2 Fluid Management in Dengue Hemorrhagic Fever Dengue





- Slides: 39
2. Fluid Management in Dengue Hemorrhagic Fever Dengue Expert Advisory Group
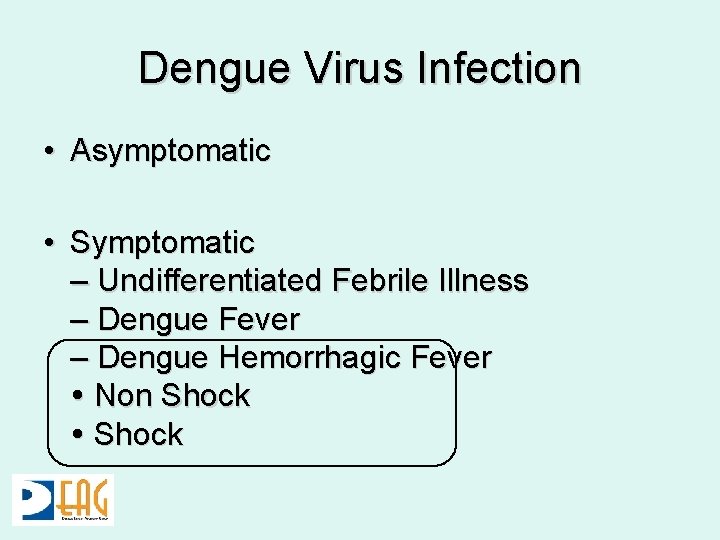
Dengue Virus Infection • Asymptomatic • Symptomatic – Undifferentiated Febrile Illness – Dengue Fever – Dengue Hemorrhagic Fever Non Shock
Dengue Hemorrhagic Fever • Febrile Phase • Critical phase characterized by plasma leak • Convalescent Phase
Dengue “Leak” Fever • Plasma leak during critical phase is the hall mark • Leading to 3 rd space losses – peritoneal cavity – pleural cavity • Variable in magnitude and exact timing
Pathogenesis of leak • Infection with a virulent dengue virus • Presence of antibodies that enhance dengue virus infection (ADE) • Intense immune activation
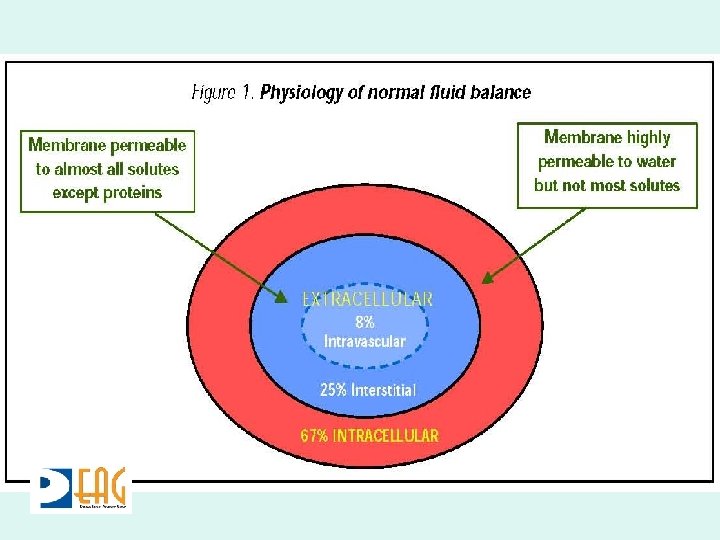
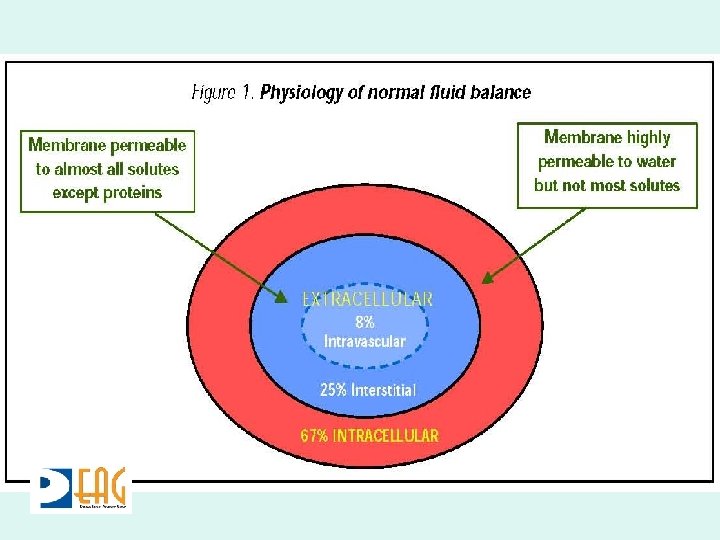
Pathogenesis • Rapidly elevated cytokines (TNF-a, IL-2, IL -6, IL-8, IL-10, IL-12, and IFN-g) • Malfunction of vascular endothelial cells • Plasma leakage from intra to extravascular space
Pathogenesis • In severe DHF the loss of plasma is critical • Patient becomes hypovolaemic • Signs of circulatory compromise • Progress to shock, organ failure, death
Pathogenesis • Cytokine Storm • Self limited • Ends after 48 hours
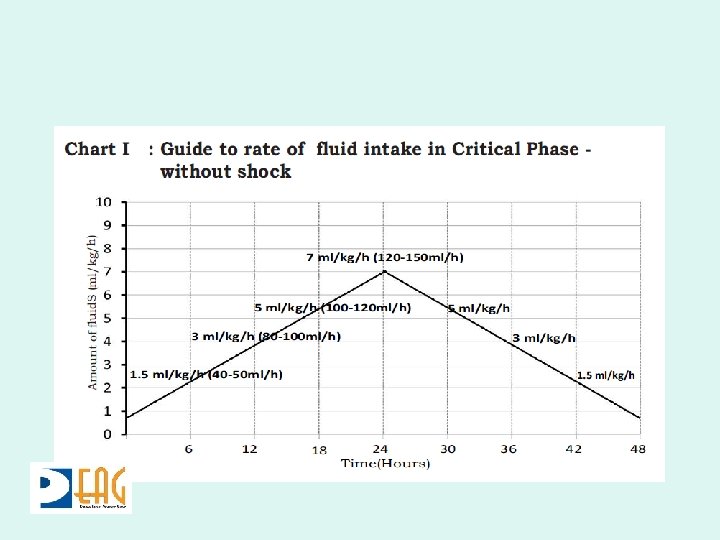
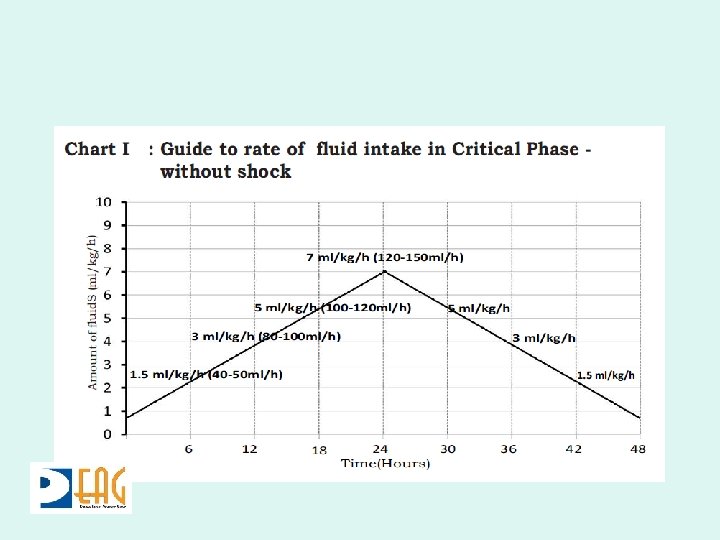
Clinical Implications • Extravascular fluid loss at variable rate that has to be matched ml for ml • Lasting 48 hours • Resorption of fluid during convalescent phase
Key Points • Manage critical phase with appropriate volume – Don’t under transfuse – Don’t over transfuse • Meticulous monitoring during critical phase to match rate of fluid infusion with rate of leak
Monitoring Parameters • Clinical – Pulse Rate – Blood and Pulse Pressure – Capillary Refill Time – Urinary Output • Lab – Hematocrit
Fluid Management Critical Phase
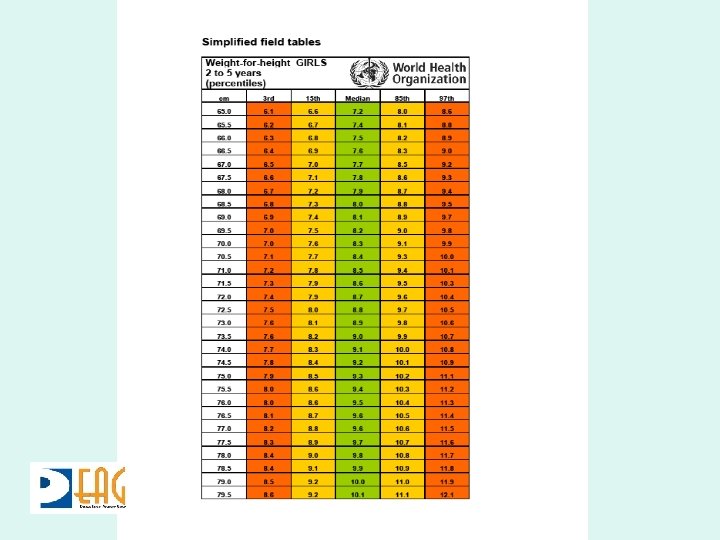
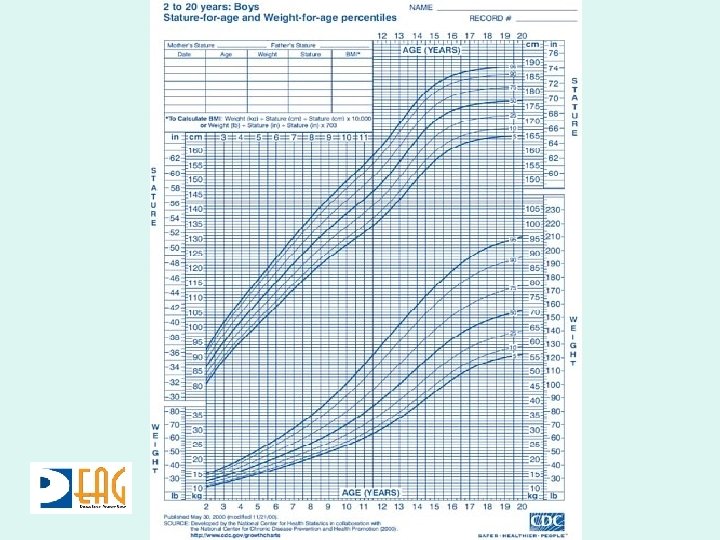
Amount of Fluid? • Based on weight • Adults – If less than 50 kg use actual weight – If more take weight as 50 kg • Paediatrics – Current OR Ideal body weight whichever is lower

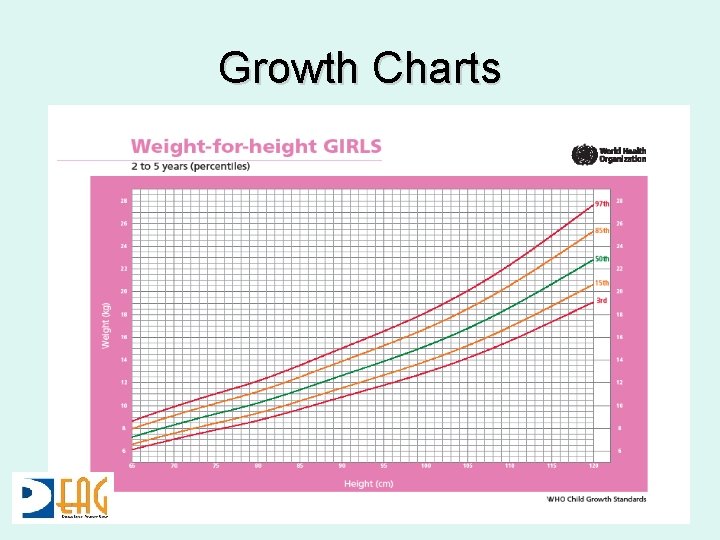
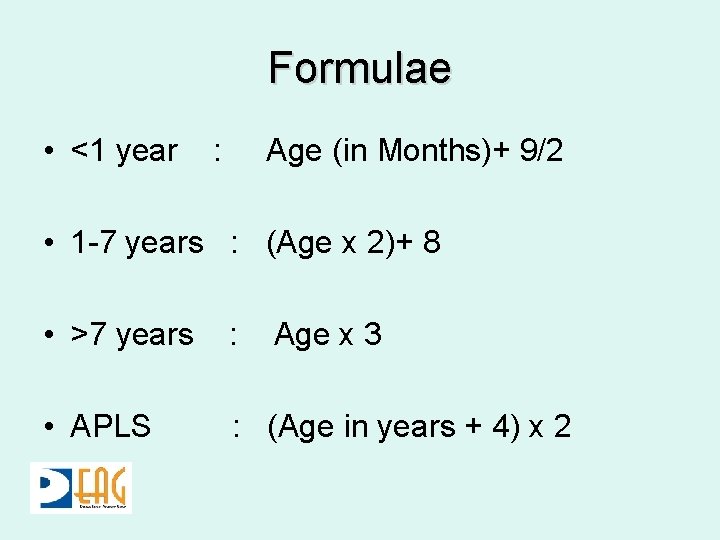
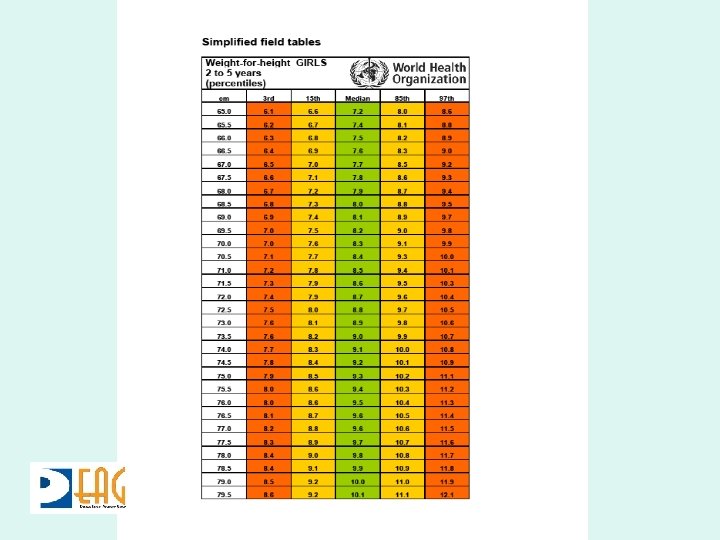
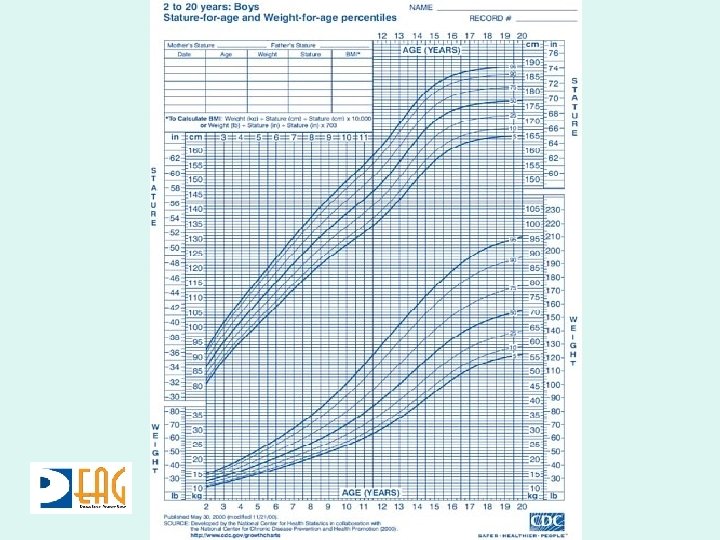
Ideal Body Weight • Weight for height using a growth chart • Weight for age • Formulae in emergency
Growth Charts
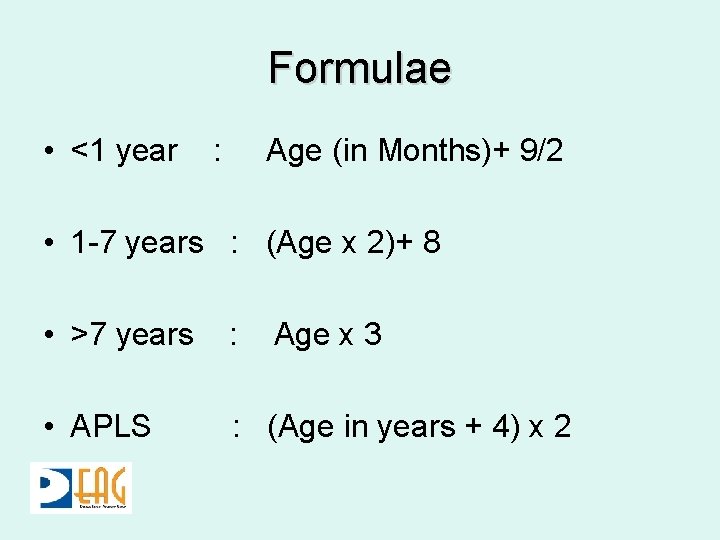
Formulae • <1 year : Age (in Months)+ 9/2 • 1 -7 years : (Age x 2)+ 8 • >7 years : • APLS : (Age in years + 4) x 2 Age x 3
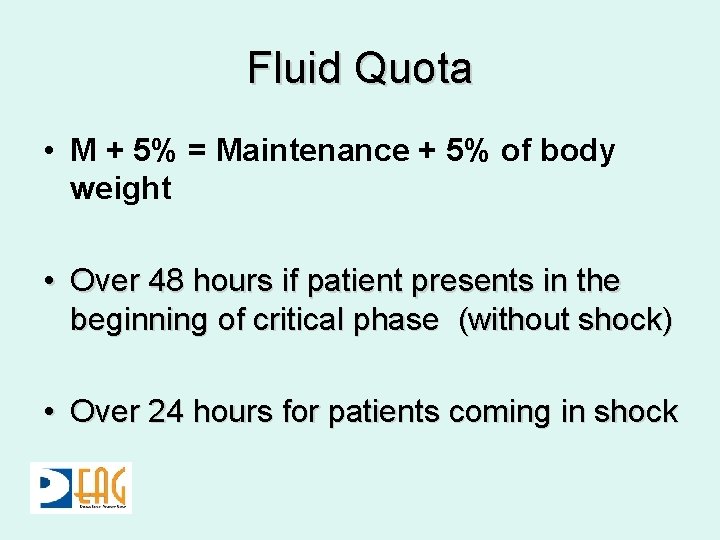
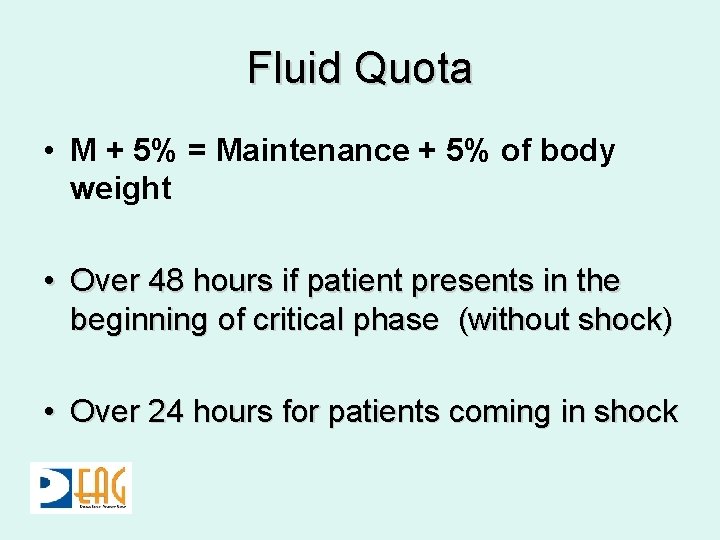
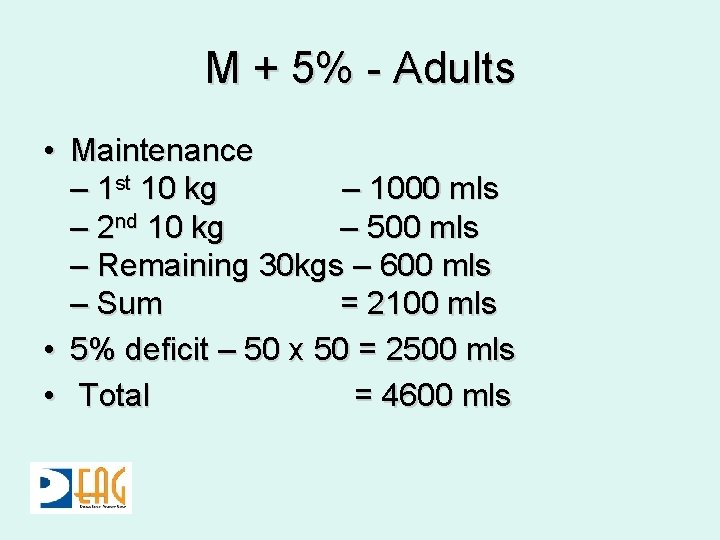
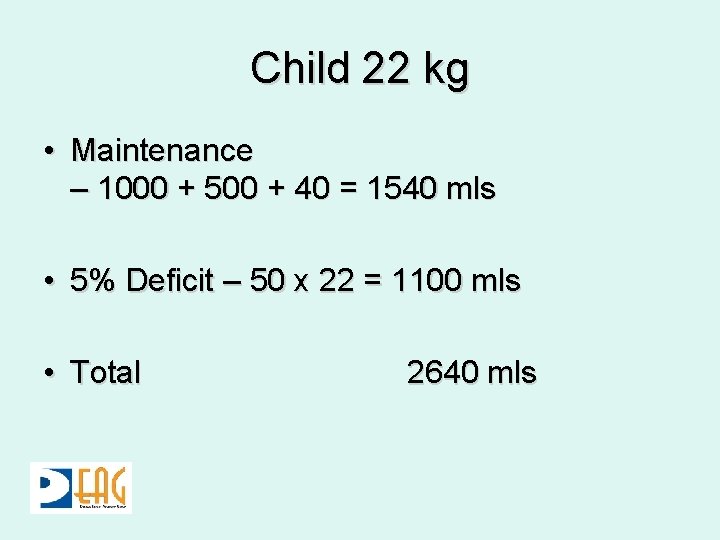
Fluid Quota • M + 5% = Maintenance + 5% of body weight • Over 48 hours if patient presents in the beginning of critical phase (without shock) • Over 24 hours for patients coming in shock

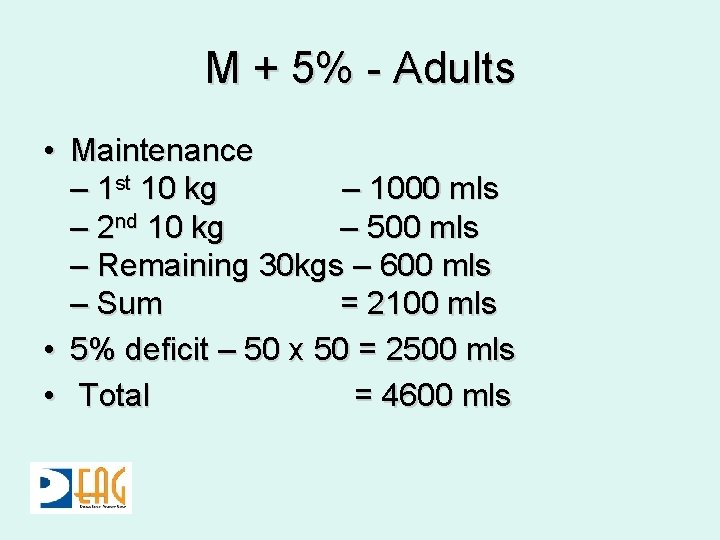
M + 5% - Adults • Maintenance – 1 st 10 kg – 1000 mls – 2 nd 10 kg – 500 mls – Remaining 30 kgs – 600 mls – Sum = 2100 mls • 5% deficit – 50 x 50 = 2500 mls • Total = 4600 mls
Child 22 kg • Maintenance – 1000 + 500 + 40 = 1540 mls • 5% Deficit – 50 x 22 = 1100 mls • Total 2640 mls
Types of Fluid • Crystalloids – 0. 9% Saline – 5%Dextrose 0. 9% Saline – 5% Dextrose ½ saline
Monitoring – Critical Phase • Vital parameters - hourly • Fluid balance chart - assess three hourly • HCT - six hourly
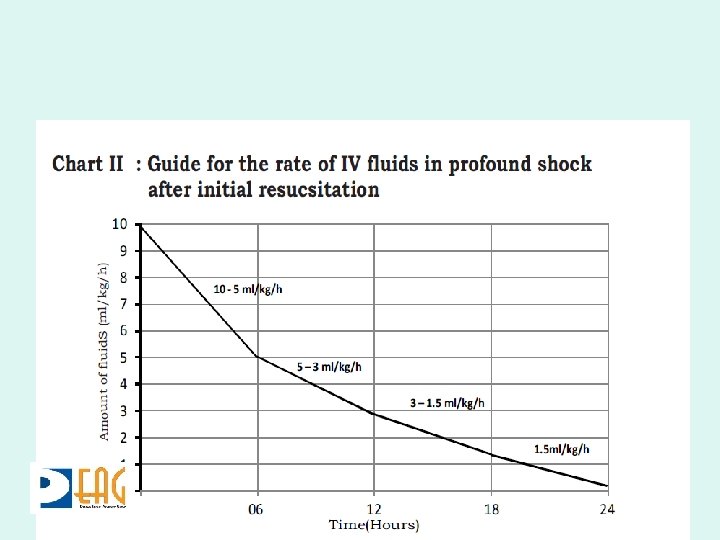
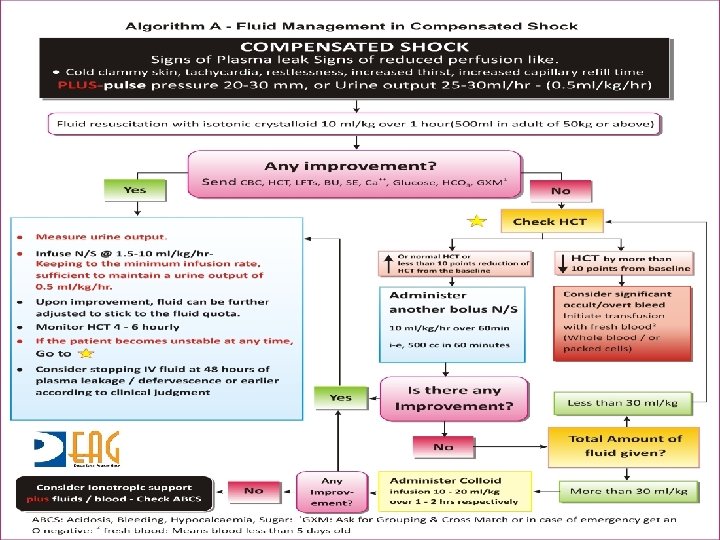
Fluid Management in Dengue Shock Syndrome

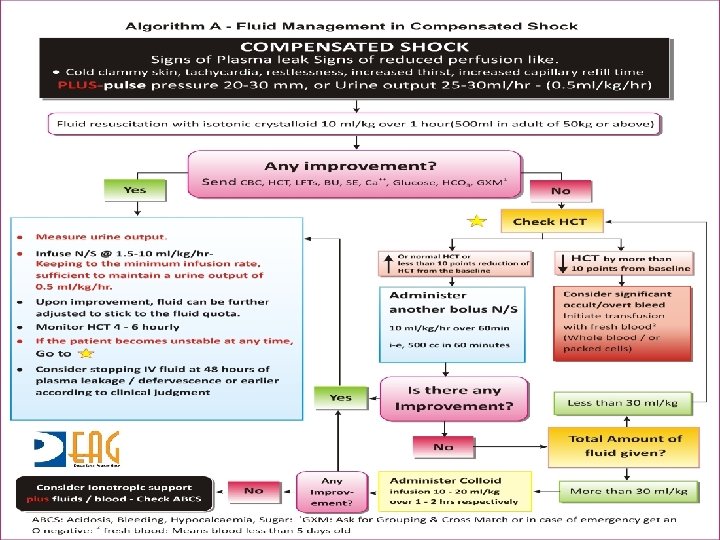
Compensated • Body compensates for fluid loss • • Tachycardia Pulse Pressure narrows Prolonged CRT Fall in urine output to 0. 5 mls/kg/hr
Decompensated • Pulse pressure narrows further leading to unrecordable pulse and BP • Urine output falls less than 0. 5 mls/kg/hour • Supply to myocardium and brain compromised
Fluid Resuscitation • Crystalloids – N Saline • Colloids – Dextran 40 in saline – 6% Starch • All boluses part of fluid quota
Indications for Colloid • Failure of crystalloid boluses to normalize pulse /BP • Development of shock – with fluid overload – amount of fluid exceeding M + 5% deficit • 10 ml/kg over 1 hour

Colloids • Dextran may sometimes interfere with grouping and cross matching • 3 doses of Dextran 40 during a 24 hour • 5 doses of 6% Starch during 24 hour • Remain in circulation for much longer

Refractory Shock - ABCS • Blood – packed cells – whole blood • Bicarbonate • Glucose • Calcium
Monitoring During Shock • 15 minute monitoring of vital signs • HCT immediately before and after each fluid bolus and then at least two to four hourly
Key Points – Managing DHF • Recognizing the start of critical phase of DHF • Predicting the rate of leak which may vary from patient to patient and within the same patient • Matching the rate of infusion to rate of leak • Being cognizant of the end of critical
Key Points – Managing DSS • Meticulous monitoring • Switching appropriately from crystalloids to colloids • Recognizing need for blood transfusion
 Causes of viral hemorrhagic fever
Causes of viral hemorrhagic fever Hantavirus humans
Hantavirus humans Pathogenesis dengue fever
Pathogenesis dengue fever Phase of dengue fever
Phase of dengue fever Lowgrade fever
Lowgrade fever Reactionary hemorrhage definition
Reactionary hemorrhage definition Atls classes of hemorrhagic shock
Atls classes of hemorrhagic shock Ischemic vs hemorrhagic stroke
Ischemic vs hemorrhagic stroke Hemorrhagic diathesis
Hemorrhagic diathesis Antihemorrhagic vitamin is
Antihemorrhagic vitamin is Necrotizing fasciitis hemorrhagic bullae
Necrotizing fasciitis hemorrhagic bullae Abdominal ultrasound scan glasgow
Abdominal ultrasound scan glasgow Andy rekito
Andy rekito Hypovolemic shock classification
Hypovolemic shock classification What is acute hemorrhagic pancreatitis
What is acute hemorrhagic pancreatitis Stages of hemorrhagic shock
Stages of hemorrhagic shock Clinical manifestation of epistaxis
Clinical manifestation of epistaxis Viscoseal
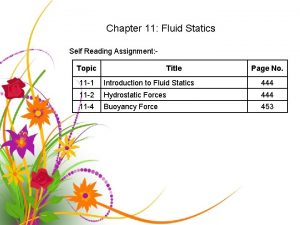
Viscoseal Fluid statics deals with fluid at rest
Fluid statics deals with fluid at rest Fluid statics deals with fluid at rest
Fluid statics deals with fluid at rest Total body water
Total body water Intracellular extracellular fluid
Intracellular extracellular fluid Interstitial fluid vs extracellular fluid
Interstitial fluid vs extracellular fluid Fluid kinematics example
Fluid kinematics example Extracellular fluid and interstitial fluid
Extracellular fluid and interstitial fluid Mild ascites symptoms
Mild ascites symptoms Fever chart project management
Fever chart project management Historia natural de la enfermedad del dengue
Historia natural de la enfermedad del dengue Criterios diagnosticos dengue
Criterios diagnosticos dengue Dengue duo
Dengue duo Etapas del dengue comezón
Etapas del dengue comezón Dengue monitoring chart
Dengue monitoring chart Dengue shock syndrome
Dengue shock syndrome Surah al an'am ayat 16 and 17 for dengue
Surah al an'am ayat 16 and 17 for dengue Taksonomi virus dengue
Taksonomi virus dengue Haemaccel in dengue
Haemaccel in dengue Symptoms dengue
Symptoms dengue Abcd dengue
Abcd dengue Dengue fisiopatologia
Dengue fisiopatologia Dengue
Dengue