Kritikus Foundation Presents SHOCK Shock is a syndrome








- Slides: 56
Kritikus Foundation Presents
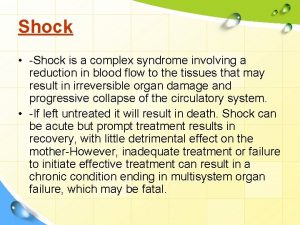
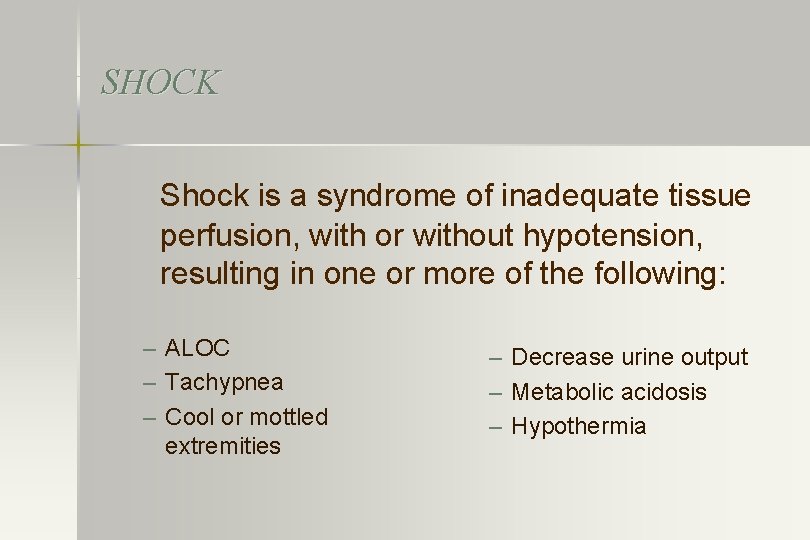
SHOCK Shock is a syndrome of inadequate tissue perfusion, with or without hypotension, resulting in one or more of the following: – ALOC – Tachypnea – Cool or mottled extremities – Decrease urine output – Metabolic acidosis – Hypothermia
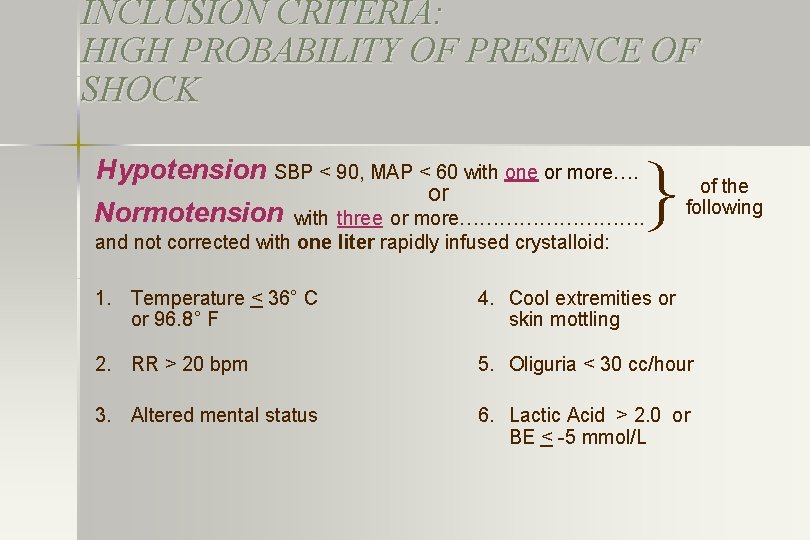
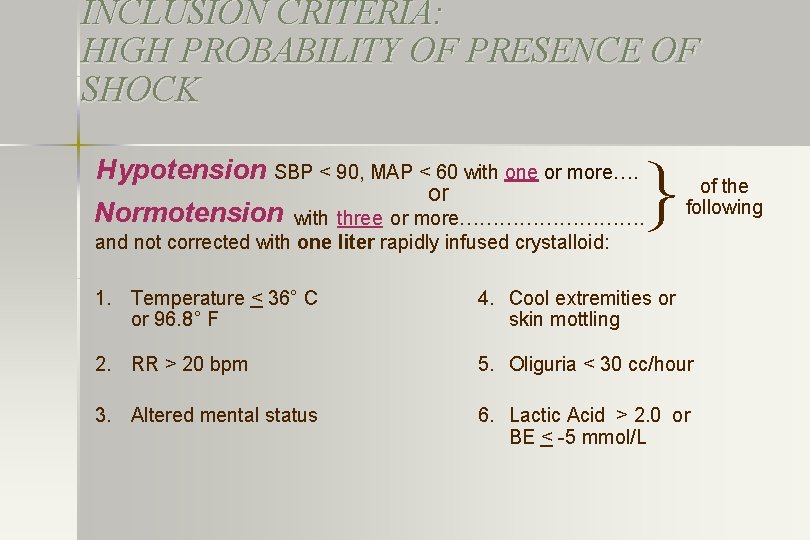
INCLUSION CRITERIA: HIGH PROBABILITY OF PRESENCE OF SHOCK Hypotension SBP < 90, MAP < 60 with one or more…. Normotension or } with three or more……………. and not corrected with one liter rapidly infused crystalloid: of the following 1. Temperature < 36° C or 96. 8° F 4. Cool extremities or skin mottling 2. RR > 20 bpm 5. Oliguria < 30 cc/hour 3. Altered mental status 6. Lactic Acid > 2. 0 or BE < -5 mmol/L
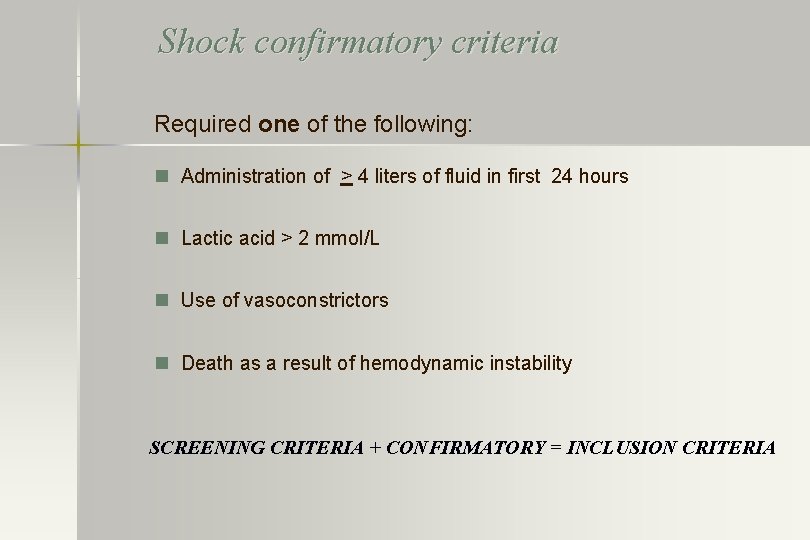
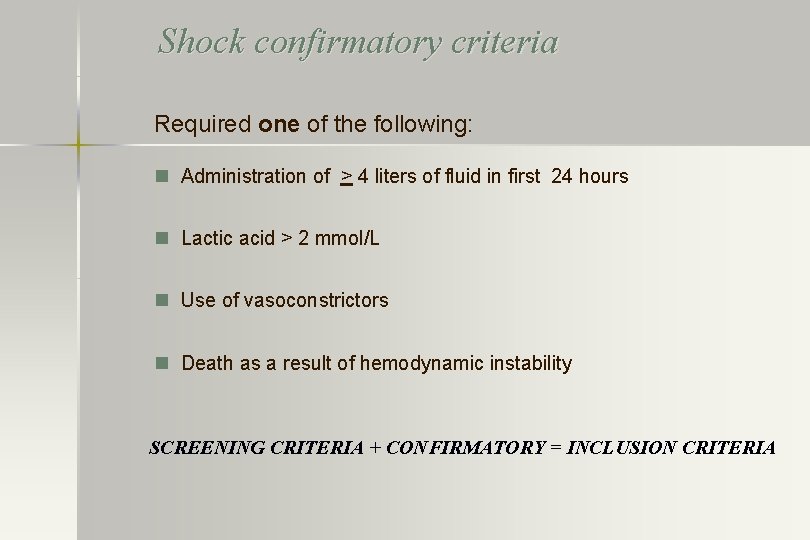
Shock confirmatory criteria Required one of the following: n Administration of > 4 liters of fluid in first 24 hours n Lactic acid > 2 mmol/L n Use of vasoconstrictors n Death as a result of hemodynamic instability SCREENING CRITERIA + CONFIRMATORY = INCLUSION CRITERIA
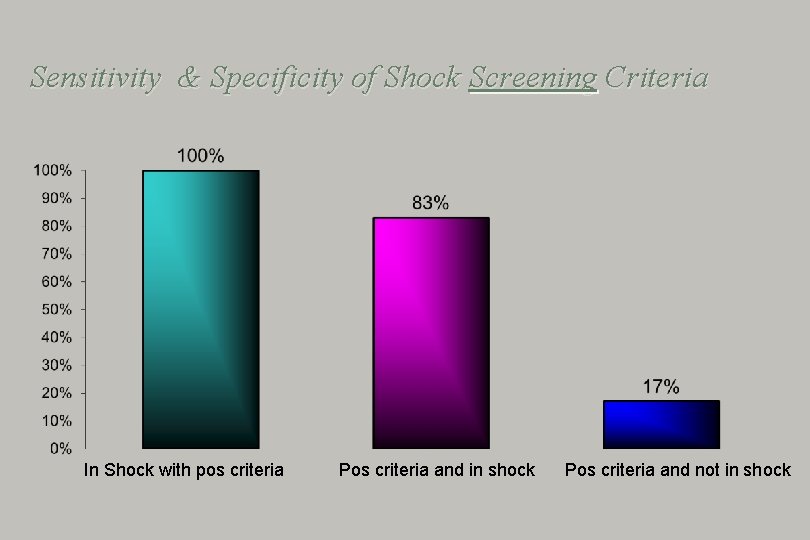
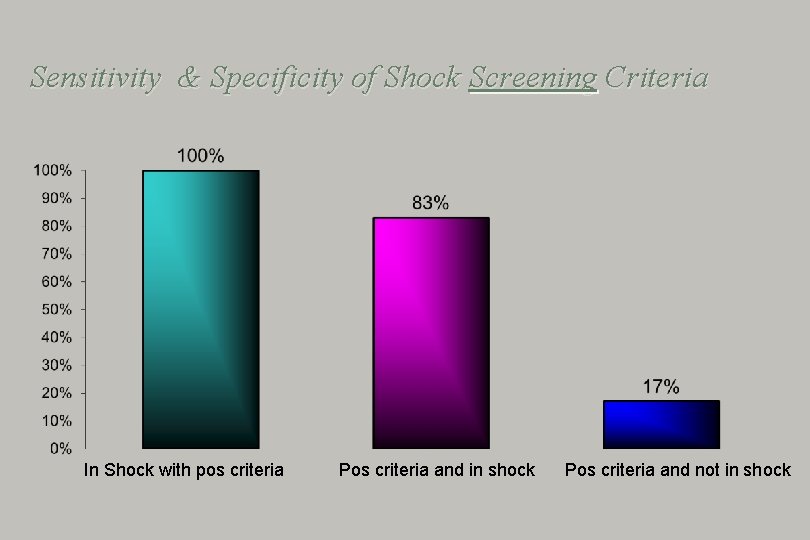
Sensitivity & Specificity of Shock Screening Criteria In Shock with pos criteria Pos criteria and in shock Pos criteria and not in shock
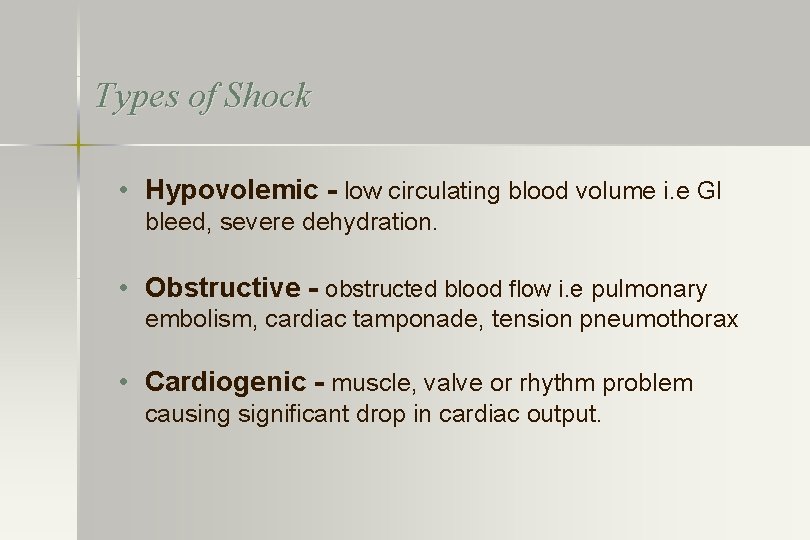
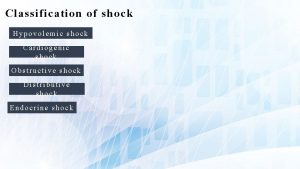
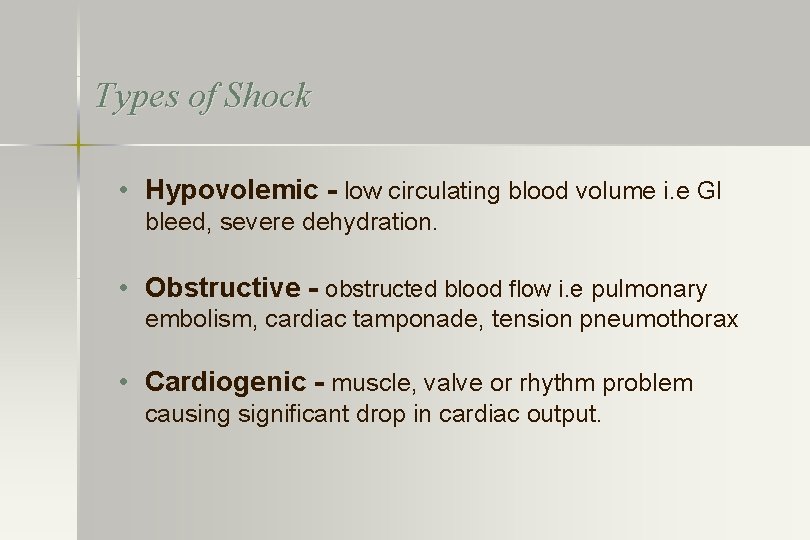
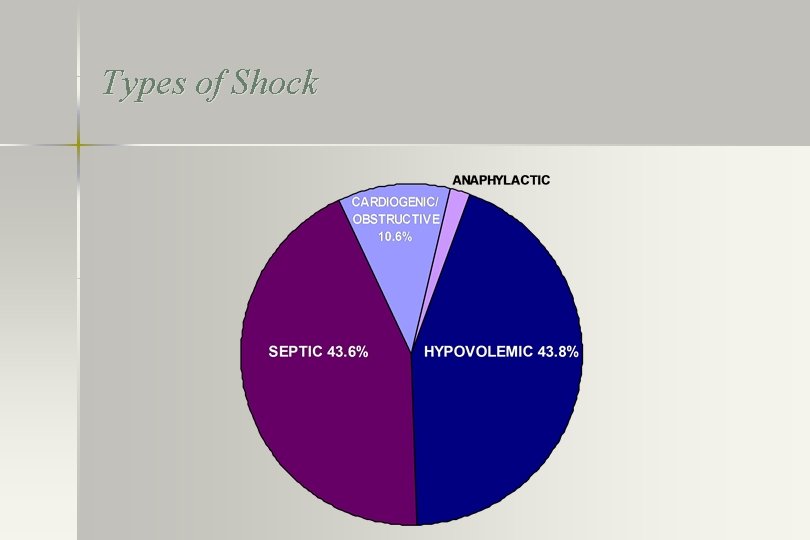
Types of Shock • Hypovolemic - low circulating blood volume i. e GI bleed, severe dehydration. • Obstructive - obstructed blood flow i. e pulmonary embolism, cardiac tamponade, tension pneumothorax • Cardiogenic - muscle, valve or rhythm problem causing significant drop in cardiac output.

Types of Shock • Septic or Distributive - vasodilation loss of arterial tone with redistribution of vol to tissues, viens i. e. infection, pancreatitis or other sources of tissue injury • Anaphylactic – same as distributive shock i. e reaction to drug or environmental agent • Hypoxic – not considered a classic form of shock - but is a is the most rapidly progressive and fatal case of global inadequate delivery of oxegen; if not reversed
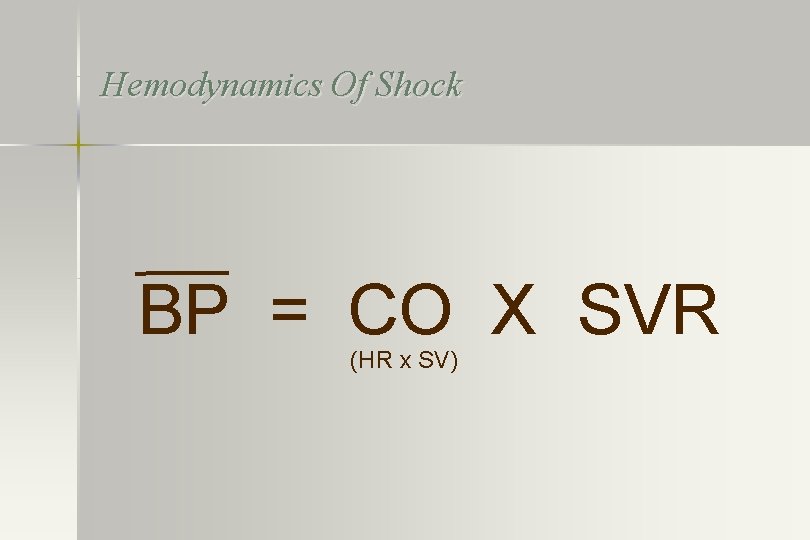
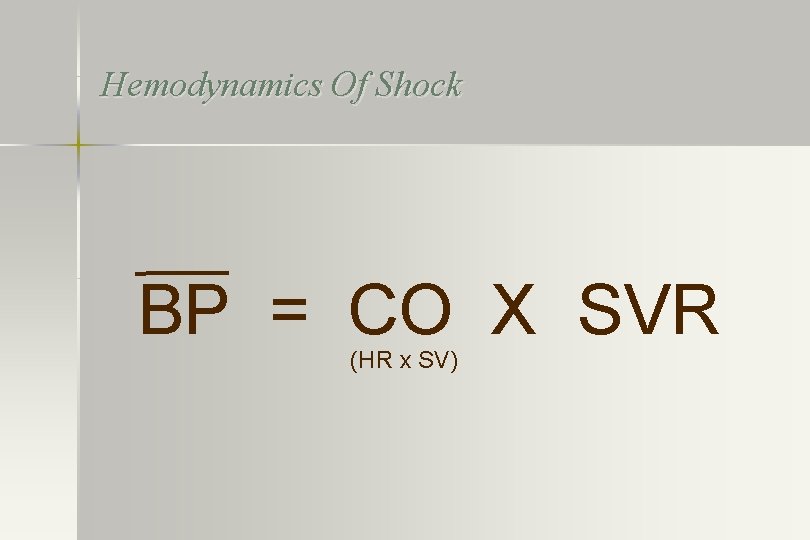
Hemodynamics Of Shock BP = CO X SVR (HR x SV)
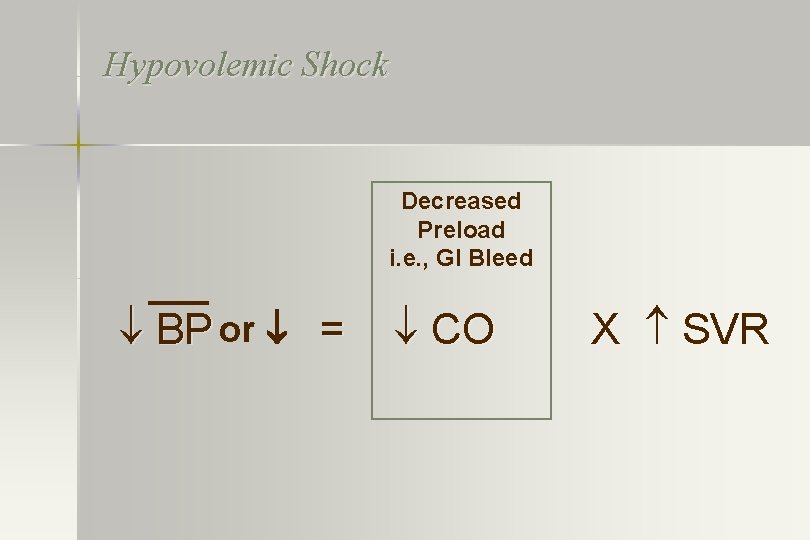
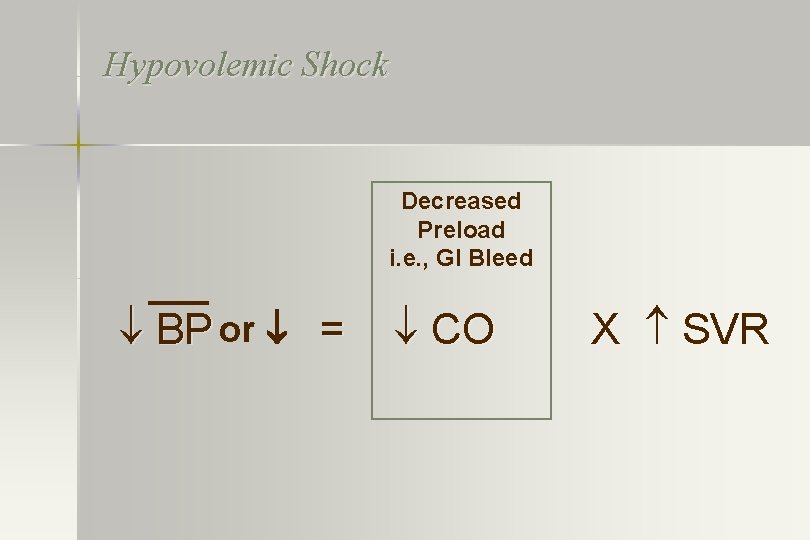
Hypovolemic Shock Decreased Preload i. e. , GI Bleed BP or = CO X SVR
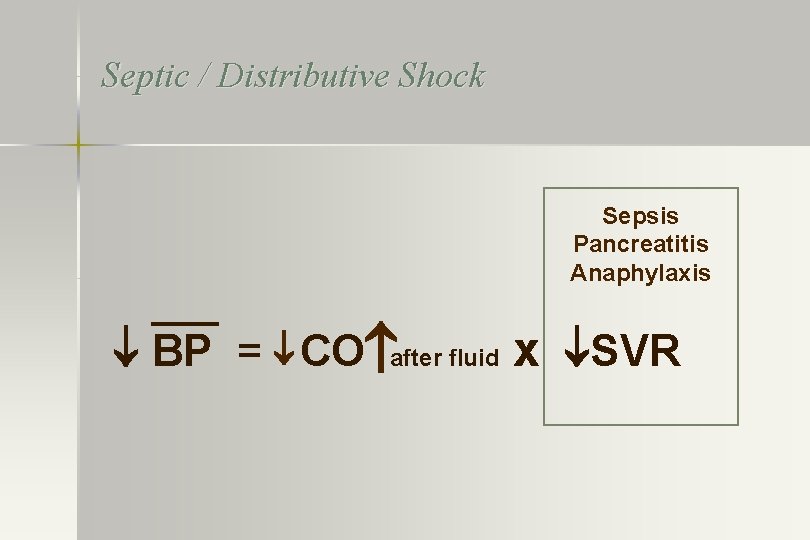
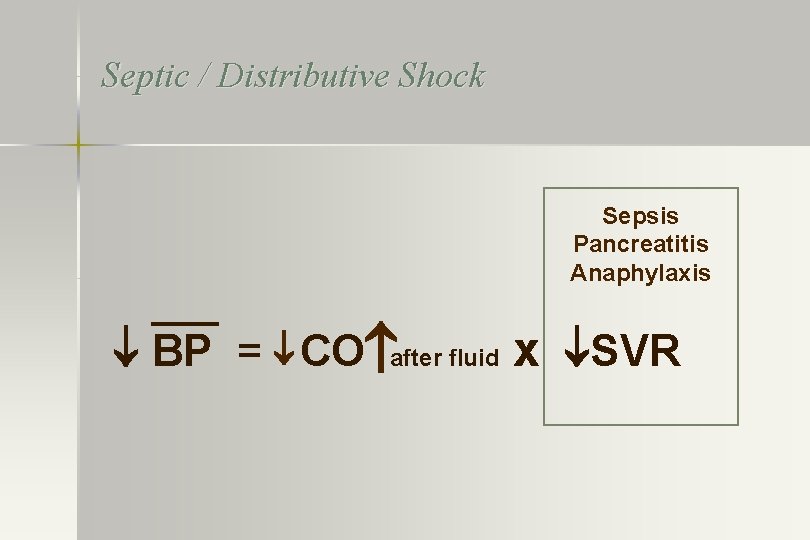
Septic / Distributive Shock Sepsis Pancreatitis Anaphylaxis BP = CO after fluid x SVR
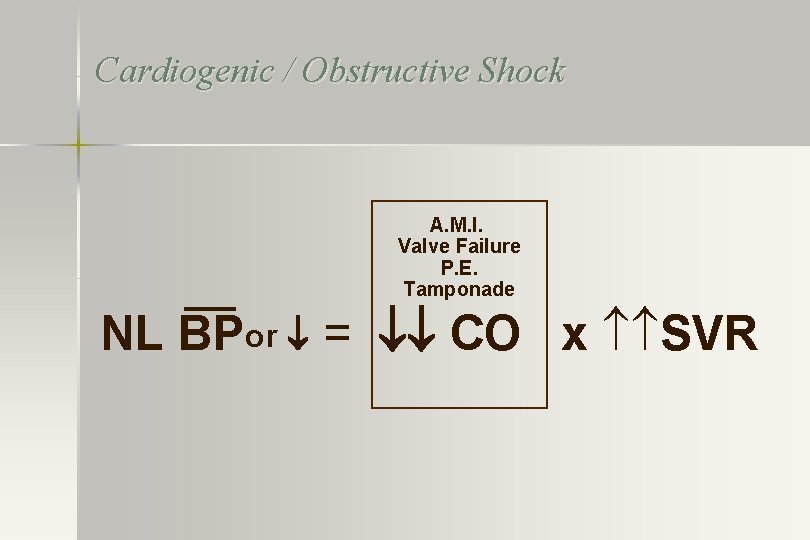
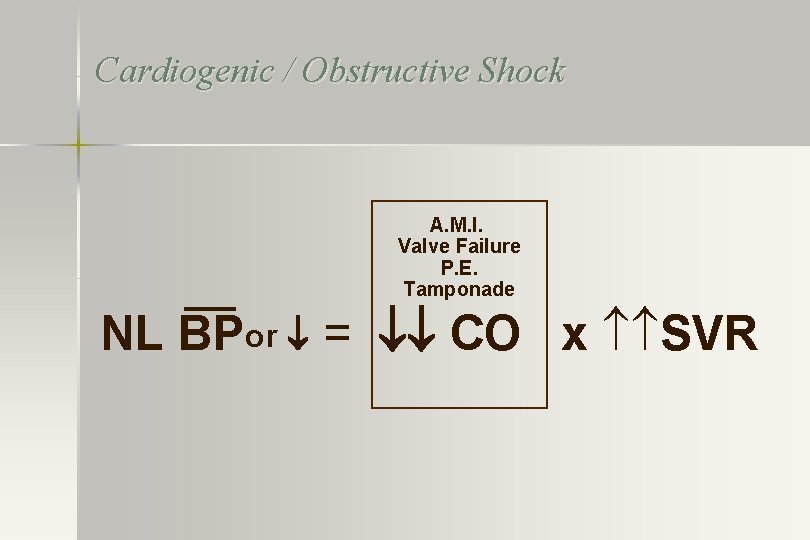
Cardiogenic / Obstructive Shock A. M. I. Valve Failure P. E. Tamponade NL BPor = CO x SVR
Why a Shock Educational Program and System • A standardized and systematic approach to shock will lead to: • Early Recognition • Early Initiation of Best Practice Improved Outcomes !

Background & Prior Experience
Medical Emergency Teams A Shock Team In A General Hospital Edward D. Frank, M. D. Department of Surgery Harvard Medical School Published in Anesthesia and Analgesia November - December 1967
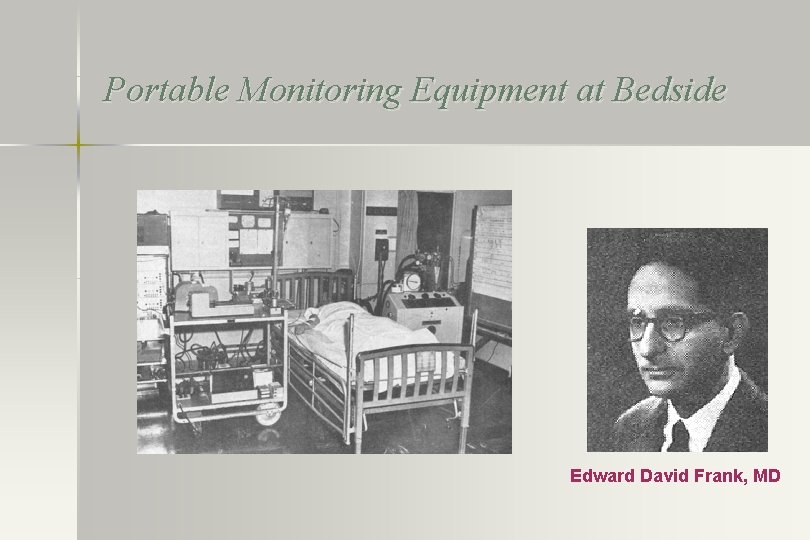
Portable Monitoring Equipment at Bedside Edward David Frank, MD
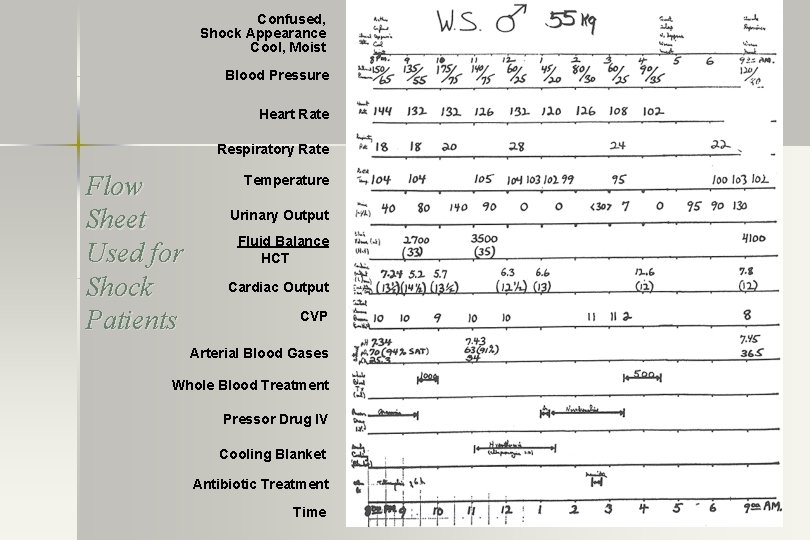
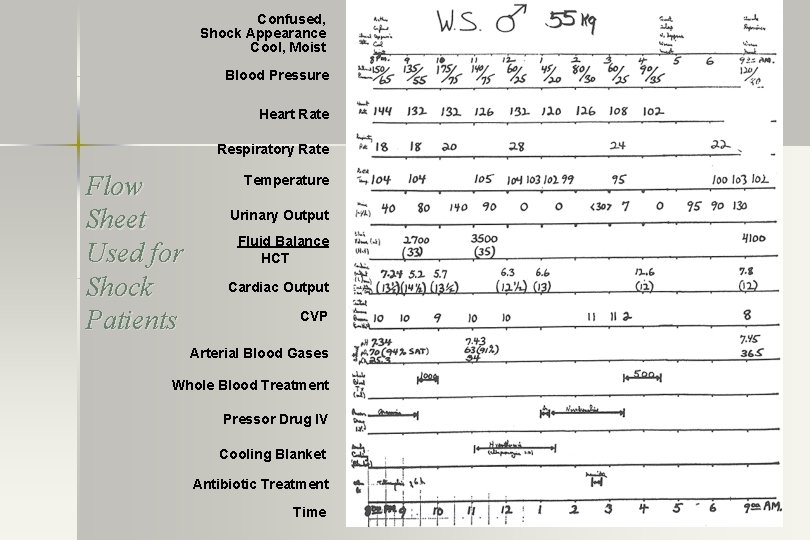
Confused, Shock Appearance Cool, Moist Blood Pressure Heart Rate Respiratory Rate Flow Sheet Used for Shock Patients Temperature Urinary Output Fluid Balance HCT Cardiac Output CVP Arterial Blood Gases Whole Blood Treatment Pressor Drug IV Cooling Blanket Antibiotic Treatment Time
Shock (Septic) Mortality • • • None reported 1967 by Dr Frank 70% septic shock in 1970 s 50% in 1990 s 40 to 30% in 2000 -2005 30% to 27% in 2015 to present 10% reported with a dedicated Shock program and team in 2005
Shock Program and Team Effect of a Rapid Response System for Patients in Shock on Time to Treatment and Mortality During 5 Years CC Med 2007 Frank Sebat, MS, MD, FCCP, FCCM; Amjad A. Musthafa, FCCP; David Johnson, MD; Andrew A. Kramer, Ph. D; Debbie Shoffner; Mark Eliason, BSN; Kristen Henry, BSN; Bruce Spurlock, M • Mortality of septic shock decreased from 50% (2000) to 10% (2005) • Decreased time from when shock could have been recognized till administration of Key interventions - 310 min to 80 min
Shock - Why such high fatality rates? • Frequently not recognized early • When recognized often have the onset of end organ damage (MOF) AND
ALL SHOCK Leads to cardiogenic shock
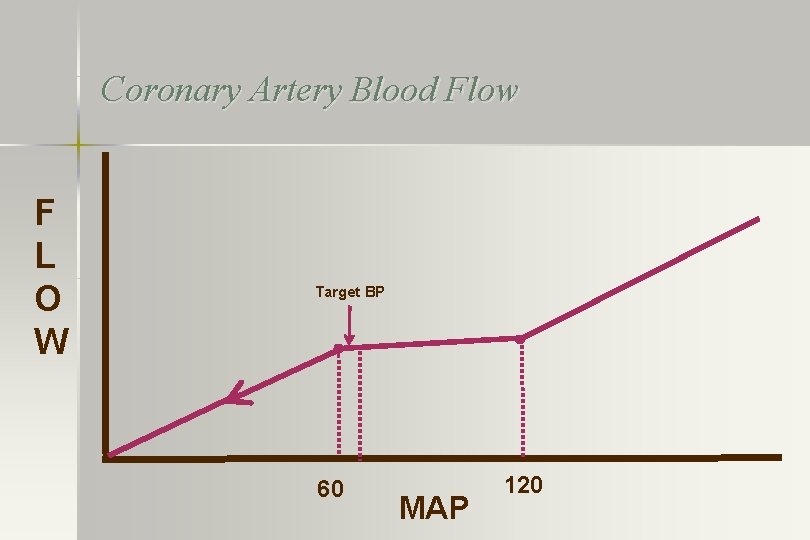
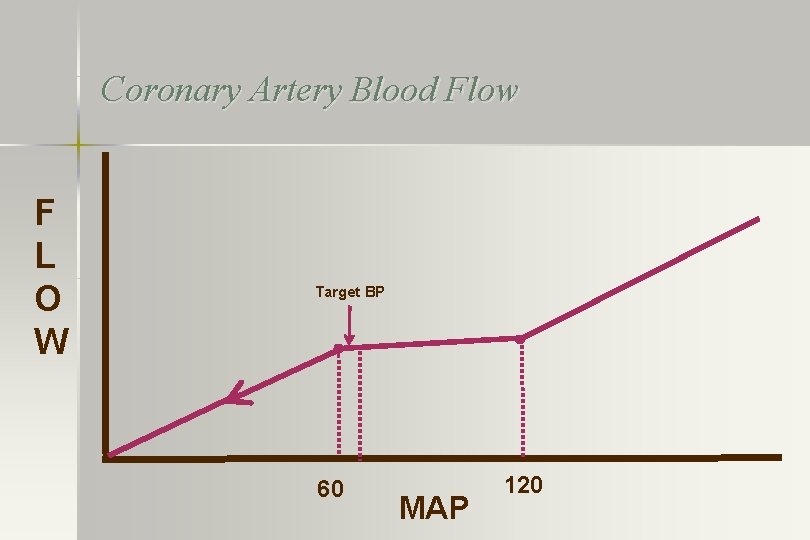
Coronary Artery Blood Flow F L O W Target BP 60 MAP 120
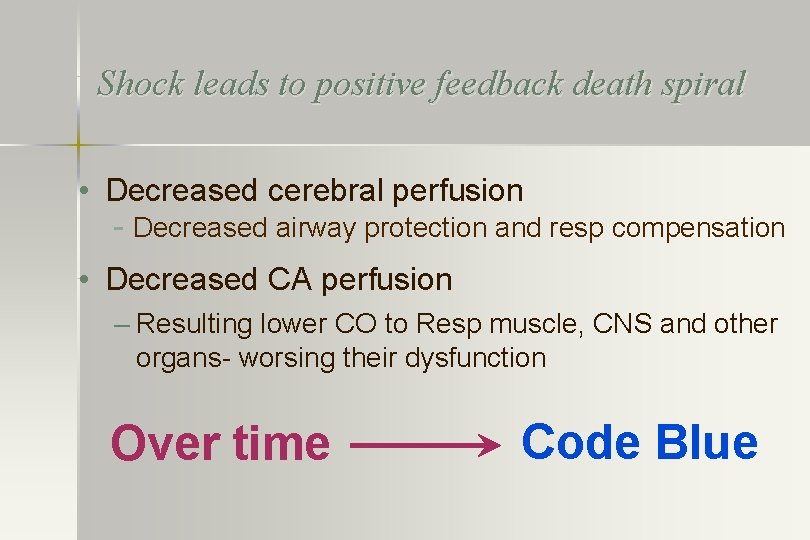
Shock leads to positive feedback death spiral • Decreased cerebral perfusion - Decreased airway protection and resp compensation • Decreased CA perfusion – Resulting lower CO to Resp muscle, CNS and other organs- worsing their dysfunction Over time Code Blue
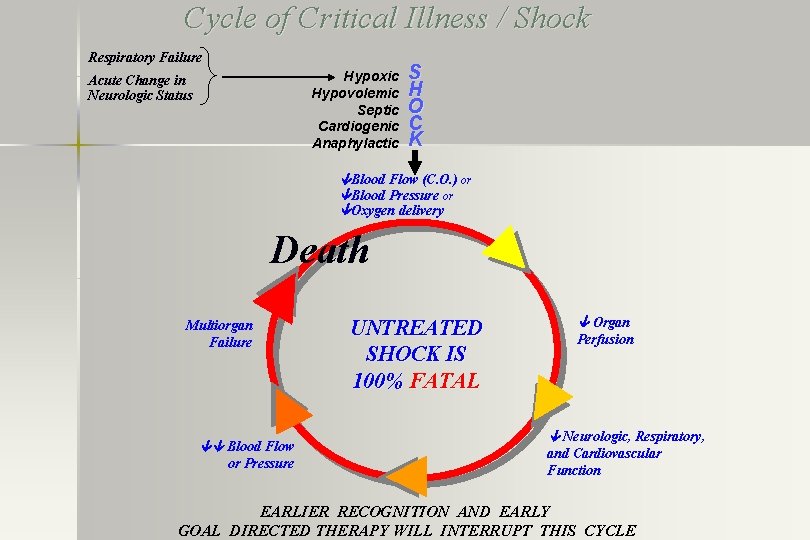
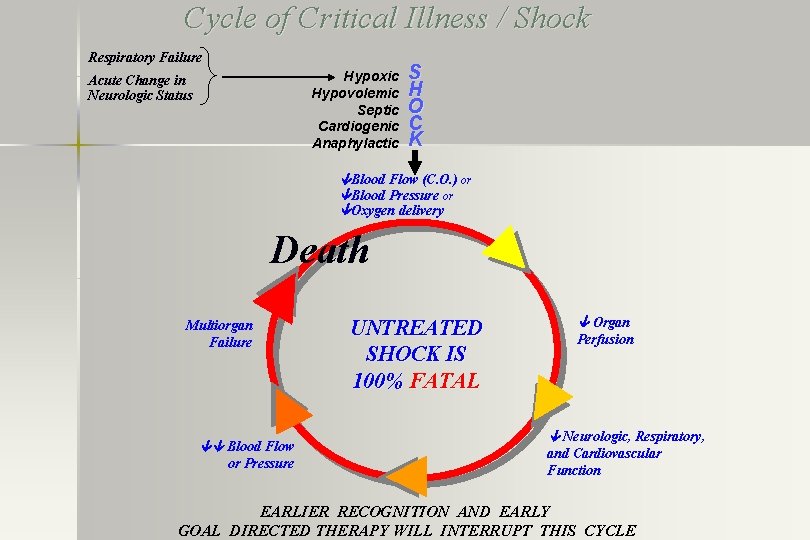
Cycle of Critical Illness / Shock Respiratory Failure Hypoxic Hypovolemic Septic Cardiogenic Anaphylactic Acute Change in Neurologic Status S H O C K Blood Flow (C. O. ) or Blood Pressure or Oxygen delivery Death Multiorgan Failure Blood Flow or Pressure UNTREATED SHOCK IS 100% FATAL Organ Perfusion Neurologic, Respiratory, and Cardiovascular Function EARLIER RECOGNITION AND EARLY GOAL DIRECTED THERAPY WILL INTERRUPT THIS CYCLE
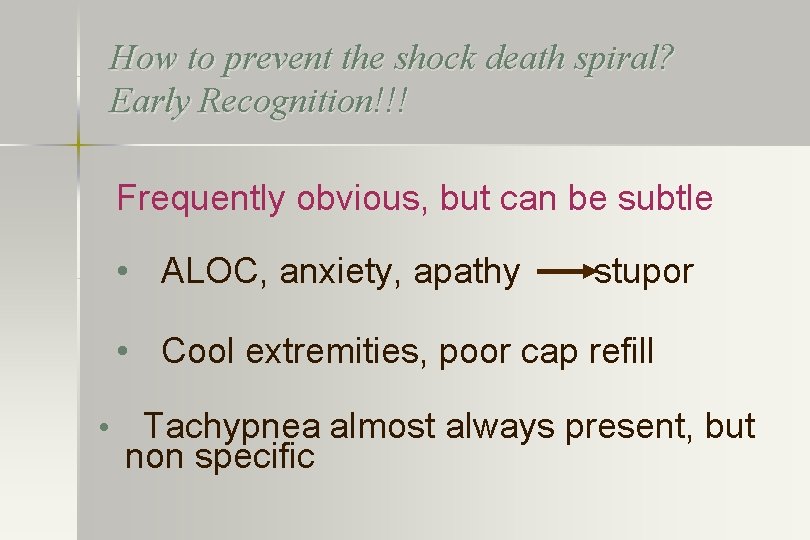
How to prevent the shock death spiral? Early Recognition!!! Frequently obvious, but can be subtle • ALOC, anxiety, apathy stupor • Cool extremities, poor cap refill • Tachypnea almost always present, but non specific
Recognition of Shock Frequently obvious, but can be subtle • Hypotension--frequently, but not always present or worse not detected • Oliguria--takes time to assess • Metabolic acidosis/LA may take time to develop or wash out of the tissues
How Do We Recognize Shock Sooner? • Learn the manifestations • Have a high index of suspicion • Once the question of shock is raised, go through the drill, i. e. , Hx, exam, lab, repeat observation Burden of proof on the caregiver i. e. , prove to yourself the patient is not in shock !
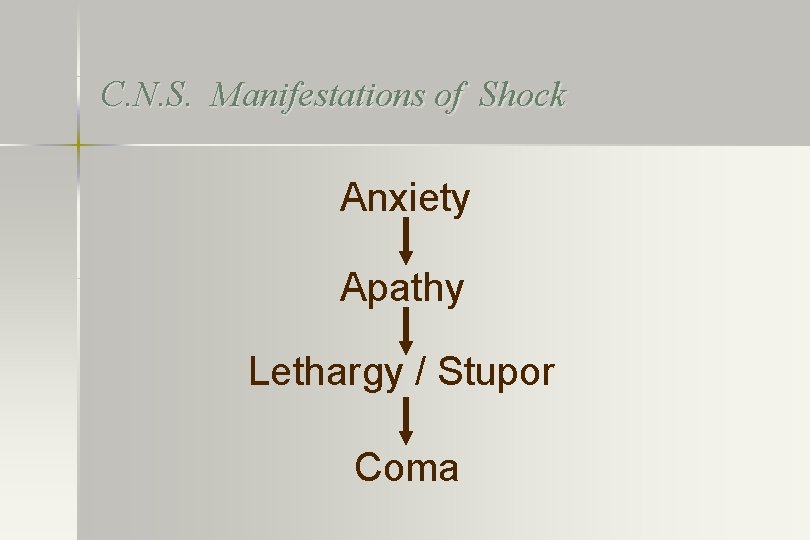
C. N. S. Manifestations of Shock Anxiety Apathy Lethargy / Stupor Coma
Cardiac Manifestations of Shock Dysrhythmias Myocardial ischemia, chest pain Myocardial depression ALL SHOCK LEADS TO CARDIOGENIC SHOCK
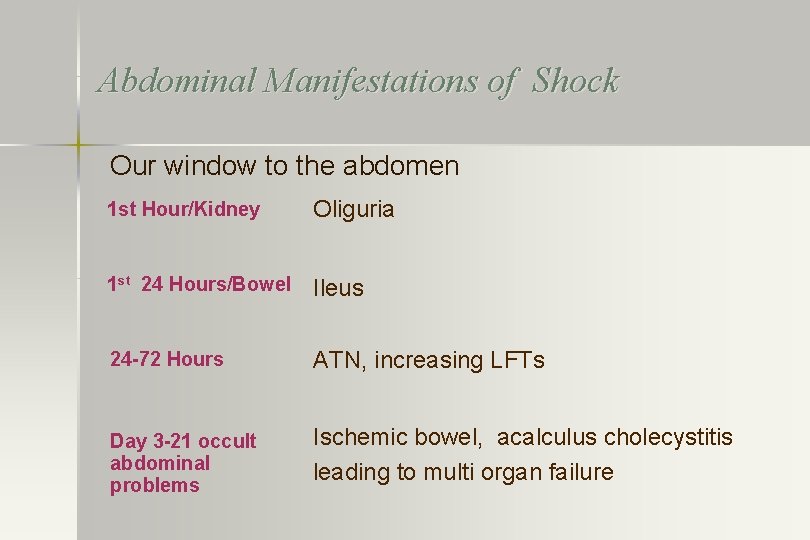
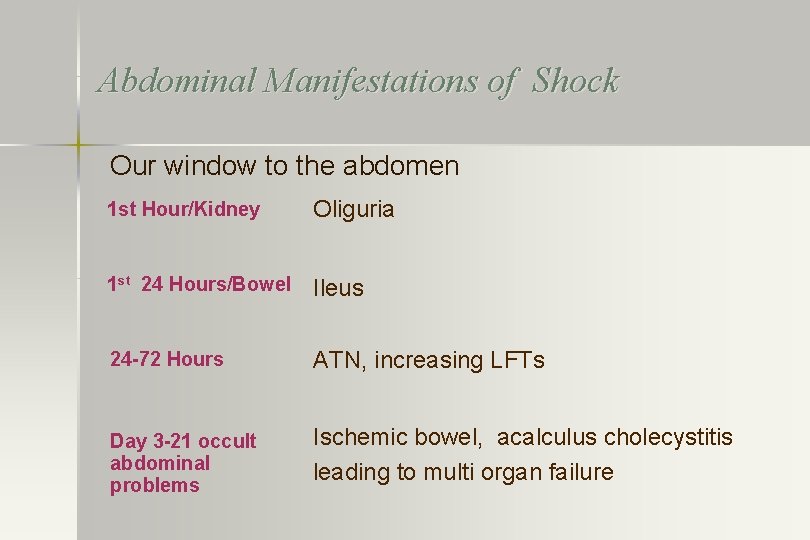
Abdominal Manifestations of Shock Our window to the abdomen 1 st Hour/Kidney Oliguria 1 st 24 Hours/Bowel Ileus 24 -72 Hours ATN, increasing LFTs Day 3 -21 occult abdominal problems Ischemic bowel, acalculus cholecystitis leading to multi organ failure

Skin Manifestations of Shock: Livedo reticularis
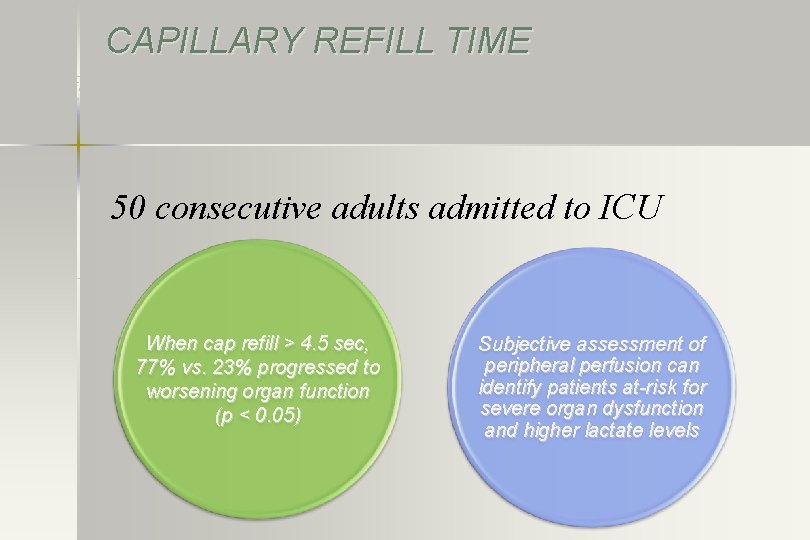
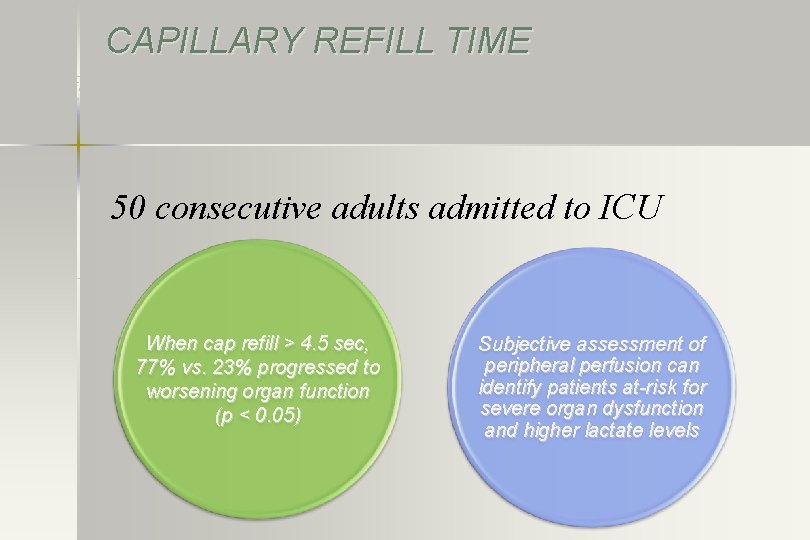
CAPILLARY REFILL TIME Critical Care Medicine. 37(3): 934 -938, March 2009 50 consecutive adults admitted to ICU When cap refill > 4. 5 sec, 77% vs. 23% progressed to worsening organ function (p < 0. 05) Subjective assessment of peripheral perfusion can identify patients at-risk for severe organ dysfunction and higher lactate levels

Metabolic Manifestations of Shock Acid accumulation in the body BE < -5 meq/L Lactic Acid > 2. 0 meq/L
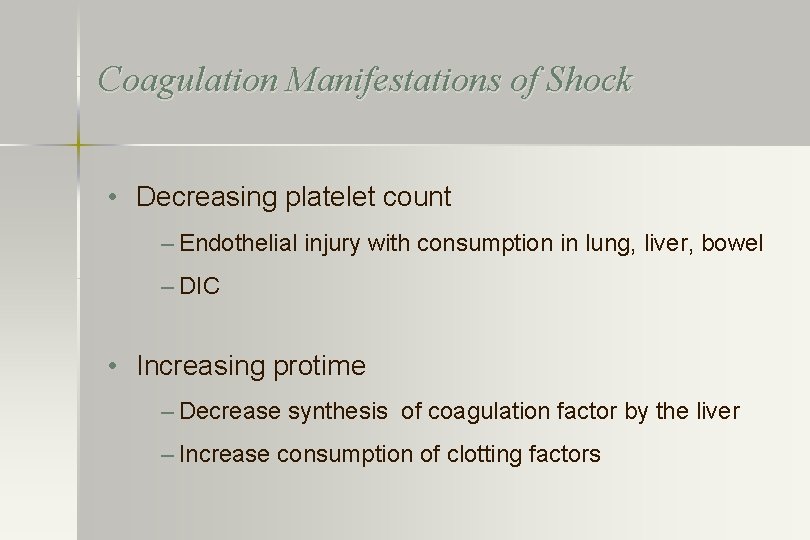
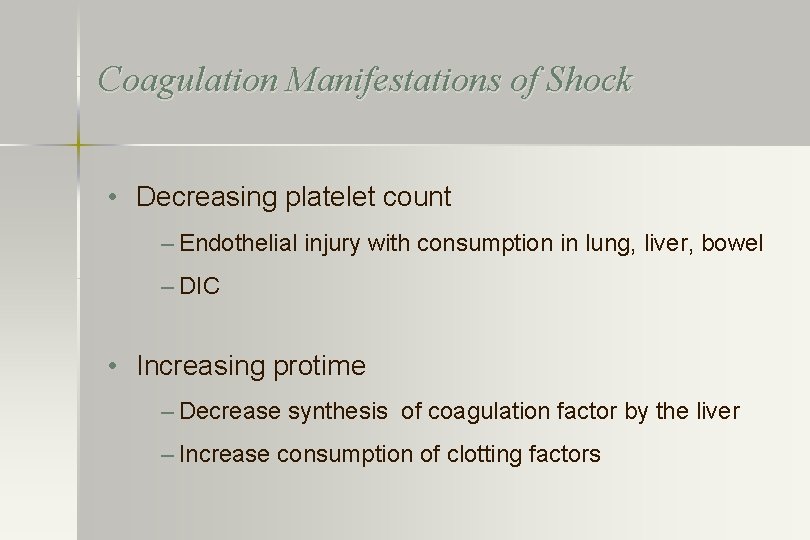
Coagulation Manifestations of Shock • Decreasing platelet count – Endothelial injury with consumption in lung, liver, bowel – DIC • Increasing protime – Decrease synthesis of coagulation factor by the liver – Increase consumption of clotting factors
Shock If Crtieria Met Then What?

? CALL RRT ALERT?

Treatment
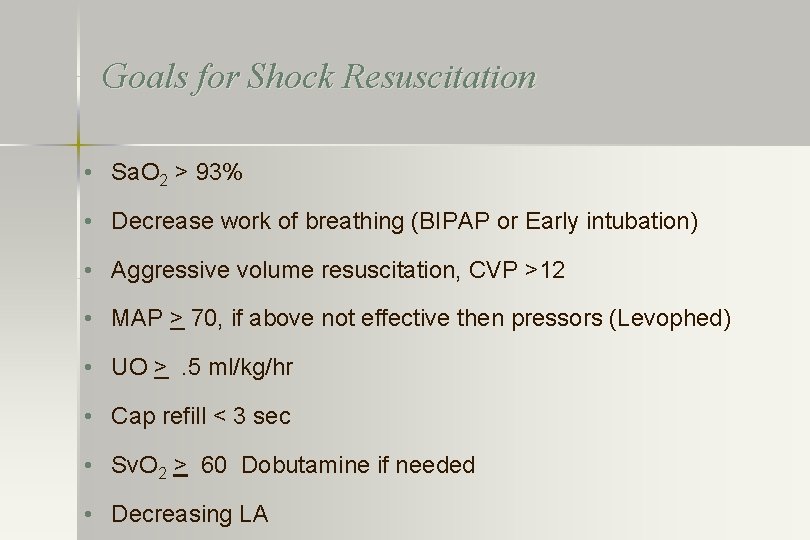
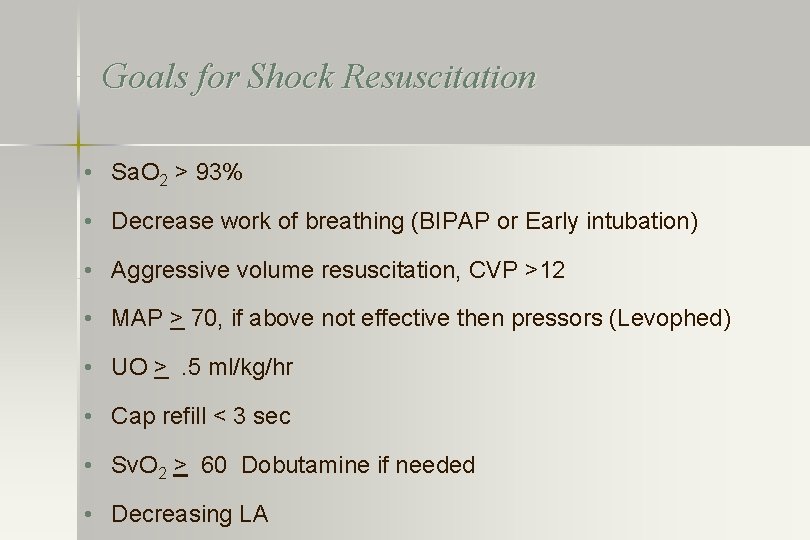
Goals for Shock Resuscitation • Sa. O 2 > 93% • Decrease work of breathing (BIPAP or Early intubation) • Aggressive volume resuscitation, CVP >12 • MAP > 70, if above not effective then pressors (Levophed) • UO >. 5 ml/kg/hr • Cap refill < 3 sec • Sv. O 2 > 60 Dobutamine if needed • Decreasing LA
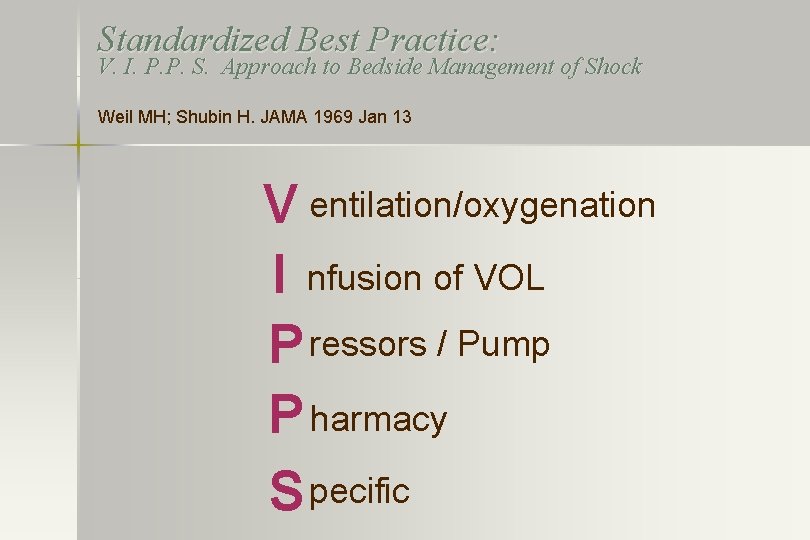
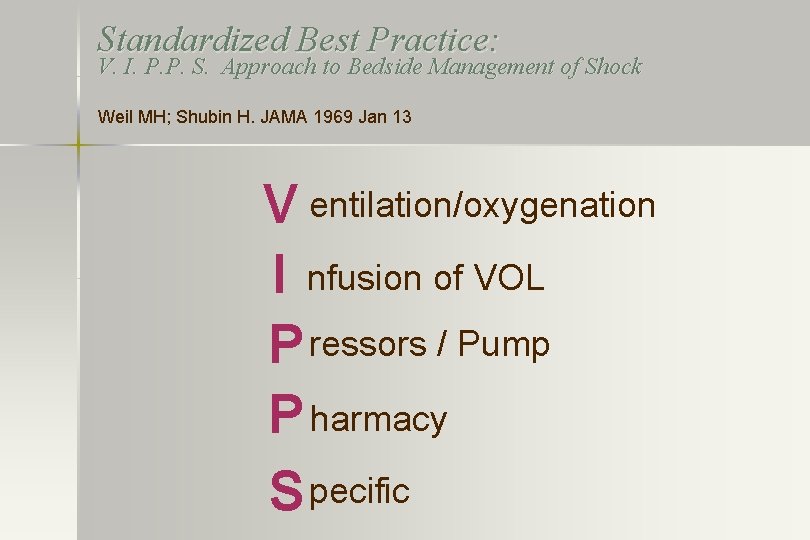
Standardized Best Practice: V. I. P. P. S. Approach to Bedside Management of Shock Weil MH; Shubin H. JAMA 1969 Jan 13 V entilation/oxygenation I nfusion of VOL P ressors / Pump P harmacy S pecific
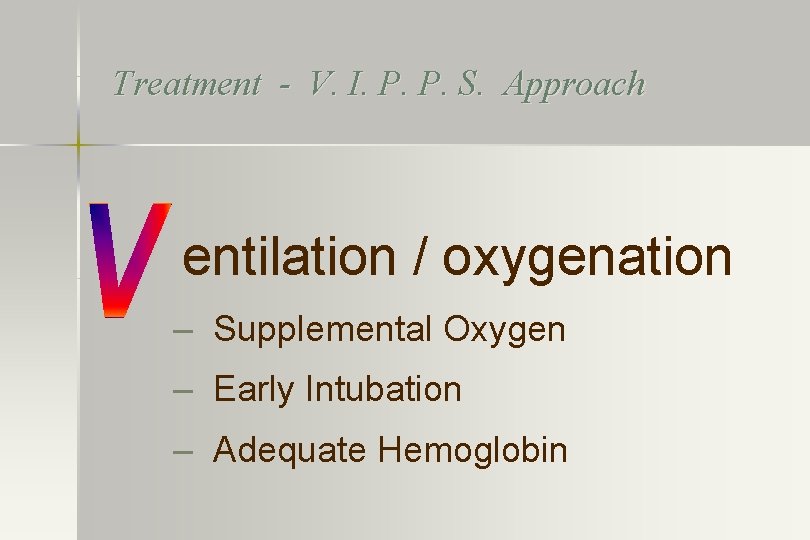
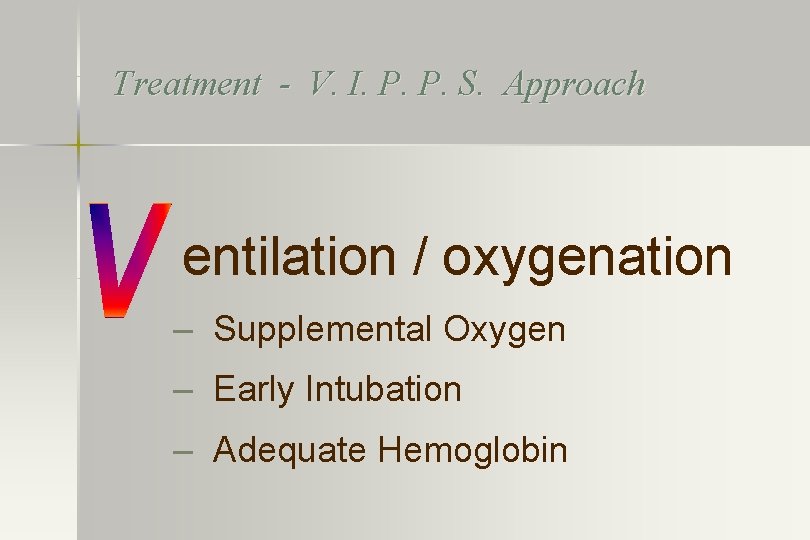
Treatment - V. I. P. P. S. Approach entilation / oxygenation – Supplemental Oxygen – Early Intubation – Adequate Hemoglobin
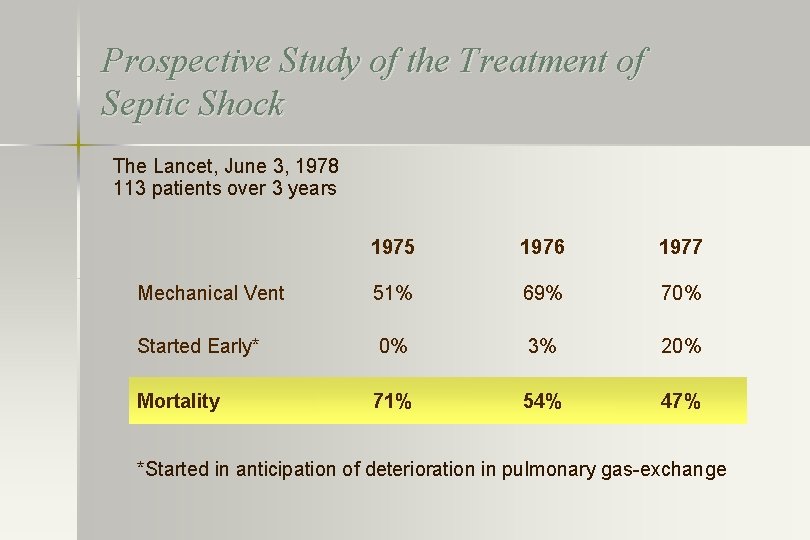
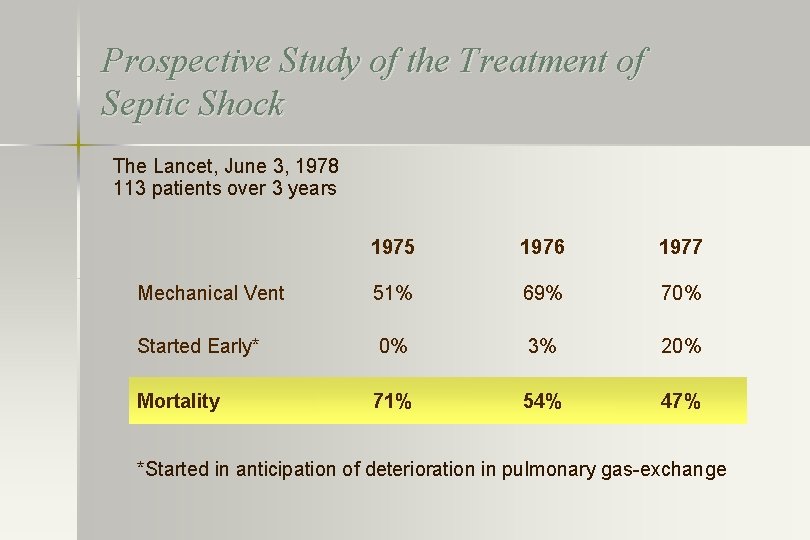
Prospective Study of the Treatment of Septic Shock The Lancet, June 3, 1978 113 patients over 3 years 1975 1976 1977 Mechanical Vent 51% 69% 70% Started Early* 0% 3% 20% Mortality 71% 54% 47% *Started in anticipation of deterioration in pulmonary gas-exchange
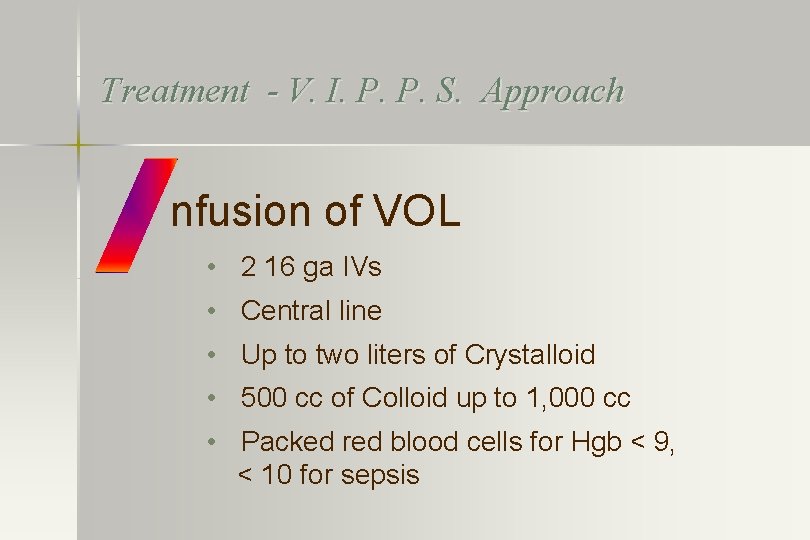
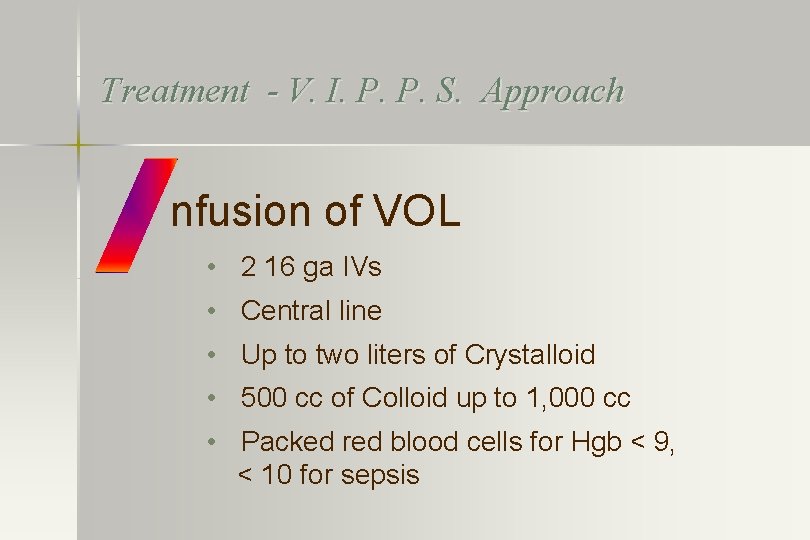
Treatment - V. I. P. P. S. Approach nfusion of VOL • 2 16 ga IVs • Central line • Up to two liters of Crystalloid • 500 cc of Colloid up to 1, 000 cc • Packed red blood cells for Hgb < 9, < 10 for sepsis
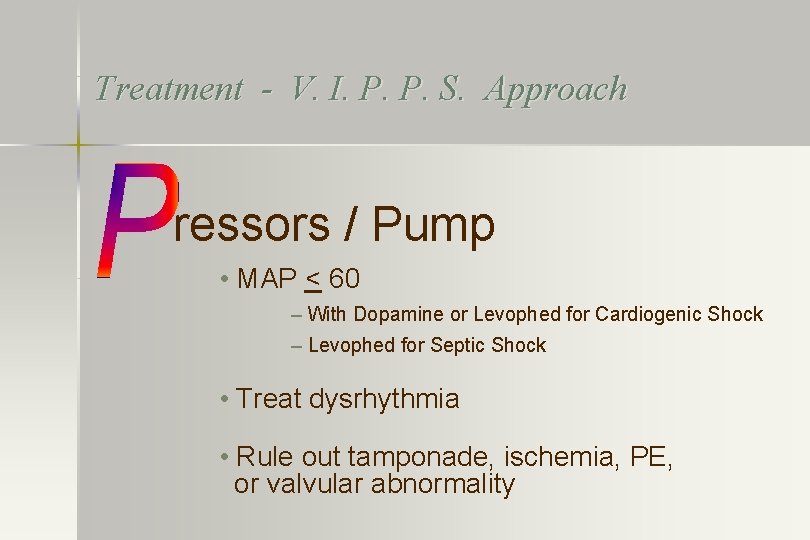
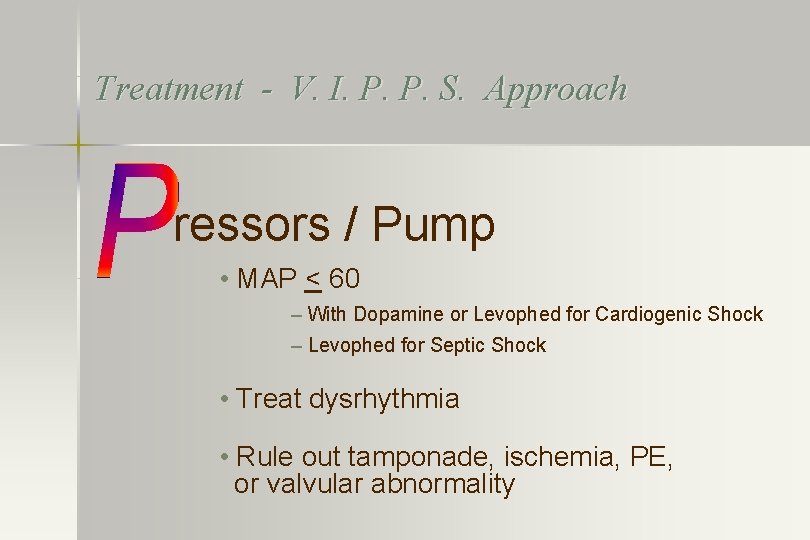
Treatment - V. I. P. P. S. Approach ressors / Pump • MAP < 60 – With Dopamine or Levophed for Cardiogenic Shock – Levophed for Septic Shock • Treat dysrhythmia • Rule out tamponade, ischemia, PE, or valvular abnormality
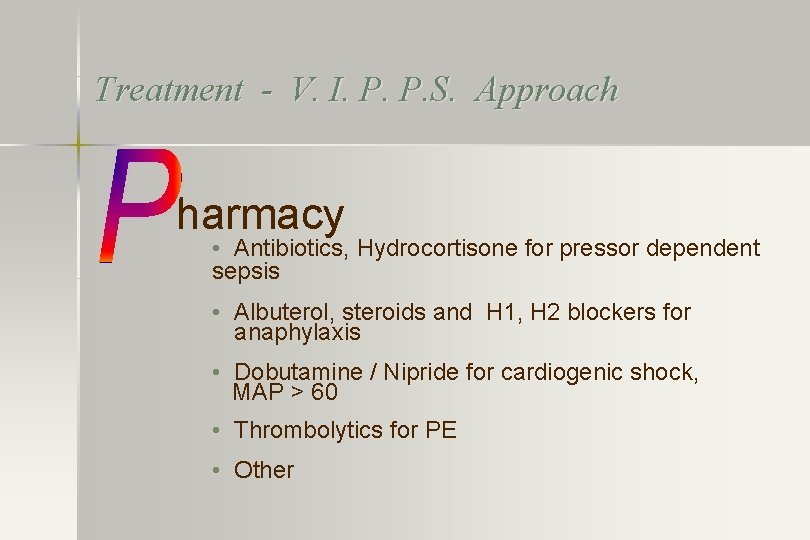
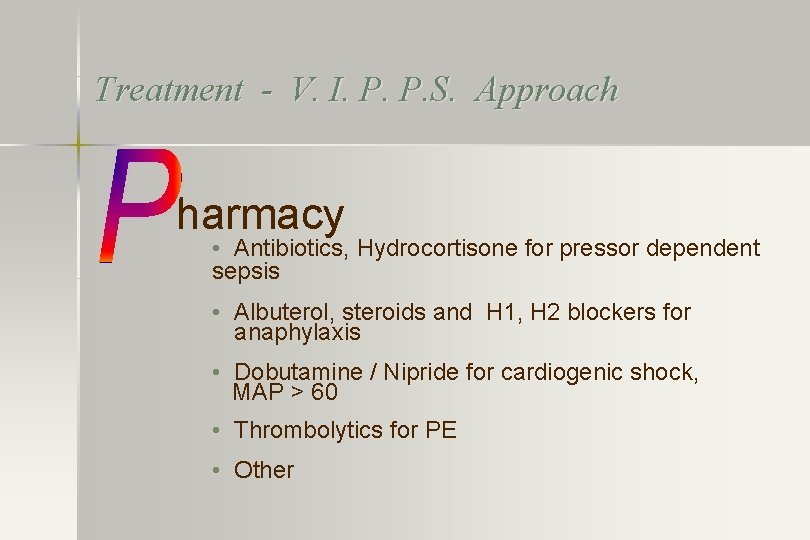
Treatment - V. I. P. P. S. Approach harmacy • Antibiotics, Hydrocortisone for pressor dependent sepsis • Albuterol, steroids and H 1, H 2 blockers for anaphylaxis • Dobutamine / Nipride for cardiogenic shock, MAP > 60 • Thrombolytics for PE • Other
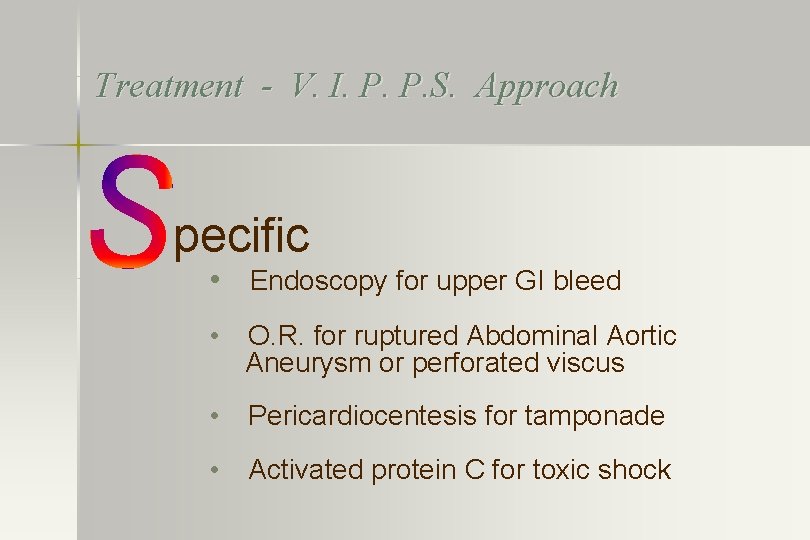
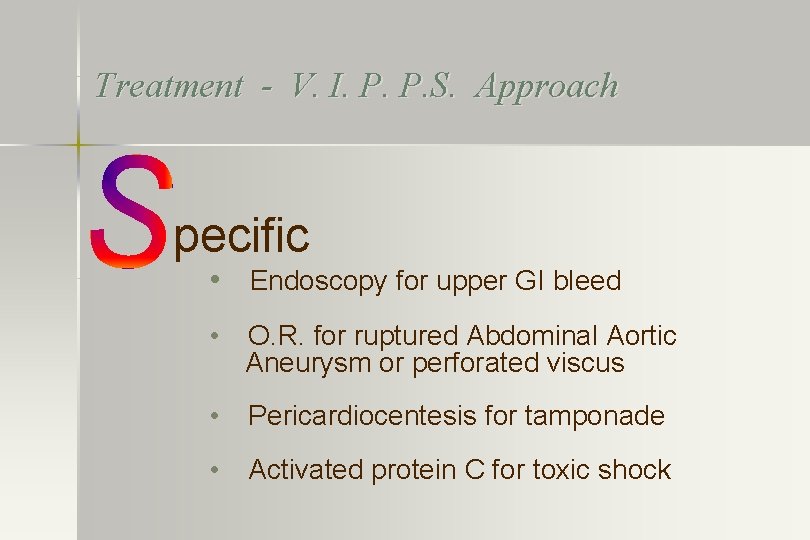
Treatment - V. I. P. P. S. Approach pecific • Endoscopy for upper GI bleed • O. R. for ruptured Abdominal Aortic Aneurysm or perforated viscus • Pericardiocentesis for tamponade • Activated protein C for toxic shock
Key Points of Shock Program • Early recognition • Rapid Response by Team • Early / Aggressive Application of Best Practice • Rapid transfer to ICU or O. R.
Study Methods • Control Group were patients who came into Redding Medical Center between 1998 and June 2000 who qualified by inclusion / exclusion criteria • Intensive education and implementation of protocols and mock shock alerts during June 2000 • Treatment Group were all patients who qualified by inclusion/exclusion criteria starting July 1, 2000


Results
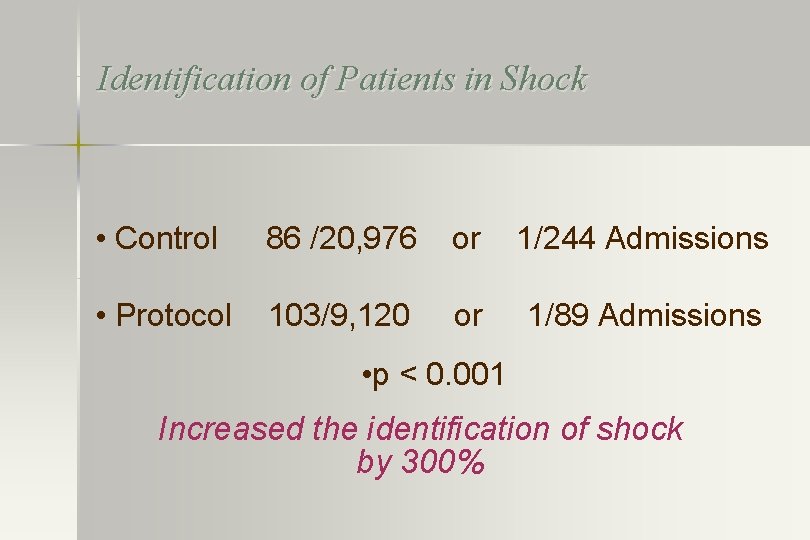
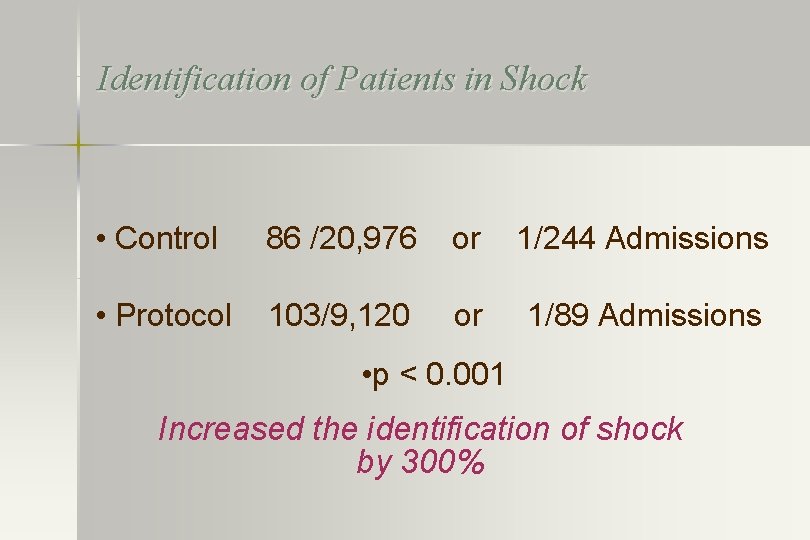
Identification of Patients in Shock • Control 86 /20, 976 or 1/244 Admissions • Protocol 103/9, 120 or 1/89 Admissions • p < 0. 001 Increased the identification of shock by 300%
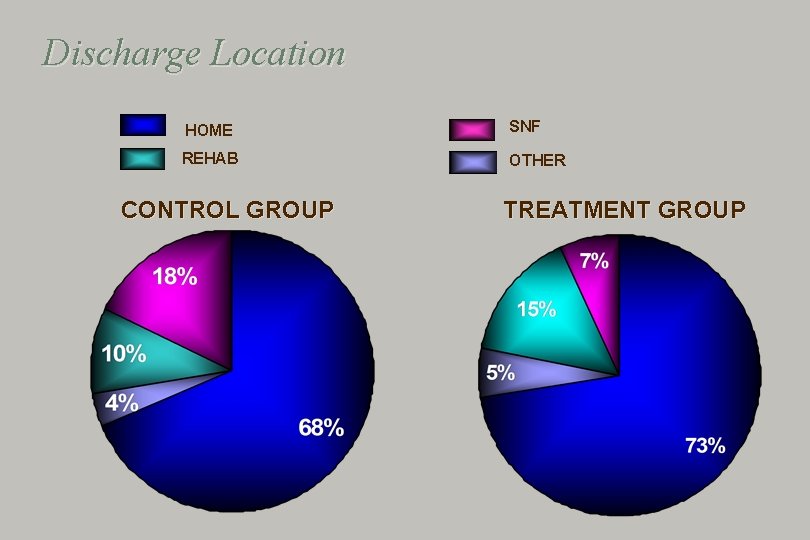
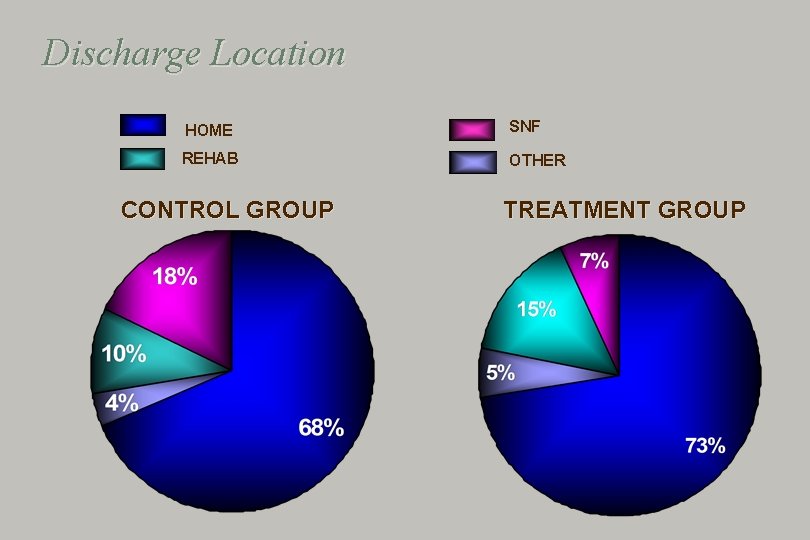
Discharge Location HOME SNF REHAB OTHER CONTROL GROUP TREATMENT GROUP
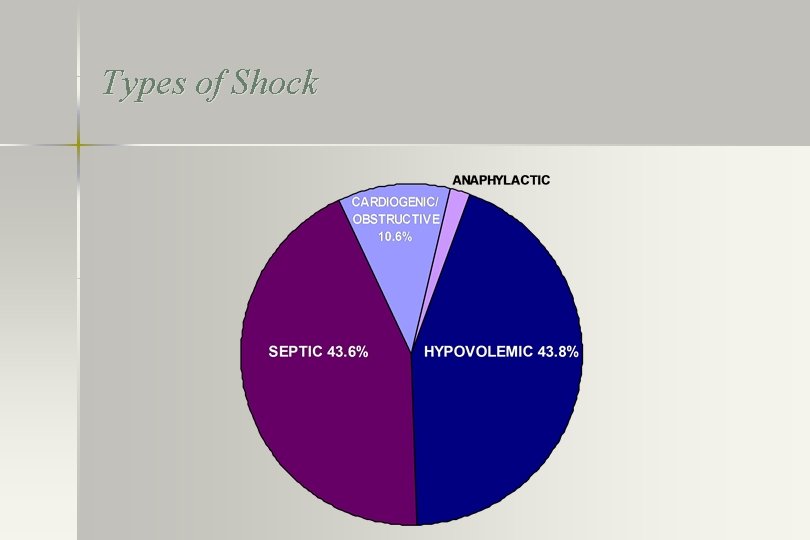
Types of Shock
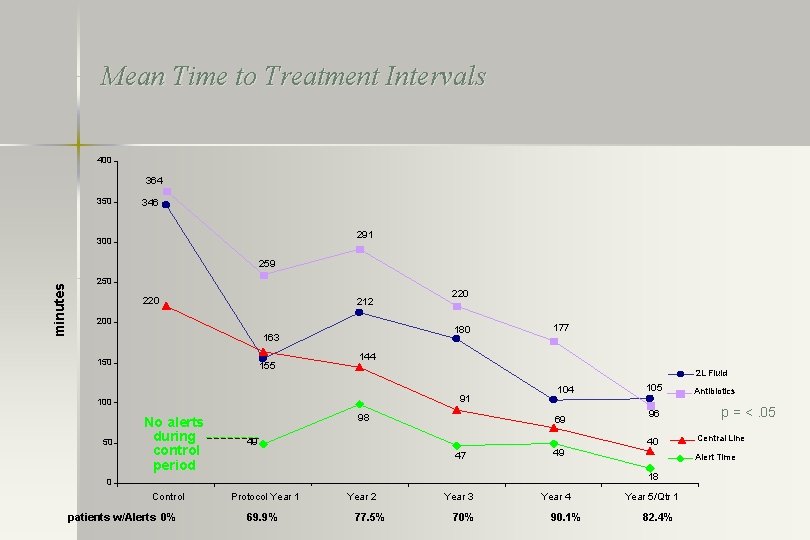
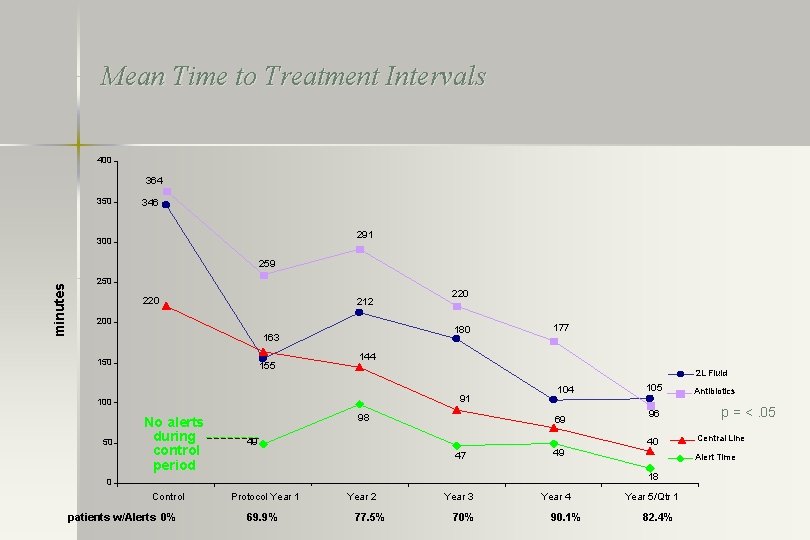
Mean Time to Treatment Intervals 400 364 350 346 291 300 minutes 259 250 220 212 200 180 163 150 155 2 L Fluid 91 No alerts during control period 177 144 100 50 220 98 104 69 49 patients w/Alerts 0% 96 40 47 49 Protocol Year 1 69. 9% Year 2 77. 5% Year 3 70% Year 4 90. 1% Antibiotics p = <. 05 Central Line Alert Time 18 0 Control 105 Year 5/Qtr 1 82. 4%
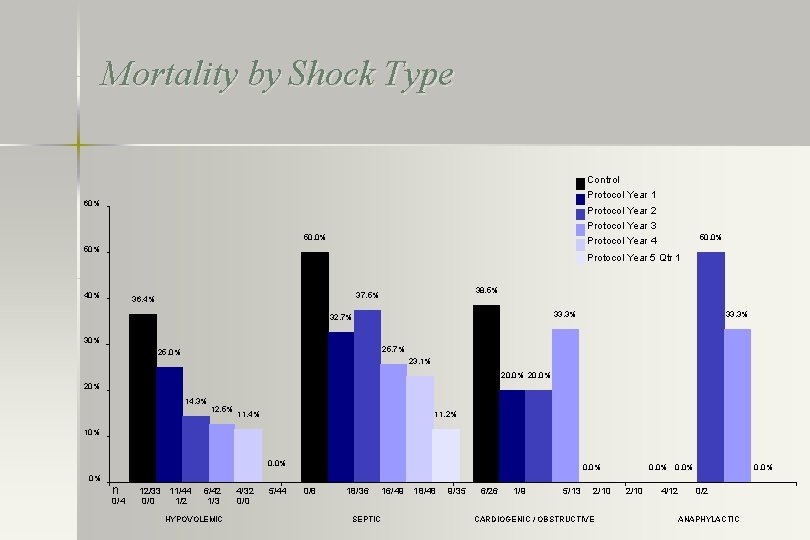
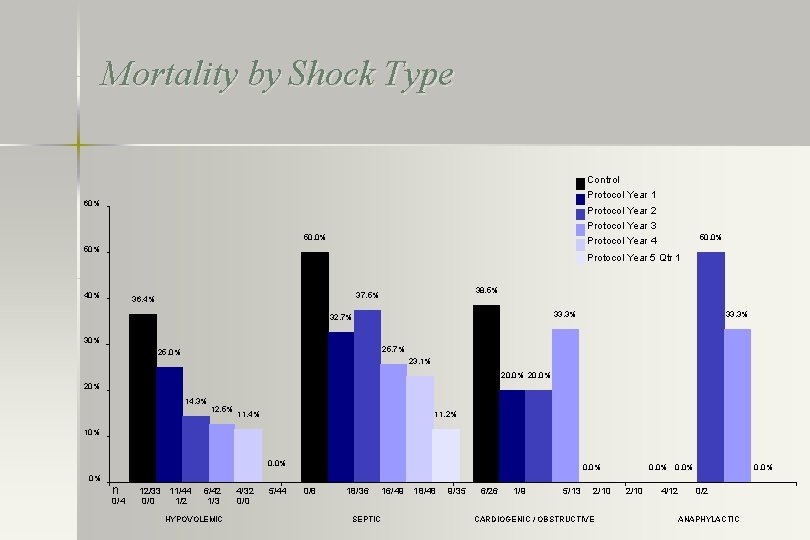
Mortality by Shock Type Control Protocol Year 1 60% Protocol Year 2 Protocol Year 3 50. 0% Protocol Year 4 50% Protocol Year 5 Qtr 1 40% 38. 5% 37. 5% 36. 4% 33. 3% 32. 7% 30% 33. 3% 25. 7% 25. 0% 23. 1% 20. 0% 20% 14. 3% 12. 5% 11. 2% 11. 4% 10% 0. 0% 0% n 0/4 12/33 11/44 0/0 1/2 6/42 1/3 HYPOVOLEMIC 4/32 0/0 5/44 0/8 18/36 SEPTIC 16/49 18/48 9/35 6/26 1/9 5/13 2/10 CARDIOGENIC / OBSTRUCTIVE 2/10 4/12 0/2 ANAPHYLACTIC
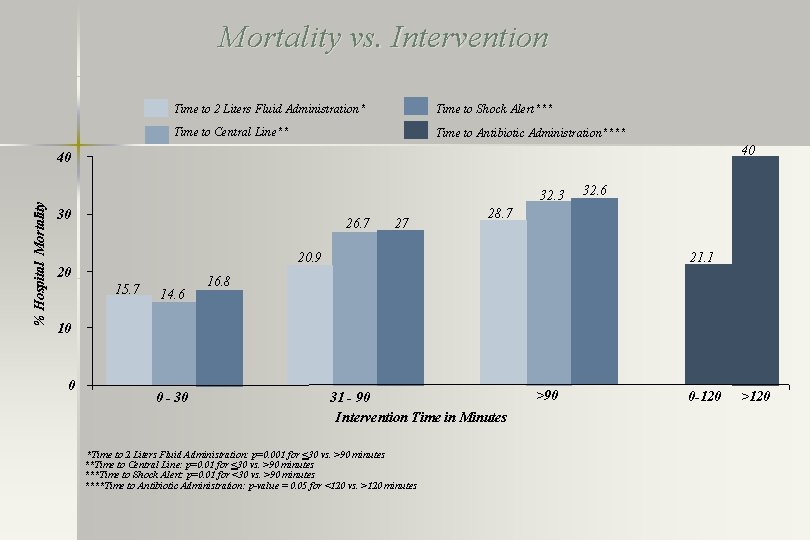
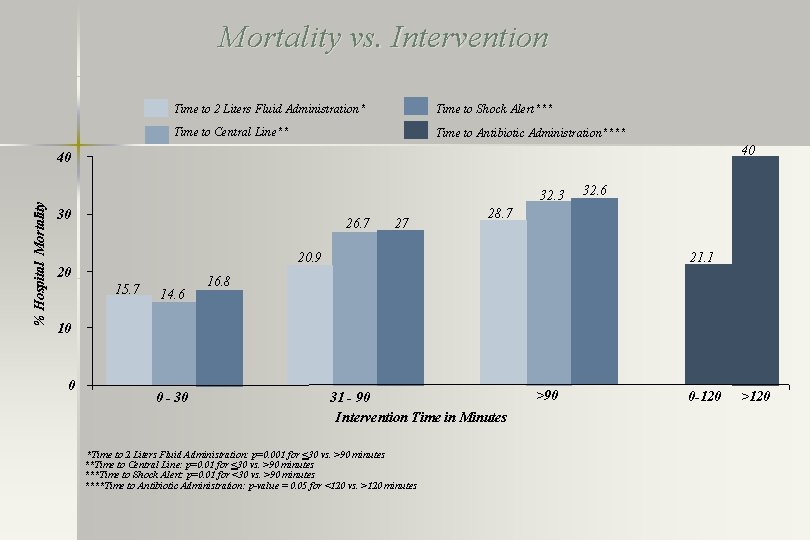
Mortality vs. Intervention Time to 2 Liters Fluid Administration* Time to Shock Alert*** Time to Central Line** Time to Antibiotic Administration**** 40 % Hospital Mortality 40 32. 3 30 26. 7 27 28. 7 21. 1 20. 9 20 15. 7 14. 6 32. 6 16. 8 10 0 0 - 30 31 - 90 Intervention Time in Minutes *Time to 2 Liters Fluid Administration: p=0. 001 for <30 vs. >90 minutes **Time to Central Line: p=0. 01 for <30 vs. >90 minutes ***Time to Shock Alert: p=0. 01 for <30 vs. >90 minutes ****Time to Antibiotic Administration: p-value = 0. 05 for <120 vs. >120 minutes >90 0 -120 >120
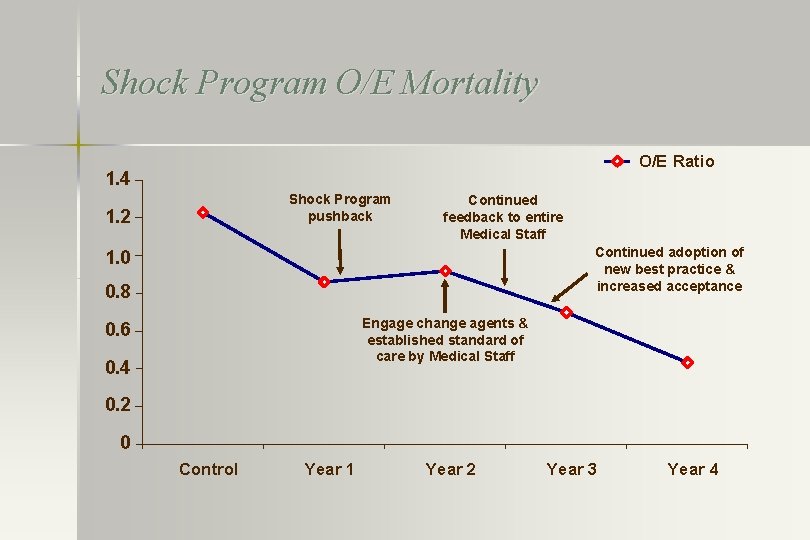
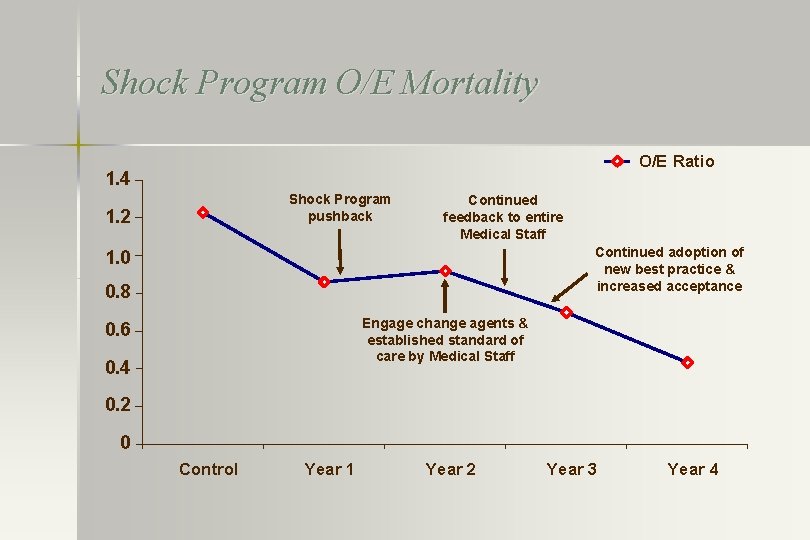
Shock Program O/E Mortality O/E Ratio 1. 4 Shock Program pushback 1. 2 Continued feedback to entire Medical Staff Continued adoption of new best practice & increased acceptance 1. 0 0. 8 Engage change agents & established standard of care by Medical Staff 0. 6 0. 4 0. 2 0 Control Year 1 Year 2 Year 3 Year 4
Conclusion • A comprehensive educational program and systems approach to early identification shock resulted in: – Early recognition – Rapid initiation of protocol driven goal directed treatment – Decreases the time to the initiation of fluids, antibiotics, intensivist involvement and ICU arrival – Decreases time to hemodynamic optimization – Decrease mortality
 Pada tahap analisis tugas kritikus adalah
Pada tahap analisis tugas kritikus adalah Ciri-ciri kritik
Ciri-ciri kritik Kritikus sikertényezők
Kritikus sikertényezők Kritikus út kiszámítása
Kritikus út kiszámítása Cara menutup cerita membuat pembaca mengulang kembali
Cara menutup cerita membuat pembaca mengulang kembali Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Spinal shock symptoms
Spinal shock symptoms Hangman fracture
Hangman fracture Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Diferencia entre shock medular y shock neurogenico
Diferencia entre shock medular y shock neurogenico Double positive t cells
Double positive t cells Dengue shock syndrome
Dengue shock syndrome Pile foundation details
Pile foundation details Composition of urine
Composition of urine Rainbow cause and effect
Rainbow cause and effect What type of communication is a poster
What type of communication is a poster Where does “snowflake girl” help to deliver presents
Where does “snowflake girl” help to deliver presents Section 15-3 darwin presents his case answers
Section 15-3 darwin presents his case answers A text that presents both side of the topic
A text that presents both side of the topic Prose writing that presents and explains ideas
Prose writing that presents and explains ideas Pear paragraph structure
Pear paragraph structure A thesis statement presents
A thesis statement presents Pour cet immense bonheur alléluia
Pour cet immense bonheur alléluia This presents
This presents Zids and zods answers
Zids and zods answers Shcedules
Shcedules Prose writing that presents and explains ideas
Prose writing that presents and explains ideas Business agility metrics
Business agility metrics Which sentence presents a faulty either/or argument?
Which sentence presents a faulty either/or argument? A dramatic work that presents the downfall of a character
A dramatic work that presents the downfall of a character Thesis main idea
Thesis main idea Sue palmer skeletons
Sue palmer skeletons Tragedy
Tragedy Zids and zods
Zids and zods 16 3 darwin presents his case answer key
16 3 darwin presents his case answer key Chapter 17 neurologic emergencies
Chapter 17 neurologic emergencies Structure in drama
Structure in drama A 26 year old female presents
A 26 year old female presents Zids and zods
Zids and zods Presents from my aunts in pakistan poem
Presents from my aunts in pakistan poem Triad of death
Triad of death Ahmad gaber
Ahmad gaber Types of haemorrhage
Types of haemorrhage Golden hour politrauma
Golden hour politrauma Speric shock
Speric shock Diabetic coma
Diabetic coma Compensated shock
Compensated shock Shock bundle
Shock bundle Secondo shock petrolifero
Secondo shock petrolifero Navmat p-9492
Navmat p-9492 Ync shock
Ync shock Progressive stage of shock
Progressive stage of shock Chapter 17 providing first aid
Chapter 17 providing first aid Jesuit handbook on lycanthropic culture shock
Jesuit handbook on lycanthropic culture shock Osmotic shock
Osmotic shock Aortrix
Aortrix Anaphylactic shock hemodynamics
Anaphylactic shock hemodynamics