Haema Non Mal 1 Platelets Platelets are fragments

![Haema - Non Mal: 27 Thrombopoietin normal platelet count thrombocytopenia plasma TPO platelet [TPO] Haema - Non Mal: 27 Thrombopoietin normal platelet count thrombocytopenia plasma TPO platelet [TPO]](https://slidetodoc.com/presentation_image_h2/65c1291b5f40b7701c4cdd45781ffd79/image-27.jpg)

- Slides: 55
Haema - Non Mal: 1 Platelets • Platelets are fragments of cytoplasm of bone marrow megakaryocytes • Count 150 – 400 x 109/l • Major role in coagulation Shashi: 03/00
Haema - Non Mal: 2 Non-Malignant Platelets Disorders Shashi: 03/00
Haema - Non Mal: 3 Hemostasis Primary vs. Secondary vs. Tertiary • Primary Hemostasis • Platelet Plug formation • Dependent on normal platelet number & function • Initial manifestation of clot formation • Secondary Hemostasis • Activation of the clotting cascade • Deposition & Stabilization of fibrin • Tertiary Hemostasis • Dissolution of the fibrin clot • Dependent on Plasminogen Activation Shashi: 03/00
Haema - Non Mal: 4 PLT disorders: • Quantitative disorders: – “Penias” & “Philias” & Malignancies. • Qualitative disorders - function disorders – Congenital • Thrombasthenia, Bernad Soulier syndrome. – Acquired • Aspirin, Heparin. • Uremia, diabetes, hyperglobulinemia. Shashi: 03/00
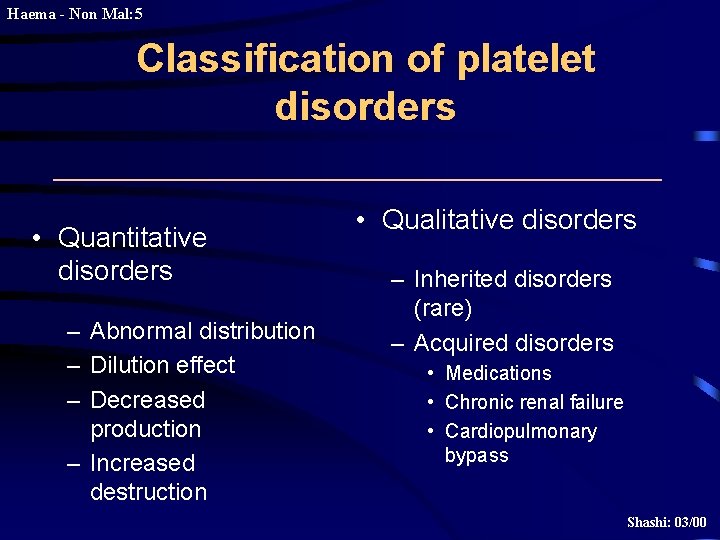
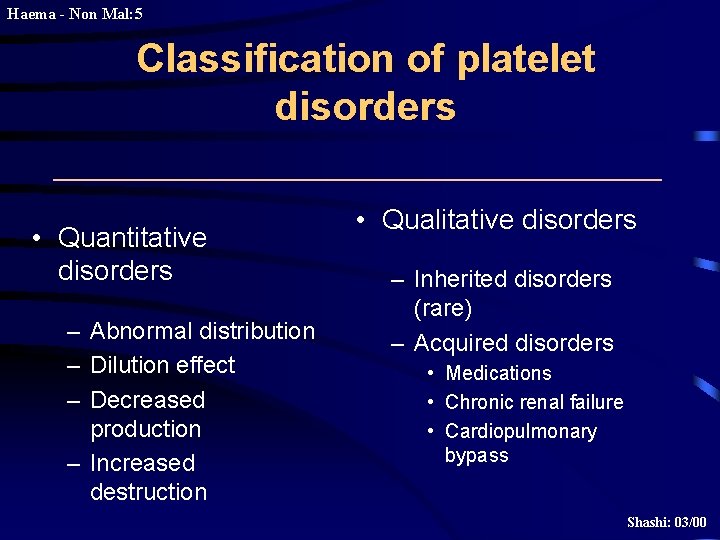
Haema - Non Mal: 5 Classification of platelet disorders • Quantitative disorders – Abnormal distribution – Dilution effect – Decreased production – Increased destruction • Qualitative disorders – Inherited disorders (rare) – Acquired disorders • Medications • Chronic renal failure • Cardiopulmonary bypass Shashi: 03/00

Haema - Non Mal: 6 Quantitative PLT disorders: • Decreased Production: – Marrow failures - aplasia, malignancy, drugs • Increased consumption: – DIC, TTP, Septicemia • Increased destruction: – Autoimmune, drugs, SLE, viral infections. • Dilutional thrombocytopenia: – Massive transfusions of stored blood. Shashi: 03/00
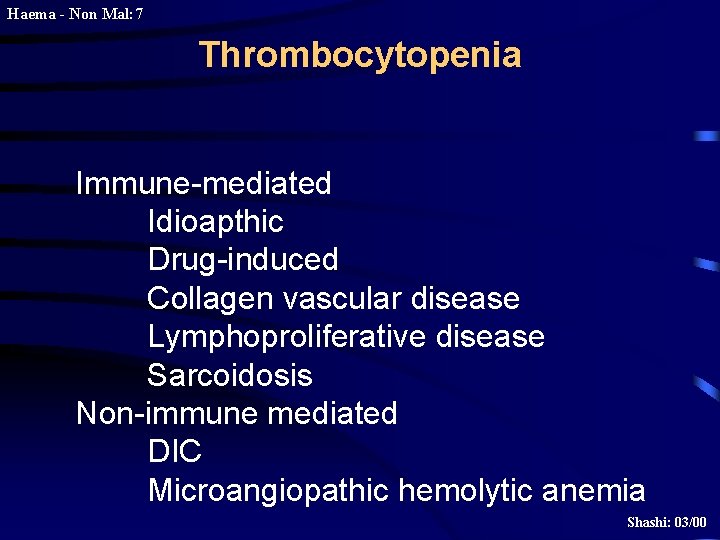
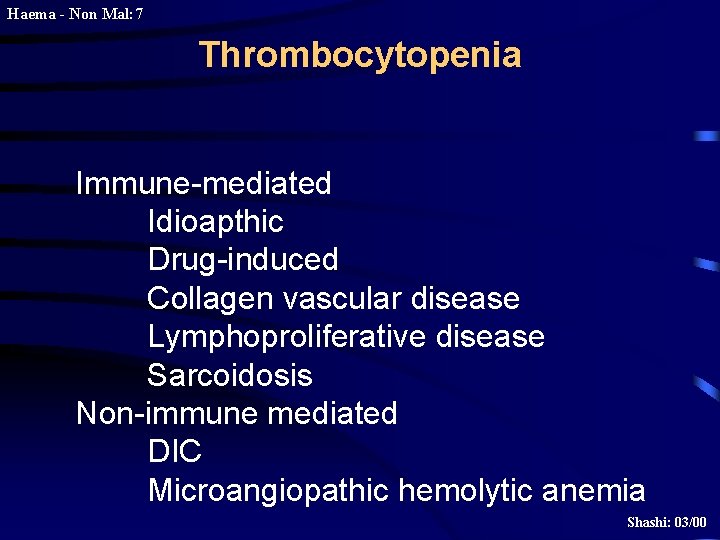
Haema - Non Mal: 7 Thrombocytopenia Immune-mediated Idioapthic Drug-induced Collagen vascular disease Lymphoproliferative disease Sarcoidosis Non-immune mediated DIC Microangiopathic hemolytic anemia Shashi: 03/00
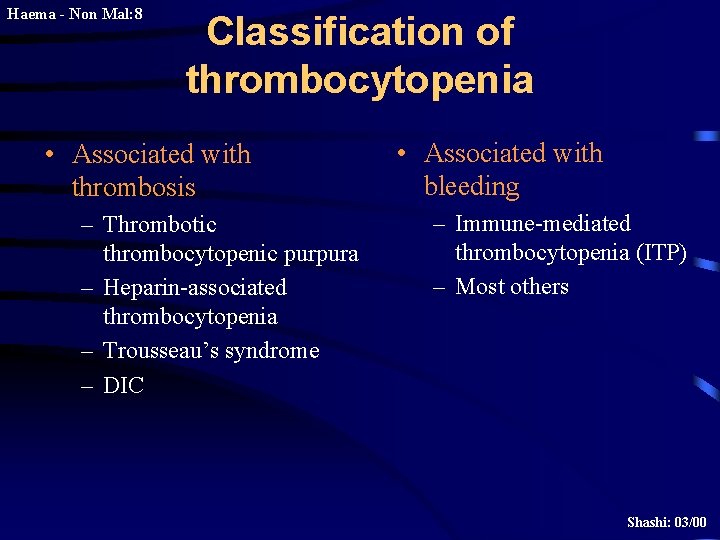
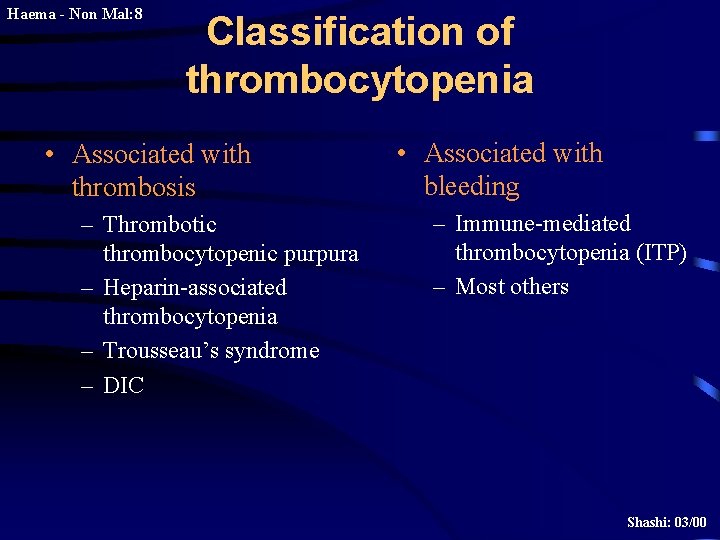
Haema - Non Mal: 8 Classification of thrombocytopenia • Associated with thrombosis – Thrombotic thrombocytopenic purpura – Heparin-associated thrombocytopenia – Trousseau’s syndrome – DIC • Associated with bleeding – Immune-mediated thrombocytopenia (ITP) – Most others Shashi: 03/00
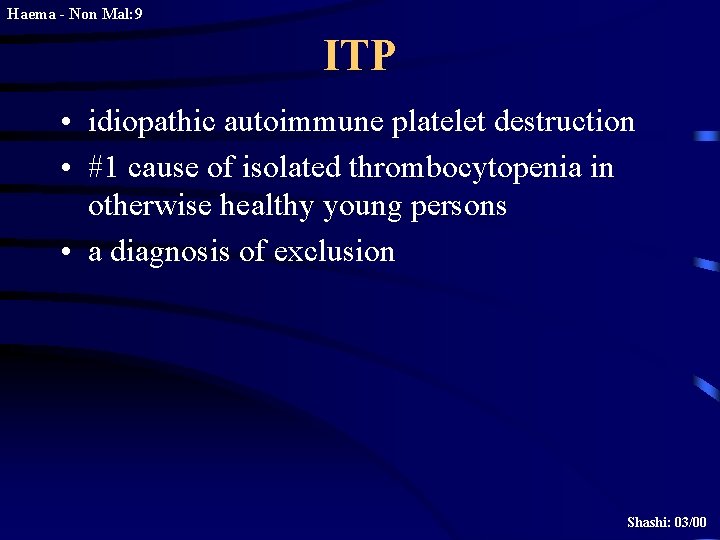
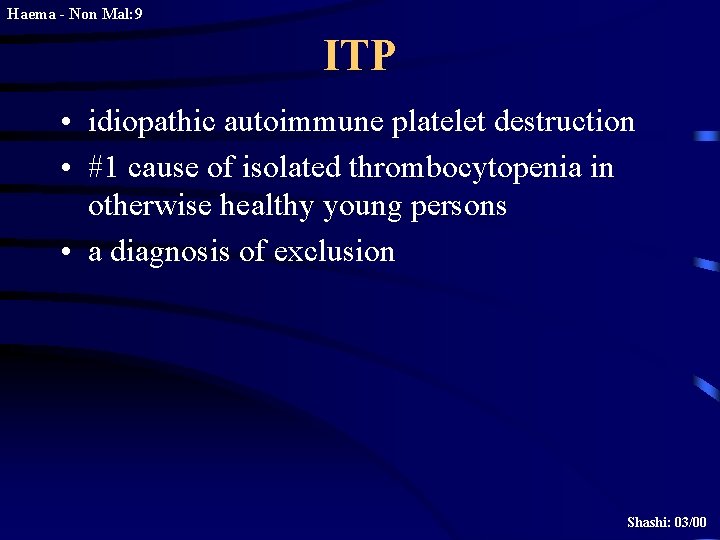
Haema - Non Mal: 9 ITP • idiopathic autoimmune platelet destruction • #1 cause of isolated thrombocytopenia in otherwise healthy young persons • a diagnosis of exclusion Shashi: 03/00
Haema - Non Mal: 10 ITP: Clinical features • occurs in any age or sex, but typically young female • can be preceeded by viral infection • signs and symptoms depend on platelet count • onset usually insidious Shashi: 03/00
Haema - Non Mal: 11 ITP: Laboratory features • • • ITP IS A DIAGNOSIS OF EXCLUSION no sensitive and specific test for ITP isolated thrombocytopenia increased MPV normal PT, PTT bone marrow investigation not essential in straightforward cases Shashi: 03/00
Haema - Non Mal: 12 ITP: Treatment Patient is not bleeding • plt > 50: Rx not indicated • plt 20 -50: Rx usually not needed, monitor closely • plt < 20: Rx indicated with one or more of: – prednisone – IVIG – anti-D if Rh pos – splenectomy if relapsing severe ITP (No role for prophylactic platelet transfusion, even if plt = 0) Shashi: 03/00
Haema - Non Mal: 13 ITP: Treatment Patient is bleeding • For serious bleeding (eg. CNS, retroperitoneal, GI) – Prednisone and IVIG – Transfuse platelets – consider urgent splenectomy – Provide other supportive/resuscitative care as needed Shashi: 03/00
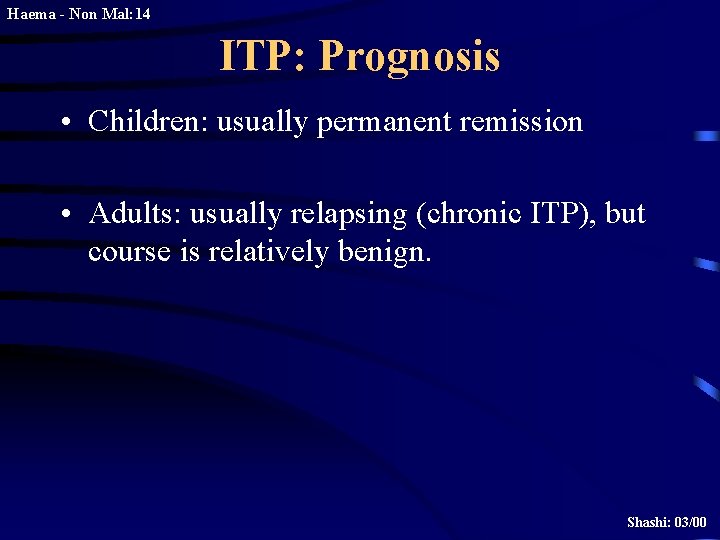
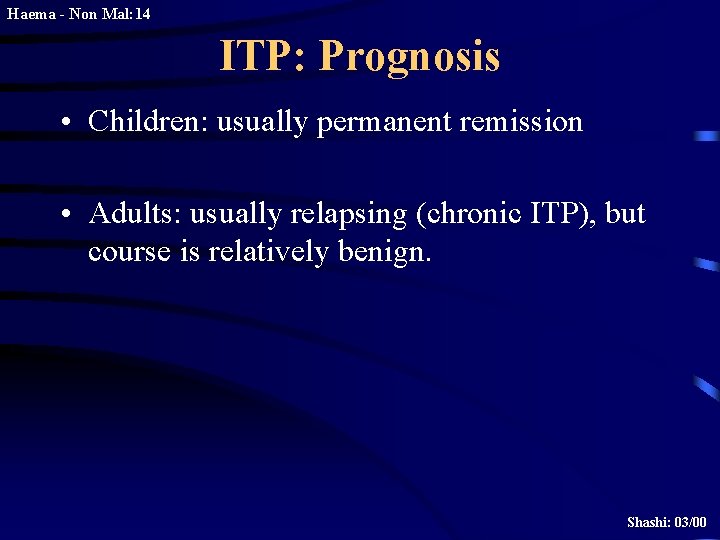
Haema - Non Mal: 14 ITP: Prognosis • Children: usually permanent remission • Adults: usually relapsing (chronic ITP), but course is relatively benign. Shashi: 03/00
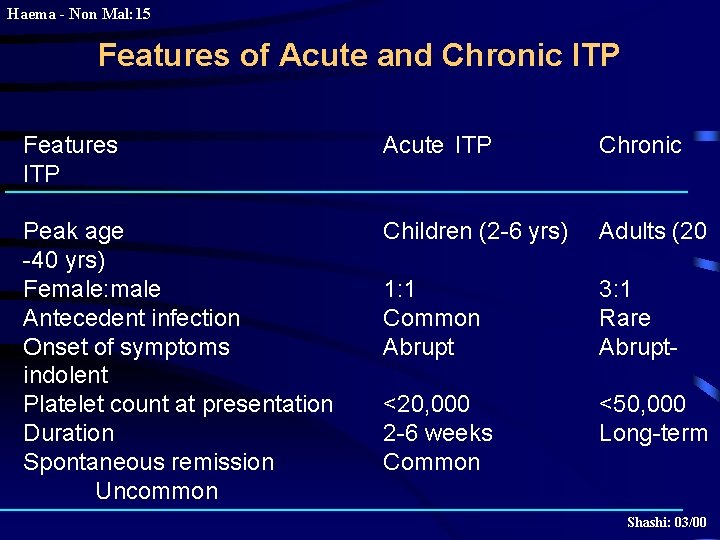
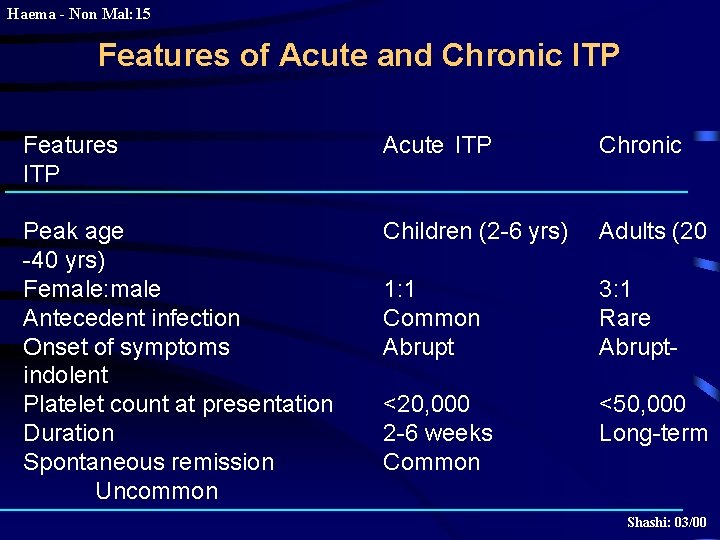
Haema - Non Mal: 15 Features of Acute and Chronic ITP Features ITP Acute ITP Chronic Peak age -40 yrs) Female: male Antecedent infection Onset of symptoms indolent Platelet count at presentation Duration Spontaneous remission Uncommon Children (2 -6 yrs) Adults (20 1: 1 Common Abrupt 3: 1 Rare Abrupt- <20, 000 2 -6 weeks Common <50, 000 Long-term Shashi: 03/00
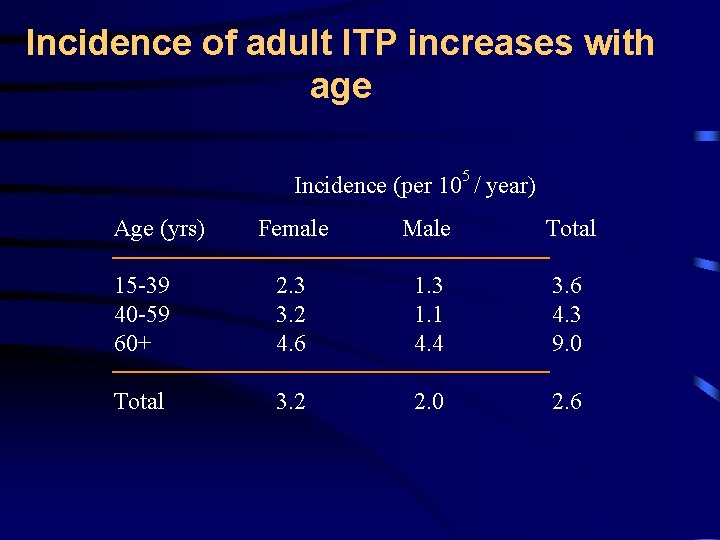
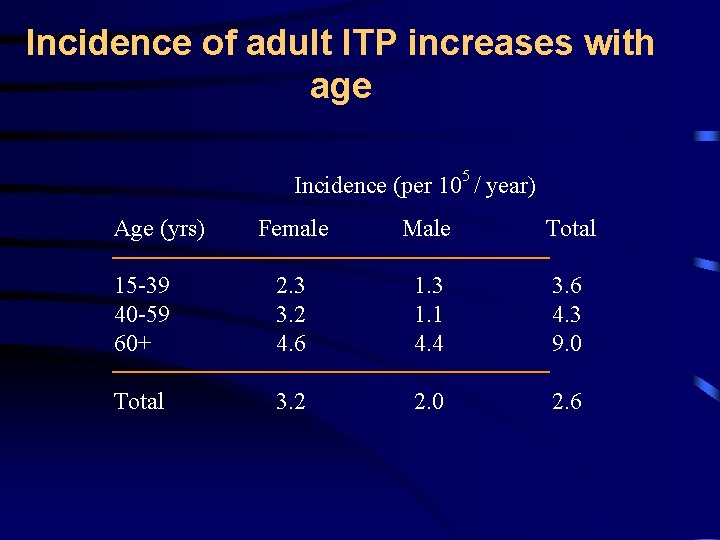
Incidence of adult ITP increases with age Incidence (per 105 / year) Age (yrs) Female Male Total 15 -39 40 -59 60+ 2. 3 3. 2 4. 6 1. 3 1. 1 4. 4 3. 6 4. 3 9. 0 Total 3. 2 2. 0 2. 6
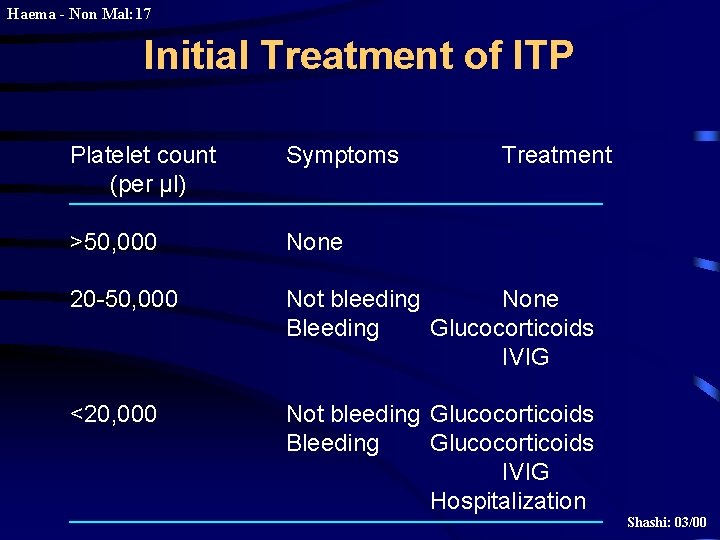
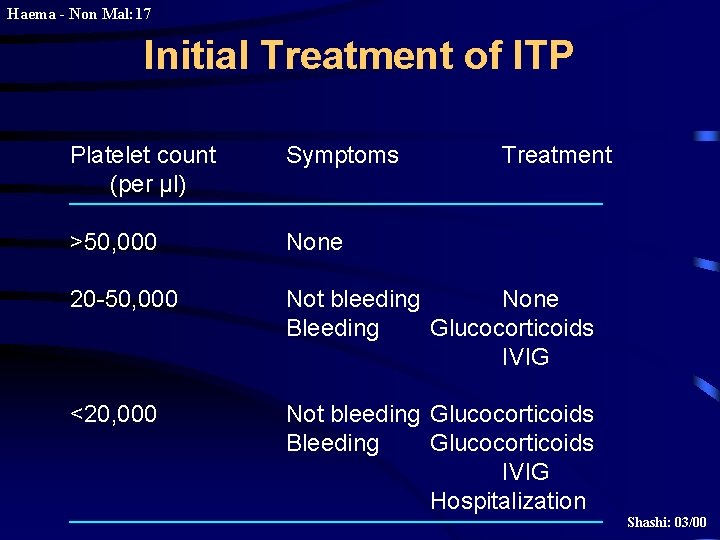
Haema - Non Mal: 17 Initial Treatment of ITP Platelet count (per µl) Symptoms Treatment >50, 000 None 20 -50, 000 Not bleeding None Bleeding Glucocorticoids IVIG <20, 000 Not bleeding Glucocorticoids Bleeding Glucocorticoids IVIG Hospitalization Shashi: 03/00
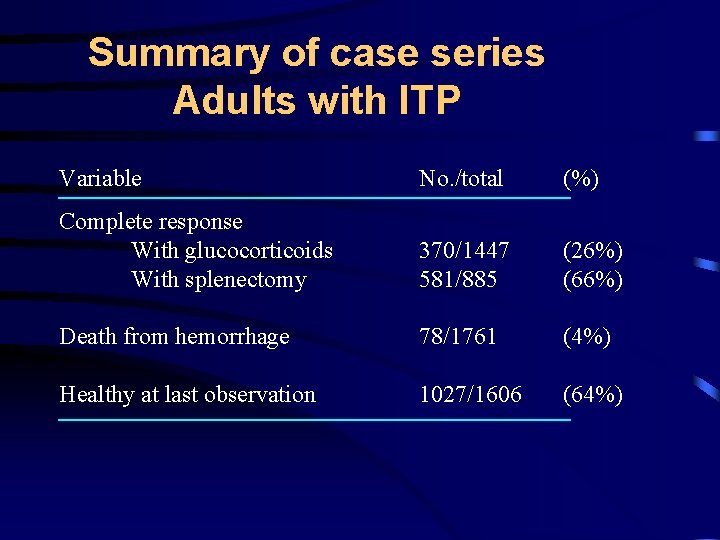
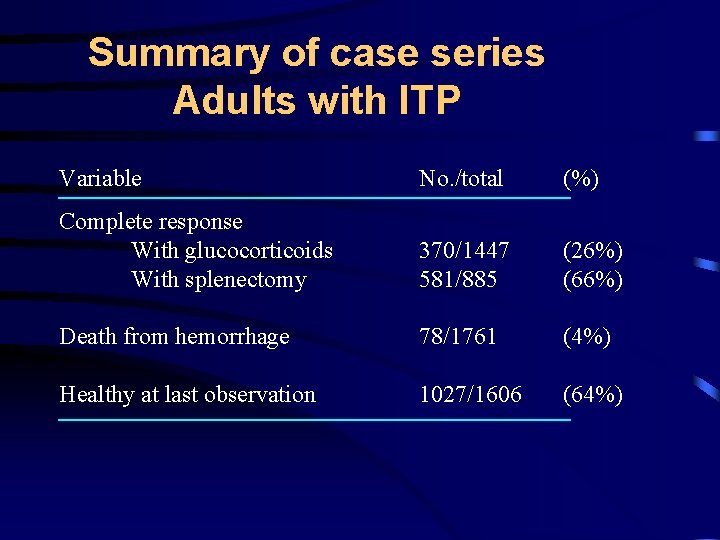
Summary of case series Adults with ITP Variable No. /total (%) Complete response With glucocorticoids With splenectomy 370/1447 581/885 (26%) (66%) Death from hemorrhage 78/1761 (4%) Healthy at last observation 1027/1606 (64%)
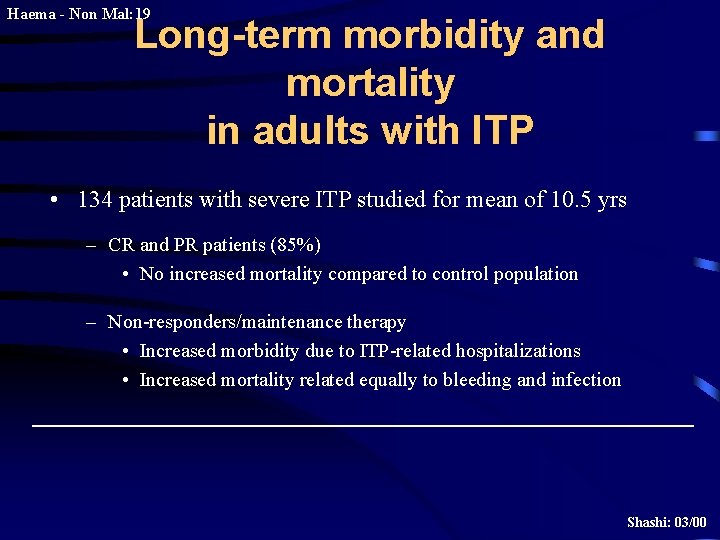
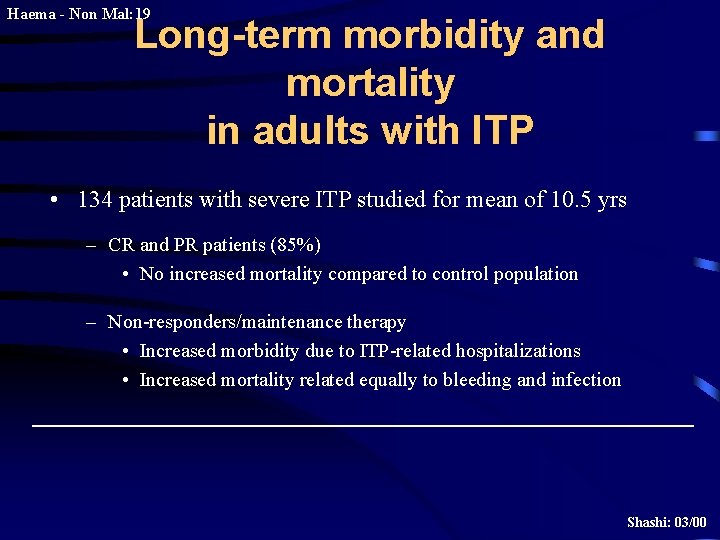
Haema - Non Mal: 19 Long-term morbidity and mortality in adults with ITP • 134 patients with severe ITP studied for mean of 10. 5 yrs – CR and PR patients (85%) • No increased mortality compared to control population – Non-responders/maintenance therapy • Increased morbidity due to ITP-related hospitalizations • Increased mortality related equally to bleeding and infection Shashi: 03/00
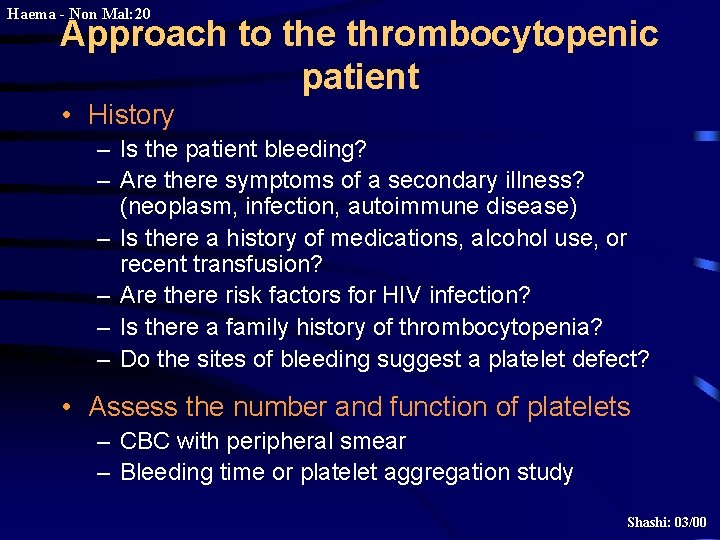
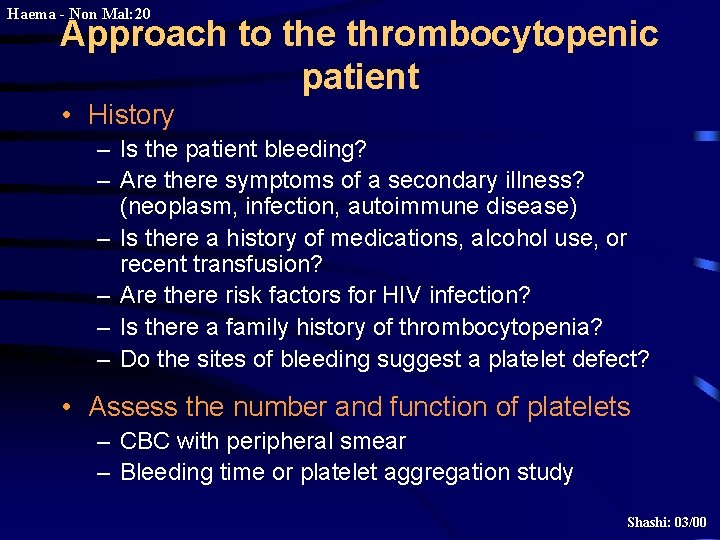
Haema - Non Mal: 20 Approach to the thrombocytopenic patient • History – Is the patient bleeding? – Are there symptoms of a secondary illness? (neoplasm, infection, autoimmune disease) – Is there a history of medications, alcohol use, or recent transfusion? – Are there risk factors for HIV infection? – Is there a family history of thrombocytopenia? – Do the sites of bleeding suggest a platelet defect? • Assess the number and function of platelets – CBC with peripheral smear – Bleeding time or platelet aggregation study Shashi: 03/00
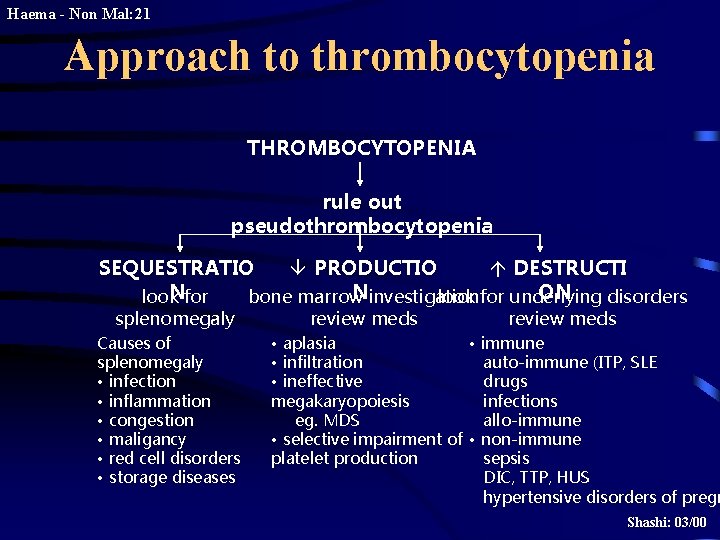
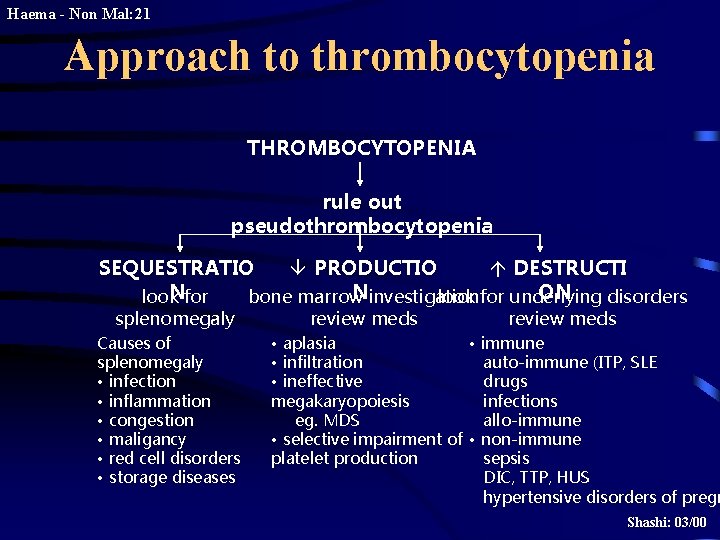
Haema - Non Mal: 21 Approach to thrombocytopenia THROMBOCYTOPENIA rule out pseudothrombocytopenia SEQUESTRATIO â PRODUCTIO á DESTRUCTI Nfor Ninvestigation ON look bone marrow look for underlying disorders splenomegaly Causes of splenomegaly • infection • inflammation • congestion • maligancy • red cell disorders • storage diseases review meds • aplasia • immune • infiltration auto-immune (ITP, SLE • ineffective drugs megakaryopoiesis infections eg. MDS allo-immune • selective impairment of • non-immune platelet production sepsis DIC, TTP, HUS hypertensive disorders of pregn Shashi: 03/00
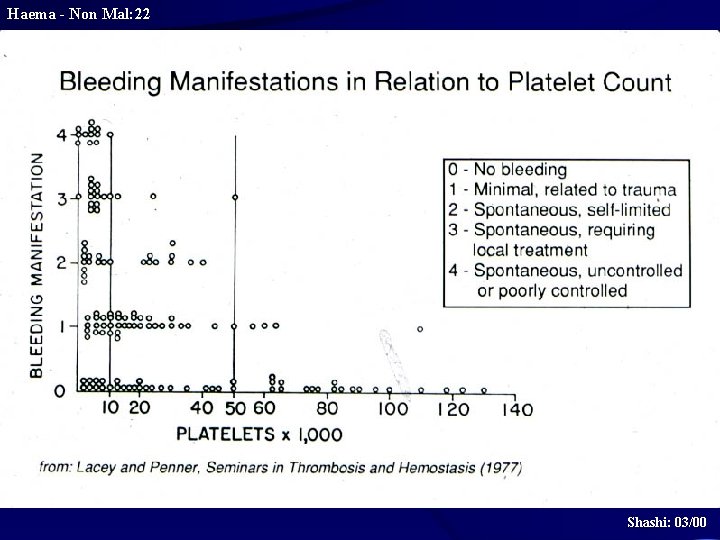
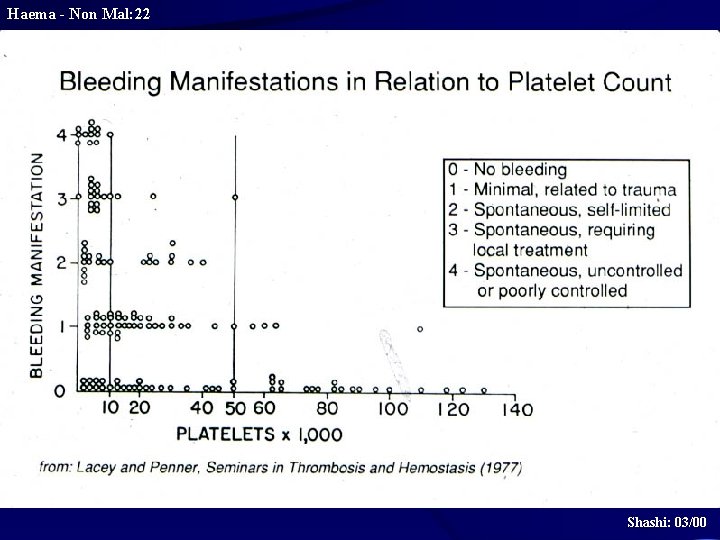
Haema - Non Mal: 22 Shashi: 03/00
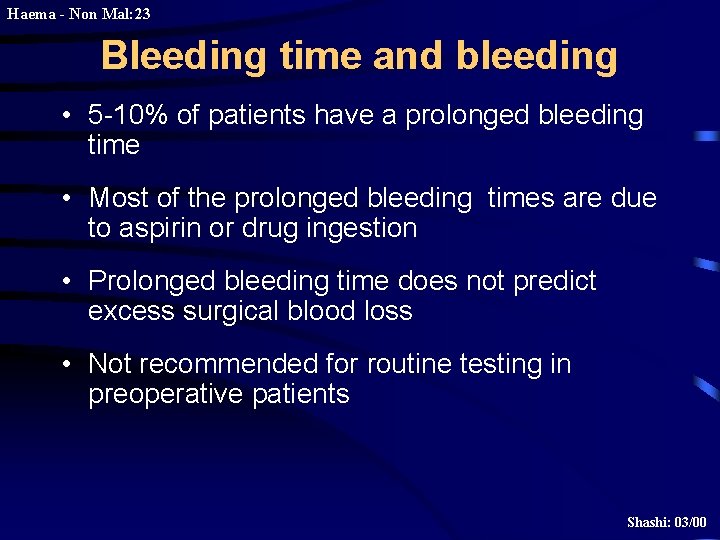
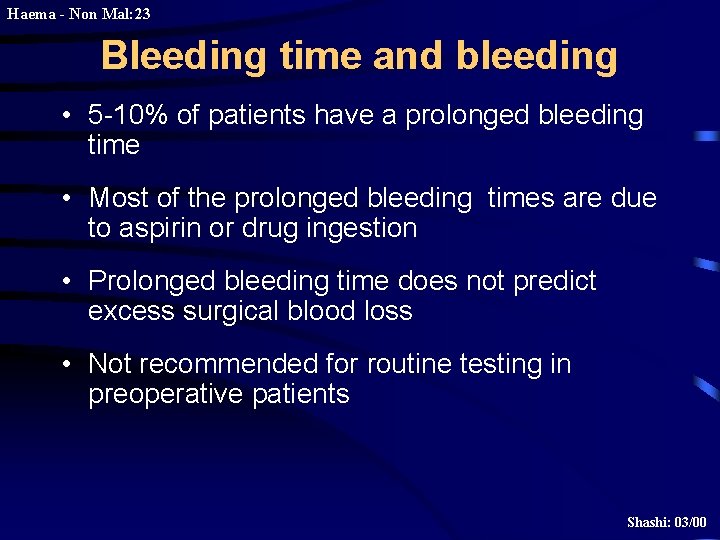
Haema - Non Mal: 23 Bleeding time and bleeding • 5 -10% of patients have a prolonged bleeding time • Most of the prolonged bleeding times are due to aspirin or drug ingestion • Prolonged bleeding time does not predict excess surgical blood loss • Not recommended for routine testing in preoperative patients Shashi: 03/00
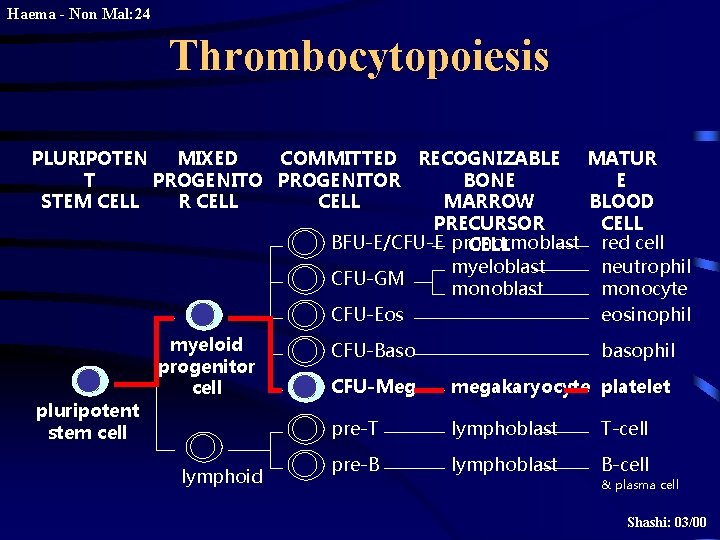
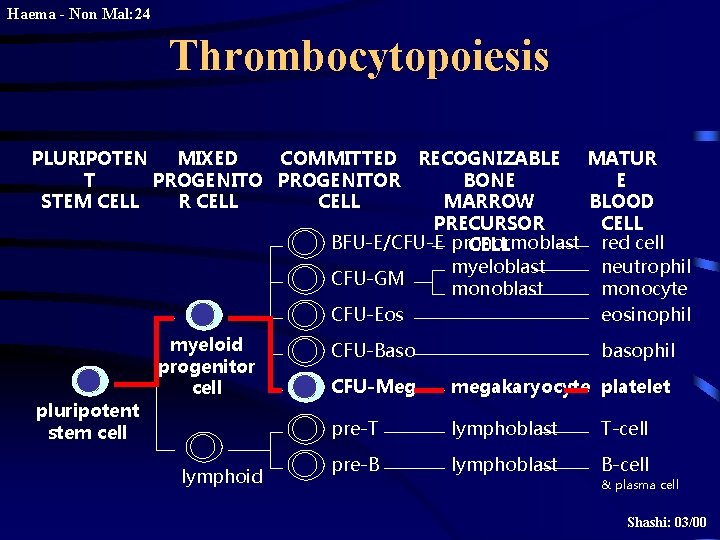
Haema - Non Mal: 24 Thrombocytopoiesis PLURIPOTEN MIXED COMMITTED RECOGNIZABLE MATUR T PROGENITOR BONE E STEM CELL R CELL MARROW BLOOD PRECURSOR CELL BFU-E/CFU-E pronormoblast red cell CELL myeloblast neutrophil CFU-GM monoblast monocyte CFU-Eos eosinophil pluripotent stem cell myeloid progenitor cell lymphoid CFU-Baso basophil CFU-Meg megakaryocyte platelet pre-T lymphoblast T-cell pre-B lymphoblast B-cell & plasma cell Shashi: 03/00
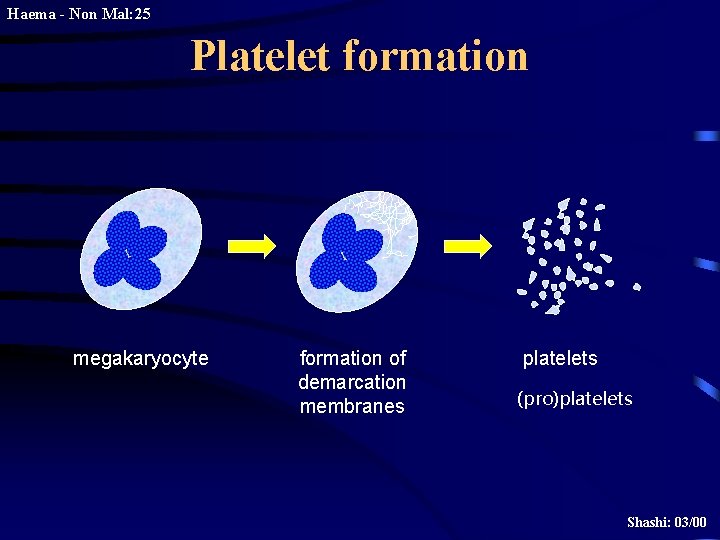
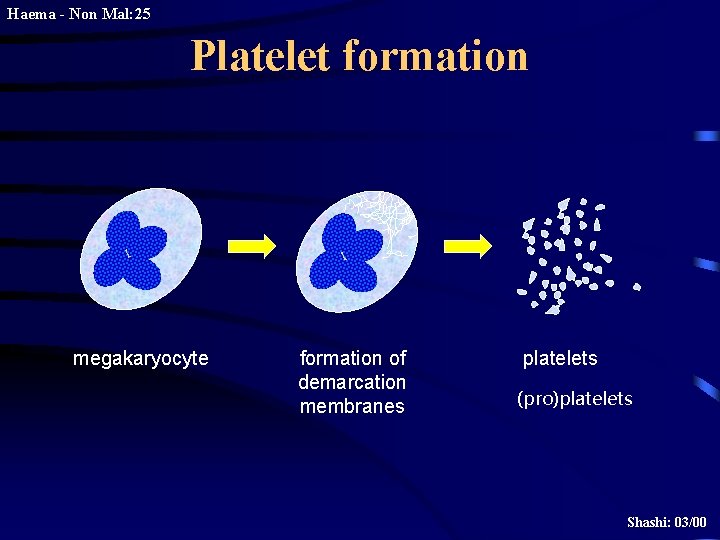
Haema - Non Mal: 25 Platelet formation megakaryocyte formation of demarcation membranes platelets (pro)platelets Shashi: 03/00
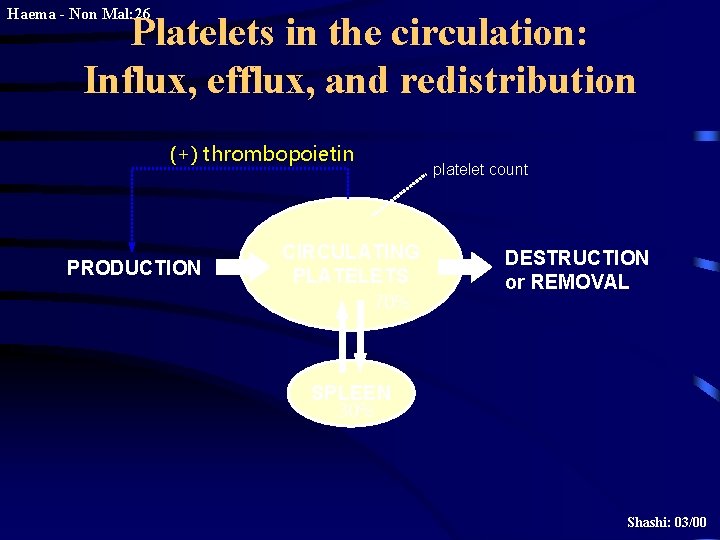
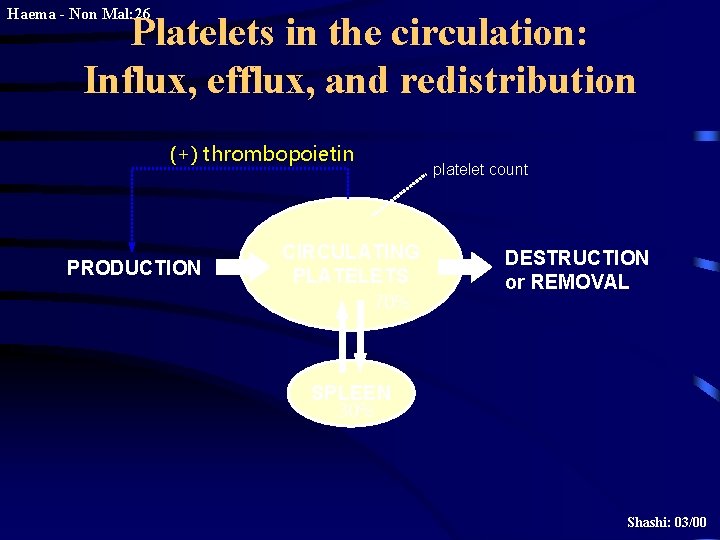
Haema - Non Mal: 26 Platelets in the circulation: Influx, efflux, and redistribution (+) thrombopoietin PRODUCTION platelet count CIRCULATING PLATELETS 70% DESTRUCTION or REMOVAL SPLEEN 30% Shashi: 03/00
![Haema Non Mal 27 Thrombopoietin normal platelet count thrombocytopenia plasma TPO platelet TPO Haema - Non Mal: 27 Thrombopoietin normal platelet count thrombocytopenia plasma TPO platelet [TPO]](https://slidetodoc.com/presentation_image_h2/65c1291b5f40b7701c4cdd45781ffd79/image-27.jpg)
Haema - Non Mal: 27 Thrombopoietin normal platelet count thrombocytopenia plasma TPO platelet [TPO] total [TPO] normal norm al increased free Shashi: 03/00
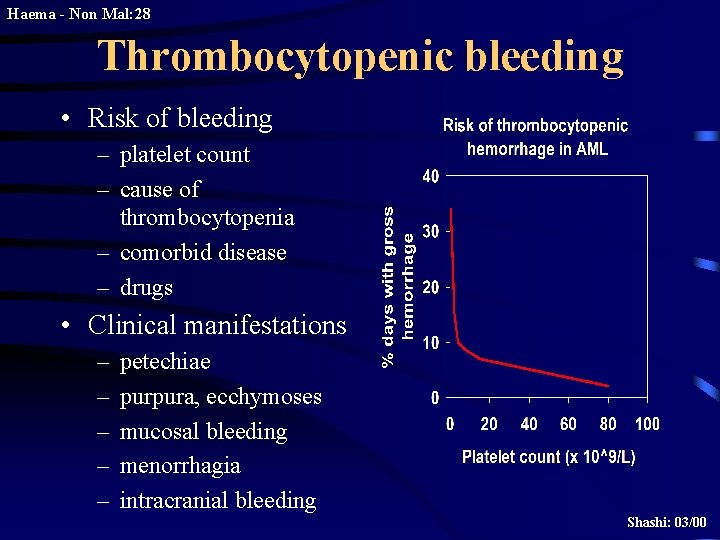
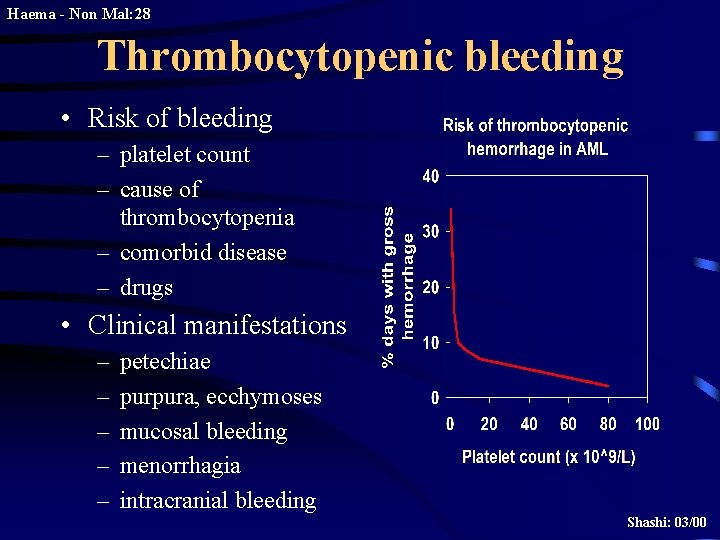
Haema - Non Mal: 28 Thrombocytopenic bleeding • Risk of bleeding – platelet count – cause of thrombocytopenia – comorbid disease – drugs • Clinical manifestations – – – petechiae purpura, ecchymoses mucosal bleeding menorrhagia intracranial bleeding Shashi: 03/00
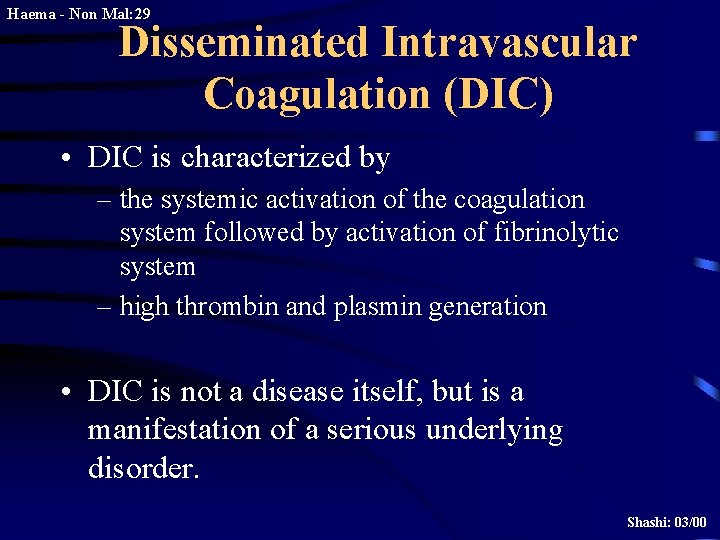
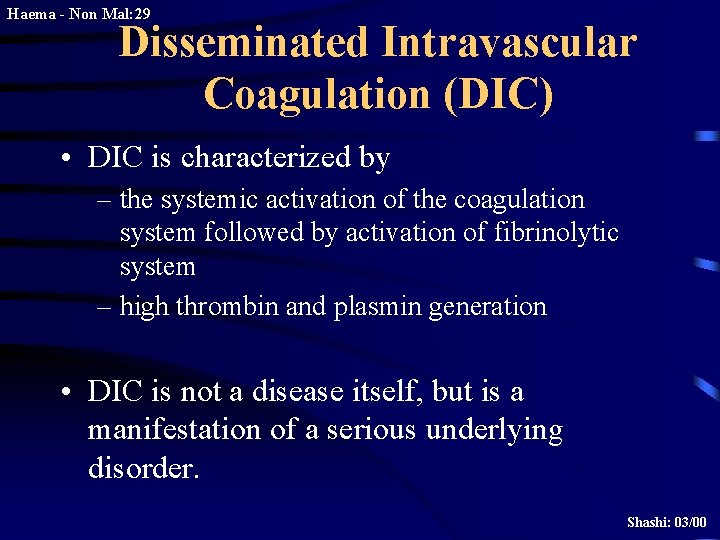
Haema - Non Mal: 29 Disseminated Intravascular Coagulation (DIC) • DIC is characterized by – the systemic activation of the coagulation system followed by activation of fibrinolytic system – high thrombin and plasmin generation • DIC is not a disease itself, but is a manifestation of a serious underlying disorder. Shashi: 03/00
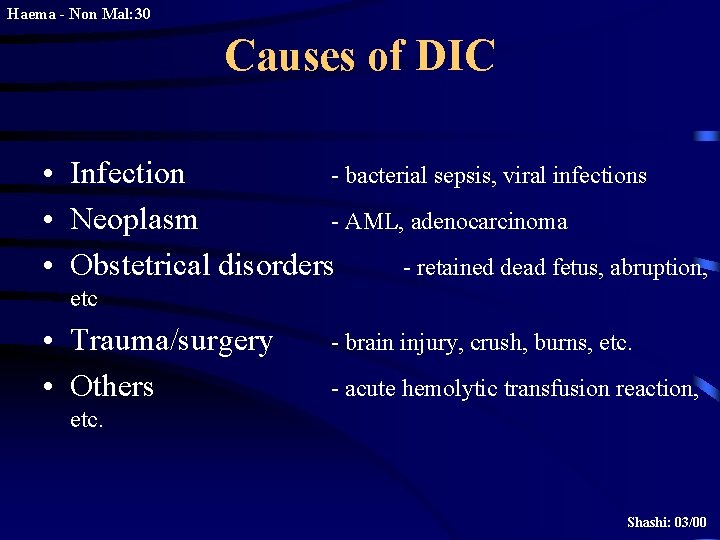
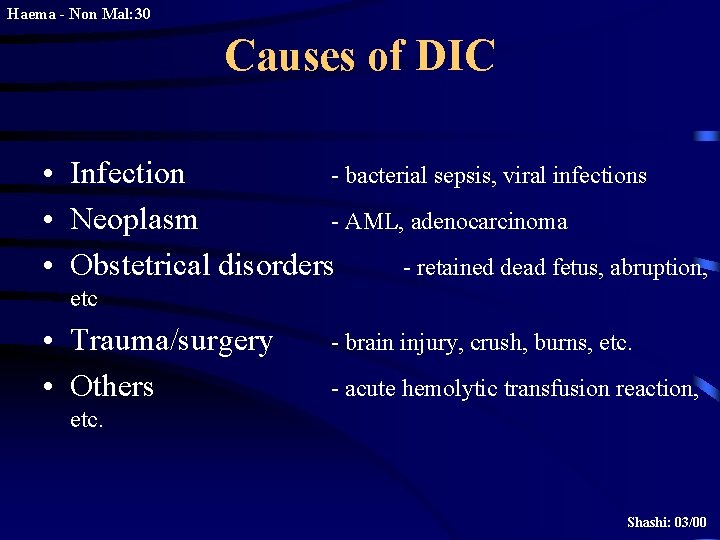
Haema - Non Mal: 30 Causes of DIC • Infection - bacterial sepsis, viral infections • Neoplasm - AML, adenocarcinoma • Obstetrical disorders - retained dead fetus, abruption, etc • Trauma/surgery • Others - brain injury, crush, burns, etc. - acute hemolytic transfusion reaction, etc. Shashi: 03/00
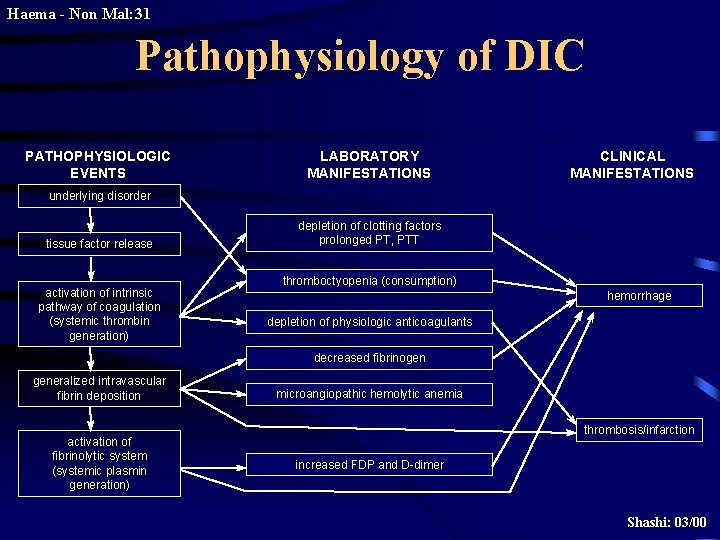
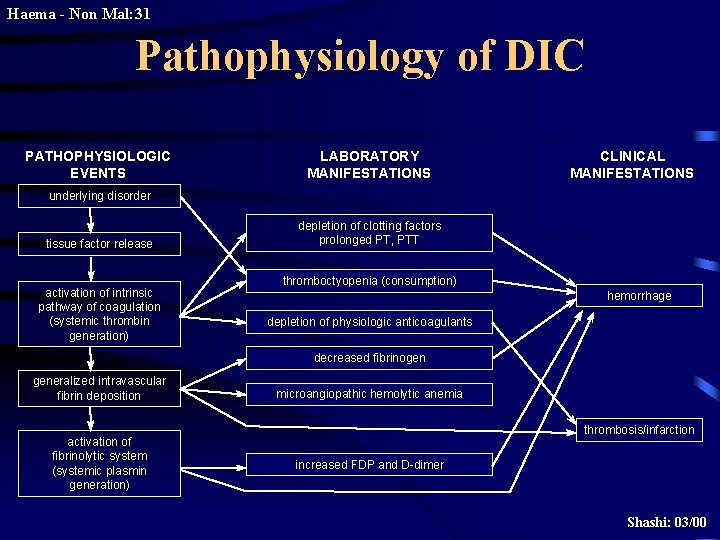
Haema - Non Mal: 31 Pathophysiology of DIC PATHOPHYSIOLOGIC EVENTS LABORATORY MANIFESTATIONS CLINICAL MANIFESTATIONS underlying disorder tissue factor release activation of intrinsic pathway of coagulation (systemic thrombin generation) depletion of clotting factors prolonged PT, PTT thromboctyopenia (consumption) hemorrhage depletion of physiologic anticoagulants decreased fibrinogen generalized intravascular fibrin deposition activation of fibrinolytic system (systemic plasmin generation) microangiopathic hemolytic anemia thrombosis/infarction increased FDP and D-dimer Shashi: 03/00
Haema - Non Mal: 32 Treatment of DIC • treat the underlying disease • replacement therapy – cryoprecipitate – FFP – platelet concentrate – packed red cells • consider additional pharmacologic therapy – controversial or investigational agents • AT, APC, PC concentrate, heparin, antifibrinolytic agents. Shashi: 03/00
Thrombasthenia
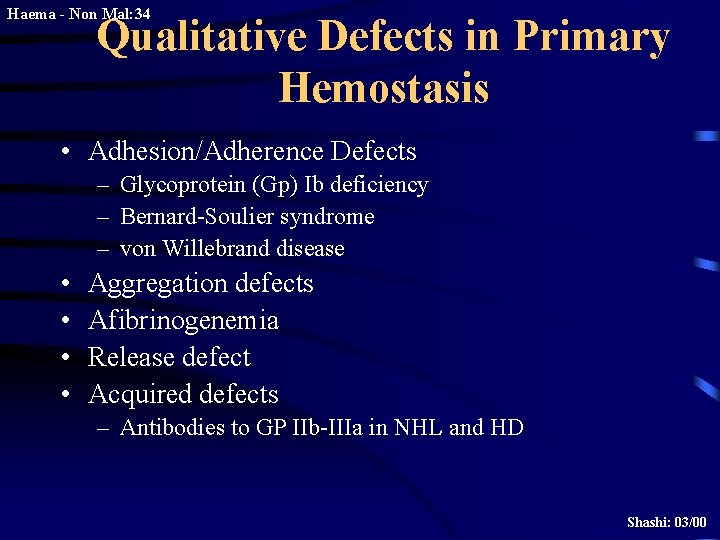
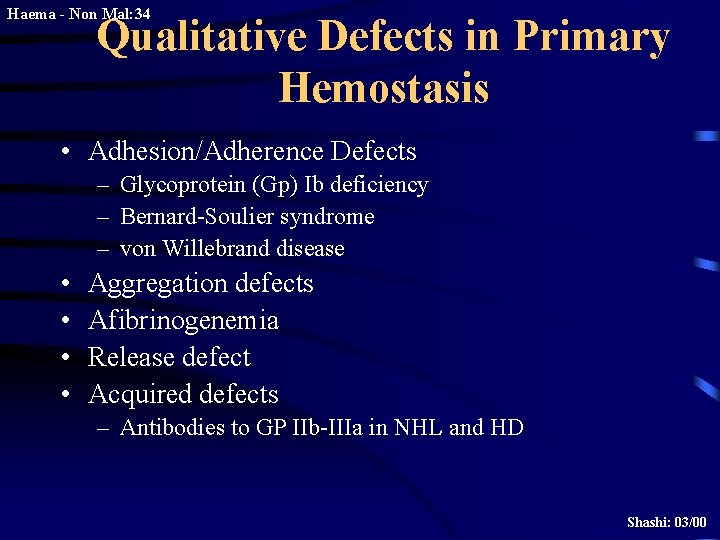
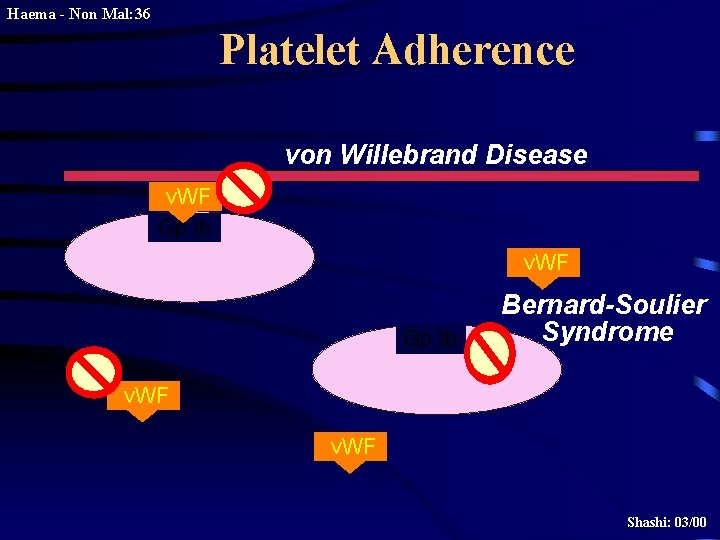
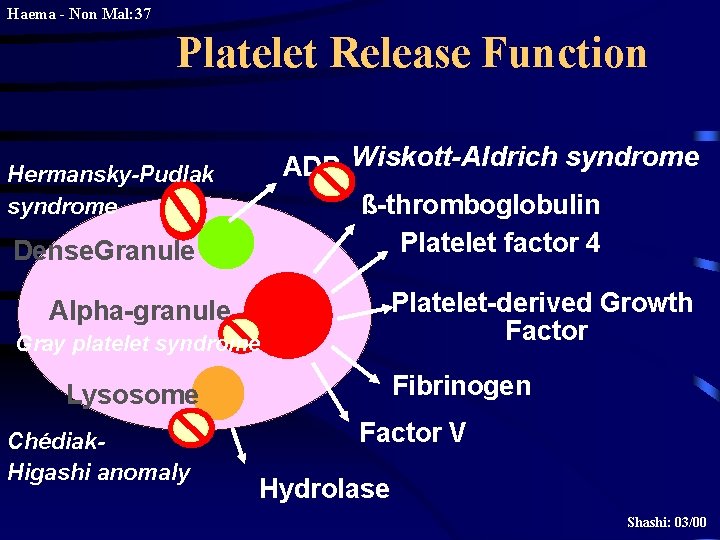
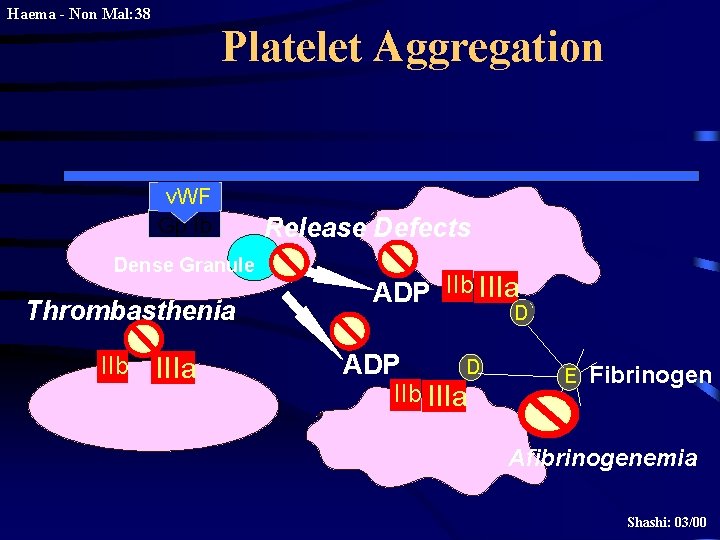
Haema - Non Mal: 34 Qualitative Defects in Primary Hemostasis • Adhesion/Adherence Defects – Glycoprotein (Gp) Ib deficiency – Bernard-Soulier syndrome – von Willebrand disease • • Aggregation defects Afibrinogenemia Release defect Acquired defects – Antibodies to GP IIb-IIIa in NHL and HD Shashi: 03/00
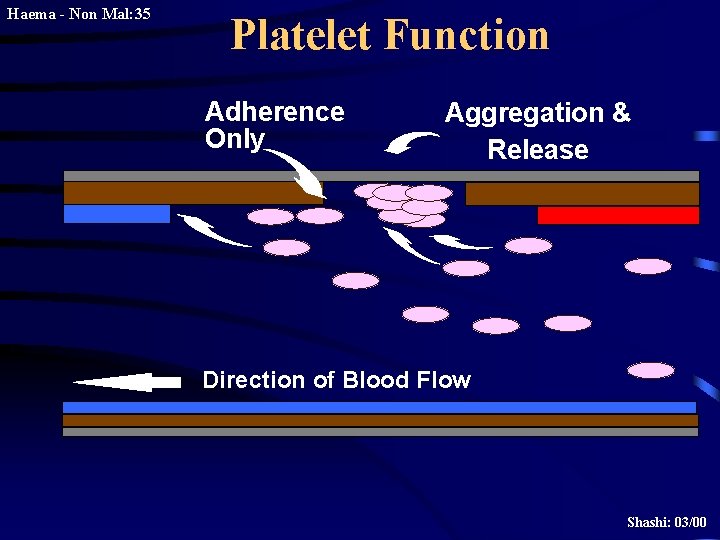
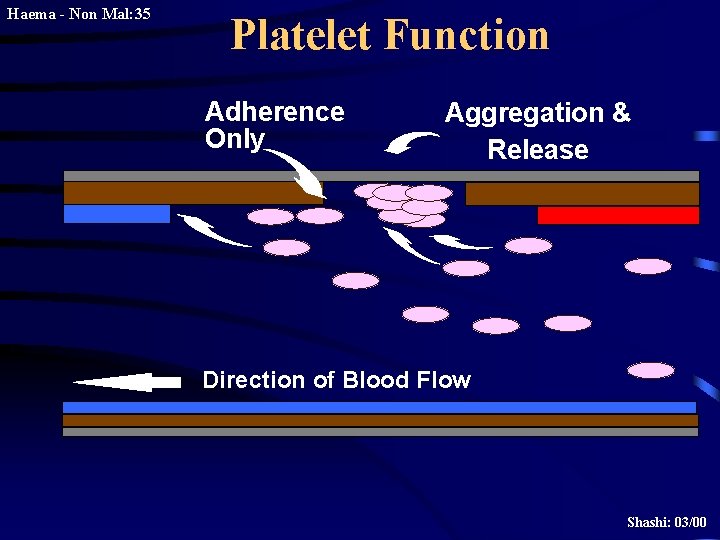
Haema - Non Mal: 35 Platelet Function Adherence Only Aggregation & Release Direction of Blood Flow Shashi: 03/00
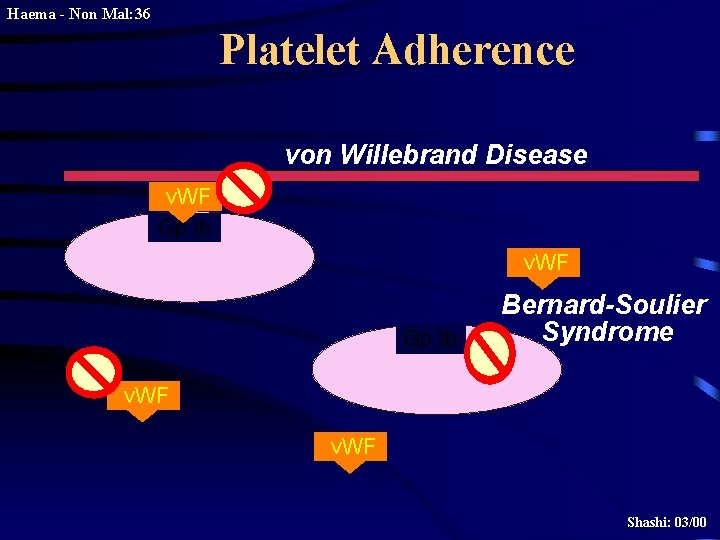
Haema - Non Mal: 36 Platelet Adherence von Willebrand Disease v. WF Gp Ib Bernard-Soulier Syndrome v. WF Shashi: 03/00
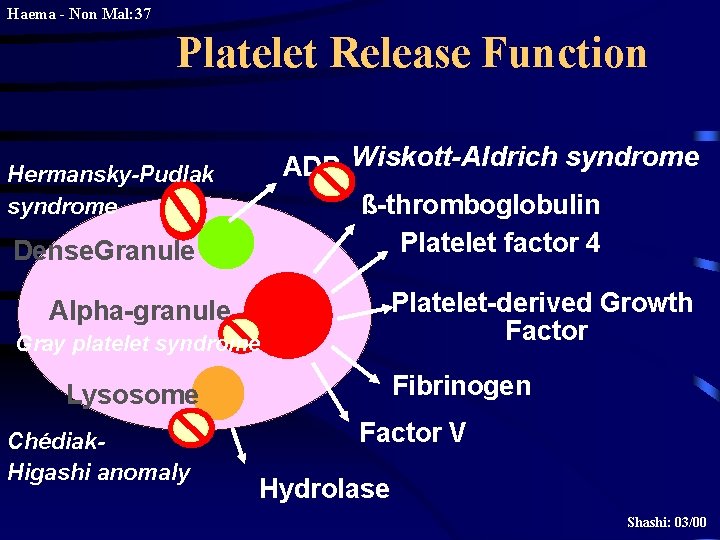
Haema - Non Mal: 37 Platelet Release Function ADP Wiskott-Aldrich syndrome ß-thromboglobulin Platelet factor 4 Hermansky-Pudlak syndrome Dense. Granule Platelet-derived Growth Factor Alpha-granule Gray platelet syndrome Fibrinogen Lysosome Chédiak. Higashi anomaly Factor V Hydrolase Shashi: 03/00
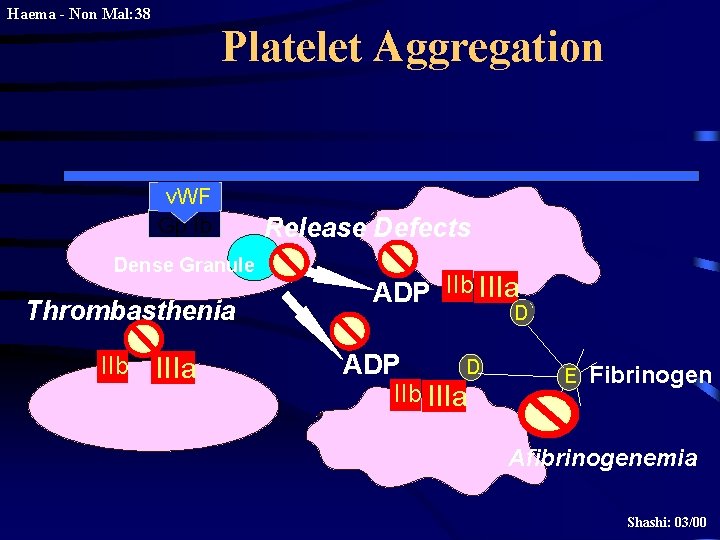
Haema - Non Mal: 38 Platelet Aggregation v. WF Gp Ib Dense Granule Thrombasthenia IIb IIIa Release Defects ADP IIb IIIa D D ADP D IIb IIIa E Fibrinogen Afibrinogenemia Shashi: 03/00
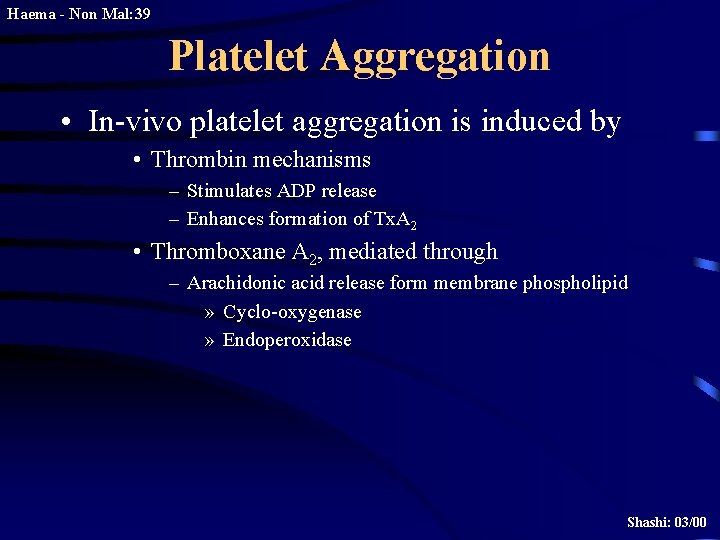
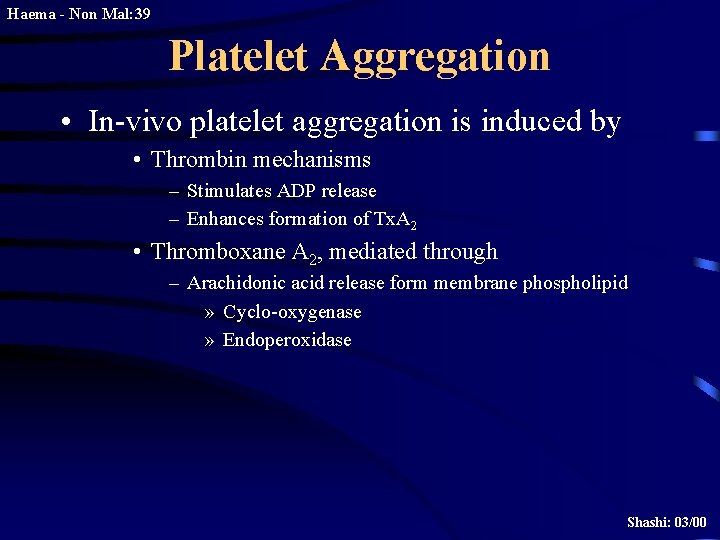
Haema - Non Mal: 39 Platelet Aggregation • In-vivo platelet aggregation is induced by • Thrombin mechanisms – Stimulates ADP release – Enhances formation of Tx. A 2 • Thromboxane A 2, mediated through – Arachidonic acid release form membrane phospholipid » Cyclo-oxygenase » Endoperoxidase Shashi: 03/00
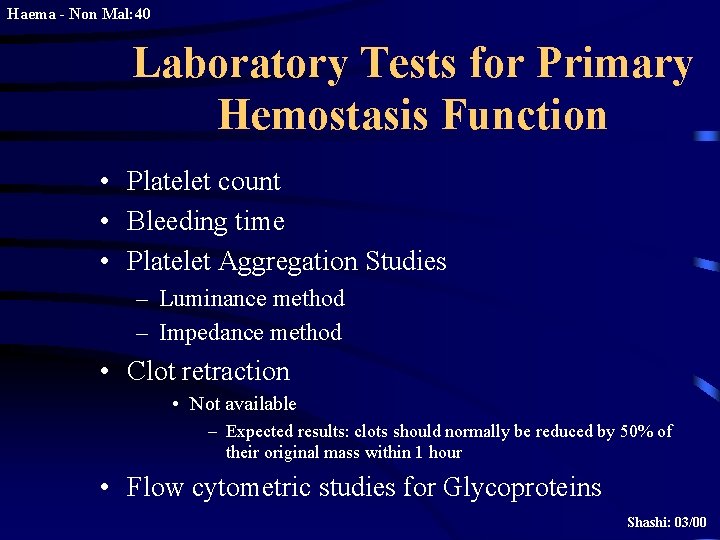
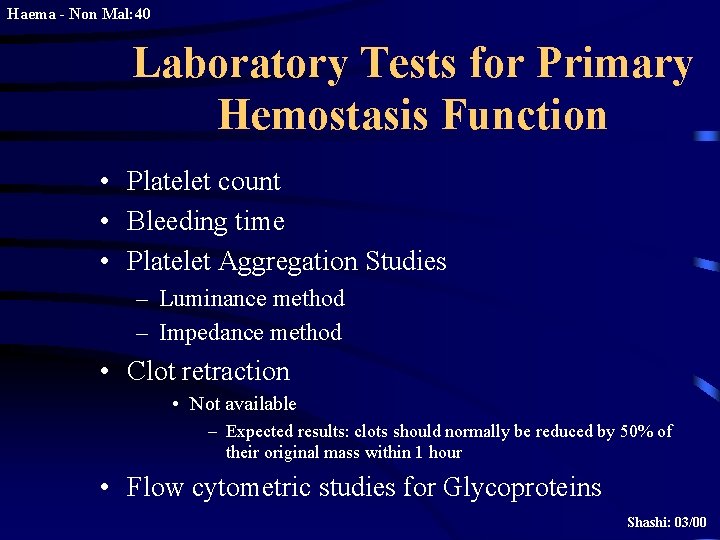
Haema - Non Mal: 40 Laboratory Tests for Primary Hemostasis Function • Platelet count • Bleeding time • Platelet Aggregation Studies – Luminance method – Impedance method • Clot retraction • Not available – Expected results: clots should normally be reduced by 50% of their original mass within 1 hour • Flow cytometric studies for Glycoproteins Shashi: 03/00
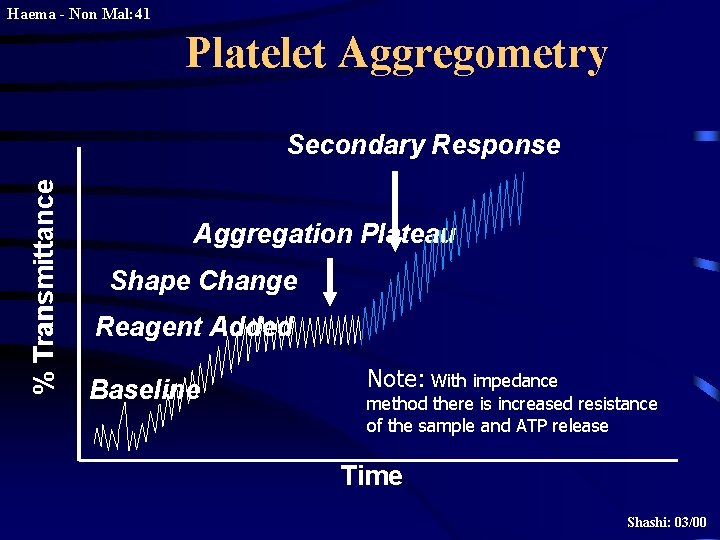
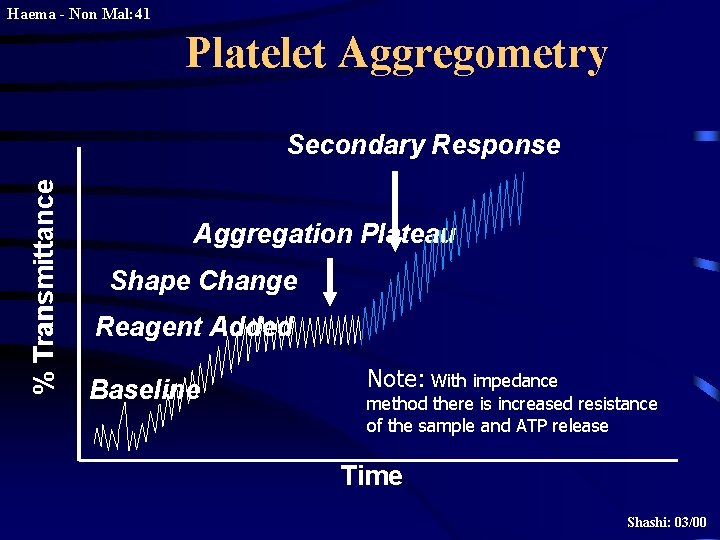
Haema - Non Mal: 41 Platelet Aggregometry % Transmittance Secondary Response Aggregation Plateau Shape Change Reagent Added Baseline Note: With impedance method there is increased resistance of the sample and ATP release Time Shashi: 03/00
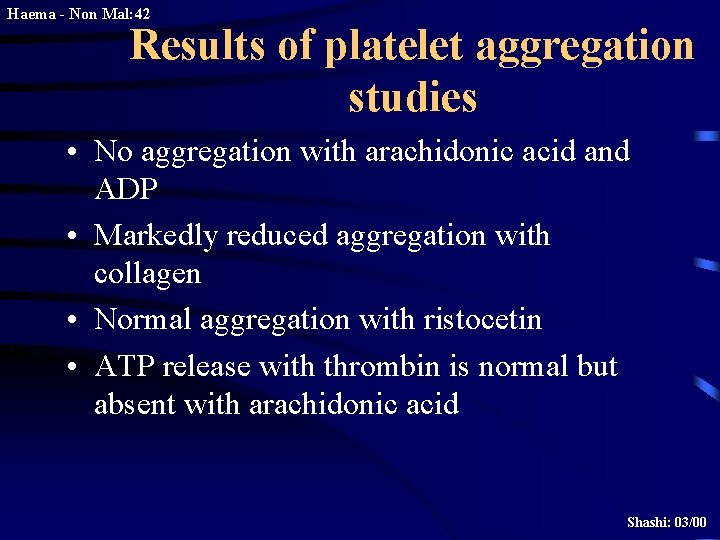
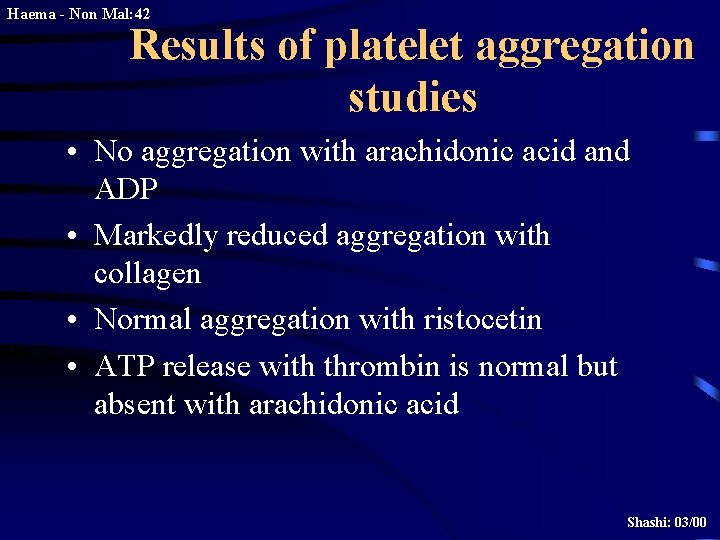
Haema - Non Mal: 42 Results of platelet aggregation studies • No aggregation with arachidonic acid and ADP • Markedly reduced aggregation with collagen • Normal aggregation with ristocetin • ATP release with thrombin is normal but absent with arachidonic acid Shashi: 03/00
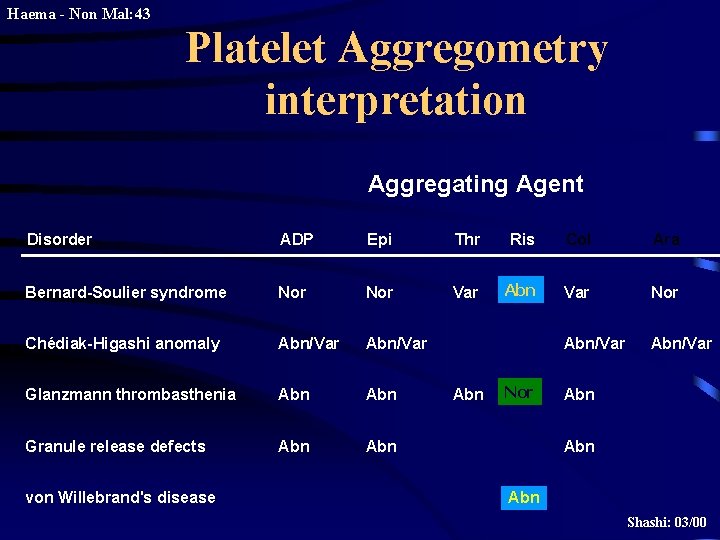
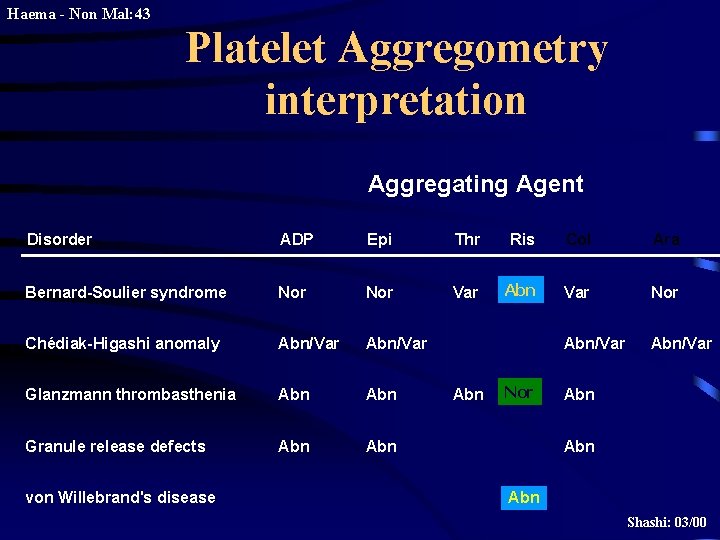
Haema - Non Mal: 43 Platelet Aggregometry interpretation Aggregating Agent Disorder ADP Epi Thr Ris Col Ara Bernard-Soulier syndrome Nor Var Abn Var Nor Chédiak-Higashi anomaly Abn/Var Glanzmann thrombasthenia Abn Granule release defects Abn von Willebrand's disease Abn Nor Abn Abn Shashi: 03/00
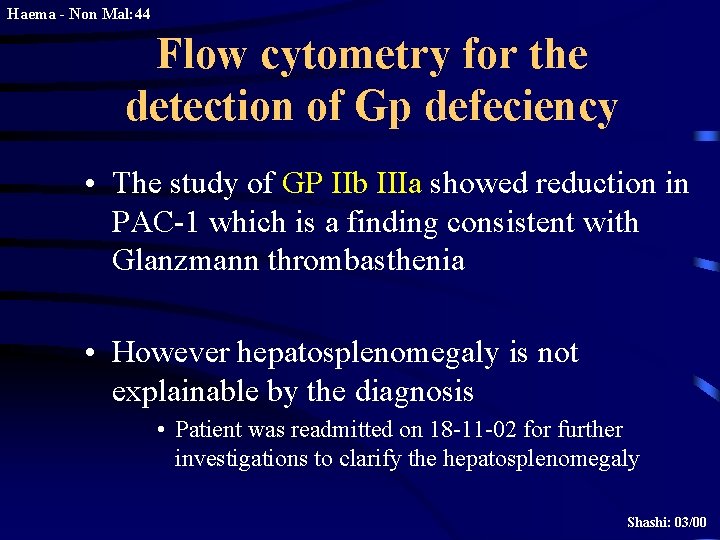
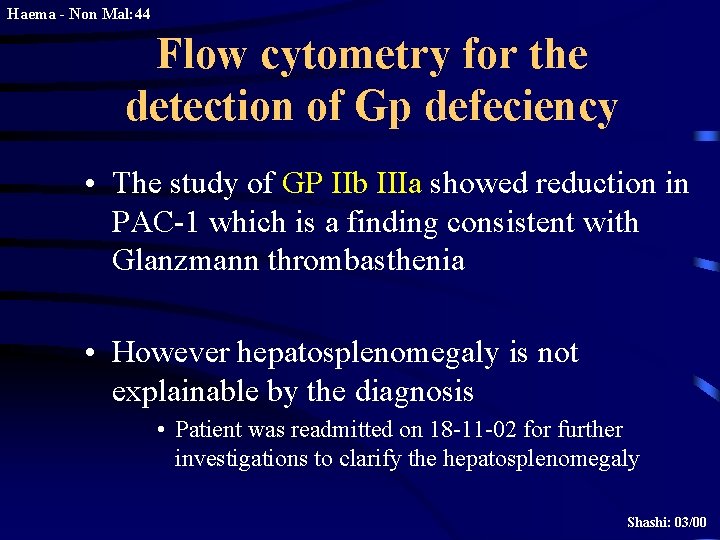
Haema - Non Mal: 44 Flow cytometry for the detection of Gp defeciency • The study of GP IIb IIIa showed reduction in PAC-1 which is a finding consistent with Glanzmann thrombasthenia • However hepatosplenomegaly is not explainable by the diagnosis • Patient was readmitted on 18 -11 -02 for further investigations to clarify the hepatosplenomegaly Shashi: 03/00
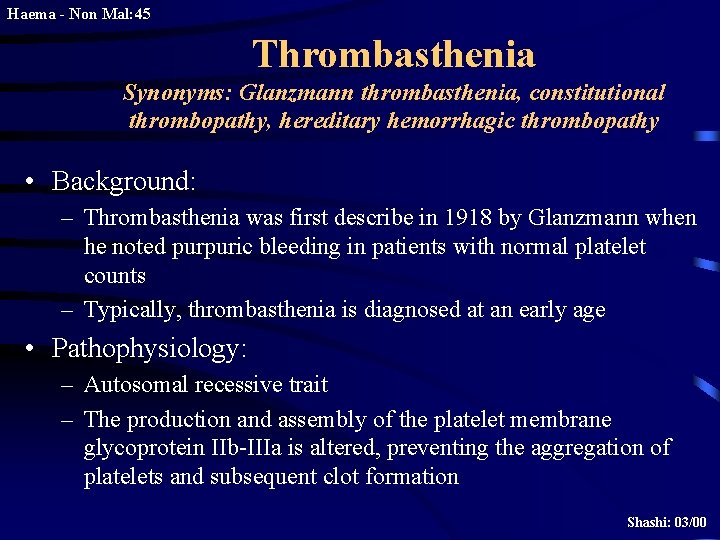
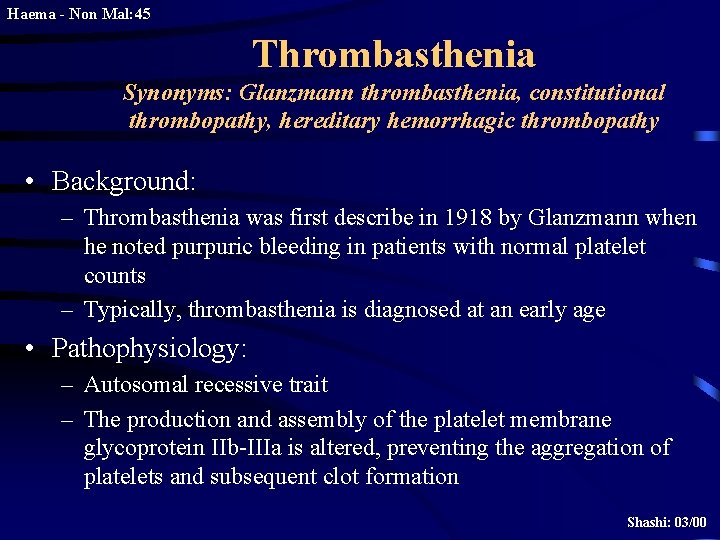
Haema - Non Mal: 45 Thrombasthenia Synonyms: Glanzmann thrombasthenia, constitutional thrombopathy, hereditary hemorrhagic thrombopathy • Background: – Thrombasthenia was first describe in 1918 by Glanzmann when he noted purpuric bleeding in patients with normal platelet counts – Typically, thrombasthenia is diagnosed at an early age • Pathophysiology: – Autosomal recessive trait – The production and assembly of the platelet membrane glycoprotein IIb-IIIa is altered, preventing the aggregation of platelets and subsequent clot formation Shashi: 03/00
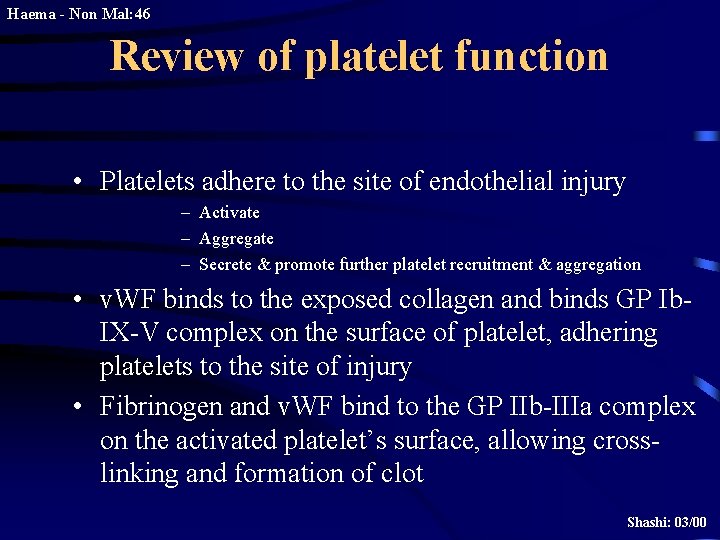
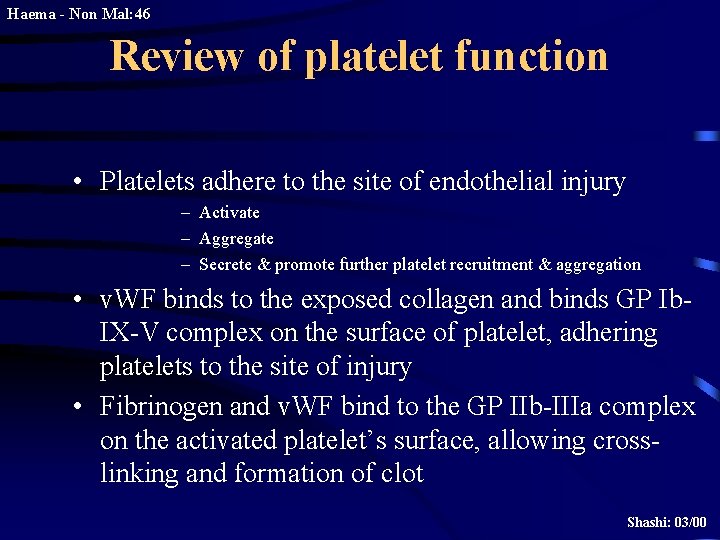
Haema - Non Mal: 46 Review of platelet function • Platelets adhere to the site of endothelial injury – Activate – Aggregate – Secrete & promote further platelet recruitment & aggregation • v. WF binds to the exposed collagen and binds GP Ib. IX-V complex on the surface of platelet, adhering platelets to the site of injury • Fibrinogen and v. WF bind to the GP IIb-IIIa complex on the activated platelet’s surface, allowing crosslinking and formation of clot Shashi: 03/00
Haema - Non Mal: 47 Specific Deficiency • GP IIb and IIIa have separate genes on the long arm of chromosome 17 • Specific genetic abnormalities of each GP include • • • Missense mutations Nonsense mutations Splice site mutations Deletions and Point mutations • Abnormalities in either gene or in the assembly of the complex result in an abnormal or deficient receptor Shashi: 03/00
Haema - Non Mal: 48 • Consequently – One or other GP is not formed properly, leaving the other unpaired in the endoplasmic reticulum, where it is degraded – Platelet aggregation is rendered deficient or completely absent • Heterozygotes are asymptomatic • Binding sites for thrombin are preserved in thrombasthenic platelets Shashi: 03/00
Haema - Non Mal: 49 • Patients are classified into: type 1, type 2, or the variant type, depending on the degree of GP IIb -IIIa deficiency, fibrinogen binding, and clot retraction • Type 1 : most severe form, less than 5% of normal GP IIb -IIIa present with absent fibrinogen binding and clot retraction • Type 2 : 10 -20% of GP IIb-IIIa, normal to moderately deficient clot retraction with fibrinogen binding • Variant type : 50% of the normal amount of GP IIb-IIIa with extremely variable fibrinogen binding and clot retraction Shashi: 03/00
Haema - Non Mal: 50 • Frequency: – 300 cases are reported in medical literature – 1 st case diagnosed in HUSM • Mortality/Morbidity: – Death following bleeding approx. 5% • Age: – Typically diagnosed during infancy – Epistaxis is more severe in children but rare in adults • History – In the neonatal period: mucocutaneous bleeding – In childhood: purpura, epistaxis & gingival bleeding – The bleeding tendency decreases with age Shashi: 03/00
Haema - Non Mal: 51 • Additional presentations include – – GI bleeding Excessive bleeding at menarche & following parturition Post surgical bleeding Hemarthrosis and deep hematomas are unusual • The absence of family history should not delay a workup for thrombasthenia as it is a recessive trait • Beyond identification of hemorrhage, physical examination is usually of limited use Shashi: 03/00

Haema - Non Mal: 52 • Other disorders to be considered in the differential diagnosis: – – – Gray platelet syndrome Hermansky-Pudlak syndrome Chediak-Higashi syndrome ITP DIC Medication-induced platelet inhibition • • • Prostaglandin synthetase inhibitors (Aspirin, NSAIDS) ADP receptor inhibitors (Clopidogrel, Ticlopidine) Receptor blocking drugs (Dipyridamole) Beta-lactam antibiotics Heparin – Others • Alcohol • Uremia • hyperglobulinemias • Lab investigations: – – – Bleeding time Aggregation studies Platelet count and morphology PT/ APTT Flow cytometric studies Shashi: 03/00
Haema - Non Mal: 53 Medical Care • Emergency care: – Refractory bleeding requires transfusion of normal platelets – HLA-matched platelets is the treatment of choice – In rare cases, antibodies to Gp IIb-IIIa are detectable • Medical treatment: – Antifibrinolytic agents inhibit fibrinolysis via inhibition of plasminogen activator substances • Aminocaproic acid; may be useful in controlling bleeding after dental extraction • Contraindicated in the evidence of active intravascular clotting process (DIC) • Hematuria is relative contraindication • Co-administration with estrogens may cause increase clotting factors, Shashi: 03/00 leading to hypercoagulable state
Haema - Non Mal: 54 Medical treatment contd – Vasopressin analogs, act like ADH to increase factor VIII levels • Desmopressin (DDAVP); synthetic vasopressin analog – The use of DDAVP not recommended routinely – Contraindicated in documented hypersensitivity – Clotting factors • Coagulation factor VIIa, recombinant • Otherapies cited in literature – IV Igs – Repeated plasma pheresis – Bone marrow transplant Shashi: 03/00
Haema - Non Mal: 55 Conclusion & Take home message • Final diagnosis of our patient was Glanzmann thrombasthenia • Family studies for platelet function defect are recommended • However, further investigations are required to clarify the cause of hepatosplenomegaly and low factor IX • Refractory haemorrhage in the presence of normal platelet count and normal coagulation factors need to be investigated further (Now in HUSM) Shashi: 03/00