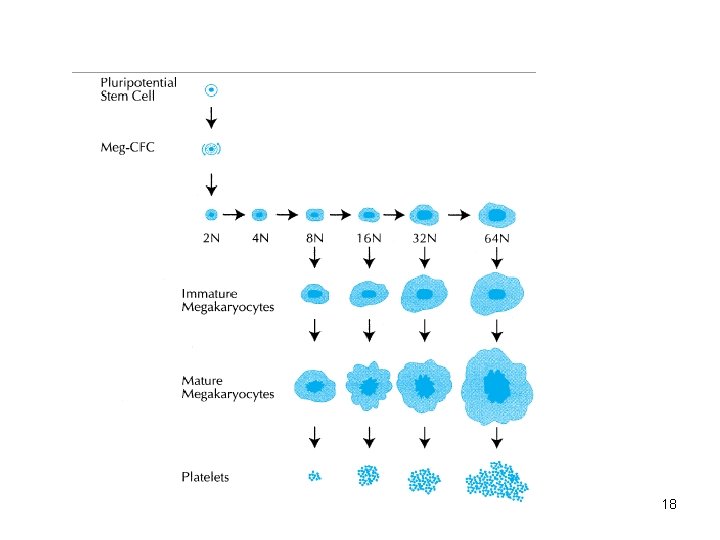
• Development: From the pluripotentstem cells in the bone marrow. • CFU-M Colony forming megakaryocytes • Megakaryoblast • Promegakaryoctye • Megakaryocytes • Platelets
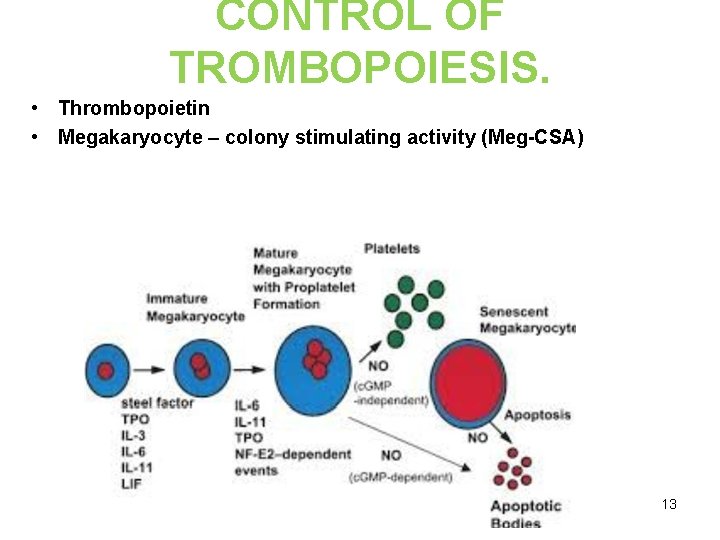
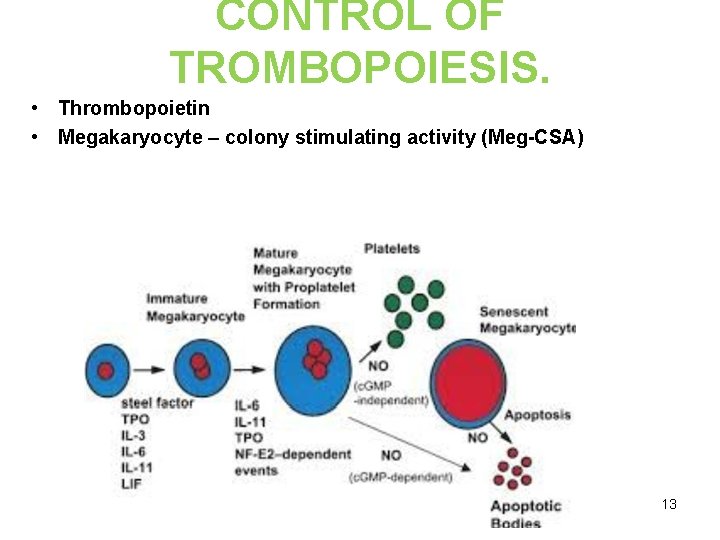
CONTROL OF TROMBOPOIESIS. • Thrombopoietin • Megakaryocyte – colony stimulating activity (Meg-CSA) 13
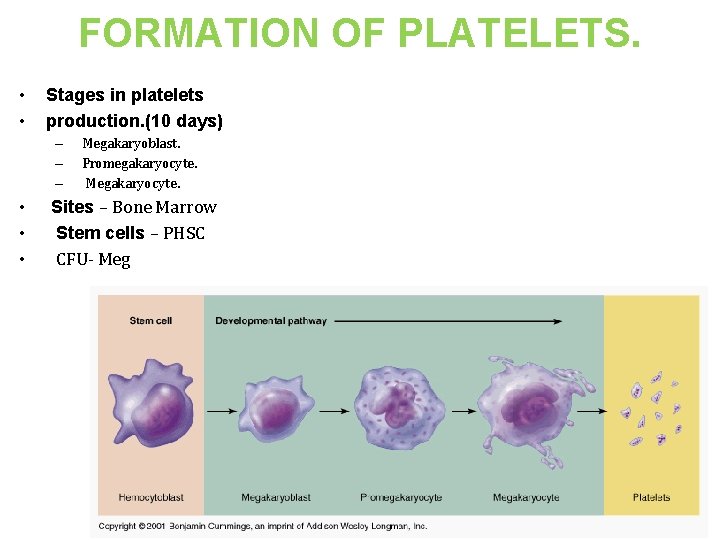
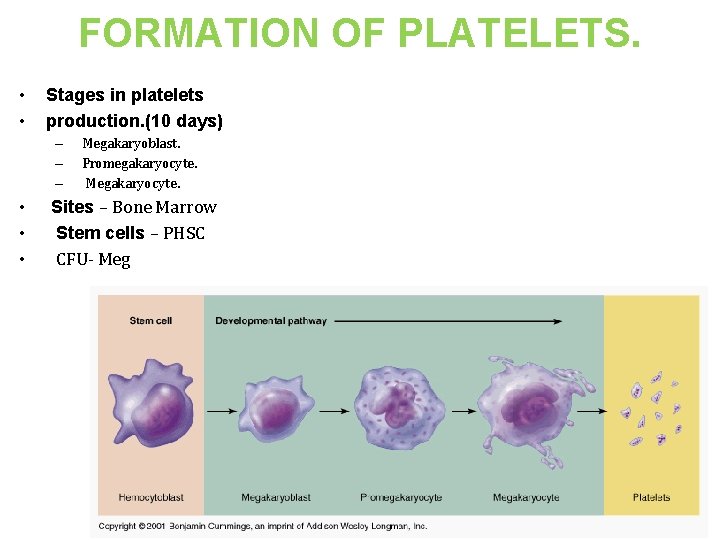
FORMATION OF PLATELETS. • • Stages in platelets production. (10 days) – – – • • • Megakaryoblast. Promegakaryocyte. Megakaryocyte. Sites – Bone Marrow Stem cells – PHSC CFU- Meg 14
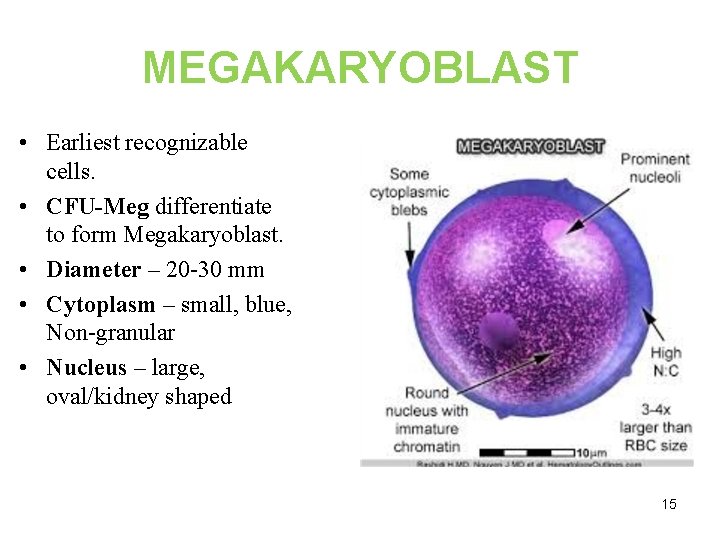
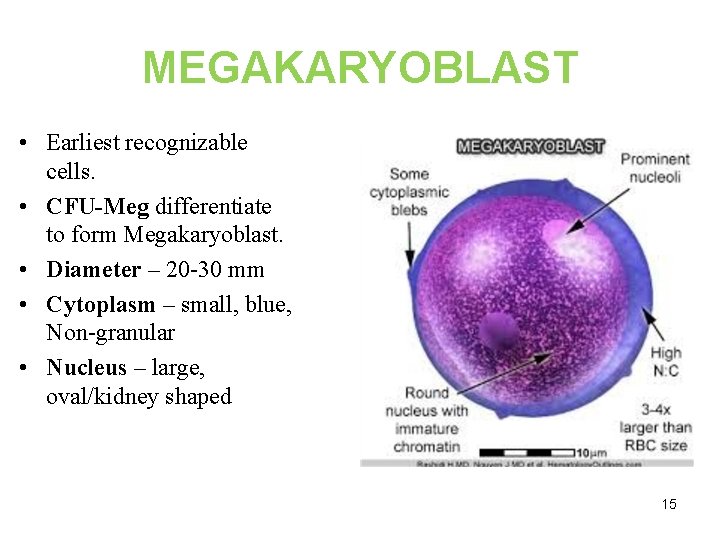
MEGAKARYOBLAST • Earliest recognizable cells. • CFU-Meg differentiate to form Megakaryoblast. • Diameter – 20 -30 mm • Cytoplasm – small, blue, Non-granular • Nucleus – large, oval/kidney shaped 15
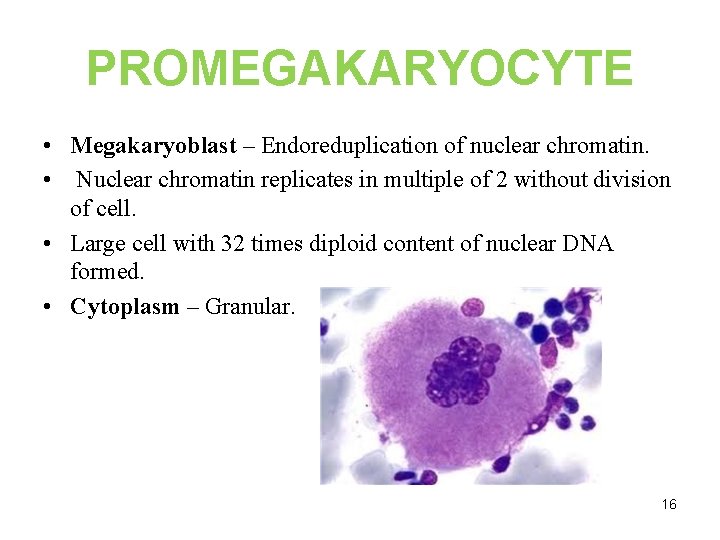
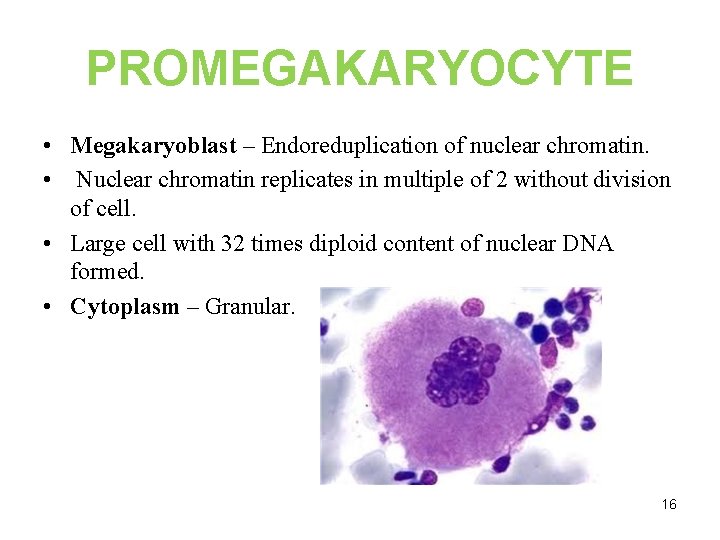
PROMEGAKARYOCYTE • Megakaryoblast – Endoreduplication of nuclear chromatin. • Nuclear chromatin replicates in multiple of 2 without division of cell. • Large cell with 32 times diploid content of nuclear DNA formed. • Cytoplasm – Granular. 16
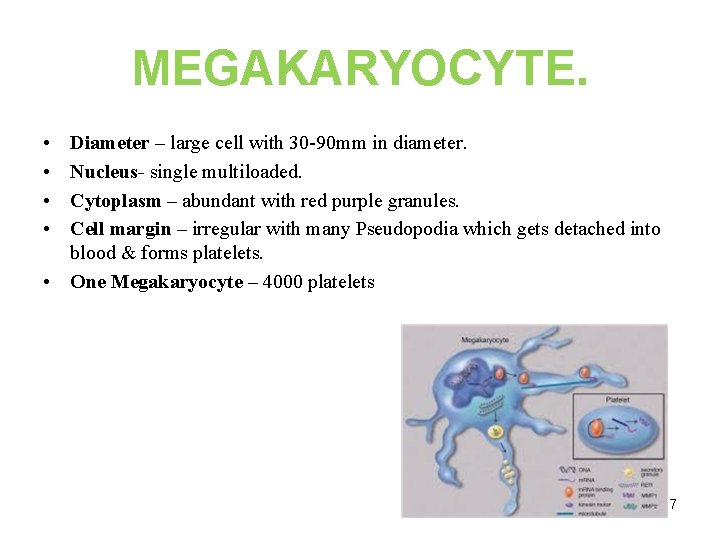
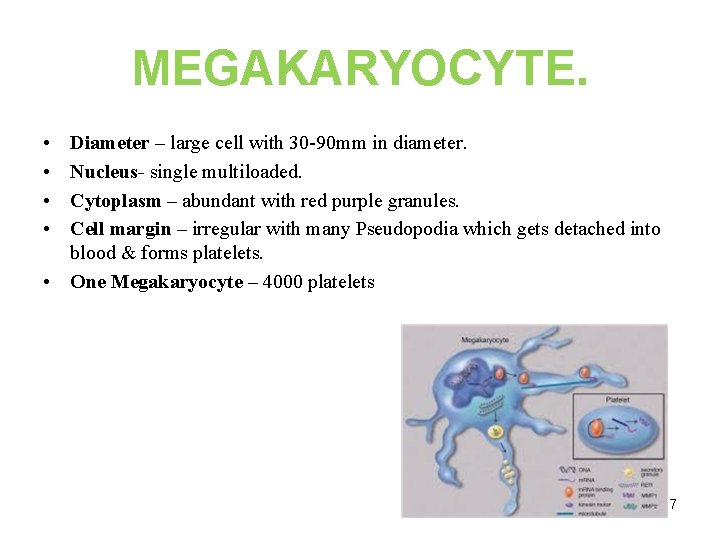
MEGAKARYOCYTE. • • Diameter – large cell with 30 -90 mm in diameter. Nucleus- single multiloaded. Cytoplasm – abundant with red purple granules. Cell margin – irregular with many Pseudopodia which gets detached into blood & forms platelets. • One Megakaryocyte – 4000 platelets 17
18
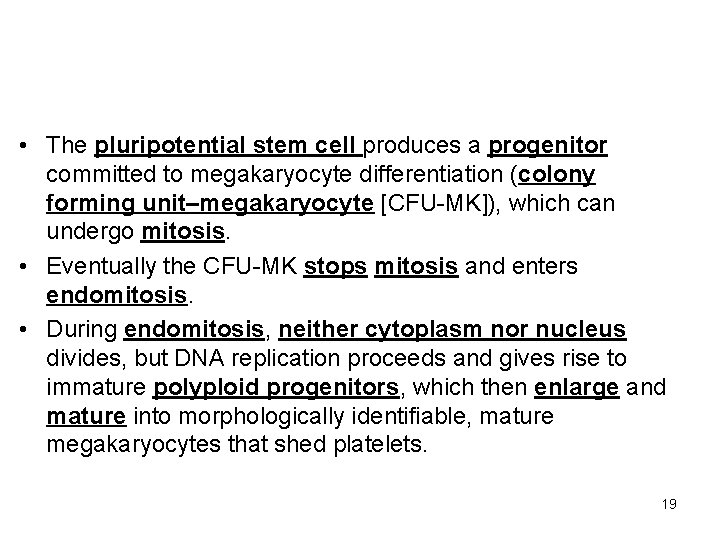
• The pluripotential stem cell produces a progenitor committed to megakaryocyte differentiation (colony forming unit–megakaryocyte [CFU-MK]), which can undergo mitosis. • Eventually the CFU-MK stops mitosis and enters endomitosis. • During endomitosis, neither cytoplasm nor nucleus divides, but DNA replication proceeds and gives rise to immature polyploid progenitors, which then enlarge and mature into morphologically identifiable, mature megakaryocytes that shed platelets. 19
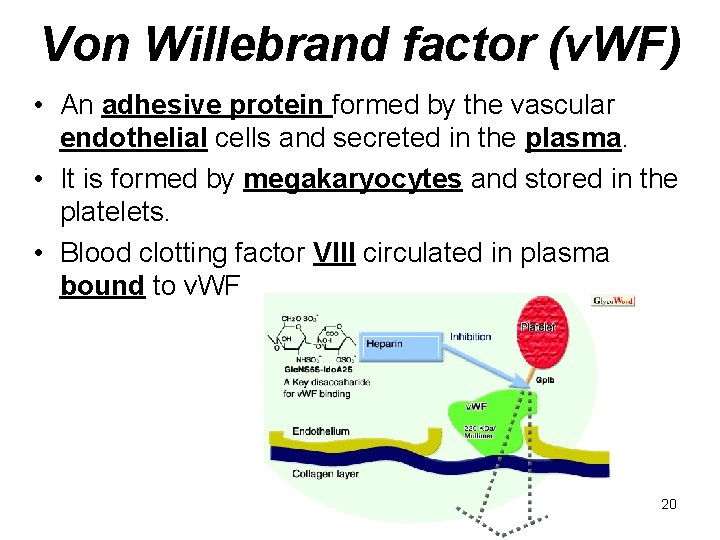
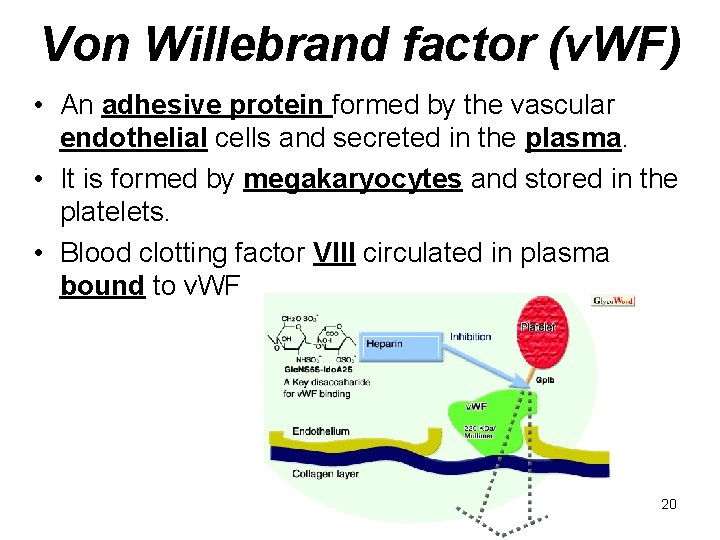
Von Willebrand factor (v. WF) • An adhesive protein formed by the vascular endothelial cells and secreted in the plasma. • It is formed by megakaryocytes and stored in the platelets. • Blood clotting factor VIII circulated in plasma bound to v. WF 20
Thrombus formation • The function of platelets is the maintenance of hemostasis. This is achieved primarily by the formation of thrombi, when damage to the endothelium of blood vessels occurs. On the converse, thrombus formation must be inhibited at times when there is no damage to the endothelium. • It depends on: • the vascular wall, platelets and the clotting factors 21
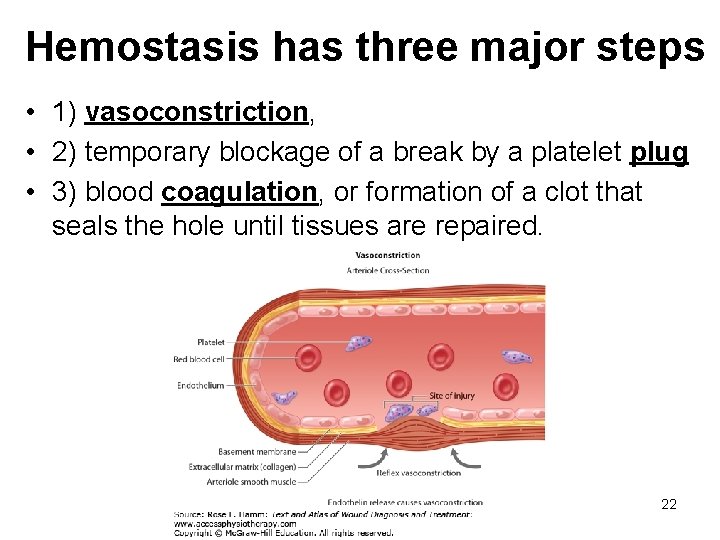
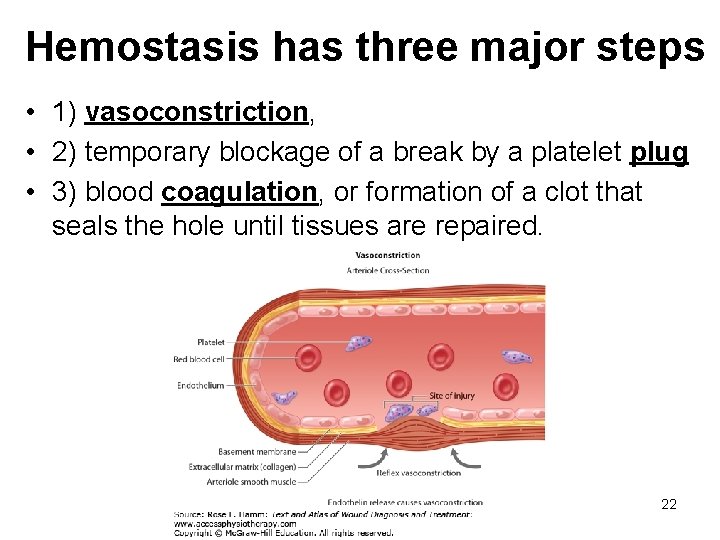
Hemostasis has three major steps • 1) vasoconstriction, • 2) temporary blockage of a break by a platelet plug • 3) blood coagulation, or formation of a clot that seals the hole until tissues are repaired. 22
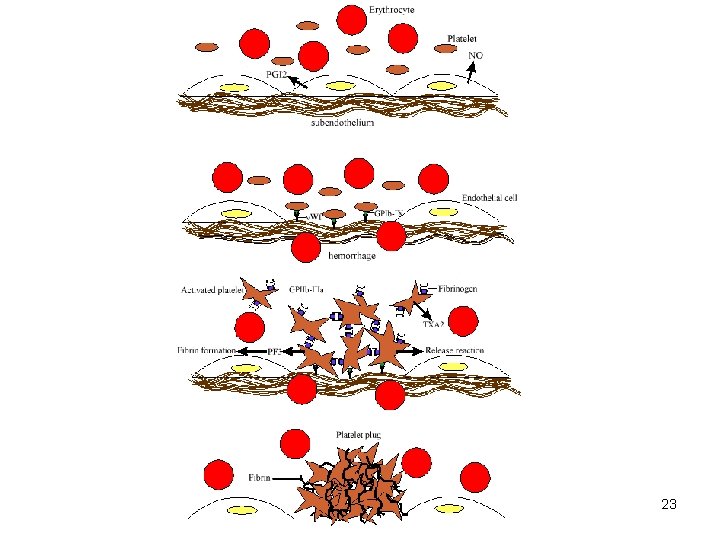
23
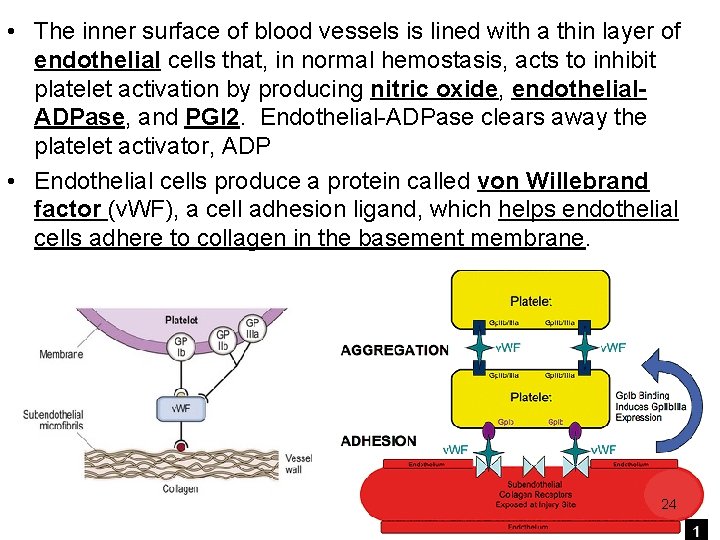
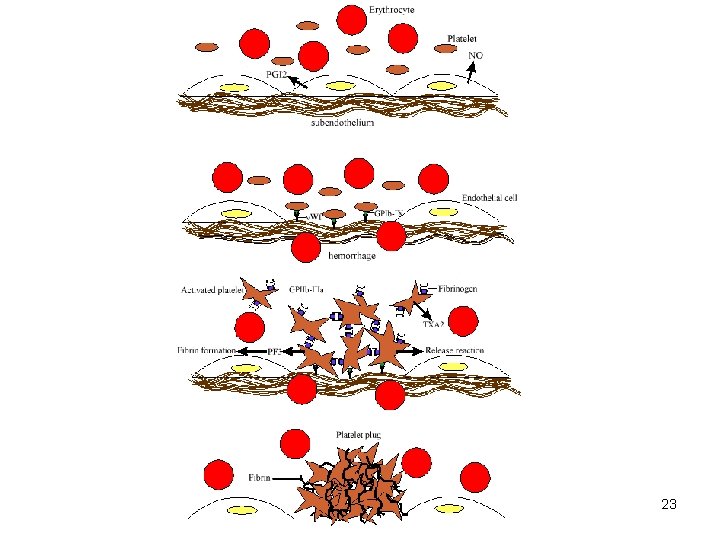
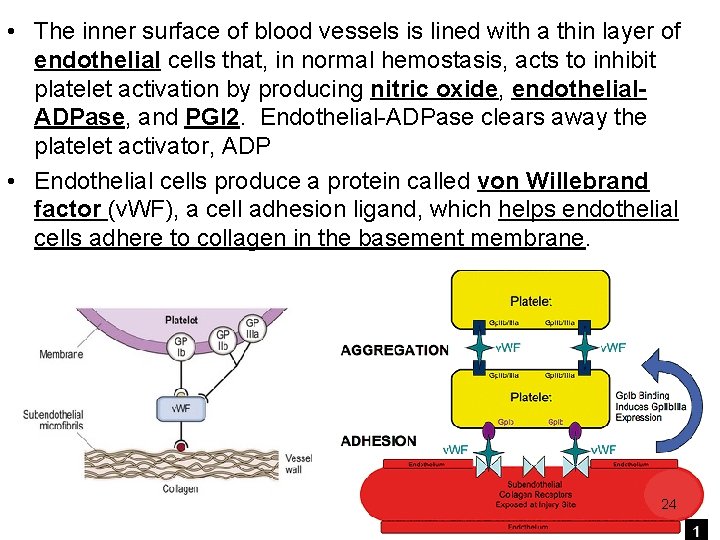
• The inner surface of blood vessels is lined with a thin layer of endothelial cells that, in normal hemostasis, acts to inhibit platelet activation by producing nitric oxide, endothelial. ADPase, and PGI 2. Endothelial-ADPase clears away the platelet activator, ADP • Endothelial cells produce a protein called von Willebrand factor (v. WF), a cell adhesion ligand, which helps endothelial cells adhere to collagen in the basement membrane. 24
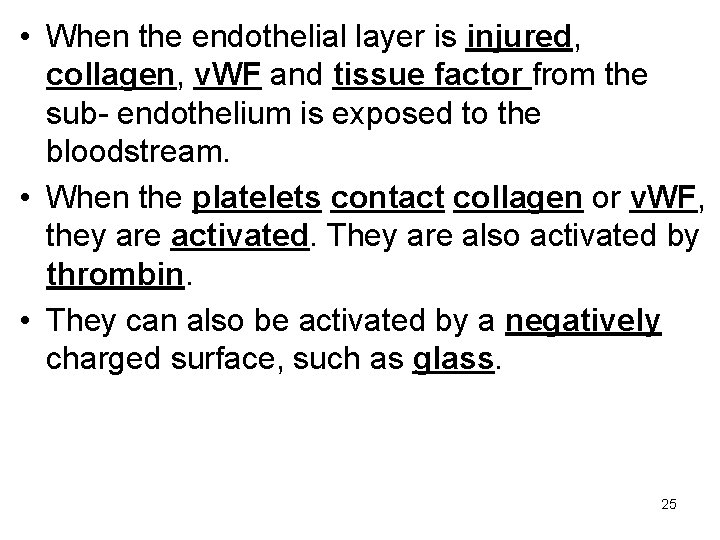
• When the endothelial layer is injured, collagen, v. WF and tissue factor from the sub- endothelium is exposed to the bloodstream. • When the platelets contact collagen or v. WF, they are activated. They are also activated by thrombin. • They can also be activated by a negatively charged surface, such as glass. 25
• Non-physiological flow conditions caused by arterial stenosis or artificial devices can also lead to platelet activation • Calcium ions are essential for binding of these coagulation factors. • Larger platelets are metabolically and functionally more active than small platelets. 26
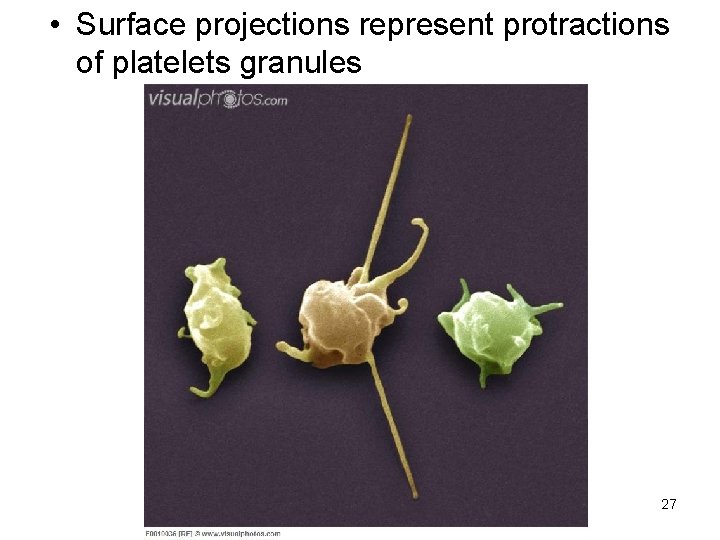
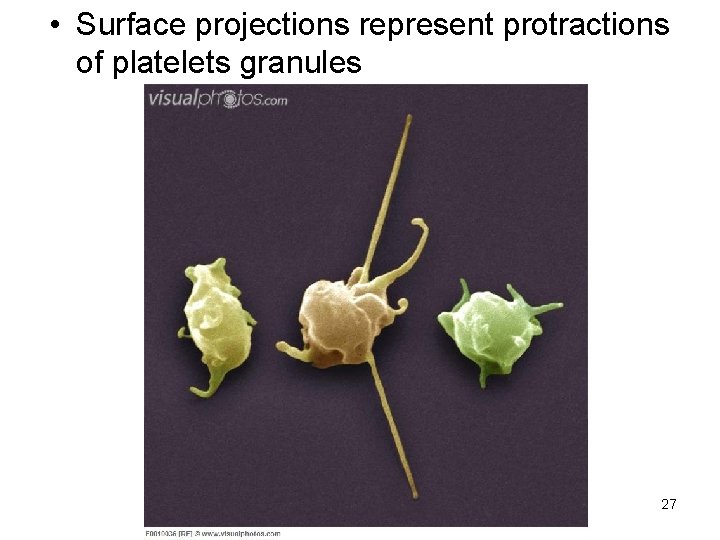
• Surface projections represent protractions of platelets granules 27
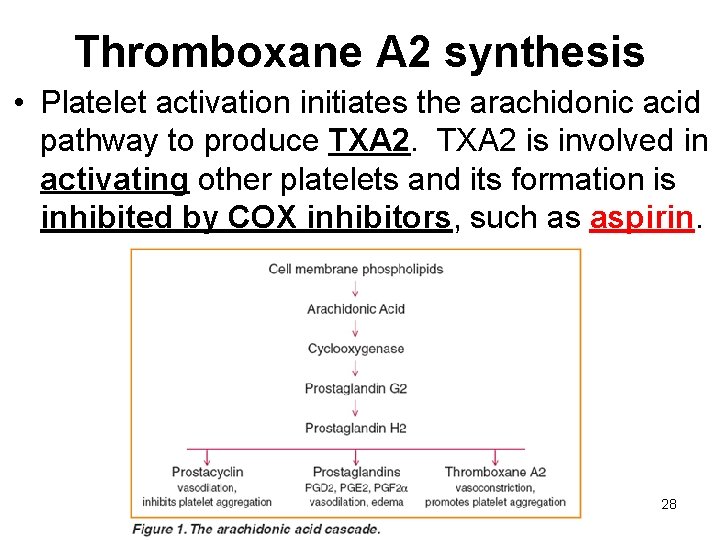
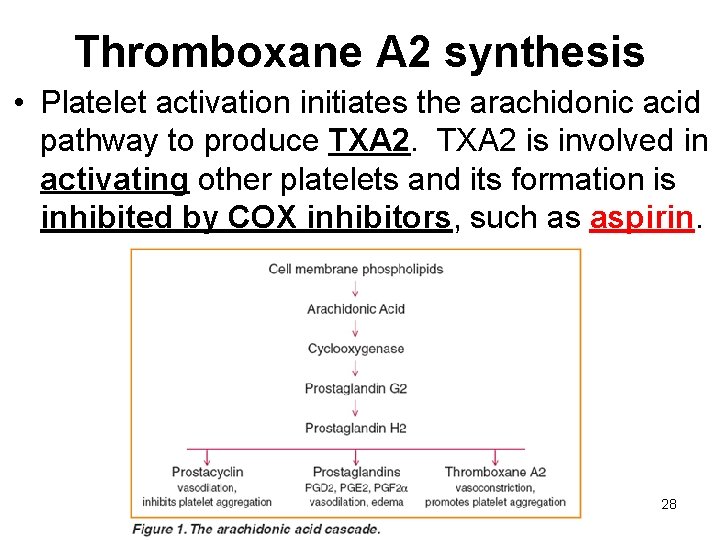
Thromboxane A 2 synthesis • Platelet activation initiates the arachidonic acid pathway to produce TXA 2 is involved in activating other platelets and its formation is inhibited by COX inhibitors, such as aspirin. 28
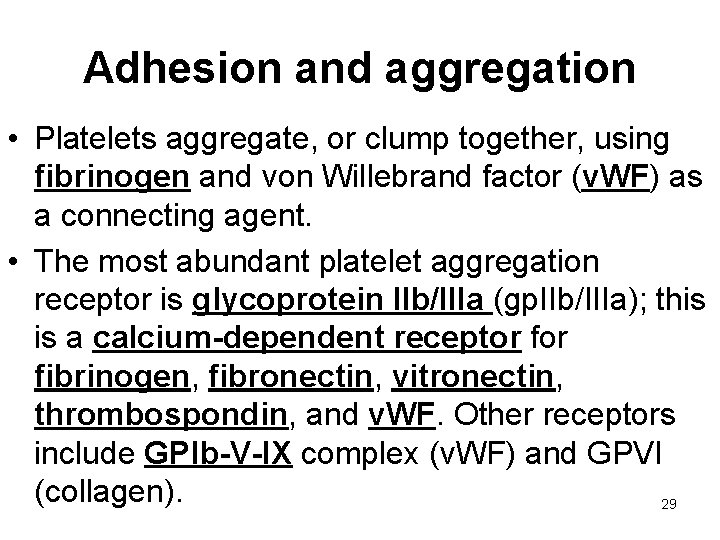
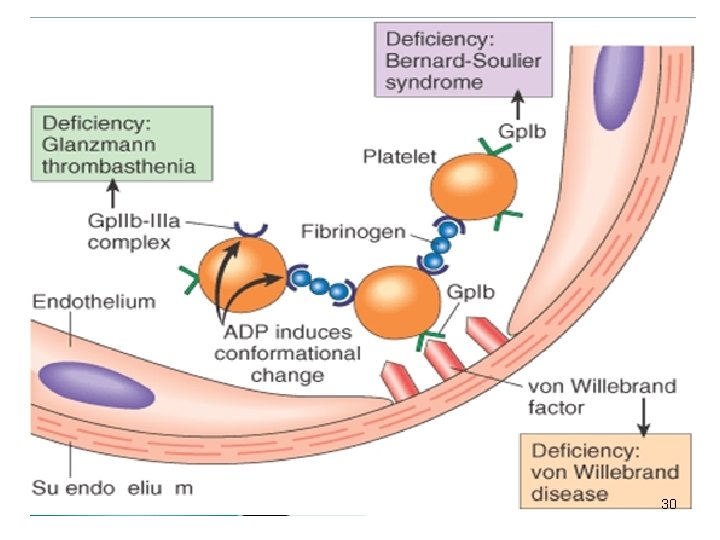
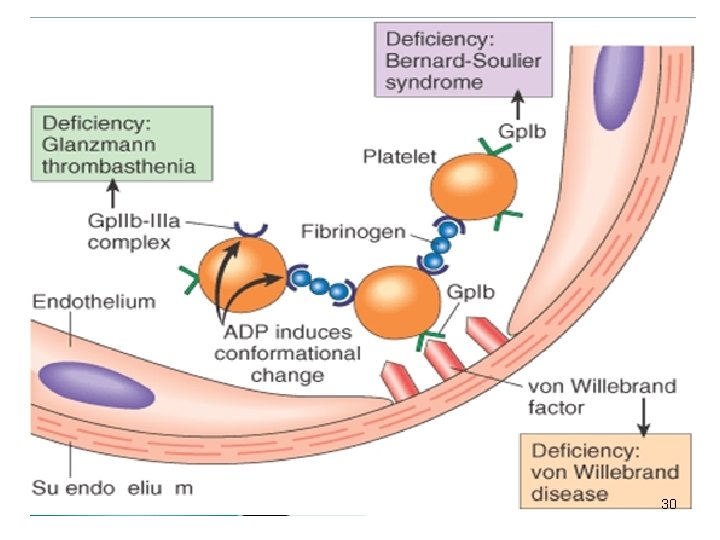
Adhesion and aggregation • Platelets aggregate, or clump together, using fibrinogen and von Willebrand factor (v. WF) as a connecting agent. • The most abundant platelet aggregation receptor is glycoprotein IIb/IIIa (gp. IIb/IIIa); this is a calcium-dependent receptor fibrinogen, fibronectin, vitronectin, thrombospondin, and v. WF. Other receptors include GPIb-V-IX complex (v. WF) and GPVI (collagen). 29
30
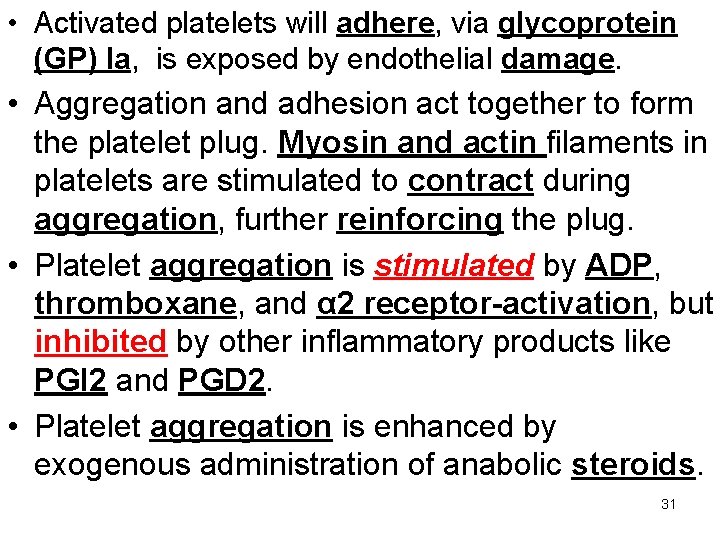
• Activated platelets will adhere, via glycoprotein (GP) Ia, is exposed by endothelial damage. • Aggregation and adhesion act together to form the platelet plug. Myosin and actin filaments in platelets are stimulated to contract during aggregation, further reinforcing the plug. • Platelet aggregation is stimulated by ADP, thromboxane, and α 2 receptor-activation, but inhibited by other inflammatory products like PGI 2 and PGD 2. • Platelet aggregation is enhanced by exogenous administration of anabolic steroids. 31
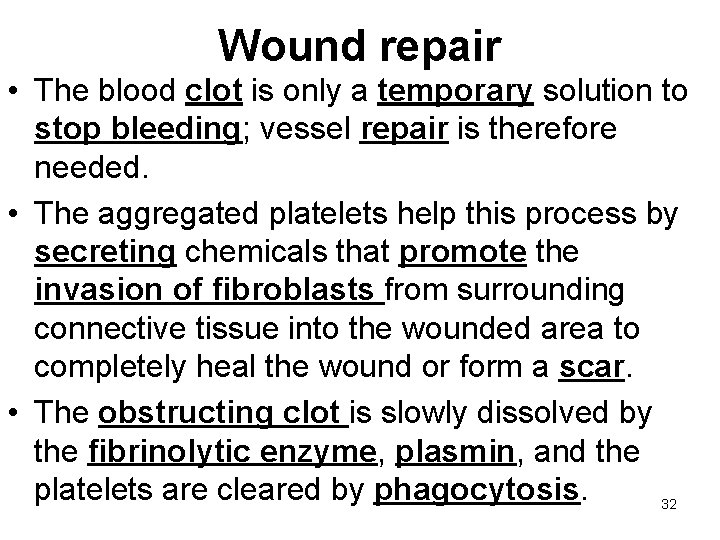
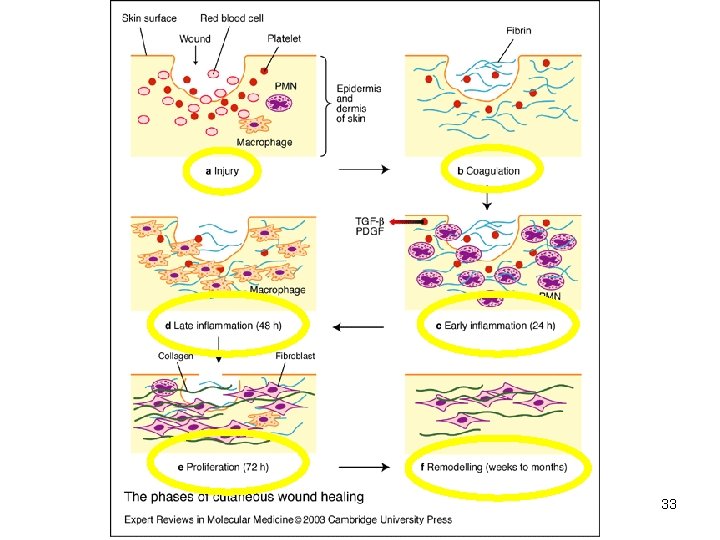
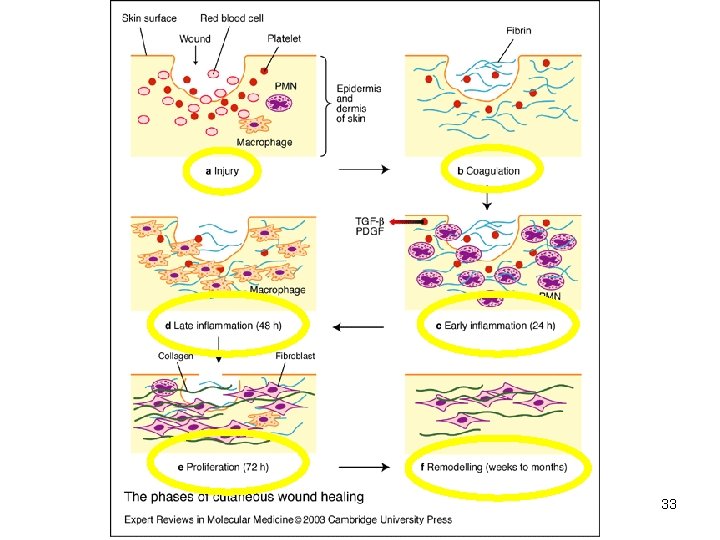
Wound repair • The blood clot is only a temporary solution to stop bleeding; vessel repair is therefore needed. • The aggregated platelets help this process by secreting chemicals that promote the invasion of fibroblasts from surrounding connective tissue into the wounded area to completely heal the wound or form a scar. • The obstructing clot is slowly dissolved by the fibrinolytic enzyme, plasmin, and the platelets are cleared by phagocytosis. 32
33
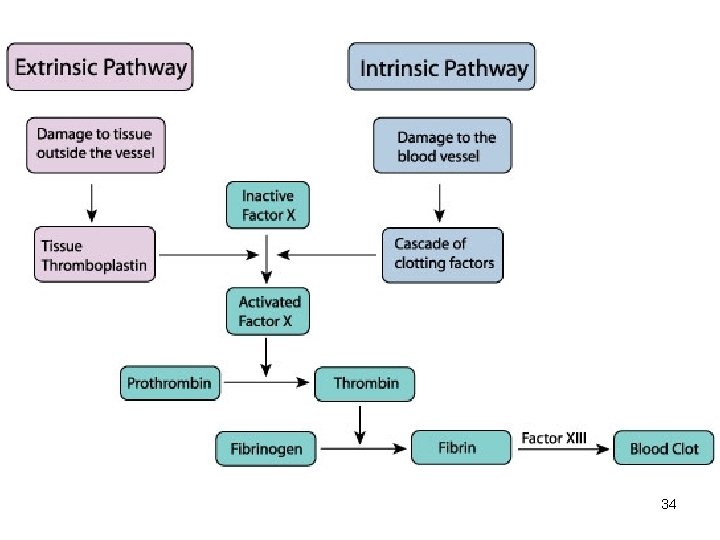
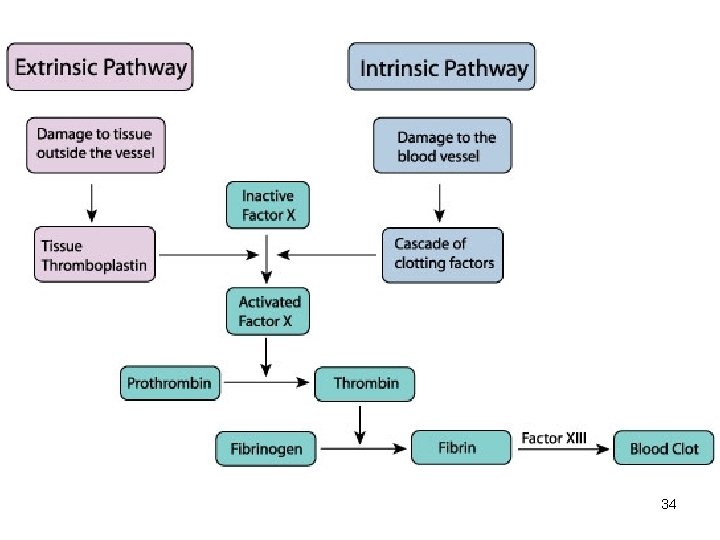
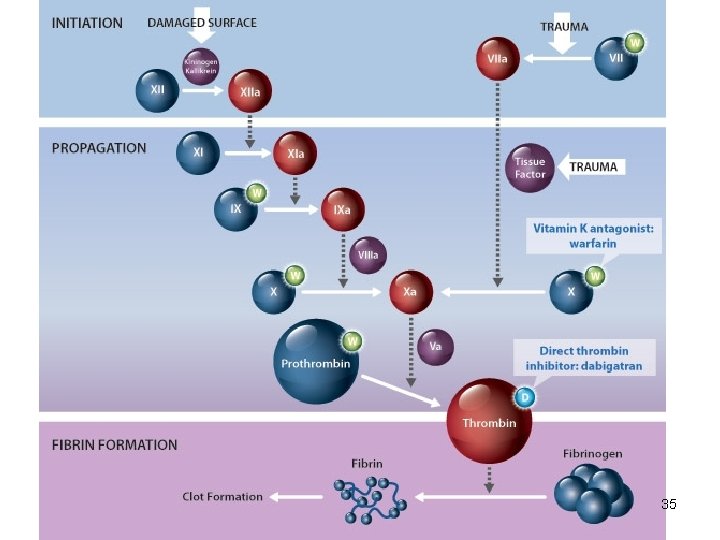
34
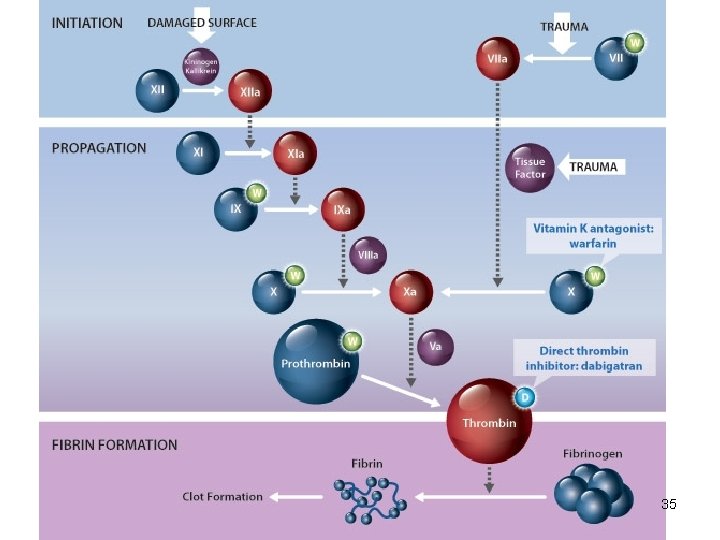
35