Platelets and hemostasis Platelets 250 000 500 000







- Slides: 25
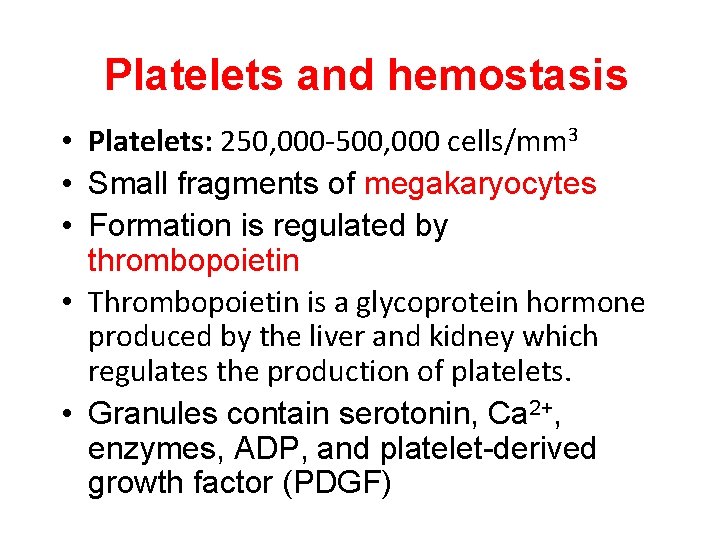
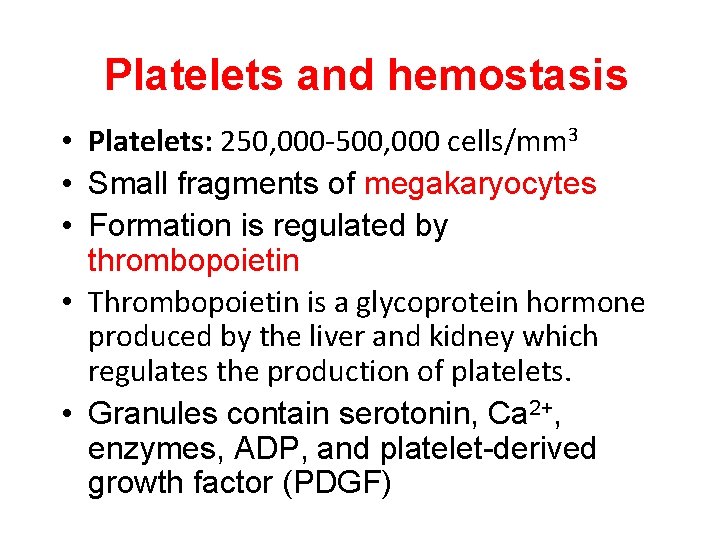
Platelets and hemostasis • Platelets: 250, 000 -500, 000 cells/mm 3 • Small fragments of megakaryocytes • Formation is regulated by thrombopoietin • Thrombopoietin is a glycoprotein hormone produced by the liver and kidney which regulates the production of platelets. • Granules contain serotonin, Ca 2+, enzymes, ADP, and platelet-derived growth factor (PDGF)
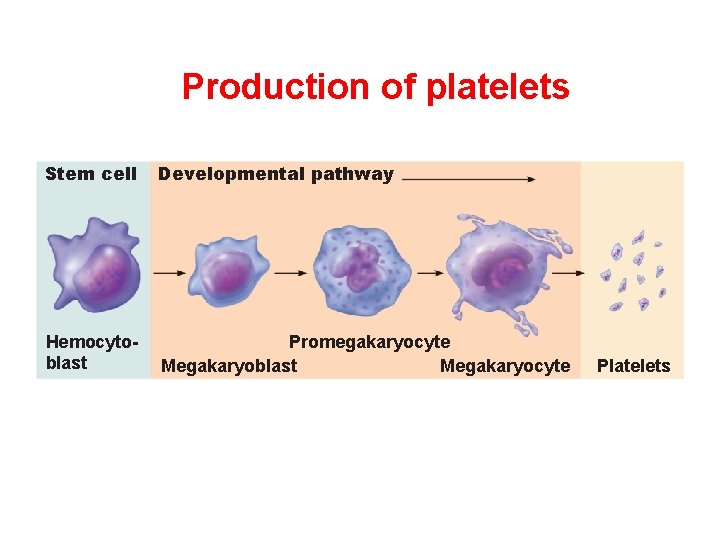
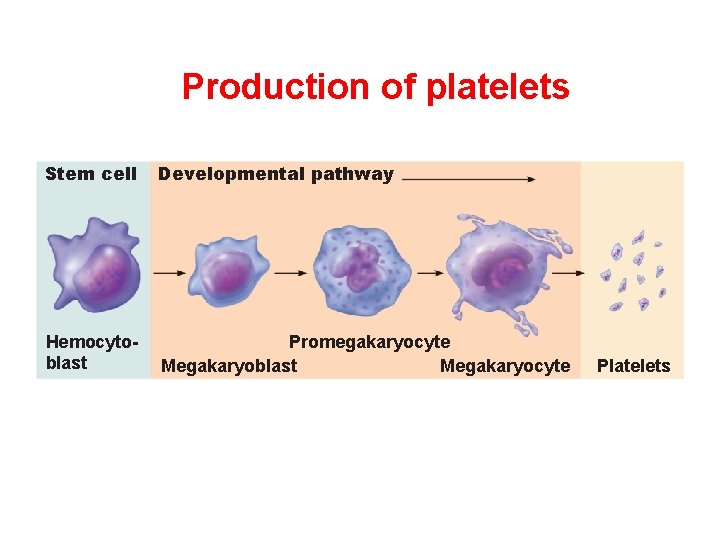
Production of platelets Stem cell Developmental pathway Hemocytoblast Promegakaryocyte Megakaryoblast Megakaryocyte Platelets
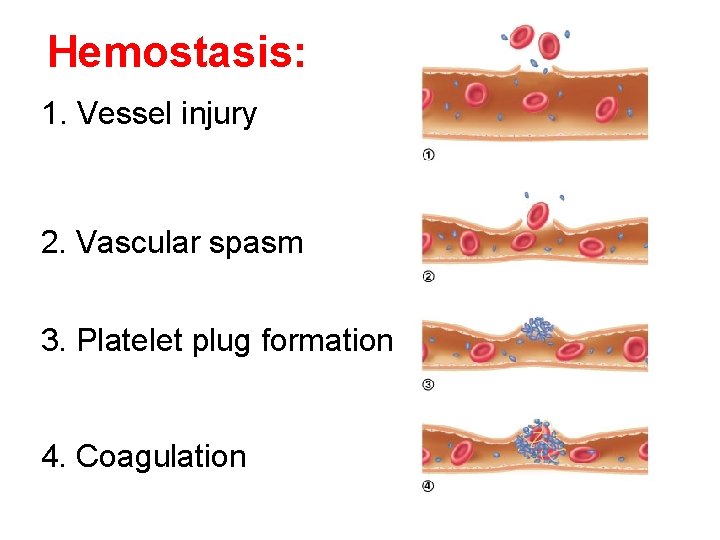
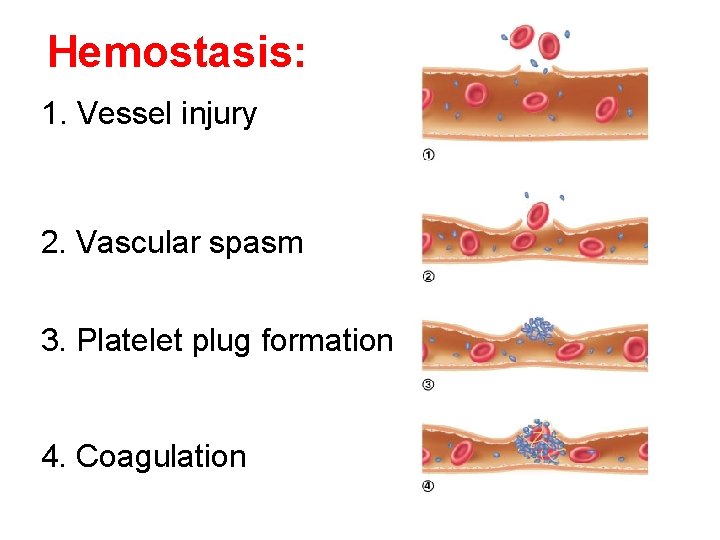
Hemostasis: 1. Vessel injury 2. Vascular spasm 3. Platelet plug formation 4. Coagulation
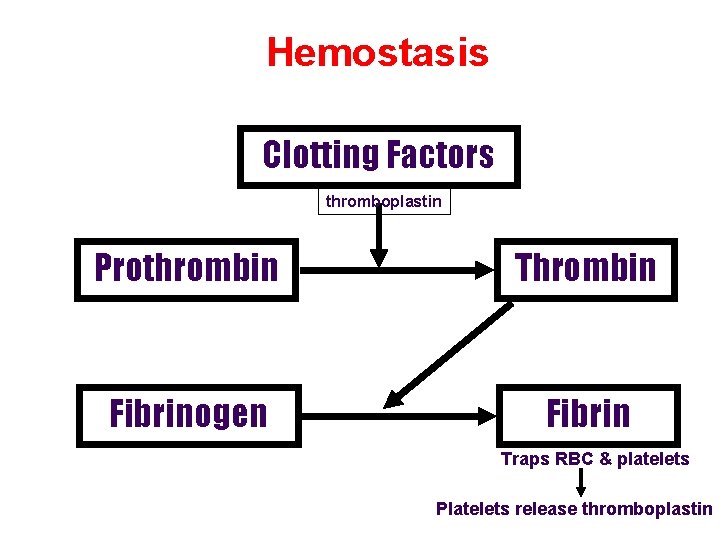
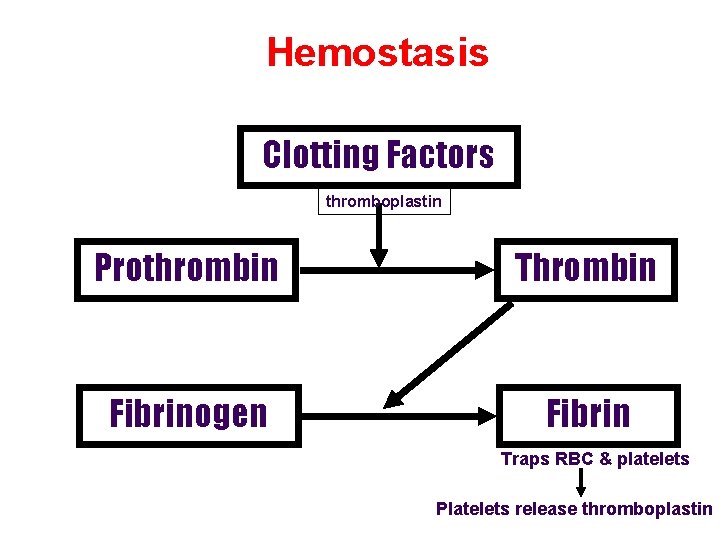
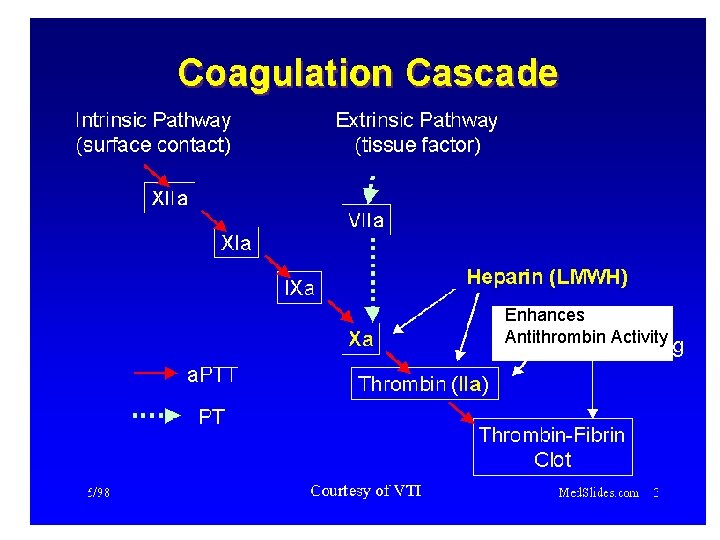
Hemostasis Clotting Factors thromboplastin Prothrombin Thrombin Fibrinogen Fibrin Traps RBC & platelets Platelets release thromboplastin
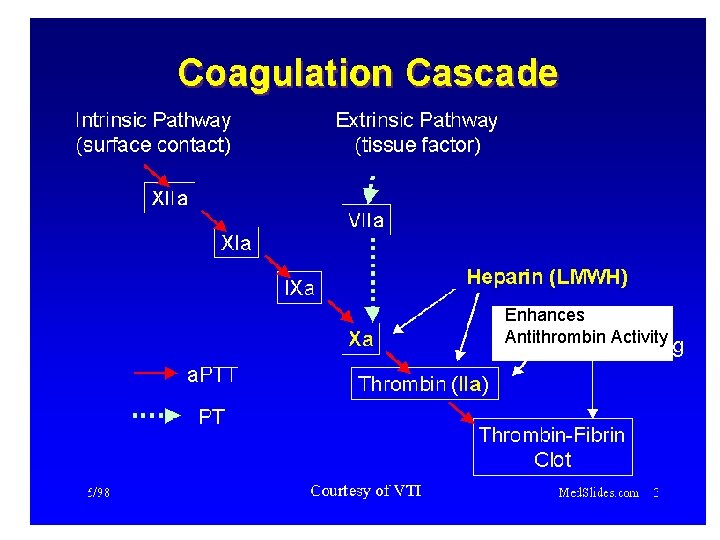
Enhances Antithrombin Activity
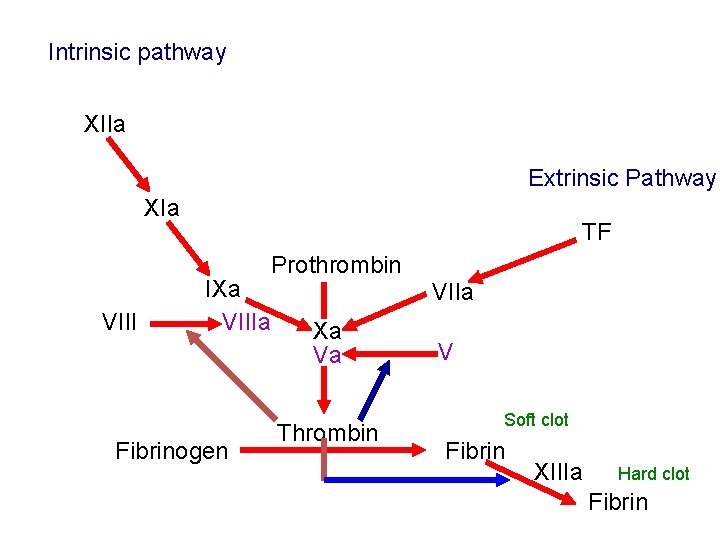
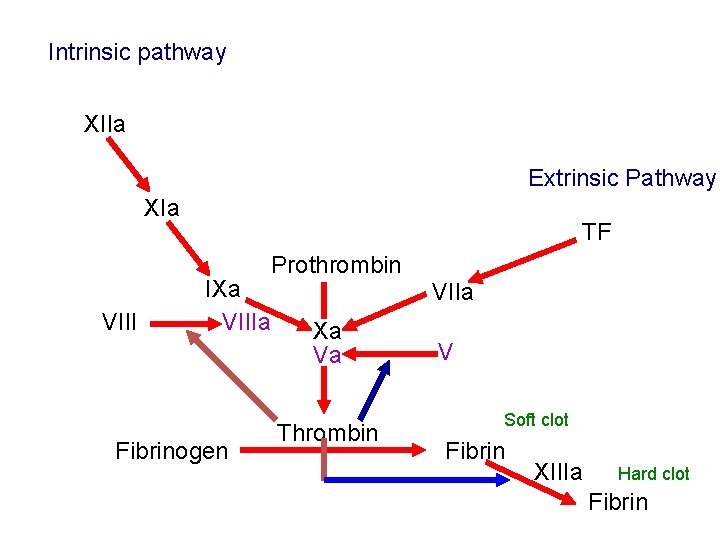
Intrinsic pathway XIIa Extrinsic Pathway XIa TF Prothrombin VIII IXa VIIIa Fibrinogen VIIa Xa Va Thrombin V Soft clot Fibrin XIIIa Hard clot Fibrin
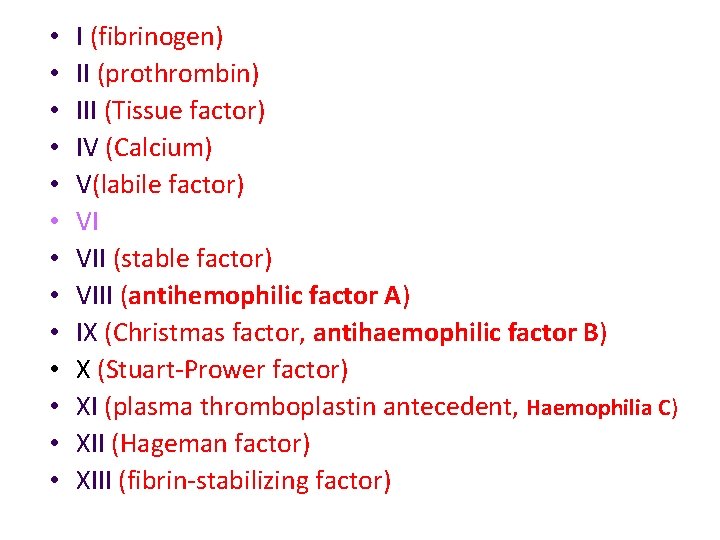
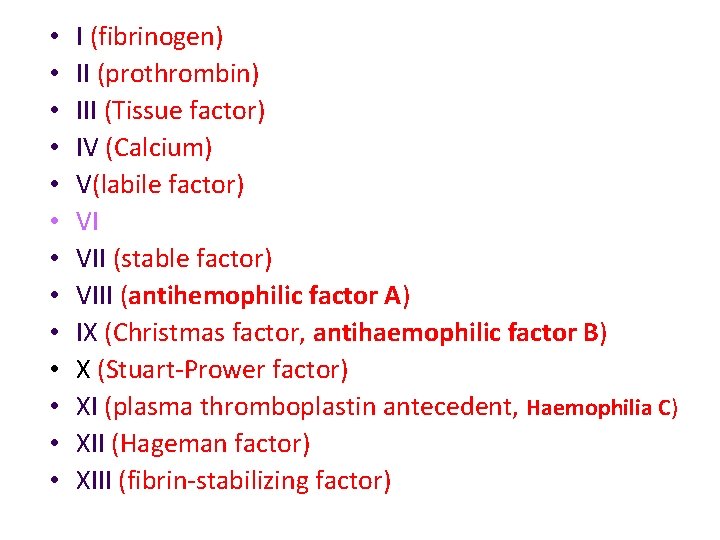
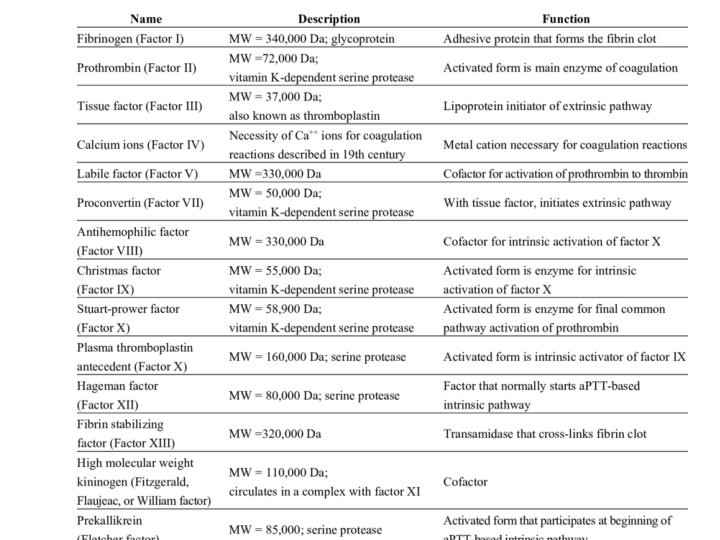
• • • • I (fibrinogen) II (prothrombin) III (Tissue factor) IV (Calcium) V(labile factor) VI VII (stable factor) VIII (antihemophilic factor A) IX (Christmas factor, antihaemophilic factor B) X (Stuart-Prower factor) XI (plasma thromboplastin antecedent, Haemophilia C) XII (Hageman factor) XIII (fibrin-stabilizing factor)
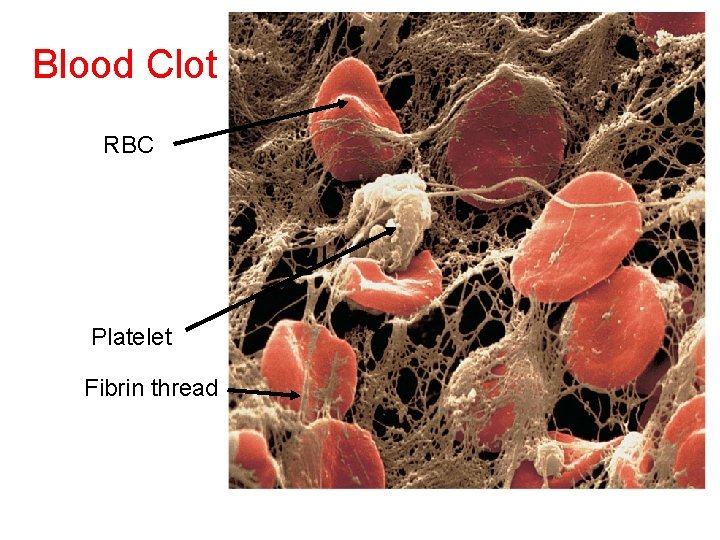
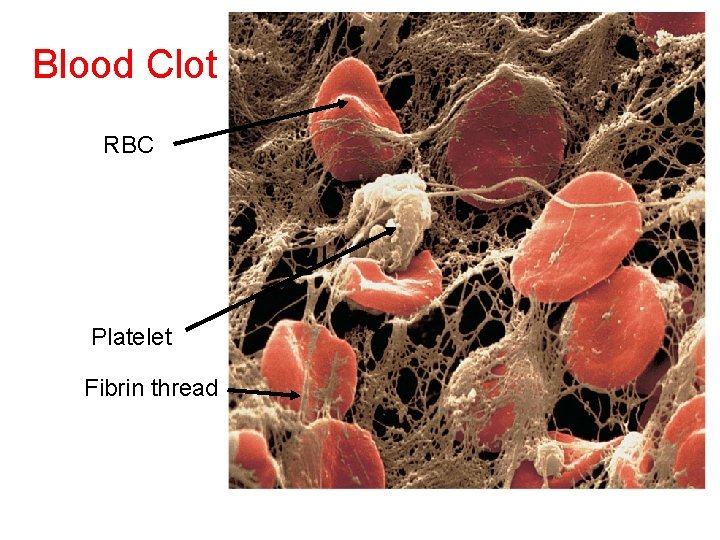
Blood Clot RBC Platelet Fibrin thread

Inside of a vessel SEM x 2, 500
Clot removal
Fibrinolysis • Enhance degradation of clots • Activation of endogenous protease • Plasminogen (inactive form) is converted to Plasmin (active form) • Plasmin breaks down fibrin clots

Fibrinolysis Plasminogen t. PA u. PA Fibrin Plasmin Fibrin Split Products (FSP)
Disorders of Hemostasis • Thrombosis or thromboembolytic disorders: undesirable clot formation • Bleeding disorders: abnormalities that prevent normal clot formation
Thromboembolytic Conditions • Prevented by – Aspirin • Antiprostaglandin that inhibits thromboxane A 2 – Heparin • Anticoagulant used clinically for pre- and postoperative cardiac care – Warfarin • Used for those prone to atrial fibrillation
Thrombocytopenia- too few platelets • causes spontaneous bleeding • due to suppression or destruction of bone marrow (e. g. , malignancy, radiation) – Platelet count <50, 000/mm 3 is diagnostic – Treated with transfusion of concentrated platelets

Impaired liver function – Inability to synthesize procoagulants – Causes include vitamin K deficiency, hepatitis, and cirrhosis – Liver disease can also prevent the liver from producing bile, impairing fat and vitamin K absorption

Hemophilia • Hemophilias include several similar hereditary bleeding disorders • Symptoms include prolonged bleeding, especially into joint cavities • Treated with plasma transfusions and injection of missing factors


Tests of Hemostasis • Bleeding Time • Coagulation Time • Prothrombin Time 21
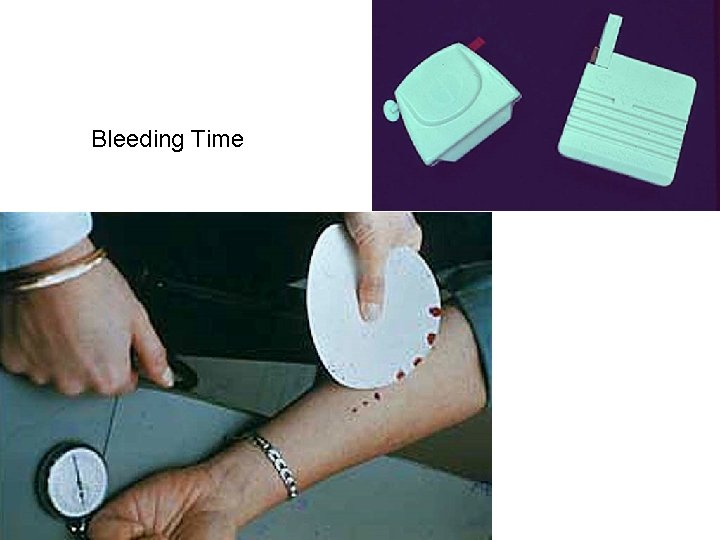
Bleeding Time • It is the time which passes between the formation of a small cut and the stoppage of bleeding from the cut of small blood vessel • (2 -5 minutes)

Coagulation Time • It is the time which passes between the start of bleeding and the formation of a clot • (4 -8 minutes)
Prothrombin Time • The test is done by precipitating calcium ions, so blood cannot coagulate • Calcium and thromboplastins are quickly added • The time taken by blood to clot is inversely proportional to prothrombin concentration in blood • (12 -30 seconds)
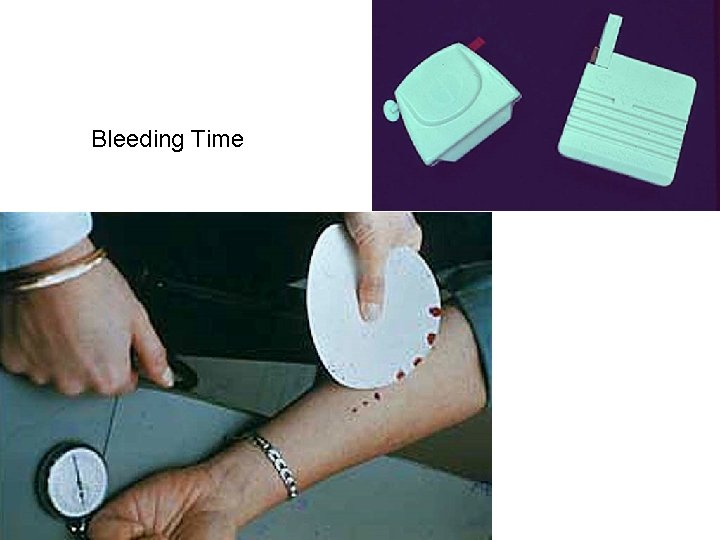
Bleeding Time